Abstract
Background
Suicide is a leading cause of death and has been strongly associated with affective disorders. The influence of affective disorder polarity on subsequent suicide attempts or completions and any differential effect of suicide risk factors by polarity were assessed in a prospective cohort.
Methods
Participants with major affective disorders in the National Institute of Mental Health Collaborative Depression Study were followed prospectively for up to twenty-five years. A total of 909 participants meeting prospective diagnostic criteria for major depressive and bipolar disorders were followed through 4,204 mood cycles. Suicidal behavior was defined as suicide attempts or completions. Mixed-effects, grouped-time survival analysis assessed risk of suicidal behavior and differential effects of risk factors for suicidal behavior by polarity. In addition to polarity, the main effects of age, gender, hopelessness, married status, prior suicide attempts, and active substance abuse were modeled with mood cycle as the unit of analysis.
Results
After controlling for age of onset, there were no differences in prior suicide attempts by polarity though bipolar participants had more prior severe attempts. During follow-up, forty cycles ended in suicide and 384 cycles contained at least one suicide attempt. Age, hopelessness, and active substance abuse but not polarity predicted suicidal behavior. The effects of risk factors did not differ by polarity.
Conclusions
Bipolarity does not independently influence risk of suicidal behavior or the influence of well-established suicide risk factors within affective disorders. Suicide risk assessment strategies may continue to appraise these common risk factors without regard to mood polarity.
Keywords: Adult, major depression, bipolar disorder, completed suicide, prospective cohort study, risk factors
Introduction
Unipolar and bipolar disorders differ with regard to several clinical and course of illness variables (Serretti et al., 2002). The validity of the bipolar versus unipolar distinction for affective disorders is supported by a general diagnostic stability (Rice et al., 1986; Coryell et al., 1989; Rice et al., 1992), familial aggregation (Coryell et al., 1984; Endicott et al., 1985; Rice et al., 1987), and course of illness (Coryell et al., 1989; Goldberg and Harrow, 2004). One important sequela of affective disorders is suicide. Suicide was the fifth leading cause of death when ranked by years of potential life lost before age 65 in the United States from 1999 to 2002 (C.D.C., 2005), and the majority of suicide victims have a unipolar or bipolar depressive disorder at the time of suicide (Rihmer, 1996; Mann et al., 2005).
Several (Dunner et al., 1976; Kupfer et al., 1988; Tondo et al., 1999) but not all (Cassano et al., 1992) retrospective studies have suggested higher rates of suicide attempts among individuals with bipolar, particularly type II, versus unipolar disorders. Bipolar disorder was associated with greater risk of suicide attempts and completions in one prospective study of 2,826 Italian outpatients with affective disorders followed for a mean of 3.6 years, during which 27 completed suicides and 363 suicide attempts were recorded (Tondo et al., 2007). However, bipolar disorder has not consistently been associated with greater risk of suicidality prospectively (Coryell et al., 1987). For bipolar patients, suicide attempts appear most likely to occur in the setting of depressed states (Tondo et al., 1999; Oquendo et al., 2000; Valtonen et al., 2005) though mixed states or cycling also been associated (Tondo et al., 1999; Dalton et al., 2003; Valtonen et al., 2005). To our knowledge, there are no studies that directly test for differential effects of well-established risk factors for suicide by affective disorder polarity.
The Collaborative Depression Study (CDS) dataset provides a unique opportunity to assess differential effects of risk factors for suicide owing to its duration, size and scope. To enhance the accuracy of diagnosis and reduce the risk of misclassification from relying solely on cross-sectional diagnoses, we examined the risk of suicide outcomes based on a prospective rather than initial diagnosis. To effectively utilize our long-term prospective dataset, we further analyzed risk factors at the beginning of a mood cycle rather than simply at study intake. Given disparate findings in previous studies regarding risk of suicide outcomes by subtype of affective disorder, we sought to explore potential differential effects of previously identified risk factors by affective disorder polarity. With limited background research on this topic, we hypothesized that risk factors for suicide would not differ significantly by polarity. While a number of analyses of the entire CDS dataset have assessed suicide risk factors (Scheftner et al., 1988; Fawcett et al., 1990; Young et al., 1994; Coryell et al., 2001; Coryell et al., 2002; Maser et al., 2002), only one has looked at affective disorder type as a risk factor for suicide (Fawcett et al., 1987). The Fawcett et al. (1987) study compared 25 patients who committed suicide by four year follow-up with those who did not over a variety of clinical variables. Diagnostic subcategories did not differentiate completers from non-completers as assessed by Fisher’s exact test. No CDS analysis has utilized prospective diagnoses in the study of suicide risk or compared the differential effects (interaction) of risk factors by affective disorder polarity.
Method
Study Design
Patients with affective disorders were recruited for participation in the National Institute of Mental Health Collaborative Program on the Psychobiology of Depression from five academic centers: Massachusetts General Hospital and Harvard University in Boston, Rush Presbyterian – St. Luke’s Medical Center in Chicago, the University of Iowa in Iowa City, New York State Psychiatric Institute and Columbia University in New York, and Washington University School of Medicine in St. Louis. Participants were Caucasian, English-speaking, and knowledgeable regarding their biological parents. Participants further met Research Diagnostic Criteria (RDC) (Spitzer et al., 1978) for major depressive disorder, schizoaffective disorder, or manic disorder. Intake diagnosis was used to identify 936 probands. This sample was further restricted to 909 participants with at least one follow-up assessment. Participants in this sample were followed for a mean of 15.4 (median: 19; SD: 8.8) years and for up to twenty-five years. Seventy-eight percent of participants were followed for a decade or more.
