Abstract
Mechanisms that may allow circulating monocytes to persist as CD4 T cells diminish in HIV-1 infection have not been investigated. We have characterized steady-state gene expression signatures in circulating monocytes from HIV-infected subjects and have identified a stable antiapoptosis gene signature comprised of 38 genes associated with p53, CD40L, TNF, and MAPK signaling networks. The significance of this gene signature is indicated by our demonstration of cadmium chloride- or Fas ligand-induced apoptosis resistance in circulating monocytes in contrast to increasing apoptosis in CD4 T cells from the same infected subjects. As potential mechanisms in vivo, we show that monocyte CCR5 binding by HIV-1 virus or agonist chemokines serves as independent viral and host modulators resulting in increased monocyte apoptosis resistance in vitro. We also show evidence for concordance between circulating monocyte apoptosis-related gene expression in HIV-1 infection in vivo and available datasets following viral infection or envelope exposure in monocyte-derived macrophages in vitro. The identification of in vivo gene expression associated with monocyte resistance to apoptosis is of relevance to AIDS pathogenesis since it would contribute to: 1) maintaining viability of infection targets and long-term reservoirs of HIV-1 infection in the monocyte/macrophage populations, and 2) protecting a cell subset critical to host survival despite sustained high viral replication.
Monocytes/macrophages (M/M)3 bind HIV-1, are a target of HIV-1 infection, and they support continued virus replication (1, 2), which can be further enhanced by coinfections and immune activation (3). CD4 T cells, the other target of HIV-1, and the predominantly uninfected peripheral CD4 T cells (4) are known to decline over the course of HIV-1 disease as a consequence of both HIV-1 and bystander mechanisms of apoptosis induction (5–7). In contrast, the predominantly uninfected peripheral monocyte pool (8) does not diminish during steady-state viral replication (9, 10). HIV-1-infected tissue macrophages are proposed to serve as long-lived HIV-1 reservoirs (3). There is limited information on in vivo apoptosis gene expression and functional outcomes for M/M apoptosis response from HIV-1-infected persons. However, data from in vitro models of HIV-1 infection of monocyte-derived macrophages (MDM) have repeatedly shown a relationship between MDM persistence (11, 12) and antiapoptotic regulation in association with the expression of HIV-1 accessory proteins nef or tat (13–15). Indeed, our collective understanding of gene regulatory effects present during chronic HIV-1 infection in infected subjects has been defined largely by in vitro models of infection rather than by direct study of HIV-1-infected subjects (16).
Circulating monocytes in HIV-1 infection have been described as a distinct cell population in comparison to monocytes from uninfected subjects as reflected by their multiple differences in phenotype and function (17, 18). This disparity is further highlighted by the presence of productive infection in circulating monocytes from infected persons (infectious proviral DNA has been isolated (19, 20)) in contrast to monocytes from uninfected subjects that remain largely refractory to HIV-1 infection ex vivo until macrophage differentiation. Furthermore, in vivo and in vitro environments are well accepted to be distinct microenvironments such that modulation in vitro lacks a multitude of additional host (21) or microbial (22) regulatory factors that may contribute to overall in vivo regulation of circulating monocyte gene expression during steady-state viral replication in chronic HIV infection.
Here, we describe the identification of a stable antiapoptosis gene signature in association with multiple regulatory networks in circulating monocytes in HIV-1 infection together with a functional resistance to induced apoptosis. Our data provide an in vivo multigene antiapoptosis signature in monocytes from HIV-infected subjects in association with functional resistance to induced apoptosis in contrast to CD4 T cells from the same HIV-infected subjects showing greater apoptosis. We also show monocyte apoptosis resistance to be independently induced by chemokine or HIV-1 envelope ligation of CCR5, indicating a role for CCR5 tropic HIV-1 or immune activation in actively maintaining monocyte survival during chronic HIV-1 infection.
Materials and Methods
Donors, cell subset isolations, and viruses
Chronically HIV-seropositive viremic patients, with a mean age of 43 years and not on therapy, from the Jonathan Lax Immune Disorder Clinic (Philadelphia Field Initiation Group for HIV Trials) served as our donor population for microarray experiments and apoptosis-induction assays. For inclusion, CD4 T cell counts needed to be >200 cells/mm3 (mean of 460 cells/mm3) and viral load >10,000 copies/ml (mean of 32,000 copies/ml) (Table I). HIV donors were selected if asymptomatic with no clinical evidence of active comorbidity (from hematocrit, body temperature). Age-and gender-matched healthy HIV-1-seronegative donors from the Wistar Institute Blood Donor Program were included as control subjects. Institutional Review Board approval from the Wistar Institute and Philadelphia Field Initiation Group for HIV Trials (FIGHT) and informed consent from patients were obtained before blood donation. As with HIV-infected donors, uninfected donors with an abnormal temperature, abnormal hematocrit, or reporting any symptoms were excluded. Blood was processed within 2–3 h from drawing. All reagents used were selected for their low levels of endotoxin contamination. PBMCs were separated by Ficoll-Paque (Amersham Pharmacia Biotech) density gradient separation and monocytes were isolated by adherence enrichment or by negative selection following column purification (Miltenyi Biotec, catalog no. 130-091-155) per the manufacturer’s instructions. Adherent monocytes were detached from culture by use of cold media and pipetting (not scraping). Flow cytometry at isolation required a minimum of >90% of cell expression for CD3−CD14+ (BD Biosciences; anti-CD14, catalog no. 555399; anti-CD3, catalog no. 555340) with a mean purity of CD14+ monocyte preparations used in the study of 95% (±3%). The percentage distribution of total CD14 cells between 24 HIV-1 and 16 control subjects tested was found not to be different. Gene expression samples collected from adherent monocyte fractions were collected within 2 h of cell isolation by lysing samples in TRI reagent (Molecular Research Center) as described below, while all functional assays were performed in isolated monocytes subsequently cultured over 36 h in adherent or nonadherent (Teflon) conditions. For functional apoptosis experiments, 21 additional untreated viremic individuals meeting the same criteria and remaining asymptomatic (CD4 T cell counts >200 cells/mm3 (with a mean of 438 cells/mm3) and viral load >10,000 copies/ml (with a mean of 21,766 copies/ml)) served as donors. HIV-1 BAL and HIV-1 aldrithriol-2-inactivated (AT2) virus SF162 were obtained from the Center for AIDS Research viral cell core. M657 inhibitor (23, 24) was kindly provided by M. Miller (Merck). MIP-1α, MIP-1β, and RANTES were obtained commercially (R&D Systems, catalog nos. 270-LD, 271-BME, and 278-RN, respectively).
TABLE I.
HIV-1 conor characteristics for differential expression studya
| Donor ID | Experiment | CD4 Count (Cells/Cubic mm) | Viral Load RNA (Copies/ml) | Sex | Age (Years) |
|---|---|---|---|---|---|
| 1 | Microarray | 352 | 22,170 | F | 48 |
| 1ab | Repeat microarray | 333 | 100,550 | F | 49 |
| 2 | Microarray | 458 | 23,262 | M | 46 |
| 2ab | Repeat microarray | 435 | 18,196 | M | 46 |
| 3 | Microarray | 300 | 10,611 | M | 40 |
| 3ab | Repeat microarray | 201 | 44,650 | M | 41 |
| 4 | Microarray | 353 | 24,075 | M | 54 |
| 4ab | Repeat microarray | 408 | 36,561 | M | 55 |
| 5 | Microarray | 332 | 29,587 | F | 46 |
| 6 | Microarray | 306 | 3,283 | F | 55 |
| 7 | Microarray | 504 | 61,470 | M | 36 |
| 8 | Microarray | 201 | 56,643 | M | 35 |
| 9 | Microarray | 1128 | 9,810 | F | 35 |
| 10 | Microarray | 416 | 74,296 | M | 38 |
| 11 | Microarray | 896 | 18,088 | F | 39 |
| 12 | Microarray | 604 | 22,150 | F | 20 |
| 13 | Microarray | 168 | 61,432 | M | 33 |
| 14 | Protein assays | 525 | 3,104 | F | 40 |
| 15 | Protein assays | 264 | 30,640 | F | 43 |
| 16 | Protein assays | 701 | 32,168 | F | 42 |
| 17 | Protein assays | 290 | 24,849 | M | 54 |
| 18 | Protein assays | 266 | 24,795 | F | 52 |
| 19 | Protein assays | 293 | 14,832 | F | 52 |
| 20 | Protein assays | 203 | 65,329 | F | 42 |
Nos. 1–13 served as donors for microarray experiments; the four individuals resampled after 7 mo are indicated as 1a, 2a, 3a, and 4a. Nos. 14–20 served as donors for protein assays. Donors were asymptomatic and had a history of viremia with >10,000 copies of virus/ml of plasma and were not on therapy. Viral load and CD4 T cell count measured on the day of blood drawing are indicated.
Second sample that was taken 7 mo after the initial samples.
RNA isolation, amplification, and hybridization
Total cellular RNA was extracted from individual enriched monocytes of 13 viremic HIV-1 and 12 control uninfected donors immediately following cell isolation using TRI reagent (Molecular Research Center). One microgram of total RNA was linearly amplified as previously described (25). [α-33P]dCTP-labeled cDNA probes (1.6 μg) were hybridized to cDNA arrays (manufactured at the Wistar Institute Microarray Facility) that contained 19,200 human probes representing ~14,000 known genes. All amplifications and hybridizations were performed in a single batch to minimize experimental variations. Arrays were subjected to high stringency washes, exposed to PhosphorImager screens (Packard Instruments) for 7–10 days, scanned in a Storm 820 PhosphorImager, and visualized using ImageQuant (Molecular Dynamics) (25). Using the identical approach, RNA was isolated individually from a subset of 4 viremic HIV-1 and 4 control donors selected from this initial group of 13 HIV-1 and 12 control donors after 7–9 mo (in the absence of change in subject characteristics) and hybridized to the same gene filters. The data from this second longitudinal subset served to determine/confirm gene modulation maintained over time.
Gene expression data
The microarray gene expression data discussed in this publication have been deposited in National Center for Biotechnology Information’s Gene Expression Omnibus (GEO) and are accessible through GEO Series accession no. GSE14542 (www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc).
Gene expression analysis and study criteria for stable expression
Image analysis was performed using ImaGene 4.0 (BioDiscovery). The radioactive signal intensity measurements obtained were then converted to the corresponding gene expression measurements referred to as normalized median density (NMD) by performing global normalization. The gene expression data obtained by global normalization were renormalized by performing quantile normalization with subsequent log2 transformation (QL2). The p values were determined using an unpaired heteroscedastic two-tail Student’s t test. Statistically significant genes between HIV-1 and control groups had a p value of ≤0.05 when using either NMD- or QL2-normalized data. The false discovery rate of the initial dataset was determined (26) to be 50% for genes with a p value of ≤0.05. Significant genes (p ≤ 0.05) were further selected by differential expression based on an absolute fold change (AFC) value of ≥2 between HIV-1 and control groups when using either NMD- or QL2-normalized data. Genes having a p value of ≤0.05 and an AFC of ≥2 selected in the original 13 HIV-1 subjects and 12 controls and that also exhibited the same expression trend (i.e., up-/down-regulation) in a second sample from 4 of the HIV-1 subjects and 4 of the controls taken seven months after the first samples were considered stably expressed.
