Abstract
Objective:
We examined latent classes of alcohol use among current drinkers ages 60 and older and explored risk factors associated with class.
Method:
We used a subsample of older current drinkers (≥60 years; n = 4,646) from the National Epidemiologic Survey on Alcohol and Related Conditions. Employing alcohol consumption and diagnostic indicators, latent class analysis was used to identify classes. We analyzed the associations between class membership and sociode-mographic, psychiatric, health, and mental health variables using multinomial and linear regression.
Results:
Latent class analysis identified three latent classes. Individuals in the low-risk drinker class (89.17%) displayed low endorsement of heavy episodic use, at-risk consumption, and alcohol abuse/dependence criteria. Individuals in the moderate-risk drinker class (9.65%) were more likely to exceed consumption guidelines, and those in the high-risk drinker class (1.17%) displayed high probabilities of both Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), criteria and risky alcohol consumption items. Female gender, older age, and African-American race were associated with decreased risk of being a moderate-risk drinker. Being the adult child of an alcoholic, being a previous smoker, and being a current smoker were associated with increased risk. Female gender, older age, and college education were associated with decreased odds of being a high-risk drinker. Having major depression, being the child of an alcoholic, and being a current smoker were associated with increased odds of being a high-risk drinker. Individuals classified in the high-risk drinker class had significantly lower self-rated mental and physical health than low-risk drinkers.
Conclusions:
A subpopulation of older drinkers may exceed consumption guidelines without DSM-defined alcohol-related problems. However, for some older drinkers, risky alcohol use is part of a larger pattern of health risks including current smoking, major depression, and alcohol abuse/dependence history.
Alcohol misuse by older adults is an important public health concern with significant consequences. It is associated with poor mental health functioning (Blow et al., 2000), increased odds of suicide (Sorock et al., 2006; Waern, 2003), and increased risk of accidental and recurrent falls (Bell et al., 2000; Sorock et al., 2006). Although researchers have identified health benefits resulting from light to moderate drinking (Byles et al., 2006), at-risk or heavy drinking is associated with increased mortality (Moore et al., 2006). Because of its pattern of underdetection, alcohol problems in the elderly have been described as an "invisible epidemic" (Blow, 1998).
Although alcohol misuse is a significant problem, different indicators of problem use have led to varied estimates of its nature and depth among older adults. One common benchmark of alcohol misuse is the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV; American Psychiatric Association, 1994), Alcohol Abuse/ Dependence criteria. Consumption-based measures are an alternate approach to identifying alcohol-related risk in older adults. Alcohol consumption and DSM-IV problems represent two means of screening for alcohol-related problems in older adults.
Consumption-based guidelines
The Center for Substance Abuse Treatment (Blow, 1998) and the National Institute on Alcohol Abuse and Alcoholism (NIAAA; NIAAA 1995) have recommended that older men (≥65 years) consume no more than one standard drink per day with a maximum of two drinks on any one occasion, or seven drinks on average per week. The standards for older women are stricter—less than one drink per day and a maximum of four drinks per week. Further, consumption in a single session of five or more drinks for men and four or more for women constitutes another component of risky drinking. Recent population-based research has found that exceeding drinking guidelines is associated with increased risk of alcohol-use disorders, with particularly high risk among individuals exceeding daily consumption guidelines of five or more drinks for men and four or more drinks for women (Dawson et al., 2005), leading to calls for the inclusion of quantity and frequency measures as a component of diagnosis of alcohol disorders (Li et al., 2007). Research specific to older adults has questioned the wisdom of concise consumption guidelines. One criticism is that confounding variables such as health status and psychiatric/medical comorbidity make estimates of healthy and unsafe levels of drinking invalid for many older adults. Recent research has questioned whether individuals who exceed recommended alcohol intake for older adults suffer health consequences (Lang et al., 2007).
DSM-IV diagnoses
DSM-IV criteria represent another approach to quantifying alcohol-related risk among older adults. They represent a direct measure of alcohol-related problems. Analyses using item Response theory modeling techniques suggest that DSM-IV related problems measure a higher level of severity along the alcohol continuum than alcohol consumption guidelines (Saha et al., 2007), but this was not specifically examined in older age groups. Different indicators of pathology likely identify different groups of older drinkers; considerable overlap may exist between individuals who consume above the NIAAA limits and are diagnosed with DSM-IV alcohol abuse/dependence. Based on recent item Response theory analyses, the use of a consumption cutoff is likely more inclusive, whereas DSM-IV diagnosis is more stringent.
In older adults, problem use (As defined by DSM-IV) and consumption are the primary indicators for screening. These different measures of risk yield distinct subpopulations of drinkers with unique risk factors and consequences. By combining both consumption and DSM-IV criteria, it is possible to discern risk-drinking profiles of older adults. One can also consider the extent to which the DSM-IV criteria and consumption guidelines identify different types of drinkers (E.g., criteria endorsement without exceeding drinking guidelines versus exceeding guidelines without endorsing criteria). Because older adults metabolize alcohol more slowly, they may endorse alcohol-related problems at lower consumption levels.
Indicators and latent classes of older drinkers
With these factors in mind, we sought to explore how these different alcohol indicator variables among older adults may yield distinct subpopulations with risk factors and health impact. We had the following aims: (1) to examine the number and characterization of latent classes of alcohol use among older adult current drinkers using latent class analysis (LCA) of alcohol symptoms and alcohol consumption measures; (2) to explore the relationship between these empirically derived latent classes and current/lifetime DSM-IV diagnoses; (3) to examine sociodemographic and psychiatric risk factors associated with latent class status; and (4) to investigate associations between latent class status and physical health and mental health disability.
