Abstract
Objectives. A 1993 study found a 25% higher risk of death among uninsured compared with privately insured adults. We analyzed the relationship between uninsurance and death with more recent data.
Methods. We conducted a survival analysis with data from the Third National Health and Nutrition Examination Survey. We analyzed participants aged 17 to 64 years to determine whether uninsurance at the time of interview predicted death.
Results. Among all participants, 3.1% (95% confidence interval [CI] = 2.5%, 3.7%) died. The hazard ratio for mortality among the uninsured compared with the insured, with adjustment for age and gender only, was 1.80 (95% CI = 1.44, 2.26). After additional adjustment for race/ethnicity, income, education, self- and physician-rated health status, body mass index, leisure exercise, smoking, and regular alcohol use, the uninsured were more likely to die (hazard ratio = 1.40; 95% CI = 1.06, 1.84) than those with insurance.
Conclusions. Uninsurance is associated with mortality. The strength of that association appears similar to that from a study that evaluated data from the mid-1980s, despite changes in medical therapeutics and the demography of the uninsured since that time.
The United States stands alone among industrialized nations in not providing health coverage to all of its citizens. Currently, 46 million Americans lack health coverage.1 Despite repeated attempts to expand health insurance, uninsurance remains commonplace among US adults.
Health insurance facilitates access to health care services and helps protect against the high costs of catastrophic illness. Relative to the uninsured, insured Americans are more likely to obtain recommended screening and care for chronic conditions2 and are less likely to suffer undiagnosed chronic conditions3 or to receive substandard medical care.4
Numerous investigators have found an association between uninsurance and death.5–14 The Institute of Medicine (IOM) estimated that 18 314 Americans aged between 25 and 64 years die annually because of lack of health insurance, comparable to deaths because of diabetes, stroke, or homicide in 2001 among persons aged 25 to 64 years.4 The IOM estimate was largely based on a single study by Franks et al.5 However, these data are now more than 20 years old; both medical therapeutics and the demography of the uninsured have changed in the interim.
We analyzed data from the Third National Health and Nutrition Examination Survey (NHANES III). NHANES III collected data on a representative sample of Americans, with vital status follow-up through 2000. Our objective was to evaluate the relationship between uninsurance and death.
METHODS
The National Center for Health Statistics (NCHS) conducted NHANES III between 1988 and 1994. The survey combined an interview, physical examination, and laboratory testing. NHANES III employed a complex sampling design to establish national estimates of disease prevalence among the noninstitutionalized civilian population in the United States.15 Staff performed interviews in English and Spanish.
The NHANES III Linked Mortality File matched NHANES III records to the National Death Index (NDI). The NCHS's linkage, which uses a probabilistic matching strategy through December 31, 2000, is described elsewhere.16 The NCHS perturbed the file to prevent reidentification of survey participants. Vital status was not altered in this process. The publicly released data yield survival analysis results virtually identical to the restricted-use NHANES III Linked Mortality File.17
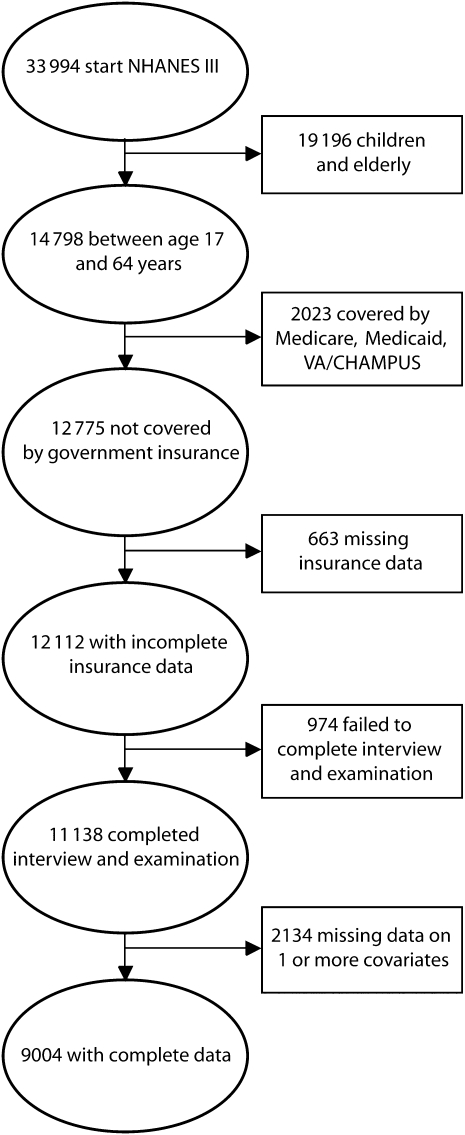
In designing our analysis, we hewed closely to Franks'5 methodology to facilitate interpretation of time trends. We analyzed data for individuals who reported no public source of health insurance at the time of the NHANES III interview. First, we excluded those aged older than 64 years, as virtually all are eligible for Medicare. Of the 33 994 individuals participating, 14 798 were aged between 17 and 64 years at the time of the interview. In keeping with earlier analyses,5–7,13 we also excluded nonelderly Medicare recipients and persons covered by Medicaid and the Department of Veterans Affairs/Civilian Health and Medical Program of the Uniformed Services military insurance (n = 2023), as a substantial proportion of those individuals had poor health status as a prerequisite for coverage. Of the 12 775 