SYNOPSIS
Objectives
Integration of surveillance for sexually transmitted diseases (STDs), human immunodeficiency virus (HIV), hepatitis, and tuberculosis (TB) may improve disease prevention and control. We determined the extent of surveillance integration in these programs, the benefits of integration, and barriers to increased integration.
Methods
We e-mailed a survey to the 58 federally funded local and state STD control programs and followed up with phone interviews of nine program representatives.
Results
The response rate was 81%. Many had compared infections by population subgroup for STDs and HIV (89%), STDs and hepatitis (53%), or STDs and TB (28%). Most (74%) had examined co-infections with HIV and STDs at the individual level and entered STD and HIV surveillance data into the same database (54%). All respondents thought some integration would be useful. Many (72%) used integrated data to disseminate information or change program strategies. The most commonly reported barriers to integration were policies preventing work with HIV data (85%) and incompatible databases (59%).
Conclusions
Most STD control programs in the United States have some experience integrating surveillance data, but the degree of integration varies widely. Specific barriers to further integration were identified. The Centers for Disease Control and Prevention can help address these barriers by facilitating access to information and sharing technical solutions. Local and state programs can continue advancing surveillance integration by improving understanding of where integrated data are needed, increasing the use of available data, and pressing for appropriate and secure data sharing.
Public health surveillance is “the ongoing systematic collection, analysis, and interpretation of outcome-specific data for use in planning, implementation, and evaluation of public health practice.”1 In the United States, surveillance systems generally focus on specific diseases and do not integrate information about different diseases at individual or population levels. This silo approach to disease surveillance has several benefits (e.g., data collection tailored appropriately to different disease processes, logistical simplicity based on following the organization of programs, funding, and subject matter expertise),2 but this approach has disadvantages as well. While many public health programs are organized around disease entities, most reporters of surveillance information (e.g., emergency room physicians and laboratories) are not. Redundancies and variation in data collection for different infections may create reporting burdens. In addition, individuals and populations are not limited in susceptibility to single diseases and can face multiple health threats with potentially synergistic effects. Some populations may be especially vulnerable to more than one infection. For example, men who have sex with men (MSM) and injection drug users (IDUs) have elevated incidences of sexually transmitted diseases (STDs), human immunodeficiency virus (HIV), and hepatitis; immigrants may face higher risks for tuberculosis (TB) and hepatitis; and prisoners are at risk for STDs, HIV, and TB.
Separate surveillance systems may lead to missed opportunities to prioritize effective interventions. For example, other STDs may facilitate HIV transmission.3 Bacterial STDs among HIV-infected individuals suggest recent unprotected sex and can help identify where interventions might prevent new HIV infections. Co-infection alters treatment recommendations because of changes in clinical course and effects of treatment on drug resistance. These issues may be particularly important in international settings where limited resources for testing and clinical management mean country-specific regimens for HIV treatment are implemented without knowledge of other infections. Integrated surveillance might guide more effective and efficient public health action. Because STDs, HIV, and hepatitis can be spread by the same behaviors and limited by similar prevention messages and activities, public health resources (e.g., testing, counseling, and partner services) may be pooled. New services could also be offered for people with repeated or multiple infections. Such individuals may compose core groups among whom interventions would be most efficient in preventing new infections.
Program collaboration and service integration for different infections is a priority for the Centers for Disease Control and Prevention's (CDC's) National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention.4 Several state and local programs have already integrated STD, HIV/AIDS, hepatitis, and/or TB prevention and control activities within the same administrative and programmatic infrastructure.2,5–7
The Outcome Assessment through Systems of Integrated Surveillance (OASIS) workgroup was established to promote innovative surveillance methods among STD programs, including integrated interpretation and use of surveillance data to improve public health programs.8 It is not known how many STD programs use integrated surveillance to guide program activities or how comprehensively surveillance is integrated within different programs. Providing effective, appropriately integrated services requires data about overlapping infections in each community. For example, there is evidence that adults seen in STD clinics are at sufficiently high risk for hepatitis B to justify vaccination;9 whether screening all STD clinic patients for hepatitis C is efficient depends on local data.10 Some questions may be resolved by limited special studies. However, for responsive interventions to evolving epidemics, and for continuing evaluation of interventions, ongoing surveillance is needed. We sought to determine the current level of surveillance integration in local STD control programs, to learn when integration has been useful, and to identify barriers to increased integration.
