Abstract
Objectives. We predicted the future economic burden attributable to high rates of current adolescent overweight.
Methods. We constructed models to simulate the costs of excess obesity and associated diabetes and coronary heart disease (CHD) among adults aged 35–64 years in the US population in 2020 to 2050.
Results. Current adolescent overweight is projected to result in 161 million life-years complicated by obesity, diabetes, or CHD and 1.5 million life-years lost. The cumulative excess attributable total costs are estimated at $254 billion: $208 billion because of lost productivity from earlier death or morbidity and $46 billion from direct medical costs. Currently available therapies for hypertension, hyperlipidemia, and diabetes, used according to guidelines, if applied in the future, would result in modest reductions in excess mortality (decreased to 1.1 million life-years lost) but increase total excess costs by another $7 billion (increased to $261 billion total).
Conclusions. Current adolescent overweight will likely lead to large future economic and health burdens, especially lost productivity from premature death and disability. Application of currently available medical treatments will not greatly reduce these future burdens of increased adult obesity.
Excessive weight gain in childhood and adolescence has risen over the past several decades. The prevalence of overweight adolescents tripled between the 1970s and 2000 and reached 17% as of 2000 to 2004.1 Overweight adolescents are likely to become obese adults,2–4 thereby producing a substantial, long-lasting future health burden. The prevalence of adult obesity was reported to be 34% in 2007.5 A recent study forecast that current adolescent overweight will increase future adult obesity by 5% to 15% by 2035, resulting in more than 100 000 excess prevalent cases of coronary heart disease (CHD) by 2035.1
The economic burden attributable to this future excess obesity has not been estimated. In addition to the costs of medical treatment of the higher rates of obesity, CHD, and other obesity-related illness such as diabetes, the costs of lost productivity resulting from premature morbidity and mortality in the working-age population may also be high.
We used the CHD Policy Model6–8 to estimate the increase from 2020 to 2050 in adult obesity, obesity-associated CHD, and obesity-related diabetes attributable to increases in prevalence of adolescent overweight between the late 1970s and 2000. We then estimated the attributable increases in direct medical costs and indirect productivity costs. We also estimated the economic costs associated with medical treatment protocols (or standards of care or policies) that might mitigate the projected rise of modifiable, obesity-related cardiovascular risk factors.
METHODS
The CHD Policy Model is a computer-simulation, state-transition (Markov cohort) model of the incidence, prevalence, mortality, and costs of CHD in US residents aged 35 to 84 years.6–8 The demographic–epidemiological submodel predicts the incidence of CHD and death from other causes among persons without CHD, stratified according to age, gender, and as many as 6 categorized risk factors, including diastolic blood pressure, smoking status, levels of high-density lipoprotein (HDL) and low-density lipoprotein (LDL) cholesterol, body mass index (BMI; defined as weight in kilograms divided by height in meters squared), and the presence or absence of diabetes mellitus.
After CHD develops, the bridge submodel characterizes the initial CHD event (cardiac arrest, myocardial infarction, or angina) and its sequelae for 30 days. Then, the disease history submodel predicts the number of subsequent CHD events, revascularization procedures, and deaths from CHD and other causes among persons with CHD, stratified according to age, gender, and history of events. All population distributions, risk factor levels, coefficients, event rates, case-fatality rates, and costs can be modified. The predictions of the current version of the model have been validated with data from randomized controlled trials for the reduction in coronary events with statins and other risk factors.9–11
Obesity Estimates
We defined adolescent overweight as BMI above the 95th percentile on the growth charts of the Centers for Disease Control and Prevention12 and adult obesity as a BMI of 30 kg/m2 or higher.13 We used data from the National Health and Nutrition Examination Survey for 1971 to 1974, 1976 to 1980, 1988 to 1994, and 1999 to 2000 to determine the proportion of adolescents aged between 12 and 19 years who were above the 95th percentile for BMI and the proportion of obese 35-year-old adults.13,14 We then estimated a linear time trend function derived from these historical data to predict the rate at which overweight adolescents become obese adults 20 years later.
We implemented the change in the prevalence of obesity as a shift in the distribution of adult BMI, assuming the magnitude of the shift was proportional to the projected increase in mean BMI. After age 35, we applied transition probabilities derived from the BMI distribution to simulate the natural increase in BMI that occurs with age. For each historical trend, we modeled separate projections of future obesity. We decided, on the basis of our analysis of data from the Framingham Heart Study and other epidemiological data, not to assign a CHD risk function to obesity but to assume that increased BMI results in higher rates of CHD, primarily through its effects on diastolic blood pressure, LDL and HDL cholesterol, and diabetes.1 The resulting relative risk of death from any cause attributable to obesity in our model was not statistically different from those reported in previous studies, such as Flegal et al.15
Assumptions About Future Treatment Policies
We modeled 4 medical treatment policies, or settings, in which treatments for CHD risk factors and for hyperglycemia became progressively more intensive. In these analyses, hypertension was treated with chlorthalidone; additional treatment of diabetic patients included angiotensin-converting enzyme inhibitors.16–18 Hyperlipidemia (elevated LDL cholesterol) was treated with statins.18–21 Glycemic control for diabetic patients was achieved with insulin and oral antiglycemic agents.21,22
The costs and effectiveness of statin and glycemic treatments were estimated from randomized controlled trial data.16–18,21–24 The costs of these medical treatments included the costs of professional visits, blood draws, laboratory tests and evaluations, and side effects. However, we assumed that all diagnoses of hypertension, hyperglycemia, and diabetes would be made at routine periodic visits to health care providers at no additional cost.
