Abstract
Dysesthetic blebs can complicate filtration surgery. Lubrication often reduces symptoms; however, some cases require surgical intervention. Limited conjunctivoplasty reduces the symptoms of dysesthetic blebs without sacrificing control of intraocular pressure (IOP). However, this may not sufficiently lower these blebs, particularly if the bleb is thick and dense. We describe a modified conjunctivoplasty technique that includes removal of sub-conjunctival scar tissue within the interpalpebral fissure and provide a 1-year follow-up of 13 eyes treated in this manner. All patients reported rapid, complete symptom resolution. The IOP was controlled in all 13 eyes following conjunctivoplasty; 3 required topical antiglaucoma therapy. Subconjunctival scar tissue may contribute to the formation of dysesthetic blebs owing to its thickness and by encouraging local dissection of aqueous humor. Our report demonstrates that removal of this tissue does not compromise IOP control when performed with conjunctivoplasty.
Adjunctive use of antimetabolites in glaucoma filtration surgery has greatly reduced the primary failure rate of these procedures and provides adequate control of intraocular pressure (IOP) in most patients undergoing surgery. However, the diffuse, thin, avascular filtering blebs that antimetabolites frequently produce are prone to a number of short- and long-term complications such as bleb leak, endophthalmitis, dellen formation, overfiltration, and associated bleb dysesthesia. Bleb dysesthesia describes ocular discomfort (burning, foreign body sensation, tearing, or pain) and is sometimes associated with a large filtration bleb. The amount of discomfort seems to be directly related to the area of the bleb exposed in the interpalpebral fissure and to the height of the bleb adjacent to the cornea.1 The constant irritation experienced by patients with dsyesthetic blebs should not be underestimated, as patients frequently report significant discomfort and dissatisfaction.
The presence of a dysesthetic bleb in an eye with adequate IOP control is a challenge to surgeons who treat patients with glaucoma. Many methods have been described for managing dysesthetic blebs following successful filtering surgery. Aggressive surface lubrication is almost universally used as an initial conservative measure. Other nonsurgical approaches including treatment with topical trichloroacetic acid2 and injection of autologous blood3 are designed to reduce the height of the bleb by stimulating scarring, but they also risk filtration failure. The use of scleral compression sutures has been described alone or in conjunction with autologous blood injection.4,5 Laser applications to the surface of the bleb have also been suggested with either argon6 or Nd:Yag7 laser, but these modalities may require multiple treatment sessions.
When surgery must be used, the ideal procedure for a dysesthetic bleb should not only be safe and effective in relieving the symptoms, but it must also protect the functioning filter from any increased risk of failure. In 2003, Rahman and Thaller8 described a novel surgical technique, bleb-limiting conjunctivoplasty, to eliminate dissection of aqueous humor into the interpalpebral fissure, with favorable results in 2 patients. Anis et al9 recently provided an excellent review of the literature concerning surgical management of dysesthetic blebs. They also describe the favorable results of 15 eyes (10 with at least 12 months of follow-up) that had surgical reduction for bleb dysesthesia similar to that described by Rahman and Thaller.8 Sixteen of the 17 eyes in these articles reported resolution of their symptoms and none required additional glaucoma therapy.
Since November 2000 we have been treating dysesthetic blebs using a technique similar to that described in the articles discussed above, but with an important addition. Our technique includes removal of the subconjunctival scar tissue from the sclera in the interpalpebral fissure. We propose this step as an added component of bleb-limiting conjunctivoplasty that can be particularly useful in patients with thick, dense dysesthetic blebs. Here we describe our first patient treated with this method and submit a case series of 12 additional eyes followed up over a 1-year period to demonstrate the lack of adverse effects of this additional step on long-term IOP control.
METHODS
After approval by the Institutional Review Board of the Oregon Health & Science University, a retrospective review of the medical records was performed for all patients who underwent bleb reduction surgery at the Casey Eye Institute from November 2000 until April 2007. Thirteen eyes of 11 patients with a minimum of 1 year of follow-up were identified who were treated surgically for dysesthetic blebs.