METHODS
Survey design
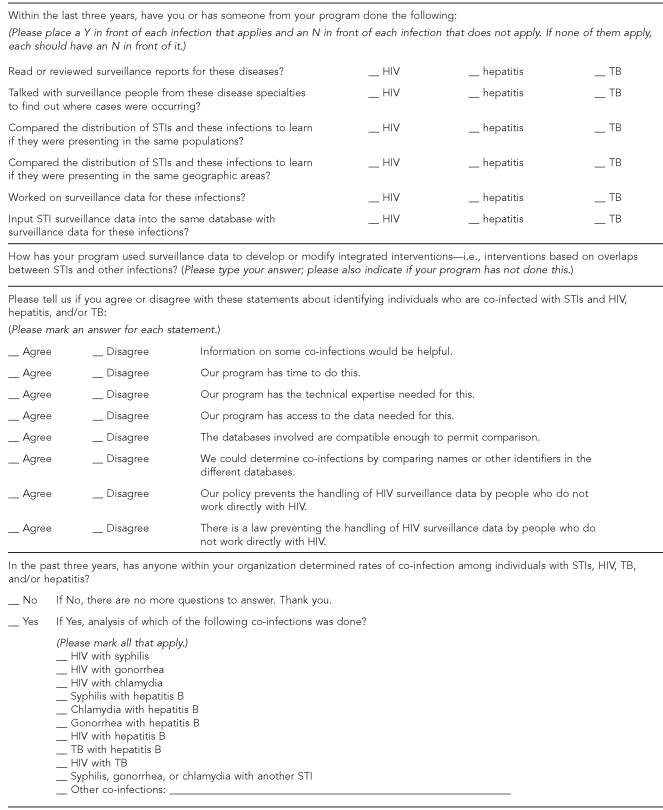
We developed a survey to elicit the scope and frequency of integrated surveillance activities, perceived usefulness, and barriers to further integration within the three years prior to the survey (Figure 1). The survey asked specific questions about determination and reporting of different infections in groups and individuals, usefulness and dissemination of integrated information, and potential barriers to integrated surveillance, including time, expertise, database compatibility, and data security concerns. For most questions, respondents were prompted to choose among different answers. One question about use of integrated surveillance information requested a free-text response.
Figure 1.
Survey questions asked of program directors of federally funded local and state STD programs, September–October 2007
STD = sexually transmitted disease
HIV = human immunodeficiency virus
TB = tuberculosis
STI = sexually transmitted infection
Distribution
We e-mailed our survey on September 14, 2007, to program directors of 58 federally funded local and state STD programs in the U.S. The program director or anyone designated by the program director and knowledgeable about that program's STD surveillance system could answer the survey. Surveys were returned by e-mail or fax. We collected surveys through October 11, 2007.
Evaluation of responses
We calculated proportions of programs that were engaged in different integrated surveillance activities, disseminated information based on integrated surveillance, and reported various potential barriers to integration. We determined the level of surveillance integration for each program using the following definitions:
Nonintegrated.
Surveillance systems for different infections (i.e., STDs, HIV, hepatitis, and TB) are separate.
Limited integration.
Surveillance systems are separate, but data from specific populations or geographic areas are compared to guide public health interventions.
Expanded integration.
Separate data sources are matched to determine rates of co-infection or multiple infections at the individual level.
Comprehensive integration.
Data about different infections are routinely reported within the same database. Integrated surveillance (defined as annually, or more frequently, for the last three years) routinely informs public health practice.
In determining these levels, we considered integration of STD surveillance with surveillance for HIV, hepatitis, and/or TB. Programs that had compared data but had not used those comparisons for interventions, evaluations, or dissemination of information were considered to be nonintegrated.