Follow-up assessments were completed using various forms of the Longitudinal Interval Follow-up Evaluation (LIFE) (Keller et al., 1987), which categorizes severity of psychopathology and was administered semiannually in the first five years and annually thereafter. The LIFE tracked each RDC syndrome weekly and was utilized to prospectively diagnose participants into one of two groups: unipolar and bipolar. An initial diagnosis of bipolar disorder was based on an intake RDC diagnosis of bipolar II, bipolar I, schizoaffective manic, or schizoaffective depressed with a history of mania or schizoaffective-mania, mainly affective. The latter category was included as it is virtually identical to mania as defined by the 4th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). An initial diagnosis of unipolar depression was based on intake RDC diagnosis of major depressive disorder or schizoaffective-disorder, depressed, mainly affective. The latter category was included as it is analogous to major depression as defined by the DSM-IV. Follow-up ratings from the LIFE Psychiatric Status Rating (PSR) were used to reclassify participants diagnostically. Participants with unipolar depression on intake, who developed mania or hypomania during follow-up, were thus classified as having bipolar disorder. For consistency and to utilize the most accurate diagnoses, prospective diagnoses were utilized for all subsequent analyses.
Data Analytic Procedures
Baseline demographics and prior suicide attempts were compared between participants with unipolar and bipolar disorders. Age of onset was estimated using the earliest of age of first psychiatric treatment, onset of depressive symptoms, or onset of manic symptoms from the Schedule of Affective Disorders (SADS) (Endicott and Spitzer, 1978; Endicott and Spitzer, 1979). A retrospective analysis of suicide attempts was performed to explore differences in baseline suicidality prior to enrollment in this prospective cohort study. Separate analyses were conducted for suicide attempts and severe suicide attempts. Severity of attempt was determined from the SADS using previously utilized cutoffs, wherein a severe attempt was operationally defined as a SADS suicidal intent (item 249) or medical lethality (item 250) score ≥ 4 (Fiedorowicz and Coryell, 2007). These cut-offs require a “serious” level of suicidal intent to kill oneself or at least “moderate” medical lethality (i.e. “had brief unconsciousness”). Logistic regression was performed to control for age of onset in assessing suicide attempts prior to intake by polarity.
Descriptive statistics related to suicidal behaviors during follow-up and burden of depressive symptoms were compiled for those with prospective diagnoses of unipolar or bipolar disorder. Burden of depressive symptoms during prospective follow-up was obtained from the LIFE Psychiatric Status Rating (PSR) scales, which were anchored to diagnostic thresholds for RDC disorders. Based on previously published criteria (Judd et al., 2002), a week of depressive symptoms was operationalized as a PSR cutoff score of ≥ 3/6 (moderate symptoms or impairment) on the major depression or schizoaffective depression scale or a score of 3/3 (definite criteria) for minor or intermittent depression with a PSR of ≤ 2 on the major depressive scale. Differences in percentage of time depressed were assessed non-parametrically using the Wilcoxon rank sum test.
Any suicidal act was included in the survival analysis, regardless of intent or lethality and including those acts with minimal if any intent or no actual threat to life. Suicidal behaviors were broadly defined and encompassed suicide attempts or suicide completions. Time to suicide attempt or completion by prospective diagnosis was illustrated using Kaplan-Meier methods. Survival time represented the number of weeks from intake into the cohort study until the outcome of interest: suicide attempt or suicide completion. Cases lost to follow-up prior to suicide attempts or completions were censored. This analysis assumed that censoring and suicide attempts or completions were independent. Death indices from vital statistics were methodically searched, minimizing the risk that suicide completions went unrecognized in censored cases. When the cause of death was unknown, the death was not included as a suicide in our analysis. The above analyses were completed utilizing SAS version 9.1 (SAS Institute Inc, Cary, NC, 2003) and SPSS version 13.0.
The strength of the association between each of several previously established and a priori selected risk factors for completed suicide were examined in a grouped-time mixed-effects survival analysis (Hedeker et al., 2000). Given that risk factors may change over time, the unit of analysis was changed from individual participant to mood cycle to best utilize the prospective data. The mood cycle included a mood episode and the subsequent period of recovery until next episode, if applicable. Cycle length was grouped as a grouped-time, ordinal variable into the following ten categories: ≤ 8 weeks (≤2 months), 9–16 weeks (2–4 months), 17–26 weeks (4–6 months), 27–36 weeks (6–9 months), 37–52 weeks (9–12 months), 53–104 weeks (1–2 years), 105–156 weeks (2–3 years), 157–208 weeks (3–5 years), 209–312 weeks (4–6 years), or more than 312 weeks (> 6 years). The beginning of a cycle was determined by study intake or the first week of any recurrence following a period of recovery. The end of a cycle was determined by the week prior to any recurrence following a period of recovery or the point at which the participant was lost to follow-up. A recovery was defined as eight consecutive weeks with no or only residual symptoms (PSR ≤ 2) on the major depressive, manic, schizoaffective depressive, or schizoaffective manic scales of the PSR with no symptoms on the hypomania, minor depression, or intermittent depression scales. A recurrence was defined as any PSR scale > 2 lasting one or two weeks, for (hypo)manic and depressive symptoms respectively.
Age at cycle onset was included as a continuous covariate in the assessment of the following risk factors: gender, feelings of hopelessness, history of suicide attempt, history of multiple suicide attempts, marital status (married versus others), and substance abuse. Data on hopelessness was collected only on intake. With the exception of hopelessness and gender, the most recent assessment prior to cycle onset was used for other main effects. The model containing main effects thus contained the following variables: age, male gender, hopelessness, married status, prior suicide attempts, current substance abuse, and polarity. A differential effect of these risk factors by polarity was then assessed. For each assessed polarity by main effect interaction, the likelihood ratio test compared the full model with an interaction term to the reduced model without the interaction term (main effects only). Each statistical test used a two-tailed alpha of 0.05. These mixed-effects grouped-time regression models were calculated using SuperMix software.
Results
Stability of Diagnosis
Diagnostic categories were stable during follow-up for the majority of participants though clinically meaningful rates of conversion from unipolar major depression to a bipolar disorder were observed during follow-up. Of the patients who entered the CDS with unipolar major depression, the prospectively observed conversion rate to a diagnosis of bipolar II or I was 10.6 % and 6.9 % respectively. Participants were followed for a mean of 799 (median: 988; SD: 460) weeks or 15.4 (19; 8.8) years of prospective follow-up. Comparisons of baseline and demographic variables between diagnostic groups are detailed in Table 1. Unipolar patients were significantly older at study intake and more likely to be married.
