Abstract
Purpose: The objectives of this study were to develop measures of end-of-life (EOL) care processes in nursing homes and to validate the instrument for measuring them. Design and Methods: A survey of directors of nursing was conducted in 608 eligible nursing homes in New York State. Responses were obtained from 313 (51.5% response rate) facilities. Secondary data on structural characteristics of the nursing homes were obtained from the Online Survey Certification and Reporting System. Exploratory factor analyses and internal consistency reliability analyses were performed. Multivariate regression models with fixed and random effects were estimated. Results: Four EOL process domains were identified—assessment, delivery, communication and coordination of care among providers, and communication with residents and families. The scales measuring these EOL process domains demonstrated acceptable to high internal consistency reliability and face, content, and construct validity. Facilities with more EOL quality assurance or monitoring mechanisms in place and greater emphasis on EOL staff education had better scores on EOL care processes of assessment, communication and coordination among providers, and care delivery. Facilities with better registered nurse and certified nurse aide staffing ratios and those with religious affiliation also scored higher on selected care process measures. Implications: This study offers a new validated tool for measuring EOL care processes in nursing homes. Our findings suggest wide variations in care processes across facilities, which in part may stem from lack of gold standards for EOL practice in nursing homes.
Keywords: End of life, Assessment, Delivery, Communication, Practice
Today, one in three Americans dies in a nursing home (Weitzen, Teno, Fennell, & Mor, 2003). With the aging of the baby boomers, the proportion of deaths occurring in nursing homes is projected to reach 40% by 2020 (Christopher, 2000). Additionally, as many as 30% of those who die in hospitals have been transferred from long-term care (LTC) facilities and die within 3 days of transfer (Smith, Kellerman, & Brown, 1995).
Excellence in end-of-life (EOL) care must become a major priority, but relatively, little is known about the quality of EOL care in nursing homes (National Hospice and Palliative Care Organization, 1998; Reynolds, Henderson, Schulman, & Hanson, 2002), and existing research has been largely descriptive, exploratory, and based on small samples (Dy & Lynn, 2006; Parker Oliver, Porock, & Zweig, 2004). Current findings from nursing homes point to high incidence of pain (Miller, Mor, Wu, Gozalo, & Lapane, 2002), poor assessment and management of pain and other symptoms (Teno et al., 2004), excessive reliance on hospitalizations (Castle & Mor, 1996; Miller, Gozalo, & Mor, 2001), inadequate use of hospice (Jones, Nackerud, & Boyle, 1997), inattention to advance care planning (Castle, 1997), and a widespread use of feeding tubes (Mitchell, Teno, Roy, Kabumoto, & Mor, 2003), all indicating inadequate EOL quality of care.
Prior studies of factors associated with EOL quality of care have focused largely on measures of nursing home capacity and capability (Carter & Porell, 2003; Mor, Papandonatos, & Miller, 2005; Troyer & McAuley, 2006). Although researchers have readily acknowledged the importance of processes of care in influencing EOL quality of care and outcomes, only a handful of empirical studies have been focused on EOL care processes in nursing homes (Forbes, Bern-Klug, & Gessert, 2000; Jenq, Guo, Drickamer, Marottoli, & Reid, 2004; McAuley, Buchanan, Travis, Wang, & Kim, 2006).
Care processes include assessment of EOL symptoms, delivery of appropriate medications or treatments, and effective communication among providers and with patients or families. As a component of effective EOL care, good communication among providers and with residents and their families is considered critical (Yabroff, Mandelblatt, & Ingham, 2004). Counseling or appropriate guidance for residents and family members regarding the benefits and burdens of EOL treatment options such as feeding tubes is rare; consequently, they are generally dissatisfied with the quality of such communication by nursing home staff (Forbes et al., 2000). Nursing home staff repeatedly demonstrate inadequate assessment and management of common EOL symptoms such as pain and shortness of breath, often due to lack of knowledge and skill in recognizing terminal illness (Miller, Teno, & Mor 2004) and in delivering EOL care (Ersek, Kraybill, & Hansberry, 2000; Ersek, Grant, & Kraybill, 2005; Teno et al., 2004).
To improve nursing home resident outcomes, measures are needed to determine whether or not good EOL care is being provided. To date, reliable and valid measures for assessing EOL care processes have not been available. The purpose of this study was to develop and validate an instrument for measuring EOL care processes using a large sample of nursing homes in New York State (NYS), one of the most populous states in the country.
Conceptual Framework
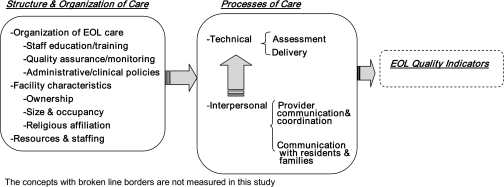
In developing the framework for measuring EOL care processes in nursing homes, we turned to the model proposed by Stewart, Teno, Donals, Pattrick, and Lynn (1999). That model was in turn based on the Donabedian's structure–process–outcomes (SPO) model (Donabedian, 1966). SPO-based studies concerned with nursing home quality of care addressed, predominantly, the relationship between structure and outcomes (Zinn & Mor, 1998), whereas the model proposed by Stewart recognized the importance of processes of care for individuals at the EOL (Stewart et al., 1999). We adapted these two models to identify components of nursing home processes and organizational structure that are hypothesized to influence EOL quality (Figure 1). In order to test the validity of this model, we postulated several hypotheses stated below.
Figure 1.
End-of-life quality of care in nursing homes: Conceptual framework.
Our conceptual framework included three overarching categories: (a) processes of care focusing on technical and interpersonal aspects, (b) structure and organization of care, and (c) risk-adjusted EOL quality indicators, examination of which is outside the scope of this study. Within this framework, processes of care such as timely recognition and effective management of distressing symptoms and better communication are considered crucial for obtaining good quality care for persons at the EOL. Both processes and outcomes of EOL care may be influenced by the way EOL care is organized (e.g., administrative and clinical policies), by the availability of resources (e.g., hospice) and staffing, and by facility characteristics (e.g., religious affiliation, ownership). The following discussion is organized along the first two dimensions as presented in Figure 1.
Processes of Care
Building on existing research, clinical guidelines for optimal care of dying patients, and our own qualitative research in NYS nursing homes, we identified technical and interpersonal care processes that are likely to affect EOL care quality for nursing home residents (Forbes-Thompson & Gessert, 2005; Froggatt & Payne, 2006; Rice, Coleman, Fish, Levy, & Kutner, 2004; Stewart et al., 1999; Thompson & Chochinov, 2006; Yabroff et al., 2004).