Multidimensional scaling and cluster analysis
Multidimensional scaling was performed in two dimensions using nonmetric multidimensional scaling using a Pearson correlation-based distance metric, standard Guttman-Lingoes starting configuration, with a minimum and maximum number of iterations set respectively to 6 and 50. Clustering was performed using the Pearson correlation-based distance metric and Ward linkage. The expression measurements of each gene were converted to z scores by subtracting the mean value of the gene (computed across all samples being clustered) from its expression measurement and dividing the result by the corresponding SD, thus bringing the measurements of every gene to a common scale.
Quantitative real-time PCR and quantitative PCR normalization
PCR was performed in a 20-μl reaction volume in an Opticon IV (MJ Research). cDNA from 0.5 μg of amplified messenger RNA was prepared using SuperScript II as previously described (25). PCR product specificity was assessed by melting curve analysis. The expression levels for each gene relative to that in the reference sample, in our case, the Stratagene Universal Standard RNA, were derived from the fluorescence intensity measurements determined using LightCycler analysis software version 3.5. The housekeeping gene, β-actin (ACTB), was selected as an internal control for the amount of cDNA in each assay based on its constant expression observed in our microarray. The primer sequences are indicated in Table II.
TABLE II.
Primer sequences for apoptosis-related genes validated by real-time PCRa
| Gene Symbol | Forward Primer 5′–3′ | Reverse Primer 5′–3′ |
|---|---|---|
| MT-1G | CAA CTG CTC CTG TGC C | AGC TGC ACT TCT CCG A |
| MT-1H | CCT CTT CTC TTC TCG CTT GG | GCA AAT GAG TCG GAG TTG TAG |
| PAI2 | GCT TCC AGA TGA AAT TGC CGA | GCT TCA GTG CCC TCC TCA TTC |
| CCL2 | ATC AAT GCC CCA GTC ACC | AGT CTT CGG AGT TTG GG |
| IER3 | CCA GCA TCT CAA CTC CGT CTG T | CAC CCT AAA GGC GAC TTC AAG A |
| IL6 | CAA TCT GGA TTC AAT GAG GAG AC | CTC TGG CTT GTT CCT CAC TAC TC |
| MBD4 | CAC ATC TCT CCA GTC TGC | CGA CGT AAA GCC TTT AAG AA |
| HIVEP1 | GCA CAC ATT CCA GGT CTC CA | TGA GTT CAG GCT TGG GCT T |
| p21 | TTA GCA GCG GAA CAA GGA GT | CAG TAC AGG GTG TGG TCC CT |
| SIVA | ACA TGG CAA AAC CCT GTC TC | TCT TCT CGA AGA CCT CCT GC |
| CD153 | CTC CTG GAG ACA CAG CC | GGT GCT TGT ATC TAT GTA CT |
| PPBP | GGT TGT CTT TAT ACA CAT GCA G | ATG AGC CTC AGA CTT GAT AC |
| SELL | 5′CTC ATC ATG GGT TGG ATT AG | CTG CAA GTG ACA TCT CTT T |
| BIGM103 | AGT GTG GTA TCT CTA CAG G | CAA GGC TTG TCG AGT G |
| CCL20 | CTG CTT TGA TGT CAG TGC TGC | TCA CCC AAG TCT GTT TTG G |
| LPL | CCG AGA GTG AGA ACA TCC CAT TCA | CCT TTC TGC AAA TGA GAC ACT TTC TC |
Gene symbols and forward and reverse primer sequences for differentially expressed genes that were validated by real-time PCR are indicated.
Apoptosis induction and caspase-3 assay
Intracellular caspase-3 staining was performed in human cells using the protocol BD Cytofix/Cytoperm permeabilization kit provided by BD Biosciences (catalog no. 554714). After incubation in the presence or absence of 20 μM CdCl2 (Sigma-Aldrich, catalog no. 202908), an established apoptosis inducer (27–35), for 20 h, or with 100 ng/ml FasL (Sigma-Aldrich, catalog no. F0427) for 6 h, a million cells were stained with surface Abs purchased from BD Biosciences (CD14 for monocytes), Lineage cocktail (anti-CD56, catalog no. 555516; anti-CD3, catalog no. 555340; CD19, catalog no. 555413; and CD20, catalog no. 555623), and HLA-DR (catalog no. 340549) for Lin−DR+ myeloid cells and CD4 (catalog no. 555349) and CD3 for CD4 T cells. 7-Aminoactinomycin D (7-AAD; BD Biosciences, catalog no. 559925) was used for dead cell exclusion. Cells were incubated for 30 min at 4°C for cell subset phenotyping. Cells were then fixed/permeabilized and human cells were stained with intracellular anti-active caspase-3 FITC Ab (BD Biosciences, catalog no. 559341) for 30 min at 4°C and measured for active caspase-3 expression on a FACSCalibur flow cytometer. The Abs were titrated to determine the appropriate saturating concentrations. These concentrations were in the range of 0.5–1 μg/million cells for all Abs used. Isotype-matched mAbs were used in each staining experiment to determine gates for positive events in monocyte and lymphocyte subsets in all experiments. A total of 100,000 events were collected and analyzed in both control and HIV-1 samples. Before analysis, all samples were gated by forward and side scatter to exclude dead cells, and 7-AAD was additionally used to exclude dead cells. CD14+ caspase-3+7-AAD− cells (percentage of caspase-3) were used to measure CdCl2-induced apoptotic monocyte fractions, while CD14+ caspase-3−7-AAD− cells were used for analysis of live cell fractions (percentage of live cells). Surface annexin-V staining was performed for CD4 T cells using the apoptosis staining kit (Santa Cruz Biotechnology, catalog no. sc-4252 AK). After incubation in the presence or absence of CdCl2 (100 μM) for 20 h, a million cells were stained with surface Abs (CD4 and CD3 for CD4 T cells; from BD Biosciences) and incubated for 30 min at 4°C for cell subset phenotyping. Cells were washed once with buffer (1× PBS with 1% human serum). Five microliters (1 μg) 7-AAD and 1.5 μl (0.5 μg) annexin-V FITC were then added and incubated for 15 min, following which 300 μl of 1× annexin-V binding buffer (10× buffer provided with the kit and 1× made fresh on the day of use) was added and analyzed using an EPICS Elite (Beckman Coulter) flow cytometer. As above, a minimum of 100,000 positive events collected for CD4+CD3+ CD4 T cells in both control and HIV-1 samples were used for analysis. Analysis of acquired data was performed using FlowJo software (Tree Star). Before analysis, all samples were gated by forward and side scatter to exclude dead cells, and 7-AAD was additionally used to exclude dead cells before gating on CD3−CD14+ (monocytes), CD3−CD19−CD20−CD56−HLA-DR+ (myeloid cells), or CD3+ CD4+ (CD4 T cells) for data collection (100,000 events collected). Annexin-V+7-AAD−/dim cells were used for analysis of apoptotic cell fractions (percentage of annexin-V) and annexin-V−7-AAD− cells were used for analysis of live cell fractions (percentage of live cells).
Virus and chemokine binding/inhibition assays and CCR5 surface expression
Adherence-enriched monocytes from uninfected donors were cultured for 36 h in the presence of CCR5-tropic HIV-1 BAL (250 pg/ml) or aldrithriol-2-inactivated CCR5-tropic HIV-1 SF162 (AT2R5) (150 pg/ml) to study apoptosis modulation by HIV-1 binding to CCR5, or in the presence of MIP-1α (1 μM), MIP-1β (1 μM), and RANTES (1 μM) (R&D Systems) as natural CCR5 ligands (36), following which they were challenged with CdCl2 (20 μM) for 6 h. Intracellular active caspase-3 expression was measured by flow cytometry in the cultured monocytes using the same protocol that was used to measure caspase-3 in ex vivo cells described above. The CCR5 binding inhibitor M657 (1 nM) (24) was added 30 min before the 36-h AT2R5 SF162 and MIP-1β incubations to inhibit AT2R5 SF162 or MIP-1β binding to CCR5. Overall, monocytes were cultured in absence of any treatment for 42 h (binding experiments) or 42.5 h (binding/inhibition experiments) (labeled as C for control), or as untreated for 36 h followed by exposure to CdCl2 for 6 h (labeled as CdCl2) (binding experiments), or treated with M657 for 36.5 h followed by exposure to CdCl2 for 6 h (labeled as Inh + CdCl2) (binding/inhibition experiments). When indicated, CCR5 levels were measured in CD3−CD14+ cells using anti-CCR5 (BD Biosciences, catalog no. 555992).
Statistical analyses
For analysis of significance between unrelated groups, unpaired two-tailed Student’s t test were used if samples exhibited a normal distribution, a Wilcoxon two-sample test was used when samples exhibited non-normal distribution, and a two-tailed paired Student’s t test was used to compare paired treatment groups. For all tests, a p value of 0.05 or less was considered significant. All tests were performed using JMP (SAS Institute) statistical software.
Microarray datasets for comparative analyses
Microarray datasets (significant gene lists) for in vitro macrophage HIV-1 exposure and infection studies were kindly provided by Drs. A. S. Fauci, M. M. Goodenow and S. M. Wahl (37–39) and were compared with our in vivo significant gene lists to determine genes modulated in both in vivo and in vitro settings, as determined by identical LocusLink IDs.
Pathway analysis
We used three different approaches to explore the functional relationships among the genes identified: DAVID (Database for Annotation, Visualization, and Integrated Discovery; david.abcc.ncifcrf.gov/), the Ingenuity Pathway Analysis tool (www.ingenuity.com), and Pathway Miner tool version 1.1 (BioRag, Bio Resource for Array Genes, at www.biorag.org). We employed DAVID functional clustering and functional annotation clustering algorithms to obtain biologically enriched functional genes groups with reference to our background list containing 19,200 probes based on Fisher exact probability and kappa statistics to define similarity. The second approach conducted using the Ingenuity Pathway Analysis tool examined functional associations among genes and identified significant gene networks on the basis that they had more of the interconnected genes present than would be expected by chance. Overrepresented apoptosis/death-related genes that were functionally relevant in gene networks were identified. We also estimated significant (p ≤ 0.05) overrepresented pathways using the Pathway Miner tool version1.1 that uses a one-sided Fisher exact test to rank significant pathways based on their p values from each of the three different open source pathway resources: KEGG (Kyoto Encyclopedia of Genes and Genomes, www.genome.ad.jp), BioCarta (www.biocarta.com), and GenMAPP (Gene Map Annotator and Pathway Profiler, www.genmapp.org).
