Abstract
Study Design
Prospective Observational Cohorts
Objective
To describe sociodemographic and clinical features, and non-operative (medical) resource utilization prior to enrollment, in patients who are candidates for surgical intervention for intervertebral disc herniation (IDH), spinal stenosis (SpS), and degenerative spondylolisthesis (DS) according to SPORT criteria.
Summary of Background Data
Intervertebral disc herniation, spinal stenosis, and degenerative spondylolisthesis with stenosis are the three most common diagnoses of low back and leg symptoms for which surgery is performed. There is a paucity of descriptive literature examining large patient cohorts for the relationships among baseline characteristics and medical resource utilization with these three diagnoses.
Methods
The Spine Patient Outcomes Research Trial (SPORT) conducts three randomized and three observational cohort studies of surgical and non-surgical treatments for patients with IDH, SPS, and DS. Baseline data include demographic information, prior treatments received, and functional status measured by SF-36 and the Oswestry Disability Index (ODI-AAOS/Modems version). The data presented represents all 1,417 patients (745 IDH, 368 SpS, 304 DS) enrolled in the SPORT observational cohorts. Multiple logistic regression was used to generate independent predictors of utilization adjusted for sociodemographic variables, diagnosis, and duration of symptoms.
Results
The average age was 41 years for the IDH group, 64 years for the SPS group, and 66 years for the DS group.
At enrollment, IDH patients presented with the most pain as reported on the SF-36 (BP 26.2 vs 33 SPS and 33.7 DS) and were the most impaired (ODI 51 vs 42.3 SPS and 41.5 DS). IDH patients utilized more chiropractic treatment (42% vs 33% SPS and 26% DS); had more Emergency Department (ED) visits (21% vs 7 % SPS and 4% DS); and used more opiate analgesics (50% vs 29% SPS and 28% DS).
After adjusting for age, gender, diagnosis, education, race, duration of symptoms, and compensation, Medicaid patients used significantly more opiate analgesics (58% Medicaid vs 41% no insurance, 42% employer, 33% Medicare, and 32% private) and had more ED visits compared to other insurance types. (31% Medicaid vs 22% no insurance, 16% employer, 3% Medicare, and 11% private).
Conclusion
IDH patients appear to have differences in sociodemographics, resource utilization, and functional impairment when compared to the SpS/DS patients. In addition, the differences in resource utilization for Medicaid patients may reflect differences in access to care. The data provided from these observational cohorts will serve as an important comparison to the SPORT randomized cohorts in the future.
Keywords: SPORT, Disc herniation, spinal stenosis, degenerative spondylolisthesis, epidemiology, outcomes, utilization of healthcare resources
Introduction
Intervertebral disc herniation (IDH), spinal stenosis (SpS), and degenerative spondylolisthesis with stenosis (DS) are the three most common diagnoses of low back and leg symptoms for which surgery is performed.1 For this population of patients, there is a paucity of literature which has examined baseline medical resource utilization, as well as its relation to various demographic variables (age, sex, race, education, insurance type), or health status measures (SF-36, ODI).2,3
Most epidemiologic literature in the area of spine is related to low back pain and its nonspecific diagnoses such as sprain, strain, etc.4,5 Information regarding the use of medical treatment for patients with a confirmed diagnosis of disc herniation, spinal stenosis, and degenerative spondylolisthesis is scarce at best. Studies comparing surgical treatment to conservative therapy for these three diagnoses give little detail as to which non-operative therapies are utilized prior to surgical intervention.6–16 Most of the literature is based on case series or case reports.
The Spine Patient Outcomes Research Trial (SPORT) is prospectively collecting primary data from patients diagnosed as potential surgical candidates with IDH, SpS, and DS enrolled at multiple centers across the US.17 Baseline information from SPORT will help inform patients, physicians, and healthcare organizations about the non-operative treatments frequently utilized by patients with a diagnosis of IDH, SpS, or DS who are potential surgical candidates, as well as providing epidemiologic characterization of these groups of patients. The extent to which the choice of initial non-operative treatment prior to enrollment in SPORT is affected by specific clinical, demographic, or socioeconomic factors is unknown.
The purpose of this paper is to provide descriptive epidemiologic data on resource utilization in patients who are potential candidates for surgical intervention by SPORT criteria for IDH, SpS, and DS. Because there are a wide variety of non-operative treatment options for these diagnoses without clear clinical evidence as to which is best, we examined whether there are any differences in treatments provided to patients based on age, race, sex, education, insurance type, or health status. These baseline resource utilization data will lay the foundation for future SPORT publications in which we will examine how these treatments impact patient preference and outcomes.
Materials and Methods
The Spine Patient Outcomes Research Trial (SPORT) is being conducted at multiple clinical centers around the United States. The study design includes three separate prospective randomized clinical trials for IDH, SpS, and DS, accompanied by parallel observational studies of patients who meet inclusion criteria but decline to participate in the randomized studies.17 After patients met inclusion criteria (which includes a consistent clinical presentation, confirmatory imaging study, no prior spine surgery, and determination by the enrolling study physician that the patient is in fact a candidate for surgery) as previously described in detail,17 baseline data was obtained, including demographic information, prior treatments undertaken for their current spine-related problem, and Short Form 36 (SF-36)2 and Oswestry Disability Index (ODI-AAOS/Modems version)3 baseline information. The final determination of being a “surgical candidate” was made by the enrolling physician and necessarily included some degree of clinical judgment regarding the severity of symptoms and overall health status. The generalizability of this cohort will thus need to be judged in part by closely examining the baseline demographic and health status information provided later in the manuscript. The data presented represents all 1,417 patients (745 IDH, 368 SpS, 304 DS) enrolled in the observational arm of the study. The randomization arm was still enrolling patients at the time of this writing, and this data will be presented elsewhere when complete.