We identified two interpersonal processes measures: (a) communication and coordination among providers: characterized by promptness and accuracy of communication between assessing and prescribing staff, and along the chain of command, regarding residents’ symptoms and conditions and (b) communication with residents and families: characterized by accurate communication about prognosis and the risks and benefits of EOL treatments. We also identified two technical process measures: (a) assessment: characterized by recognition and timely detection of distressing physical and emotional EOL symptoms and (b) delivery: characterized by effective provision of care and management of EOL symptoms such as pain, dyspnea, and depression. In the proposed model, better performance with regard to interpersonal measures is expected to be associated with better performance on technical process measures.
Although empirical evidence is scarce, several studies suggested that EOL symptom assessment and management in nursing homes may be adversely affected by poor communication among providers, patients, and families (Forbes-Thompson & Gessert, 2005; Jenq et al., 2004; Stewart et al., 1999; Yabroff et al., 2004). We therefore hypothesized that
Hypothesis 1: Nursing homes with better (higher score) interpersonal EOL care processes, such as communication and coordination among providers and communication with residents and families, have better (higher score) EOL technical processes of care such as assessment and delivery.
Structure and Organization of Care
Our conceptual framework suggests that structure and organization of care may facilitate or hinder EOL care processes. The model specifically focuses on the organization of EOL care, facility characteristics, and resources and staffing availability as directly affecting care processes and indirectly influencing EOL outcomes.
Organization of EOL Care.—
Regardless of the level of staff training on other topics, palliative care training with regard to symptom identification, management, communication, decisions about EOL treatments, and the like is generally low (Ersek et al., 2000, 2005; Kyriacou & Nidetz, 2002; Miller et al., 2004). To date, evidence about the impact of EOL staff training on facility performance has been sparse and inconclusive (Keay, Alexander, McNally, Crusse, & Eger, 2003; Molloy et al., 2000). Research has identified several strategies considered by nursing home administrators and/or directors of nursing (DONs) to be important in improving quality of care (Brazil et al., 2006). These strategies include presence of administrative policies that focus specifically on EOL care and address resident and family treatment preferences, clinical policies and practices that focus on EOL care planning and assessment of physical and spiritual care needs, and practices for monitoring the delivery of palliative care and for assessing EOL care quality. Presence of sound EOL policies and practices that are well documented in administrative and clinical protocols provide the foundation for developing EOL organizational competencies (Hill, Ginsburg, Citko, & Cadogan, 2005). Therefore, we hypothesized that
Hypothesis 2: Nursing homes with greater emphasis on EOL-specific administrative and clinical policies and practices have better EOL care processes.
Facility Characteristics.—
Although findings are conflicting, facility performance or quality of care has been found to vary based on facility ownership and religious affiliation. Not-for-profit facilities exhibited better risk-adjusted patient outcomes (Spector, Selden, & Cohen, 1998) and have been more likely to have special EOL programs (hospice or palliative care) and staff trained in EOL care (Remsburg & Han, 2006). Religiously affiliated nursing homes have been more likely than facilities without a religious mission to pursue EOL medical treatments contrary to patients’ wishes (Hosay, 2002). We therefore hypothesized that
Hypothesis 3: Facilities that are nonprofit and are not religiously affiliated have better EOL care processes than for-profit and religiously affiliated facilities.
Resources and Staffing Availability.—
Adequate staff-to-resident ratios among nursing personnel have been shown to be directly related to quality of EOL care in nursing homes (Miller et al., 2004). Nursing homes may structure the provision of EOL care in a number of ways. They may provide care to EOL residents directly in a manner largely similar to the overall care provided to all other residents. However, they may choose to rely on hospice or palliative care. Hospice, as it refers to a specific set of services provided to the terminally ill residents, involves skilled management of pain and other symptoms, provision of personal care, spiritual counseling, and bereavement services. Palliative care refers to a similar set of services, but without the eligibility requirements mandated by Medicare and Medicaid (Ersek & Wilson, 2003). Facilities may create specialized hospice or palliative care units or contract for such care with outside organizations (Ersek & Wilson, 2003; Strumpf, Tuch, Stillman, Parrish, & Morrison, 2004). We hypothesized that
Hypothesis 4: Facilities with more EOL resources have better EOL care processes than facilities with fewer EOL resources.
Methods
Study Sample
Data for this study were obtained from primary and secondary sources. We collected primary data through a survey conducted from June through November 2007. Eligible facilities included 619 nursing homes in NYS, which (a) were certified for Medicare or Medicaid, as some information for uncertified facilities is not included in the secondary databases used in the study (note, however, that all NYS facilities are certified); (b) had more than 50 beds, as care processes in small facilities could be substantially different due to limited staff size; (c) did not specifically focus on special needs patients (e.g., pediatric facilities or those providing only rehabilitative care) as such facilities have fundamentally different organizational structures and strategic aims; and (d) had at least 2 years of operational experience, as new facilities are more likely to be experiencing a learning curve. Eleven facilities were closed or surveys could not be delivered. In total, 313 completed surveys were returned for a response rate of 51.5%.
Requests for participation in the survey were addressed to DONs and included letters of support from the New York Association of Homes and Services for the Aging and the New York State Health Facilities Association. DONs, in NYS, are registered nurses (RNs) in senior management positions. They are responsible for all nursing services provided to the residents. They plan, coordinate, establish, and maintain standards of care within their facilities. Based on the literature (Brazil et al., 2006), and on the interviews we conducted with nursing home employees during the instrument development phase, it became clear that the DONs were best positioned to provide the most comprehensive appraisal of the care provided to residents at the EOL. Respondents mailed back the surveys to the research team using prepaid envelopes. Several approaches, such as mailings, phone calls, faxes, and emails, were used to maximize the response rates.
Secondary data, containing additional information on facility characteristics, were obtained from the Online Survey Certification and Reporting System (OSCAR). OSCAR is the most comprehensive national source of facility-level information collected by the Centers for Medicare and Medicaid Services.
The study protocol was approved by the institutional review board.
