Abstract
This study was designed to assess whether histological and biological factors of breast cancer can predict chemoresponse to specific agents. Adenosine triphosphate-based chemotherapy response assay (ATP-CRA) was employed to retrieve chemoresponse to 5-fluorouracil (5-FU), doxetaxel, doxorubicin, epirubicin, and paclitaxel in 49 patients. Tumors with high histologic and nuclear grade have higher response rate to doxorubicin (P<0.05) and palitaxel (P<0.05). Estrogen receptor (ER)-negative tumors respond well to doxorubicin (P=0.038), and progesterone receptor (PR)-negative tumors to 5-FU (P=0.039), doxetaxel (P=0.038), doxorubicin (P=0.000), epirubicin (P=0.010), and paclitaxel (P=0.003). Among the breast cancer subtypes determined by ER, PR, and HER-2 immunohistochemical stains, the HER-2+/ER- subtype has a higher response rate to doxorubicin (P=0.008). This in vitro result suggests that the combination of histologic and nuclear grade, hormone receptor, and HER-2 status can be a predictive factor of response to specific chemotherapy agents. Further in vivo study should be followed for clinical trials.
Keywords: Breast Neoplasms, Drug Therapy, Tumor Markers
INTRODUCTION
Breast cancer is one of the most common malignancies in women in the United States and a major cause of death among those in the age group of 35-60 yr (1). Chemotherapy is an established therapeutic modality for the treatment of breast cancer. Many successful developments have been made over the past few decades in the field of breast cancer treatment, however, it remains a highly dangerous disease. It is because drug responsiveness in individual patients varies and those who do not respond have a tendency toward higher rates of recurrence or metastasis. Raised thus is the need for individualized in vitro chemosensitivity assay. A number of in vitro methods, such as human tumor cloning assay (HCTA), tritiated thymidine incorporation assay (TIA), radioactive precursor incorporation assay, succinate dehydrogenase inhibition (SDI) test, 3-[4,5-dimethylethiazol-2-yl]-2, 5-diphenyltetrazolium bromide (MTT) assay, differential staining cytotoxicity (DiSC) assay, 3-dimensional agarose-based extreme drug resistance assay (EDRA), and histoculture drug response assay (HDRA), have been developed to predict therapeutic response and improve response rate and prognosis in individual patients (2-5). However, these assays have not gained popular clinical acceptance due to the considerable number of cells required, unexpected cell death and/or growth signals from contaminated normal cells, prolonged time needed to obtain results, and uncertain criteria for defining "sensitivity" or "resistance" (2, 6, 7).
The introduction of adenosine triphosphate-based chemotherapy response assay (ATP-CRA) has overcome these technical problems. Because intracellular ATP is the basic energy source for all living cells, decreased cellular ATP levels after treatment with chemotherapeutic drugs mean the loss of cell viability. ATP-CRA was found to have a substantial success rate in primary cell culture and requires only a small number of cells. It eliminates the problems caused by fibroblast contamination and can be performed relatively quickly (6, 8). Moreover, recent studies have found that ATP-CRA results predict chemosensitivity in patients with breast cancer (9).
Prognostic factors are used to aid clinical decision making and select the appropriate treatment for individual patients. Among prognostic factors, biological factors are the most important and integral (10). Tumor biological markers are able to predict the likelihood of a response to chemotherapy and can determine which agent would most likely be effective for each patient. Well-known biological factors for breast cancers are ER, PR, HER-2, p53, and Ki-67, which, along with histological factors, are widely used as prognostic factors (17). However, their role as predictive factors of chemotherapeutic responsiveness is obscure. Biological factors such as ER, PR, p53, Ki-67, and HER-2 are considered predictive or prognostic factors in the neoadjuvant setting (11, 12), but these factors are often contradictory and inconclusive because of heterogeneous patient populations and different chemotherapeutic regimens.
In the current study, we explored the possibility of histological and biological factors of breast cancers as predictive factors of chemoresponsiveness to specific chemotherapeutic agents using ATP-CRA.
MATERIALS AND METHODS
Patient selection and analysis of clinicopathologic parameters
Forty-nine patients newly diagnosed with breast cancer between July 2006 and January 2007 at Yongdong Severance Hospital, Yonsei University College of Medicine, Seoul, Korea, were enrolled in this study. This study was approved by the Institutional Review Board of Yonsei University Severance Hospital and written Informed consent was obtained from all participants. All patients were diagnosed as having invasive breast carcinoma by a pathologist. Case of only invasive ductal carcinoma, not otherwise specified (NOS) was included in this study. All tissues were fixed in 10% buffered formalin and embedded in paraffin. All archival hematoxylin and eosin (H&E)-stained slides for each case were reviewed by two pathologists. Histological grade was assessed using the modified Bloom-Richardson classification and nuclear grade was evaluated according to the modified Black's system (1=low, 2=intermediate, and 3=high) (13). Tubule formation score was evaluated as follow; score 1, tubule formation >75% of tumor, score 2, tubule formation 10-75% of tumor, score 3, tubule formation <10% of tumor. Mitosis was scored as follow; score 1, mitosis count 0-9/10 high power fields (HPFs), score 2, mitosis count 10-19/10 HPFs, score 3, mitosis count >20/10 HPFs. Histologic parameters were analyzed from H&E-stained slides. Clinicopathologic parameters evaluated in each tumor included patient age at initial diagnosis, and sex.