In addition, we categorized STD programs according to program factors including burden of disease in the program's area (high burden defined as ≥100 cases of primary and secondary [P&S] syphilis in 2007), and by the administrative association between STD and HIV programs. We used program name as a marker for administrative association. Programs with both HIV and STD in their name, or with a general name under which both HIV and other STDs would be included, were considered to be administratively related. We identified associations among integration activities, program factors, and perceived barriers to integration using Chi-square tests with a two-sided significance level of p<0.05.
Follow-up phone survey
We interviewed representatives of nine programs to verify that our questions were understood as intended. We chose programs from each of the four levels of surveillance integration (as determined by analysis of completed surveys), programs with high and low P&S syphilis burden, and programs with and without HIV included in their name. We asked representatives how co-infections were determined, recorded, and analyzed. We also asked about specific barriers to integration and the relative importance of those barriers. Questions were developed with input from members of the OASIS workgroup.
RESULTS
Eighty-one percent (47/58) of programs responded to the survey, all by e-mail. Among the respondents were 14 program directors, 11 program managers, eight public health advisors, five surveillance coordinators, and nine others. According to program name, 23 STD programs were administratively related to HIV programs. Twenty-seven programs that responded had at least 100 P&S syphilis cases reported in their area in 2007. There were no significant differences between programs that did and did not respond to the survey by U.S. census region11 or by number of P&S syphilis cases reported in 2007.
Integration activities
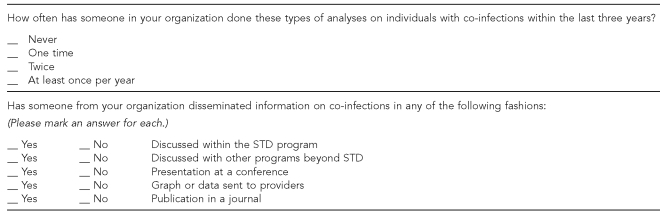
Overlaps in disease incidence by population subgroups had been evaluated by 89% of programs for STDs and HIV, 53% for STDs and hepatitis, and 28% for STDs and TB (Figure 2). Comparisons of incidence by geographic region were reported by 85% for STDs and HIV, 43% for STDs and hepatitis, and 26% for STDs and TB. Most programs (74%) had examined co-infections of STDs and HIV at the individual level; only 6% had done this for STDs and hepatitis, and none for STDs and TB. Surveillance data for STDs and for HIV were entered into the same database by 54% of programs; 11% had done this for STDs and hepatitis, and 11% for STDs and TB. According to our designated levels of integration, 21% of programs were nonintegrated, 28% had limited integration, 26% had expanded integration, and 26% had comprehensive integration. Level of integration was not significantly associated with U.S. region or with reporting more than 100 cases of P&S syphilis in 2007. Most (70%) of the 37 programs with at least limited surveillance integration were integrated for STDs and HIV only. Sixteen percent had integrated surveillance for STDs, HIV, and hepatitis; 5% for STDs, HIV, and TB; and 8% for all four disease categories.
Figure 2.
Percentages of federally funded state and local STD programs (n=47) that assessed co-infections with STD and HIV, hepatitis, or TB, by type of assessment, September–October 2007
STD = sexually transmitted disease
HIV = human immunodeficiency virus
TB = tuberculosis
At the individual level, programs monitored HIV co-infection among patients with syphilis (74%), gonorrhea (38%), chlamydia (36%), hepatitis B (15%), and hepatitis C (6%). Many programs (34%) had looked at co-infection with multiple STDs (e.g., chlamydia, gonorrhea, and syphilis). Some programs (4%) determined co-infection with syphilis and hepatitis B. Other co-infections were analyzed by one program each: chlamydia and hepatitis B, gonorrhea and hepatitis B, gonorrhea and hepatitis A, and HIV and hepatitis A. U.S. census region was not significantly associated with determination of co-infections. Programs that reported at least 100 cases of P&S syphilis in 2007 were more likely to have determined occurrence of any co-infections than programs that reported fewer cases of syphilis (93% vs. 60%, p=0.006).
