Abstract
Young adulthood is a period renowned for engagement in impulsive and risky behaviors, including gambling. There are some indications that young adults exhibit higher gambling rates in comparison to older adults. Problem gambling has also been linked to ADHD. This longitudinal study examines the relationship between gambling and ADHD among an epidemiological sample of young adults (n = 235; males = 179, females = 56) aged 18–24. Results indicate that individuals who report childhood ADHD symptoms which persist into young adulthood experience greater gambling problem severity than participants with no ADHD or those with non-persistent ADHD.
Keywords: ADHD, Gambling, Young adulthood
Introduction
Gambling among adolescents and young adults is a widespread problem with a variety of psychological and public health implications (Kaminer and Petry 1999; Messerlian et al. 2005). In a recent meta-analysis of 146 prevalence studies, Shaffer and Hall (2001) found that roughly 8% of adolescents met criteria for being a Level 2 (problem) gambler in their lifetime, and an additional 3% met criteria for a Level 3 (pathological) gambling problem. Even higher rates were reported for gambling in college students, with nearly 10% qualifying as problem gamblers and 6% as pathological gamblers. The rates of disordered gambling are higher for these age groups than in the adult population (4% and 2%, respectively; Shaffer and Hall 2001). Although there is significant variation in prevalence rates across studies, researchers consistently find a higher prevalence of disordered gambling in adolescents and college students than adults (National Research Council 1999; Petry 2005).
Even more concerning than the high rates of adolescent and young adult gambling are the outcomes often associated with early gambling. Gambling activity during adolescence is related to higher frequencies of problem gambling in adulthood (Hardoon and Derevensky 2002). In addition, individuals who start to gamble during adolescence are more likely to develop severe gambling problems as an adult (Lynch et al. 2004; National Research Council 1999). Longitudinal studies have found that there is a more rapid progression from social gambling to problem gambling in adolescents as compared to adults (Gupta and Derevensky 1998).
Previous research has shown that pathological and problem gambling in college-age young adults is related to a higher incidence of many psychological disorders and psychosocial concerns. For example, addictive behaviors are the most frequently cited correlates of young adult gambling (Huang et al. 2007; LaBrie et al. 2003; Slutske et al. 2005; Winters et al. 1998), as are greater rates of depression and suicidal thoughts (Feigelman et al. 2006). Negative emotionality, a trait involving poor ability to cope with stress, anxiety, anger, and other emotions, was also found to be higher in young adult problem gamblers than in a control group of young adults (Slutske et al. 2005). Finally, several personality traits, including risk-taking (LaBrie et al. 2003; Slutske et al. 2005), sensation-seeking (Langewisch and Frisch 1998; Powell et al. 1999), intensity-seeking (Nower et al. 2004), and impulsivity (Nower et al. 2004; Slutske et al. 2005) are related to problem gambling in young adults.
Impulsivity and its relationship to gambling behaviors in particular has been heavily studied, though the results are mixed. Most studies found impulsivity to be associated with pathological and problem gambling in young adults (Langewisch and Frisch 1998; Lightsey and Hulsey 2002; Nower et al. 2004; Slutske et al. 2005), though other studies have not found this relationship (Barnes et al. 2005). The connection of impulsivity and gambling may be mediated by a mental disorder that frequently co-exists with impulsivity––Attention-Deficit/Hyperactivity Disorder (ADHD). ADHD includes symptoms that reflect the concept of impulsivity, such as difficulty waiting one’s turn, interrupting others, and blurting out answers before questions are completed (American Psychiatric Association 2000).
To date, only a handful of studies have examined the possible link of ADHD and problem gambling. Most of these studies have relied on retrospective data (Carlton and Manowitz 1992; Carlton et al. 1987) or have focused solely on current symptomology of gamblers in treatment (Specker et al. 1995). Derevensky et al. (2007) examined the relationship between impulsivity and gambling among adolescents and found that adolescents who reported problem gambling behaviors were more likely to have a greater number of ADHD symptoms.
However, no studies of which we are aware have attempted to link ADHD and young adult gambling based on the persistence of ADHD over time. Persistent ADHD may exert its effect through impulsive and poorly planned behaviors, including problem gambling. Remittent ADHD may have set in place various positive life strategies that remain despite the absence of impulsive symptoms. This study examines the association of gambling behaviors among young adults with their longitudinal history of ADHD.
Method
Participants
The young adults who took part in this study were participants in a longitudinal study of ADHD that began in 1991. The study, called the Minnesota Competence Enhancement Program (MnCEP), initially identified elementary school students between the ages of 7 and 11 who were screened for disruptive behavior (see August et al. 1995). The Conners’ Hyperactivity Index (HI-T, HI-P; Goyette et al. 1978) was administered to the students’ classroom teacher and parents. Those students who obtained scores of 1.75 standard deviations above the mean on both a teacher (HI-T) and parent (HI-P) report of hyperactivity were placed into the “disruptive” participant group (n = 318). Students with a HI-T and HI-P score below 1.0 SD above the normal mean were placed into the control group (n = 144). All students had IQ scores of 80 or above, based on the Kaufman Brief Intelligence Test (KBIT; Kaufman and Kaufman 1990) and had not been diagnosed with a pervasive developmental disorder. The sample was primarily Caucasian and middle-class (Hollingshead 1975), and the male/female ratio was approximately 4:1, consistent with the prevalence ratio for gender and ADHD (American Psychiatric Association 2000). The disruptive and control groups were not significantly different on demographic variables. Multiple follow up assessments were conducted on these students since the initial assessment, with the current sample comprising the seventh and most recent follow up assessment. A more detailed description of original study methodology is available in August et al. (1995).
