Abstract
Objective:
We examined the relationship of childhood exposure to adversity and risk of substance-use disorder in two culturally distinct American Indian reservation communities, exploring both the role of early initiation of substance use in mediating this relationship and variation in risk across types of adversity exposure.
Method:
The American Indian Service Utilization, Psychiatric Epidemiology, Risk and Protective Factors Project provided data from 2,927 American Indians on the occurrence and age at onset of adversities, substance use, and substance-use-disorder symptoms.
Results:
The risk of substance-use disorder associated with early adversity was explained partially by early initiation of substance use. Three types of adversity (major childhood events, traumas, and witnessed violence) were associated with early onset of substance use and increased risk of substance-use disorder. Gender and tribe were also related to variation in both early substance use and substance-use disorder.
Conclusions:
Early exposure to adverse events was associated with early substance use and the subsequent development of substance-use disorders among American Indians. Public health initiatives targeting substance use and substance-use disorders in American Indian communities should include efforts to help children in these communities cope with adversities they encounter.
Problematic substance use is widespread in many American Indian communities, and disparities in rates of Diagnostic and Statistical Manual of Mental Disorders (DSM)-defined substance-use disorders (SUDs) are well documented (Beals et al., 2003b, 2005; Hisnanick, 1992; Koss et al., 2003; Kunitz, 2008; Kunitz et al., 1999; Kunitz and Levy, 1994; May, 1996; May and Gossage, 2001; Oetting and Beauvais, 1989; Whitesell et al., 2006, 2007c). Use of drugs, tobacco, and alcohol is more common among American Indian adolescents than among other groups in the United States and is often characterized by earlier and heavier use (Anthony and Petronis, 1995; Beauvais, 1998; Hawkins et al., 1992; Hisnanick, 1992; Bachman et al., 2001; Kunitz, 2008; Mitchell et al., 2003; Novins and Barón, 2004; Oetting and Beauvais, 1989; Robins and Przybeck, 1985; Wallace et al., 2002; Whitbeck et al., 2008; Whitesell et al., 2007a, b). Reducing these disparities has become part of the national public health agenda (Center for Mental Health Services, 2001; National Institutes of Health, 2002). Efforts to address these disparities, however, have been hampered by the lack of sufficient information regarding the etiology of substance-use problems and factors related to their development.
Exposure to adversity and risk for substance-use disorder
Considerable speculation about the causes underlying higher rates of SUD among American Indians has centered on the high rates of exposure to adversity within American Indian communities (Manson et al., 2005; Robin et al., 1997a). Evidence of clear links between adversity and SUD in other populations (Dawson et al., 2005; Dohrenwend, 2000; Kessler et al., 1997; Turner and Lloyd, 1995, 2003) has led to speculation that the harsh and often violent conditions on some reservations may be one root cause of substance-use disparities. A growing body of research on the association of adversity with substance-use problems among American Indians supports this possibility, but many questions remain (Hawkins et al., 2004; Koss et al., 2003; Libby et al., 2004; Robin et al., 1999; Rodgers and Fleming, 2003; Walters et al., 2002; Whitesell et al., 2007a).
To begin with, although it is clear that adversity and substance use often co-occur and that they co-occur with particular frequency in American Indian communities, most studies have relied on correlational findings. It is thus impossible to determine whether adversity increases the odds of SUD or SUD increases exposure to adversity. Both possibilities have some support. Self-medication or tension-reduction hypotheses suggest that exposure to adversity is primary and that individuals use substances in an effort to alleviate their emotional distress in the wake of adversity (Aneshensel, 1999; Conger, 1956; Dawson et al., 2005; Walters et al., 2002; Witt, 2007). On the other hand, once substance use has begun, misuse of substances can make individuals more prone to put themselves in risky situations (e.g., driving while intoxicated and fighting) and encounter adversity (e.g., automobile accidents, physical assault) (Hingson et al., 2008; Spooner, 1999; Turner and Lloyd, 2003). Empirical evidence supports the role of stressors in the initiation and early development of substance use (LeMaster et al., 2002; Whitesell et al., 2007a). Yet most agree that once use is initiated, the developmental progression is characterized by a cyclical interplay of stress and increasing substance use (Aneshensel, 1999; Brennan et al., 1999; Stewart and Conrod, 2002), both because use increases subsequent exposure to stressful events and because it may interfere with adaptive responses to such events (Chilcoat and Menard, 2003). Our focus in this study was on the emergence of substance problems and on the possibility that adversity plays a role in the etiology of such problems. Central to our analyses, then, was placement of adverse experiences and the initiation of substance use in temporal order, determining whether experiences of adversity are associated with greater risk of subsequent SUD.