participants not covered by government insurance, we excluded 663 (5.2%) who lacked information on health insurance. We excluded 974 of the remaining 12 112 who were covered by private insurance or uninsured at the time of the interview because of failure to complete the interview and physical examination. Of the remaining 11 138, we included only the 9005 with complete baseline data from both the interview and physical examination in our final analysis (Figure 1). Among those with complete insurance data, those with complete interview and examination data were both less likely to be uninsured (16.4% vs 21.6%; P < .001) and less likely to die (3.0% vs 4.5%; P < .001).
FIGURE 1.
Study population and exclusions.
Note. NHANES III = National Health and Nutrition Examination Survey; VA/CHAMPUS = Veterans Affairs/Civilian Health and Medical Program of the Uniformed Services.
NHANES III staff interviewed respondents in their homes regarding demographics (including health insurance). Participants responded to questions about race, ethnicity, income, and household size. The sample design permits estimation for 3 racial/ethnic groups: non-Hispanic White, non-Hispanic Black, and Mexican American. The NCHS created a variable that combined family income and the poverty threshold during the year of interview (the poverty income ratio), allowing income to be standardized for family size and compared across the 6 years of data collection.18
NHANES III interviewers also collected data on education, employment, tobacco use, alcohol use, and leisure exercise. We analyzed education dichotomously, comparing those with 12 years or more education to those with less than 12 years. We considered respondents to be unemployed if they were looking for work, laid off, or unemployed. All others, including the employed, students, homemakers, and retirees were considered “not unemployed.” We considered smokers in 3 categories: current smokers, former smokers (those who had smoked more than 200 cigarettes in their lifetime), and nonsmokers. We labeled those drinking more than 6 alcoholic beverages per week as regular drinkers. We analyzed exercise in 2 groups: those achieving greater than or equal to 100 metabolic equivalents (METs) per month, versus those achieving less than 100 METs per month.19,20
NHANES III measured participants' self-perceived health in 5 categories: excellent, very good, good, fair, and poor. We combined the last 2 groups because of small numbers. NHANES physicians performed physical examinations on all participants and provided an impression of overall health status rated as excellent, very good, good, fair, and poor.21 We combined the final 2 groups because of small numbers. We analyzed body mass index (BMI; weight in kilograms divided by height in meters squared) in 4 categories: less than 18.5; 18.5 to 25; more than 25 to less than 30; and 30 and higher.
NHANES III oversampled several groups, including Black persons, Mexican Americans, the very young (aged 2 months to 5 years), and those aged older than 65 years. To account for this and other design variables we used the SUDAAN (version 9.1.3, Research Triangle Institute, Research Triangle Park, NC) SURVIVAL procedure and SAS (version 9.1, SAS Institute Inc, Cary, NC) PROC SURVEYFREQ to perform all analyses. We (as did Franks et al.5) employed unweighted survival analyses and controlled for the variables used in determining the sampling weights (age, gender, and race/ethnicity) because of the inefficiency of weighted regression analyses.22
We analyzed the relation between insurance, demographics, baseline health status variables, and mortality by using χ2 tests. We then used a Cox proportional hazards survival analysis controlling only for age and gender to determine if lack of health insurance predicted mortality. We repeated the analysis of the relationship of insurance to mortality after forcing all covariates in the model. In this Cox proportional hazards analysis, we controlled for gender, age, race/ethnicity (4 categories), income (poverty income ratio), education, current unemployment, smoking status (3 categories), regular alcohol use, self-rated health (4 categories), physician-rated health (4 categories), and BMI (4 categories). We tested for significant interactions between these variables and health insurance status (i.e., P < .05). We handled tied failure times by using the Efron method.