For the current phase of the study, a sub-sample of these participants was re-assessed between the ages of 18 and 24 years. The mean age at administration was 20.2 (SD = 1.5). This sub-sample was selected largely for diagnostic reasons, to ensure that the disruptive participants met diagnostic criteria for ADHD and that the control sample was absent of any mental health diagnoses. Youth with a childhood diagnosis of ADHD were re-categorized using both their childhood and current young adult diagnosis of ADHD. Those participants who had an ADHD diagnosis as a child and as a young adult were placed into the “ADHD persisters” (n = 47) group to reflect the persistent nature of their diagnosis. Participants with a childhood diagnosis of ADHD, but not as an adult, were placed into the “ADHD desisters” group (n = 95) since their ADHD diagnosis appeared to desist. Participants who never met criteria for an ADHD diagnosis remained in the control group. Thus, our final sample size resulted in 235 participants (ADHD n = 142, Control n = 93). Further explanation of sample size and attrition is provided in the Attrition Analysis section.
There were no significant differences among the three groups (ADHD persisters, ADHD desisters and controls) in terms of their age at assessment, gender, ethnicity, IQ, or socioeconomic status of their parents. However, significant differences were found for their high school graduation status. In this case, the control group had a higher percentage of high school graduates, followed by the ADHD desisters and ADHD persisters, respectively (χ2 = 8.11, P <.05). Complete demographic information is provided in Table 1.
Table 1.
Demographic data (n = 235)
| ADHD persisters (n = 47) |
ADHD desisters (n = 95) |
Controls (n = 93) |
|||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Male | 40 | 85.1 | 75 | 78.9 | 64 | 68.8 | 5.24 (non-sig) |
| Caucasian | 43 | 91.5 | 89 | 93.7 | 91 | 97.8 | 12.06 (non-sig) |
| HS Graduation | 38 | 80.9 | 86 | 90.5 | 89 | 95.7 | 8.11* |
| Mean (SD) | Mean (SD) | Mean (SD) | |||||
| Mean age | 20.0 (1.4) | 20.4 (1.4) | 19.9 (1.5) | 2.97 (non-sig) | |||
| KBIT composite score (baseline) |
101.9 (21.3) | 101.9 (11.7) | 107.2 (1.6) | 2.79 (non-sig) | |||
| Parent SES (baseline) |
46.6 (10.3) | 46.8 (11.6) | 50.3 (10.5) | 2.86 (non-sig) | |||
P < .05
Measures
Childhood diagnosis of ADHD was obtained using the Revised Parent Version of the Diagnostic Interview for Children and Adolescents (DICA-R; Reich et al. 1992) and was administered by trained assessment technicians. A battery of instruments was also administered at the baseline assessment, one of which was the Behavioral Assessment System for Children and Adolescents (BASC; Reynolds and Kamphaus 1992), which was briefly used for an exploratory analysis in this follow-up. Young adult DSM-IV diagnosis of ADHD was obtained using a revised, DSM-IV based structured interview, the Adolescent Diagnostic Interview (ADI; Winters and Henly 1993). The demographic portion of the ADI was also used to obtain employment outcomes. Further data were obtained using the Brief Symptom Inventory (BSI; Derogatis 1975) to measure mental health outcomes, and the Personal Experience Inventory (PEI; Henly and Winters 1989) to measure legal difficulties. DSM-IV-based items of antisocial personality disorder were administered as well (Murphy 1992).
Gambling behavior was assessed with the South Oaks Gambling Screen- Revised for Adolescents (SOGS-RA; Winters et al. 1993). The SOGS (Lesieur and Blume 1987) is associated with extensive reliability and validity evidence (Stinchfield 2002; Volberg and Banks 1990; Weinstock et al. 2007). We adjusted the gambling frequency items to reflect the prior 12 months rather than the participant’s lifetime, and the gambling participation variable consisted of any prior year involvement in card games, the lottery, slot/gambling machines, horse/dog racing, sports betting, dice games, bingo, the stock market, or games of personal skill. In addition, we derived two gambling problem severity variables from the SOGS-RA: count of the number of SOGS-RA problem severity items (range, 0–12) and breakdowns of gambling problem severity groups (social gamblers, 0–1; possible problem gamblers (PPGs), 2+) based on suggestions from previous research (Winters et al. 1993; Carlson and Moore 1998). Carlson and Moore (1998) reported that a “narrow” definition of problem gambling, consisting of a score of 4 or more on the SOGS-RA, may be too conservative of an estimate for adolescents because it may underestimate the number of youth that many would consider problem gamblers in an anecdotal or clinical setting. Their definition of gamblers who score 2 or 3 on the SOGS-RA was defined as those who have some familial, social, or financial difficulties associated with their gambling, but not enough to be considered a significant problem. Carlson and Moore (1998) estimated that approximately 5% of the adolescent population score in this 2–3 range, whereas only 1% scored 4 or more on the SOGS-RA. Because there is no single agreed-upon method for defining problematic gambling, we chose this broader gambling severity breakdown so we could capture this population who are showing early signs of problem gambling behavior, as well as those who already exhibit problem gambling.