TABLE 1.
Baseline Demographic and Clinical Characteristics of Participants by Polarity
| Unipolar | Bipolar | |
|---|---|---|
| N | 501 | 435 |
| # (%) Female | 294 (58.7%) | 250 (57.5%) |
| Age, Mean (SD) a | 39.9 (15.0) | 36.3 (13.2) |
| Educational Level, # (%) b | ||
| Without Diploma | 100 (20.1%) | 53 (12.2%) |
| High School Grad | 141 (28.3%) | 115 (26.4%) |
| Some College | 137 (27.5%) | 147 (33.8%) |
| College Graduate | 120 (24.1%) | 120 (27.6%) |
| Marital Status, # (%) c | ||
| Married | 240 (47.9%) | 148 (34.0%) |
| Divorced/Separated | 78 (15.6%) | 99 (22.8%) |
| Never Married | 158 (31.5%) | 178 (40.9%) |
| Widowed | 25 (5.0%) | 10 (2.3%) |
| Prior Suicide Attempt d | 144 (28.7%) | 167 (38.4%) |
| Multiple Prior Attempts e | 61 (12.2%) | 79 (18.2%) |
| Prior Severe Attempt f | 71 (14.2%) | 107 (24.6%) |
The above table outlines baseline and demographic information obtained from participants on intake from the Schedule for Affective Disorders and Schizophrenia (SADS) and Personal History of Depressive Disorders (PHDD). Differences in suicide attempts are not significant after controlling for age of onset.
t=3.8, df=933, p<0.0001
X2=13.2, df=3, p<0.005
X2=27.4, df=3, p<0.0001
X2=9.8, df=1, p<0.002
X2=6.6, df=1, p<0.02
X2=16.4, df=1, p<0.0001
Suicide Attempts Prior to Intake into the Collaborative Depression Study (CDS)
Participants with bipolar disorder (38.4%) were somewhat more likely than those with unipolar disorder (28.7%) to have attempted suicide prior to intake, although bipolar participants were not at significantly greater risk for any prior suicide attempt (HR=1.14, 95% C.I. 0.95–1.38, p=0.16) or multiple prior suicide attempts (HR=1.08, 0.91–1.39, p=0.38) when age of onset was controlled for in logistic regression. However, participants with a bipolar disorder were 30% more likely than those with unipolar disorder to have had prior severe suicide attempts (HR=1.30, 1.09–1.38, p<0.005) controlling for age of onset in logistic regression.
Suicide Attempts and Depressive Morbidity after Intake into the CDS
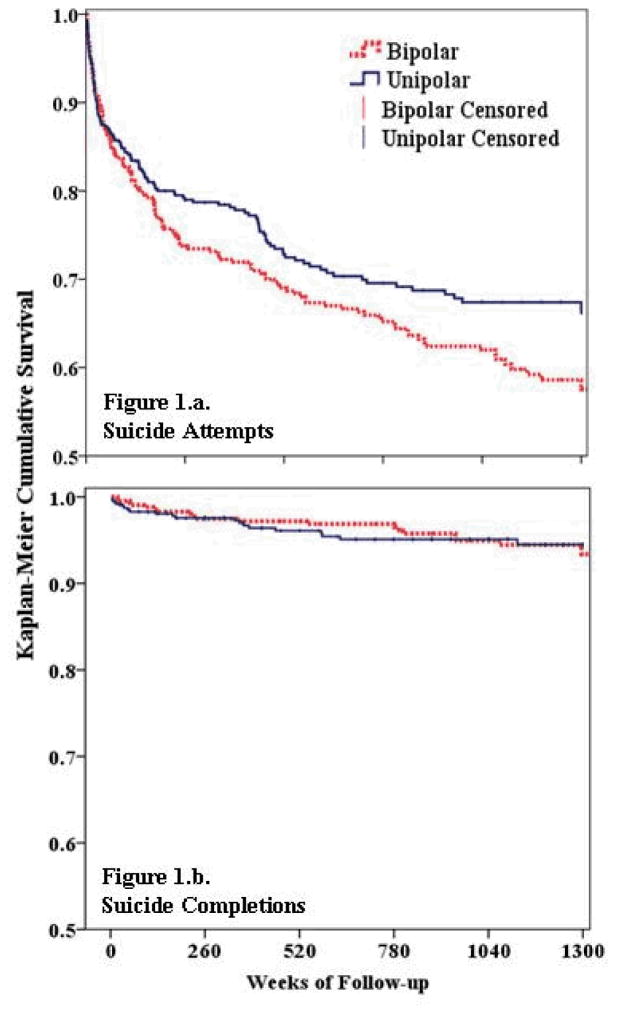
The frequency of suicide outcome measures by diagnosis during follow-up is detailed in Table 2. Individuals with bipolar disorder had a greater frequency of suicide attempts during prospective follow-up than those with unipolar depression (34.0% vs. 27.2%). Bipolar participants were not more likely to complete suicide than their unipolar counterparts, however (4.4% vs. 4.2%). A total of 40 completed suicides were recorded in this study: 21 among those with unipolar depression, 19 with bipolar disorder. Consistent with previously published results (Judd et al., 2003), significant differences in the percentage of weeks depressed for each diagnostic category were observed (Table 2), with bipolar disorder associated with a lower cumulative depressive burden. Kaplan-Meier survival curves illustrated suicide attempts and suicide completions (Figure 1) over the course of prospective follow-up in the CDS for individuals by prospective diagnosis.
TABLE 2.