Immunohistochemical staining
Immunohistochemical staining for ER, PR, HER-2, p53, and Ki-67 was performed on tissue blocks. Briefly, all immunostainings were performed using formalin-fixed, paraffin-embedded tissue sections. Five-µm-thick sections were obtained with a microtome, transferred onto adhesive slides, and dried at 62℃ for 30 min. After incubation with primary antibodies against ER (1:50 dilution; Dinona, Seoul, Korea), PR (1:100 dilution; Dinona), Her2/neu (1:250 dilution; Dako, Glostrup, Denmark), p53 (1:1,600 dilution; Dako), and Ki-67 (1:400 dilution; Novocastra, Newcastle, U.K.), immunodetection was performed with biotinylated antimouse immunoglobulin, followed by peroxidase-labeled streptavidin using a labeled streptavidin biotin kit with 3,3'-diaminobenzidine chromogen as substrate. The primary antibody incubation step was omitted in negative controls. Slides were counterstained with Harris hematoxylin. Normal breast tissues entrapped within the block and appropriate control tissues were used as positive controls.
Interpretation of immunohistochemical staining
All immunohistochemical markers were assessed by light microscopy. ER and PR immunohistochemistry signal was assessed using the Allred Score. Briefly, a proportion score was assigned representing the estimated proportion of positive staining tumor cells (0=none, 1≤1/100, 2=1/100 to <1/10, 3=1/10 to <1/3, 4=1/3-2/3, and 5≥2/3). The average estimated intensity of staining in positive cells was assigned an intensity score (0=none, 1=weak, 2=intermediate, and 3=strong). Proportion score and intensity score were added to obtain a total score that ranged from 0 to 8. A score of 0 to 2 was considered negative and 3 to 8 was considered positive. HER-2 immunostaining was considered positive when strong (3+) membranous staining was observed in at least 10% of tumor cells whereas cases with 0 to 2+ were regarded as negative.
Breast cancer subtyping was done based on immunohistochemical staining results for ER, PR, and HER-2. We defined the basal-like subtypes as ER-, PR-, and HER-2-; HER-2+/ER- subtypes as ER-, PR-, and HER-2+; luminal A subtypes as ER+ or PR+; and HER-2 - and luminal B subtypes as ER+ or PR+ and HER-2+.
Immunohistochemical staining results of p53 were considered positive when more than 10% of tumor cell nuclei were stained. Immunohistochemical staining of Ki-67 was scored by counting the number of positively stained nuclei and expressed as a percentage of total tumor cells. These results were classified as follows: Group 1: ≤10%, Group 2: 10-29%, and Group 3: ≥30%. All samples were evaluated without knowledge of ATP-CRA results.
ATP-CRA methodology
ATP-CRA was performed as described (14). Tumor tissues were stored in Hank's balanced salt solution (Gibco BRL, Rockville, MD, U.S.A.) containing 100 IU/mL of penicillin (Sigma, St. Louis, MO, U.S.A.), 100 µg/mL of streptomycin (Sigma), 100 µg/mL of gentamicin (Gibco BRL), 2.5 µg/mL of amphotericin B (Gibco BRL), and 5% fetal bovine serum (Gibco BRL). When required, tissues were washed, quantitated, minced, and then incubated with a mixture of dispase, pronase, and DNase (Sigma) for 12-16 hr at 37℃. Isolated cells were separated from tissue fragments by passing through a cell strainer (BD Falcon, Bedford, MA, U.S.A.). Tumor cells were separated from dead cells and red blood cells by ficoll (1.077 g/mL) gradient centrifugation at 400 G for 15 min. When a sufficient amount of cells were isolated, blood-derived normal cells were removed using anti-CD45 antibody conjugated magnetic beads (Miltenyi Biotech, Auburn, CA, U.S.A.) (15). The separated tumor cell preparation was suspended in IMDM (Gibco BRL) including 10% FBS. Cells were then diluted to a cell concentration between 2000 and 20,000 viable cells/100 µL for plating into a 96-well ultra low attachment (ULA) microplate (Costar, Cambridge, MA, U.S.A.) with or without anticancer drugs and cultured for 48 hr in a CO2 incubator. The cytotoxic agents selected for assay were those commonly used in the treatment of breast cancer: 5-FU, doxetaxel, doxorubicin, epirubicin, and paclitaxel.