Direct and Indirect Costs
We divided economic costs into direct medical costs and indirect costs resulting from loss of productivity stemming from morbidity and premature mortality. The annual cost of health care by chronic condition and normal weight are shown in Table 1. (Other parameters used in the simulation are in Tables A–C, available as a supplement to the online version of this article at http://www.ajph.org.) We reported all costs in 2007 US dollars. Future costs were discounted at 3% annually, with 2007 as the baseline year.
TABLE 1.
Estimated Annual Excess Health Care Costs Of Chronic Conditions and Total Cost of Normal Weight Individuals: United States, 2020–2050
| Excess Costs, Chronic Conditions a |
Total Cost, Normal Weight,a $ | |||
| Age, y | Obesity, $ | Diabetes, $ | CHD, $ | |
| Men | ||||
| 35–44 | 219 | 3690 | 12 482 | 2 979 |
| 45–54 | 213 | 4914 | 15 206 | 4 230 |
| 55–64 | 215 | 4914 | 14 857 | 6 546 |
| 65–74 | 531 | 9229 | 11 538 | 9 293 |
| Women | ||||
| 35–44 | 219 | 3690 | 11 926 | 4 432 |
| 45–54 | 213 | 4914 | 16 687 | 5 719 |
| 55–64 | 215 | 4914 | 18 137 | 8 159 |
| 65–74 | 531 | 9229 | 15 302 | 11 310 |
Note. CHD = cardiovascular disease. Direct health care costs, expressed as 2007 dollars.
Cost per year per person; includes all costs of treatment.
Total CHD health care costs were estimated in 2007 dollars by the method of Hodgson and Cohen.25,26 We used data from the Medical Expenditure Panel Survey27 to estimate the proportion of expenditures attributable to CHD and applied that estimate to aggregate national data.28 We estimated the inpatient CHD cost component with California data,29 deflated first with California hospital-specific cost-to-charge ratios and then with the ratios30 of the US national average cost per patient admission to California's average cost per patient admission.31
We used 2 estimates for non-CHD costs. The base case used disease- and condition-specific estimates for obesity32 and diabetes33 from national survey data. A sensitivity analysis used non-CHD mortality and the distribution of non-CHD mortality risk factors (e.g., blood pressure, smoking, diabetes) to estimate non-CHD costs.1
Indirect costs were defined as the social value of lost productivity attributable to earlier mortality and morbidity as a result of excess obesity and associated CHD and diabetes. Indirect costs attributable to morbidity were lost work because of sick and disability leave, early long-term disability, and other early retirement and lost workdays caused by illness. We used employee compensation to measure the value of lost productivity; household production was excluded, following the definition of productivity used for the US national income and product accounts.34 The value of employee compensation was measured by median annual age- and gender-specific compensation for full- and part-time employees, including money wage35,36 and other employee benefits.37 We calculated the value of employee benefits from the money wage by adjusting for the proportion of total compensation derived from money income. Median wage served as a measure of per-person money compensation because obesity is concentrated at the lower end of the income distribution,38,39 and we considered the median to be a better measure of central tendency. In the base case, no productivity growth was assumed to occur between 2007 and 2050. An alternative case assumed a long-run annual productivity growth rate of 1.98%.40
We were unable to find published estimates for absence from work because of obesity, diabetes, and CHD simultaneously adjusted for diabetes and CHD. Therefore, we calculated overall indirect costs resulting from obesity and associated comorbidities; we then subtracted indirect costs attributable to diabetes and CHD from the total obesity costs. The indirect costs of diabetes were adjusted for presence of obesity and absence of CHD. We calculated the indirect costs of CHD with the assumption that these costs were driven by clinical events. For settings with aggressive glycemic control in diabetic patients, we adjusted indirect diabetes costs for treatments that included aggressive glycemic control, with the same proportional reduction in CHD events attributable to treatment.
Mortality costs, which were annual flow costs that measured the difference in production attributable to differences in alternative employed populations over the 2020 to 2050 simulation, were equal to the difference in annual population multiplied by the age- and gender-specific employment population ratios41 multiplied by the median wage by age and 10-year age category.35,36 We estimated morbidity-related productivity losses by the reduction in probability of employment attributable to the diseases among working adults with obesity42 (adjusted for sociodemographic characteristics, health behaviors, and absence of diabetes) and diabetes43 (adjusted for sociodemographic characteristics and health behaviors). We calculated workdays lost among the employed attributable to obesity44 and diabetes33,45 by the same method, except that the workdays lost were multiplied by the employment-to-population ratio.