Method
Sample
This analysis used a subsample of current drinkers ages 60 or older (n = 4,646) from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Wave 1 conducted in 2001-2002. The NESARC survey is a nationally representative sample of 43,093 noninstitutionalized individuals ages 18 years and older (Grant et al., 2003). The NESARC oversampled Hispanics and African Americans in the interest of obtaining reliable statistical estimation in these populations and to ensure appropriate representation of racial/ethnic subgroups (Grant et al., 2003). The response rate for NESARC was 81% (Grant et al., 2003). United States census workers conducted in-person interviews using the Alcohol Use Disorder and Associated Disabilities Interview Schedule–DSM-IV version, which has been shown to have excellent internal consistency reliability in assessing alcohol disorders and consumption (Grant et al., 1995; Hasin et al., 1997).
Measures
Dichotomous indicators of 11 diagnostic criteria of alcohol abuse/dependence in the past year were created. Additionally, past-year binary indicators of the quantity and frequency of alcohol consumption were created based on NIAAA guidelines for healthy drinking cutoffs. These include no more than one drink per day (maximum of seven drinks per week) and no more than five drinks on any occasion for both men and women (Blow, 1998). A specific question regarding consumption of five drinks on a single day was used. This reflects the more liberal cutoff used for heavy episodic drinking in the general population (Dawson, 2000).
Other measured data include sociodemographic information (e.g., gender), self-rated health/mental health disability, past-year mental health and alcohol-use diagnoses, anxiety disorders, major depression, antisocial personality disorder, and current/former smoking status. Individuals were coded as married if they endorsed being currently married or cohabitating. Education was dummy-coded with three categories: less than high school, high school, and any post-high school education. Age was coded in years, and income was rescaled into increments of $10,000 for interpretability. Self-rated health disability was measured using the Medical Outcomes Study Short Form-12 (SF-12; Ware et al., 1996), a valid and reliable measure in older adults (Resnick and Nahm, 2001).
Major depression for this analysis refers to past-year diagnosis. Because of low prevalence of individual anxiety disorders, we grouped into a single indicator any past-year diagnosis of panic disorder with or without agoraphobia and past-year generalized anxiety disorder. Individuals were coded as a child of an alcoholic if they endorsed that either of their biological parents had an alcohol problem. Respondents were considered past-year users of alcohol treatment services if they endorsed one or more types of services/help seeking, including both formal inpatient and outpatient speciality alcohol treatment as well as informal help seeking such as self-help groups like Alcoholics Anonymous. Smoking status was also dummy-coded based on whether individuals were lifetime nonsmokers, former smokers (not in the past 12 months), or current smokers (smoked in the past 12 months).
Analyses
LCA was used to identify subgroups of older adult (≥60 years) current drinkers. LCA is considered a "person-centered" methodology (McCutcheon, 2002; Muthén, 2002). Compared with other cluster analysis methods, individuals are not assigned to groups but rather are given probabilities of membership in each group adding to 1 for each individual. This method disaggregates heterogeneous patterns, fostering understanding of risk factors and outcomes related to distinct subpopulations. Dichotomous indicators used in latent class models included 11 items reflecting symptoms of DSM-IV alcohol abuse/dependence and 2 items based on exceeding NIAAA frequency guidelines (more than seven drinks per week and more than five drinks on one occasion in the past year for both men and women). Mplus (Muthén and Muthén, 1998–2008) was used for LCA models, as this statistical package is capable of analyzing complex survey data. Using robust maximum likelihood estimation, two-, three-, four-, and five-class models were analyzed. Bayesian Information Criterion, Akaike Information Criterion, sample size-adjusted Bayesian Information Criterion, average class probabilities, and substantive considerations were used to evaluate the optimum number of classes (Nylund et al., 2007).
Following LCA model estimation, bivariate and multi-variate analyses were carried out using SUDAAN software (Research Triangle Institute, 2004). Like Mplus, SUDAAN is used to adjust statistical analyses for complex survey design. Because each individual has probabilities of being in all latent classes, weighted replicates of individuals were created based on the number of classes. Individual probabilities of membership in each class were multiplied by the NESARC sampling weight. To avoid missing replicates when multiplying by zero probabilities, individuals with zero probability of being in a given class were assigned a class probability of half the lowest possible class probability (.0005). We used weighted replicates to offset bias in regression estimates because, in LCA, individuals have a probability of class membership and are not perfectly assigned to a given class. This strategy is more conservative, offsetting the possibility that findings are the result of misclassification.
We used a multinomial model to analyze the relationship between class membership and sociodemographic and psychiatric predictors. The influence of latent class on self-rated physical health and mental health status was assessed using linear regression. We conducted separate models based on the theory that drinking patterns influence health status and to derive differences in self-rated health in different classes.
Results
Sample characteristics
In Table 1, characteristics are listed for the older adult current drinker subsample (age ≥60), all current drinkers (all ages), and the complete sample. The older sample is notable for having a larger weighted percentage (87%) of white respondents than in the overall NESARC sample (70.89%). A lower proportion of individuals in the full NESARC sample were currently married (62%) than in the older adult sub-sample (68%). Past-year prevalence of major depression, anxiety disorders, and antisocial personality disorder was lower in the older sample than in NESARC current drinkers and the sample as a whole (Table 1). Rates of alcohol abuse and dependence and current smoking were lower than in younger age groups. The prevalence of past-year alcohol abuse or dependence in the sample (3.9%) was lower than the 12.9% past-year prevalence rate that has been reported among current drinkers of all ages in prior NESARC publications (National Institute on Alcohol Abuse and Alcoholism, 2006).
Table 1.