We performed multiple sensitivity analyses to analyze the robustness of our results. We developed a propensity score model and controlled for the variables in our previous models (with the exception of health insurance status), as well as marital status; household size; census region; number of overnight visits in hospital in past 12 months; number of visits to a physician in past 12 months; limitations in work or activities; job or housework changes or job cessation because of a disability or health problem; and number of self-reported chronic diseases, including emphysema, prior nonskin malignancy, stroke, congestive heart failure, hypertension, diabetes, or hypercholesterolemia. Next, we included the propensity score in the multivariable model with the indicator for insurance status. In addition, we tested for the effect of including those covered by Medicaid by using our original Cox model and the propensity score adjusted analysis. In a subsidiary analysis, we excluded employment and self- and physician-rated health, as these covariates may be a result of limited access to health care because of uninsurance.
To facilitate interpretation of our hazard ratio, we first replicated the calculation in the IOM report to estimate the number of US adults who die annually because of lack of health insurance. This approach applies the overall hazard ratio to 9-year age strata and sums these figures to arrive at an annual number of deaths attributable to lack of health insurance. We then recalculated this figure by using the slightly different approach utilized by the Urban Institute, which does not age stratify when calculating total mortality. We believe this approach to be more accurate than that used to produce the IOM estimate, as it calculates mortality from the entire age range that the hazard ratio was calculated from, as opposed to calculating mortality over 10-year age strata.23
RESULTS
We display baseline characteristics of the sample in Table 1; 9004 individuals contributed 80 657 person-years of follow-up time between 1988 and 2000. Of these, 16.2% (95% confidence interval [CI] = 14.1%, 18.2%) were uninsured at the time of interview. Uninsurance was associated with younger age, minority race/ethnicity, unemployment, smoking, exercise (less than 100 METs per month), self-rated health, and lower levels of education and income (P < .001 for all comparisons). Regular alcohol use and physician-rated health were also associated with higher rates of uninsurance (P < .05 for both comparisons).
TABLE 1.
Insurance and Mortality Among Nonelderly US Adults Aged 17 to 64 Years: NHANES III (1986–1994) With Follow-Up Through 2000
| Characteristic | No. (weighted %) | % Uninsured (SE) | % Died (SE) |
| Vital status as of December 31, 2000 | |||
| Alive | 8653 (96.9) | 16.2 (1.0) | 0 |
| Deceased | 351 (3.1) | 17.2 (2.8) | 100 |
| Insurance statusa | |||
| Privately insured | 6655 (83.8) | 0 | 3.0 (0.3) |
| Uninsured | 2350 (16.2) | 100 | 3.3 (0.6) |
| Gender | |||
| Female | 4695 (50.2) | 15.1 (1.1) | 2.6 (0.3) |
| Male | 4311 (49.8) | 17.3 (1.3) | 3.5 (0.4) |
| Age, y | |||
| 17–24 | 1750 (17.1) | 28.5 (2.5) | 0.7 (0.2) |
| 25–34 | 2338 (27.1) | 19.7 (1.5) | 1.4 (0.4) |
| 35–44 | 2177 (26.2) | 11.6 (1.2) | 1.7 (0.3) |
| 45–54 | 1529 (16.8) | 10.8 (1.4) | 5.1 (0.9) |
| 55–64 | 1344 (12.7) | 8.9 (1.4) | 10.7 (1.1) |
| Race/ethnicity | |||
| Non-Hispanic White | 3484 (78.1) | 12.3 (0.8) | 3.1 (0.4) |