The difference in the probability of employment among the obese is sensitive to the distribution of BMI and resulting differential rates of diabetes.46 We did not model the distribution of BMI among the obese. Therefore, for the main analysis, we used a conservative approach and adjusted overall indirect costs of obesity to exclude the effects of diabetes46,47; that is, we assumed that published estimates of differential employment by BMI included effects of diabetes among the obese, and we estimated the net loss of employment caused by obesity as being equal to the difference between obese persons without diabetes and their nonobese counterparts. A low-cost case incorporated similar assumptions but adjusted for both diabetes and CHD46,47 (i.e., assumed that the probability of employment and lost workdays for all obese persons was equal to that for nondiabetic obese without CHD). A high-cost case used published estimates with no adjustments for diabetes or CHD. A final sensitivity analysis estimated indirect costs by summing the subtotals for CHD, diabetes adjusted for the presence of obesity and absence of CHD, and obesity adjusted for no diabetes or obesity.
Both the probability of employment and workdays lost because of diabetes were adjusted for presence of obesity and absence of CHD according to observational data.45,46 For CHD, we assumed the average loss of employment to be 63%, the rate of not returning to work among workers after a myocardial infarction, angina, or other diagnosed CHD.48–51 This overall rate was adjusted by age and gender with odds ratios for the probability of employment among enrollees in cardiac rehabilitation programs.52 We could not find data for estimating lost workdays caused by CHD among those still employed, so we omitted this indirect cost.
Simulation Design
The simulations compared 2 adult populations aged 35 to 64 years, from 2020 to 2050, that were identical except for the prevalence of obesity that would result from the prevalence of adolescent overweight in 2000. In 1 population, the current overweight adolescents were projected to increase the number of obese adults; in the alternative case, they did not. Further details are described in our previous work.1 We compared the costs of the increased adult obesity with our 4 treatment settings.
Setting 1.
Historical treatment protocols observed around 2000 continue into the future (the base case). We simulated the prevalence and costs under an assumption that treatment protocols and the resulting distribution of cardiovascular risk factors as a function of the distribution of adult BMI that existed in 2000 would continue through 2050. We assumed that additional obesity was linked to a less favorable distribution of blood pressure, LDL and HDL cholesterol, and diabetes.
Setting 2.
Population-based primary prevention of cardiovascular risk factors through drug treatment is adopted. This hypothetical program would consist of treatments to lower diastolic blood pressure and LDL cholesterol for all adults, whether obese or not, treating diastolic blood pressure over 90 mmHg (treatment mean diastolic blood pressure reduced by 8.6 mmHg) with chlorthalidone, and LDL over 160 mg/dL (relative reduction in LDL of 27%) with low-potency statins.
Setting 3.
Treatment such as that in setting 2, plus more aggressive regimens, is adopted. Diabetic patients with elevated diastolic blood pressure would be treated with chlorothalidone and angiotensin-converting enzyme inhibitors to reach a target of 80 mmHg. Treatment of hyperlipidemia in diabetic patients would be more aggressive: high-potency statins to be given for LDL over 130 mg/dL, assuming a relative reduction in LDL of 54%, and low-potency statins to be prescribed for LDL between 100 mg/dL and 130 mg/dL.
Setting 4.
Treatment such as that in setting 3, plus glycemic control, is adopted. Diabetic patients would receive insulin or oral glycemic agents or both. Trials of tight glycemic control in diabetic patients have demonstrated benefit for non-CHD outcomes in the United Kingdom Prospective Diabetes Study, but the beneficial effects on CHD outcomes were not statistically significant. For purposes of this aggressive treatment setting, we optimistically assumed that glycemic control reduced both CHD and non-CHD events by 13%.18,21–24
For each year between 2020 and 2050, we estimated the excess number of 4 mutually exclusive states: life-years lost because of death, prevalent CHD, prevalent diabetes without CHD, and prevalent obesity without CHD or diabetes. We applied our estimates for direct medical costs (events and treatments) and indirect economic costs to these states each year.