Results
Monocytes in chronically infected HIV-1 subjects are characterized by a stable antiapoptosis gene signature in vivo
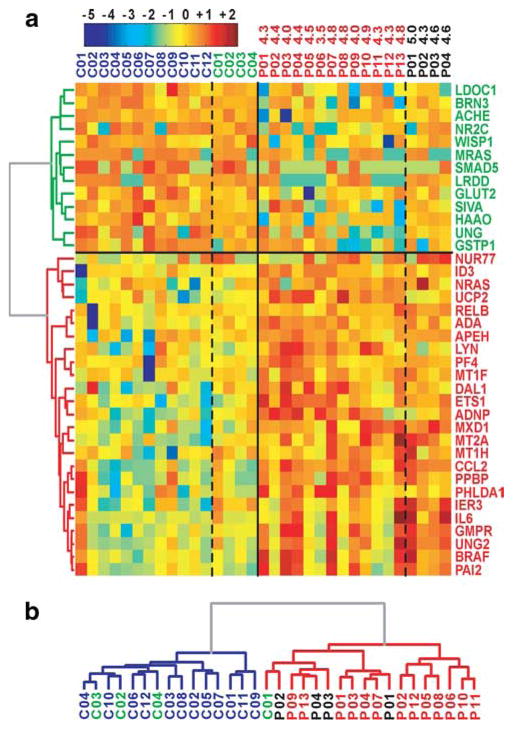
We first compared baseline gene expression between monocytes from HIV-1-infected persons in the absence of therapy (Table I lists subjects’ characteristics) and control donor monocytes. Significant and differentially expressed genes (p ≤ 0.05 and AFC ≥ 2) between HIV-1 and control donor monocytes were identified (supplemental Table I).4 Among the number of genes found to be differentially regulated, we focused on apoptosis-related genes that were significantly overrepresented by functional group clustering analysis DAVID and identified 58 genes associated with the modulation of apoptosis. Forty-one of these 58 (70.7%) apoptosis genes were validated by retesting a subset of the same donors >6 mo later (four control and four HIV-1 donors) and establishing these genes as maintaining the same direction of expression (i.e., up-regulation or down-regulation). Importantly, repeat donors had maintained similar viral load and CD4 counts and remained off antiretroviral therapy. Of these 41 genes, 38 genes have been directly reported to have distinct pro- or antiapoptotic function. Fig. 1a shows individual expression patterns of these 38 in vivo-validated genes in both the original 25 samples and the retested 8 repeat samples. Of interest, the 38 apoptosis-related gene signatures alone could segregate HIV-1 and uninfected groups with 97% accuracy (32 of 33) on the basis of their respective differential expression (Fig. 1b). The regulation of these 38 genes predicted for a greater resistance to apoptosis in circulating monocytes during HIV-1 infection, as 28 of the 38 genes (73.7%) were stably modulated to suggest increased monocyte survival (proapoptotic genes were down-regulated or antiapoptotic genes were up-regulated). The additional 3 genes accounting for the total gene number of 41 noted above (EDN1, LTB, and NME) are associated with both a pro- or antiapoptotic role and thus are excluded from Fig. 1a due to their uncertain role in apoptosis. Apart from in vivo validation of differential gene expression by repeat sampling, we also validated the expression of IL6, MT1G, MT1H, CCL2, IER3, PAI2, CD153, PPBP, SIVA, CCL4, and p21 within the individual 13 HIV-1 and 12 control donors’ samples by quantitative real-time PCR analysis and confirmed their differential expression (Table III). Analysis of major gene regulation pathways associated with this group of 38 stably and differentially expressed genes using Ingenuity Pathway Analysis and Pathway Miner identified four dominant pathways linking most of the genes: 1) p53 modulation (SIVA, p21, LDOC1, and LRDD), 2) TNF signaling (IL6, RELB, CCL2, UCP2, IER3, PAI2, and ADNP), 3) CD40L/CD40L signaling (MTs and CD153, a proapoptotic gene expressed by activated monocytes (40)), and 4) MAPK signaling (including PAI2, BRAF, NRAS, and LYN).
FIGURE 1.
Stable antiapoptosis gene modulation in HIV-1 monocytes ex vivo. a, Tree view of 38 apoptosis genes exhibiting stable differential expression between HIV-1 (P) and control (C) donors. Gene symbols are shown for the 38 genes. Genes down-regulated in P are in green and genes up-regulated in P are in red. C01–C12 are in blue, C01–C04 repeats are in green, P01–P13 are in red, and P01–P04 repeats are in black. Log values for viral load in HIV-1 individuals are indicated. For visual enhancement, expression levels of each gene were converted to z scores. b, Cluster dendrogram of P and C samples for the 38 apoptosis-related genes exhibiting stable expression.
TABLE III.
Real-time PCR confirmation of differentially expressed apoptosis genesa
| Accession No. | Gene Symbol | Gene Name | p Value for Comparison of HIV-1-Infected Individuals vs Controls (Quantitative PCR) | Ratio of Signal between HIV-1-Infected Individuals and Controls |
|---|---|---|---|---|
| N98591 | IL6 | IL-6 | 0.0004 | 166.40 |
| W92812 | PPBP | Proplatelet basic protein (chemokine (C-X-C motif) ligand 7) | 0.0010 | 3.58 |
| AA425102 | CCL2 | Chemokine (C-C motif) ligand 2 | 0.0001 | 12.85 |
| NM_002984 | CCL4 | Chemokine (C-C motif) ligand 4 | 0.0050 | 5.99 |
| AA457705 | IER3 | Immediate early response 3 | 0.0071 | 3.06 |
| H77597 | MT1H | Metallothionein 1H | 0.0002 | 8.58 |
| H53340 | MT1G | Metallothionein 1G | 0.0008 | 5.09 |
| T49159 | PAI2 | Serine (or cysteine) proteinase inhibitor, clade B (OVA), member 2 | 0.0043 | 6.88 |
| W02699 | CD153 | CD30L | 0.0004 | 0.38 |
| AA167728 | SIVA | CD27-binding (Siva) protein | 0.0180 | 0.48 |
| AI952615 | p21 | CDKN1A/Waf1/Cip1/Sdi1 | 0.0220 | 1.54 |
Differentially expressed apoptosis genes validated by real-time PCR are shown. The accessions, gene symbols, gene names, p values, and fold ratios for apoptosis genes differentially expressed between HIV-1 and control monocytes (all but CCL4 and p21 were also identified as significant by microarray analysis) were confirmed for significance by real-time PCR analysis and are indicated.
Evidence for concordance between in vivo monocyte apoptosis gene signature and in vitro gene regulation by HIV-1 infection or HIV-1 binding in MDMs
As in vivo steady-state gene expression represents the summation of chronic modulation by host and viral factors, we sought to determine the relationship between our circulating monocyte apoptosis signature and gene expression results obtained from models of in vitro HIV-1 infection and/or viral binding. We compared our in vivo monocyte gene signature with three independent available microarray data sets (37–39) from in vitro studies of gene modulation in MDMs infected with R5 HIV-1 or acutely stimulated with R5 HIV-1 gp120. Of the 38 stable apoptosis-related genes in vivo, 34 were available for comparison in these independent microarray-based studies and 1 gene was further independently reported as regulated by HIV-1 infection in vitro (41, 42). Overall, 21 of the 34 apoptosis-related in vivo genes analyzed were also found to be differentially expressed in monocyte/MDM within in vitro cultures exposed to/infected with HIV-1 (Table IV). Differentially expressed apoptosis genes that were identified to be similarly regulated both in vitro and in vivo included p53 network-associated (p21), TNF network-associated (IER3 and CCL2), and ERK/MAPK network-associated genes, including genes induced by CCR5 signaling (LYN and NRAS) (11, 12, 14, 15, 39). Taken together, this comparative analysis identified surprisingly strong similarities in acute viral-induced regulation as reported in vitro with long-term steady-state regulation of monocytes in vivo indicating that direct viral exposure (or products from infected cells) may have a strong influence on circulating monocyte gene expression despite the fact that monocytes in circulation remain largely uninfected.
TABLE IV.
21 Stable apoptosis genes in vivo are previously reported in HIV-1-exposed/infected M/Ma
| Accession No. | Gene Symbol | Gene Name | Reference to Previous HIV-1 Report(s) |
|---|---|---|---|
| N63940 | ACHE | Acetylcholinesterase (YT blood group) | (38) |
| AA683578 | ADA | Adenosine deaminase | (38) |
| AA455941 | APEH | N-acylaminoacyl-peptide hydrolase | (38) |
| AA425102 | CCL2 | Chemokine (C-C motif) ligand 2 | (18, 37–39, 77) |
| AA101971 | ETS1 | V-ets erythroblastosis virus E26 oncogene homolog 1 (avian) | (38) |
| AA410375 | GMPR | Guanosine monophosphate reductase | (38) |
| H50114 | GRIN2C | Glutamate receptor, ionotropic, N-methyl-D-aspartate 2C | (38) |
| T80846 | HAAO | 3-Hydroxyanthranilate-3,4-dioxygenase | (38) |
| AA457705 | IER3 | Immediate early response 3 | (39) |
| AI870374 | LDOC1 | Leucine zipper, down-regulated in cancer 1 | (38) |
| R83837 | LYN | V-yes-1 Yamaguchi sarcoma viral-related oncogene homolog | (24, 39) |
| H86558 | MAD | MAX dimerization protein 1 | (38) |
| NM_012219 | MRAS | Muscle RAS oncogene homolog | (38) |
| AA872383 | MT1E | Metallothionein 1E (functional) | (38) |
| N55459 | MT1F | Metallothionein 1F (functional) | (38) |
| H77597 | MT1H | Metallothionein 1H | (38) |
| AA446246 | NRAS | Neuroblastoma RAS viral (v-ras) oncogene homolog | (39) |
| AI952615 | p21 | CDKN1A/Waf1/Cip1/Sdi1 | (39) |
| AA258001 | RELB | V-rel reticuloendotheliosis viral oncogene homolog B, nuclear factor of κ light polypeptide gene enhancer in B cells 3 (avian) | (38) |
| AI473336 | WISP1 | WNT1 inducible signaling pathway protein 1 | (37) |
| AA425900 | UNG2 | Uracil-DNA glycosylase 2 | (41, 42) |
Indicated are the accession numbers, gene symbols, and gene names for 21 genes from the stable apoptosis signature that we identify in in vivo HIV-1 monocytes that have also been previously reported as modulated in in vitro macrophages by HIV-1. The references for previous studies that have reported HIV-1-associated modulation of these genes are additionally provided.