Analysis
Univariate group comparisons were made using t-tests, chi-square tests, and one-way ANOVA as appropriate. Although most questions on the patient surveys are required (i.e. the computerized questionnaire does not allow the patient to proceed to the next question before responding) and therefore contain no missing data, there are some questions which permit the patient to respond “I prefer not to answer,” including race, ethnicity, and marital status. The proportion of “no answer” responses is very low (0–3%) and these counts and percents are omitted from the tables. For this reason, some column totals may not add to exactly 100%.
Adjusted Analyses
In order to isolate the independent association between diagnosis, demographic characteristics and prior treatments, multiple logistic regression modeling was employed. These analyses were limited to treatments and medications found to have statistically significant predictors in the univariate analysis. (Utilization of “passive modalities” was nearly universal across diagnosis groups and not analyzed.) The binary response “outcome” for each model (a different model was fitted for each treatment) was set to one if the patient reported having had the treatment and zero otherwise. Each model included variables for age, gender, diagnosis, education, race, insurance type, duration of symptoms, and compensation. The logistic regression model results were used to estimate the adjusted proportions of patients receiving treatment in each diagnostic and demographic category. Adjusted proportions were computed by assuming covariate values equal to the mean values in the study population. All analyses were performed using S-Plus 6.1 (Insightful Corp, Seattle, WA).
Results
Patient Characteristics
A total of 1,417 patients were included in the observational cohort data collected between April 2000 and February 2003, with 745 in the IDH group, 368 in the SpS group, and the remaining 304 in the DS group (Table 1). 914 of the 1,417 patients (64.5%) enrolled in the surgical arm of the cohort (70% of IDH patients, 60% of SpS patients, and 57% of DS patients). The average age of the IDH group was 41 years, over 20 years younger than the average of 64 and 66 years in the SpS and DS groups, reflective of the typical age distribution of these diagnostic categories. Significantly more females composed the DS group (71%) versus 43% IDH and 40% SpS. There are significantly fewer blacks in the IDH group (6%), compared to SpS (9%) and DS (11%), and there were slightly more Hispanics in the IDH group (3%) versus 1% in both the SpS and DS groups.
Table 1.
Baseline Patient Characteristics
| IDH (n=745) | SPS (n=368) | DS (n=304) | P-value§ | |
|---|---|---|---|---|
| Mean Age (SD) | 41.4 (11.2) | 63.9 (12.5) | 66.2 (10.6) | <0.001 |
| Female | 43% | 40% | 71% | <0.001 |
| Race | <0.001 | |||
| White | 88% | 82% | 82% | |
| Black | 6% | 9% | 11% | |
| Asian | 1% | 0% | 1% | |
| Other/Mixed | 2% | 6% | 5% | |
| Ethnicity | 0.05 | |||
| Hispanic | 3% | 1% | 1% | |
| Non-Hispanic | 96% | 96% | 98% | |
| Education | <0.001 | |||
| Less than HS | 2% | 8% | 6% | |
| High School Grad | 22% | 27% | 28% | |
| Some College | 26% | 22% | 26% | |
| College Grad | 29% | 20% | 16% | |
| Post-Grad Degree | 19% | 21% | 24% | |
| Marital Status | <0.001 | |||
| Married | 69% | 70% | 66% | |
| Divorced | 11% | 9% | 11% | |
| Widowed | 1% | 13% | 18% | |
| Single | 18% | 6% | 5% | |
| Work Status | <0.001 | |||
| Full Time | 47% | 23% | 19% | |
| Part Time | 6% | 5% | 5% | |
| No Time | 10% | 3% | 1% | |
| Unemployed | 2% | 1% | 0% | |
| Disabled | 11% | 7% | 4% | |
| Retired | 2% | 30% | 25% | |
| Homemaker | 5% | 7% | 11% | |
| Student | 1% | 0% | 0% | |
| (Multiple) | 15% | 24% | 35% | |
| Worker’s Comp/Disability* | 21% | 8% | 7% | <0.001 |
| Comorbidities | ||||
| Hypertension | 12% | 44% | 45% | <0.001 |
| Stroke | 0% | 2% | 3% | <0.001 |
| Diabetes | 4% | 13% | 14% | <0.001 |
| Osteoporosis | 2% | 11% | 12% | <0.001 |
| Cancer | 3% | 6% | 9% | <0.001 |
| Fibromyalgia | 2% | 2% | 3% | 0.34 |
| Migraine | 9% | 7% | 8% | 0.61 |
| CFS | 1% | 1% | 2% | 0.62 |
| Depression | 11% | 10% | 14% | 0.28 |
| Anxiety | 7% | 4% | 6% | 0.28 |
| PTSD | 1% | 1% | 2% | 0.73 |
| Alcoholism | 1% | 2% | 1% | 0.52 |
| Drug Dependency | 0% | 1% | 0% | 0.91 |
| Heart Disease | 4% | 24% | 21% | <0.001 |
| Lung Disease | 3% | 8% | 7% | <0.001 |
| Stomach Problem | 12% | 22% | 23% | <0.001 |
| Bowel or Intestinal | 6% | 14% | 9% | <0.001 |
| Liver Disease | 1% | 2% | 2% | 0.29 |
| Kidney Disease | 2% | 5% | 5% | 0.017 |
| Blood Vessel Disease | 2% | 6% | 7% | <0.001 |
| Nervous System Disease | 2% | 2% | 3% | 0.22 |
| Joint Disease | 17% | 52% | 57% | <0.001 |
| Symptom Duration (Most Recent Episode) | <0.001 | |||
| 6 Weeks or Less | 3% | 0% | 0% | |
| 7–12 Weeks | 32% | 3% | 2% | |
| 3–6 Months | 42% | 39% | 38% | |
| 7–12 Months | 14% | 25% | 26% | |
| ≥1 Year | 9% | 33% | 35% |
The p value is a Chi-square p value for the entire variable;
Percentage of “yes” responses to the question: “Have you applied to, or are you now receiving payments from either Worker’s Compensation, Social Security Disability Insurance or any other disability insurance programs for your spine-related problem?”