Usefulness of integrated surveillance
All survey respondents thought that some integration would be useful. Seventy-two percent reported that their integrated surveillance activities had been useful. Forty percent of programs had disseminated data from integrated surveillance at a conference, 38% had sent reports to providers, and 15% had published information.
Integrated surveillance led to changes in program operations. One program used mobile vans for STD and HIV screening, with locations determined based on spatial analysis of co-infection data. The program offered HIV tests to males older than age 30 years who were diagnosed with gonorrhea, based on a match of STD and HIV databases. Another program adapted inSPOT, an Internet-based technology to help individuals with STDs notify their partners,12 based on risks reported by men with co-infections and repeat infections. One program implemented hepatitis A and B vaccines in STD clinics after surveillance data demonstrated higher rates of hepatitis A and B among MSM and high-risk heterosexual populations.
Barriers to integrated surveillance
The most common barriers to further integration were policies that prevented use of HIV data (reported by 85% of respondents) and incompatibility of databases (59%). Other barriers included lack of program time (47%) or expertise (19%). Among STD programs that included HIV in their program name, 74% stated they had access to data needed to determine co-infections, while only 43% of those without HIV in their program name reported sufficient access (p-value for difference = 0.03). One program reported specific barriers related to data security concerns: “Although the technical issues have been eliminated, there is resistance both internal and external. .. [from CDC] for the STD program to have access to HIV data.”
Follow-up phone survey
All nine programs confirmed the scope and frequency of integration activities indicated on their e-mail survey. In particular, those programs that reported entry of multiple infections into the same database confirmed that this meant a database in which information was stored and could be linked at the individual level (e.g., entry of HIV information into the STD Management Information Systems13).
DISCUSSION
According to our survey, most STD control programs in the U.S. have had some experience with surveillance integration. The degree of surveillance integration at each program varied widely, as measured by level of granularity and frequency with which data were compared. Programs with at least 100 syphilis cases reported were most likely to have examined co- infections, suggesting that the public health importance of the syphilis and HIV overlap in a given area may have driven advances in integration. Alternatively, program resources may have made integration activities more feasible in larger programs. All respondents believed integration would be useful, and many respondents had used integrated surveillance data to disseminate information or to change program strategies. The two most commonly perceived barriers to further integration were (1) policies that restrict access to HIV data and (2) separate or incompatible data management systems.
Moving integration forward requires the development of mutually acceptable data security standards. Technical standards established by one program may be difficult for others to achieve. For example, CDC's Technical Guidance for HIV/AIDS Surveillance Programs14 lists 34 requirements for data security and confidentiality, many of which are followed by STD and other programs or could be easily incorporated. However, one physical security recommendation—installing a computer in a separate, secure area not connected to the Internet—may be difficult for small programs with limited space and funding. Revised data security guidelines were published in “Recommendations for Partner Services Programs for HIV Infection, Syphilis, Gonorrhea, and Chlamydial Infection” in Morbidity and Mortality Weekly Reports in 2008.15 These simplified guidelines list requirements that may be easier for smaller programs to follow. Other challenges to integration include technical issues, such as how to match cases on an individual level when identifiers do not match exactly.16
For most programs, increasing integration will require resources, including time to develop compatible systems or to cross-match information from different datasets. There is also a risk of losing appropriate focus for individual diseases.17 In some cases, integration of surveillance may not be efficient. For example, while STDs and TB both affect populations with lower socioeconomic status, and control efforts rely on overlapping strategies (such as contact tracing and antibiotic therapy), different modes of transmission might mean little overlap between these infections at the individual level. While some respondents to our survey had compared information from surveillance for STDs and TB, only one reported using that information (to flag HIV-positive individuals suspected of also having TB when they presented to the STD clinic).
However, in many cases, integrated surveillance has led to more effective and efficient public health interventions. For example, programs have alerted HIV care providers to increases in HIV/syphilis co-infection and the potential need for more education on symptom recognition and prevention. One of the principles of electronic health records is the ability to maintain collective medical data for an individual that will enable providers to make better decisions. When combining information leads to more effective interventions, it may be argued that it is unethical to keep surveillance data separate.