Survey Instrument
Survey tool development followed accepted questionnaire construction methods (Dillman, 1978). A review of the literature provided initial direction on item development. Interviews with key informants (clinicians and nursing home managers) provided additional input. We identified a pool of 24 nursing homes in three cities in upstate New York. We selected nursing homes with a diversity of reputations with regard to EOL care quality in order to maximize the variability of opinions as to what worked well and not so well in these facilities. All homes were then approached with a request to conduct a series of in-person interviews with staff about EOL care. In total, six nursing homes were selected (two in each geographic location) representing facilities on either spectrum on EOL quality reputation. Three cross-trained interviewers conducted the interviews, which in all facilities included the following key informants: facility administrator, DON, RN, medical director (MD) or nurse practitioner (NP) or physician assistant (PA), and certified nurse aide (CNA). In three of the facilities, a licensed practical nurse and two social workers (SWs) were also interviewed. In total, 33 interviews were conducted with staff, across professions and disciplines, directly responsible for the provision of EOL care and/or facility policies guiding care delivery. An instrument containing 25 open-ended questions was used to guide the interviews. All interviews were tape-recorded, transcribed verbatim, and uploaded to Atlas.ti to facilitate data management. Using descriptive content and constant comparison techniques, our analyses focused on identifying processes (within and across homes) and roles associated with the delivery of EOL care. We then developed the survey instrument built on the identified processes.
The survey instrument consisted of three components designed to measure care processes, organizational structure, and availability of EOL resources. The first component included four care process domains as depicted in Figure 1. Altogether 29 items, on a 5-point Likert scale, characterized the domains of assessment, delivery, communication or coordination among providers, and communication with residents or families. The second component included four measures of organizational structure specific to EOL care. The four domains measured the presence of administrative policies, clinical policies and practices, monitoring quality of care, and staff education and contained 39 binary questions (“yes” or “no”). The third component included a variety of questions relating to the availability (e.g., presence of hospice contract, palliative care consultation) and use of resources (e.g., hospice use intensity), staffing, and use of certain medical treatments (e.g., feeding tubes).
First, content and clinical experts (former DONs, nurses, palliative care physicians, and EOL in nursing home researchers) reviewed the drafts of the instruments and commented on content, relevance, face validity, and clarity. The survey was then pilot tested with a group of individuals (n = 6) resembling the target population (former DONs and LTC nurses) in order to identify questions that were ambiguous or poorly written and to ascertain clarity of instructions and the time needed to complete the survey. Following the pilot, the questionnaire was slightly revised. Sample items from the domains of EOL process measures and organizational structure are presented in Appendices A and B, respectively. A copy of the full survey is available upon request.
Variable Construction
Process Measures.—
Four EOL care process domains were constructed: communication and coordination among providers, communication with residents and families, assessment, and care delivery. Each domain was measured by multiple questions or statements, both positively and negatively phrased. When two thirds or more of the items in each of these domains were not completed, the response to the domain was considered to be missing. For each item included in any given domain, a numerical score was assigned ranging from 1 for strongly disagree to 5 for strongly agree. An average score was computed by adding the values of nonmissing items in a domain and dividing the sum by the number of nonmissing items in the domain. A score of 5 represents the most positive and the score of 1 the most negative appraisal of a domain.
Organization of EOL Care.—
We constructed measures assessing the presence of EOL-specific administrative; clinical; quality monitoring; and educational policies, protocols, and practices. For each domain, we employed a measure depicting the percent of policies or practices that were documented or present in each nursing home. Higher scores imply greater organizational commitment to EOL care within a given domain.
Resources, Staffing Availability, Aggressiveness of Treatment.—
We included two measures of hospice—availability and intensity of use. We defined availability of hospice as the presence of a formal contract between a nursing home and a hospice service (dichotomous variable). The intensity with which hospice was used in the facility, as reported by the DON, was measured as a score (continuous variable) derived from two 5-point Likert scale items. These items assessed the extent to which hospice is routinely offered to EOL residents or is only offered when requested by residents or their families. Higher score reflects greater propensity to use hospice.
Staffing of RNs and CNAs for EOL care was also measured on a 5-point Likert scale and reflected the DONs’ perceptions of the degree to which sufficient staff-to-resident ratios were available to support care to dying residents. Higher scores represent better perceived staffing. The availability of on-site medical or advance practice clinicians was also measured, expressed as the sum of physicians, NPs, and PAs divided by the number of beds and multiplied by occupancy (to adjust for the size of the patient population).
Facility characteristics included two dichotomous variables—profit status (from OSCAR) and religious affiliation (from survey data).
Statistical Analysis
Survey Reliability and Validity.—
In addition to consultations with experts and our assessment that the process domains and items within were theoretically meaningful for nursing homes, we also employed exploratory factor analysis using the Statistical Analysis Software to examine structure in the relationships between items. Pearson correlation coefficients were calculated between the domains to assess redundancy or conceptual independence and between items to assess convergent–divergent validity. Reliability was assessed by measuring the internal consistency of items within each domain. Standardized Cronbach's alphas, used for this purpose, range between 0 and 1, with values exceeding .70 indicating moderate-to-high reliability (Ghiselli, Campbell, & Zedeck, 1981).
To assess construct validity, we examined whether the data provide support for the theoretical model in which the relationships between the domains of interest were defined. Several multivariate regression models were fit. In the first two models, the dependent variables were EOL care delivery and assessment. The independent variables included the remaining care processes (communication and coordination among providers and communication with residents and families) and the control variables of resources and staffing.
We estimated multivariate regression models with random effects for the metropolitan statistical area (MSA) to account for the possibility that facility-specific factors not explicitly identified may influence the dependent variables. The sample nursing homes were distributed across 11 MSAs. We also estimated a fixed-effects model in order to calculate the incremental adjusted R2 when process and resource variables were added to a model with site effects only. The incremental R2 indicates the contribution of the independent variables to the explanation of variations in the dependent variables. The results from the random and the fixed-effects models, which we reported, were essentially the same. In the remaining models, the dependent variables were the four EOL care processes, whereas the independent variables included measures of the organizational structure, resource availability and use, and selected facility characteristics.
We performed diagnostic tests for collinearity using variance inflation factor among the independent variables and detected no evidence of significant effects that may inflate standard errors.
Results
Sample Characteristics
Characteristics of participating nursing homes are displayed in Table 1. Because the survey was based on voluntary participation of eligible NYS nursing homes and was not a randomly selected sample, we compared the 313 responding homes with all eligible NYS facilities on characteristics that could affect assessment of EOL care processes (Table 1). The participating homes were significantly different (p < .0001) in terms of occupancy rates from all NYS facilities, but this difference was not operationally meaningful (93.22% vs. 92.56%, respectively). We found no other significant differences between the study sample and all eligible homes on other measures.