Sociodemographic and clinical characteristics of the sample
| Variable | Older adult analysis sample (n = 4,646) n (weighted%) | All age current drinkers (n = 26,946) n (weighted%) | Full NESARC sample (n = 43,093) n (weighted%) |
| Gender | |||
| Male | 2,280 (52.14%) | 13,067 (52.59%) | 18,518 (47.92%) |
| Female | 2,366 (47.86%) | 13,879 (47.41%) | 24,575 (52.08%) |
| Marital status | |||
| Not currently | 2,147 (32.08%) | 12,684 (37.57%) | 21,012 (38.38%) |
| Married | 2,497 (67.92%) | 14,262 (62.43%) | 22,081 (61.62%) |
| Race | |||
| White | 3,578 (86.50%) | 16,732 (75.30%) | 24,507 (70.89%) |
| Black | 475 (4.89%) | 4,185 (9.00%) | 8,245 (11.07%) |
| Native American | 66 (1.64%) | 416 (1.89%) | 701 (2.12%) |
| Asian American | 52 (2.13%) | 664 (3.22%) | 1,332 (4.36%) |
| Latino/Hispanic | 475 (4.83%) | 4,949 (10.59%) | 8,038 (11.56%) |
| Education | |||
| Less than high school | 861 (16.04%) | 3,381 (11.09%) | 7,849 (15.65%) |
| High school/GED | 1,486 (32.61%) | 7,359 (27.29%) | 12,547 (29.33%) |
| College | 2,299 (51.35%) | 16,206 (61.63%) | 22,697 (55.02%) |
| Mental health | |||
| Major depression | 172 (3.47%) | 2,349 (8.30%) | 3,485 (7.90%) |
| Anxiety Disordera | 225 (1.54%) | 1,098 (3.99%) | 1,730 (4.02%) |
| ASPD | 39 (0.97%) | 1,094 (4.34%) | 1,422 (3.63%) |
| Smoking | |||
| Former smoker | 2,041 (45.21%) | 5,214 (19.76%) | 8,074 (19.19%) |
| Current smoker | 912 (19.60%) | 8,552 (33.14%) | 11,118 (27.66%) |
| Lifetime nonsmoker | 1,693 (35.20%) | 13,180 (47.09%) | 23,901 (53.15%) |
| Other | |||
| Past-year service use | 22 (0.34%) | 340 (1.24%) | 609 (1.40%) |
| Contemplated help | 174 (1.48%) | 718 (3.48%) | 1,078 (3.33%) |
| Child of alcoholic | 669 (14.50%) |
6,306 (23.47%) |
9,170 (21.86%) |
| Mean (median) |
Mean (median) |
Mean (median) |
|
| Age, in years | 70.10 (68.33) | 42.67 (40.30) | 45.24 (42.73) |
| Income, in U.S. $ | 47,509 (33,982) | 58,626 (44,949) | 52,335 (39,999) |
Notes: NESARC = National Epidemiologic Survey on Alcohol and Related Conditions; GED = General Educational Development Credential; ASPD = antisocial personality disorder.
Diagnosis of panic disorder with/without agoraphobia or generalized anxiety disorder.
Results of fitting latent class models
LCAs were completed using DSM-IV abuse/dependence criteria (11 items) and NIAAA alcohol consumption thresholds (2 items) as indicators. Models were estimated using two-, three-, four-, and five-class solutions. Based on measures of model fit, a three-class solution was deemed to fit the data best. Bayesian Information Criterion and adjusted Bayesian Information Criterion were at a minimum in the three-class model. Additionally, average posterior probabilities were all above .90, the likelihood ratio chi-square was nonsignificant (denoting good model fit), and only one class represented less than 5% of the sample. Based on these factors and examination of the substantive meaningfulness of the classes, three drinking classes were identified.
Three-class solution
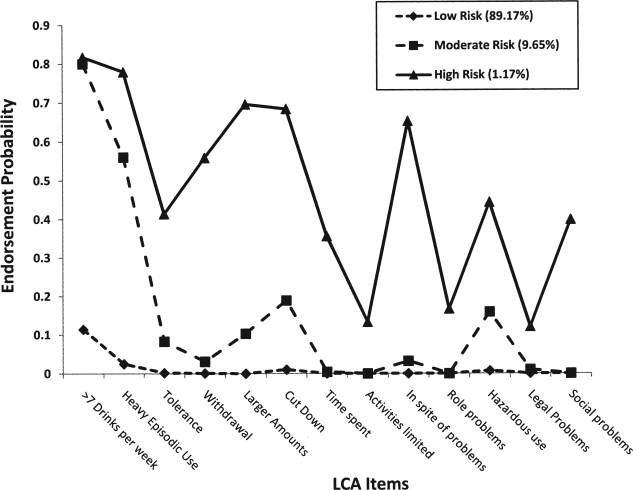
Figure 1 depicts the item probabilities for each item of the three-class model based on the class membership. Item probabilities denote the likelihood of endorsement of a given criteria (DSM-IV) or threshold (NIAAA) for individuals in a given class. The three classes are shown as three lines: a class defined as a low-risk (89.17%), a moderate-risk (9.65%), and a high-risk (1.17%) drinking class based on most likely class status. Each line in the figure represents a pattern of endorsement probabilities unique to members of a given class. Rather than reflecting heterogeneity, the classes derived from this model represent levels of severity based on endorsement of LCA indicators.
Figure 1.
Item endorsement by alcohol subgroup; LCA = latent class analysis
Individuals in the most common class (89.17%), the low-risk drinker class, showed very low probabilities of endorsement of heavy episodic use and at-risk consumption, and almost no probability of endorsing any DSM-IV criteria for either alcohol abuse or alcohol dependence. The moderate-risk drinkers, comprising about 9.65% of the sample of current drinkers, are distinct from the low-risk drinkers by their endorsements of consuming more than seven drinks per week (.80) and drinking more than five drinks on a single occasion (.56). Moderate-risk drinkers were also more likely to endorse a number of DSM-IV abuse/dependence criteria, including drinking more/longer than intended (.10), attempting to cut down on drinking (.19), and using alcohol in hazardous situations (.16), but these probabilities were generally low, implying that the moderate-risk drinker class is characterized primarily by exceeding recommended consumption guidelines.