Regarding education, the IDH patients were more likely to have college degrees (29%) compared to the SpS (20%) and DS (16%) patients, but the stenosis groups (SpS and DS) were more likely to have graduate degrees. More of the IDH patients are single (18%), but this is likely a reflection of age difference between groups, as more of the SpS and DS patients are widowed (18% and 13%). A significantly larger proportion of the IDH patients are working, but they are also more disabled at baseline. Also, more IDH patients report having applied for or receiving worker’s compensation (21% IDH versus 8% SpS and 7% DS). These results are consistent with the older age and high number of retirees in the stenosis groups.
Co-Morbidities
As expected, there were significantly more co-morbidities in the stenosis groups (SpS and DS) compared to the IDH patients (Table 1). The most common co-morbidities reported in order of frequency are: concomitant joint disease, hypertension, heart disease, stomach/intestinal problems, diabetes, and osteoporosis.
Duration of Symptoms
Patients in all three diagnostic groups most commonly had symptoms for between 3 and 6 months. In the SpS and DS groups, a significantly larger proportion of patients had a duration of symptoms greater than 1 year (33% and 33%), compared to the IDH group (9%) (Table 1). Thirty-five percent of patients in the IDH group had symptoms for fewer than 3 months.
Health Status
At baseline, IDH patients presented with the most pain as reported on the Bodily Pain (BP) scale of the SF-36, with an average score of 26.3 compared to SpS (33.2) and DS (33.8). The IDH group was also the most disabled with a score of 51.1 on the modified ODI compared to SpS (42.3) and DS (41.4) (Figure 1). The IDH group reported significantly lower scores on several other SF-36 scales, including Role Physical, Vitality, Social Function, Role Emotional, and Mental Health. The one scale that was significantly worse among the SPS and DS patients was the General Health Perception scale, which is consistent with the older age and greater number of co morbidities in these two groups.
Figure 1.
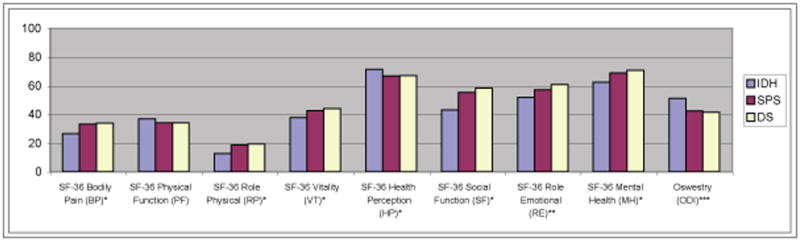
*IDH patients significantly different from SPS and DS (p<0.05)
**IDH patients significantly different from DS and not SPS (p<0.05)
***ODI has reverse scale: 100=disabled, 0=normal, IDH significantly different from SPS and DS (p<0.05)
Non-Operative Treatments Received Prior to Enrollment
Diagnosis
Significantly more IDH patients (42%) had received chiropractic treatment, compared to SPS (33%) and DS (26%). (Figure 2) IDH patients were also significantly more likely to have been seen in an Emergency Department (ED) setting (21%) compared to SpS (7%) and DS (4%) patients. Furthermore, prior use of opiate medications was significantly higher in the IDH group (50%) compared to SpS (29%) and DS (28%) patients, as was antidepressant and muscle relaxant use (28%) compared to SPS (20%) and DS (23%).
Figure 2.
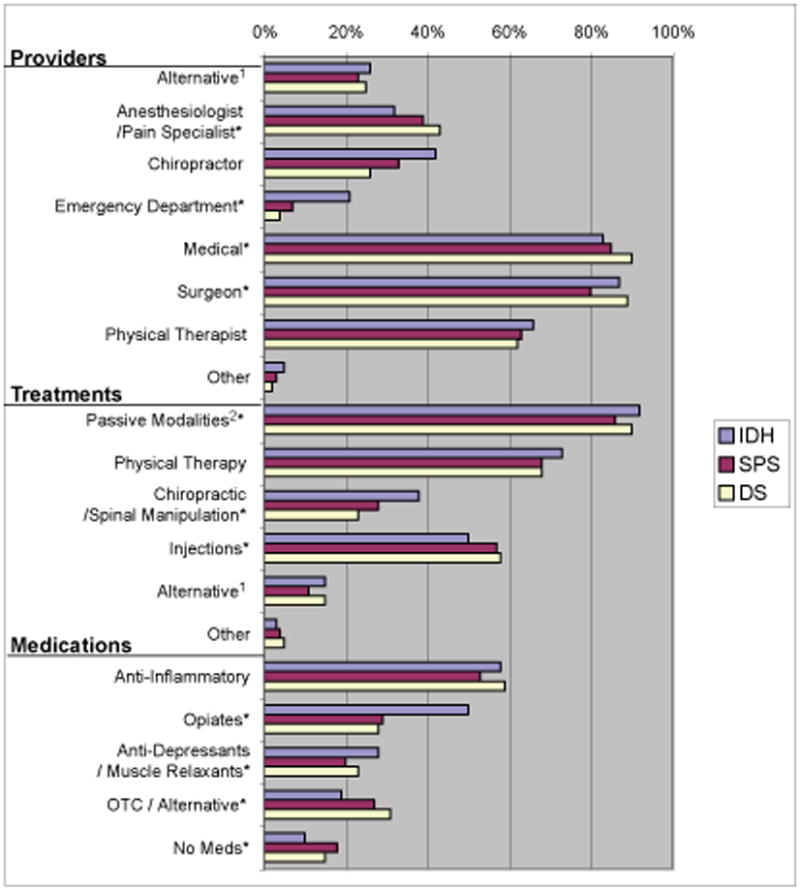
*Significant difference in reported utilzation between diagnosis groups. (p<0.05)