Table 1.
Comparison of Facility Characteristics: Analytical Sample and All Eligible Nursing Homes in NYS
| Participating nursing homes (N = 313) | All NYS nursing homes (N = 608) | p | |
| Quality measuresa | |||
| Number of health-related citations | 13.68 (8.52) | 13.78 (8.78) | .8346 |
| Number of nonhealth-related citations | 4.97 (4.82) | 4.71 (4.75) | .3376 |
| Staffing characteristicsa | |||
| Registered nurse hours per resident per day | 0.59 (0.27) | 0.58 (0.26) | .6134 |
| Total nursing hours per resident per day | 3.71 (0.67) | 3.64 (0.65) | .0650 |
| Facility characteristicsb | |||
| Bed size | 186.11 (113.99) | 196.08 (129.51) | .1240 |
| Occupancy rate | 93.22 (7.03) | 92.56 (7.72) | <.0001 |
| Church affiliated | 7.19% | 6.68% | .7731 |
| Chain membership | 12.46% | 12.46% | .9996 |
| For profit | 43.41% | 48.52% | .1417 |
Notes: NYS = New York State.
Source: Centers for Medicare and Medicaid Services Nursing Home Compare.
Source: Online Survey Certification and Reporting System.
Instrument and Model Testing
Descriptive statistics for dependent and independent variables are presented in Table 2. The dependent variables, EOL care processes, had means ranging from 3.61 to 3.84 on a scale from 1 (worst) to 5 (best) and considerable variation across facilities as demonstrated by the standard deviations. Means and standard deviations (as appropriate) are also shown for all the independent variables. EOL organization of care is characterized by the number of EOL policies present in a facility. On average, nursing homes reported having 84% of the 11 EOL clinical policies and practices surveyed as present, with other policies or practices being reported less frequently and with greater variability.
Table 2.
Variables Included in the Analyses: Descriptive Statistics (N = 313)
| Variables | Definition | Mean (SD) |
| Dependent variables | ||
| EOL process measures | ||
| Assessment | Range 1–5: 1 = worst score, 5 = best score | 3.70 (0.61) |
| Delivery | Range 1–5: 1 = worst score, 5 = best score | 3.84 (0.68) |
| Communication and coordination among providers | Range 1–5: 1 = worst score, 5 = best score | 3.76 (0.63) |
| Communication with residents and families | Range 1–5: 1 = worst score, 5 = best score | 3.61 (0.62) |
| Independent variables | ||
| Organization of EOL care | No. policies present; range 0–1 (none to all) | |
| Administrative policy | Total: 8 policies | 0.65 (0.42) |
| Clinical policies or practices | Total: 11 policies | 0.84 (0.21) |
| Quality monitoring | Total: 5 policies | 0.66 (0.28) |
| Staff education | Total: 13 policies | 0.69 (0.30) |
| EOL resources | ||
| Hospice use intensity | Range 1–5: 1 = least intense, 5 = most intense | 3.72 (1.14) |
| Hospice contracts | Presence of contracts with hospice agencies | 84.74% |
| Advance care planning | Range 1–5: 1 = worst, 5 = best | 4.04 (0.76) |
| Physicians, NPs, PAsa | Total adjusted for bed size and occupancy | 0.04 (0.05) |
| RN staffing ratio for EOL support | Range 1–5: 1 = least, 5 = most sufficient | 3.37 (1.23) |
| CNA staffing ratio for EOL support | Range 1–5: 1 = least, 5 = most sufficient | 3.31 (1.15) |
| Facility characteristics | ||
| Facility ownershipa | Profit versus nonprofit status | 56.59% |
| Religious affiliation | Religiously affiliated facility | 23.64% |
Notes: EOL = end of life; CNA = certified nurse aide, NP = nurse practitioner; PA = physician assistant, RN = registered nurse.
Source: Online Survey Certification and Reporting System. All other variables are from the EOL care process survey (authors’ primary data).
Reliability and Validity
Cronbach's analyses were performed to confirm the internal consistency reliability of scales for EOL process domains. Several items were deleted from each domain because they showed weak correlations with other domain items. The final domains of assessment and delivery demonstrated good-to-high reliability, with Cronbach's alphas of .82 and .72, respectively, and acceptable correlations with all other items (Table 3). The reliability measures for the other two domains, communication and coordination among providers (Cronbach's alpha = .63) and communication with residents and families (Cronbach's alpha = .69), were considered acceptable given the small number of items within the scales.
Table 3.
End-of-life Process Domains: Psychometric Validity and Reliability
| Factor analysis |
Internal consistency reliability |
|||||
| Domains | No. items | Mean responsea (SD) | Factor 1 loadings (range) | Eigenvalue | Standardized Cronbach's alpha | Item—total correlation (range) |
| Assessment | 10 | 3.70 (0.61) | 0.53–0.73 | 3.87 | 0.82 | 0.42–0.62 |
| Delivery | 6 | 3.84 (0.68) | 0.57–0.76 | 2.52 | 0.72 | 0.36–0.52 |
| Communication and coordination among providers | 5 | 3.76 (0.63) | 0.48–0.74 | 2.04 | 0.63 | 0.25–0.50 |
| Communication with residents and families | 8 | 3.61 (0.62) | 0.43–0.61 | 2.56 | 0.69 | 0.29–0.43 |
Note: a1 = most negative; 5 = most positive.
Principal factor analyses were also performed to confirm dimensionality in the relationship between items within each domain. Items within the four domains loaded well on a single factor, as shown by factor loadings and eigenvalues (Table 3).
As posited in the conceptual model and in Hypothesis 1, interpersonal care process measures (communication and coordination of care among providers and communication with residents and families) predicted technical care processes, that is, assessment and care delivery (p < .0001, Table 4). The DONs’ perceptions of the CNA staffing ratios as sufficient for EOL support also predicted these outcomes. The incremental adjusted R2 indicates the contribution of the process variables to the explanation of the variation in outcome measures. The interpersonal process measures and the resource and staffing variables explained 48.5% of the variation across facilities in EOL delivery and 54.4% in EOL assessment, respectively.
Table 4.