The high-risk drinker class was the smallest (1.17%) but most severe class; with few exceptions, endorsement probabilities of alcohol diagnostic criteria were .4 or greater. Nonetheless, probabilities of endorsement of certain criteria were relatively low, including interference with activities (0.13), role problems (0.17), and legal problems (0.12). Although endorsement of NIAAA risk guidelines differentiated low-risk and moderate-risk drinkers, high-risk drinkers were as likely as moderate-risk drinkers to endorse more than seven drinks per week (.82 vs .80) but more likely to endorse heavy episodic drinking (.78 vs .56). Although the consumption-related risk factor differentiated the moderate-risk drinker from the low-risk drinker, the high-risk drinking class was distinct because of its high likelihood of DSM-IV criteria endorsement.
Class status and DSM-IV diagnoses
Table 2 displays the relationship of the latent classes with past-year and lifetime DSM-IV abuse/dependence. In the low-risk class, rates of past-year alcohol abuse/dependence were very low, whereas lifetime alcohol-use disorder rates in this group were approximately 20%. Among moderate-risk drinkers, rate of any past-year alcohol abuse and/or alcohol-dependence disorder was 23%, with most individuals in this class diagnosed with abuse, but the majority had no alcohol-use disorder in the past year. However, a large proportion of this group (63%) had been diagnosed with alcohol abuse or dependence at some point in their life, with most qualifying for lifetime alcohol abuse. In contrast, high-risk drinkers had very high prevalence of past-year and previous-to-past-year (≥12 months) alcohol abuse/dependence, with 94% endorsing a previous-to-past-year disorder and with nearly all qualifying for a past-year disorder.
Table 2.
Sociodemographic and clinical characteristics by class membership
| Variable | Low risk n = 4,134 (89.17%) n (weighted%) | Moderate risk n = 453 (9.65%) n (weighted%) | High risk n = 59 (1.17%) n (weighted%) | Wald F |
| Gender | ||||
| Male | 1,881 (48.73%) | 351 (80.02%) | 48 (81.60%) | 46.80‡ |
| Female | 2,253 (51.27%) | 102 (19.98%) | 11 (18.40%) | |
| Marital status | ||||
| Not currently | 1,907 (32.02%) | 207 (30.67%) | 35 (48.26%) | 2.32 |
| Married | 2,227 (67.98%) | 246 (69.33%) | 24 (51.74%) | |
| Race | ||||
| White | 3,194 (86.51%) | 346 (88.18%) | 38 (71.98%) | 2.56 |
| African American | 412 (4.78%) | 49 (4.30%) | 14 (18.39%) | 2.29 |
| Native American | 57 (1.52%) | 8 (2.80%) | 1 (1.41%) | 0.66 |
| Asian American | 51 (2.37%) | 1 (0.20%) | 0 (0%) | 5.69† |
| Latino/Hispanic | 420 (4.82%) | 49 (4.51%) | 6 (8.22%) | 0.38 |
| Education | ||||
| Less than high school | 725 (15.33%) | 116 (20.32%) | 20 (35.52%) | 5.00† |
| High school/GED | 1,351 (32.95%) | 120 (30.46%) | 15 (24.62%) | 1.11 |
| College | 2,058 (51.73%) | 217 (49.22%) | 24 (39.85%) | 1.64 |
| Mental health | ||||
| Major depression | 139 (3.22%) | 20 (3.18%) | 13 (24.90%) | 4.06* |
| Anxiety Disordera | 60 (1.37%) | 11 (2.28%) | 4 (8.78%) | 1.28 |
| ASPD | 30 (0.87%) | 6 (1.24%) | 3 (5.91%) | 1.11 |
| Smoking | ||||
| Former smoker | 1,811 (44.97%) | 216 (49.88%) | 14 (24.81%) | 4.31* |
| Current smoker | 710 (17.25%) | 170 (37.06%) | 32 (53.80%) | 26.96‡ |
| Lifetime nonsmoker | 1,613 (36.78%) | 67 (13.06%) | 13 (21.40%) | 29.79‡ |
| Other | ||||
| Past-year service use | 6 (0.10%) | 10 (1.67%) | 6 (7.46%) | 5.44† |
| Contemplated help | 26 (0.85%) | 15 (2.51%) | 17 (28.59%) | 9.44‡ |
| Child of alcoholic | 550 (13.36%) | 99 (22.28%) | 20 (37.77%) | 9.46‡ |
| Current, past year | ||||
| No diagnosis | 4,104 (99.33%) | 358 (77.20%) | 3 (0.82%) | 14.55‡ |
| Abuse | 30 (0.67%) | 94 (22.42%) | 9 (15.66%) | |
| Dependence | 0 (0%) | 1 (0.17%) | 16 (26.55%) | |
| Abuse/dependence | 0 (0%) | 0 (0%) | 33 (56.97%) | |
| Lifetime, ≥12 months | ||||
| No diagnosis | 3,402 (81.18%) | 173 (36.97%) | 3 (5.78%) | 17.95‡ |
| Abuse | 605 (15.57%) | 224 (51.46%) | 3 (7.39%) | |
| Dependence | 22 (0.49%) | 11 (2.37%) | 15 (4.95%) | |
| Abuse/dependence | 105 (2.76%) |
45 (9.20%) |
48 (81.88%) |
|
| Mean (median) |
Mean (median) |
Mean (median) |
F |
|
| Age, in years | 70.45 (68.72) | 67.49 (65.31) | 64.77 (63.06) | 136.46‡ |
| Income, in U.S. $ | 47,652 (33,964) | 47,532 (35,072) | 36,396 (23,598) | 0.42 |
Notes: GED = General Educational Development credential; ASPD = antisocial personality disorder.
Diagnosis of panic disorder with/without agoraphobia or generalized anxiety disorder.
p <.05;
p < .01;
p < .001.