1 Alternative health care providers/therapies, including acupuncture, homeopathic, osteopathic, psychotherapy.
2 Passive modalities include education, passive PT, activity restriction, devices.
On the other hand, more patients in the stenosis groups (SpS (43%) and DS (39%)) had been treated by an anesthesiologist or pain doctor for their symptoms than IDH (32%). Also, more over-the-counter medication use was reported by the DS and SpS patients (31% and 27%) vs IDH (19%).
Age
These same trends hold true when the study populations are stratified into age groups, reflective of the age distribution difference seen when the IDH group (younger) is compared to the SpS and DS groups (older). Patients under 60 years old were more likely to have seen a chiropractor and undergone manipulation compared to patients over age 60 (40% vs 28%) (Table 2). Patients under age 40 are also more likely to have visited the ED (22%) compared to patients over 60 (5%), and were more likely to have received physical therapy (76%) compared to patients age 60 and over (65%). The trend in medication use was similar. Patients under age 40 used significantly more opiate medications (50% vs 28%), and anti-depressants and muscle relaxants (26% vs 19%) compared to patients over age 60, while older patients used more over-the-counter medications (33% vs 16%) compared to patients under age 40.
Table 2.
Healthcare utilization prior to enrollment in SPORT, by age, gender, race and insurance provider.
| AGE | GENDER | RACE | EDUCATION | INSURANCE | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| < 40 | 40–60 | Over 60 |
Female | Male | White | Black | Asian | Other/ Mixed |
Less than High School |
High School Grad |
Some College |
College Grad |
Post Grad degree |
None | Employer | Medicare | Medicaid | Private | ||||||
| 378 | 557 | 482 | P value | 687 | 730 | P value | 1204 | 107 | 12 | 51 | P value |
66 | 350 | 351 | 356 | 292 | P value | 32 | 909 | 219 | 36 | 214 | P value | |
| Providers | ||||||||||||||||||||||||
| Alternative | 26% | 26% | 22% | 0.29 | 29% | 21% | <0.001 | 25% | 22% | 25% | 24% | 0.97 | 23% | 23% | 24% | 29% | 26% | 0.22 | 25% | 26% | 22% | 31% | 24% | 0.74 |
| Anesthes/Pain | 31% | 36% | 41% | 0.021 | 40% | 33% | 0.007 | 37% | 33% | 8% | 41% | 0.065 | 35% | 40% | 36% | 34% | 37% | 0.73 | 41% | 34% | 41% | 39% | 42% | 0.14 |
| Chrio/Manip | 40% | 41% | 28% | <0.001 | 35% | 37% | 0.49 | 38% | 20% | 42% | 27% | 0.002 | 29% | 38% | 39% | 38% | 32% | 0.21 | 47% | 39% | 26% | 33% | 32% | 0.002 |
| Emergency Dept. | 22% | 16% | 5% | <0.001 | 15% | 13% | 0.44 | 13% | 21% | 25% | 6% | 0.012 | 12% | 17% | 14% | 13% | 10% | 0.2 | 22% | 16% | 3% | 31% | 11% | <0.001 |
| Medical (Family, Internist, Neuro, Rheum) | 84% | 84% | 87% | 0.47 | 88% | 82% | 0.005 | 85% | 93% | 100% | 75% | 0.009 | 89% | 86% | 85% | 85% | 85% | 0.66 | 78% | 85% | 88% | 86% | 82% | 0.36 |
| Surgeon | 88% | 85% | 84% | 0.14 | 85% | 86% | 0.44 | 85% | 85% | 83% | 90% | 0.9 | 86% | 86% | 85% | 87% | 86% | 0.31 | 81% | 85% | 87% | 86% | 86% | 0.92 |
| Physical Therapist | 69% | 66% | 59% | 0.007 | 68% | 61% | 0.008 | 65% | 65% | 75% | 63% | 0.71 | 52% | 62% | 66% | 69% | 65% | 0.061 | 78% | 66% | 58% | 75% | 61% | 0.033 |
| None | 1% | 0% | 0% | 0.24 | 0% | 0% | 0.6 | 0% | 0% | 0% | 0% | 0.97 | 0% | 0% | 0% | 0% | 1% | 0.44 | 0% | 0% | 0% | 0% | 1% | 0.18 |
| Treatments | ||||||||||||||||||||||||
| Passive Modalities | 92% | 90% | 88% | 0.14 | 91% | 89% | 0.12 | 90% | 90% | 92% | 92% | 0.93 | 91% | 89% | 91% | 91% | 88% | 0.026 | 88% | 90% | 89% | 94% | 88% | 0.68 |
| Physical Therapy | 76% | 72% | 65% | 0.002 | 75% | 67% | 0.003 | 71% | 72% | 67% | 65% | 0.49 | 64% | 67% | 74% | 75% | 69% | 0.14 | 78% | 73% | 65% | 75% | 67% | 0.12 |
| Chiro/Manip | 38% | 34% | 25% | <0.001 | 31% | 33% | 0.64 | 34% | 18% | 42% | 25% | 0.008 | 24% | 33% | 33% | 34% | 29% | 0.16 | 44$ | 35% | 23% | 25% | 29% | 0.004 |
| Injections | 50% | 54% | 56% | 0.26 | 56% | 51% | 0.089 | 53% | 56% | 42% | 57% | 0.47 | 55% | 56% | 54% | 53% | 49% | 0.55 | 63% | 53% | 51% | 56% | 57% | 0.6 |