Test drug concentration (TDC) was determined by preliminary experiment that exhibited scattered distribution of cell death from each specimen (20, 21). The TDCs used were as follows: 5-FU, 50 µg/mL; doxetaxel, 3.7 µg/mL; doxorubicin, 1.5 µg/mL; epirubicin, 1.2 µg/mL; and paclitaxel, 8.5 µg/mL. To measure ATP level, ATP in the cell lysate was reacted with luciferin and excessive luciferase (Roche, Mannheim, Germany) using Victor 3 multilabel counter (PerkinElmer, Boston, MA, U.S.A.). Excel-based raw data was analyzed by Report Maker version 1.1 (ISU ABXIS, Seoul, Korea). Briefly, the cell death rate for each drug was calculated as follows: cell death rate (%)=(1-[mean luminescence in treated group/mean luminescence in untreated controls group])×100. To calculate the intra-assay mean coefficient of variation (CV), luminescence values of each specimen were measured 3-6 times in negative and positive control groups. We then determined whether measured values at 280 pg of ATP were higher than at 105 pg of ATP. If microorganism contamination was present, if there was an inadequate number of cells, or if the intra-assay mean CV exceeded 30, the test concerned was considered a failure. If measured values in the untreated control group were lower than in the positive group (105 pg of ATP), the specimen was considered to have unacceptable viability.
Statistical analysis
Statistical analyses were carried out using SPSS for Windows version 12.0 (SPSS Inc., Chicago, IL, U.S.A.). The statistical significance of any differences observed for the expression of biological markers and histologic factors in response to cytotoxic drugs was calculated using t-test. Variables having more than 3 groups (histologic grade, tubule formation score, nuclear grade, mitosis score, and Ki-67) were analyzed with 1-way ANOVA and Turkey b multiple comparison test.
RESULTS
Patient and tumor characteristics
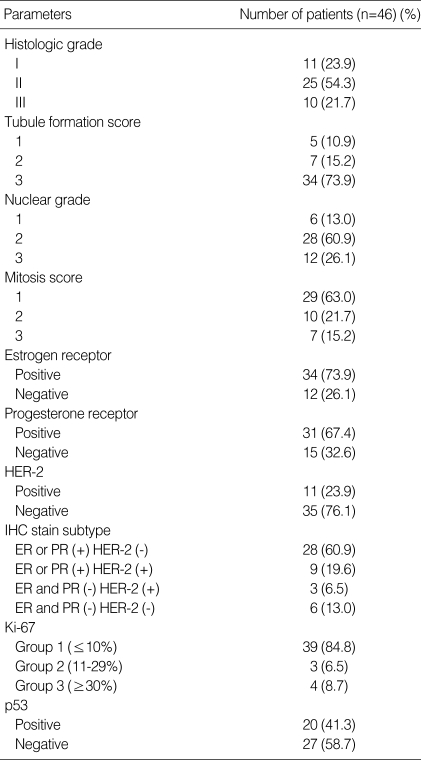
Patient and tumor characteristics are summarized in Table 1. Forty-six patients were included in this study. All patients were women with a mean age of 50.1±10.5 yr (range, 35-76 yr). Histologic grade was scored as follows: grade I, 11 cases (23.9%); grade II, 25 (54.3%); and grade III, 10 (21.7%). Tubule or gland formation score was also evaluated. Thirty-four cases (73.9%) had tubule formation score 3, 7 (15.2%) had score 2, and 5 had (10.9%) score 1. Cases of nuclear grade 1 were 6 (13.0%), nuclear grade 2 were 28 (60.9%), and nuclear grade 3 were 15 (26.1%). The cases with mitosis score 1 were 29 (63.0%), score 2 were 10 (21.7%), and score 3 were 7 (15.2%). Thirty-four cases (73.9%) were ER positive and 31 (67.4%) were PR positive. Thirty-five cases (77.6%) were considered HER-2- and 11 (23.9%) were classified as HER-2+. The staining results of Ki-67 were scored as follows: group 1, 39 cases (84.8%); group 2, 3 (6.5%); and group 3, 4 (8.7 %). Twenty-seven cases (58.7%) were p53 negative.
Table 1.
Characteristics of breast cancer
ER, estrogen receptor; PR, progesterone receptor; HER-2, human epidermal growth factor receptor 2.