Sociodemographic and psychiatric features of latent classes
There were a number of sociodemographic differences in the groups at the bivariate level. As shown in Table 2, the moderate-risk and high-risk drinker groups were predominantly male (Wald F = 46.80, 2/65 df, p < .001) and were younger than low-risk drinkers (F = 136.36, 2/65 df, p < .001). Asian Americans were less likely to be in either risky drinking class (Wald F = 5.69, 2/65 df, p = .005). Those with less than a high school education showed progressively higher representation in the moderate-risk and high-risk drinking classes (Wald F = 5.00, 2/65 df, p = .009). Those in the high-risk drinking class had very high rates of past-year major depression compared with the moderate-risk and low-risk groups (Wald F = 4.06, 2/65 df, p = .022). There were more former smokers than current smokers in the low-risk (45% former vs 17% current) and moderate-risk (50% former vs 37% current) groups, whereas current smokers were most common in the high-risk group (54% current vs 24% former). In the high-risk drinking class, rates of past-year service use were higher (7.46%) compared with the moderate-risk and low-risk classes (less than 2% each), and greater numbers of high-risk drinkers considered obtaining treatment but did not. Rates of reported alcoholism in either parent among respondents in the classes were progressively higher from low-risk (13.36%) to moderate-risk (22.28%) drinkers, with rates among high-risk drinkers the most elevated at 37.77%.
Multivariate predictors of latent class membership
A multinomial model was used to assess sociodemo-graphic and psychiatric predictors of class status with low-risk drinkers as the reference class (Table 3). Female gender (odds ratio [OR] = 0.25, p < .001; reference: male), older age (OR = 0.94, p < .001), being married (OR = 0.69, p < .01), and African-American race (OR = 0.66, p = .026) were associated with decreased risk of being in the moderate-risk drinking class. Being the adult child of an alcoholic (OR = 1.75, p < .001), being a previous (but not current) smoker (OR = 2.49, p < .001), and being a current smoker (OR = 3.92, p < .001) were associated with increased odds of being in the moderate-risk drinker class.
Table 3.
Demographic and psychiatric predictors of class membership
| Variable | Moderate-risk class OR (95% CI) | High-risk class OR (95% CI) |
| Gender, ref.: male | 0.25‡ (0.19, 0.33) | 0.15‡ (0.06, 0.38) |
| Age, per year | 0.94‡ (0.93, 0.96) | 0.87‡ (0.83, 0.92) |
| Annual income, in thousands of dollars | 0.99 (0.97, 1.02) | 0.97 (0.88, 1.06) |
| Marital status | ||
| ref.: not married | 0.69† (0.56, 0.86) | 0.52 (0.24, 1.16) |
| African American | ||
| ref.: non-African American | 0.66* (0.46, 0.95) | 2.25 (1.00, 5.10) |
| High school graduate | ||
| ref.: less than high school | 0.80 (0.58,1.10) | 0.43 (0.19,1.01) |
| College | ||
| ref.: less than high school | 0.77 (0.56, 1.05) | 0.42* (0.20, 0.88) |
| Current major depression | 1.07 (0.58, 1.98) | 9.57‡ (3.59, 25.53) |
| Adult child of alcoholic | 1.75‡ (1.30, 2.36) | 3.19‡ (1.68, 6.07) |
| Antisocial personality disorder | 0.55 (0.20,1.52) | 1.54 (0.38,6.26) |
| Former smoker | ||
| ref.: lifetime nonsmoker | 2.49‡ (1.74, 3.57) | 0.74 (0.32,1.70) |
| Current smoker | ||
| ref.: lifetime nonsmoker | 3.92‡ (2.71, 5.68) | 2.49* (1.17, 5.29) |
Notes: OR = odds ratio; CI = conference interval; ref. = reference.
p <.05;
p <.01;
p <.001.
Female gender (OR = 0.15, p < .001), older age (OR = 0.87, p < .001), and college education (OR = 0.42, p < .001) were associated with decreased odds of being in the high-risk drinking class. Past-year major depression (OR = 9.57, p < .001), being the child of an alcoholic (OR = 3.19, p < .001), and being a current smoker (OR = 2.49, p = .039) were associated with increased odds of membership in the high-risk drinking class. Additionally, African-American race displayed a trend toward (OR = 2.25, p = .051) significance with membership in the high-risk drinking class.
Latent class membership and health
Two linear regression models assessed the relationship between latent class membership and ratings of physical and mental health. Using the SF-12 mental health subscale as the dependent variable (see Table 4), high-risk drinker class and female gender were significantly associated with poorer self-rated mental health. Greater income, being married, and high school or college education were associated greater self-rated mental health. In a parallel model (Table 4), physical health status (SF-12 physical health subscale) was regressed on the drinking classes and sociodemographic and psychiatric variables. High-risk drinker class membership was significantly associated with lower self-rated physical health, although this relationship was less pronounced than was observed for mental health. Increased age and being a current or former smoker also were associated with decreased physical health. Higher income, being married, and greater education (high school and college) were associated with greater physical health.
Table 4.