| Non-Hispanic Black | 2567 (9.9) | 22.6 (2.1) | 4.1 (0.5) |
| Mexican American | 2598 (5.1) | 45.5 (1.9) | 3.1 (0.4) |
| Other | 355 (6.9) | 29.5 (7.3) | 0.9 (0.4) |
| Education, y | |||
| < 12 | 2917 (19.6) | 37.4 (3.0) | 4.1 (0.5) |
| ≥ 12 | 6087 (80.4) | 11.0 (0.7) | 2.8 (0.3) |
| Employment | |||
| Unemployedb | 511 (4.0) | 49.8 (3.9) | 5.3 (1.3) |
| All others | 8493 (96.0) | 14.8 (0.9) | 3.0 (0.3) |
| Poverty income ratioc | |||
| 0–1 | 1678 (9.2) | 56.2 (2.7) | 4.3 (0.9) |
| > 1–3 | 4171 (39.7) | 22.1 (1.7) | 3.0 (0.3) |
| > 3 | 3155 (51.2) | 4.4 (0.5) | 3.0 (0.4) |
| Smoking status | |||
| Current smoker | 2465 (29.1) | 22.8 (1.8) | 4.6 (0.5) |
| Former smokerd | 1794 (22.3) | 10.4 (1.1) | 4.2 (0.7) |
| Nonsmoker | 4745 (48.6) | 14.9 (1.1) | 1.7 (0.3) |
| Drinking status, alcoholic drinks/wk | |||
| < 6 | 7193 (78.3) | 15.3 (1.1) | 4.3 (0.7) |
| ≥ 6 | 1811 (21.7) | 19.6 (1.5) | 2.8 (0.4) |
| Exercise, METs/mo | |||
| ≥ 100 | 3475 (42.0) | 13.7 (1.1) | 2.9 (0.4) |
| < 100 | 5529 (58.0) | 18.0 (1.1) | 3.2 (0.4) |
| Self-rated health | |||
| Excellent | 1675 (23.4) | 9.3 (1.3) | 2.0 (0.4) |
| Very good | 2499 (34.9) | 12.0 (0.9) | 1.4 (0.4) |
| Good | 3288 (31.7) | 20.5 (1.9) | 3.3 (0.4) |
| Fair or poor | 1542 (9.9) | 33.6 (2.5) | 10.8 (1.2) |
| Physician-rated health on examination | |||
| Excellent | 4627 (54.2) | 16.8 (1.2) | 1.8 (0.3) |
| Very good | 2179 (24.4) | 13.3 (1.2) | 2.6 (0.5) |
| Good | 1858 (18.4) | 17.2 (1.4) | 4.9 (0.7) |
| Fair or poor | 340 (3.0) | 21.7 (4.8) | 19.0 (2.6) |
| Measured BMI | |||
| < 18.5 | 205 (2.7) | 19.8 (4.0) | 4.0 (1.4) |
| 18.5–25 | 3764 (46.8) | 16.4 (1.2) | 2.4 (0.3) |
| > 25–< 30 | 2853 (30.4) | 14.9 (1.2) | 3.3 (0.7) |
| ≥ 30 | 2182 (20.0) | 17.2 (1.8) | 4.3 (0.8) |
Notes. BMI = body mass index (weight in kg divided by height in meters squared); METs = metabolic equivalents; NHANES = National Health and Nutrition Examination Survey.
For those with complete data for all characteristics; excludes those covered by any government insurance.
Looking for work, laid off, or unemployed.
Combines family income, poverty threshold, and year of survey to allow analysis of income data across the 6 years of NHANES III; less than 1 indicates less than the poverty threshold.
Smoked more than 200 cigarettes in lifetime.
By the end of follow-up in 2000, 351 individuals, or 3.1% (95% CI = 2.5%, 3.7%) of the sample, had died (Table 1). Significant bivariate predictors of mortality included male gender (P = .04), age (P < .001), minority race/ethnicity (P < .001), less than 12 years of education (P = .008), unemployment (P = .02), smoking (P < .001), regular alcohol use (P = .04), worse self-rated health status (P < .001), and worse physician-rated health status (P < .001).
In the model adjusted only for age and gender, lack of health insurance was significantly associated with mortality (hazard ratio [HR] = 1.80; 95% CI = 1.44, 2.26). In subsequent models adjusted for gender, age, race/ethnicity, poverty income ratio, education, unemployment, smoking, regular alcohol use, self-rated health, physician-rated health, and BMI, lack of health insurance significantly increased the risk of mortality (HR = 1.40; 95% CI = 1.06, 1.84; Table 2). We detected no significant interactions between lack of health insurance and any other variables. Our sensitivity analyses yielded substantially similar estimates.
TABLE 2.