HIV-1 monocytes exhibit resistance to apoptosis induction ex vivo
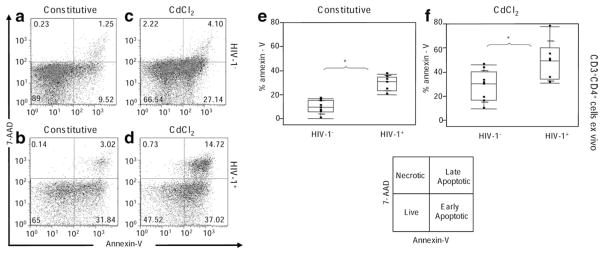
To investigate if circulating monocytes in chronic HIV-1 infection exhibit differential apoptosis resistance when compared with CD4 T cells, we measured expression of molecules indicative of apoptosis (active caspase-3, annexin V) after gating on CD3−CD14+ (monocytes), CD3−CD19−CD20−CD56−HLA-DR+ (myeloid cells), or CD3+CD4+ (CD4 T cells) positive events in independent HIV-1 donors (subjects satisfying similar criteria for viremia, CD4 T cell count, and no therapy status as in earlier gene expression cohorts) as compared with uninfected donors after ex vivo stimulation with CdCl2 or FasL. CdCl2 stimulation was used due to its well-established apoptosis-inducing potential by activation of multiple apoptosis pathways, including activation of p38MAPK/ERK, p53, Fas, oxidative stress, and mitochondrial membrane potential disruption (27–35). Consistent with previous reports of constitutive and induced apoptosis in CD3+ CD4+ T cells from HIV-1 subjects (43), we found significantly higher constitutive (p < 0.0001) and CdCl2-induced (p = 0.0194) apoptosis in CD3+ CD4+ T cells from HIV-1 donors as compared with controls, based on annexin V expression (Fig. 2) and by live cell subset percentage (p < 0.0001 for constitutive live cells and p = 0.0176 for CdCl2-induced live cells, results not shown).
FIGURE 2.
HIV-1+ monocytes exhibit resistance to apoptosis in contrast to HIV-1+ CD4 T cells ex vivo. HIV-1 CD4 T cells exhibit greater constitutive apoptosis (b) than do control (HIV-1−) CD4 T cells (a). HIV-1 CD4 T cells exhibit greater CdCl2-induced apoptosis (d) than do control (HIV-1−) CD4 T cells (c). Results represent the median ± SD for percentage of annexin V CD4 T cells in the unstimulated (e) and CdCl2-stimulated (f) conditions in eight control donors and six viremic donors.*, p ≤ 0.05.
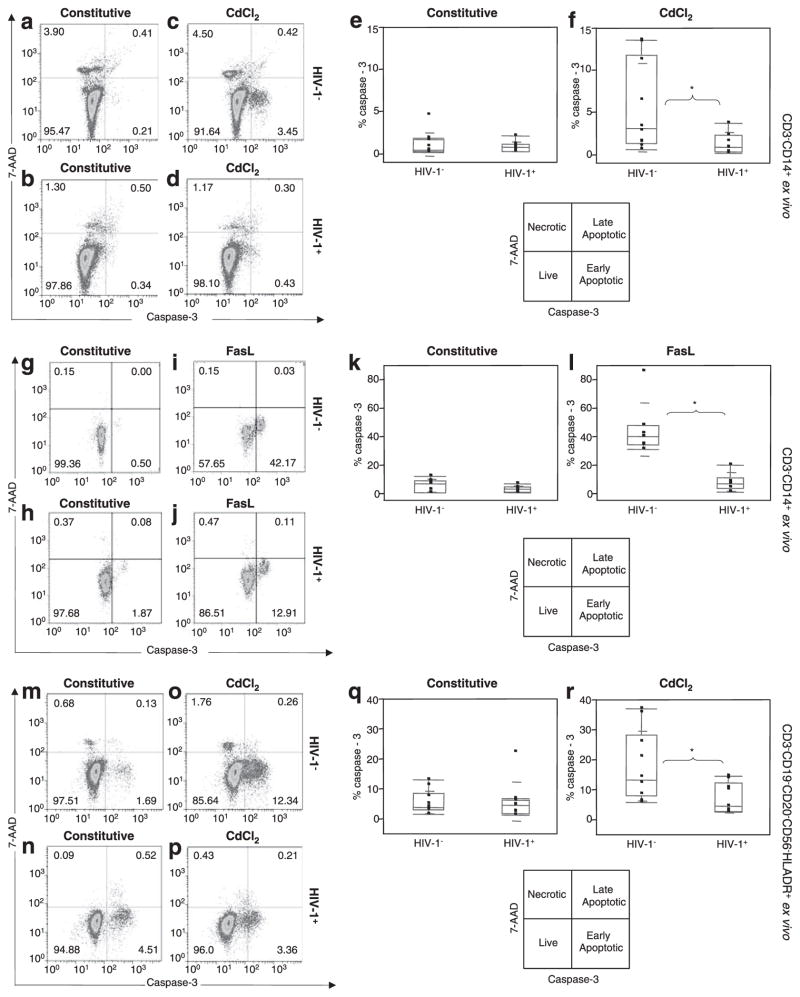
We next examined apoptotic induction in monocytes from HIV-1-infected subjects as compared with uninfected subjects by measuring acute induction of active/cleaved caspase-3 expression. We used the active/cleaved caspase-3 assay in the monocyte experiments, as the annexin V Ab was found to cross-react with monocyte membrane annexin V isoforms. CdCl2 has been shown to induce caspase-3-dependent apoptosis induction in M/Ms (27). While no difference in constitutive caspase-3 levels was detected between control and HIV-1 monocytes (Fig. 3, a and b), we observed a significant resistance to CdCl2-induced apoptosis in CD3−CD14+ monocytes from HIV-1 subjects based on caspase-3 expression (p = 0.041, Fig. 3a–f) and live cell percentages (p = 0.0058, results not shown). We also confirmed higher apoptosis resistance (p = 0.03) in HIV-1 vs control monocytes (Fig. 3g–l) to FasL, a more physiologically relevant apoptosis inducer that is known to be elevated in plasma (serum) of viremic subjects (44–46). Furthermore, using a gating approach independent of CD14 but inclusive of all myeloid subsets, we show a similar significant resistance to CdCl2-induced apoptosis in Lin− (CD3−, CD56−, CD19−, CD20−) HLA-DR+ cells (which include both CD14- and CD16-expressing monocyte pools and dendritic cells) from the same HIV-1 donors on the basis of caspase-3 (p = 0.02) and live cell subsets (p = 0.044, results not shown) (Fig. 3m–r). Taken together, these observations show apoptosis resistance of monocytes in the presence of active HIV-1 replication in vivo and provide a functional correlate to the presence of a steady-state predicted antiapoptosis gene regulation in HIV-1 monocytes as described earlier.
FIGURE 3.
HIV-1+ monocytes exhibit resistance to apoptosis in contrast to HIV-1+ CD4 T cells ex vivo. In contrast to CD4 T cells, no difference was found in constitutive apoptosis between control (HIV-1−) (a) and HIV-1+ (b) monocytes, but a higher CdCl2-induced apoptosis was found in HIV-1− (c) than in HIV-1+ (d) monocytes. Results represent the median ± SD for percentage of caspase-3 monocytes for constitutive (e) and for CdCl2-stimulated (f) conditions in 10 control and 9 viremic HIV-1 donors. Following FasL stimulation, no difference was found in constitutive apoptosis between control (HIV-1−) (g) and HIV-1+ (h) monocytes, but a higher FasL-induced apoptosis was noted in HIV-1− (i) than in HIV-1+ (j) monocytes. Results represent the median ± SD for percentage of caspase-3 monocytes for constitutive (k) and for FasL-stimulated (l) conditions in seven control and six viremic HIV-1 donors. Independent confirmation of results further show no difference in constitutive apoptosis between control (HIV-1−) (m) and HIV-1+ (n) myeloid cells but a higher CdCl2-induced apoptosis in control (HIV-1−) (o) than in HIV-1+ (p) myeloid cells. Results represent the median ± SD for percentage of caspase-3 in constitutive (q) and in CdCl2-stimulated (r) conditions for 10 controls and 9 viremic HIV-1 donors. *, p ≤ 0.05.
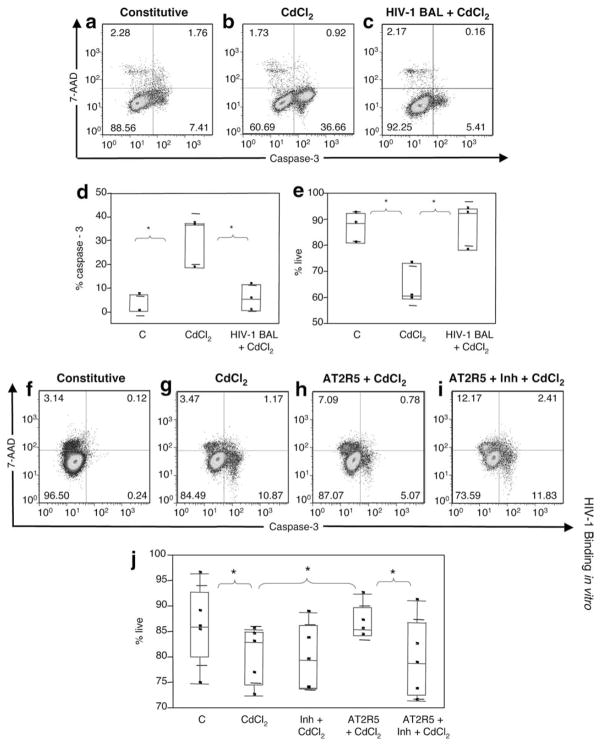
HIV-1 interactions with CCR5 confer monocyte apoptosis resistance in vitro
Recent reports in murine models have shown that interactions with macrophage/neuron CCR5 confer apoptosis resistance to these cells by inducing ERK/MAPK and PI3K/AKT survival pathways (47, 48). Given the central role of CCR5 in mediating R5 tropic HIV-1 binding to monocytes and our observed modulation of genes associated with CCR5 and ERK/MAPK signaling (LYN, CCL4, and CCL4L1) (24, 36, 49), we tested whether CCR5 engagement of uninfected monocytes via HIV-1 envelope for 36 h before CdCl2 challenge could confer apoptosis resistance in cultured monocytes. First, we tested exposure to infectious HIV-1 BAL; this led to a significant decrease in CdCl2-induced apoptosis (p = 0.012 for CdCl2-induced caspase-3 and p = 0.014 for CdCl2-induced live cells) based on caspase-3 expression (p = 0.022) and live cell percentages (p = 0.023) (Fig. 4a– e). We also corroborated these observations by demonstrating a decrease in CdCl2-induced DNA fragmentation in cultured CD14+ monocytes pre-treated with infectious HIV-1 BAL vs in monocytes not treated with virus, using the TUNEL assay (data not shown).
FIGURE 4.
HIV-1 binding via CCR5 induces resistance in in vitro MDM cultures. Constitutive apoptosis in MDMs is shown in a and f. MDM binding by R5 tropic virus mediates MDM apoptosis resistance in vitro. CdCl2 induces cultured monocyte apoptosis (b) that is decreased upon preincubation with infectious HIV-1 BAL (c). Results represent the median ± SD for percentage of caspase-3 (d) and percentage of live (e) cells of three donors that were untreated (C), treated with CdCl2, and preincubated with HIV-1 BAL (HIV-1 BAL ± CdCl2). CdCl2 induces cultured monocyte apoptosis (g) that is decreased upon preincubation with noninfectious AT2R5 (h). CCR5 binding inhibitor M657 reverses AT2R5-mediated protection (i). Results represent the median ± SD for percentage of live (j) cells in 5 donors that were untreated (C), treated with CdCl2, preincubated with M657 (Inh + CdCl2), preincubated with AT2R5 (AT2R5 + CdCl2), and preincubated with M657 and AT2R5 (AT2R5 + Inh + CdCl2).*, p ≤ 0.05.