Procedure
Informed consent was obtained before the assessments were completed. The structured interviews were primarily conducted in person; however, some participants who could not meet due to location or availability issues were interviewed over the telephone. Participants were paid $75 for their participation in the study, which included completing a large battery of measures at a single timepoint as part of the larger MnCEP study. Interviews took approximately one hour and were administered by trained interviewers with a Bachelor’s or Master’s degree in Psychology or a related field.
Statistical Analyses
All statistical analyses were conducted using Statistical Package for the Social Sciences (SPSS) version 12.0. ANOVAs were conducted to compare the group means on all outcome variables, including several mental health screens, legal issues, and employment status. Chi-squares were also conducted for non-parametric data. MANOVAs and MANCOVAs provided a measure of the effect of gambling on psychosocial variables when co-varied by ADHD status in moderating analyses. These moderating analyses were conducted to help determine the strength of the relationship, or the interaction, between ADHD and gambling severity when psychosocial variables were used as outcome measures. Intercorrelations and a Sobel test were used in mediating analyses to examine how baseline variables (i.e., IQ, SES, and level of impulsivity) affected the relationship between gambling severity and ADHD symptomology. Linear regression analyses were also conducted to determine the relationship between ADHD and gambling outcomes. The regression analyses revealed no significant findings and are not reported in the results section.
Attrition Analysis
At the original assessment in 1991, 318 disruptive children and 144 control children were included in the study (n = 462). Subsequent follow-ups yielded attrition due to parental refusal to participate (n = 127; 101 disruptive children and 26 control children). Those families were not contacted to participate in this follow-up portion of the longitudinal study based on their previous refusal. Of the remaining 335 participants, 13 passively declined (e.g. did not return calls, repeatedly missed appointments, or could not be found), 13 actively declined (i.e. communicated disinterest in participation), and 5 were in the military and unable to be reached. Thus, the original MnCEP sample that remained consisted of 304 participants.
Of the 304 participants who were eligible for this extension of the MnCEP study, 69 (55 disruptive and 14 control) did not meet criteria for inclusion in the sub-sample. For the control sample, all 14 ineligible participants were excluded because they were found to have a psychiatric diagnosis of ADHD, an internalizing disorder, or an externalizing disorder at least once during the course of the longitudinal study. In regards to the ineligible disruptive sample, 46 participants were excluded due to a lack of an ADHD diagnosis across all childhood assessments, and nine were excluded due to an excess (more than 10%) of omitted responses. Thus, the final sample size for this analysis was 235. A 2 × 2 chi-square was conducted (2 levels of eligibility versus 2 disruptive types) to measure the statistical difference between the groups and the results indicate that significantly more disruptive participants were ineligible for inclusion in the sub-sample (χ2 (4, N = 235) = 11.7, P = .008).
Results
Gambling Frequency
The three ADHD status groups did not differ in terms of their gambling participation (see Table 2). Approximately 79% of the ADHD persisters reported gambling in the past year, along with 77% of the ADHD desisters. In the control group, approximately 80% reported past-year gambling activity. There was no significant difference in the prevalence rate among the groups (χ2 (2, N = 235) = .21, P = .899). No significant differences were found when examining the mean number of types of games played (i.e. playing cards with friends, purchasing lottery tickets, etc.) either.
Table 2.
Gambling participation and problem severity by ADHD status
| ADHD persisters (n = 47) |
ADHD desisters (n = 95) |
Controls (n = 93) |
χ2/P value | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |||
| Gambling participation (n = 235) |
No gambling | 10 | 21.3 | 22 | 23.2 | 19 | 20.4 | 0.21(non-sig) |
| Any gambling | 37 | 78.7 | 73 | 76.8 | 74 | 79.6 | ||
| Gambling problem severity (n = 235) |
No gambling | 10 | 21.3 | 22 | 23.2 | 19 | 20.4 | 10.05* |
| Social gambling (SOGS-RA 0–1) |
28 | 59.6 | 68 | 71.6 | 69 | 74.2 | ||
| PPG (SOGS-RA 2+) | 9 | 19.1 | 5 | 5.3 | 5 | 5.4 | ||
| Gambling problem severity––gamblers only (n = 184) |
Social gambling (SOGS-RA 0–1) |
28 | 75.7 | 68 | 93.2 | 69 | 93.2 | 9.80** |
| PPG (SOGS-RA 2+) | 9 | 24.3 | 5 | 6.8 | 5 | 6.8 | ||
| Mean (SD) | Mean (SD) | Mean (SD) | ||||||
| SOGS-RA score | 0.5 (0.9) | 0.2 (0.6) | 0.2 (0.6) | 3.60* | ||||
| Count of games played |
3.0 (2.3) | 2.4 (2.3) | 2.7 (2.1) | 1.37 (non-sig) | ||||
P <.05;
P <.01
Gambling Problem Severity
However, significant differences were observed in regard to gambling problem severity. The ADHD persisters reported higher rates of gambling problem severity, including a higher mean SOGS-RA score and a higher percentage of possible problem gambling (PPG). Approximately 19% of ADHD persisters met criteria for possible problem gambling, while just 5% of the ADHD desisters and 5% of the controls met the criteria (χ2(4, N = 235) = 10.05, P = .04). No significant differences existed between the ADHD desisters and the control groups. An additional analysis of only those participants who reported past-year gambling revealed the ADHD persisters were significantly more likely to be categorized as possible problem gamblers (χ2 (2, N = 184) = 9.80, P = .007). Approximately 24% of ADHD persisters who gambled met PPG criteria, compared to 7% of the desisters and controls.