Frequency of Suicidal Behavior and Proportion of Time Depressed During Follow-up by Polarity
| Unipolar | Bipolar | |
|---|---|---|
| Any Suicide Attempt a | 131 (27.2%) | 148 (34.0%) |
| Multiple Suicide Attempts b | 75 (15.6%) | 87 (20.0%) |
| Severe Suicide Attempt c | 79 (16.4%) | 97 (22.3%) |
| Multiple Severe Attempts | 35 (7.3%) | 44 (10.1%) |
| Completed Suicide | 21 (4.2%) | 19 (4.4%) |
| Mean (Median; SD) % Weeks Depressed d | 38.6 (27.2; 33.1) % | 31.7 (22.1; 30.4) % |
The above table outlines the rate of selected suicide outcomes by prospective diagnosis during a median prospective follow-up of 19 years. Severity of suicide attempt was determined by a previously utilized score of 4 or greater for intent or lethality on the SADS.
X2=6.9, df=1, p<0.01
X2=4.1, df=1, p<0.05
X2=6.5, df=1, p<0.02
Wilcoxon rank sum test, p<0.001
Figure 1. Survival by affective diagnosis.
Kaplan-Meier survival estimates for participants based on prospective diagnosis for time to: (a) suicide attempt and (b) completed suicide.
Main Effect of Risk Factors on Suicidal Behavior: Unipolar vs. Bipolar
The effect of polarity on suicidal behavior, defined as suicide attempts or completions, was assessed in mixed-effects grouped-time survival analysis (Table 3). Age at cycle onset was included as a continuous covariate for analysis of main effects. A statistically significant linear protective effect of age was noted (HR=0.95, 95% C.I. 0.94–0.96, p<0.001). Independent statistically significant main effects were also seen for hopelessness (HR=3.00, 95% C.I. 1.97–4.51, p<0.001) and substance abuse (HR=2.28, 95% C.I. 1.64–3.15, p<0.001). The impact of male gender, married status, and prior suicide attempts did not reach statistical significance. Polarity did not independently predict risk of suicidal behavior.
TABLE 3.
Main Effects and Main Effect by Polarity Interactions on Suicidal Behavior
| Main effect | Hazard Ratio | Likelihood Ratio |
|---|---|---|
| Male Gender | 0.76 | X2 = 0.42 |
| 0.55 – 1.04 | df = 1 | |
| p = 0.87 | p = 0.52 | |
| Hopeless † | 3.00 | X2 = 0.01 |
| 1.97 – 4.57 | df = 1 | |
| p < 0.001 | p = 0.93 | |
| Married | 1.00 | X2 = 0.53 |
| 0.76 – 1.31 | df = 1 | |
| p = 0.98 | p =0.46 | |
| Prior Suicide Attempts | 1.25 | X2 = 0.56 |
| 0.91 – 1.70 | df = 1 | |
| p = 0.17 | p = 0.45 | |
| Substance Abuse † | 2.28 | X2 = 0.33 |
| 1.64 – 3.15 | df = 1 | |
| p < 0.001 | p = 0.56 | |
| Bipolar polarity | 1.16 | |
| 0.85 – 1.58 | ||
| p = 0.34 |
The above table details the hazard ratios, 95% confidence intervals of the hazard ratio, and p-values for each main effect modeled in a mixed-effects, grouped-time survival analysis to predict suicide attempts or completions. Age at cycle onset was included as a covariate in the model. Interactions were individually compared utilizing the likelihood ratio test for comparing nested models where the interaction term was removed for the reduced model.
Denotes a statistically significant main effect. There were no statistically significant polarity by risk factor interactions on risk of suicidal behavior.
Differential Effect of Risk Factors on Suicidal Behavior: Unipolar vs. Bipolar
Polarity by main effect interactions terms were individually added to the above model to assess for differential effects of risk factors on suicidal behavior by polarity. No statistically significant polarity by risk factor interactions were noted.
Discussion
The increased rate of suicide attempts prior to study entry in participants with bipolar disorder appears to largely reflect an earlier age of onset which has been previously noted with bipolar disorder (McMahon et al., 1994). While a trend was noted in our retrospective analyses of increased prior suicide attempts with bipolar disorder compared with unipolar disorder, the differences observed were statistically significant, after controlling for age of onset, only for severe suicide attempts. These findings differ somewhat with an analysis of the Epidemiologic Catchment Area database which revealed an excess of suicide attempts in individuals with bipolar disorder even after controlling for age of onset (Chen and Dilsaver, 1996). While frequency data may have been suggestive of increased suicidal behaviors during follow-up in participants with bipolar disorder, polarity did not independently predict suicidal behaviors when modeled in a mixed-effects grouped-time survival analysis. Age at cycle onset, hopelessness at study intake, and active substance abuse did independently predict suicidal behavior during mood cycles. The likelihood ratio tests revealed no significant main effect by polarity interactions and therefore demonstrated no evidence of differential effects of risk factors for suicidal behavior by polarity.
Prior studies have contrasted risk of suicide between those with bipolar and unipolar disorders with mixed results. Several studies have assessed suicide risk factors in unipolar and bipolar disorders (Fawcett et al., 1990; Krupinski et al., 1998; Schneider et al., 2001; Angst et al., 2002; Oquendo et al., 2007; Tondo et al., 2007), and some have conducted separate analyses by polarity (Black et al., 1988; Kallner et al., 2000; Angst et al., 2005a). An assumption of the former studies is that risk factors do not vary by diagnosis and the latter studies do little to validate this assumption. To date, the assumption that established risk factors do not vary by polarity has not been empirically tested in a well-defined prospective cohort. None of these studies have statistically assessed, using an interaction term, differential effects of risk factors by polarity. A community sample of registered admissions did assess for differential effects of risk factors by polarity using an interaction term, but given limitations in available data was not able to test for any traditionally established risk factors apart from age, instead focusing on variables related to time from hospital admission (Hoyer et al., 2004). Another study assessed interactions though did not assess differential affects by diagnosis or polarity (Young et al., 1994). Our study uniquely addresses this long-maintained assumption for some established suicide risk factors and supports the now empirically-validated assessment of risk factors independent of polarity in affective disorders.