RESULTS
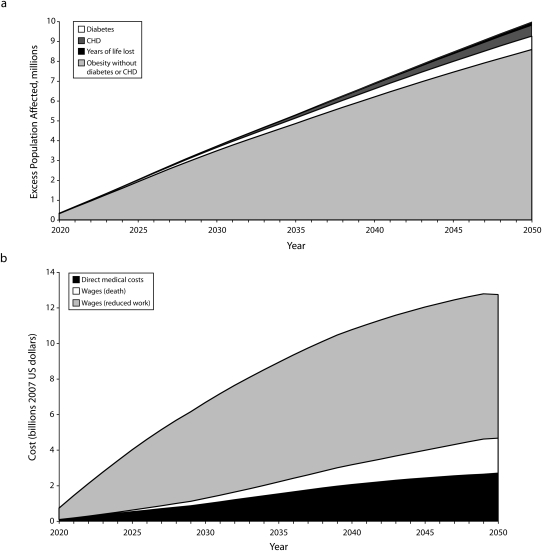
In treatment setting 1 (base case), current adolescent overweight is projected to increase the excess prevalence of total adult obesity resulting from adolescent overweight from 330 000 in 2020 to more than 9 700 000 in 2050. The number of additional obese individuals with CHD is estimated to increase to 540 000 by 2050, 5.6% of the total of excess obese persons. The number of excess diabetic patients without CHD is projected to increase to 680 000, representing 7.0% of the excess obese individuals (Figure 1a).
FIGURE 1.
The effect of increased adolescent overweight on future (a) excess obesity, diabetes, cardiovascular heart disease (CHD), and years of lost life and (b) total discounted direct and indirect costs: United States, 2020–2050.
Note. Discounted to 2007 dollars at 3% per year.
This excess future obesity is projected to increase mortality: the total adult population would be reduced by 165 000 persons by 2050. A cumulative total of 1.48 million life-years are projected to be lost between 2020 and 2050; 161 million healthy life-years in the population would be replaced by life-years with obesity; approximately 5.5 million of those life-years are projected to be lived with CHD and 9.4 million with diabetes without CHD (Table 2).
TABLE 2.
Projected Excess Mortality and Morbidity Attributable to Current Adolescent Obesity: United States, 2020–2050
| Mortality, 1 000 Life-Years Lost | Morbidity, 1 000 Life-Years |
||||
| Treatment Setting | CHD | Diabetes Without CHD | Obesity Onlya | Totalb | |
| Without additional treatments (setting 1, base case) | 1480 | 5500 | 9 390 | 146 000 | 161 000 |
| Universal treatment of hypertension and hyperlipidemia (setting 2) | 1190 | 4210 | 9 780 | 148 000 | 162 000 |
| Universal treatment of hypertension and hyperlipidemia, plus lower targets for patients with diabetes with these risk factors (setting 3) | 1090 | 3490 | 10 600 | 148 000 | 162 000 |
| Universal treatment of hypertension and hyperlipidemia, with lower targets for patients with diabetes with these risk factors, plus tight glycemic control for diabetes (setting 4) | 1060 | 3430 | 10 700 | 148 000 | 162 000 |
Note. CHD = cardiovascular disease.
Obesity without diabetes or CHD.
May not add up because of rounding.
Excess annual undiscounted attributable direct medical costs are estimated to increase from approximately $130 million in 2020 to $10 billion in 2050, with annual indirect costs of lost productivity rising from $942 million in 2020 to $36 billion in 2050. The cumulative discounted direct, indirect, and total costs between 2020 and 2050 are projected to be $46 billion, $208 billion, and $254 billion, respectively. The cumulative undiscounted costs are projected to be $125 billion, $544 billion, and $669 billion, respectively (Table 3). Most of the projected economic burden consists of indirect costs from lost productivity caused by premature death or absence from work, with direct health care costs accounting for only 12% to 21% of the total economic burden (Figure 1b).
TABLE 3.
Projected Excess Costs Attributable to Current Adolescent Obesity: United States, 2020–2050
| Indirect Costs |
|||||||
| Morbidity |
|||||||
| Treatment Setting | Mortality, $ | CHD, $ | Diabetes Without CHD, $ | Obesity Only,a $ | Total,b $ | Direct Medical Costs, $ | Total,b $ |
| Discounted costsc | |||||||
| Without additional treatments (setting 1, base case) | 24.6 | 38.8 | 13.6 | 131 | 208 | 46.1 | 254 |
| Universal treatment of hypertension and hyperlipidemia (setting 2) | 19.9 | 29.8 | 14.1 | 140 | 204 | 54.5 | 258 |
| Universal treatment of hypertension and hyperlipidemia, plus lower targets for patients with diabetes with these risk factors (setting 3) | 18.3 | 24.7 | 15.1 | 144 | 202 | 59.7 | 262 |
| Universal treatment of hypertension and hyperlipidemia, with lower targets for patients with diabetes with these risk factors, plus tight glycemic control for diabetes (setting 4) | 17.9 | 24.2 | 13.2 | 145 | 200 | 60.6 | 261 |
| Undiscounted costs | |||||||
| Without additional treatments (setting 1, base case) | 70.8 | 114 | 36.5 | 323 | 544 | 125 | 669 |
| Universal treatment of hypertension and hyperlipidemia (setting 2) | 57.2 | 87.4 | 37.9 | 350 | 533 | 146 | 679 |
| Universal treatment of hypertension and hyperlipidemia, plus lower targets for patients with diabetes with these risk factors (setting 3) | 52.4 | 72.2 | 40.7 | 363 | 528 | 156 | 684 |
| Universal treatment of hypertension and hyperlipidemia, with lower targets for patients with diabetes with these risk factors, plus tight glycemic control for diabetes (setting 4) | 51.4 | 70.9 | 35.7 | 364 | 522 | 162 | 684 |
Note. CHD = cardiovascular disease. Costs expressed as billions of 2007 dollars.