Adjusted Hazards for Mortality Among US Adults Aged 17 to 64 Years: NHANES III, 1988–2000
| Characteristic | Hazards Ratio (95% CI) |
| Insurance status | |
| Privately insureda (Ref) | 1.00 |
| Uninsured | 1.40 (1.06, 1.84) |
| Ageb | 1.06 (1.05, 1.07) |
| Gender | |
| Female (Ref) | 1.00 |
| Male | 1.37 (1.13, 1.68) |
| Race/ethnicity | |
| Non-Hispanic White (Ref) | 1.00 |
| Non-Hispanic Black | 1.32 (0.98, 1.79) |
| Mexican American | 0.88 (0.64, 1.19) |
| Other | 0.46 (0.24, 0.90) |
| Exercise, METs/mo | |
| ≥ 100 (Ref) | 1.00 |
| < 100 | 1.05 (0.80, 1.38) |
| Smoking status | |
| Nonsmoker (Ref) | 1.00 |
| Current smoker | 2.02 (1.43, 2.85) |
| Former smokerc | 1.42 (1.09, 1.85) |
| Drinking status, alcoholic drinks/wk | |
| < 6 (Ref) | 1.00 |
| ≥ 6 | 1.38 (0.99, 1.92) |
| Education, y | |
| ≥ 12 (Ref) | 1.00 |
| < 12 | 0.98 (0.75, 1.27) |
| Employment | |
| Not unemployedd (Ref) | 1.00 |
| Unemployed | 1.40 (0.92, 2.14) |
| Self-rated health | |
| Excellent (Ref) | 1.00 |
| Very good | 0.67 (0.42, 1.09) |
| Good | 1.27 (0.84, 1.90) |
| Fair or poor | 2.26 (1.40, 3.64) |
| Physician-rated health | |
| Excellent (Ref) | 1.00 |
| Very good | 0.99 (0.77, 1.27) |
| Good | 1.17 (0.90, 1.52) |
| Fair or poor | 3.22 (2.26, 4.58) |
| Measured BMI | |
| < 18.5 | 1.26 (0.69, 2.29) |
| 18.5–25 (Ref) | 1.00 |
| > 25–< 30 | 0.87 (0.66, 1.15) |
| ≥ 30 | 0.89 (0.69, 1.15) |
| Poverty income ratioe | 1.03 (0.95, 1.12) |
Notes. BMI = body mass index (weight in kg divided by height in meters squared); CI = confidence interval; METs = metabolic equivalents.
For those with complete data for all characteristics; excludes those covered by any government insurance.
Hazard ratio reflects risk for every 1-year increase in age.
Smoked more than 200 cigarettes in lifetime.
Looking for work, laid off, or unemployed.
Combines family income, poverty threshold, and year of survey to allow analysis of income data across the 6 years of NHANES III; less than 1 indicates less than the poverty threshold. Entered into regression model as a continuous variable. Hazard ratio represents change for every 1 unit increase in the poverty income ratio.
Replicating the methods of the IOM panel with updated census data24,25 and this hazard ratio, we calculated 27 424 deaths among Americans aged 25 to 64 years in 2000 associated with lack of health insurance. Applying this hazard ratio to census data from 200526 and including all persons aged 18 to 64 years yields an estimated 35 327 deaths annually among the nonelderly associated with lack of health insurance. When we repeated this approach without age stratification, (thought by investigators at the Urban Institute to be an overly conservative approach)23 we calculated approximately 44 789 deaths among Americans aged 18 to 64 years in 2005 associated with lack of health insurance.
DISCUSSION
The uninsured are more likely to die than are the privately insured. We used a nationally representative data set to update the oft-cited study by Franks et al. and demonstrate the persistence of increased mortality attributable to uninsurance. Our findings are in accord with earlier research showing that lack of health insurance increases the likelihood of death in select illnesses and populations.5–7,13 Our estimate for annual deaths attributable to uninsurance among working-age Americans is more than 140% larger than the IOM's earlier figure.23
By using methodologies similar to those used in the 1993 study, we found that being uninsured is associated with a similar hazard for mortality (1.40 for our study vs 1.25 for the 1993 study). Although the NHANES I study methodology and population were similar to those used in NHANES III, differences exist. The population analyzed in the original study was older on average than were participants in our sample (22.8% vs 55.6% aged 34 years or younger). The maximum length of follow-up was less (16 years vs 12 years), and the earlier analysis was limited to White and Black persons, whereas the present study also includes Mexican Americans.
The relative youthfulness and shorter follow-up in our study population would be expected to reduce our power to detect an elevated risk of death. In addition, if gaining Medicare reduces the effect of uninsurance on mortality, then the younger age and shorter length of follow-up in our study might strengthen the association between uninsurance and mortality compared with the earlier study. It is less clear how the differences in the racial and ethnic make-up of our study population would affect our ability to detect difference in risk of death. In fact, the increased likelihood of uninsurance among Mexican Americans who were nonetheless no more likely to die than non-Hispanic Whites might also be expected to reduce our power compared with the earlier study.