Regression models of Medical Outcomes Study Short Form-12 (SF-12) scores
| Variable | SF-12: Mental health |
SF-12: Physical health |
||||
| b | SE | t | b | SE | t | |
| Moderate-risk class | ||||||
| ref.: low risk | −0.46 | 0.56 | −0.95 | −0.40 | 0.66 | −0.61 |
| High-risk class | ||||||
| ref.: low risk | −7.53 | 1.97 | −3.95‡ | −4.54 | 2.06 | −2.20* |
| Gender | ||||||
| ref.: male | −1.35 | 0.31 | −4.33‡ | 0.03 | 0.36 | 0.08 |
| Age, in years | −0.04 | 0.03 | −1.96 | −0.31 | 0.02 | −12.73‡ |
| Income, per $10,000 | 0.03 | 0.01 | 3.09† | 0.09 | 0.03 | 3.23† |
| Marital status | ||||||
| ref.: not married | 1.19 | 0.30 | 4.00‡ | 0.77 | 0.38 | 2.01* |
| African American | ||||||
| ref.: non-African American | −1.01 | 0.63 | −1.93 | −1.28 | 0.69 | −1.85 |
| High school | ||||||
| ref.: less than high school | 1.95 | 0.57 | 1.65† | 3.31 | 0.64 | 5.20‡ |
| College | ||||||
| ref.: less than high school | 2.43 | 0.49 | 2.94‡ | 4.80 | 0.57 | 8.48‡ |
| Former smoker | ||||||
| ref.: lifetime nonsmoker | 0.64 | 0.39 | 1.65 | −1.74 | 0.42 | −4.18‡ |
| Current smoker | ||||||
| ref.: lifetime nonsmoker | −0.49 | 0.47 | −1.31 | −2.85 | 0.53 | −5.38‡ |
Notes: Ref. = reference.
p < .05;
p < .01;
p < .001
Discussion
Although older adults manifest lower rates of alcohol abuse/dependence than their younger counterparts, there is variation in late-life drinking patterns. Our latent class model suggests a hierarchical structure based on diagnostic and NIAAA thresholds. LCA-derived latent classes were associated with differences in gender, race, age, current and past alcohol-use disorders, psychiatric comorbidity, and smoking. Drinking class was associated with current physical and mental health disability in the high-risk drinking class but not in moderate-risk drinkers.
Correlates of alcohol risk among older adults
Consistent with previous research, younger individuals and men were more likely to be in the moderate-risk and high-risk drinking classes. Cross-sectional (Grant et al., 2004) and longitudinal (Karlamangla et al., 2006; Rice et al., 2003) studies have shown higher rates of at-risk or hazardous use, alcohol abuse, and alcohol dependence among men. Although rates are lower for women, both genders show declines in alcohol use with advancing age (Moos et al., 2004).
Although age and gender were associated with both moderate-risk and high-risk drinker classes, African-American older adults showed decreased likelihood of being in the moderate-risk drinker class, but African-American race showed a near-significant association with being in the high-risk drinking class. Research suggests that older African-American alcoholics may also suffer greater medical and psychosocial consequences as a result of their drinking (Gomberg and Nelson, 1995), which may increase their likelihood of endorsing DSM-IV criteria. Although levels of problem drinking have been shown to be higher among African Americans, abstinence rates are also higher.
Major depression was also significantly associated with drinking class among older adults but only among the small percentage of individuals in the problem drinking class. Although it is difficult to infer causality, high levels of major depression in the problem drinking group may be the result of chronic alcohol problems. Among older adults discharged from inpatient psychiatric treatment, Blixen et al. (1997) found that 37% had some substance abuse/psychiatric comorbidity. In this dual-diagnosis group, more than 70% had depression. In a study of comorbidity among alcoholics in the Veterans Affairs system, researchers found that comorbid depression was more common with increasing age (Blow et al., 1992) even as levels of posttraumatic stress disorder, schizophrenia, and other comorbidities were lower. Because alcohol use has been implicated as a factor in suicides among older adults (Sorock et al., 2006; Waern, 2003), further investigation of the processes underlying depression and alcohol consumption is warranted.
Our findings also suggest that parental alcoholism remains an important event among older adults as history of parental alcoholism predicted membership in risk and problem drinking classes. In a study of older adult lifetime alcohol use, Prescott and colleagues (1994), "found strong evidence for family resemblance for liability to lifetime alcohol abuse and alcohol-related problems, with about 50% of the variance estimated as familial" (p. 198).
Among individuals in the problem drinker class, rates of current alcoholism treatment use were relatively low (7.46%). Other research studies have found that elderly individuals are least likely to have recent treatment (Proudfoot and Teesson, 2002; Satre et al., 2003) even as older adults show greater likelihood of lifetime treatment use (Cohen et al., 2007). Treatment outcomes for older adults are favorable compared with younger age groups (Janik and Dunham, 1983; Rice et al., 1993; Satre et al., 2004), implying that efforts to engage these older problem drinkers will have a potentially positive public health impact.
Health, mental health, and alcohol risk among older adults
Relationships between the problem drinking class and mental health and physical health disability support the value of engaging older problem drinkers. High-risk drinking class was associated with SF-12 greater mental health and physical health disability. Yet, these differences were not found among moderate-risk drinkers, suggesting that higher levels of consumption in the absence of problem use are not disabling.
Although membership in the moderate-risk drinker class was not associated with self-reported physical or mental health disability, both moderate-risk and high-risk drinkers were more likely to be current smokers. Moderate-risk and high-risk drinkers may be at greater risk if their alcohol use is combined with other problematic health behaviors. Satre et al. (2007), in a study of health plan members, found that exceeding NIAAA drinking limits was associated with current smoking and poor dietary practices in men. In considering public health goals, drinking should be seen in light of overall health behaviors.
Limitations
Although this analysis benefited from a nationally representative sample of older drinkers, cross-sectional data were used. Potential causal mechanisms could not be explored. Additionally, this study was limited to current drinkers only. This likely affected estimates of high-risk drinker prevalence among African Americans because high levels of abstinence in this group were not considered. Although this research looked at the role of consumption and problem use as indicators of drinking problems, this study was unable to consider other important indicators of older adult risk drinking. These include medical conditions or medications that make alcohol use risky for older adults (Moore et al., 2002). These omissions may have obscured some risky drinking patterns in this population. Finally, using LCA, individuals can have a probability of being in multiple groups. We used weighted replicates to adjust for this fact, and average class probabilities were greater than .90 for each class, but LCA interpretation is more complex than diagnostic classifications.