Next, we tested exposure to noninfectious enriched inactivated viral particles. Using aldrithriol-2-inactivated R5 HIV-1 SF162 particles (AT2R5, which can bind but not infect), we once again observed a significant decrease (p = 0.02) in CdCl2-induced caspase-3 expression (Fig. 4f–j) and a significant increase in live cell percentages (p = 0.022) in cells exposed to AT2R5 (Fig. 4h). Importantly, we establish a direct role for HIV-1 interactions with CCR5 in mediating MDM apoptosis resistance based on the reversal of AT2R5-mediated apoptosis resistance in the presence of a CCR5 binding inhibitor, M657 (p = 0.028) (Fig. 4, i and j). The effect of the inhibitor is further validated by a significant increase in CCR5 expression in MDMs incubated with M657 as compared with MDMs unexposed to M657 (p = 0.001, results not shown).
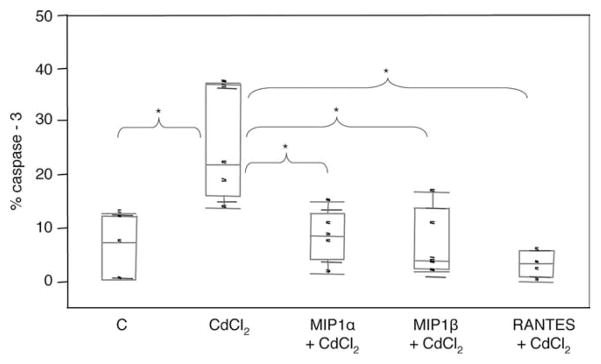
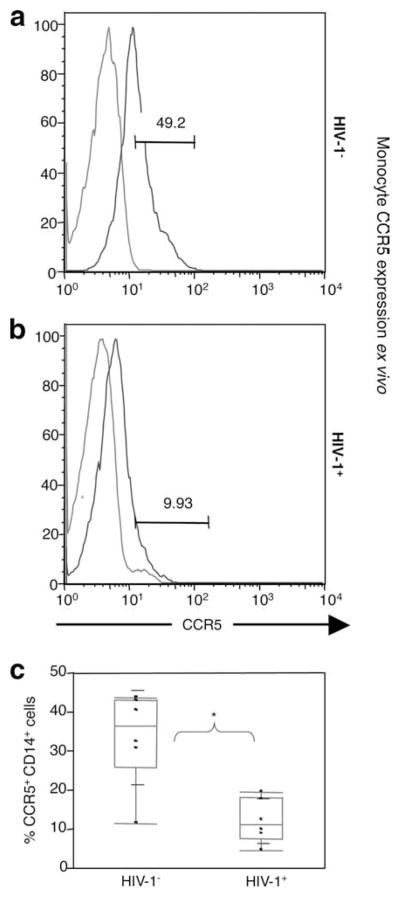
CCR5-binding chemokines confer monocyte apoptosis resistance in vitro
We next tested cultured monocyte apoptosis modulation by exposure to the CCR5-binding chemokines MIP-1α, MIP-1β, and RANTES before CdCl2 challenge. Similar to our observations on viral interactions with CCR5, we observed a significant reduction in CdCl2-induced MDM apoptosis (p = 0.039 for CdCl2-induced caspase-3 and p = 0.015 for CdCl2-induced live cells) based on caspase-3 expression and live cell subsets after exposure to MIP-1α (p = 0.015 for CdCl2-induced caspase-3 and p = 0.029 for CdCl2-induced live cells), MIP-1β (p = 0.028 for CdCl2-induced caspase-3 and p = 0.018 for CdCl2-induced live cells), or RANTES (p = 0.007 for CdCl2-induced caspase-3 and p = 0.021 for CdCl2-induced live cells) (Fig. 5). Notably, monocytes from viremic donors demonstrated significantly lower surface CCR5 expression when compared against monocytes from controls (p = 0.0034), consistent with a role for ongoing in vivo CCR5 signaling by either virus/chemokine binding (Fig. 6). To test whether differential levels of CCR5-binding chemokines also corresponded with differences between groups, constitutive soluble CCR5-binding chemokine (RANTES, MIP-1α, MIP-1β) levels between HIV-1 viremic asymptomatic and uninfected subjects were measured in plasma (n = 20 for each group). Results showed no clear difference between groups (not shown), leading us to conclude that while chemokines are present, chemokine levels alone do not segregate our study groups.
FIGURE 5.
HIV-1 binding via CCR5 induces resistance in in vitro MDM cultures. MDM binding by CCR5 chemokines mediates MDM apoptosis resistance in vitro. Indicated is the median ± SD for percentage of caspase-3 cells in five donors that were untreated (C), treated with CdCl2, and preincubated with MIP-1α (MIP1α + CdCl2) MIP1β (MIP-1β + CdCl2), and RANTES (RANTES + CdCl2).*, p ≤ 0.05.
FIGURE 6.
Lower ex vivo surface CCR5 expression in HIV-1 monocytes versus control monocytes. Surface CCR5 expression was significantly lower in HIV-1 monocytes vs controls as indicated by lower CCR5 mean fluorescence intensity in HIV-1 monocytes (a) vs control monocytes (b) and lower percentage of CCR5+CD14+ monocytes in HIV-1 vs control groups (c). A total of six HIV-1 and six control donors were tested for CCR5 expression.*, p ≤ 0.05.
Discussion
Herein we provide the first evidence for the presence of a steady-state, stable antiapoptosis gene expression signature in circulating monocytes in chronic HIV-1 infection in association with monocyte resistance to apoptosis induction. Similarities between monocyte apoptotic gene modulation in vivo with in vitro gene regulation, the down-regulation of CCR5 expression in circulating HIV-1 monocytes in vivo, and our data showing M/M apoptosis resistance following CCR5 binding support a prominent role for viral envelope-mediated interactions and/or chemokine expression in the maintenance of steady-state gene expression in vivo. Indeed, as <1% of circulating monocytes are directly infected in vivo (8) and monocytes express CCR5 at levels able to bind and signal but not support infection (50), our data support a leading role for HIV-1 binding or soluble factors in regulating monocyte gene expression in vivo. Finally, gene pathway analysis, in conjunction with a review of published data on the identified apoptotic gene signature in our study, strongly indicate in vivo regulation of p53, CD40, and TNF networks as steady-state features of monocyte apoptosis modulation during chronic HIV infection. Our observations in infected human subjects now complement studies on HIV-1-infected MDMs in vitro, where HIV-1 accessory proteins (such as nef or tat) or envelope-dependent induction of M-CSF have been shown to also contribute to apoptosis modulation within infected cell cultures (13–15, 51). Indeed, our circulating monocyte data strongly suggest that apoptosis modulation of monocytes/macrophages is broader than just within infected cells alone. Noteworthy is the strong impact of chronic HIV infection (virus- and host immune activation-mediated effects) on monocyte gene expression, clearly acting to segregate HIV and control samples on the basis of expression of all genes tested (14,000) in our study as a wider definition of a difference than the differentially expressed genes or apoptosis-related genes emphasized in our report. This reflects the overall higher homogeneity in composite gene expression in HIV-infected vs control subjects’ monocytes as a consequence of active HIV replication in vivo (supplemental Fig. 1, see summary multidimensional scaling plot).
An antiapoptotic gene modulation in monocytes from HIV-1-infected subjects as a result of viral envelope binding stands in direct contrast to reports of apoptotic rate in CD4 T cells where HIV-1 envelope binding to CCR5 (p53, MAPK) and host-initiated immune activation pathways (TNF, FAS) are shown to preferentially lead to CD4 T cell death (6, 52–55). Indeed, differential monocyte apoptosis may underlie previously reported observations indicating lower monocyte turnover in the presence of HIV-1 replication in vivo in contrast to a higher CD4 T cell turnover (9). HIV-1 monocyte resistance to FasL (Fig. 3) in addition to CdCl2 may also bear on the persistence of the circulating monocyte pool during periods of chronic circulating CD4 T cell loss known to be associated with the presence of viral replication and elevated circulating levels of proapoptotic mediators such as soluble FasL, TNF, and TRAIL (44–46, 56–58). Supporting this interpretation is the recent observation of in vitro HIV-1-infected macrophage resistance to TRAIL-induced apoptosis (51).
As a mechanism of action, we provide evidence for HIV-1 envelope interaction with CCR5 as being able to trigger resistance to apoptosis in monocyte cultures (Fig. 4). Furthermore, since the CCR5 agonistic chemokines MIP-1α, MIP-1β, and RANTES are known to be produced by activated T cells and are elevated in HIV-1-infected individuals (59–61), our observation showing chemokine/CCR5 binding mediated apoptosis resistance (Fig. 5) establishes the presence of redundant host mechanisms for monocyte protection in the presence of either viral replication or immune activation. Our observation of significantly lower CCR5 expression in monocytes from HIV-infected subjects when compared with controls is consistent with greater engagement and down-regulation of CCR5 in vivo (Fig. 6).
Our data showing a lack of difference in circulating levels of CCR5-binding chemokines RANTES, MIP-1α and MIP-1β between HIV-1 and control groups is also consistent with our cohort not being at end-stage disease (i.e., <100 CD4 with >100,000 copies/ml viral load), as previous studies have shown decreasing levels of serum β-chemokines in HIV-1-infected individuals to correlate with severity of disease progression (59, 60, 62–64). It remains to be tested whether unchanged expression levels of serum β-chemokines we report reflect the preferential recruitment of asymptomatic subjects at mid-stage disease (in absence of comorbidities). It is also possible that quantification of intracellular chemokine levels in monocytes may be required to detect expression differentials specific to this subset.
We also find support for our interpretation of virus/chemokine CCR5 binding mediating monocyte apoptosis resistance in the overrepresentation of in vivo genes otherwise already associated with outcomes of CCR5 ligation by HIV-1 gp120 or chemokines in vitro such as p38/ERK/MAPK pathway genes (including LYN, NRAS, BRAF, PAI2) (24, 37, 47, 48, 65). Of interest, LYN, which is known to activate ERK/MAPK following in vitro HIV-1 gp120 or MIP-1β interaction with macrophage CCR5 (24), was noted in our results to be up-regulated in circulating monocytes in vivo. A role for p53 in inhibiting apoptosis in infected MDMs in vitro has been suggested by the reported p53-mediated expression of genes (including p21) that inhibit DNA damage-induced apoptosis and facilitate viral replication (38, 39). p21, which is known to contribute to inhibiting monocyte apoptosis (66), and p53 (67, 68) in vitro were noted to be up-regulated in vivo, raising p53 regulation/expression as a potential mechanism of apoptosis regulation in circulating monocytes during HIV-1 infection. Furthermore, our results showing the in vivo up-regulation of the MT gene family (which is modulated by CD40L signaling and IL-6), known to confer apoptotic resistance to a variety of stress inducers (e.g., reactive oxygen species, heavy metals, including cadmium (32), and DNA damage) and to inhibit p53-mediated apoptosis (69), further support our interpretation of p53 expression and associated modulation of gene expression as one target mechanism of action consistent with our data.