The original analysis confirmed vital status by review of decedents' death certificates. The NCHS had developed a probabilistic matching strategy to establish vital status. A subsample underwent death certificate review and verification; 98.7% were found to be correctly classified following this review.16 Again, it is not clear how any misclassification would bias our results. Moreover, Congress extended Medicare coverage in 1972 to 2 nonelderly groups: the long-term disabled and those with end-stage renal disease.27 So, although both studies excluded Medicare enrollees, only ours entirely excluded disabled nonelderly adults who are at particularly high risk of death.
The mechanisms by which health insurance affects mortality have been extensively studied. Indeed, the IOM issued an extensive report summarizing this evidence.29 The IOM identified 3 mechanisms by which insurance improves health: getting care when needed, having a regular source of care, and continuity of coverage.
The uninsured are more likely to go without needed care than the insured. For instance, Lurie et al. demonstrated that among a medically indigent population in California, loss of government-sponsored insurance was associated with decreased use of physician services and worsening control of hypertension.28,29 The uninsured are also more likely to visit the emergency department30 and be admitted to the hospital31 for “ambulatory care sensitive conditions,” suggesting that preventable illnesses are a consequence of uninsurance.
The chronically ill uninsured are also less likely to have a usual source of medical care,32 decreasing their likelihood of receiving preventative and primary care. Discontinuity of insurance is also harmful; those intermittently uninsured are more likely to die than the insured.13
All of these factors likely play a role in the decline in health among middle-aged uninsured persons detected by Baker et al.33,34 This trend appears to reverse at age 65, when the majority gains access to Medicare coverage.35 Other studies suggest that extending health insurance not only improves health, but also may be cost effective.36
Limitations
Our study has several limitations. NHANES III assessed health insurance at a single point in time and did not validate self-reported insurance status. We were unable to measure the effect of gaining or losing coverage after the interview. Point-in-time uninsurance is associated with subsequent uninsurance.6 Intermittent insurance coverage is common and accelerates the decline in health among middle-aged persons.33 Among the near-elderly, point-in-time uninsurance was associated with significant decline in overall health relative to those with private insurance.13 Earlier population-based surveys that did validate insurance status found that between 7% and 11% of those initially recorded as being uninsured were misclassified.13 If present, such misclassification might dilute the true effect of uninsurance in our sample. We excluded 29.5% of the sample because of missing data. These individuals were more likely to be uninsured and to die, which might also bias our estimate toward the null.
We have no information about duration of insurance coverage from this survey. Further, we have no data regarding cost sharing (out-of-pocket expenses) among the insured; cost sharing worsened blood pressure control among the poor in the RAND Health Insurance Experiment, and was associated with decreased use of essential medications, and increased rates of emergency department use and adverse events in a random sample of elderly and poor Canadians.37,38
Unmeasured characteristics (i.e., that individuals who place less value on health eschew both health insurance and healthy behaviors) might offer an alternative explanation for our findings. However, our analysis controlled for tobacco and alcohol use, along with obesity and exercise habits. In addition, research has found that more than 90% of nonelderly adults without insurance cite cost or lack of employer-sponsored coverage as reasons for being uninsured, whereas only 1% percent report “not needing” insurance.39 In fact, the variables included in our main survival analysis may inappropriately diminish the relationship between insurance and death. For example, poor physician-rated health, poor self-rated health, and unemployment may result from medically preventable conditions. Indeed, earlier analyses suggest that the true effect of uninsurance is likely larger than that measured in multivariate models.13,40 In addition, Hadley found that accounting for endogeneity bias by using an instrumental variable increases the protective effect of health insurance on mortality.40
Conclusions
Lack of health insurance is associated with as many as 44 789 deaths per year in the United States, more than those caused by kidney disease (n = 42 868).41 The increased risk of death attributable to uninsurance suggests that alternative measures of access to medical care for the uninsured, such as community health centers, do not provide the protection of private health insurance. Despite widespread acknowledgment that enacting universal coverage would be life saving, doing so remains politically thorny. Now that health reform is again on the political agenda, health professionals have the opportunity to advocate universal coverage.
Acknowledgments
A. P. Wilper was supported by a Health Resources and Service Administration National Research Service Award (5T32 HP110011).
Human Participant Protection
The institutional review board of Cambridge Health Alliance deemed this study exempt from formal review.