Without diagnosis of diabetes or CHD.
May not add up because of rounding.
Discounted to 2007 dollars at 3% per year.
The economic burden of future obesity resulting from current adolescent overweight is projected to affect both young and middle-aged adults. Even adults aged 35 to 44 years can be expected to experience economic loss from the excess morbidity and mortality attributable to obesity, with 83% of this cost coming from lost wages attributable to morbidity. The percentage of the economic cost attributable to direct health care costs and premature mortality (rather than to indirect costs of morbidity) is projected to increase from approximately 17% in adults aged 35 to 44 years in 2020 to a percentage of attributable direct costs of approximately 58% in men and 41% in women aged 55 to 64 years in 2050, because of a higher incidence of major CHD events with age.
Treatment with currently available therapies for hypertension, hyperlipidemia, and glycemic control would reduce the excess morbidity and mortality resulting from the projected increase in future obesity (Table 2), but even the most aggressive treatment (setting 4) is estimated to reduce excess mortality by only 28%, from 1.48 to 1.06 million life-years lost. In this setting, the projected number of life-years with CHD would be reduced by 38% (from 5.5 to 3.4 million). Treatment settings 2 and 3 are projected to yield smaller benefits.
Discounted direct medical costs in treatment settings 2 to 4 are estimated to increase by 18% to 31% over the base case costs (setting 1); indirect costs are estimated to decrease by only 2% to 4%. The total economic costs in all 3 treatment settings are projected to increase over the base case; the most aggressive treatment strategy (setting 4) would increase by approximately 3% (from $254 billion to $261 billion).
The sensitivity analysis with alternative non-CHD direct medical cost estimates reduced total costs slightly but did not materially change the comparative costs of the 4 treatment settings. In the sensitivity analysis that assumed that long-run labor productivity trends will continue to grow at a 1.98% rate per year, the indirect costs of adolescent obesity approximately doubled. The low estimates of morbidity-related indirect costs reduced indirect and total costs by between 2% and 4%; the high estimates increased obesity-related indirect, total indirect, and total costs by approximately 34%, 22%, and 17%, respectively. The sensitivity analysis that summed adjusted diabetes- and obesity-related indirect costs increased discounted indirect obesity costs by approximately 15% and total costs by 8%.
DISCUSSION
High rates of adolescent overweight are projected to increase future adult obesity, resulting in substantial future economic costs and health burdens. The economic costs are incurred primarily from lost productivity because a greater proportion of a young and middle-aged working population will be prematurely deceased or disabled from CHD, diabetes, or other obesity-related morbidity. Most of these costs cannot be avoided with currently available medical therapies, even according to the very optimistic assumptions in our models. Prevention of excessive weight gain in childhood and adolescence may be the only effective way to reduce the prevalence of serious chronic conditions and the resulting economic costs.
The forecasted excess costs through 2050 are substantial compared with the total current burden of obesity. Wolf and Colditz34 estimated that the annual direct, indirect, and total costs of obesity in 1995 were $82 billion, $64 billion, and $146 billion, respectively, in 2007 dollars. By 2050, the additional adult costs attributable to current adolescent overweight are projected to increase these direct costs by 10% to 13% and the indirect costs by 45% to 55%. The projected excess costs attributable to current adolescent overweight alone will be more than one third of the total costs of obesity in 1995. The cumulative discounted costs of work loss caused by obesity, according to the main and sensitivity analyses, are estimated to be between $196 billion and $254 billion.
Projections to 2050 cannot account for future medical advances that may combat diabetes and obesity, but our simulations suggest that these advances would need to be much more cost effective than currently available therapies to reverse the projected high future burden of disease. Our projected rates of obesity do not assume additional increasing trends for weight gain in adults. We also assume that the current rate of adolescent overweight will remain stable, which is consistent with recent work suggesting no additional increase in the prevalence of adolescent overweight from 1999 to 2006.53
Our results were conservative because we used traditional national productivity and income accounting methods to measure indirect productivity costs that ignored real human welfare costs of obesity, such as loss of household production, labor diverted into unpaid caregiving for disabled and ill relatives, and costs of pain and restricted activity resulting from disability in nonwork activities. These omitted costs included both the value of nonmarket consumption activities lost (leisure and household services) and the loss of human and social capital formation attributable to increased demands on informal caregivers and to disability in the chronically ill, from forgone education, training, and work experience.
Our estimates of direct medical cost focused on CHD and diabetes and may have underestimated other consequences of long-term, continuous obesity starting in adolescence. Examples of other conditions caused by obesity are liver disease,54 pregnancy complications for mother and child,55 several musculoskeletal disorders,56 and complications from surgery and in intensive care.57 Interactions have also been found between obesity and development of asthma,58 osteoarthritis,56,59 kidney disease,60 and severity of chronic obstructive pulmonary disease.61,62 Obesity has many serious consequences that increase costs and reduce population health and quality of life that were not included in these estimates.