Psychosocial Functioning
Table 3 summarizes the psychosocial functioning variables that were examined among three gambling status groups: non-gamblers, social gamblers, and possible problem gamblers (PPGs). The PPGs consistently scored higher on legal problems in comparison with the other two groups, indicating the presence of more legal difficulties. In particular, they scored significantly higher on reports of “trouble with the law” (χ2(2, N = 235) = 7.59, P = .022) and on an overall count of legal problems (F(2, 234) = 3.29, P = .039). Regarding employment difficulties, the PPGs reported significantly more problems than the other groups on all employment items except for “frequent unemployment” (χ2(2, N = 235) = 5.18, P = .075).
Table 3.
Psychosocial functioning broken down by gambling severity groups (n = 235)
| Non-gamblers (n = 51) |
Social gamblers (n = 165) |
PPGs (n = 19) |
χ2/F | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Legal problems | |||||||
| Trouble with the law | 8 | 15.7 | 49 | 29.7% | 9 | 47.4 | 7.59* |
| Involved in criminal activities |
7 | 13.7 | 33 | 20.0% | 6 | 31.6 | 2.87 |
| Being arrested | 8 | 15.7 | 38 | 23.0% | 6 | 31.6 | 2.29 |
| Driving while intoxicated | 10 | 19.6 | 45 | 27.3% | 8 | 42.1 | 3.63 |
| Frequent physical fights | 3 | 5.9 | 17 | 10.3% | 2 | 10.5 | .93 |
| Count of legal problems | x̄ = .71 | SD = 1.3 | x̄ = 1.11 | SD = 1.47 | x̄ = 1.68 | SD = 1.8 | 3.29* |
| Employment problems | |||||||
| Frequent unemployment | 11 | 21.6 | 17 | 10.3% | 4 | 21.1% | 5.18 |
| Fired from several jobs | 0 | 0.0 | 8 | 4.8% | 3 | 15.8% | 7.77* |
| Being in large debt | 10 | 19.6 | 28 | 17.0% | 8 | 42.1% | 6.84* |
| Count of employment problems |
x̄ = .41 | SD = .64 | x̄.32 | SD = .60 | x̄ = .79 | SD = .79 | 4.94** |
| x̄ | SD | x̄ | SD | x̄ | SD | F | |
| Mental health (from BSI) | |||||||
| Depression | .44 | .72 | .31 | .43 | .33 | .43 | 1.325 |
| Anxiety | .31 | .43 | .31 | .40 | .36 | .33 | .125 |
| Hostility | .38 | .49 | .46 | .46 | .53 | .48 | .771 |
| Somatization | .18 | .36 | .23 | .37 | .17 | .27 | .453 |
| Obsession–compulsion | .56 | .60 | .60 | .49 | .84 | .54 | 2.211 |
| Interpersonal sensitivity | .40 | .61 | .34 | .45 | .45 | .53 | .542 |
| Phobic anxiety | .08 | .25 | .09 | .20 | .16 | .24 | 1.031 |
| Paranoid ideation | .38 | .56 | .38 | .48 | .69 | .65 | 3.224* |
| Psychoticism | .31 | .54 | .25 | .40 | .21 | .40 | .569 |
| BSI global severity | .34 | .38 | .34 | .31 | .41 | .34 | .410 |
| ASPD symptom count | 1.52 | 2.32 | 2.13 | 2.50 | 3.16 | 2.50 | 3.138* |
P <.05,
P <.01
Results from the BSI revealed that the PPGs generally scored higher on measures of psychological symptomology than those in the social or non-gambling groups. Specifically, the PPGs scored significantly higher on the paranoid ideation scale (F (2, 230) = 3.22, P = .042) but had higher scores in general on most of the variables. A DSM-IV-based measure of antisocial personality disorder (ASPD) revealed that PPGs also endorsed a significantly higher number of ASPD symptoms than the other groups (F (2, 232) = 6.81, P = .001).