Test of Construct Validity: Multivariate Regression Model with Fixed MSA Effectsa
| Outcome = Deliveryb |
Outcome = Assessmentc |
|||
| Independent variable | Parameter estimate | p | Parameter estimate | p |
| Coordination and communication among providers | 0.26398 | <.0001 | 0.37752 | <.0001 |
| Communication with residents and families | 0.50941 | <.0001 | 0.26852 | <.0001 |
| Resources | 0.11769 | .3335 | −0.01041 | .9194 |
| RN staffing ratio | 0.01077 | .7236 | 0.05044 | .0509 |
| CNA staffing ratio | 0.07952 | .0123 | 0.10949 | <.0001 |
Notes: MSA = metropolitan statistical area RN = registered nurse, CNA = certified nurse aide.
MSA coefficients are not shown.
Adjusted R2 = .487; incremental adjusted R2 (calculated for a model in which independent variables were added to MSA fixed effects) = .485; N = 302.
Adjusted R2 = .547; incremental adjusted R2 = .544; N = 302.
We further tested construct validity by estimating four multivariate regression models in which the four EOL care processes were the dependent variables, and the independent variables were the organization of care, EOL resources, and facility characteristics (Table 5). The proportions of administrative or clinical policies that a nursing home had in place did not appear to be associated with any of the four EOL care process measures. However, in partial support of Hypothesis 2, having more EOL quality assurance or monitoring mechanisms in place and greater emphasis on EOL staff education were positively associated with better assessment, communication and coordination among providers, and delivery.
Table 5.
Factors Predicting EOL Care Processes: Multivariate Regression with MSA Random Effects (N = 278 facilities)
| Assessment |
Provider communication and coordination |
Delivery |
Communication with residents and families |
|||||
| Independent variables | Estimate | p | Estimate | p | Estimate | p | Estimate | p |
| Organization of care | ||||||||
| Administrative policy | 0.007 | .921 | 0.127 | .127 | 0.016 | .863 | 0.110 | .184 |
| Clinical policies or practices | 0.208 | .210 | 0.013 | .945 | 0.154 | .461 | 0.175 | .359 |
| Quality monitoring | 0.370 | .012 | 0.361 | .036 | 0.424 | .023 | 0.275 | .103 |
| Staff education | 0.424 | .001 | 0.283 | .049 | 0.261 | .093 | 0.061 | .667 |
| EOL resources | ||||||||
| Hospice use intensity | 0.000 | .987 | 0.023 | .466 | 0.057 | .092 | 0.066 | .033 |
| Hospice contracts | −0.110 | .231 | −0.074 | .479 | −0.028 | .808 | 0.008 | .936 |
| Physicians, NPs, PAsa | −0.470 | .439 | −1.075 | .127 | −0.636 | .408 | −0.645 | .355 |
| RN staffing ratio for EOL support | 0.123 | <.001 | 0.132 | <.001 | 0.105 | .003 | 0.146 | <.001 |
| CNA staffing ratio for EOL support | 0.143 | <.001 | 0.096 | .007 | 0.140 | .001 | 0.076 | .030 |
| Facility characteristics | ||||||||
| For-profit facility | 0.012 | .846 | 0.020 | .762 | 0.059 | .435 | 0.012 | .866 |
| Religiously affiliated facility | 0.054 | .429 | 0.158 | .047 | −0.024 | .780 | 0.205 | .010 |
Notes: EOL = end of life; CNA = certified nurse aide, MSA = metropolitan statistical area; NP = nurse practitioner; PA = physician assistant.
Adjusted for bed size and occupancy.
Facilities with religious affiliation scored higher on EOL communication and coordination among providers and communication with residents and families, thus providing partial support for Hypothesis 3. In support of Hypothesis 4, we found that facilities in which hospice care was routinely offered to residents rather than only when requested by residents or families (hospice use intensity) had better scores for communication with residents or families and for care delivery. Furthermore, better RN and CNA staffing ratios for EOL support predicted all four process measures.
Discussion
Nursing homes are increasingly the site of care at EOL, but reports about the quality of such care have not been positive. Although studies have identified a number of structural and organizational barriers to optimal EOL care in nursing homes, empirical evidence about EOL care processes has been scarce. In this study, we contributed a validated measure of four EOL care processes—assessment, delivery, communication and coordination among providers, and communication with residents and families—for nursing homes, developed in a large sample of facilities in NYS. Our findings suggest that these measures are psychometrically sound with regard to both reliability and validity. The results provide support for the conceptual model we used and for the relationships we hypothesized among its components.
Nursing homes with better communication and coordination of care among providers, and better communication with residents and their families, also had better scores on EOL assessment and delivery of care process measures. Presence of administrative and clinical policies focusing on EOL care did not seem to influence EOL care processes, but greater emphasis on EOL practices did. Facilities with more quality monitoring practices and greater focus on staff education had better scores on three of the four EOL care process measures—assessment, delivery, and provider communication and coordination—when other factors such as EOL resources and facility characteristics were controlled.
We observed considerable variation in EOL care process scores and their components across nursing homes. During survey development, nursing home respondents typically told us that EOL care was a very important component of nursing home care, but based on the survey results, nursing homes did only a slightly better than an average job, as indicated by the mean values for the four process measures, with significant variations across facilities. Only slightly more than half of nursing homes reported that EOL residents were always assessed with regard to emotional needs or that residents who did not complain of pain were assessed on every shift (Appendix A).
This wide variation in care processes may stem, at least in part, from the lack of gold standards for EOL practice in nursing homes. Although a number of organizations (e.g., Joint Commission on Accreditation of Healthcare Organizations, American Medical Directors Association) have issued guidelines, they primarily address pain management. Recommendations relating to assessment and to management of other symptoms have focused on community-dwelling elderly individuals and may not be appropriate for nursing home residents. Similarly, there are no published recommendations as to when clinicians should be notified about a resident's pain status. Thus, although disturbing, perhaps it is not surprising to learn that in fewer than 40% of nursing homes, nursing assistants consistently reported pain and other distressing symptoms of EOL residents to the appropriate clinicians (Appendix A).
In absence of such guidelines, individual nursing homes may devise their own policies for the provision of EOL care, with significant variation across institutions. Almost 75% of the surveyed facilities reported having a written policy or principles regarding care of residents at the EOL (Appendix B). However, fewer reported having specific clinical policies for managing distressing EOL symptoms (67%) or addressing symptoms of depression (69%). Even fewer facilities reported having quality monitoring mechanisms to review, for example, the appropriateness of hospital transfers for dying residents (50%).
Furthermore, as has been demonstrated in other studies, staff education and training with regard to EOL care appeared to be seriously lacking. In our sample, only two thirds of the nursing homes reported ongoing in-service education for nursing staff that included communication skills for understanding and supporting dying patients and their families (63%) or understanding symptoms and stages of death and dying (68%) (Appendix B). These findings underscore the need for standardized procedures, clinical policies, practices, and skills for routinely assessing nursing home residents with regard to their terminal status.