| Alternative | 14% | 15% | 13% | 0.74 | 15% | 12% | 0.12 | 14% | 13% | 25% | 14% | 0.82 | 12% | 12% | 13% | 15% | 17% | 0.22 | 9% | 14% | 16% | 17% | 14% | 0.85 |
| None | 1% | 0% | 1% | 0.37 | 0% | 1% | 0.21 | 1% | 1% | 0% | 0% | 0.93 | 2% | 0% | 1% | 0% | 1% | 0.009 | 3% | 0% | 1% | 0% | 1% | 0.35 |
| Medications | ||||||||||||||||||||||||
| Anti-inflammatory | 60% | 57% | 54% | 0.21 | 59% | 55% | 0.25 | 57% | 63% | 67% | 55% | 0.033 | 58% | 55% | 58% | 59% | 56% | 0.97 | 50% | 59% | 54% | 61% | 54% | 0.45 |
| Narcotics | 50% | 42% | 28% | <0.001 | 42% | 37% | 0.12 | 40% | 34% | 17% | 41% | 0.15 | 48% | 44% | 40% | 42% | 27% | <0.001 | 41% | 42% | 33% | 58% | 32% | 0.003 |
| Anti-Depress/Muscle Relaxants | 26% | 30% | 19% | <0.001 | 32% | 18% | <0.001 | 24% | 32% | 8% | 27% | 0.17 | 27% | 24% | 28% | 27% | 18% | 0.075 | 28% | 27% | 21% | 36% | 20% | 0.082 |
| OTC/Alternative | 16% | 22% | 33% | <0.001 | 27% | 21% | 0.003 | 24% | 28% | 8% | 22% | 0.52 | 23% | 25% | 25% | 21% | 25% | 0.52 | 22% | 21% | 32% | 22% | 29% | 0.002 |
| None | 11% | 11% | 18% | 0.003 | 10% | 16% | 0.003 | 13% | 12% | 25% | 16% | 0.71 | 11% | 13% | 11% | 13% | 17% | 0.16 | 19% | 11% | 17% | 8% | 19% | 0.008 |
Gender
Among different gender groups, females were more likely to have used alternative health care providers (29% vs 21%), were more likely to have seen a pain doctor (40% vs 33%), and reported more visits to medical specialists (88% vs 82%) and physical therapists (68% vs 61%) (Table 2). With regard to medication use, females used significantly more anti-depressants and muscle relaxants (32% vs 18%), as well as more over-the-counter medications (27% vs 21%). Males were more likely not to have used any medication (16% vs 10%).
Race
The breakdown into racial groups shows that Whites and Asians were more likely to have received treatment from a chiropractor (38% and 42%) compared to Blacks and others (20% and 27%), while the use of other therapeutic modalities were at similar rates (Table 2). Medication use among the different groups was also similar. Due to the small number of racial minorities enrolled in SPORT, differences of similar magnitude that were statistically significant for other sociodemographic variables were not statistically significant for race.
Education
Overall, the analysis of the patients based on level of education shows similar rates of usage of health care providers and treatment modalities at all educational levels. However, patients with lower levels of education had received significantly more opiate pain medication (less than HS (48%) vs Post graduate degree (27%)), while patients with graduate degrees had used significantly less opiate pain medication compared to all other groups (Table 2).
Type of Insurance
Chiropractic use
Finally, analysis of patients based on type of insurance indicates that patients with no insurance and those with employer insurance were more likely to have visited and received treatment from a chiropractor (47% and 39%) compared to patients with other forms of insurance (e.g., 26% Medicare, 33% Medicaid, and 32% private) (Table 2).
ED (Emergency Department)
Medicaid patients had significantly more visits to the ED (31%) compared to patients with all other insurance types (22% no insurance, 16% employer, 3% Medicare, 11% private) (Table 2).
Medications
Medicaid patients also used significantly more opiate medication compared to all other patients (58% vs 41% no insurance, 42% employer, 33% Medicare, and 32% private), and there was also a trend toward more usage of anti-depressant and muscle relaxant medication in the Medicaid group. Medicare and private insurance patients used significantly more over-the-counter medication compared to the other insurance groups (32% and 29% vs 22% no insurance, 21% employer, and 22% Medicaid) (Table 2).
Adjusted results (Table 3)
Table 3.
Adjusted proportion of patients in each subcategory who received treatment (multiple logistic regression analysis results).