Preoperative data were recorded including age, sex, eye (right or left), glaucoma type, visual acuity, prior surgical procedures, IOP, symptoms, and drop usage. All patients subsequently underwent bleb reduction surgery. All surgical procedures were performed by the same surgeon (J.C.M.). All patients were seen postoperatively after 1 day, 1 week, 1month, 3months, and 1 year, at a minimum. Our case-report patient had bleb reduction combined with trabeculectomy with mitomycin C and phacoemulsification. Two additional patients (eyes 3 and 11) had concurrent phacoemulsification with intraocular lens implantation at the time of bleb reduction.
At each follow-up visit IOP was measured, drop usage was recorded, and comfort and/or satisfaction was assessed. Preoperative and postoperative photographs were taken for some patients. Success criteria included elimination of bleb dysesthesia as reported subjectively by the patient and maintenance of IOP without further surgery.
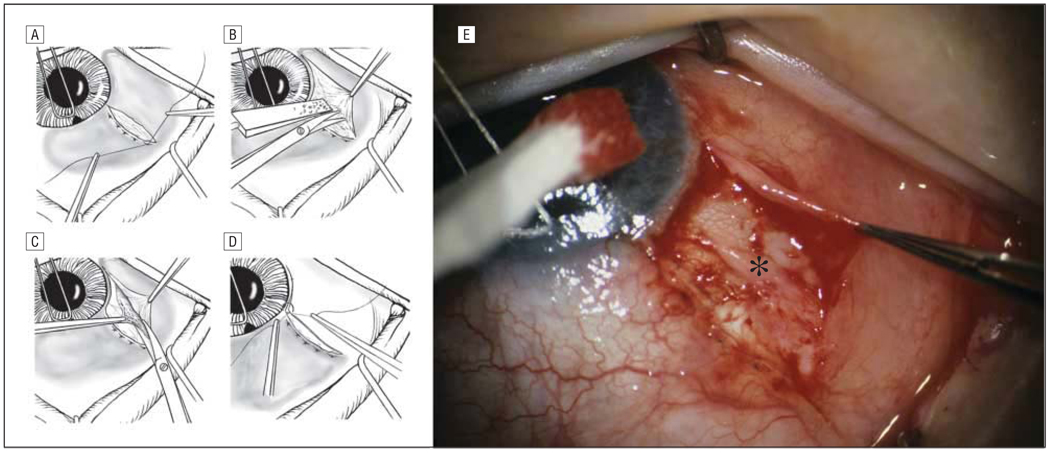
All patients received moderate parenteral sedation. Patients then received an O’Brien facial nerve block using a 1:1 mixture of 2% xylocaine (Lidocaine; Hospira Inc, Lake Forest, Illinois) and 0.75% marcaine (Bupivicaine; Hospira Inc) followed by a retrobulbar injection of approximately 3 mL of the same mixture. A radial conjunctival incision to bare sclera at the desired limit of the bleb, beginning at the limbus, was then made in either the superotemporal or superonasal quadrant, outside the palpebral fissure. Following light cautery, the conjunctival edge nearest the filter was then secured to the episclera with multiple horizontal mattress sutures of 9-0 polyglactan 910 (Vicryl; Ethicon, Piscataway, New Jersey) using a noncutting needle (Figure 1A). All knots were tied over the conjunctiva to reduce the chance of the suture cutting through the thin conjunctiva. A peritomy was then carried inferiorly from the initial incision to a position that corresponded to the extent of the unwanted portion of the bleb. Sharp and blunt dissection was then used to separate the conjunctiva from the subconjunctival and episcleral scar tissue, using a methylcellulose sponge to stabilize the latter tissue (Figure 1B). This tissue was then removed from the episclera posteriorly to the level of the rectus muscle insertion (Figure 1C). Cautery was carried out as needed. The conjunctiva was then re-approximated to the limbus with buried, interrupted, 9-0 vicryl sutures (Figure 1D). The new margin of the bleb was checked for leakage. If any leakage was found, it was repaired with interrupted 9-0 vicryl sutures. Patients received inferior postoperative subconjunctival injections of 0.15 mL of cefazolin (Ancef; Sandoz Inc, Broomfield, Colorado) and 0.1 mL of Decadron (Dexamethasone Baxter Healthcare Corporation, Deerfield, Illinois). Erythromycin ophthalmic ointment (E Fougera & Co, Melville, New York), a sterile eye pad, and a shield were then placed on the eye.
Figure 1.