Recent increases in adolescent overweight will lead to enormous future costs, primarily from productivity lost to premature death and disability among adults. Preventing the development of adolescent overweight as well as implementing effective weight-loss strategies for overweight adolescents before they reach adulthood could yield significant future savings in economic costs and population health.
Acknowledgments
The Framingham Heart Study (FHS) and the Framingham Offspring Study (FOS) are conducted and supported by the National Heart, Lung, and Blood Institute (NHLBI) in collaboration with the FHS and FOS investigators. Data collection from Olmsted County was supported in part by grants from the Public Health Service and the National Institutes of Health (AR30582 and RO1 HL 59205). This research was also supported by a grant from the Flight Attendants Medical Research Institute.
Note. This study used a limited-access data set obtained by the NHLBI; this article does not necessarily reflect the opinions or views of the FHS, the FOS, or the NHLBI.
Human Participant Protection
No protocol approval was required for this study because no human participants were involved.
References
- 1.Bibbins-Domingo K, Coxson P, Pletcher MJ, Lightwood J, Goldman L. Adolescent overweight and future adult coronary heart disease. N Engl J Med 2007;357(23):2371–2379 [DOI] [PubMed] [Google Scholar]
- 2.Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. The relation of childhood BMI to adult adiposity: the Bogalusa Heart Study. Pediatrics 2005;115(1):22–27 [DOI] [PubMed] [Google Scholar]
- 3.Serdula MK, Ivery D, Coates RJ, Freedman DS, Williamson DF, Byers T. Do obese children become obese adults? A review of the literature. Prev Med 1993;22(2):167–177 [DOI] [PubMed] [Google Scholar]
- 4.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med 1997;337(13):869–873 [DOI] [PubMed] [Google Scholar]
- 5.Ogden CL, Carroll MD, McDowell MA, Flegal KM. Obesity Among Adults in the United States—No Change Since 2003–2004 Hyattsville, MD: National Center for Health Statistics; 2007. NCHS Data Brief No 1 [Google Scholar]
- 6.Gaspoz JM, Coxson PG, Goldman PA, et al. Cost effectiveness of aspirin, clopidogrel, or both for secondary prevention of coronary heart disease. N Engl J Med 2002;346(23):1800–1806 [DOI] [PubMed] [Google Scholar]
- 7.Hunink MG, Goldman L, Tosteson AN, et al. The recent decline in mortality from coronary heart disease, 1980-1990. The effect of secular trends in risk factors and treatment. JAMA 1997;277(7):535–542 [PubMed] [Google Scholar]
- 8.Weinstein MC, Coxson PG, Williams LW, Pass TM, Stason WB, Goldman L. Forecasting coronary heart disease incidence, mortality, and cost: the Coronary Heart Disease Policy Model. Am J Public Health 1987;77(11):1417–1426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cholesterol Treatment Trialists' Collaborators Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomized trials of statins. Lancet 2005;366:1267–1278 [DOI] [PubMed] [Google Scholar]
- 10.West of Scotland Coronary Prevention Study Group Influence of pravastatin and plasma lipids on clinical events in the West of Scotland Coronary Prevention Study (WOSCOPS). Circulation 1998;97(15):1440–1445 [DOI] [PubMed] [Google Scholar]
- 11.Bibbins-Domingo K, Coxson P, Pletcher M, Lightwood J, Goldman L. Adolescent overweight and future adult coronary heart disease [supplementary appendix]. N Engl J Med 2007;357(23):2371–2379 Available at: http://content.nejm.org/cgi/content/full/357/23/2371/DC1. Accessed August 28, 2008 [DOI] [PubMed] [Google Scholar]
- 12.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11 2002;246:1–190 [PubMed] [Google Scholar]
- 13.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999-2002. JAMA 2004;291(23):2847–2850 [DOI] [PubMed] [Google Scholar]
- 14.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA 2006;295(13):1549–1555 [DOI] [PubMed] [Google Scholar]
- 15.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA 2005;293(15):1861–1867 [DOI] [PubMed] [Google Scholar]
- 16.Ramsey S, Summers KH, Leong SA, Birnbaum HG, Kemner JE, Greenberg P. Productivity and medical costs of diabetes in a large employer population. Diabetes Care 2002;25(1):23–29 [DOI] [PubMed] [Google Scholar]