| Chiropractor | P-Value | ED | P-Value | Injections | P-Value | Opiates | P-Value | Antidepressants | P-Value | OTC Meds | P-Value | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | < 40 years | 32% | 0.88 | 12% | 0.29 | 52% | 0.81 | 43% | 0.074 | 23% | 0.073 | 16% | 0.003 |
| 40–60 years | 33% | 11% | 53% | 42% | 27% | 21% | |||||||
| > 60 years | 31% | 7% | 55% | 31% | 19% | 32% | |||||||
| Gender | Male | 31% | 0.57 | 9% | 0.058 | 51% | 0.061 | 34% | 0.005 | 17% | <0.001 | 20% | 0.038 |
| Female | 33% | 12% | 56% | 43% | 31% | 25% | |||||||
| Diagnosis | IDH | 38% | 0.001 | 17% | <0.001 | 51% | 0.45 | 47% | <0.001 | 27% | 0.038 | 24% | 0.79 |
| SPS | 28% | 7% | 56% | 30% | 19% | 21% | |||||||
| DS | 22% | 4% | 56% | 28% | 19% | 22% | |||||||
| Education | < High School | 29% | 0.7 | 12% | 0.53 | 49% | 0.17 | 52% | 0.004 | 25% | 0.13 | 19% | 0.76 |
| High School | 34% | 13% | 55% | 43% | 21% | 23% | |||||||
| Some College | 33% | 10% | 54% | 39% | 26% | 23% | |||||||
| College Grad | 32% | 8% | 56% | 39% | 26% | 22% | |||||||
| Post-Grad Degree | 29% | 9% | 50% | 28% | 19% | 24% | |||||||
| Race | White | 33% | 0.052 | 10% | 0.2 | 53% | 0.088 | 39% | 0.022 | 23% | 0.078 | 23% | 0.51 |
| Black | 18% | 16% | 54% | 29% | 29% | 26% | |||||||
| Asian | 40% | 16% | 46% | 14% | 7% | 10% | |||||||
| Other/Mixed | 28% | 7% | 57% | 42% | 28% | 20% | |||||||
| Insurance | Employer | 33% | 0.44 | 10% | 0.033 | 55% | 0.17 | 35% | 0.005 | 22% | 0.85 | 22% | 0.87 |
| Medicare | 26% | 5% | 45% | 50% | 26% | 21% | |||||||
| Medicaid | 29% | 25% | 48% | 62% | 29% | 21% | |||||||
| Private | 31% | 14% | 56% | 38% | 23% | 25% | |||||||
| None | 44% | 9% | 64% | 27% | 23% | 28% | |||||||
| Compensation* | No compensation | 32% | 0.48 | 10% | 0.091 | 53% | 0.32 | 36% | <0.001 | 22% | 0.022 | 23% | 0.35 |
| Compensation | 29% | 13% | 57% | 52% | 30% | 20% | |||||||
| Episode | < 6 months | 29% | 0.027 | 10% | 0.37 | 50% | 0.041 | 40% | 0.47 | 22% | 0.37 | 21% | 0.11 |
| 6–12 months | 37% | 8% | 57% | 38% | 24% | 23% | |||||||
| 1 year or more | 36% | 12% | 59% | 35% | 27% | 28% |
Defined as having applied to, or currently receiving payments from either Worker’s Compensation, Social Security Disability Insurance or any other disability insurance programs for a spine-related problem
Adjusted analysis allowed us to observe that patients over 60 years old are still twice as likely to use OTC medications as patients under 40 (32% versus 16%, p=0.003), even after controlling for diagnosis and other covariates. In the adjusted analysis, age was no longer a significant predictor of chiropractic care, ED visits, opiates, or antidepressant usage. Similarly, after controlling for covariates, the adjusted proportion of females using certain medications was significantly higher than that of men (43% versus 34% using opiates, p=0.005; 31% versus 17% using antidepressants, p<0.001; and 25% versus 20% using OTC medications, p=0.049), but gender was no longer significantly related to chiropractic or ED use.
The adjusted analysis confirms that IDH patients had visited the ED and used opiates more often than SPS and DS patients (p<0.001), and that chiropractic use varied significantly across the three diagnostic groups (IDH 38%, SPS 28%, and DS 22%, p=0.001). However, significant differences across these three groups in the use of injections, antidepressants, and OTC medications disappeared after adjustment. Education continues to show close association with the use of opiates. Fifty-two percent of patients having little formal education had used opiate medications compared to only 28% of patients with a post-graduate degree (p<0.004). Race also continued to predict opiate use, with whites having significantly more utilization than minorities (adjusted rate: 39% whites compared to 29% blacks and 14% Asians, p=0.022); however, race was no longer associated with ED visits.
Finally, after adjusting for covariates, Medicaid patients remained the most frequent users of emergency departments, with nearly double the rate of patients with any other type of insurance (p=0.033). Medicaid patients showed the highest adjusted rate of opiate use (62%), with Medicare patients following close behind (50%, p=0.005). Insurance status in and of itself did not predict utilization of chiropractic or OTC medications after adjusting for covariates. However, workers compensation patients showed adjusted utilization rates of opiates and antidepressants nearly 50% higher than non-compensation patients (p<0.001 and p=0.022 respectively).
Discussion
Greater than 250,000 surgeries on the lumbar spine are performed electively each year in the United States,19 with procedures for intervertebral disc herniation, spinal stenosis, and degenerative spondylolisthesis being the most common.4 The data from this study provide prospective information on the characteristics of patients with confirmed clinical and radiographic findings of IDH, SpS, and DS. We also provide important information about their prior utilization of healthcare at the time they enrolled in SPORT. The data presented in this paper represents a broad population base from 13 centers in 11 states, comprising 8 academic centers and 5 private practices. Each practice has many participating physicians (surgeons (orthopaedic and neurosurgery) and non-surgeons) from various disciplines that tend to see these kinds of patients.
The gender breakdown of this study population shows a greater use of anti-depressants among females, as well as a trend toward more treatment in general from all health care providers. Women also reported greater pain at baseline on the SF-36 BP scale (24 vs 28; p=0.004 data not shown). These findings are consistent with gender differences seen in the general population as regards general health care utilization,20 with females utilizing health care resources more than males. The female population also used significantly more opiate medications than men. This may be related to increased affective distress (as seen with the increase in anti-depressant use) 21 and variations in pain perception that has been reported for many conditions, including chronic low back pain. 22,23
The analysis of patients by insurance type presents some interesting findings. Medicaid patients were much more likely to have visited an Emergency Department and to have received opiates. This remained true even after controlling for multiple covariates including education level, which also was an independent predictor of opiate use. These findings are consistent with prior reports of increased Emergency Department visits from patients with Medicaid insurance due to difficulty with access to primary care. 24 As reimbursements to primary care providers continue to decrease, they become less willing to see Medicaid patients in their practice. This effectively shifts the care of non-emergency medical problems of these patients to the Emergency Department. These findings appear to emphasize the need for access to primary care for low income patients in order to improve compliance with recommended treatment guidelines and potentially decrease total cost of healthcare for these patients.