Surgical drawings (A–D) of steps for bleb reduction. A, Conjunctival mattress sutures to episclera limiting the extent of the bleb. B, Dissection of conjunctiva from underlying connective tissue. C, Excision of subconjunctival connective tissue and repositioning (D) of conjunctiva with buried interrupted sutures. E, Surgical photograph showing the conjunctival dissection with exposure of subconjunctival scar tissue (asterisk).
RESULTS
CASE REPORT
A 60-year-old woman was diagnosed with primary open-angle glaucoma in both eyes and required filtration surgery of the left eye. She underwent an uncomplicated superonasally placed trabeculectomy with mitomycin C in December 1999 and subsequently developed a large nasal dysesthetic bleb with an associated corneal delle. She underwent several attempts to reduce her symptoms, the bleb size, and the location. These included aggressive lubrication, conjunctival compression sutures, and trichloroacetic acid application. Following these procedures, she had neither alleviation of her symptoms, described by her as severe discomfort and photophobia, nor adequate IOP control. She was referred in October 2000 for further surgical treatment.
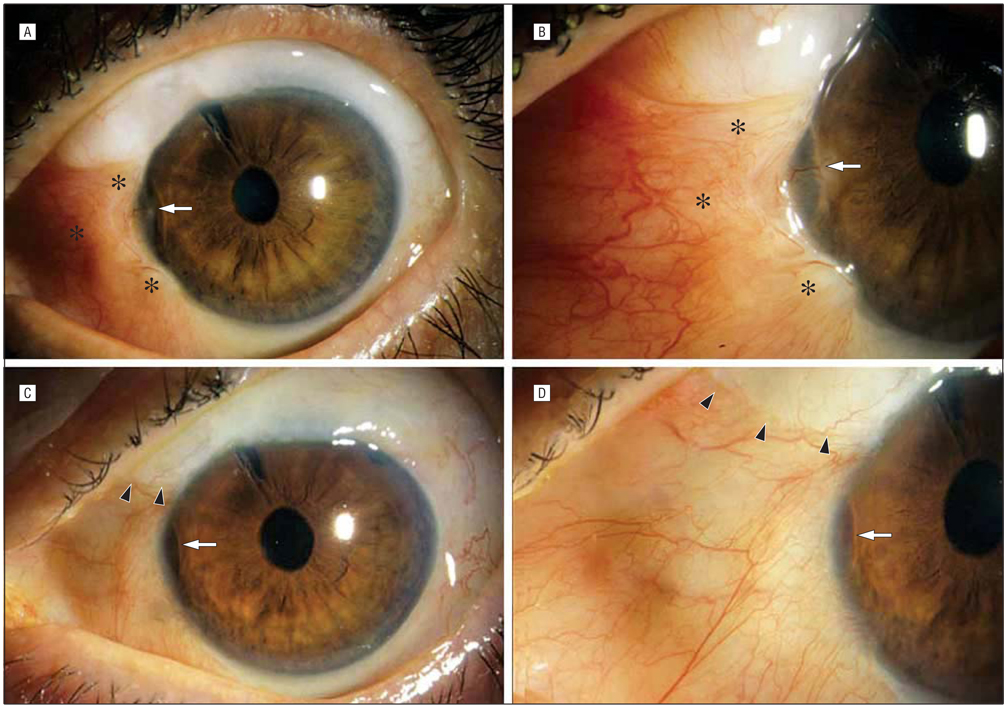
On examination, she had 20/100 visual acuity owing to a dense nuclear sclerotic cataract. She had a large, elevated, thick-appearing bleb that was scarred superiorly but extended into her nasal palpebral fissure. There was an associated well-epithelialized corneal delle (Figure 2A and B). She was using frequent artificial tears and a topical nonsteroidal antiinflammatory drop, but no pressure-lowering agents; the IOP in the left eye was 18 mm Hg and she had extensive glaucomatous optic nerve damage. Owing to her dense cataract and chronic ocular discomfort, she underwent clear cornea phacoemulsification with intraocular lens implantation and bleb-limiting conjunctivoplasty. Removal of the subconjunctival scar tissue was performed, as it was felt that the thickness and density of this tissue, rather than simple nasal diffusion of filtered aqueous humor, was the major contributor to bleb height in this area. Because of poor IOP control, the procedure concluded with a superotemporal trabeculectomy with mitomycin C.
Figure 2.