Limitations
The results of our survey are subject to several limitations. Our response rate was 81%; programs that did not respond may have been less likely to have integrated surveillance, and so the degree of surveillance integration may be overestimated. We may have overestimated the extent of surveillance integration if respondents interpreted questions differently than we intended. However, results from our follow-up phone survey indicated that programs were at least at the level of integration determined by our e-mail survey.
We may have underestimated surveillance integration activities if respondents did not know about all surveillance activities in their program. Our survey addressed surveillance system integration, but did not attempt to assess program integration more generally. However, we did ask about the use of integrated surveillance to inform program activities. Finally, because our survey was sent to STD control programs and was not designed to assess integration of surveillance for HIV and hepatitis, or HIV and TB, it can only be used to draw conclusions about integration of surveillance that involves STD control programs.
CONCLUSIONS
CDC can facilitate integration efforts by helping to minimize the barriers that currently exist. More than 10 years ago, a CDC/Agency for Toxic Substances and Disease Registry committee “reached a consensus that CDC needed to streamline and consolidate its public health surveillance and information systems into an integrated system.”18 The committee determined that elements needed to interconnect different systems included uniform “data standards, a communications infrastructure, and policy-level agreements regarding data access, sharing, and burden reduction.”19 CDC can eliminate separate and incompatible data reporting requirements. Some programs have developed compatible data management systems for STDs, HIV, and hepatitis surveillance that might be adapted by other programs.20 CDC could facilitate the sharing of technical solutions. CDC can also assist in the establishment of common, practicable data security standards, and can set an expectation of sharing necessary information appropriately and securely. CDC could allocate funds for specific needs related to informatics and data management. Finally, CDC could shift from categorical to more general funding.
This survey and other activities21–23 described in this issue of Public Health Reports show that local and state programs have often taken the lead in advancing surveillance integration. Local programs are best able to determine what is needed and what strategies are likely to work in their jurisdictions. Some STD and HIV surveillance systems have always been integrated, while others have intentionally integrated within the last 15 years to increase program efficiency. Administratively related programs have a significant advantage in terms of ability to access needed information. Other programs have developed innovations (such as computer software and matching programs) across separate programs because of a perceived need for integrated data to inform action. Some programs have encountered roadblocks because of data security concerns, especially related to HIV data. However, developing mutually acceptable data safeguards, asking for needed data, and educating other programs about usefulness of shared data will make it easier for other programs to successfully integrate data.
REFERENCES
- 1.Thacker SB, Berkelman RL. Public health surveillance in the United States. Epidemiol Rev. 1988;10:164–90. doi: 10.1093/oxfordjournals.epirev.a036021. [DOI] [PubMed] [Google Scholar]
- 2.National Alliance of State and Territorial AIDS Directors, National Coalition of STD Directors. STD/HIV prevention integration. Washington: NASTAD and NCSD; 2002. [cited 2009 Jun 2]. Also available from: URL: http://www.ncsddc.org/upload/wysiwyg/documents/STDHIVIssuePaperFinal.pdf. [Google Scholar]
- 3.Fleming DT, Wasserheit JN. From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Transm Infect. 1999;75:3–17. doi: 10.1136/sti.75.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (US), National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. An NCHHSTP green paper. Atlanta: CDC; July 2007. Program collaboration and service integration: enhancing the prevention and control of HIV/AIDS, viral hepatitis, and TB in the United States. [Google Scholar]
- 5.Delcher PC, Edwards KT, Stover JA, Newman LM, Groseclose SL, Rajnik DM. Data suppression strategies used during surveillance data release by sexually transmitted disease prevention programs. J Public Health Manag Pract. 2008;14:E1–8. doi: 10.1097/01.PHH.0000311902.95948.f5. [DOI] [PubMed] [Google Scholar]
- 6.Fox Fields H. The integration of HIV/AIDS, STD, and TB prevention and control programs. Washington: Association of State and Territorial Health Officials; 1998. [Google Scholar]
- 7.Harris JL, Jones TS, Buffington J. Hepatitis B vaccination in six STD clinics in the United States committed to integrating viral hepatitis prevention services. Public Health Rep. 2007;122(Suppl 2):S42–7. doi: 10.1177/00333549071220S208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gaffga NH, Samuel MC, Stenger MR, Stover JA, Newman LM. The OASIS Project: novel approaches to using STD surveillance data. Public Health Rep. 2009;124(Suppl 2):1–4. doi: 10.1177/00333549091240S203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sexually transmitted diseases treatment guidelines 2002. MMWR Recomm Rep. 2002;51(RR-6):1–78. [PubMed] [Google Scholar]
- 10.Honeycutt AA, Harris JL, Khavjou O, Buffington J, Jones TJ, Rein DB. The costs and impacts of testing for hepatitis C virus antibody in public STD clinics. Public Health Rep. 2007;122(Suppl 2):S55–62. doi: 10.1177/00333549071220S211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.CDC (US) Sexually transmitted disease surveillance, 2007. Atlanta: CDC; 2008. [cited 2009 Jun 2]. Also available from: URL: http://www.cdc.gov/std/stats07/main.htm. [Google Scholar]
- 12.Internet Sexuality Information Services, Inc. InSpot. [cited 2009 Jun 2]. Available from: URL: http://www.inspot.org/gateway.aspx.