Despite the variation in treatments received by patients for the different diagnostic and demographic groups, available evidence does not demonstrate that one treatment is more beneficial than another. With no clear consensus in place, it is difficult to discern if the differences in treatment that are seen are due to provider recommendation, patient preference or other factors within the health care system.
The results from this study have the advantage of coming from a variety of centers with a large number of patients in the study. However, all the patients in these three cohorts represent those who refused to be randomized in SPORT. This might select for patients with more severe symptoms, or other factors such as patient preferences, understanding risks or aversion to chance. Follow up comparisons with the SPORT randomized patients will be important in order to see whether there are any important differences between these two groups.
SPORT represents the largest cooperative multicenter, multidisciplinary study that has been undertaken for these three diagnostic groups (IDH, SPS, DS). Reporting the baseline data for the observational cohort will allow others to have a clear picture of the patients studied and how those patients relate to the practices of surgeons and non-surgeons alike. The literature is replete with studies that provide minimal information regarding the baseline characteristics of the population studied. To be compatible with the CONSORT publication recommendations, 25–27 SPORT baseline data are presented here for future reference when reporting our results at one year and beyond. Results from most studies leave the reader wondering if the results are applicable to their practice and patient population. Because SPORT involves 11 states, 13 centers and 115 physicians representing 6 medical specialties (general internal medicine, anesthesiology, rheumatology, occupational medicine, physiatry, rehabilitation medicine) and 2 surgical disciplines (orthopaedics and neurosurgery), this comprehensive data is the most generalizable published to date.
The data presented provide prospective baseline information on the three most common diagnostic groups of patients for which lumbar spine surgery is performed: IDH, SpS and DS. Understanding the baseline patient characteristics, function, treatments sought, and variability of treatment frequencies in different subgroups is important in planning future treatments. Recognizing the potential differences in race, gender, educational level, insurance type, and other factors may be important in predicting short and long term effectiveness of the treatments these patients receive. In analyzing the SPORT outcomes we will be able to consider the effects of these variables and better understand their role in the results of subsequent treatments. With this extensive collection of baseline information we will be prepared to evaluate the outcomes of different treatments among different subgroups with the same diagnosis, determining if those outcomes are related to baseline patient variability.
Acknowledgments
The authors would like to acknowledge funding from the following sources: The National Institute of Arthritis and Musculoskeletal and Skin Diseases (U01-AR45444-01A1 and P60-AR048094-01A1) and the Office of Research on Women’s Health, the National Institutes of Health, and the National Institute of Occupational Safety and Health, the Centers for Disease Control and Prevention. Dr. Lurie is supported by a Research Career Award from NIAMS (1 K23 AR 048138-01). Dr. Birkmeyer is supported by AHRQ K02 HS11288.
Footnotes
This study is dedicated to the memory of Brieanna Weinstein.
SPORT Sites and PI’s (James N. Weinstein, DO, MS, SPORT Principal Investigator) Dartmouth-Hitchcock Medical Center, Lebanon, NH
William A. Abdu, MD, MS
New York University Medical Center’s Hospital for Joint Diseases, NY, NY
Thomas Errico, MD
Hospital for Special Surgery, NY, NY
Frank P. Cammisa, MD
Nebraska Foundation for Spinal Research, Omaha, NE
Michael Longley, MD
Rothman Institute @ Thomas Jefferson University, Philadelphia, PA
Todd Albert, MD; Alan Hilibrand, MD
Rush-Presbyterian-St. Luke’s Medical Center, Chicago, IL
Gunnar Andersson, MD, PhD
The Emory Clinic, Decatur, GA
Scott Boden, MD
University of California Medical Center, San Francisco, CA
Serena Hu, MD
University Hospitals of Cleveland, Cleveland, OH
Chris Furey, MD; Sanford Emery, MD
Washington University Hospital, St. Louis, MO
Lawrence Lenke, MD
William Beaumont Hospital, Royal Oak, MI
Harry Herkowitz, MD
Kaiser-Permanente, Oakland, CA
Harley Goldberg, DO
References
- 1.Cherkin DC, Deyo RA, Loeser JD, et al. An international comparison of back surgery rates. Spine. 1994;19(11):1201–6. doi: 10.1097/00007632-199405310-00001. [DOI] [PubMed] [Google Scholar]
- 2.Ware JE., Jr SF-36 health survey update. Spine. 2000;25(24):3130–9. doi: 10.1097/00007632-200012150-00008. [DOI] [PubMed] [Google Scholar]
- 3.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine. 2000;25(22):2940–52. doi: 10.1097/00007632-200011150-00017. discussion 52. [DOI] [PubMed] [Google Scholar]
- 4.Deyo RA, Weinstein JN. Low back pain. New England Journal of Medicine. 2001;344(5):363–70. doi: 10.1056/NEJM200102013440508. [DOI] [PubMed] [Google Scholar]