Of the 4,204 cycles assessed, 40 ended in suicide and 384 contained suicide attempts. To ensure adequate power to assess the differential effect of risk factors for suicidal behavior by polarity, we utilized suicidal behavior, representing suicide attempts or completions, as an outcome. The inclusion of suicide attempts may nonetheless limit the generalizability of our findings to the prediction of risk for completed suicide. Those who complete suicide may represent an overlapping but not identical population from those who attempt suicide (Beautrais, 2001). Our focus on polarity further did not allow the assessment of a differential effect of risk factors by bipolar subtype. The lower cumulative depression burden in those with bipolar disorder reflects those with bipolar I, but not bipolar II spending less time depressed. Comparison by bipolar subtype would further allow assessment of other risk factors, such as mixed states or cycling. Our analyses controlled for a linear effect of age on suicide, which may not adequately control for a non-linear age effect. A significant linear effect of age was nonetheless revealed and analysis of the data did not suggest a non-linear age effect. The adjustment of our diagnosis for prospective changes in the psychiatric status of participants strengthens the comparison of these groups by reducing the risk of misclassification. Length of follow-up considered, our observed rate of conversion from unipolar to bipolar disorder is generally consistent with the previous literature (Akiskal et al., 1983; Akiskal et al., 1995; Goldberg et al., 2001; Angst et al., 2005b). Screening of vital statistics and obtaining death certificates reduces our risk of misclassification for suicide; however, it remains possible that those who died of unknown causes may have actually died of suicide and have been misclassified. The Collaborative Depression Study uniquely provides comprehensive demographic, diagnostic, and phenomenological data for a large clinical sample of individuals with affective disorders followed for an extended period of time. Other advantages of this sample include rigorous clinical evaluations and low rates of loss to follow-up.
The mixed-effects grouped-time models used in this analysis pose several advantages for the assessment of suicide risk factors in a longitudinal study of this duration. Many studies in psychiatry using survival analysis have utilized more traditional time-to-event approaches such as the logrank test or Cox proportional hazards models (Leon et al., 1990). These approaches assume independence among observations and therefore cannot include repeated observations per participant. To accommodate changes in risk factors over time, we changed the unit of analysis to mood cycle, allowing risk factors to be re-assessed each cycle. The mixed-effects grouped-time survival method represents a modern approach to examine correlated observations, such as multiple mood cycles, in a single model (Hedeker et al., 2000). This allows for correlation in within-subject mood cycles and for the number of mood cycles to vary widely. All prospectively observed mood cycles were able to be analyzed together, allowing us to assess polarity as a predictor of suicidal behavior and a differential effect of risk factors by polarity within a mood cycle. Many of these risk factors vary over time and our statistical modeling was able to account for this.
The lack of any independent or differential effects of polarity on suicide risk poses several clinical and public health implications. Previous research has suggested that suicide risk factors may differ between those with alcoholism and those without (Murphy et al., 1992). Our data does not support any such differences by polarity in affective disorders. While the presence of an affective disorder shapes suicide risk assessment, polarity may be of limited relevance for suicidal risk or the effect of other suicide risk factors. This information may inform current efforts to develop standardized tools to augment the clinical suicide risk assessment. In the light of growing interest in the use of standardized suicide assessment psychometrics, it will be important to clearly delineate that suicide risk factors do not vary by diagnosis. While the current study suggests no differences in risk factors between the bipolar and unipolar disorders, these findings may not generalize outside of the affective disorders. Suicide risk remains difficult to predict (Goldstein et al., 1991) and public health initiatives should continue to target the identification and appropriate treatment of affective disorders as a general preventative approach (Rihmer, 1996; Mann et al., 2005).
Acknowledgments
We thank Nancy Hsuing, Carol A. Moss, and Barbara M. Robb for graciously sharing their understanding of the data collection and recording procedures involved.
This study was funded by NIMH grants 5R01MH025416-33 (W Coryell), 5R01MH023864-35 (J Endicott), 5R01MH025478-33 (M Keller), 5R01MH025430-33 (J Rice), and 5R01MH029957-30 (WA Scheftner). This study was conducted with the current participation of the following investigators: M.B. Keller, M.D. (Chairperson, Providence, RI); W. Coryell, M.D. (Co-Chairperson, Iowa City, IA); D.A. Solomon, M.D. (Providence, RI); W. Scheftner, M.D. (Chicago, IL); J. Endicott, Ph.D., A.C. Leon, Ph.D., and J. Loth, M.S.W. (New York, NY); and J. Rice, Ph.D., (St. Louis, MO).
This manuscript has been reviewed by the Publication Committee of the Collaborative Depression Study and has its endorsement. The data for this manuscript came from the National Institute of Mental Health (NIMH) Collaborative Program on the Psychobiology of Depression - Clinical Studies. The Collaborative Program was initiated in 1975 to investigate nosologic, genetic, family, prognostic, and psychosocial issues of mood disorders, and is an ongoing, long-term multidisciplinary investigation of the course of mood and related affective disorders. The original principal and co-principal investigators were from five academic centers and included Gerald Klerman, M.D.* (Co-Chairperson), Martin Keller, M.D., Robert Shapiro, M.D.* (Massachusetts General Hospital, Harvard Medical School), Eli Robbins, M.D.*, Paula Clayton, M.D., Theodore Reich, M.D.,* Amos Wellner, M.D.* (Washington University Medical School), Jean Endicott, Ph.D., Robert Spitzer, M.D., (Columbia University), Nancy Andreasen, M.D., Ph.D., William Coryell, M.D., George Winokur, M.D.* (University of Iowa), Jan Fawcett, M.D., William Scheftner, M.D. (Rush-Presbyterian-St. Luke’s Medical Center). The NIMH Clinical Research Branch was an active collaborator in the origin and development of the Collaborative Program with Martin M. Katz, Ph.D., Branch Chief as the Co-Chairperson and Robert Hirschfeld, M.D. as the Program Coordinator. Other past collaborators include J. Croughan, M.D., M.T. Shea, Ph.D., R. Gibbons, Ph.D., M.A. Young, Ph.D., D.C. Clark, Ph.D.