Mediator and Moderator Analyses
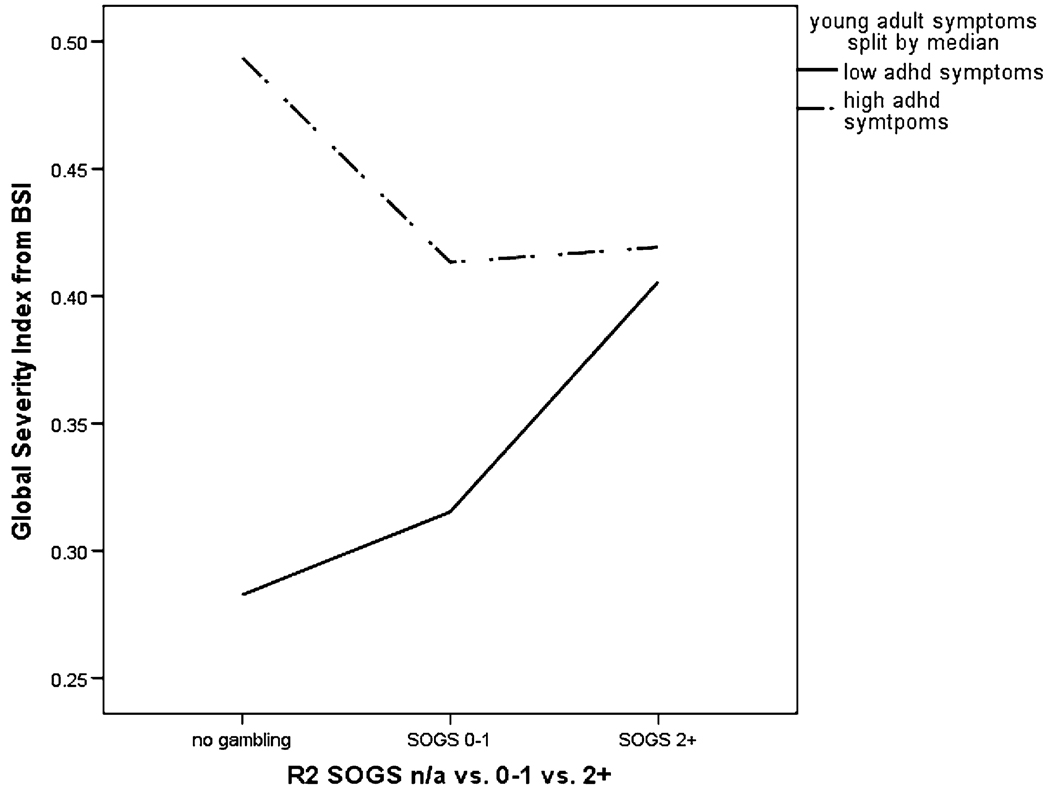
A MANCOVA was conducted to determine the role of ADHD in the above relationship between gambling status and psychosocial outcomes. In this model, we entered gambling severity groups and ADHD symptom count (at young adulthood) as independent variables, and BSI psychological scales as the dependent variables. The BSI Global Scale was omitted as a dependent variable to reduce redundancy in the data. We also included an interaction term between gambling severity and ADHD symptom count to test the moderating effect of ADHD. Results revealed a significant interaction effect (F = 1.46, P = .000), suggesting that the count of current (young adult) ADHD symptoms was in fact a significant moderator variable in this relationship (see Fig. 1).
Fig. 1.
Interaction of gambling severity groups and ADHD severity using BSI Global scale as outcome measure
In addition, ANCOVAs were conducted on the counts of legal and employment problems to examine ADHD as a moderator for these variables as well, utilizing gambling severity as the independent variable and ADHD symptom count as the covariate. A significant interactional effect occurred for both legal and employment outcomes (F (3) = 6.06, P = .001; F (3) = 8.23, P = .000, respectively). Again, these analyses revealed that ADHD significantly moderated the relationship between gambling and legal difficulties, as well as between gambling and work difficulties.
Finally, a mediational analysis was also conducted to determine if any baseline variables (including socioeconomic status, IQ, and level of impulsivity) mediated the relationship between gambling and ADHD status. To conduct this analysis, an intercor-relation was first performed to verify that gambling, ADHD, and the aforementioned baseline variables were significantly related. However, significant correlations were not found between SOGS-RA scores and the possible mediators, thus negating the mediational analysis.
Discussion
Results from this study on the persistence of ADHD and its effect on gambling indicate that individuals with sustained ADHD throughout childhood and young adulthood have a greater likelihood of increased gambling problem severity. Though participation in gambling activities did not differ among the groups of young adults in this sample, those with persistent ADHD had significantly higher rates of problem gambling.
The prevalence rates of gambling participation and possible problem gambling that were found in this study for both the desister and control groups were consistent with those of previous studies. Approximately 78% of those participants reported gambling in the past year with 5% meeting criteria for PPG. However, the persisters reported significantly higher rates of problem gambling than were found in previous prevalence studies (approximately 19%). This indicates that not only did the group of participants with persistent ADHD have higher rates of problem gambling than the rest of the sample, they had higher rates than the general population as well.