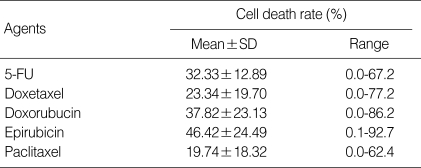
In vitro drug sensitivity of breast cancer cells by ATP-CRA
A list of the chemotherapeutic agents tested and their corresponding results are presented in Table 2. The cell death rate ranged from 0.0 to 92.7%. The results showed that paclitaxel had the narrowest range of cytotoxic effects (0.0-62.4%) with the lowest mean cell death rate (19.7%) and epirubicin had the widest range of cytotoxic effects (0.1-92.7%) with the highest mean cell death rate (46.4%).
Table 2.
Summary of ATP assay for cytotoxic agents tested
ATP, adenosine triphosphate; 5-FU, 5-fluorouracil.
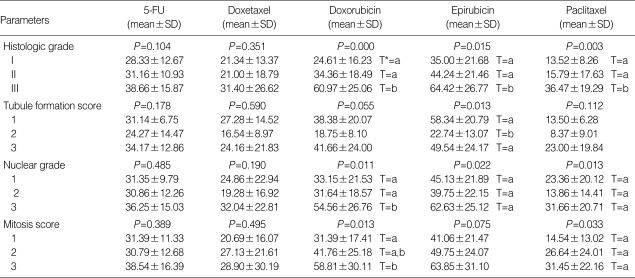
Correlation between ATP-CRA results and tumor histologic factors
Various histologic factors (histologic grade, tubule or gland formation, nuclear grade, and mitosis) were analyzed to assess any association between these factors and breast cancer cell response to cytotoxic agents. Table 3 shows the correlation between ATP-CRA results and tumor histologic factors. The response to doxorubicin (P<0.001), epirubicin (P=0.015), and paclitaxel (P=0.003) significantly increased as histologic grade increased. Multiple comparison tests revealed that there was a significant difference between grade I and III and between II and III in all of these agents. In all cytotoxic agents, higher cell death rate was noted in tubule formation score 1 and 3 than score 2, which was also true in nuclear grade scores. Epirubicin (P=0.013) revealed significant differences between score 1 and 2 and between score 2 and 3. Higher cell death rates were noted in nuclear grade 1 and 3 than grade 2. Doxorubicin (P=0.011), epirubicin (P=0.022), and paclitaxel (P=0.013) revealed significant differences. Multiple comparison tests showed that there was a significant difference between nuclear grade1 and 3 and between nuclear grade 2 and 3 only in doxorubicin and epirubicin.
Table 3.
Various tumor histological factors and ATP-CRA results
*The same letters indicate nonsignificant difference between groups based on Tukey's multiple comparison test.
ATP-CRA, adenosine triphosphate-based chemotherapy response assay; 5-FU, 5-fluorouracil; ER, estrogen receptor; PR, progesterone receptor; HER-2, human epidermal growth factor receptor 2.
As mitosis score increased, cell death rate increased in doxorubicin, epirubicin, and paclitaxel. Doxorubicin (P=0.013) and paclitaxel (P=0.033) showed significant differences. However, multiple comparison analysis revealed that a significant difference was noted between mitosis score 1 and score 3 in doxorubicin only.
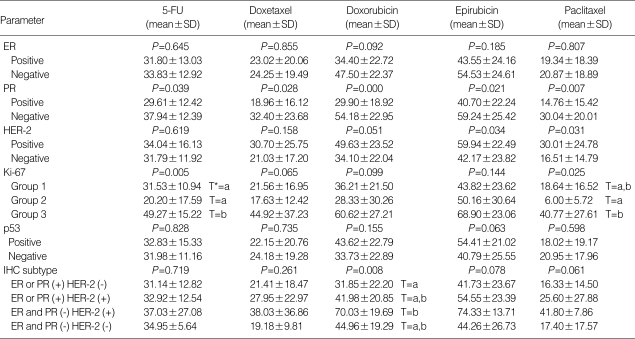
Correlation between ATP-CRA results and tumor biological factors
Expression of various biological factors (ER, PR, HER-2, Ki-67, and p53) as determined by immunohistochemistry were analyzed to assess any association between these factors and breast cancer cell response to cytotoxic agents. Table 4 demonstrates the correlation between ATP-CRA results and various tumor biological factors. All cytotoxic agents showed a trend toward higher cell death rate in ER-negative breast cancer. A significant difference was observed in doxorubicin (P=0.038). Similar results were observed in response to PR status. All cytotoxic agents represented high cell death rate in PR-negative tumors. 5-FU, doxetaxel, doxorubicin, epirubicin, and paclitaxel showed significant differences (P=0.039, 0.028, 0.000, 0.021, and 0.007, respectively). There was a tendency toward higher cell death rate in HER-2+ tumors. However, epirubicin (P=0.034) and paclitaxel (P=0.031) showed significant difference. As for the Ki-67 index, group 3 showed the highest rate of cell death, but statistical significance was noted between group1and 3 and between group 2 and 3 in 5-FU (P=0.005) and between group 2 and 3 in paclitaxel (P=0.025) only. Expression of p53 was not found to be related to tumor response to chemotherapy. Lastly, the HER-2+/ER- subtype showed the highest cell inhibition rate among all other subtypes in all cytotoxic agents. A significant difference was observed in doxorubicin (P=0.008).