- 13.CDC (US) Sexually transmitted diseases: STD*MIS. [cited 2009 Jun 2]. Available from: URL: http://www.cdc.gov/std/std-mis.
- 14.CDC (US), Council of State and Territorial Epidemiologists. Technical guidance for HIV/AIDS surveillance programs, volume III: security and confidentiality guidelines. Atlanta: CDC; 2006. [Google Scholar]
- 15.Recommendations for partner services programs for HIV infection, syphilis, gonnorhea, and chlamydial infection. MMWR Recomm Rep. 2008;57(RR-9):1–83. [PubMed] [Google Scholar]
- 16.Newman LM, Samuel MC, Stenger MR, Gerber TM, Macomber K, Stover JA, et al. Practical considerations for matching STD and HIV surveillance data with data from other sources. Public Health Rep. 2009;124(Suppl 2):7–17. doi: 10.1177/00333549091240S203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wroten JE, Crockett LK, Kertesz C. Trial marriage: Florida's experience in consolidating HIV/AIDS, STD, and TB programs. Public Health Rep. 1999;114:74–80. doi: 10.1093/phr/114.1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morris G, Snider D, Katz M. Integrating public health information and surveillance systems. J Public Health Manag Pract. 1996;2:24–7. doi: 10.1097/00124784-199623000-00007. [DOI] [PubMed] [Google Scholar]
- 19.CDC (US), Agency for Toxic Substances and Disease Registry. Integrating public health information and surveillance systems. A report and recommendations from the CDC/ATSDR Steering Committee on Public Health Information and Surveillance System Development, spring 1995. [cited 2009 Feb 12]. Available from: URL: http://www.cdc.gov/nedss/Archive/katz.pdf.
- 20.Shiver SA, Schmitt K, Cooksey A. Use of a business approach to improve disease surveillance data management systems and information technology process in Florida's Bureau of STD Prevention and Control. Public Health Rep. 2009;124(Suppl 2):98–102. doi: 10.1177/00333549091240S214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jennings JM, Stover JA, Bair-Merritt MH, Fichtenberg C, Munoz MG, Maziad R, et al. Identifying challenges to the integration of of computer-based surveillance information systems in a large city health department: a case study. Public Health Rep. 2009;124(Suppl 2):39–48. doi: 10.1177/00333549091240S207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stenger MR, Courogen MT, Carr JB. Trends in Neisseria gonorrhoeae incidence among HIV-negative and HIV-positive men in Washington State, 1996–2007. Public Health Rep. 2009;24(Suppl 2):18–23. doi: 10.1177/00333549091240S204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chow JM, Kang M-S, Samuel MC, Bolan G. Assessment of the association of Chlamydia trachomatis infection and adverse perinatal outcomes with the use of population-based chlamydia case report registries and birth records. Public Health Rep. 2009;24(Suppl 2):24–30. doi: 10.1177/00333549091240S205. [DOI] [PMC free article] [PubMed] [Google Scholar]