Our results point to several potentially modifiable factors associated with better technical and interpersonal EOL care processes. In facilities in which the responding DON considered the RN and CNA staffing ratios to be sufficient to support quality EOL care, all EOL care processes were reported to be significantly better. Improvements in staffing ratios are costly, and nursing homes (particularly for-profit facilities) are not likely to implement such changes voluntarily. Several recent incentive programs in Florida and California have shown mixed results. Additional payments to nursing homes resulted in increases in staff wages and some increases in staffing, but there was no substantial impact on residents’ outcomes (Hyer, Johnson, Harman, & Mehra, 2007; Schnelle, Mukamel, Sato, & Chang, 2008). Without additional empirical support, and particularly in times of economic distress, it is unlikely that state agencies or nursing homes themselves will have sufficient incentives to increase staffing ratios.
The findings also suggest an association between hospice use and EOL care processes. Prior studies showed that nursing home residents who were enrolled in hospice were less likely to be hospitalized at the EOL and received better pain management care than residents who were not enrolled in hospice (Miller, Mor, & Teno, 2003; Miller et al., 2004). Almost 85% of nursing homes in our study had contracts with hospice. Although we found no association between the presence of a hospice contract and EOL care processes, there was considerably greater variability with regard to the intensity of hospice use across these facilities, with 68% of homes scoring between 2.58 and 4.86 (i.e., within 1 SD of the mean) on a scale from 1 being the worst to 5 being the best. Hospice intensity was assessed by the extent to which hospice was offered routinely to EOL residents rather than only when specifically requested. We found higher intensity of hospice use to be associated with better communication with residents and families (p = .033) and also moderately associated with better EOL care delivery process (p = .092). Simply having a contract with a hospice organization may be necessary but not sufficient for better EOL care processes. A number of studies have focused on government regulations and practices that deter hospice use in nursing homes, but these barriers are unlikely to explain the variation we observed within a single state. Further research is needed to identify facility-specific factors that are conducive to greater hospice penetration in some facilities but not in others.
A few limitations should be noted. First, in conducting interviews with nursing home staff during the qualitative data collection phase, we relied to some extent on a convenience sample stratified by disciplines. RNs and CNAs who were interviewed were identified for the interviews by their nursing home administrators. Second, our survey relied on a single respondent, the DON, in each facility. As previously explained, in our qualitative research, when administrators, MDs, charge nurses, and SWs were directly asked to identify the individual with the broadest and most comprehensive understanding of the facility's day-to-day EOL practices and challenges, the DONs were identified as best positioned to provide the most accurate appraisal of EOL care in their facilities. Evidence from the literature provided additional support for this choice. For example, a survey of MDs and DONs from more than 400 nursing homes in 25 states showed that they tended to agree about factors that influence hospitalization and other care of residents in their facilities (Buchanan et al., 2006). In another study testing a case-finding questionnaire completed by nursing home facility managers, when the results from the survey were compared with quality of care measures of all residents in the surveyed homes, the case-finding questionnaire had high specificity and sensitivity, suggesting that responses provided by a single manager per facility were a simple and inexpensive way of gathering valid data (Dubois, Bravo, & Charpentier, 2001). Nevertheless, it would be prudent for future studies to use more than one respondent per facility if possible. Third, the measures of EOL care processes were based on single point in time estimates. Over longer periods of time, point estimates are not likely to accurately reflect care processes as facility characteristics may change.
In conclusion, the tool we developed and validated may be used to examine EOL care processes in nursing homes and to target quality improvement efforts when scores for a particular care process, or its components, are deemed unsatisfactory. Better EOL care processes are likely to produce better resident outcomes. Further research is needed to examine if facilities with better EOL care processes produce better risk-adjusted outcomes for their dying residents.
Funding
We gratefully acknowledge funding from the Foundation for Healthy Living in Albany, NY; the National Institute on Nursing Research, Grant R01 NR010727; and the National Institute on Aging, Grant R01 AG23077.
Acknowledgments
We also express our gratitude to the nursing homes that participated in the study and to the members of the NYS Palliative Care Research Consortium for their feedback and support.
Appendix A. End-of-Life Organizational and Process Measures in Nursing Homes: Sample Survey Items
| EOL process domains and sample items | Percent agree or strongly agree |
| Assessment (10 items) | |
| Nursing staff always assess for the emotional needs of residents at the end-of-life | 54.9% |
| When EOL residents do not complain of pain, nursing staff assess their symptoms on every shift | 55.7% |
| Nursing staff has good understanding of the needs of family members of residents who are at the end-of-life | 61.9% |
| Delivery (6 items) | |
| When residents are depressed at the end-of-life, counseling and/or medications are promptly initiated | 58.8% |
| There is sufficient pain management expertise in our facility | 59.2% |
| Medical staff are reluctant to prescribe opioids, when appropriate, for residents who are significantly short of breath | 18.6% |
| Communication/coordination among providers (5 items) | |
| Nursing assistants consistently report pain and other distressing symptoms of residents to the appropriate clinician | 39.6% |