Table 4.
Various tumor biological factors and ATP-CRA results
*The same letters indicate nonsignificant difference between groups based on Tukey's multiple comparison test.
ATP-CRA, adenosine triphosphate-based chemotherapy response assay; 5-FU, 5-fluorouracil; IHC, immunohistochemical stain; ER, estrogen receptor; PR, progesterone receptor; HER-2, human epidermal growth factor receptor 2.
DISCUSSION
Aided by recent developments in chemotherapeutic modalities, survival rates of breast cancer patients continue to rise. As demonstrated by the increased overall and disease-free survival in patient groups who show pathologic complete response after neoadjuvant chemotherapy (18), it is of utmost importance that chemoresponsiveness in breast cancer patients can be predicted. In this study, the in vitro chemosensitivity ATP-CRA test was used to correlate the chemosensitivity of given tumors to specific chemotherapeutic agents with various histological and biological factors to ascertain their possibility as predictive factors of chemoresponsiveness.
Traditionally, histologic grade has been known as an important prognostic factor related to survival of patients receiving preoperative chemotherapy (18), yet in our study, it was also shown to be positively correlated with the chemoresponsiveness to doxorubicin (P<0.001), epirubicin (P=0.015), and paclitaxel (P=0.003). Previous reports of in vitro chemosensitivity studies did not include evaluations of chemoresponsiveness according to histologic grade. Moreover, our study stands out by the fact that we were able to evaluate chemoresponsiveness to a single agent as opposed to clinical trials that are mostly about combined chemotherapy. Chemoresponsiveness according to scores on tubule formation and nuclear grades, 2 histological factors that together determine histologic grade, was also analyzed. Epirubicin (P=0.013) showed higher tumor cell death in tubule formation score 1 and 3 than score 2. It is well known that tumors with tubule formation score 3 show higher cell death rate as tumors with minimal tubule formation generally have higher nuclear grade and mitotic count, and hence higher chemoresponsiveness. However, the same result for tumors with score 1 for tubule formation is somewhat unexpected. Since there is no published data on chemoresponsiveness according to the degree of tubule formation in breast cancer, further research is necessary. In doxorubicin (P=0.011), tumors of nuclear grade 3 showed higher tumor cell death rate. This result concurs with a previous report stating that tumors with higher nuclear grade show higher rates of complete response to chemotherapy compared to those with lower nuclear grade (20). Tumors with high mitotic rates and Ki-67 scores, both of which are proliferative indices of tumor cell proliferation, have demonstrated increased response to cytotoxic agents, the former especially to doxorubicin (P=0.013) and the latter to 5-FU (P=0.005) and paclitaxel (P=0.025). There are contrasting views on the Ki-67 index, with some suggesting that it has no relevance to chemoresponsiveness (19) while others report that rapidly proliferating tumors with a high Ki-67 index have better response to chemotherapy and those with a lower Ki-67 index show good response to hormone therapy (21). These reports were based on combined chemoendocrine therapy and thus, the proliferation markers must have lost their predictive capacity in the studies. Additionally, this discordance may be attributable to the absence of a uniform methodology for staining and counting of the Ki-67 index. In this study, ER- and PR-negative tumors showed higher response to chemotherapy, which is in agreement with previous reports (22). According to Kiang et al., ER-positive tumors respond better to chemotherapy (23), and yet others report that ER and PR are not related to responsiveness to chemotherapy (4). Such discrepancies are due to differences in methods of ER and PR assays, diagnostic criteria, and chemotherapeutic regimens. With regard to diagnostic criteria, reports that have established no relevance of ER or PR to chemoresponsiveness had regarded tumors as ER or PR positive when tumors show positive reactions in more than 10% of the tumor cells, precluding those with strong immunoreactivity in less than 10%. We have chosen to include both in the positive immunoreactive group and as such, we have found that about 15% of the tumors previously stated to be ER-negative are, in fact, ER-positive. Our results show that PR-negative tumors respond better to all chemotherapeutic agents with statistical significance. PR has been known to be a weak prognostic and predictive factor compared to ER but in our study, it has shown itself to be better. Over the years, much has been learned about chemoresponsiveness according to HER-2 expression. Pritchard et al. have stated that tumors with HER-2 amplification respond better to anthracycline-containing chemotherapy (24), whereas other investigators have reported that either HER-2 overexpression is responsible for the poor response to chemotherapy (27) or it has no relevance at all (25). Our study, in contrast, showed that overexpression of HER-2 was positively correlated with chemoresponsiveness, especially in epirubicin (P=0.034) and paclitaxel (P=0.031).