Footnotes
deceased
Declaration of Interest
Dr. Fiedorowicz is supported by L30 MH075180-02, the Nellie Ball Trust Research Fund, and a NARSAD Young Investigator Award. He has further received support for participating in a colleague’s investigator-initiated study with Eli Lilly. Dr. Leon has served as a consultant to the National Institute of Mental Health and Food and Drug Administration and as a member of Data and Safety Monitoring Boards for Pfizer, Organon, and Dainippon Sumitomo Pharma America. Dr. Keller has served as a consultant or received honoraria from Collegium, Cypress Bioscience, Cyberonics, Eli Lilly, Forest Laboratories, Janssen, Organon, Otsuka, Pfizer, Pharmastar, Sepracor, Vela Pharmaceuticals, Wyeth Pharmaceuticals. He has received grants from Eli Lilly, Pfizer, and Wyeth Pharmaceuticals. He has served on advisory boards for Abbott Laboratories, Bristol-Myers Squibb, Cyberonics, Cypress Bioscience, Eli Lilly, Forest Laboratories, GlaxoSmithKline, Janssen, Novartis, Organon, Pfizer, Sepracor, and Wyeth Pharmaceuticals. Dr. Solomon has served as an investigator for research funded by Jansenn Pharmaceutica, as a consultant to Solvay Pharmaceuticals, Shire, and Novartis, and has served on the lecture bureaus of AstraZeneca, Pfizer, GlaxoSmithKline, and Shire. Dr. Rice is listed as an inventor on a patent (US 20070258898) held by Perlegen Sciences, Inc., covering the use of certain single nucleotide polymorphisms in determining the diagnosis, prognosis, and treatment of addiction. All other authors declare that they have no conflicts of interest.
References
- Akiskal HS, Maser JD, Zeller PJ, Endicott J, Coryell W, Keller M, Warshaw M, Clayton P, Goodwin F. Switching from ‘unipolar’ to bipolar II. An 11-year prospective study of clinical and temperamental predictors in 559 patients. Archives of General Psychiatry. 1995;52:114–123. doi: 10.1001/archpsyc.1995.03950140032004. [DOI] [PubMed] [Google Scholar]
- Akiskal HS, Walker P, Puzantian VR, King D, Rosenthal TL, Dranon M. Bipolar outcome in the course of depressive illness. Phenomenologic, familial, and pharmacologic predictors. Journal of Affective Disorders. 1983;5:115–128. doi: 10.1016/0165-0327(83)90004-6. [DOI] [PubMed] [Google Scholar]
- Angst F, Stassen HH, Clayton PJ, Angst J. Mortality of patients with mood disorders: follow-up over 34–38 years. Journal of Affective Disorders. 2002;68:167–181. doi: 10.1016/s0165-0327(01)00377-9. [DOI] [PubMed] [Google Scholar]
- Angst J, Angst F, Gerber-Werder R, Gamma A. Suicide in 406 mood-disorder patients with and without long-term medication: a 40 to 44 years’ follow-up. Archives of Suicide Research. 2005a;9:279–300. doi: 10.1080/13811110590929488. [DOI] [PubMed] [Google Scholar]
- Angst J, Sellaro R, Stassen HH, Gamma A. Diagnostic conversion from depression to bipolar disorders: results of a long-term prospective study of hospital admissions. Journal of Affective Disorders. 2005b;84:149–157. doi: 10.1016/S0165-0327(03)00195-2. [DOI] [PubMed] [Google Scholar]
- Beautrais AL. Suicides and serious suicide attempts: two populations or one? Psychological Medicine. 2001;31:837–845. doi: 10.1017/s0033291701003889. [DOI] [PubMed] [Google Scholar]
- Black DW, Winokur G, Nasrallah A. Effect of psychosis on suicide risk in 1,593 patients with unipolar and bipolar affective disorders. American Journal of Psychiatry. 1988;145:849–852. doi: 10.1176/ajp.145.7.849. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Years of Potential Life Lost (YPLL) Before Age 65, 1999 – 2002 United States. [Accessed 21 October 2005];WISQARS Years of Potential Life Lost (YPLL) Reports, 1999 – 2002. 2005 ( http://webapp.cdc.gov/sasweb/ncipc/ypll10.html)
- Cassano GB, Akiskal HS, Savino M, Musetti L, Perugi G. Proposed subtypes of bipolar II and related disorders: with hypomanic episodes (or cyclothymia) and with hyperthymic temperament. Journal of Affective Disorders. 1992;26:127–140. doi: 10.1016/0165-0327(92)90044-7. [DOI] [PubMed] [Google Scholar]
- Chen YW, Dilsaver SC. Lifetime rates of suicide attempts among subjects with bipolar and unipolar disorders relative to subjects with other Axis I disorders. Biological Psychiatry. 1996;39:896–899. doi: 10.1016/0006-3223(95)00295-2. [DOI] [PubMed] [Google Scholar]
- Coryell W, Andreasen NC, Endicott J, Keller M. The significance of past mania or hypomania in the course and outcome of major depression. American Journal of Psychiatry. 1987;144:309–315. doi: 10.1176/ajp.144.3.309. [DOI] [PubMed] [Google Scholar]
- Coryell W, Arndt S, Turvey C, Endicott J, Solomon D, Mueller T, Leon AC, Keller M. Lithium and suicidal behavior in major affective disorder: a case-control study. Acta Psychiatrica Scandinavica. 2001;104:193–197. doi: 10.1034/j.1600-0447.2001.00338.x. [DOI] [PubMed] [Google Scholar]
- Coryell W, Endicott J, Reich T, Andreasen N, Keller M. A family study of bipolar II disorder. British Journal of Psychiatry. 1984;145:49–54. doi: 10.1192/bjp.145.1.49. [DOI] [PubMed] [Google Scholar]