Childhood exposure to adversity
Another important gap in our understanding of the associations between adversity and SUD is in understanding the mechanisms through which potential effects of adversity are realized. The literature suggests several factors that may be particularly important in understanding how and when adversity increases risk. One clue lies in findings that the timing of exposure to adversity is important. Exposure in childhood is more likely to be associated with the development of substance-use problems than is exposure later in life (Kessler et al., 1997; Libby et al., 2004). One explanation for the association of early adversity with SUD is that, when adversity occurs early, it may disrupt developmental processes, causing disorganization that interferes with normal psychological growth. Compromised development, in turn, puts individuals at risk for a variety of mental health problems. Another explanation for the association between early adversity and SUD is that childhood adversity may be a marker for more prolonged exposure (e.g., ongoing family violence that a child witnesses repeatedly for many years). To the extent that it results in repeated diversion of psychological resources from developmental tasks, chronic exposure is likely to have more profound consequences than are isolated encounters with adversity.
Role of early substance initiation
A specific mechanism through which early exposure to adversity may be related to long-term substance-use problems is through early initiation of substance use. Although adversity at any age appears to result in increased risk of substance use, such use is associated with much greater risk of SUD if it first occurs in late childhood or early adolescence rather than in adulthood (Anthony and Petronis, 1995; Hawkins et al., 1992; Hingson et al., 2008; Kunitz, 2008; Novins and Barón, 2004; Robins and Przybeck, 1985; Stueve and O'Donnell, 2005; Warner et al., 2007; Whitesell et al., 2007a; York et al., 2004). Researchers trying to understand the potent impact of early substance use have focused on how the unique biological, social, cognitive, emotional, and identity processes at work in adolescence relate to susceptibility to either the initiation or escalation of substance use.
One line of research has focused on biological factors and physiological responses to substances, finding, for example, that young adolescents are less sensitive to some effects of alcohol, such as motor impairment and sedation, but more sensitive to other effects, including social facilitation and impairment in brain plasticity (Windle et al., 2008; Witt, 2007). Another line of research has focused on psychological development, noting marked changes in the way adolescents relate to their social environments (most notably, with peers and parents); qualitative changes in cognitive capabilities (the emergence of abstract reasoning); increasingly complex emotional experiences that accompany social and cognitive maturation; and construction of coherent self-concept and personal identity (Foshee et al., 2007; Tschann et al., 1994; Westling et al., 2008; Wichstrom, 2001). This work has identified a number of intertwined developmental risk factors with implications for emergent substance-use patterns.
Early initiation of substance use might also help to directly explain disparities in SUD between American Indian and other populations. Studies consistently show earlier onset of use among American Indians than in other U.S. groups (Kunitz, 2008; Novins and Barón, 2004; Whitbeck et al., 2008), a pattern that parallels, at least to some extent, disparities in SUD. It is thus important to consider the role of early use in explaining SUD disparities in American Indian communities.
Risk associated with different kinds of adversity
It is also clear from the literature that the relationship between adverse events and SUD is dependent on the type of event. Most research linking early exposure to adversity with SUD has focused on the significance of sexual or physical victimization (Libby et al., 2004; Robin et al., 1997b; Widom et al., 1999). Systematic comparison of the associations between different types of events and SUD is lacking, however, particularly in American Indian populations. Turner and Lloyd (2003) examined diverse types of adversity, including a wide range of experiences varying in direct involvement of the child, violence, and interpersonal nature. Across several ethnic groups (although not including American Indians), they found SUD to be related to major childhood events (salient adversities that are typically not violent, such as parental divorce or serious illness); traumas (events that are usually violent and/or involve force or coercion, such as sexual assault or automobile accident); witnessed violence (particularly family violence); and traumatic news (hearing of a trauma suffered by a significant other). They did not find associations between SUD and deaths of immediate family members.