A, Preoperative photograph of case report patient showing thick vascularized bleb in the nasal interpalpebral space (asterisks) with corneal delle (arrow). B, Close-up showing corneal delle (arrow) with vascularization and thick, elevated bleb extending to limbus (asterisks). C, One-year postoperative photo showing superonasal limit of bleb (arrowheads) with moderate persistence of delle (arrow). D, Close-up postoperative photograph. Comparison to B shows resolution of thick interpalpebral bleb. Delle (arrow) is much improved and no longer vascularized.
Postoperatively, the patient reported immediate resolution of her bleb discomfort despite the persistence of the corneal delle. Her conjunctiva was nasally well apposed to the underlying sclera and she developed a diffuse superotemporal bleb. Her vision improved to 20/20 and her IOP was well controlled in the low teens without medication. After 1 year her IOP and visual acuity were unchanged (Figure 2C and D). During the subsequent 7 years, she eventually required 2 pressure-lowering medications to control her IOP, but she has had no changein visual acuity, no bleb dysesthesia, and has required no additional surgery in that eye.
Owing to the dramatic improvement in the appearance and comfort of this patient’s bleb, which we felt was aided substantially by the removal of subconjunctival scar tissue, we incorporated this step into our standard dysesthetic bleb repair technique. The following case series is presented to assess the effect of this modification on long-term IOP control.
CASE SERIES
Demographic characteristics of 13 eyes with a minimum 1-year follow-up after bleb reduction are listed in Table 1. The median (SD) age at the time of surgery was 60 (11.0) years (range, 46–81 years). All patients had previous trabeculectomies with a limbal-based conjunctival flap and adjunctive mitomycin C. All eyes had large, functioning, dysesthetic blebs with some component of the bleb in the interpalpebral fissure. All patients remained symptomatic despite frequent use of lubricating drops and ointment. No patients were taking IOP-controlling medications prior to surgery. Two patients had bleb-related dellen formation. One patient had diplopia in association with the bleb. All patients reported displeasure in the appearance of their bleb. Despite good IOP control, all patients were vocally displeased with the discomfort following the initial surgery. The median time from trabeculectomy to bleb revision was 24 weeks (range, 11 weeks to 16 months).
Table 1.
Patient Demographics
| Eye No. | Age, y/Sex/Eye | Type of Glaucoma | Additional Problems |
|---|---|---|---|
| 1a | 60/F/left | POAG | |
| 2b | 69/F/right | LTG | |
| 3 | 73/F/left | POAG | |
| 4 | 81/M/left | POAG | |
| 5b | 71/F/left | LTG | |
| 6 | 57/M/right | POAG | Dellen formation |
| 7c | 56/M/right | LTG | |
| 8c | 58/M/left | LTG | |
| 9 | 81/M/right | PXF | Diplopia |
| 10 | 46/M/left | POAG | |
| 11 | 73/M/left | POAG | |
| 12 | 56/M/left | Steroid-induced | |
| 13 | 54/F/right | Pigmentary |
Abbreviations: LTG, low-tension glaucoma; POAG, primary open-angle glaucoma; PXF, pseudoexfoliation glaucoma.
Eye 1 belongs to case report patient.
Eyes 2 and 5 are the right and left eyes of the same patient.
Eyes 7 and 8 are the left and right eyes of the same patient.