The moderation analysis revealed that ADHD appeared to be accounting for most of the significant differences in psychosocial factors among the gambling groups. This indicates that the severity of ADHD plays a more prominent role in psychosocial difficulties than does gambling severity, as participants with high ADHD symptom counts had a consistently higher mean on the BSI scales. This is consistent with other research showing a strong relationship between ADHD and many psychosocial variables, including legal problems, employment problems, and psychosocial difficulties (Hansen et al. 1999). This may be due to the high prevalence of conduct problems in individuals with ADHD, which is often associated with negative psychosocial outcomes. In addition, the moderation analysis showed that one outcome variable, count of employment difficulties, significantly differed by gambling severity group even after ADHD was used as a moderator. This too is consistent with previous research which found a link between problem gambling and employment problems (Petry and Armentano 1999).
This study supports other research which has found strong associations between ADHD and addictive behavior, including substance abuse, alcoholism, and nicotine dependence (August et al. 2006; Barkley et al. 2004; Elkins et al. 2007). There also appears to be a common link between substance abuse, disordered gambling, and impulsivity, a common trait of ADHD (Petry 2001). One retrospective study found that both alcoholics and pathological gamblers reported higher levels of ADHD behavior in childhood and that certain subsets of pathological gamblers have deficits in behavior restraint that is similar to alcoholics (Carlton and Manowitz 1992). This study and others (August et al. 2006; Barkley et al. 2004; Petry 2001) suggest that substance use, gambling, and ADHD are closely intertwined. Though we can not draw conclusions from the limited number of studies, the possible connection among these areas can serve as a basis for future research.
The results also lend support to previous research in the neurological basis of impulse control deficits. Previous studies have hypothesized that both ADHD and problem gambling may be due to neurological deficits in the areas of the brain that control impulsiveness and executive functioning (Fuentes et al. 2006; Krain and Castellanos 2006; Rugle and Melamed 1993). ADHD has been associated with dysfunction in the frontostriatal region of the brain (Rubia et al. 2001), as well as decreased brain volume, especially in the prefrontal cortex (Krain and Castellanos 2006). Pathological gambling studies have found deficits indicating frontal lobe circuitry dysfunction (Goudriaan et al. 2006) and support the idea of executive function impairment (Rugle and Melamed 1993). Finally, other studies have found that pathological gambling is highly correlated with ADHD and other impulse control disorders, including compulsive buying and compulsive sexual behavior (Specker et al. 1995). One such study of pathological gamblers found that 38% of their sample met full or subthreshold criteria for ADHD (Specker et al. 1995). Future research on the neurological bases of ADHD, gambling, and impulsive behaviors may give further support to these findings.
The current study is limited in its predominantly Caucasian sample and its inability to examine the effect of disorders that commonly co-exist with ADHD (primarily externalizing disorders). The relatively small sample size was also somewhat limiting for the groups that were created and the statistical analyses conducted. However, this study is strengthened by the longitudinal nature of the ADHD diagnosis, as well as from the epidemiological sample from which it was comprised. Very few studies have examined the relationship between ADHD and gambling problem severity among young adults, and none were found that look specifically at the persistence of ADHD and its effect on gambling problem severity. Future research would benefit from addressing the limitations of this study, as well as examining the co-occurrence of these disorders with additional addictions and psychosocial outcomes. In addition, further research on the biological mechanisms of addiction and ADHD may reveal other parallels between the disorders as well.
Acknowledgment
This study was supported by National Institute on Drug Abuse grants DA12995 and DA14717 (Winters).
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (text revision) Washington, DC: Author; 2000. [Google Scholar]
- August GJ, Realmuto GM, Crosby RD, MacDonald AW., III Community-based multiplegate screening of children at risk for conduct disorder. Journal of Abnormal Child Psychology. 1995;23(4):521–544. doi: 10.1007/BF01447212. [DOI] [PubMed] [Google Scholar]