- Coryell W, Haley J, Endicott J, Solomon D, Leon AC, Keller M, Turvey C, Maser JD, Mueller T. The prospectively observed course of illness among depressed patients who commit suicide. Acta Psychiatrica Scandinavica. 2002;105:218–223. doi: 10.1034/j.1600-0447.2002.1o127.x. [DOI] [PubMed] [Google Scholar]
- Coryell W, Keller M, Endicott J, Andreasen N, Clayton P, Hirschfeld R. Bipolar II illness: course and outcome over a five-year period. Psychological Medicine. 1989;19:129–141. doi: 10.1017/s0033291700011090. [DOI] [PubMed] [Google Scholar]
- Dalton EJ, Cate-Carter TD, Mundo E, Parikh SV, Kennedy JL. Suicide risk in bipolar patients: the role of co-morbid substance use disorders. Bipolar Disorders. 2003;5:58–61. doi: 10.1034/j.1399-5618.2003.00017.x. [DOI] [PubMed] [Google Scholar]
- Dunner DL, Gershon ES, Goodwin FK. Heritable factors in the severity of affective illness. Biological Psychiatry. 1976;11:31–42. [PubMed] [Google Scholar]
- Endicott J, Nee J, Andreasen N, Clayton P, Keller M, Coryell W. Bipolar II. Combine or keep separate? Journal of Affective Disorders. 1985;8:17–28. doi: 10.1016/0165-0327(85)90068-0. [DOI] [PubMed] [Google Scholar]
- Endicott J, Spitzer RL. A diagnostic interview: the schedule for affective disorders and schizophrenia. Archives of General Psychiatry. 1978;35:837–844. doi: 10.1001/archpsyc.1978.01770310043002. [DOI] [PubMed] [Google Scholar]
- Endicott J, Spitzer RL. Use of the Research Diagnostic Criteria and the Schedule for Affective Disorders and Schizophrenia to study affective disorders. American Journal of Psychiatry. 1979;136:52–56. doi: 10.1176/ajp.136.1.52. [DOI] [PubMed] [Google Scholar]
- Fawcett J, Scheftner W, Clark D, Hedeker D, Gibbons R, Coryell W. Clinical predictors of suicide in patients with major affective disorders: a controlled prospective study. American Journal of Psychiatry. 1987;144:35–40. doi: 10.1176/ajp.144.1.35. [DOI] [PubMed] [Google Scholar]
- Fawcett J, Scheftner WA, Fogg L, Clark DC, Young MA, Hedeker D, Gibbons R. Time-related predictors of suicide in major affective disorder. American Journal of Psychiatry. 1990;147:1189–1194. doi: 10.1176/ajp.147.9.1189. [DOI] [PubMed] [Google Scholar]
- Fiedorowicz JG, Coryell WH. Cholesterol and suicide attempts: A prospective study of depressed inpatients. Psychiatry Research. 2007;152:11–20. doi: 10.1016/j.psychres.2006.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg JF, Harrow M. Consistency of remission and outcome in bipolar and unipolar mood disorders: a 10-year prospective follow-up. Journal of Affective Disorders. 2004;81:123–131. doi: 10.1016/S0165-0327(03)00161-7. [DOI] [PubMed] [Google Scholar]
- Goldberg JF, Harrow M, Whiteside JE. Risk for bipolar illness in patients initially hospitalized for unipolar depression. American Journal of Psychiatry. 2001;158:1265–1270. doi: 10.1176/appi.ajp.158.8.1265. [DOI] [PubMed] [Google Scholar]
- Goldstein RB, Black DW, Nasrallah A, Winokur G. The prediction of suicide. Sensitivity, specificity, and predictive value of a multivariate model applied to suicide among 1906 patients with affective disorders. Archives of General Psychiatry. 1991;48:418–422. doi: 10.1001/archpsyc.1991.01810290030004. [DOI] [PubMed] [Google Scholar]
- Hedeker D, Siddiqui O, Hu FB. Random-effects regression analysis of correlated grouped-time survival data. Statistical Methods in Medical Research. 2000;9:161–179. doi: 10.1177/096228020000900206. [DOI] [PubMed] [Google Scholar]
- Hoyer EH, Olesen AV, Mortensen PB. Suicide risk in patients hospitalised because of an affective disorder: a follow-up study, 1973–1993. Journal of Affective Disorders. 2004;78:209–217. doi: 10.1016/S0165-0327(02)00311-7. [DOI] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS, Schettler PJ, Coryell W, Maser J, Rice JA, Solomon DA, Keller MB. The comparative clinical phenotype and long term longitudinal episode course of bipolar I and II: a clinical spectrum or distinct disorders? Journal of Affective Disorders. 2003;73:19–32. doi: 10.1016/s0165-0327(02)00324-5. [DOI] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS, Schettler PJ, Endicott J, Maser J, Solomon DA, Leon AC, Rice JA, Keller MB. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Archives of General Psychiatry. 2002;59:530–537. doi: 10.1001/archpsyc.59.6.530. [DOI] [PubMed] [Google Scholar]
- Kallner G, Lindelius R, Petterson U, Stockman O, Tham A. Mortality in 497 patients with affective disorders attending a lithium clinic or after having left it. Pharmacopsychiatry. 2000;33:8–13. doi: 10.1055/s-2000-7965. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC. The Longitudinal Interval Follow-up Evaluation. A comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Krupinski M, Fischer A, Grohmann R, Engel R, Hollweg M, Moller HJ. Risk factors for suicides of inpatients with depressive psychoses. European Archives of Psychiatry and Clinical Neuroscience. 1998;248:141–147. doi: 10.1007/s004060050031. [DOI] [PubMed] [Google Scholar]