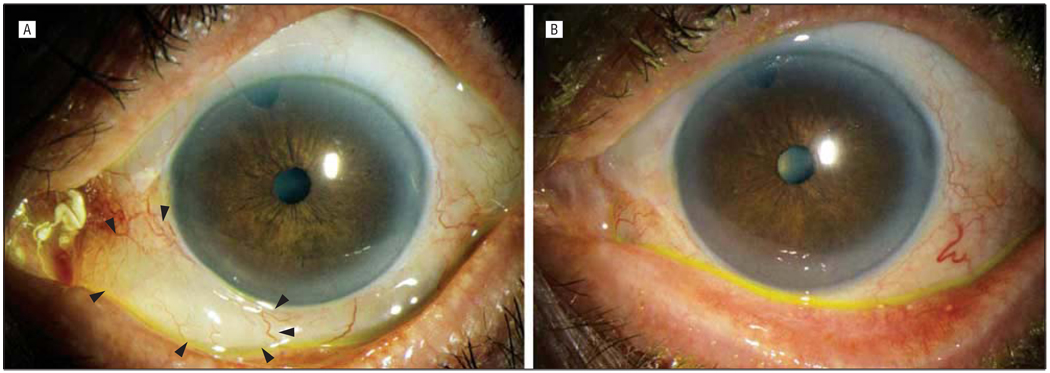
Results following bleb reduction are listed in Table 2. Objective reduction of bleb size by slit-lamp examination was noted in all 13 eyes at the 1-month postoperative visit and symptomatic improvement (increased comfort and cosmesis) was noted by every patient shortly after surgery (Figure 3). All eyes retained excellent comfort and cosmesis for the duration of their follow-up. Bleb functionality (defined as adequate IOP control without further surgery) was seen after 1 year in every eye that had conjunctivoplasty alone, although 1 eye did require topical antiglaucoma medication. Two patients (eyes 3 and 11) had concurrent phacoemulsification with their bleb reduction; both of these eyes required topical antiglaucoma medication.
Table 2.
Results After Bleb Reduction
| Eye No. |
Previous Procedure(s) |
Mean Preoperative IOP, mm Hg |
Procedure | 1 wk | 1 mo | 3 mo | 6 mo | 1 y | Preoperative VA |
Postoperative VA |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Trab/MMC, revision, TCA 3 times, compression sutures, autologous blood injection |
18 | Bleb reduction, trabeculectomy revision, phaco/IOL |
10 | 11 | 10 | 13 | 14 | 20/100 | 20/20 |
| 2 | Trab/MMC | 5.3 | Bleb reduction | 8 | 9 | 6 | 9 | 11 | 20/25 | 20/20 |
| 3 | Trab/MMC | 5.5 | Bleb reduction, phaco/IOL | 24 | 20 | 21a | 15a | 12a | CF | CF |
| 4 | Trab/MMC | 10.7 | Bleb reduction | 10 | 12 | 10 | 12 | 16 | 20/25 | 20/20 |
| 5 | Trab/MMC | 10.3 | Bleb reduction | 13 | 11 | 11 | 10 | 10 | 20/20 | 20/20 |
| 6 | Trab/MMC | 10.5 | Bleb reduction | 9 | 9 | 8 | 8 | 10 | 20/15 | 20/20 |
| 7 | Trab/MMC | 8 | Bleb reduction | 7 | 7 | 8 | 8 | 7b | 20/200 | 20/20 |
| 8 | Phaco/IOL, Trab/MMC | 12 | Bleb reduction | 9 | 9 | 9 | 10 | 11 | 20/20 | 20/20 |
| 9 | Trab/MMC, cryotherapy, TCA, phaco/IOL |
11 | Bleb reduction | 22 | 26a | 19a | 16a | 18a | 20/25 | 20/30+2 |
| 10 | Trab/MMC | 8.7 | Bleb reduction | 10 | 9 | 8 | 9 | 11 | 20/25−1 | 20/25−2 |
| 11 | Trab/MMC, ALT | 15 | Bleb reduction, phaco/IOL | 16 | 16a | 19a | 15a | 15a | 20/40 | 20/20 |
| 12 | Trab/MMC | 11.6 | Bleb reduction | 13 | 13 | 12 | 12 | 16 | 20/150 | 20/150 |
| 13 | Trab/MMC | 11.5 | Bleb reduction | 11 | 15 | 12 | 12 | 13 | 20/20 | 20/20−3 |
Abbreviations: ALT, argon laser trabeculoplasty; CF, counting fingers visual acuity; IOP, intraocular pressure; phaco/IOL, phacoemulsification with intraocular lens implantation; TCA, topical trichloroacetic acid treatment; Trab/MMC, trabeculectomy with adjunctive mitomycin C; VA, visual acuity.
Patient receiving topical medication to control IOP.
Patient had interval phaco/IOL.
Figure 3.
A, Preoperative photo of eye 2 showing filtering bleb (arrowheads) extending infernasally into interpalpebral fissure. B, Postoperative photograph at 3 months showing resolution of the inferonasal bleb.
CONCLUSION
Many patients with symptoms due to a large bleb can be adequately treated with judicious use of lubricating eye drops and ointments. However, alternatives are needed for patients who remain symptomatic despite these regimens. Any intervention, to be of practical value, must be safe, effective at eliminating the irritating symptoms, and should preserve adequate filtration to maintain IOP control.