- August GJ, Winters KC, Realmuto GM, Fahnhorst T, Botzet A, Lee S. Prospective study of adolescent drug use among community samples of ADHD and non-ADHD participants. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45(7):824–832. doi: 10.1097/01.chi.0000219831.16226.f8. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Fischer M, Smallish L, Fletcher K. Young adult follow-up of hyperactive children: Antisocial activities and drug use. Journal of Child Psychology and Psychiatry. 2004;45(2):195–211. doi: 10.1111/j.1469-7610.2004.00214.x. [DOI] [PubMed] [Google Scholar]
- Barnes GM, Welte JW, Hoffman JH, Dintcheff BA. Shared predictors of youthful gambling, substance use, and delinquency. Psychology of Addictive Behaviors. 2005;19(2):165–174. doi: 10.1037/0893-164X.19.2.165. [DOI] [PubMed] [Google Scholar]
- Carlson MJ, Moore TL. [Retrieved May 28, 2008];Adolescent gambling in oregon: A report to the oregon gambling addiction treatment foundation. 1998 from http://www.gamblingaddiction.org/adolescent/CHAPTER1.htm. [Google Scholar]
- Carlton PL, Manowitz P. Behavioral restraint and symptoms of attention deficit disorder in alcoholics and pathological gamblers. Neuropsychobiology. 1992;25:44–48. doi: 10.1159/000118808. [DOI] [PubMed] [Google Scholar]
- Carlton PL, Manowitz P, McBride H, Nora R, Swartzburg M, Goldstein L. Attention deficit disorder and pathological gambling. Journal of Clinical Psychiatry. 1987;48(12):487–488. [PubMed] [Google Scholar]
- Derevensky J, Pratt L, Hardoon K, Gupta R. Gambling problems and features of attention-deficit hyperactivity disorder among children and adolescents. Journal of Addiction Medicine. 2007;1(3):165–172. doi: 10.1097/ADM.0b013e318142d081. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. Brief symptom inventory. Baltimore, MD: Clinical Psychometric Research; 1975. [Google Scholar]
- Elkins IJ, McGue M, Iacono WG. Prospective effects of attention-deficit/hyperactivity disorder, conduct disorder, and sex on adolescent substance use and abuse. Archives of General Psychiatry. 2007;64:1145–1152. doi: 10.1001/archpsyc.64.10.1145. [DOI] [PubMed] [Google Scholar]
- Feigelman W, Gorman BS, Lesieur H. Examining the relationship between at-risk gambling and suicidality in a national representative sample of young adults. Suicide and Life-Threatening Behavior. 2006;36(4):396–408. doi: 10.1521/suli.2006.36.4.396. [DOI] [PubMed] [Google Scholar]
- Fuentes D, Tavares H, Artes R, Gorenstein C. Self-reported and neuropsychological measures of impulsivity in pathological gambling. Journal of the International Neuropsychological Society. 2006;12:907–912. doi: 10.1017/S1355617706061091. [DOI] [PubMed] [Google Scholar]
- Goudriaan AE, Oosterlaan J, de Beurs E, van den Brink W. Neurocognitive functions in pathological gambling: A comparison with alcohol dependence, Tourette syndrome, and normal controls. Addiction. 2006;101:534–547. doi: 10.1111/j.1360-0443.2006.01380.x. [DOI] [PubMed] [Google Scholar]
- Goyette CH, Conners CK, Ulrich RF. Normative data on revised conners parent and teacher rating scales. Journal of Abnormal Child Psychology. 1978;6:221–236. doi: 10.1007/BF00919127. [DOI] [PubMed] [Google Scholar]
- Gupta R, Derevensky J. Adolescent gambling behavior: A prevalence study and examination of the correlates associated with problem gambling. Journal of Gambling Studies. 1998;14(4):319–345. doi: 10.1023/a:1023068925328. [DOI] [PubMed] [Google Scholar]
- Hansen C, Weiss D, Last CG. ADHD boys in young adulthood: Psychosocial adjustment. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38(2):165–171. doi: 10.1097/00004583-199902000-00015. [DOI] [PubMed] [Google Scholar]
- Hardoon K, Derevensky J. Child and adolescent gambling behavior: Our current knowledge. Clinical Child Psychology and Psychiatry. 2002;7(2):263–281. [Google Scholar]
- Henly GA, Winters KC. Development of psychosocial scales for the assessment of adolescents involved with alcohol and drugs. International Journal of the Addictions. 1989;24(10):973–1001. doi: 10.3109/10826088909047324. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB. Four factor index of social status. New Haven, CT: Yale University Department of Sociology; 1975. [Google Scholar]
- Huang J, Jacobs DF, Derevensky JL, Gupta R, Paskus TS. Gambling and health risk behaviors among U. S. college student athletes: Findings from a national study. Journal of Adolescent Health. 2007;40:390–397. doi: 10.1016/j.jadohealth.2006.11.146. [DOI] [PubMed] [Google Scholar]
- Kaminer V, Petry N. Gambling behavior in youths: Why we should be concerned. Alcohol and Drug Abuse. 1999;50(2):167–168. doi: 10.1176/ps.50.2.167. [DOI] [PubMed] [Google Scholar]
- Kaufman AS, Kaufman NL. Kaufman brief intelligence test manual. Circle Pines, MN: American Guidance Service; 1990. [Google Scholar]
- Krain AL, Castellanos FX. Brain development and ADHD. Clinical Psychology Review. 2006;26:433–444. doi: 10.1016/j.cpr.2006.01.005. [DOI] [PubMed] [Google Scholar]
- LaBrie RA, Shaffer HJ, LaPlante DA, Wechsler H. Correlates of college student gambling in the United States. Journal of American College Health. 2003;52(2):53–62. doi: 10.1080/07448480309595725. [DOI] [PubMed] [Google Scholar]