Conclusions
Although more complex than other methods, LCA identified three groups of older drinkers with distinctive sociodemographic and health-related characteristics. Our findings suggest that a substantial subpopulation of older drinkers exceed consumption guidelines without displaying alcohol-related problems. Some of these individuals have a history of alcohol abuse/dependence but do not display increased mental or physical health disability compared with individuals who do not exceed drinking guidelines. African Americans were less likely to be in this group but showed higher rates of being high-risk users. In multivariate models, these relationships were attenuated, implying a complex relationship between race and other factors (e.g., education, income). For drinkers in the high-risk drinker class, alcohol use may be part of a larger pattern of health risks, including smoking, major depression, and a history of alcohol abuse/dependence earlier in life. Our findings support the need for continued outreach to older problem drinkers, as the health impacts are substantial. Consuming more than the NIAAA cutoffs may not necessitate services, but longitudinal analysis may uncover risks for at-risk drinkers as they age. Future longitudinal analysis is necessary to determine the long-term drinking patterns and health outcomes for moderate-risk and high-risk older drinkers. Wave 2 of the NESARC survey will allow us to compare the 3-year outcomes by latent class membership.
Footnotes
This research was supported by National Institute on Alcohol Abuse and Alcoholism (NIAAA) grant P50AA011998 through the Midwest Alcoholism Research Center, National Institute of Mental Health grant P30 MH068579 through the Center for Mental Health Services Research, National Institute on Drug Abuse grant T32 DA015035 awarded to Paul Sacco, the John A. Hartford Doctoral Fellows Program, and NIAAA grant F31 AA018050.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) Washington, DC: 1994. [Google Scholar]
- Bell AJ, Talbot-Stern JK, Hennessy A. Characteristics and outcomes of older patients presenting to the emergency department after a fall: A retrospective analysis. Med. J. Aust. 2000;173:179–182. doi: 10.5694/j.1326-5377.2000.tb125596.x. [DOI] [PubMed] [Google Scholar]
- Blixen CE, McDougall GJ, Suen L-J. Dual diagnosis in elders discharged from a psychiatric hospital. Int. J. Geriat. Psychiat. 1997;12:307–313. doi: 10.1002/(sici)1099-1166(199703)12:3<307::aid-gps475>3.0.co;2-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blow FC. Substance Abuse Among Older Adults. Treatment Improvement Protocol (TIP) Series No. 26, DHHS Publication No. (SMA) 98-3179. Rockville, MD: Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; 1998. [PubMed] [Google Scholar]
- Blow FC, Cook AA, Booth BM, Falcon SP, Friedman MJ. Age-related psychiatric comorbidities and level of functioning in alcoholic veterans seeking outpatient treatment. Hosp. Commun. Psychiat. 1992;43:990–995. doi: 10.1176/ps.43.10.990. [DOI] [PubMed] [Google Scholar]
- Blow FC, Walton MA, Barry KL, Coyne JC, Mudd SA, Copeland LA. The relationship between alcohol problems and health functioning of older adults in primary care settings. J. Amer. Geriat. Soc. 2000;48:769–774. doi: 10.1111/j.1532-5415.2000.tb04751.x. [DOI] [PubMed] [Google Scholar]
- Byles J, Young A, Furuya H, Parkinson L. A drink to healthy aging: The association between older women's use of alcohol and their health-related quality of life. J. Amer. Geriat. Soc. 2006;54:1341–1347. doi: 10.1111/j.1532-5415.2006.00837.x. [DOI] [PubMed] [Google Scholar]
- Cohen E, Feinn R, Arias A, Kranzler HR. Alcohol treatment utilization: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2007;86:214–221. doi: 10.1016/j.drugalcdep.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Dawson DA. Us low-risk drinking guidelines: An examination of four alternatives. Alcsm Clin. Exp.Res. 2000;24:1820–1829. [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Li T-K. Quantifying the risks associated with exceeding recommended drinking limits. Alcsm Clin. Exp. Res. 2005;29:902–908. doi: 10.1097/01.alc.0000164544.45746.a7. [DOI] [PubMed] [Google Scholar]
- Gomberg ESL, Nelson BW. Black and white older men: Alcohol use and abuse. In: Beresford TP, Gomberg E, editors. Alcohol and Aging. New York: Oxford Univ. Press; 1995. pp. 307–323. [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991-1992 and 2001-2002. Drug Alcohol Depend. 2004;74:223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Grant BF, Harford TC, Dawson DA, Chou PS, Pickering RP. The Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): Reliability of alcohol and drug modules in a general population sample. Drug Alcohol Depend. 1995;39:37–44. doi: 10.1016/0376-8716(95)01134-k. [DOI] [PubMed] [Google Scholar]
- Grant BF, Kaplan K, Shepard J, Moore T. Source and Accuracy Statement for Wave 1 of the 2001-2002 National Epidemiologic Survey on Alcohol and Related Conditions. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. [Google Scholar]
- Hasin D, Carpenter KM, McCloud S, Smith M, Grant BF. The Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): Reliability of Alcohol and drug modules in a clinical sample. Drug Alcohol Depend. 1997;44:133–141. doi: 10.1016/s0376-8716(97)01332-x. [DOI] [PubMed] [Google Scholar]
- Janik SW, Dunham RG. A nationwide examination of the need for specific alcoholism treatment programs for the elderly. J. Stud. Alcohol. 1983;44:307–317. doi: 10.15288/jsa.1983.44.307. [DOI] [PubMed] [Google Scholar]