Our case report patient required concurrent filtering surgery and cataract extraction—thus we cannot comment on the effect of our reduction procedure on her IOP control. Her case is, however, instructive regarding the effectiveness of this procedure at eliminating the symptoms of dysesthetic blebs. She reported an immediate substantial improvement in the comfort of this eye following surgery. Because this dramatic improvement occurred despite the persistence of the delle, we feel that her discomfort was due less to corneal pathology than to the extremely thick and dense scar tissue that was removed concurrently with the conjunctivoplasty. Two other patients (eyes 3 and 11) required concurrent cataract surgery with their bleb reductions for chronic severe discomfort; each also reported a rapid dramatic improvement in comfort following this procedure, but eventually needed topical medication to control their IOP.
Histologically, dense cellular connective tissue consisting of randomly arranged collagen fibers and fibroblasts has been described within functional and encapsulated filtering blebs.10–13 We suggest that such tissue, if present beneath the conjunctiva in the interpalpebral fissure, likely encourages the formation and maintenance of these dysesthetic blebs through 2 mechanisms. First, it physically contributes to the bleb height, as we often find that the thickness of tissue removed is greater than expected by the preoperative appearance of the bleb. Second, this tissue has a smooth surface and is easily separated from the sclera. Prior histopathologic studies of Descemet membrane and Bowman layer incarcerations in penetrating keratoplasties have demonstrated that these are associated with a high incidence of wound defects, suggesting that the smooth surface of both structures interferes with normal healing.14,15
We hypothesize that the smooth surface of subconjunctival connective tissue in dysesthetic blebs similarly prevents adequate healing of the conjunctiva to the underlying episclera and therefore allows accumulation of fluid in the interpalpebral area. These factors, in addition to the possibility of discomfort caused by unusually thick connective tissue, all indicate that its removal at the time of bleb sequestration can improve the chances of long-term symptom resolution.
Successful bleb-reduction surgery should be defined as resolution of the preoperative symptoms without compromise of filtering function. In their study of conjunctivoplasty alone, Anis and colleagues9 described 15 patients, 10 with IOP data lasting 1 year. All but 1 patient had relief of symptoms and none of their patients required further surgery or topical medication, although 5 did have IOP at 1 year that was higher than their preoperative IOP. In comparison, all 13 eyes in our 1-year series had total resolution of their symptoms and 9 of the 10 eyes with conjunctivoplasty only maintained medication-free IOP control for 1 year postoperatively. Five eyes had postoperative IOPs marginally higher than the pressures measured prior to conjunctivoplasty, but were judged to be clinically stable and not in need of topical therapy. Thus we feel that our 1-year pressure-control results are comparable with those following conjunctivoplasty alone, despite the additional surgical removal of the subconjunctival scar tissue.
Three eyes in our series required topical medication for IOP control after 1 year, 2 of which had concurrent phacoemulsification at the time of bleb reduction. The third eye had trichloroacetic acid application and cryotherapy before surgical reduction and ultimately required an additional filtering surgery 28 months after the repair. These additional interventions may have played a role in promoting local inflammation, scarring, and ultimate failure of this filter. None of the eyes reported by Anis et al9 appear to have had these additional treatments.
Two of our cases with unusually thick blebs due to subconjunctival scarring had previously received trichloroacetic acid and cryotherapy as well as compression sutures to lower the height of the bleb. It is possible that these methods, by encouraging inflammation, may exacerbate the formation of this scar tissue and the patients’ symptoms. For this reason, we now favor the procedure described in this article as our primary approach in patients with significant bleb dysesthesia that is not relieved with time and simple lubrication.
Although conjunctivoplasty alone is effective at reducing the symptoms of dysesthetic blebs,9 we feel that, particularly in eyes with thick interpalpebral blebs, simply limiting subconjunctival dissection of aqueous humor into this area may have a limited effect in some eyes, as subconjunctival scar tissue will still contribute to bleb height and discomfort. Our experience suggests that removing this tissue can have a striking effect on patient comfort, and our case series demonstrates that this maneuver can be routinely added to conjunctivoplasty without adversely affecting long-term IOP control.