| Nursing staff regularly discuss issues concerning management of pain and other symptoms of residents during daily reports/meetings | 65.5% |
| When a prescribing clinician is informed about a resident being in pain a new order is typically written within 2 hours or less | 79.7% |
| Communication with residents and families (8 items) | |
| Our residents/families understand what hospice is | 54.6% |
| Residents/families do not have a good understanding of the risks of CPR | 40.0% |
| Our physicians are reluctant to discuss end-of-life issues with residents/families | 16.6% |
Appendix B. End-of-Life Organizational Policies and Practices: Selected Items
| Selected EOL Organizational Policies and Practices | Percent “YES” |
| Administrative policy | |
| Is there currently a written statement of the facility's principles or policy regarding care of residents at the end-of-life? | 73.2% |
| If so, does it address: | |
| Withholding and withdrawing life-sustaining measures such as artificial nutrition? | 80.7% |
| Clinical policies and practices | |
| Are there palliative care policies for managing distressing symptoms such as dyspnea, nausea? | 66.7% |
| Are there policies for arranging for palliative care or hospice when appropriate? | 81.5% |
| Quality monitoring | |
| Have quality assurance mechanisms been established for monitoring delivery of palliative care, such as pain control, management of distressing symptoms (e.g. shortness of breath, anxiety)? | 69.9% |
| When residents are transferred to acute care, is there a routine quality review to assess the appropriateness of transfer? | 50.2% |
| Education | |
| Does on-going in-service education for nursing staff (CNA/LPN/RN) include the symptoms and stages of death and dying? | 68.4% |
| Are there educational materials available for residents/families on decision making and care for those near the end-of-life? | 74.5% |
References
- Brazil K, Krueger P, Bedard M, Kelley M, McAiney C, Justice C, et al. Quality of care for residents dying in Ontario long-term care facilities: Findings from a survey of directors of care. Journal of Palliative Care. 2006;22:18–25. [PubMed] [Google Scholar]
- Buchanan J, Murkofsky R, O’Malley A, Karon S, Zimmerman D, Caudry D, et al. Nursing home capabilities and decisions to hospitalize: A survey of medical directors and directors of nursing. Journal of the American Geriatrics Society. 2006;54:458–465. doi: 10.1111/j.1532-5415.2005.00620.x. [DOI] [PubMed] [Google Scholar]
- Carter MW, Porell FW. Variations in hospitalization rates among nursing home residents: The role of facility and market attributes. Gerontologist. 2003;43:175–191. doi: 10.1093/geront/43.2.175. [DOI] [PubMed] [Google Scholar]
- Castle N. Advance directives in nursing homes: Resident and facility characteristics. Omega: Journal of Death and Dying. 1997;34:321–332. doi: 10.2190/ykjv-wuxm-efvf-x1tn. [DOI] [PubMed] [Google Scholar]
- Castle N, Mor V. Hospitalization of nursing home residents: A review of the literature. Medical Care Research and Review. 1996;53:123–148. doi: 10.1177/107755879605300201. [DOI] [PubMed] [Google Scholar]
- Christopher M. Benchmarks to improve end of life care. Kansas City, MO: Midwest Bioethics Center; 2000. [Google Scholar]
- Dillman D. Mail and telephone surveys: The total design method. New York: Wiley; 1978. [Google Scholar]
- Donabedian A. Evaluating the quality of medical care. Milbank Memorial Fund Quarterly. 1966;44:166–203. [PubMed] [Google Scholar]
- Dubois M, Bravo G, Charpentier M. Which residential care facilities are delivering inadequate care? A simple case-finding questionnaire. Canadian Journal of Aging. 2001;20:339–355. [Google Scholar]
- Dy S, Lynn J. Palliative care/end of life measures. Background paper. In: Committee on Redesigning Health Insurance Performance Measures, editor. Performance measurement. Accelerating improvement. Washington, DC: National Academies Press; 2006. pp. 249–274. [Google Scholar]
- Ersek M, Grant M, Kraybill B. Enhancing end-of-life care in nursing homes: Palliative Care Educational Resource Team (PERT) Program. Journal of Palliative Medicine. 2005;8:556–566. doi: 10.1089/jpm.2005.8.556. [DOI] [PubMed] [Google Scholar]
- Ersek M, Kraybill B, Hansberry J. Assessing the educational needs and concerns of nursing home staff regarding end-of-life care. Journal of Gerontological Nursing. 2000;26:16–26. doi: 10.3928/0098-9134-20001001-05. [DOI] [PubMed] [Google Scholar]
- Ersek M, Wilson S. The challenges and opportunities in providing end-of-life care in nursing homes. Journal of Palliative Medicine. 2003;6:45–57. doi: 10.1089/10966210360510118. [DOI] [PubMed] [Google Scholar]
- Forbes S, Bern-Klug M, Gessert C. End-of-life decision making for nursing home residents with dementia. Journal of Nursing Scholarship. 2000;32:251–258. doi: 10.1111/j.1547-5069.2000.00251.x. [DOI] [PubMed] [Google Scholar]
- Forbes-Thompson S, Gessert C. End of life in nursing homes: Connections between structure, process, and outcomes. Journal of Palliative Medicine. 2005;8:545–555. doi: 10.1089/jpm.2005.8.545. [DOI] [PubMed] [Google Scholar]
- Froggatt K, Payne S. A survey of end-of-life care in care homes: Issues of definition and practice. Health and Social Care in the Community. 2006;14:341–348. doi: 10.1111/j.1365-2524.2006.00628.x. [DOI] [PubMed] [Google Scholar]
- Ghiselli FE, Campbell JP, Zedeck S. Measurement theory for the social sciences. San Francisco: Freeman; 1981. [Google Scholar]
- Hill T, Ginsburg M, Citko J, Cadogan M. Improving end-of-life care in nursing facilities: The community state partnership to improve end-of-life care—California. Journal of Palliative Medicine. 2005;8:300–312. doi: 10.1089/jpm.2005.8.300. [DOI] [PubMed] [Google Scholar]
- Hosay C. Compliance with patients’ end-of-life wishes by nursing homes in New York City with conscience policies. Omega: Journal of Death and Dying. 2002;44:57–76. doi: 10.2190/rc21-29wg-qtce-2ny1. [DOI] [PubMed] [Google Scholar]
- Hyer K, Johnson C, Harman J, Mehra S. Staffing mandates matter: Florida nursing home provider response to financial incentives to increase nurse staffing. 2007. Retrieved February 22, 2009, from http://www.academyhealth.org/2007/tuesday/oceanic5/hyer.ppt#392,8, Staffing Mandates Matter: Florida Nursing Home Provider Response to Financial Incentives to Increase Nurse Staffing. [Google Scholar]
- Jenq G, Guo Z, Drickamer M, Marottoli R, Reid C. Timing in the communication of pain among nursing home residents, nursing staff, and clinicians. Archives of Internal Medicine. 2004;164:1508–1512. doi: 10.1001/archinte.164.14.1508. [DOI] [PubMed] [Google Scholar]