- Karlamangla A, Zhou K, Reuben D, Greendale G, Moore A. Longitudinal trajectories of heavy drinking in adults in the United States of America. Addiction. 2006;101:91–99. doi: 10.1111/j.1360-0443.2005.01299.x. [DOI] [PubMed] [Google Scholar]
- Lang I, Guralnik J, Wallace RB, Melzer D. What level of alcohol consumption is hazardous for older people? Functioning and mortality in U.S. and English national cohorts. J. Amer. Geriat. Soc. 2007;55:49–57. doi: 10.1111/j.1532-5415.2006.01007.x. [DOI] [PubMed] [Google Scholar]
- Li T-K, Hewitt BG, Grant BF. Is there a future for quantifying drinking in the diagnoses, treatment, and prevention of alcohol use disorders? Alcohol Alcsm. 2007;42:57–63. doi: 10.1093/alcalc/agl125. [DOI] [PubMed] [Google Scholar]
- McCutcheon AL. Basic concepts and procedures in single- and multiple-group latent class analysis. In: Hagenaars JA, McCutcheon AL, editors. Applied Latent Class Analysis. Cambridge, MA: Cambridge Univ. Press; 2002. pp. 56–87. [Google Scholar]
- Moore AA, Beck JC, Babor TF, Hays RD, Reuben DB. Beyond alcoholism: Identifying older, at-risk drinkers in primary care. J. Stud. Alcohol. 2002;63:316–325. doi: 10.15288/jsa.2002.63.316. [DOI] [PubMed] [Google Scholar]
- Moore AA, Giuli L, Gould R, Hu P, Zhou K, Reuben D, Greendale G, Karlamangla A. Alcohol use, comorbidity, and mortality. J. Amer. Geriat. Soc. 2006;54:757–762. doi: 10.1111/j.1532-5415.2006.00728.x. [DOI] [PubMed] [Google Scholar]
- Moos RH, Schutte K, Brennan P, Moos BS. Ten-year patterns of alcohol consumption and drinking problems among older women and men. Addiction. 2004;99:829–838. doi: 10.1111/j.1360-0443.2004.00760.x. [DOI] [PubMed] [Google Scholar]
- Muthén BO. Beyond SEM: General latent variable modeling. Behaviormetrika. 2002;29:81–117. [Google Scholar]
- Muthén LK, Muthén BO. Mplus Users Guide, Version 4. Los Angeles, CA: Muthén & Muthén; 1998–2008. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. The Physicians' Guide to Helping Patients with Alcohol Problems, NIH Publication No. 95–3769. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 1995. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Alcohol Use and Alcohol Use Disorders in the United States: Main Findings from the 2001-2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). U.S. Alcohol Epidemiologic Data Reference Manual, Vol. 8, No. 1, NIH Publication No. 05-5737. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2006. [Google Scholar]
- Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte carlo simulation study. Struct. Equat. Model. 2007;14:535–569. [Google Scholar]
- Prescott CA, Hewitt JK, Truett KR, Heath AC, Neale MC, Eaves LJ. Genetic and environmental influences on lifetime alcohol-related problems in a volunteer sample of older twins. J. Stud. Alcohol. 1994;55:184–202. doi: 10.15288/jsa.1994.55.184. [DOI] [PubMed] [Google Scholar]
- Proudfoot H, Teesson M. Who seeks treatment for alcohol dependence? Findings from the Australian National Survey of Mental Health and Wellbeing. Social Psychiat. Psychiat. Epidemiol. 2002;37:451–456. doi: 10.1007/s00127-002-0576-1. [DOI] [PubMed] [Google Scholar]
- Research Triangle Institute. SUDAAN Language Manual, Release 9.0. Research Triangle Park, NC: Research Triangle Institute; 2004. [Google Scholar]
- Resnick B, Nahm ES. Reliability and validity testing of the revised 12-Item Short-Form Health Survey in older adults. J. Nurs. Meas. 2001;9:151–161. [PubMed] [Google Scholar]
- Rice C, Longabaugh R, Beattie M, Noel N. Age group differences in response to treatment for problematic alcohol use. Addiction. 1993;88:1369–1375. doi: 10.1111/j.1360-0443.1993.tb02023.x. [DOI] [PubMed] [Google Scholar]
- Rice JP, Neuman RJ, Saccone NL, Corbett J, Rochberg N, Hesselbrock V, Bucholz KK, McGuffin P, Reich T. Age and birth cohort effects on rates of alcohol dependence. Alcsm Clin. Exp. Res. 2003;27:93–99. doi: 10.1097/01.ALC.0000047303.89421.AA. [DOI] [PubMed] [Google Scholar]
- Saha TD, Stinson FS, Grant BF. The role of alcohol consumption in future classifications of alcohol use disorders. Drug Alcohol Depend. 2007;89:82–92. doi: 10.1016/j.drugalcdep.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satre DD, Gordon NP, Weisner C. Alcohol consumption, medical conditions, and health behavior in older adults. Amer. J. Hlth Behav. 2007;31:238–248. doi: 10.5555/ajhb.2007.31.3.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satre DD, Knight BG, Dickson-Fuhrmann E, Jarvik LF. Predictors of alcohol-treatment seeking in a sample of older veterans in the GET SMART Program. J. Amer. Geriat. Soc. 2003;51:380–386. doi: 10.1046/j.1532-5415.2003.51112.x. [DOI] [PubMed] [Google Scholar]
- Satre DD, Mertens JR, Arean PA, Weisner C. Five-year alcohol and drug treatment outcomes of older adults versus middle-aged and younger adults in a managed care program. Addiction. 2004;99:1286–1297. doi: 10.1111/j.1360-0443.2004.00831.x. [DOI] [PubMed] [Google Scholar]
- Sorock GS, Chen LH, Gonzalgo SR, Baker SP. Alcohol-drinking history and fatal injury in older adults. Alcohol. 2006;40:193–199. doi: 10.1016/j.alcohol.2007.01.002. [DOI] [PubMed] [Google Scholar]
- Waern M. Alcohol dependence and misuse in elderly suicides. Alcohol Alcsm. 2003;38:249–254. doi: 10.1093/alcalc/agg060. [DOI] [PubMed] [Google Scholar]
- Ware JE, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med. Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]