Acknowledgments
Funding/Support: This study was supported by grant RO1EY10145 from the National Institutes of Health and an unrestricted grant from Research to Prevent Blindness.
Footnotes
Financial Disclosure: None reported.
REFERENCES
- 1.Budenz DL, Hoffman K, Zacchei A. Glaucoma filtering bleb dysesthesia. Am J Ophthalmol. 2001;131(5):626–630. doi: 10.1016/s0002-9394(00)00901-6. [DOI] [PubMed] [Google Scholar]
- 2.Gehring JR, Ciccarelli EC. Trichloroacetic acid treatment of filtering blebs following cataract extraction. Am J Ophthalmol. 1972;74(4):622–624. doi: 10.1016/0002-9394(72)90821-5. [DOI] [PubMed] [Google Scholar]
- 3.Wise JB. Treatment of chronic postfiltration hypotony by intrableb injection of autologous blood. Arch Ophthalmol. 1993;111(6):827–830. doi: 10.1001/archopht.1993.01090060115034. [DOI] [PubMed] [Google Scholar]
- 4.Morgan JE, Diamond JP, Cook SD. Remodelling the filtration bleb. Br J Ophthalmol. 2002;86(8):872–875. doi: 10.1136/bjo.86.8.872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Palmberg P. Late complications after glaucoma filtering surgery. In: Leader B, Calckwood J, editors. Proceedings of the 45th Annual Symposium of the New Orleans Academy of Ophthalmology; The Hague, the Netherlands. Kugler Publications; 1996. [Google Scholar]
- 6.Fink AJ, Boys-Smith JW, Brear R. Management of large filtering blebs with the argon laser. Am J Ophthalmol. 1986;101(6):695–699. doi: 10.1016/0002-9394(86)90772-5. [DOI] [PubMed] [Google Scholar]
- 7.Lynch MG, Oresch M, Brown RH. Remodeling filtering blebs with the neodymium:YAG laser. Ophthalmology. 1996;103(10):1700–1705. doi: 10.1016/s0161-6420(96)30443-0. [DOI] [PubMed] [Google Scholar]
- 8.Rahman R, Thaller VT. Bleb-limiting conjunctivoplasty for symptomatic circumferential trabeculecomy blebs. J Glaucoma. 2003;12(3):272–274. doi: 10.1097/00061198-200306000-00016. [DOI] [PubMed] [Google Scholar]
- 9.Anis S, Ritch R, Shihadeh W, et al. Surgical reduction of symptomatic circumferential, filtering blebs. Arch Ophthalmol. 2006;124(6):890–894. doi: 10.1001/archopht.124.6.890. [DOI] [PubMed] [Google Scholar]
- 10.Van Buskirk EM. Cysts of Tenon’s capsule following filtration surgery. Am J Ophthalmol. 1982;94(4):522–527. doi: 10.1016/0002-9394(82)90248-3. [DOI] [PubMed] [Google Scholar]
- 11.Mietz H, Arnold G, Kirchof B, et al. Histopathology of episcleral fibrosis after trabeculectomy with and without mitomycin C. Graefes Arch Clin Exp Ophthalmol. 1996;234(6):364–368. doi: 10.1007/BF00190712. [DOI] [PubMed] [Google Scholar]
- 12.Schnyder CC, Shaaraway T, Ravinet E, et al. Free conjunctival autologous graft for bleb repair and bleb reduction after trabeculectomy and non-penetrating filtration surgery. J Glaucoma. 2002;11(1):10–16. doi: 10.1097/00061198-200202000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Mandal AK, Vemuganti GK, Ladda N, et al. Partial excision with a conjunctival advancement flap after a relaxing incision for a dissecting glaucoma filtering bleb. Ophthalmic Surg Lasers. 2002;33(6):497–500. [PubMed] [Google Scholar]
- 14.Morrison JC, Swan KC. Bowman’s layer in penetrating keratoplasty of the human eye. Arch Ophthalmol. 1982;100(11):1835–1838. doi: 10.1001/archopht.1982.01030040815023. [DOI] [PubMed] [Google Scholar]
- 15.Morrison JC, Swan KC. Descemet’s membrane and penetrating keratoplasties of the human eye. Arch Ophthalmol. 1983;101(12):1927–1929. doi: 10.1001/archopht.1983.01040020929020. [DOI] [PubMed] [Google Scholar]