Although we interpret CCR5 engagement to be a dominant mechanism of regulation, note that many genes in the 38 group reported herein have not been associated with CCR5, suggesting that HIV-1 monocytes in vivo are likely subject to more than a single mechanism of regulation. Our results may also be limited by the fact that our array does not include all apoptosis genes characterized to date, and thus we cannot exclude regulation of additional genes associated with apoptosis to the steady-state signature described here. We have addressed this limitation via gene network analysis, which further corroborates the presence of a coordinated multigene/redundant expression profile by identifying overrepresentation of distinct and multiple apoptosis gene pathways in monocytes from HIV-1-infected subjects. Another limitation of our data is that we do not establish whether the circulating virus in each of the subjects studied is CCR5 or CXCR4 tropic other than to expect, based on natural history studies and isolates predominant in midstage disease, that R5 isolates are highly likely to be overrepresented in our cohort. Indeed, CCR5 coreceptors utilizing macrophage tropic HIV-1 are the predominant strains for viral transmission in vivo and predominate until the detection of X4 strains (utilizing CXCR4 as coreceptor), the emergence of which correlates with rapid progression to an AIDS-defining illness or a CD4 T cell count of <200 cells/μl (70–73). Future work will need to determine whether CXCR4 signaling (via CXCR4 tropic viruses) can also confer resistance to apoptosis in monocytes/macrophages independently of immune activation. Taken together, we conclude that in chronic HIV-1 infection, the convergence of multiple and complementary gene pathways as a result of virus binding (LYN up-regulation via CCR5 signaling), host factors (CD153, CD40L, TNF and IL-6), regulation of monocyte signaling (MAPK), and transcription (NF-κB, ETS1, and p53) act in concert to impart apoptosis resistance in monocytes from HIV-infected subjects. Additional studies will be needed to determine the degree of redundancy between individual molecules or pathways in accounting for the functional apoptosis regulation present in monocytes from HIV-1 subjects.
While a driving concern of our approach remains the potential for contamination by nonmonocyte cells in our gene expression studies and functional analyses, multiple reasons make this concern minimal when evaluating our body of evidence that: 1) gene expression data or antiapoptosis responses were confirmed in both adherent monocyte cultures and in nonadherent cultures (isolation for nonadherent cells by negative selection columns) with yields >98% viable CD14+ monocytes in each method; contributions of minor nonmonocyte populations that differed from sample to sample would not have attained a p value that was considered significant in the microarray studies presented (p < 0.05 and fold change >2); 2) our apoptosis induction data on lymphocytes and gene expression on isolated lymphocytes in the literature do not resemble data on monocytes; lymphocytes in fact undergo apoptosis, an opposite response compared with monocytes, as shown herein; 3) we observed concordance between genes reported here in circulating monocytes and gene expression profiles described for isolated macrophages infected with HIV-1 in vitro or exposed to viral envelope independently; and 4) all flow cytometry data on apoptosis were obtained by CD14 staining, thereby restricting events to monocytes.
That CCR5 agonistic chemokines mediate monocyte apoptosis resistance appears paradoxical in that the host’s natural anti-HIV-1 immune response via activated CD8 T cells, CD4 T cells, and macrophages (all of which secrete MIP-1α, MIP-1β, and RANTES) at the time of infection or chronic disease (i.e., lymphoid tissue (3, 74)) may also act to directly benefit HIV-1 by promoting monocyte survival, thereby actively preserving targets for new infection as well as promoting a host-mediated “cellular sanctuary” site for viral reservoirs. The predicted survival of infected M/M and bystander M/M targets for infection in the face of active HIV-1 replication and death of CD4 T cells may thus bear on the selection for CCR5-dependent (R5) virus at acute infection and throughout the disease (75). It remains to be determined whether the addition of CCR5 inhibitors to current regimens that are unable to fully suppress viral replication even if reaching “undetectable” status (76) could act to further restrict pathogenic mechanisms for viral persistence by preventing access to long-lived infected M/M pools, thereby not only treating viral replication but also persistence mechanisms. Our initial analysis of monocyte apoptosis induction following regular antiretroviral therapy currently under investigation (i.e., in absence of CCR5 inhibitors) indicates a partial retention of monocyte resistance to apoptosis that, if confirmed, may reflect ongoing CCR5 engagement by the host independently of antiretroviral therapy-induced viral suppression.
Importantly, in contrast to CD4 T cells, M/M populations directly contribute to maintenance of the physiology of multiple systems such as immune function (dendritic cells, resident macrophage populations), hemopoiesis (RBC production), bone metabolism, and thymic function, as also reflected by the absence of any viable myeloid knockout mice to date. HIV-1 envelope may have adapted to exploit the effects of CCR5 on macrophage subsets during active replication, thereby prolonging the host’s virus transmission window, as monocytes are critical to sustain core physiological host functions during an otherwise active and progressive infection. It will be important to determine whether similar apoptotic gene modulation in M/M populations is present in other chronic human infections where microbial persistence is intricately associated with chronic immune activation and macrophage infection/persistence.
Supplementary Material
Acknowledgments
We thank D. Davis, Philadelphia Field Initiation Group for HIV Trials staff, C. Gallo, L. Alila, L. Gudipati, J. Faust, M. Farabaugh, and Shannon Southhall for their help with experiments; Drs. A. Fauci, M. Goodenow, and S. Wahl for access to in vitro HIV-1 MDM microarray data; Drs. D. Weissman, J. Hoxie, I. Sanne, and S. Gordon for critical feedback; and M. Miller (Merck) for M657.
Footnotes
This study was supported by National Institutes of Health Grant AI047760, the Philadelphia Foundation, and Wistar funds from the Commonwealth Universal Research Enhancement Program, Pennsylvania Department of Health.
Abbreviations used in this paper: M/M, monocyte/macrophage; AFC, absolute fold change; C, control subject sample; MDM, monocyte-derived macrophages; P, HIV-1 patient subject sample; 7-AAD, 7-aminoactinomycin D.
The online version of this article contains supplemental material.
Disclosures
The authors have no financial conflicts of interest.
References
- 1.Gartner S, Markovits P, Markovitz DM, Kaplan MH, Gallo RC, Popovic M. The role of mononuclear phagocytes in HTLV-III/LAV infection. Science. 1986;233:215–219. doi: 10.1126/science.3014648. [DOI] [PubMed] [Google Scholar]
- 2.Delobel P, Sandres-Saune K, Cazabat M, L’Faqihi FE, Aquilina C, Obadia M, Pasquier C, Marchou B, Massip P, Izopet J. Persistence of distinct HIV-1 populations in blood monocytes and naive and memory CD4 T cells during prolonged suppressive HAART. AIDS. 2005;19:1739–1750. doi: 10.1097/01.aids.0000183125.93958.26. [DOI] [PubMed] [Google Scholar]
- 3.Orenstein JM, Fox C, Wahl SM. Macrophages as a source of HIV during opportunistic infections. Science. 1997;276:1857–1861. doi: 10.1126/science.276.5320.1857. [DOI] [PubMed] [Google Scholar]
- 4.Brenchley JM, Hill BJ, Ambrozak DR, Price DA, Guenaga FJ, Casazza JP, Kuruppu J, Yazdani J, Migueles SA, Connors M, et al. T-cell subsets that harbor human immunodeficiency virus (HIV) in vivo: implications for HIV pathogenesis. J Virol. 2004;78:1160–1168. doi: 10.1128/JVI.78.3.1160-1168.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guadalupe M, Reay E, Sankaran S, Prindiville T, Flamm J, McNeil A, Dandekar S. Severe CD4+ T-cell depletion in gut lymphoid tissue during primary human immunodeficiency virus type 1 infection and substantial delay in restoration following highly active antiretroviral therapy. J Virol. 2003;77:11708–11717. doi: 10.1128/JVI.77.21.11708-11717.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ho DD, Neumann AU, Perelson AS, Chen W, Leonard JM, Markowitz M. Rapid turnover of plasma virions and CD4 lymphocytes in HIV-1 infection. Nature. 1995;373:123–126. doi: 10.1038/373123a0. [DOI] [PubMed] [Google Scholar]
- 7.Badley AD, Pilon AA, Landay A, Lynch DH. Mechanisms of HIV-associated lymphocyte apoptosis. Blood. 2000;96:2951–2964. [PubMed] [Google Scholar]
- 8.McElrath MJ, Pruett JE, Cohn ZA. Mononuclear phagocytes of blood and bone marrow: comparative roles as viral reservoirs in human immunodeficiency virus type 1 infections. Proc Natl Acad Sci USA. 1989;86:675–679. doi: 10.1073/pnas.86.2.675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kovacs JA, Lempicki RA, Sidorov IA, Adelsberger JW, Herpin B, Metcalf JA, Sereti I, Polis MA, Davey RT, Tavel J, et al. Identification of dynamically distinct subpopulations of T lymphocytes that are differentially affected by HIV. J Exp Med. 2001;194:1731–1741. doi: 10.1084/jem.194.12.1731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mohri H, Perelson AS, Tung K, Ribeiro RM, Ramratnam B, Markowitz M, Kost R, Hurley A, Weinberger L, Cesar D, et al. Increased turnover of T lymphocytes in HIV-1 infection and its reduction by antiretroviral therapy. J Exp Med. 2001;194:1277–1287. doi: 10.1084/jem.194.9.1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salahuddin SZ, Rose RM, Groopman JE, Markham PD, Gallo RC. Human T lymphotropic virus type III infection of human alveolar macrophages. Blood. 1986;68:281–284. [PubMed] [Google Scholar]