- Kupfer DJ, Carpenter LL, Frank E. Is bipolar II a unique disorder? Comprehensive Psychiatry. 1988;29:228–236. doi: 10.1016/0010-440x(88)90046-6. [DOI] [PubMed] [Google Scholar]
- Leon AC, Friedman RA, Sweeney JA, Brown RP, Mann JJ. Statistical issues in the identification of risk factors for suicidal behavior: the application of survival analysis. Psychiatry Research. 1990;31:99–108. doi: 10.1016/0165-1781(90)90112-i. [DOI] [PubMed] [Google Scholar]
- Mann JJ, Apter A, Bertolote J, Beautrais A, Currier D, Haas A, Hegerl U, Lonnqvist J, Malone K, Marusic A, Mehlum L, Patton G, Phillips M, Rutz W, Rihmer Z, Schmidtke A, Shaffer D, Silverman M, Takahashi Y, Varnik A, Wasserman D, Yip P, Hendin H. Suicide prevention strategies: a systematic review. JAMA. 2005;294:2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- Maser JD, Akiskal HS, Schettler P, Scheftner W, Mueller T, Endicott J, Solomon D, Clayton P. Can temperament identify affectively ill patients who engage in lethal or near-lethal suicidal behavior? A 14-year prospective study. Suicide and Life-Threatening Behavior. 2002;32:10–32. doi: 10.1521/suli.32.1.10.22183. [DOI] [PubMed] [Google Scholar]
- McMahon FJ, Stine OC, Chase GA, Meyers DA, Simpson SG, DePaulo JR., Jr Influence of clinical subtype, sex, and lineality on age at onset of major affective disorder in a family sample. American Journal of Psychiatry. 1994;151:210–215. doi: 10.1176/ajp.151.2.210. [DOI] [PubMed] [Google Scholar]
- Murphy GE, Wetzel RD, Robins E, McEvoy L. Multiple risk factors predict suicide in alcoholism. Archives of General Psychiatry. 1992;49:459–463. doi: 10.1001/archpsyc.1992.01820060039006. [DOI] [PubMed] [Google Scholar]
- Oquendo MA, Bongiovi-Garcia ME, Galfalvy H, Goldberg PH, Grunebaum MF, Burke AK, Mann JJ. Sex differences in clinical predictors of suicidal acts after major depression: a prospective study. American Journal of Psychiatry. 2007;164:134–141. doi: 10.1176/appi.ajp.164.1.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oquendo MA, Waternaux C, Brodsky B, Parsons B, Haas GL, Malone KM, Mann JJ. Suicidal behavior in bipolar mood disorder: clinical characteristics of attempters and nonattempters. Journal of Affective Disorders. 2000;59:107–117. doi: 10.1016/s0165-0327(99)00129-9. [DOI] [PubMed] [Google Scholar]
- Rice J, Reich T, Andreasen NC, Endicott J, Van Eerdewegh M, Fishman R, Hirschfeld RM, Klerman GL. The familial transmission of bipolar illness. Archives of General Psychiatry. 1987;44:441–447. doi: 10.1001/archpsyc.1987.01800170063009. [DOI] [PubMed] [Google Scholar]
- Rice JP, McDonald-Scott P, Endicott J, Coryell W, Grove WM, Keller MB, Altis D. The stability of diagnosis with an application to bipolar II disorder. Psychiatry Research. 1986;19:285–296. doi: 10.1016/0165-1781(86)90121-6. [DOI] [PubMed] [Google Scholar]
- Rice JP, Rochberg N, Endicott J, Lavori PW, Miller C. Stability of psychiatric diagnoses. An application to the affective disorders. Archives of General Psychiatry. 1992;49:824–830. doi: 10.1001/archpsyc.1992.01820100068012. [DOI] [PubMed] [Google Scholar]
- Rihmer Z. Strategies of suicide prevention: focus on health care. Journal of Affective Disorders. 1996;39:83–91. doi: 10.1016/0165-0327(96)00007-9. [DOI] [PubMed] [Google Scholar]
- Scheftner WA, Young MA, Endicott J, Coryell W, Fogg L, Clark DC, Fawcett J. Family history and five-year suicide risk. British Journal of Psychiatry. 1988;153:805–809. doi: 10.1192/bjp.153.6.805. [DOI] [PubMed] [Google Scholar]
- Schneider B, Muller MJ, Philipp M. Mortality in affective disorders. Journal of Affective Disorders. 2001;65:263–274. doi: 10.1016/s0165-0327(00)00290-1. [DOI] [PubMed] [Google Scholar]
- Serretti A, Mandelli L, Lattuada E, Cusin C, Smeraldi E. Clinical and demographic features of mood disorder subtypes. Psychiatry Research. 2002;112:195–210. doi: 10.1016/s0165-1781(02)00227-5. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Endicott J, Robins E. Research diagnostic criteria: rationale and reliability. Archives of General Psychiatry. 1978;35:773–782. doi: 10.1001/archpsyc.1978.01770300115013. [DOI] [PubMed] [Google Scholar]
- Tondo L, Baldessarini RJ, Hennen J, Minnai GP, Salis P, Scamonatti L, Masia M, Ghiani C, Mannu P. Suicide attempts in major affective disorder patients with comorbid substance use disorders. Journal of Clinical Psychiatry. 1999;60(Suppl 2):63–69. discussion 75–66, 113–116. [PubMed] [Google Scholar]
- Tondo L, Lepri B, Baldessarini RJ. Suicidal risks among 2826 Sardinian major affective disorder patients. Acta Psychiatrica Scandinavica. 2007;116:419–428. doi: 10.1111/j.1600-0447.2007.01066.x. [DOI] [PubMed] [Google Scholar]
- Valtonen H, Suominen K, Mantere O, Leppamaki S, Arvilommi P, Isometsa ET. Suicidal ideation and attempts in bipolar I and II disorders. Journal of Clinical Psychiatry. 2005;66:1456–1462. doi: 10.4088/jcp.v66n1116. [DOI] [PubMed] [Google Scholar]
- Young MA, Fogg LF, Scheftner WA, Fawcett JA. Interactions of risk factors in predicting suicide. American Journal of Psychiatry. 1994;151:434–435. doi: 10.1176/ajp.151.3.434. [DOI] [PubMed] [Google Scholar]