- Langewisch MWJ, Frisch GR. Gambling behavior and pathology in relation to impulsivity, sensation seeking, and risky behavior in male college students. Journal of Gambling Studies. 1998;14(3):245–262. [Google Scholar]
- Lesieur HR, Blume SB. South oaks gambling screen (SOGS): A new instrument for the identification of pathological gamblers. American Journal of Psychiatry. 1987;144:1184–1188. doi: 10.1176/ajp.144.9.1184. [DOI] [PubMed] [Google Scholar]
- Lightsey OR, Jr, Hulsey CD. Impulsivity, coping, stress, and problem gambling among University students. Journal of Counseling Psychology. 2002;49(2):202–211. [Google Scholar]
- Lynch WJ, Maciejewski PK, Potenza MN. Psychiatric correlates of gambling in adolescents and young adults grouped by age at gambling onset. Archives of General Psychiatry. 2004;61:1116–1122. doi: 10.1001/archpsyc.61.11.1116. [DOI] [PubMed] [Google Scholar]
- Messerlian C, Derevensky J, Gupta R. Youth gambling problems: A public health perspective. Health Promotion International. 2005;20(1):69–79. doi: 10.1093/heapro/dah509. [DOI] [PubMed] [Google Scholar]
- Murphy KR. Unpublished manuscript. Boston: University of Massachusetts Medical Center; 1992. Evaluation interview for adult ADHD, ODD, and ASP. [Google Scholar]
- National Research Council. Pathological gambling: A critical review. Washington, DC: National Academy Press; 1999. [Google Scholar]
- Nower L, Derevensky JL, Gupta R. The relationship of impulsivity, sensation seeking, coping, and substance use in youth gamblers. Psychology of Addictive Behaviors. 2004;18(1):49–55. doi: 10.1037/0893-164X.18.1.49. [DOI] [PubMed] [Google Scholar]
- Petry NM. Substance abuse, pathological gambling, and impulsiveness. Drug and Alcohol Dependence. 2001;63:29–38. doi: 10.1016/s0376-8716(00)00188-5. [DOI] [PubMed] [Google Scholar]
- Petry NM. Pathological gambling: Etiology, comorbidity, and treatment. Washington, DC: American Psychological Association; 2005. [Google Scholar]
- Petry NM, Armentano C. Prevalence, assessment, and treatment of pathological gambling: A review. Psychiatric Services. 1999;50:1021–1027. doi: 10.1176/ps.50.8.1021. [DOI] [PubMed] [Google Scholar]
- Powell J, Hardoon K, Derevensky JL, Gupta R. Gambling and risk-taking behavior among University students. Substance Use & Misuse. 1999;34(8):1167–1184. doi: 10.3109/10826089909039402. [DOI] [PubMed] [Google Scholar]
- Reich W, Shayla JJ, Taibelson C. The diagnostic interview for children and adolescents-revised (DICA-R) (structured psychiatric interview) St. Louis: Washington University; 1992. [Google Scholar]
- Reynolds C, Kamphaus RC. Circle Pines, MN: American Guidance Services, Inc.; 1992. BASC: Behavioral assessment system for children and adolescents. [Google Scholar]
- Rubia K, Taylor E, Smith AB, Oksannen H, Overmeyer S, Newman S. Neuropsychological analyses of impulsiveness in childhood hyperactivity. British Journal of Psychiatry. 2001;179:138–143. doi: 10.1192/bjp.179.2.138. [DOI] [PubMed] [Google Scholar]
- Rugle L, Melamed L. Neuropsychological assessment of attention problems in pathological gamblers. The Journal of Nervous and Mental Disease. 1993;181(2):107–112. doi: 10.1097/00005053-199302000-00006. [DOI] [PubMed] [Google Scholar]
- Shaffer HJ, Hall MN. Updating and refining prevalence estimates of disordered gambling behaviour in the United States and Canada. Canadian Journal of Public Health. 2001;92(3):168–172. doi: 10.1007/BF03404298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slutske WS, Caspi A, Moffitt TE, Poulton R. Personality and problem gambling: A prospective study of a birth cohort of young adults. Archives of General Psychiatry. 2005;62:769–775. doi: 10.1001/archpsyc.62.7.769. [DOI] [PubMed] [Google Scholar]
- Specker SM, Carlson GA, Christenson GA, Marcotte M. Impulse control disorders and attention deficit disorder in pathological gamblers. Annals of Clinical Psychiatry. 1995;7(4):175–179. doi: 10.3109/10401239509149623. [DOI] [PubMed] [Google Scholar]
- Stinchfield R. Reliability, validity, and classification accuracy of the South Oaks gambling screen (SOGS) Addictive Behaviors. 2002;27(1):1–19. doi: 10.1016/s0306-4603(00)00158-1. [DOI] [PubMed] [Google Scholar]
- Volberg RA, Banks SM. A review of two measures of pathological gambling in the United States. Journal of Gambling Studies. 1990;6(2):153–163. doi: 10.1007/BF01013495. [DOI] [PubMed] [Google Scholar]
- Weinstock J, Whelan JP, Meyers AW, McCausland C. The performance of two pathological gambling screens on college students. Assessment. 2007;14(4):399–407. doi: 10.1177/1073191107305273. [DOI] [PubMed] [Google Scholar]
- Winters KC, Bengston P, Dorr D, Stinchfield R. Prevalence and risk factors of problem gambling among college students. Psychology of Addictive Behaviors. 1998;12(2):127–135. [Google Scholar]
- Winters KC, Henly GA. Adolescent diagnostic interview (ADI) manual. Los Angeles, CA: Western Psychological Services; 1993. [Google Scholar]
- Winters KC, Stinchfield R, Fulkerson J. Toward the development of an adolescent gambling problem severity scale. Journal of Gambling Studies. 1993;9:371–386. [Google Scholar]