- Jones B, Nackerud L, Boyle D. Differential utilization of hospice services in nursing homes. Hospice Journal. 1997;12:41–57. doi: 10.1080/0742-969x.1997.11882868. [DOI] [PubMed] [Google Scholar]
- Keay TJ, Alexander C, McNally K, Crusse E, Eger RE. Nursing home physician educational intervention improves end-of-life outcomes. Journal of Palliative Medicine. 2003;6:205–213. doi: 10.1089/109662103764978452. [DOI] [PubMed] [Google Scholar]
- Kyriacou C, Nidetz A. Performance-based palliative care in the nursing home: Closing the gap between “knowing” and “practicing”. Journal of Palliative Medicine. 2002;5:757–758. doi: 10.1089/109662102320880651. [DOI] [PubMed] [Google Scholar]
- McAuley W, Buchanan R, Travis S, Wang S, Kim M. Recent trends in advance directives at nursing home admission and one year after admission. Gerontologist. 2006;46:377–381. doi: 10.1093/geront/46.3.377. [DOI] [PubMed] [Google Scholar]
- Miller S, Gozalo P, Mor V. Hospice enrollment and hospitalization of dying nursing home patients. American Journal of Medicine. 2001;111:38–44. doi: 10.1016/s0002-9343(01)00747-1. [DOI] [PubMed] [Google Scholar]
- Miller S, Mor V, Teno J. Hospice enrollment and pain assessment and management in nursing homes. Journal of Pain and Symptom Management. 2003;26:791–799. doi: 10.1016/s0885-3924(03)00284-7. [DOI] [PubMed] [Google Scholar]
- Miller S, Mor V, Wu N, Gozalo P, Lapane K. Does receipt of hospice care in nursing homes improve the management of pain at the end of life? Journal of the American Geriatrics Society. 2002;50:507–515. doi: 10.1046/j.1532-5415.2002.50118.x. [DOI] [PubMed] [Google Scholar]
- Miller S, Teno J, Mor V. Hospice and palliative care in nursing homes. Clinics in Geriatric Medicine. 2004;20:717–734. doi: 10.1016/j.cger.2004.07.005. [DOI] [PubMed] [Google Scholar]
- Mitchell S, Teno J, Roy J, Kabumoto G, Mor V. Clinical and organizational factors associated with feeding tube use among nursing home residents with advanced cognitive impairment. Journal of the American Medical Association. 2003;290:73–80. doi: 10.1001/jama.290.1.73. [DOI] [PubMed] [Google Scholar]
- Molloy DW, Guyatt GH, Russo R, Goeree R, O’Brien BJ, Bedard M, et al. Systematic implementation of an advance directive program in nursing homes: A randomized controlled trial. Journal of the American Medical Association. 2000;283:1437–1444. doi: 10.1001/jama.283.11.1437. [DOI] [PubMed] [Google Scholar]
- Mor V, Papandonatos G, Miller S. End-of-life hospitalization for African American and Non-Latino White nursing home residents: Variation by race and a facility's racial composition. Journal of Palliative Medicine. 2005;8:58–68. doi: 10.1089/jpm.2005.8.58. [DOI] [PubMed] [Google Scholar]
- National Hospice and Palliative Care Organization. Nursing home task force report. Alexandria, VA: NHPCO.; 1998. Report No. 714638. [Google Scholar]
- Parker Oliver D, Porock D, Zweig S. End-of-life care in U.S. nursing homes: A review of evidence. Journal of the American Medical Directors Association. 2004;5:147–155. doi: 10.1097/01.JAM.0000123063.79715.8E. [DOI] [PubMed] [Google Scholar]
- Remsburg R, Han B. Hospice and palliative/end of life care in nursing homes. Seattle, WA: 2006. Paper presented at the Academy Health Annual Meeting. [Google Scholar]
- Reynolds K, Henderson M, Schulman A, Hanson L. Needs of the dying in nursing homes. Journal of Palliative Medicine. 2002;5:895–901. doi: 10.1089/10966210260499087. [DOI] [PubMed] [Google Scholar]
- Rice K, Coleman E, Fish R, Levy C, Kutner J. Factors influencing models of end-of-life care in nursing homes: Results of a survey of nursing home administrators. Journal of Palliative Medicine. 2004;7:668–675. doi: 10.1089/jpm.2004.7.668. [DOI] [PubMed] [Google Scholar]
- Schnelle J, Mukamel DB, Sato H, Chang J. Study of California's new Medi-Cal reimbursement system for nursing homes. (Rep. No. California Alliance For Nursing Home Reform) 2008 Unpublished report. [Google Scholar]
- Smith W, Kellerman A, Brown J. The impact of nursing home transfer policies at the end of life on a public acute care hospital. Journal of the American Geriatrics Society. 1995;43:1052–1057. doi: 10.1111/j.1532-5415.1995.tb05573.x. [DOI] [PubMed] [Google Scholar]
- Spector WD, Selden TM, Cohen JW. The impact of ownership type on nursing home outcomes. Health Economics. 1998;7:639–653. doi: 10.1002/(sici)1099-1050(1998110)7:7<639::aid-hec373>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- Stewart A, Teno J, Donals M, Patrick D, Lynn J. The concept of quality of life of dying persons in the context of health care. Journal of Pain and Symptom Management. 1999;17:93–108. doi: 10.1016/s0885-3924(98)00131-6. [DOI] [PubMed] [Google Scholar]
- Strumpf N, Tuch H, Stillman D, Parrish P, Morrison N. Implementing palliative care in the nursing home. Annals of Long-Term Care. 2004;12:35–41. [Google Scholar]
- Teno JM, Clarridge BR, Casey V, Welch LC, Wetle T, Shield R, et al. Family perspectives on end of life care at the last place of care. Journal of the American Medical Association. 2004;291:88–93. doi: 10.1001/jama.291.1.88. [DOI] [PubMed] [Google Scholar]
- Thompson G, Chochinov H. Methodological challenges in measuring quality care at the end of life in the long-term care environment. Journal of Pain and Symptom Management. 2006;32:378–391. doi: 10.1016/j.jpainsymman.2006.05.014. [DOI] [PubMed] [Google Scholar]
- Troyer J, McAuley W. Environmental contexts of ultimate decisions: Why white nursing home residents are twice as likely as African American residents to have an advance directive. Journal of Gerontology: Social Sciences. 2006;61B:S194–S202. doi: 10.1093/geronb/61.4.s194. [DOI] [PubMed] [Google Scholar]
- Weitzen S, Teno J, Fennell M, Mor V. Factors associated with site of death: A national study of where people die. Medical Care. 2003;41:323–335. doi: 10.1097/01.MLR.0000044913.37084.27. [DOI] [PubMed] [Google Scholar]
- Yabroff K, Mandelblatt J, Ingham J. The quality of medical care at the end-of-life in the USA: Existing barriers and examples of process and outcomes measures. Palliative Medicine. 2004;18:202–216. doi: 10.1191/0269216304pm880oa. [DOI] [PubMed] [Google Scholar]
- Zinn JS, Mor V. Organizational structure and the delivery of primary care to older Americans. Health Services Research. 1998;33:354–380. [PMC free article] [PubMed] [Google Scholar]