References
- 1.US Census Bureau Income, poverty, and health insurance coverage in the United States: 2007. Available at: http://www.census.gov/prod/2008pubs/p60-235.pdf. Accessed August 29, 2008
- 2.Ayanian JZ, Weissman JS, Schneider EC, Ginsburg JA, Zaslavsky AM. Unmet health needs of uninsured adults in the United States. JAMA 2000;284:2061–2069 [DOI] [PubMed] [Google Scholar]
- 3.Ayanian JZ, Zaslavsky AM, Weissman JS, Schneider EC, Ginsburg JA. Undiagnosed hypertension and hypercholesterolemia among uninsured and insured adults in the Third National Health and Nutrition Examination Survey. Am J Public Health 2003;93:2051–2054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Institute of Medicine Care Without Coverage, Too Little, Too Late. Washington, DC: The National Academies Press; 2002 [Google Scholar]
- 5.Franks P, Clancy CM, Gold MR. Health insurance and mortality. Evidence from a national cohort. JAMA 1993;270:737–741 [PubMed] [Google Scholar]
- 6.McWilliams JM, Zaslavsky AM, Meara E, Ayanian JZ. Health insurance coverage and mortality among the near-elderly. Health Aff (Millwood) 2004;23:223–233 [DOI] [PubMed] [Google Scholar]
- 7.Sorlie PD, Johnson NJ, Backlund E, Bradham DD. Mortality in the uninsured compared with that in persons with public and private health insurance. Arch Intern Med 1994;154:2409–2416 [PubMed] [Google Scholar]
- 8.Bennett CL, Horner RD, Weinstein RA, et al. Racial differences in care among hospitalized patients with Pneumocystis carinii pneumonia in Chicago, New York, Los Angeles, Miami, and Raleigh-Durham; Arch Intern Med 1995;155:1586–1592 [PubMed] [Google Scholar]
- 9.Ayanian JZ, Kohler BA, Abe T, Epstein AM. The relation between health insurance coverage and clinical outcomes among women with breast cancer. N Engl J Med 1993;329:326–331 [DOI] [PubMed] [Google Scholar]
- 10.Roetzheim RG, Gonzalez EC, Ferrante JM, Pal N, Van Durme DJ, Krischer JP. Effects of health insurance and race on breast carcinoma treatments and outcomes. Cancer 2000;89:2202–2213 [DOI] [PubMed] [Google Scholar]
- 11.Roetzheim RG, Pal N, Gonzalez EC, Ferrante JM, Van Durme DJ, Krischer JP. Effects of health insurance and race on colorectal cancer treatments and outcomes. Am J Public Health 2000;90:1746–1754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Canto JG, Rogers WJ, French WJ, Gore JM, Chandra NC, Barron HV. Payer status and the utilization of hospital resources in acute myocardial infarction: a report from the National Registry of Myocardial Infarction 2. Arch Intern Med 2000;160:817–823 [DOI] [PubMed] [Google Scholar]
- 13.Baker DW, Sudano JJ, Durazo-Arvizu R, Feinglass J, Witt WP, Thompson J. Health insurance coverage and the risk of decline in overall health and death among the near elderly, 1992-2002. Med Care 2006;44:277–282 [DOI] [PubMed] [Google Scholar]
- 14.Bhattacharya J, Goldman D, Sood N. The link between public and private insurance and HIV-related mortality. J Health Econ 2003;22:1105–1122 [DOI] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention National Health and Nutrition Examination III data files, documentation, and SAS code. Available at: http://www.cdc.gov/nchs/about/major/nhanes/nh3data.htm. Accessed May 9, 2008
- 16.Centers for Disease Control and Prevention National Health and Nutrition Examination III Linked Mortality File: Matching Methodology. Available at: http://www.cdc.gov/nchs/data/datalinkage/matching_methodology_nhanes3_final.pdf. Accessed April 8, 2008
- 17.Wheatcroft G, Cox CS, Lochner KA. Comparative analysis of the NHANES III public-use and restricted-use linked mortality files. Available at: http://www.cdc.gov/nchs/data/datalinkage/nh3_mort_compare_2007_final.pdf. Accessed April 14, 2008
- 18.Centers for Disease Control and Prevention National Health and Nutrition Examination III adult data file documentation. Available at: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Datasets/NHANES/NHANESIII/1A/ADULT-acc.pdf. Accessed April 14, 2008
- 19.Centers for Disease Control and Prevention Physical activity for everyone Web site. Available at: http://www.cdc.gov/nccdphp/dnpa/physical/everyone/recommendations/index.htm. Accessed April 16, 2008