- 12.Guillemard E, Jacquemot C, Aillet F, Schmitt N, Barre-Sinoussi F, Israel N. Human immunodeficiency virus 1 favors the persistence of infection by activating macrophages through TNF. Virology. 2004;329:371–380. doi: 10.1016/j.virol.2004.08.030. [DOI] [PubMed] [Google Scholar]
- 13.Zheng L, Yang Y, Guocai L, Pauza CD, Salvato MS. HIV Tat protein increases Bcl-2 expression in monocytes which inhibits monocyte apoptosis induced by tumor necrosis factor-alpha-related apoptosis-induced ligand. Intervirology. 2007;50:224–228. doi: 10.1159/000100565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Olivetta E, Federico M. HIV-1 Nef protects human-monocyte-derived macrophages from HIV-1-induced apoptosis. Exp Cell Res. 2006;312:890–900. doi: 10.1016/j.yexcr.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 15.Zhang M, Li X, Pang X, Ding L, Wood O, Clouse KA, Hewlett I, Dayton AI. Bcl-2 upregulation by HIV-1 Tat during infection of primary human macrophages in culture. J Biomed Sci. 2002;9:133–139. doi: 10.1007/BF02256024. [DOI] [PubMed] [Google Scholar]
- 16.Giri MS, Nebozhyn M, Showe L, Montaner LJ. Microarray data on gene modulation by HIV-1 in immune cells: 2000–2006. J Leukocyte Biol. 2006;80:1031–1043. doi: 10.1189/jlb.0306157. [DOI] [PubMed] [Google Scholar]
- 17.Crowe S, Zhu T, Muller WA. The contribution of monocyte infection and trafficking to viral persistence, and maintenance of the viral reservoir in HIV infection. J Leukocyte Biol. 2003;74:635–641. doi: 10.1189/jlb.0503204. [DOI] [PubMed] [Google Scholar]
- 18.Pulliam L, Sun B, Rempel H. Invasive chronic inflammatory monocyte phenotype in subjects with high HIV-1 viral load. J Neuroimmunol. 2004;157:93–98. doi: 10.1016/j.jneuroim.2004.08.039. [DOI] [PubMed] [Google Scholar]
- 19.Gorry PR, Sonza S, Kedzierska K, Crowe SM. Isolation of human immunodeficiency virus type 1 from peripheral blood monocytes. Methods Mol Biol. 2005;304:25–33. doi: 10.1385/1-59259-907-9:025. [DOI] [PubMed] [Google Scholar]
- 20.Xu Y, Zhu H, Wilcox CK, van’t Wout A, Andrus T, Llewellyn N, Stamatatos L, Mullins JI, Corey L, Zhu T. Blood monocytes harbor HIV type 1 strains with diversified phenotypes including macrophage-specific CCR5 virus. J Infect Dis. 2008;197:309–318. doi: 10.1086/524847. [DOI] [PubMed] [Google Scholar]
- 21.Tilton JC, Johnson AJ, Luskin MR, Manion MM, Yang J, Adelsberger JW, Lempicki RA, Hallahan CW, McLaughlin M, Mican JM, et al. Diminished production of monocyte proinflammatory cytokines during human immunodeficiency virus viremia is mediated by type I interferons. J Virol. 2006;80:11486–11497. doi: 10.1128/JVI.00324-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brenchley JM, Price DA, Schacker TW, Asher TE, Silvestri G, Rao S, Kazzaz Z, Bornstein E, Lambotte O, Altmann D, et al. Microbial translocation is a cause of systemic immune activation in chronic HIV infection. Nat Med. 2006;12:1365–1371. doi: 10.1038/nm1511. [DOI] [PubMed] [Google Scholar]
- 23.Kim D, Wang L, Caldwell CG, Chen P, Finke PE, Oates B, MacCoss M, Mills SG, Malkowitz L, Gould SL, et al. Discovery of human CCR5 antagonists containing hydantoins for the treatment of HIV-1 infection. Bioorg Med Chem Lett. 2001;11:3099–3102. doi: 10.1016/s0960-894x(01)00654-0. [DOI] [PubMed] [Google Scholar]
- 24.Tomkowicz B, Lee C, Ravyn V, Cheung R, Ptasznik A, Collman R. The Src kinase Lyn is required for CCR5 signaling in response to MIP-1β and R5 HIV-1 gp120 in human macrophages. Blood. 2006;108:1145–1150. doi: 10.1182/blood-2005-12-012815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kari L, Loboda A, Nebozhyn M, Rook AH, Vonderheid EC, Nichols C, Virok D, Chang C, Horng WH, Johnston J, et al. Classification and prediction of survival in patients with the leukemic phase of cutaneous T cell lymphoma. J Exp Med. 2003;197:1477–1488. doi: 10.1084/jem.20021726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Storey JD, Tibshirani R. Statistical significance for genomewide studies. Proc Natl Acad Sci USA. 2003;100:9440–9445. doi: 10.1073/pnas.1530509100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim J, Sharma RP. Cadmium-induced apoptosis in murine macrophages is antagonized by antioxidants and caspase inhibitors. J Toxicol Environ Health A. 2006;69:1181–1201. doi: 10.1080/15287390600631144. [DOI] [PubMed] [Google Scholar]
- 28.Miguel BG, Rodriguez ME, Aller P, Martinez AM, Mata F. Regulation of cadmium-induced apoptosis by PKCdelta in U937 human promonocytic cells. Biochim Biophys Acta. 2005;1743:215–222. doi: 10.1016/j.bbamcr.2004.10.011. [DOI] [PubMed] [Google Scholar]
- 29.Li M, Kondo T, Zhao QL, Li FJ, Tanabe K, Arai Y, Zhou ZC, Kasuya M. Apoptosis induced by cadmium in human lymphoma U937 cells through Ca2+-calpain and caspase-mitochondria-dependent pathways. J Biol Chem. 2000;275:39702–39709. doi: 10.1074/jbc.M007369200. [DOI] [PubMed] [Google Scholar]
- 30.Oh SH, Lim SC. A rapid and transient ROS generation by cadmium triggers apoptosis via caspase-dependent pathway in HepG2 cells and this is inhibited through N-acetylcysteine-mediated catalase upregulation. Toxicol Appl Pharmacol. 2006;212:212–223. doi: 10.1016/j.taap.2005.07.018. [DOI] [PubMed] [Google Scholar]
- 31.Lag M, Westly S, Lerstad T, Bjornsrud C, Refsnes M, Schwarze PE. Cadmium-induced apoptosis of primary epithelial lung cells: involvement of Bax and p53, but not of oxidative stress. Cell Biol Toxicol. 2002;18:29–42. doi: 10.1023/a:1014467112463. [DOI] [PubMed] [Google Scholar]
- 32.Achanzar WE, Achanzar KB, Lewis JG, Webber MM, Waalkes MP. Cadmium induces c-myc, p53, and c-jun expression in normal human prostate epithelial cells as a prelude to apoptosis. Toxicol Appl Pharmacol. 2000;164:291–300. doi: 10.1006/taap.1999.8907. [DOI] [PubMed] [Google Scholar]
- 33.Galan A, Garcia-Bermejo ML, Troyano A, Vilaboa NE, de Blas E, Kazanietz MG, Aller P. Stimulation of p38 mitogen-activated protein kinase is an early regulatory event for the cadmium-induced apoptosis in human promonocytic cells. J Biol Chem. 2000;275:11418–11424. doi: 10.1074/jbc.275.15.11418. [DOI] [PubMed] [Google Scholar]
- 34.Lemarie A, Lagadic-Gossmann D, Morzadec C, Allain N, Fardel O, Vernhet L. Cadmium induces caspase-independent apoptosis in liver Hep3B cells: role for calcium in signaling oxidative stress-related impairment of mitochondria and relocation of endonuclease G and apoptosis-inducing factor. Free Radical Biol Med. 2004;36:1517–1531. doi: 10.1016/j.freeradbiomed.2004.03.020. [DOI] [PubMed] [Google Scholar]
- 35.Sancho P, Fernandez C, Yuste VJ, Amran D, Ramos AM, de Blas E, Susin SA, Aller P. Regulation of apoptosis/necrosis execution in cadmium-treated human promonocytic cells under different forms of oxidative stress. Apoptosis. 2006;11:673–686. doi: 10.1007/s10495-006-5879-3. [DOI] [PubMed] [Google Scholar]
- 36.Raport CJ, Gosling J, Schweickart VL, Gray PW, Charo IF. Molecular cloning and functional characterization of a novel human CC chemokine receptor (CCR5) for RANTES, MIP-1β, and MIP-1α. J Biol Chem. 1996;271:17161–17166. doi: 10.1074/jbc.271.29.17161. [DOI] [PubMed] [Google Scholar]
- 37.Cicala C, Arthos J, Selig SM, Dennis G, Jr, Hosack DA, Van Ryk D, Spangler ML, Steenbeke TD, Khazanie P, Gupta N, et al. HIV envelope induces a cascade of cell signals in non-proliferating target cells that favor virus replication. Proc Natl Acad Sci USA. 2002;99:9380–9385. doi: 10.1073/pnas.142287999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Coberley CR, Kohler JJ, Brown JN, Oshier JT, Baker HV, Popp MP, Sleasman JW, Goodenow MM. Impact on genetic networks in human macrophages by a CCR5 strain of human immunodeficiency virus type 1. J Virol. 2004;78:11477–11486. doi: 10.1128/JVI.78.21.11477-11486.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vazquez N, Greenwell-Wild T, Marinos NJ, Swaim WD, Nares S, Ott DE, Schubert U, Henklein P, Orenstein JM, Sporn MB, Wahl SM. Human immunodeficiency virus type 1-induced macrophage gene expression includes the p21 gene, a target for viral regulation. J Virol. 2005;79:4479–4491. doi: 10.1128/JVI.79.7.4479-4491.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Epstein ML, Windebank KP, Burt AD, Thomas L, Cant AJ. CD30 expression by peripheral blood monocytes and hepatic macrophages in a child with miliary tuberculosis. J Clin Pathol. 1992;45:638–639. doi: 10.1136/jcp.45.7.638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bouhamdan M, Benichou S, Rey F, Navarro JM, Agostini I, Spire B, Camonis J, Slupphaug G, Vigne R, Benarous R, Sire J. Human immunodeficiency virus type 1 Vpr protein binds to the uracil DNA glycosylase DNA repair enzyme. J Virol. 1996;70:697–704. doi: 10.1128/jvi.70.2.697-704.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen R, Le Rouzic E, Kearney JA, Mansky LM, Benichou S. Vpr-mediated incorporation of UNG2 into HIV-1 particles is required to modulate the virus mutation rate and for replication in macrophages. J Biol Chem. 2004;279:28419–28425. doi: 10.1074/jbc.M403875200. [DOI] [PubMed] [Google Scholar]
- 43.Groux H, Torpier G, Monte D, Mouton Y, Capron A, Ameisen JC. Activation-induced death by apoptosis in CD4+ T cells from human immunodeficiency virus-infected asymptomatic individuals. J Exp Med. 1992;175:331–340. doi: 10.1084/jem.175.2.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bahr GM, Capron A, Dewulf J, Nagata S, Tanaka M, Bourez JM, Mouton Y. Elevated serum level of Fas ligand correlates with the asymptomatic stage of human immunodeficiency virus infection. Blood. 1997;90:896–898. [PubMed] [Google Scholar]
- 45.Kottilil S, Jackson JO, Reitano KN, O’Shea MA, Roby G, Lloyd M, Yang J, Hallahan CW, Rehm CA, Arthos J, et al. Innate immunity in HIV infection: enhanced susceptibility to CD95-mediated natural killer cell death and turnover induced by HIV viremia. J Acquired Immune Defic Syndr. 2007;46:151–159. doi: 10.1097/QAI.0b013e3180dc9909. [DOI] [PubMed] [Google Scholar]