- 17.Heidenreich PA, Davis BR, Cutler JA, et al. Cost-effectiveness of chlorthalidone, amlodipine, and lisinopril as first-step treatment for patients with hypertension: an analysis of the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). J Gen Intern Med 2008;23(5):509–516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.CDC Diabetes Cost-Effectiveness Group Cost-effectiveness of intensive glycemic control, intensified hypertension control, and serum cholesterol level reduction for type 2 diabetes. JAMA 2002;287(19):2542–2551 [DOI] [PubMed] [Google Scholar]
- 19.Maron DJ, Fazio S, Linton MF. Current perspectives on statins. Circulation 2000;101(2):207–213 [DOI] [PubMed] [Google Scholar]
- 20.Pignone M, Earnshaw S, Tice JA, Pletcher MJ. Aspirin, statins, or both drugs for the primary prevention of coronary heart disease events in men: a cost-utility analysis. Ann Intern Med 2006;144(5):326–336 [DOI] [PubMed] [Google Scholar]
- 21.Clarke PM, Gray AM, Briggs A, et al. Cost-utility analyses of intensive blood glucose and tight blood pressure control in type 2 diabetes (UKPDS 72). Diabetologia 2005;48(5):868–877 [DOI] [PubMed] [Google Scholar]
- 22.UK Prospective Diabetes Study Group Intensive blood-glucose control with sulphonylureas or insulin compared to conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352:837–853 [PubMed] [Google Scholar]
- 23.Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998;352:854–865 [PubMed] [Google Scholar]
- 24.Gray A, Clarke P, Farmer A, Holman R, for the United Kingdom Prospective Diabetes Study (UKPDS) Group Implementing intensive control of blood glucose concentration and blood pressure in type 2 diabetes in England: cost analysis (UKPDS 63). BMJ 2002;325:860 Available at: http://www.bmj.com/cgi/reprint/325/7369/860. Accessed August 25, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hodgson TA, Cohen AJ. Medical expenditures for major diseases, 1995. Health Care Financ Rev 1999;21(2):119–164 [PMC free article] [PubMed] [Google Scholar]
- 26.Hodgson TA, Cohen AJ. Medical care expenditures for selected circulatory diseases: opportunities for reducing national health expenditures. Med Care 1999;37(10):994–1012 [DOI] [PubMed] [Google Scholar]
- 27.Agency for Healthcare Research and Quality Medical Expenditure Panel Survey public use files. 1996–2001. 2004. Available at: http://www.meps.ahrq.gov/mepsweb/index.jsp. Accessed May 17, 2004 [PubMed]
- 28.Centers for Medicare and Medicaid Services Personal health care spending by type of spending, age group, and source of payment distribution, calendar year 1999. 2000. Available at: http://www.cms.hhs.gov/NationalHealthExpendData/downloads/agetables.pdf. Accessed July 17, 2005
- 29.Healthcare Quality and Analysis Division California Patient Discharge Data, January 1–December 31, 2000, Public Version A-24 Sacramento, CA: California Office of Statewide Health Planning and Development; 2003 [Google Scholar]
- 30.California Office of Statewide Health Planning and Development, Healthcare Quality and Analysis Division Hospital annual financial data, pivot profiles. 1999–2000. 2003. Available at: http://www.oshpd.ca.gov/HID/Products/Hospitals/AnnFinanData/PivotProfles/default.asp. Accessed June 4, 2008
- 31.Statistical Abstract of the United States, Average Cost to Community Hospitals per Patient, by State Washington, DC: US Census Bureau; 1998: (Table 204). [Google Scholar]
- 32.Finkelstein EA, Ruhm CJ, Kosa KM. Economic causes and consequences of obesity. Annu Rev Public Health 2005;26:239–257 [DOI] [PubMed] [Google Scholar]
- 33.Hogan P, Dall T, Nikolov P, American Diabetes Association Economic costs of diabetes in the US in 2002. Diabetes Care 2003;26(3):917–932 [DOI] [PubMed] [Google Scholar]
- 34.Wolf AM, Colditz GA. Current estimates of the economic cost of obesity in the United States. Obes Res 1998;6(2):97–106 [DOI] [PubMed] [Google Scholar]
- 35.US Census Bureau Current Population Survey. Annual Social and Economic (ASEC) Supplement: PINC-01. Selected characteristics of people 15 years and over by total money income in 2006, work experience in 2006, race, Hispanic origin, and sex (male). 2007. Available at: http://pubdb3.census.gov/macro/032007/perinc/new01_010.htm. Accessed July 21, 2008
- 36.US Census Bureau Current Population Survey. Annual Social and Economic (ASEC) Supplement: PINC-01. Selected characteristics of people 15 years and over by total money income in 2006, work experience in 2006, race, Hispanic origin, and sex (female). 2007. Available at: http://pubdb3.census.gov/macro/032007/perinc/new01_019.htm. Accessed July 21, 2008