Gender and substance-use disorder
We have not yet addressed the significance of gender in understanding substance problems, but it is clearly relevant. Gender differences in substance use and SUD are well documented (Vega et al., 2002) and these differences are themselves very disparate across tribes. For example, in one southwest tribe, we found that women had dramatically lower rates of substance use and SUD than did men, whereas in a Northern plains tribe, we found substance-use patterns to be much more similar across gender (Beals et al., 2003b, 2005; Whitesell et al., 2007c). In addition, there is evidence that the relationship between adversity and substance use may vary for males and females (Dawson et al., 2005; Robin et al., 1997a). Thus, it is important that we consider gender and how these risks may vary for boys and girls who encounter adversity.
Current study
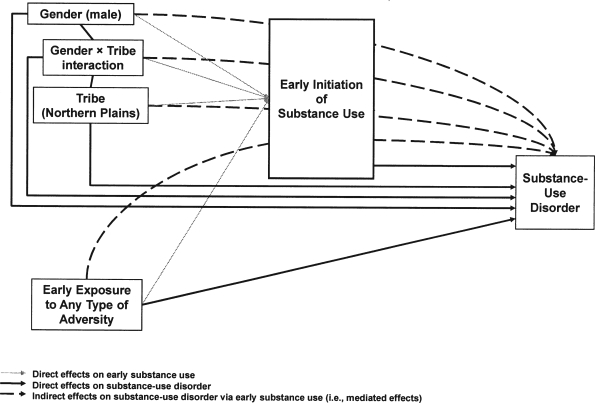
Figure 1 represents a model of relationships between exposure to adversity and the development of SUD; this model incorporates the factors introduced above and guides the work reported here. Building on evidence of tribal and gender disparities in SUD and on findings that adversity is related to increased risk, we included tribe, gender, and exposure to adversity as primary risk factors for SUD. Given reports that the timing of adversity is important, the model includes not just exposure to adversity but rather the age at which adversity is first encountered (i.e., early exposure to adversity). As suggested by the evidence of the importance of early substance-use initiation reviewed above, we included early use as a mediator of the links between these risk factors and SUD. Although not depicted in the model, we also examined the differential relationships of major childhood events, traumas, witnessed violence, traumatic news, and deaths of immediate family members with SUD.
Figure 1.
Path model of relationships among any early exposure to adversity, early initiation of substance use, and substance-use disorder, with tribe and gender effects (Model 1)
Our estimation of the model in Figure 1 extends previous work in several important ways. First, we used a large sample of American Indians from two distinct cultural groups, thus allowing a direct investigation of the relationships between adversity and SUD in this understudied population. Second, we included measures of age at first exposure to adversity, allowing tests of the inverse relationship between age at exposure and risk for subsequent SUD (i.e., later exposure associated with lower risk). We only considered adversities that occurred at least 1 year before the onset of substance use and thus clearly could not be attributed to the effects of substance use. Third, we specifically estimated the extent to which early substance initiation accounted for tribe, gender, and early adversity relationships with risk for SUD and thus might explain one mechanism through which these factors are associated with greater risk. Finally, following Turner and Lloyd (2003), we examined the differential associations between five types of adversity and SUD to help shed light on what particular features of adverse experiences might be most problematic.
Method
Participants
Data were from the American Indian Service Utilization, Psychiatric Epidemiology, Risk and Protective Factors Project (AI-SUPERPFP), a population-based study of two large, culturally distinct American Indian reservation communities. The populations of inference were 15- to 54-year-old enrolled members of two closely related Northern Plains tribes and a Southwest tribe who were living on or within 20 miles of their respective reservations at the time of sampling (1997). To protect the confidentiality of the participating communities (Norton and Manson, 1996), we refer to these tribes by general descriptors rather than by specific tribal names.
Stratified random sampling procedures were used with strata defined by tribe, gender, and age (15-24, 25-34, 35-44, and ≥45 years). Tribal rolls, the official enumeration of tribal members, were used to define the target population. In the Southwest and Northern Plains, respectively, 46.6% and 39.2% of those listed in the tribal rolls were found to be living on or near the reservations; of those located and found eligible, 76.8% in the Northern Plains (n = 1,638) and 73.7% in the Southwest (n = 1,446) agreed to participate. Sample weights accounted for differential selection probabilities across strata and for differential nonresponse by strata. A little more than one half of the sample was female (n = 1,677); 54% were living at or below the poverty line; 45% had a high school education (or equivalent); 28% had attended at least some college; 58% percent were currently employed; 55% were married or living as married. AI-SUPERPFP methods are described in greater detail elsewhere (Beals et al., 2003a); both the interview instrument and training manual are available for review on our Web site (http://aianp.uchsc.edu/ncaianmhr/research/superpfp.htm). For analyses reported here, we included adult participants (at least 18 years of age) to ensure that estimates of age at onset before 18 were not confounded with the age of the participant at the time of reporting. This analytic sample included 2,927 participants; 1,598 (54.6%) of these were female.