Tumors were divided into 4 subtypes according to the staining patterns of ER, PR, and HER-2. The HER2+/ER- subtype had the highest chemoresponsiveness, especially to doxorubicin (P=0.008). There are reports that basal-like type (ER-, PR-, and HER-2-) and HER-2+/ER- type respond well to doxorubicin/doxetaxel (26), which is explained by the fact these types show high expression of proliferation gene cluster on gene cluster analysis although they are suggested to have different genes for chemosensitivity. Our findings showed that tumors of the HER-2+/ER- subtype responded well to doxorubicin, suggesting that they are related to topoisomerase IIα(Topo II) gene amplification. Topo II is an enzyme linked to cell transcription, replication, and the repair process (27). It is a major target of the anthracycline doxorubicin. Hence, it is proposed as a chemosensitivity marker in anthracycline-containing therapy in both in vivo and in vitro studies (28). Topo II is reported to be amplified in HER-2+/ER-subtypes of breast cancer (29), supporting the data in our study.
Still, there are a few limitations in our study. First, it is not in vivo, but in vitro. Whether the results can be appropriately applied to the clinical setting is doubted. However, previous reports have stated that the concordance rate of ATP-CRA results and clinical response is up to 85% (9). Therefore, our results can be applied to the clinical setting. Unlike clinical trials on patients who received combined chemotherapy, we had the advantage of evaluating chemoresponsiveness to a single agent. Our second limitation lies in the lack of corroboration of HER-2 amplification by FISH and the lack of molecular classification by DNA microarray when subtyping the breast tumors. Subtyping the tumors based on immunohistochemical stain results of ER, PR, and HER-2 alone can be said to be a shortcoming, however, it is thought to be overcome by the high concordance rate of DNA microarray and immunohistochemical results (30).
In conclusion, ATP-CRA has shown that a few histological and biological factors in breast cancers have significance as predictive factors of chemoresponsiveness to specific agents. Tumors with high histologic grade and nuclear grade 3 have higher response rates to doxorubicin. ER-negative tumors respond well to doxorubicin and PR-negative tumors respond well to all chemotherapeutic agents. The HER-2+/ER- subtype of breast cancer, when subtyped by immunohistochemical stain results, has a higher response rate to doxorubicin. This in vitro result suggests that the combination of histologic and nuclear grade, hormone receptor, and HER-2 status can be a predictive factor of response to specific chemotherapy agents. Further in vivo study should be followed for clinical trials.
ACKNOWLEDGMENT
We thank Sung Ho Choi for his collaboration in the technical supports of ATP-CRA.
Footnotes
This study was supported by grant 07151KFDA677 from the Korea Food & Drug Administration in 2007.
References
- 1.Jemal A, Siegel R, Ward E, Murray T, Xu J, Smigal C, Thun MJ. Cancer statistics, 2006. CA Cancer J Clin. 2006;56:106–130. doi: 10.3322/canjclin.56.2.106. [DOI] [PubMed] [Google Scholar]
- 2.Kern DH, Drogemuller CR, Kennedy MC, Hildebrand-Zanki SU, Tanigawa N, Sondak VK. Development of a miniaturized, improved nucleic acid precursor incorporation assay for chemosensitivity testing of human solid tumors. Cancer Res. 1985;45:5436–5441. [PubMed] [Google Scholar]
- 3.Mechetner E, Kyshtoobayeva A, Zonis S, Kim H, Stroup R, Garcia R, Parker RJ, Fruehauf JP. Levels of multidrug resistance (MDR1) P-glycoprotein expression by human breast cancer correlate with in vitro resistance to taxol and doxorubicin. Clin Cancer Res. 1998;4:389–398. [PubMed] [Google Scholar]
- 4.Takamura Y, Kobayashi H, Taguchi T, Motomura K, Inaji H, Noguchi S. Prediction of chemotherapeutic response by collagen gel droplet embedded culture-drug sensitivity test in human breast cancers. Int J Cancer. 2002;98:450–455. doi: 10.1002/ijc.10208. [DOI] [PubMed] [Google Scholar]