- 37.Bureau of Labor Statistics National Compensation Survey. Employer cost for employee compensation (NAICS basis). 2008. Available at: http://www.bls.gov/ncs/home.htm#data. Accessed July 21, 2008
- 38.Drewnowski A. The real contribution of added sugars and fats to obesity. Epidemiol Rev 2007;29:160–171 [DOI] [PubMed] [Google Scholar]
- 39.Rosin O. The economic causes of obesity: a survey. J Econ Surv 2008;22(4):617–647 [Google Scholar]
- 40.Edge RM, Laubach T, Williams JC. Learning and shifts in long-run productivity growth. J Monet Econ 2007;54:2421–2438 [Google Scholar]
- 41.Bureau of Labor Statistics Current Population Survey. Unemployment statistics. 2008Available at: http://www.bls.gov/cps/home.htm. Accessed July 17, 2008
- 42.Tunceli K, Li K, Williams LK. Long-term effects of obesity on employment and work limitations among U.S. Adults, 1986 to 1999. Obesity (Silver Spring) 2006;14(9):1637–1646 [DOI] [PubMed] [Google Scholar]
- 43.Yassin AS, Beckles GL, Messonnier ML. Disability and its economic impact among adults with diabetes. J Occup Environ Med 2002;44(2):136–142 [DOI] [PubMed] [Google Scholar]
- 44.Finkelstein E, Fiebelkorn C, Wang G. The costs of obesity among full-time employees. Am J Health Promot 2005;20(1):45–51 [DOI] [PubMed] [Google Scholar]
- 45.Gregg EW, Beckles GL, Williamson DF, et al. Diabetes and physical disability among older U.S. adults. Diabetes Care 2000;23(9):1272–1277 [DOI] [PubMed] [Google Scholar]
- 46.Cawley J, Rizzo J, Haas K. The association of diabetes with job absenteeism costs among obese and morbidly obese workers. J Occup Environ Med 2008;50(5):527–534 [DOI] [PubMed] [Google Scholar]
- 47.Månsson NO, Eriksson KF, Israelsson B, Ranstam J, Melander A, Råstam L. Body mass index and disability pension in middle-aged men—non-linear relations. Int J Epidemiol 1996;25(1):80–85 [DOI] [PubMed] [Google Scholar]
- 48.Hawkes AL, Nowak M, Bidstrup B, Speare R. Outcomes of coronary artery bypass graft surgery. Vasc Health Risk Manag 2006;2(4):477–484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mital A, Desai A, Mital A. Return to work after a coronary event. J Cardiopulm Rehabil 2004;24(6):365–373 [DOI] [PubMed] [Google Scholar]
- 50.Perk J, Alexanderson K. Swedish Council on Technology Assessment in Health Care (SBU). Chapter 8. Sick leave due to coronary artery disease or stroke. Scand J Public Health Suppl 2004;63:181–206 [DOI] [PubMed] [Google Scholar]
- 51.Reynolds MW, Frame D, Scheye R, et al. A systematic review of the economic burden of chronic angina. Am J Manag Care 2004;10(11 Suppl):S347–S357 [PubMed] [Google Scholar]
- 52.Samkange-Zeeb F, Altenhoner T, Berg G, Schott T. Predicting non-return to work in patients attending cardiac rehabilitation. Int J Rehabil Res 2006;29(1):43–49 [DOI] [PubMed] [Google Scholar]
- 53.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA 2008;299(20):2401–2405 [DOI] [PubMed] [Google Scholar]
- 54.Marchesini G, Moscatiello S, Di Domizio S, Forlani G. Obesity-associated liver disease. J Clin Endocrinol Metab 2008;93(11 Suppl 1):S74–S80 [DOI] [PubMed] [Google Scholar]
- 55.Smith SA, Hulsey T, Goodnight W. Effects of obesity on pregnancy. J Obstet Gynecol Neonatal Nurs 2008;37(2):176–184 [DOI] [PubMed] [Google Scholar]
- 56.Anandacoomarasamy A, Caterson I, Sambrook P, Fransen M, March L. The impact of obesity on the musculoskeletal system. Int J Obes 2008;32:211–222 [DOI] [PubMed] [Google Scholar]
- 57.Malhotra A, Hillman D. Obesity and the lung: 3. Obesity, respiration and intensive care. Thorax 2008;63:925–931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sin DD, Sutherland ER. Obesity and the lung: 4. Obesity and asthma. Thorax 2008;63:1018–1023 [DOI] [PubMed] [Google Scholar]
- 59.Dennis KE. Postmenopausal women and the health consequences of obesity. J Obstet Gynecol Neonatal Nurs 2007;35(5):511–117 [DOI] [PubMed] [Google Scholar]
- 60.Griffin KA, Kramer H, Bidani AK. Adverse renal consequences of obesity. Am J Physiol Renal Physiol 2008;294:F685–F696 [DOI] [PubMed] [Google Scholar]
- 61.Crummy F, Piper A, Naughton M. Obesity and the lung: 2. Obesity and sleep-disordered breathing. Thorax 2008;63:738–746 [DOI] [PubMed] [Google Scholar]
- 62.Franssen FM, O'Donnell DE, Goossens GH, Blaak EE, Schols AM. Obesity and the lung: 5. Obesity and COPD. Thorax 2008;63:1110–1117 [DOI] [PubMed] [Google Scholar]