- 46.Sabri F, De Milito A, Pirskanen R, Elovaara I, Hagberg L, Cinque P, Price R, Chiodi F. Elevated levels of soluble Fas and Fas ligand in cerebrospinal fluid of patients with AIDS dementia complex. J Neuroimmunol. 2001;114:197–206. doi: 10.1016/s0165-5728(00)00424-0. [DOI] [PubMed] [Google Scholar]
- 47.Kaul M, Ma Q, Medders KE, Desai MK, Lipton SA. HIV-1 coreceptors CCR5 and CXCR4 both mediate neuronal cell death but CCR5 paradoxically can also contribute to protection. Cell Death Differ. 2007;14:296–305. doi: 10.1038/sj.cdd.4402006. [DOI] [PubMed] [Google Scholar]
- 48.Tyner JW, Uchida O, Kajiwara N, Kim EY, Patel AC, O’Sullivan MP, Walter MJ, Schwendener RA, Cook DN, Danoff TM, Holtzman MJ. CCL5-CCR5 interaction provides antiapoptotic signals for macrophage survival during viral infection. Nat Med. 2005;11:1180–1187. doi: 10.1038/nm1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Howard OM, Turpin JA, Goldman R, Modi WS. Functional redundancy of the human CCL4 and CCL4L1 chemokine genes. Biochem Biophys Res Commun. 2004;320:927–931. doi: 10.1016/j.bbrc.2004.06.039. [DOI] [PubMed] [Google Scholar]
- 50.Tuttle DL, Harrison JK, Anders C, Sleasman JW, Goodenow MM. Expression of CCR5 increases during monocyte differentiation and directly mediates macrophage susceptibility to infection by human immunodeficiency virus type 1. J Virol. 1998;72:4962–4969. doi: 10.1128/jvi.72.6.4962-4969.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Swingler S, Mann AM, Zhou J, Swingler C, Stevenson M. Apoptotic killing of HIV-1-infected macrophages is subverted by the viral envelope glycoprotein. PLoS Pathog. 2007;3:1281–1290. doi: 10.1371/journal.ppat.0030134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Giorgi JV, Hultin LE, McKeating JA, Johnson TD, Owens B, Jacobson LP, Shih R, Lewis J, Wiley DJ, Phair JP, et al. Shorter survival in advanced human immunodeficiency virus type 1 infection is more closely associated with T lymphocyte activation than with plasma virus burden or virus chemokine coreceptor usage. J Infect Dis. 1999;179:859–870. doi: 10.1086/314660. [DOI] [PubMed] [Google Scholar]
- 53.Biard-Piechaczyk M, Robert-Hebmann V, Richard V, Roland J, Hipskind RA, Devaux C. Caspase-dependent apoptosis of cells expressing the chemokine receptor CXCR4 is induced by cell membrane-associated human immunodeficiency virus type 1 envelope glycoprotein (gp120) Virology. 2000;268:329–344. doi: 10.1006/viro.1999.0151. [DOI] [PubMed] [Google Scholar]
- 54.Algeciras A, Dockrell DH, Lynch DH, Paya CV. CD4 regulates susceptibility to Fas ligand- and tumor necrosis factor-mediated apoptosis. J Exp Med. 1998;187:711–720. doi: 10.1084/jem.187.5.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vlahakis SR, Algeciras-Schimnich A, Bou G, Heppelmann CJ, Villasis-Keever A, Collman RC, Paya CV. Chemokine-receptor activation by env determines the mechanism of death in HIV-infected and uninfected T lymphocytes. J Clin Invest. 2001;107:207–215. doi: 10.1172/JCI11109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Scott-Algara D, Vuillier F, Marasescu M, de Saint Martin J, Dighiero G. Serum levels of IL-2, IL-1 alpha, TNF-alpha, and soluble receptor of IL-2 in HIV-1-infected patients. AIDS Res Hum Retroviruses. 1991;7:381–386. doi: 10.1089/aid.1991.7.381. [DOI] [PubMed] [Google Scholar]
- 57.Aukrust P, Liabakk NB, Muller F, Lien E, Espevik T, Froland SS. Serum levels of tumor necrosis factor-alpha (TNF alpha) and soluble TNF receptors in human immunodeficiency virus type 1 infection: correlations to clinical, immunologic, and virologic parameters. J Infect Dis. 1994;169:420–424. doi: 10.1093/infdis/169.2.420. [DOI] [PubMed] [Google Scholar]
- 58.Herbeuval JP, Boasso A, Grivel JC, Hardy AW, Anderson SA, Dolan MJ, Chougnet C, Lifson JD, Shearer GM. TNF-related apoptosis-inducing ligand (TRAIL) in HIV-1-infected patients and its in vitro production by antigen-presenting cells. Blood. 2005;105:2458–2464. doi: 10.1182/blood-2004-08-3058. [DOI] [PubMed] [Google Scholar]
- 59.Betts MR, Nason MC, West SM, De Rosa SC, Migueles SA, Abraham J, Lederman MM, Benito JM, Goepfert PA, Connors M, et al. HIV nonprogressors preferentially maintain highly functional HIV-specific CD8+ T cells. Blood. 2006;107:4781–4789. doi: 10.1182/blood-2005-12-4818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Aukrust P, Muller F, Froland SS. Circulating levels of RANTES in human immunodeficiency virus type 1 infection: effect of potent antiretroviral therapy. J Infect Dis. 1998;177:1091–1096. doi: 10.1086/517402. [DOI] [PubMed] [Google Scholar]
- 61.Cocchi F, DeVico AL, Garzino-Demo A, Arya SK, Gallo RC, Lusso P. Identification of RANTES, MIP-1α, and MIP-1β as the major HIV-suppressive factors produced by CD8+ T cells. Science. 1995;270:1811–1815. doi: 10.1126/science.270.5243.1811. [DOI] [PubMed] [Google Scholar]
- 62.Lee B, Montaner LJ. Chemokine immunobiology in HIV-1 pathogenesis. J Leukocyte Biol. 1999;65:552–565. doi: 10.1002/jlb.65.5.552. [DOI] [PubMed] [Google Scholar]
- 63.Nilsson J, Kinloch-de-Loes S, Granath A, Sonnerborg A, Goh LE, Andersson J. Early immune activation in gut-associated and peripheral lymphoid tissue during acute HIV infection. AIDS. 2007;21:565–574. doi: 10.1097/QAD.0b013e3280117204. [DOI] [PubMed] [Google Scholar]
- 64.Ullum H, Cozzi Lepri A, Victor J, Aladdin H, Phillips AN, Gerstoft J, Skinhoj P, Pedersen BK. Production of β-chemokines in human immunodeficiency virus (HIV) infection: evidence that high levels of macrophage inflammatory protein-1β are associated with a decreased risk of HIV disease progression. J Infect Dis. 1998;177:331–336. doi: 10.1086/514192. [DOI] [PubMed] [Google Scholar]
- 65.Fantuzzi L, Canini I, Belardelli F, Gessani S. HIV-1 gp120 stimulates the production of β-chemokines in human peripheral blood monocytes through a CD4-independent mechanism. J Immunol. 2001;166:5381–5387. doi: 10.4049/jimmunol.166.9.5381. [DOI] [PubMed] [Google Scholar]
- 66.Asada M, Yamada T, Ichijo H, Delia D, Miyazono K, Fukumuro K, Mizutani S. Apoptosis inhibitory activity of cytoplasmic p21(Cip1/WAF1) in monocytic differentiation. EMBO J. 1999;18:1223–1234. doi: 10.1093/emboj/18.5.1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gorospe M, Cirielli C, Wang X, Seth P, Capogrossi MC, Holbrook NJ. p21(Waf1/Cip1) protects against p53-mediated apoptosis of human melanoma cells. Oncogene. 1997;14:929–935. doi: 10.1038/sj.onc.1200897. [DOI] [PubMed] [Google Scholar]
- 68.Polyak K, Waldman T, He TC, Kinzler KW, Vogelstein B. Genetic determinants of p53-induced apoptosis and growth arrest. Genes Dev. 1996;10:1945–1952. doi: 10.1101/gad.10.15.1945. [DOI] [PubMed] [Google Scholar]
- 69.Ostrakhovitch EA, Olsson PE, Jiang S, Cherian MG. Interaction of metallothionein with tumor suppressor p53 protein. FEBS Lett. 2006;580:1235–1238. doi: 10.1016/j.febslet.2006.01.036. [DOI] [PubMed] [Google Scholar]
- 70.Gorry PR, Bristol G, Zack JA, Ritola K, Swanstrom R, Birch CJ, Bell JE, Bannert N, Crawford K, Wang H, et al. Macrophage tropism of human immunodeficiency virus type 1 isolates from brain and lymphoid tissues predicts neurotropism independent of coreceptor specificity. J Virol. 2001;75:10073–10089. doi: 10.1128/JVI.75.21.10073-10089.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Schuitemaker H, Koot M, Kootstra NA, Dercksen MW, de Goede RE, van Steenwijk RP, Lange JM, Schattenkerk JK, Miedema F, Tersmette M. Biological phenotype of human immunodeficiency virus type 1 clones at different stages of infection: progression of disease is associated with a shift from monocytotropic to T-cell-tropic virus population. J Virol. 1992;66:1354–1360. doi: 10.1128/jvi.66.3.1354-1360.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Burger H, Hoover D. HIV-1 tropism, disease progression, and clinical management. J Infect Dis. 2008;198:1095–1097. doi: 10.1086/591624. [DOI] [PubMed] [Google Scholar]
- 73.Weiser B, Philpott S, Klimkait T, Burger H, Kitchen C, Burgisser P, Gorgievski M, Perrin L, Piffaretti JC, Ledergerber B. HIV-1 co-receptor usage and CXCR4-specific viral load predict clinical disease progression during combination antiretroviral therapy. AIDS. 2008;22:469–479. doi: 10.1097/QAD.0b013e3282f4196c. [DOI] [PubMed] [Google Scholar]
- 74.Igarashi T, Brown CR, Endo Y, Buckler-White A, Plishka R, Bischofberger N, Hirsch V, Martin MA. Macrophage are the principal reservoir and sustain high virus loads in rhesus macaques after the depletion of CD4+ T cells by a highly pathogenic simian immunodeficiency virus/HIV type 1 chimera (SHIV): implications for HIV-1 infections of humans. Proc Natl Acad Sci USA. 2001;98:658–663. doi: 10.1073/pnas.021551798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Li S, Juarez J, Alali M, Dwyer D, Collman R, Cunningham A, Naif HM. Persistent CCR5 utilization and enhanced macrophage tropism by primary blood human immunodeficiency virus type 1 isolates from advanced stages of disease and comparison to tissue-derived isolates. J Virol. 1999;73:9741–9755. doi: 10.1128/jvi.73.12.9741-9755.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fatkenheuer G, Pozniak AL, Johnson MA, Plettenberg A, Staszewski S, Hoepelman AI, Saag MS, Goebel FD, Rockstroh JK, Dezube BJ, et al. Efficacy of short-term monotherapy with maraviroc, a new CCR5 antagonist, in patients infected with HIV-1. Nat Med. 2005;11:1170–1172. doi: 10.1038/nm1319. [DOI] [PubMed] [Google Scholar]
- 77.Woelk CH, Ottones F, Plotkin CR, Du P, Royer CD, Rought SE, Lozach J, Sasik R, Kornbluth RS, Richman DD, Corbeil J. Interferon gene expression following HIV type 1 infection of monocyte-derived macrophages. AIDS Res Hum Retroviruses. 2004;20:1210–1222. doi: 10.1089/aid.2004.20.1210. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.