- 5.Tanigawa N, Morimoto H, Dohmae N, Shimomatsuya T, Takahashi K, Muraoka R. In vitro growth ability and chemosensitivity of gastric and colorectal cancer cells assessed with the human tumour clonogenic assay and the thymidine incorporation assay. Eur J Cancer. 1992;28:31–34. doi: 10.1016/0959-8049(92)90378-f. [DOI] [PubMed] [Google Scholar]
- 6.Cree IA, Kurbacher CM. Individualizing chemotherapy for solid tumors--is there any alternative? Anticancer Drugs. 1997;8:541–548. doi: 10.1097/00001813-199707000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Weisenthal LM, Marsden JA, Dill PL, Macaluso CK. A novel dye exclusion method for testing in vitro chemosensitivity of human tumors. Cancer Res. 1983;43:749–757. [PubMed] [Google Scholar]
- 8.Maehara Y, Anai H, Tamada R, Sugimachi K. The ATP assay is more sensitive than the succinate dehydrogenase inhibition test for predicting cell viability. Eur J Cancer Clin Oncol. 1987;23:273–276. doi: 10.1016/0277-5379(87)90070-8. [DOI] [PubMed] [Google Scholar]
- 9.Kim HA, Yom CK, Moon BI, Choe KJ, Sung SH, Han WS, Choi HY, Kim HK, Park HK, Choi SH, Yoon EJ, Oh SY. The use of an in vitro adenosine triphosphate-based chemotherapy response assay to predict chemotherapeutic response in breast cancer. Breast. 2008;17:19–26. doi: 10.1016/j.breast.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 10.Bundred NJ. Prognostic and predictive factors in breast cancer. Cancer Treat Rev. 2001;27:137–142. doi: 10.1053/ctrv.2000.0207. [DOI] [PubMed] [Google Scholar]
- 11.Chang J, Powles TJ, Allred DC, Ashley SE, Clark GM, Makris A, Assersohn L, Gregory RK, Osborne CK, Dowsett M. Biologic markers as predictors of clinical outcome from systemic therapy for primary operable breast cancer. J Clin Oncol. 1999;17:3058–3063. doi: 10.1200/JCO.1999.17.10.3058. [DOI] [PubMed] [Google Scholar]
- 12.Willsher PC, Pinder SE, Gee JM, Ellis IO, Chan SY, Nicholson RI, Blamey RW, Robertson JF. C-erbB2 expression predicts response to preoperative chemotherapy for locally advanced breast cancer. Anticancer Res. 1998;18:3695–3698. [PubMed] [Google Scholar]
- 13.Cutler SJ, Black MM, Mork T, Harvei S, Freeman C. Further observations on prognostic factors in cancer of the female breast. Cancer. 1969;24:653–667. doi: 10.1002/1097-0142(196910)24:4<653::aid-cncr2820240402>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 14.Moon YW, Choi SH, Kim YT, Sohn JH, Chang J, Kim SK, Park MS, Chung KY, Lee HJ, Kim JH. Adenosine triphosphate-based chemotherapy response assay (ATP-CRA)-guided platinum-based 2-drug chemotherapy for unresectable nonsmall-cell lung cancer. Cancer. 2007;109:1829–1835. doi: 10.1002/cncr.22601. [DOI] [PubMed] [Google Scholar]
- 15.Iinuma H, Okinaga K, Adachi M, Suda K, Sekine T, Sakagawa K, Baba Y, Tamura J, Kumagai H, Ida A. Detection of tumor cells in blood using CD45 magnetic cell separation followed by nested mutant allele-specific amplification of p53 and K-ras genes in patients with colorectal cancer. Int J Cancer. 2000;89:337–344. doi: 10.1002/1097-0215(20000720)89:4<337::aid-ijc4>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 16.Bird MC, Bosanquet AG, Gilby ED. In vitro determination of tumour chemosensitivity in haematological malignancies. Hematol Oncol. 1985;3:1–10. doi: 10.1002/hon.2900030102. [DOI] [PubMed] [Google Scholar]
- 17.Weisenthal LM, Dill PL, Finklestein JZ, Duarte TE, Baker JA, Moran EM. Laboratory detection of primary and acquired drug resistance in human lymphatic neoplasms. Cancer Treat Rep. 1986;70:1283–1295. [PubMed] [Google Scholar]
- 18.Machiavelli MR, Romero AO, Perez JE, Lacava JA, Dominguez ME, Rodriguez R, Barbieri MR, Romero Acuna LA, Romero Acuna JM, Langhi MJ, Amato S, Ortiz EH, Vallejo CT, Leone BA. Prognostic significance of pathological response of primary tumor and metastatic axillary lymph nodes after neoadjuvant chemotherapy for locally advanced breast carcinoma. Cancer J Sci Am. 1998;4:125–131. [PubMed] [Google Scholar]