- 5.Hart LG, Deyo RA, Cherkin DC. Physician office visits for low back pain. Frequency, clinical evaluation, and treatment patterns from a U.S. national survey. Spine. 1995;20(1):11–9. doi: 10.1097/00007632-199501000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Yukawa Y, Lenke LG, Tenhula J, et al. A comprehensive study of patients with surgically treated lumbar spinal stenosis with neurogenic claudication. Journal of Bone & Joint Surgery - American Volume. 2002;84-A(11):1954–9. doi: 10.2106/00004623-200211000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Findlay GF, Hall BI, Musa BS, et al. A 10-year follow-up of the outcome of lumbar microdiscectomy. Spine. 1998;23(10):1168–71. doi: 10.1097/00007632-199805150-00019. [DOI] [PubMed] [Google Scholar]
- 8.Amundsen T, Weber H, Nordal HJ, et al. Lumbar spinal stenosis: conservative or surgical management?: A prospective 10-year study. Spine. 2000;25(11):1424–35. doi: 10.1097/00007632-200006010-00016. discussion 35–6. [DOI] [PubMed] [Google Scholar]
- 9.Moller H, Hedlund R. Surgery versus conservative management in adult isthmic spondylolisthesis--a prospective randomized study: part 1. Spine. 2000;25(13):1711–5. doi: 10.1097/00007632-200007010-00016. [DOI] [PubMed] [Google Scholar]
- 10.Keller RB, Atlas SJ, Singer DE, et al. The Maine Lumbar Spine Study, Part I. Background and concepts. Spine. 1996;21(15):1769–76. doi: 10.1097/00007632-199608010-00010. [DOI] [PubMed] [Google Scholar]
- 11.Atlas SJ, Keller RB, Chang Y, et al. Surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: five-year outcomes from the Maine Lumbar Spine Study. Spine. 2001;26(10):1179–87. doi: 10.1097/00007632-200105150-00017. [DOI] [PubMed] [Google Scholar]
- 12.Atlas SJ, Keller RB, Robson D, et al. Surgical and nonsurgical management of lumbar spinal stenosis: four-year outcomes from the maine lumbar spine study. Spine. 2000;25(5):556–62. doi: 10.1097/00007632-200003010-00005. [DOI] [PubMed] [Google Scholar]
- 13.Atlas SJ, Deyo RA, Keller RB, et al. The Main Lumbar Spine Study, Part II. 1-year outcomes of surgical and nonsurgical management of sciatica. Spine. 1996;21(15):1777–86. doi: 10.1097/00007632-199608010-00011. [DOI] [PubMed] [Google Scholar]
- 14.Atlas SJ, Deyo RA, Keller RB, et al. The Maine Lumbar Spine Study, Part III. 1-year outcomes of surgical and nonsurgical management of lumbar spinal stenosis. Spine. 1996;21(15):1787–94. doi: 10.1097/00007632-199608010-00012. discussion 94–5. [DOI] [PubMed] [Google Scholar]
- 15.Atlas SJ, Deyo RA, Keller RB, et al. The Maine Lumbar Spine Study, Part II. 1-year outcomes of surgical and nonsurgical management of sciatica. Spine. 1996;21(15):1777–86. doi: 10.1097/00007632-199608010-00011. [DOI] [PubMed] [Google Scholar]
- 16.Weber H. Lumbar disc herniation. A controlled, prospective study with ten years of observation. Spine. 1983;8(2):131–40. [PubMed] [Google Scholar]
- 17.Birkmeyer NJ, Weinstein JN, Tosteson AN, et al. Design of the Spine Patient outcomes Research Trial (SPORT) Spine. 2002;27(12):1361–72. doi: 10.1097/00007632-200206150-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cox D, Snell E. Analysis of Binary Data. 2. Chapman & Hall; 1989. [Google Scholar]
- 19.Taylor VM, Deyo RA, Cherkin DC, et al. Low back pain hospitalization. Recent United States trends and regional variations. Spine. 1994;19(11):1207–12. doi: 10.1097/00007632-199405310-00002. discussion 13. [DOI] [PubMed] [Google Scholar]
- 20.Bertakis KD, Azari R, Helms LJ, et al. Gender differences in the utilization of health care services. Journal of Family Practice. 2000;49(2):147–52. [PubMed] [Google Scholar]
- 21.Fillingim RB, Doleys DM, Edwards RR, et al. Clinical characteristics of chronic back pain as a function of gender and oral opioid use. Spine. 2003;28(2):143–50. doi: 10.1097/00007632-200301150-00010. [DOI] [PubMed] [Google Scholar]
- 22.DeLeo JA, Tanga FY, Tawfik VL. Neuroimmune activation and neuroinflammation in chronic pain and opioid tolerance/hyperalgesia. Neuroscientist. 2004;10(1):40–52. doi: 10.1177/1073858403259950. [DOI] [PubMed] [Google Scholar]
- 23.DeLeo JA, Winkelstein BA. Physiology of chronic spinal pain syndromes: from animal models to biomechanics. Spine. 2002;27(22):2526–37. doi: 10.1097/00007632-200211150-00026. [DOI] [PubMed] [Google Scholar]
- 24.de Alteriis M, Fanning T. A public health model of Medicaid emergency room use. Health Care Financing Review. 1991;12(3):15–20. [PMC free article] [PubMed] [Google Scholar]
- 25.Altman DG, Schulz KF, Moher D, et al. The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Annals of Internal Medicine. 2001;134(8):663–94. doi: 10.7326/0003-4819-134-8-200104170-00012. [DOI] [PubMed] [Google Scholar]
- 26.Moher D, Schulz KF, Altman DG, et al. The CONSORT statement: revised recommendations for improving the quality of reports of parallel group randomized trials. BMC Medical Research Methodology. 2001;1(1):2. doi: 10.1186/1471-2288-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moher D, Schulz KF, Altman D, et al. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. JAMA. 2001;285(15):1987–91. doi: 10.1001/jama.285.15.1987. [DOI] [PubMed] [Google Scholar]