- 20.Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation 2007;116:1081–1093 [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention National Health and Nutrition Examination III, Cycle 2 Physician Examiner's Training Manual. Available at: http://www.cdc.gov/nchs/data/nhanes/nhanes3/cdrom/nchs/manuals/phys.pdf. Accessed April 8, 2008
- 22.Korn EL, Graubard BI. Analysis of Health Surveys. Wiley Series in Probability and Statistics New York, NY: Wiley; 1999 [Google Scholar]
- 23.Dorn S. Uninsured and Dying Because of It: Updating the Institute of Medicine Analysis on the Impact of Uninsurance on Mortality. Available at: http://www.urban.org/UploadedPDF/411588_uninsured_dying.pdf. Accessed April 23, 2008
- 24.US Census Bureau Health insurance coverage status and type of coverage all persons by age and sex: 1999 to 2007. Available at: http://www.census.gov/hhes/www/hlthins/historic/hihistt2.xls. Accessed August 25, 2009
- 25.Centers for Disease Control and Prevention, National Center for Health Statistics Death rates by 10-year age groups: United States and each state, 2000. Available at: http://www.cdc.gov/nchs/data/statab/VS00100_TABLE23A.pdf. Accessed August 25, 2009
- 26.Centers for Disease Control and Prevention, National Center for Health Statistics Death rates by 10-year age groups: United States and each state, 2005. Available at: http://www.cdc.gov/nchs/data/statab/MortFinal2005_Worktable23R.pdf. Accessed August 25, 2009
- 27.Centers for Medicare and Medicaid Services Key milestones in CMS programs. Available at: http://www.cms.hhs.gov/History/Downloads/CMSProgramKeyMilestones.pdf. Accessed May 20, 2008
- 28.Lurie N, Ward NB, Shapiro MF, Brook RH. Termination from Medi-Cal–does it affect health? N Engl J Med 1984;311:480–484 [DOI] [PubMed] [Google Scholar]
- 29.Lurie N, Ward NB, Shapiro MF, Gallego C, Vaghaiwalla R, Brook RH. Termination of Medi-Cal benefits. A follow-up study one year later. N Engl J Med 1986;314:1266–1268 [DOI] [PubMed] [Google Scholar]
- 30.Oster A, Bindman AB. Emergency department visits for ambulatory care sensitive conditions: insights into preventable hospitalizations. Med Care 2003;41:198–207 [DOI] [PubMed] [Google Scholar]
- 31.Weissman JS, Gatsonis C, Epstein AM. Rates of avoidable hospitalization by insurance status in Massachusetts and Maryland. JAMA 1992;268:2388–2394 [PubMed] [Google Scholar]
- 32.Wilper AP, Woolhandler S, Lasser KL, McCormick D, Bor DH, Himmelstein DU. Chronically ill and uninsured: a national study of disease prevalence and access to care among U.S. adults. Ann Intern Med. 2008;149:170–176 [DOI] [PubMed] [Google Scholar]
- 33.Baker DW, Sudano JJ, Albert JM, Borawski EA, Dor A. Lack of health insurance and decline in overall health in late middle age. N Engl J Med 2001;345:1106–1112 [DOI] [PubMed] [Google Scholar]
- 34.Baker DW, Sudano JJ, Albert JM, Borawski EA, Dor A. Loss of health insurance and the risk for a decline in self-reported health and physical functioning. Med Care 2002;40:1126–1131 [DOI] [PubMed] [Google Scholar]
- 35.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Health of previously uninsured adults after acquiring Medicare coverage. JAMA 2007;298:2886–2894 [DOI] [PubMed] [Google Scholar]
- 36.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Use of health services by previously uninsured Medicare beneficiaries. N Engl J Med 2007;357:143–153 [DOI] [PubMed] [Google Scholar]
- 37.Newhouse J. Free for All? Lessons From the RAND Health Insurance Experiment. Cambridge, MA: Harvard University Press; 1993 [Google Scholar]
- 38.Tamblyn R, Laprise R, Hanley JA, et al. Adverse events associated with prescription drug cost-sharing among poor and elderly persons. JAMA 2001;285:421–429 [DOI] [PubMed] [Google Scholar]
- 39.Graves JA, Long SK. Why do people lack health insurance? Health Policy Online: Timely Analysis of Current Trends and Policy Options. Available at: http://www.urban.org/UploadedPDF/411317_lack_health_ins.pdf. Accessed May 29, 2008
- 40.Hadley J, Waidmann T. Health insurance and health at age 65: implications for medical care spending on new Medicare beneficiaries. Health Serv Res 2006;41:429–451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kung H, Hyoert D, Xu J, et al. Deaths: final data for 2005. Natl Vital Stat Rep 2008;56(10). Available at: http://www.cdc.gov/nchs/data/nvsr/nvsr56/nvsr56_10.pdf. Accessed February 17, 2009 [PubMed]