- 19.Schneeweiss A, Katretchko J, Sinn HP, Unnebrink K, Rudlowski C, Geberth M, Beldermann F, Bastert G, Strittmatter HJ. Only grading has independent impact on breast cancer survival after adjustment for pathological response to preoperative chemotherapy. Anticancer Drugs. 2004;15:127–135. doi: 10.1097/00001813-200402000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Kuerer HM, Newman LA, Smith TL, Ames FC, Hunt KK, Dhingra K, Theriault RL, Singh G, Binkley SM, Sneige N, Buchholz TA, Ross MI, McNeese MD, Buzdar AU, Hortobagyi GN, Singletary SE. Clinical course of breast cancer patients with complete pathologic primary tumor and axillary lymph node response to doxorubicin-based neoadjuvant chemotherapy. J Clin Oncol. 1999;17:460–469. doi: 10.1200/JCO.1999.17.2.460. [DOI] [PubMed] [Google Scholar]
- 21.Makris A, Powles TJ, Dowsett M, Osborne CK, Trott PA, Fernando IN, Ashley SE, Ormerod MG, Titley JC, Gregory RK, Allred DC. Prediction of response to neoadjuvant chemoendocrine therapy in primary breast carcinomas. Clin Cancer Res. 1997;3:593–600. [PubMed] [Google Scholar]
- 22.Lippman ME, Allegra JC, Thompson EB, Simon R, Barlock A, Green L, Huff KK, Do HM, Aitken SC, Warren R. The relation between estrogen receptors and response rate to cytotoxic chemotherapy in metastatic breast cancer. N Engl J Med. 1978;298:1223–1228. doi: 10.1056/NEJM197806012982203. [DOI] [PubMed] [Google Scholar]
- 23.Kiang DT, Frenning DH, Goldman AI, Ascensao VF, Kennedy BJ. Estrogen receptors and responses to chemotherapy and hormonal therapy in advanced breast cancer. N Engl J Med. 1978;299:1330–1334. doi: 10.1056/NEJM197812142992403. [DOI] [PubMed] [Google Scholar]
- 24.Pritchard KI, Shepherd LE, O'Malley FP, Andrulis IL, Tu D, Bramwell VH, Levine MN. HER2 and responsiveness of breast cancer to adjuvant chemotherapy. N Engl J Med. 2006;354:2103–2111. doi: 10.1056/NEJMoa054504. [DOI] [PubMed] [Google Scholar]
- 25.Rozan S, Vincent-Salomon A, Zafrani B, Validire P, De Cremoux P, Bernoux A, Nieruchalski M, Fourquet A, Clough K, Dieras V, Pouillart P, Sastre-Garau X. No significant predictive value of c-erbB-2 or p53 expression regarding sensitivity to primary chemotherapy or radiotherapy in breast cancer. Int J Cancer. 1998;79:27–33. doi: 10.1002/(sici)1097-0215(19980220)79:1<27::aid-ijc6>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 26.Rouzier R, Perou CM, Symmans WF, Ibrahim N, Cristofanilli M, Anderson K, Hess KR, Stec J, Ayers M, Wagner P, Morandi P, Fan C, Rabiul I, Ross JS, Hortobagyi GN, Pusztai L. Breast cancer molecular subtypes respond differently to preoperative chemotherapy. Clin Cancer Res. 2005;11:5678–5685. doi: 10.1158/1078-0432.CCR-04-2421. [DOI] [PubMed] [Google Scholar]
- 27.Berger JM, Gamblin SJ, Harrison SC, Wang JC. Structure and mechanism of DNA topoisomerase II. Nature. 1996;379:225–232. doi: 10.1038/379225a0. [DOI] [PubMed] [Google Scholar]
- 28.Gudkov AV, Zelnick CR, Kazarov AR, Thimmapaya R, Suttle DP, Beck WT, Roninson IB. Isolation of genetic suppressor elements, inducing resistance to topoisomerase II-interactive cytotoxic drugs, from human topoisomerase II cDNA. Proc Natl Acad Sci USA. 1993;90:3231–3235. doi: 10.1073/pnas.90.8.3231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Orlando L, Del Curto B, Gandini S, Ghisini R, Pietri E, Torrisi R, Balduzzi A, Cardillo A, Dellapasqua S, Veronesi P, Viale G, Goldhirsch A, Colleoni M. Topoisomerase IIalpha gene status and prediction of pathological complete remission after anthracycline-based neoadjuvant chemotherapy in endocrine non-responsive Her2/neupositive breast cancer. Breast. 2008;17:506–511. doi: 10.1016/j.breast.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 30.Nielsen TO, Hsu FD, Jensen K, Cheang M, Karaca G, Hu Z, Hernandez-Boussard T, Livasy C, Cowan D, Dressler L, Akslen LA, Ragaz J, Gown AM, Gilks CB, van de Rijn M, Perou CM. Immunohistochemical and clinical characterization of the basal-like subtype of invasive breast carcinoma. Clin Cancer Res. 2004;10:5367–5374. doi: 10.1158/1078-0432.CCR-04-0220. [DOI] [PubMed] [Google Scholar]