Measures
Adversities.
Participants were asked whether they had experienced each of 30 specific adverse events representing the five types of adversity described above. Major childhood events included 12 events associated with potentially substantial (but nonviolent) disruption in children's lives (e.g., serious illness or hospitalization, separation from parents, parental unemployment, and parental divorce). Traumas (nine events) involved violence, including rape or sexual assault, physical abuse or attack, or being in a natural disaster or serious accident. Witnessed violence included three events in which the respondent was an observer but not the direct victim of violence; most common was witnessing family violence. Traumatic news (three events) involved significant others in life-threatening situations, being victims of assault, or committing suicide. Turner and Lloyd (2003) found normative experiences with deaths of significant others, mostly grandparents, to be unrelated to risk; we thus focused specifically on nonnormative experiences of loss in childhood, namely death of a parent or sibling.
To separate the potential effects of adversity on the initiation of substance use and onset of SUD from the potential effects of substance use or SUD on adversity, we created prior-adversity variables. Prior adversities were those that first occurred more than 1 year before first use of substances; events first experienced in tandem with or subsequent to the initiation of substance use were counted as non-occurrences for the purposes of our analyses.
Respondents were asked to indicate how old they were when each reported event occurred (or first occurred, if it had happened more than once). We used the age reports to create a five-level ordinal early-adversity variable. This ordinal variable was scored 4 if an event first occurred before 6 years of age (early childhood onset), 3 if the first event was between 6 and 9 years of age (middle childhood onset), 2 if first occurrence was between 10 and 13 years of age (pre-adolescent onset), 1 if adversity first occurred between 14 and 17 years (adolescent onset), and 0 if no adversities were reported before age 18 or none was experienced before initial substance use. This categorization corresponded to major developmental periods and smoothed out trivial variation across specific ages that was likely more attributable to recall error than to precise timing of events. By coding age at onset in this way, we were able to include all participants, whereas use of a discrete age at occurrence would have eliminated those who reported no adversity before age 18 from analyses.
We created six early-adversity variables in this manner. The first represented the timing of first exposure to any adversity; each participant was assigned a score from 0 to 4 that corresponded to the age at their earliest report of any of 30 events. Five additional variables were constructed, one for each of the categories of specific types of adversities. For example, for major childhood events, each participant was given a score of 0 to 4, corresponding to the youngest age reported for any of the 12 events in that category that they had experienced.
Early substance use.
Respondents reported whether they had ever had more than a sip of alcohol or used any of nine different drugs: five illicit substances (cocaine, hallucinogens, heroin, inhalants, and marijuana) and four types of prescription drugs taken without a prescription or in excess of prescribed dose (sedatives, tranquilizers, stimulants, and analgesics). All reports of substance use were followed with a question about the age at first use. As with early adversity, we created an ordinal scale of early substance use. However, because substance use before age 6 was quite rare (n = 44), the youngest two age categories were combined: Substance use beginning before age 9 was coded as 3, between 10 and 13 as 2, between 14 and 17 as 1, and no use before age 18 as 0.
Substance-use disorder.
SUD was assessed using items from the University of Michigan version of the Composite International Diagnostic Interview (World Health Organization, 1990), adapted for use in American Indian communities as a part of a previous study (Beals et al., 2002). This measure allowed assessment of both substance abuse and dependence according to DSM, Fourth edition (American Psychiatric Association, 1994), criteria. These were combined into a single disorder category after analyses showed no significant differences between them in the relationships of interest in this study.
Design and procedure
Institutional review board approval and approval from participating tribes were obtained before project initiation. Written informed consent was obtained from all adult respondents, following complete description of the study; for minors, parental/guardian consent was obtained before requesting adolescent assent. Interviews were computer-assisted and administered by tribal members trained in research and interviewing methods. Extensive quality-control procedures verified that location, recruitment, and interview procedures were conducted in a standardized, reliable manner.
Analyses
Variable construction was completed with SPSS (14.0.1 Edition; SPSS Inc., Chicago, IL) and SAS (9.1 Edition; SAS Institute Inc., Cary, NC). Prevalence estimates were computed in Stata (Special Edition 9.1; Statacorp LP, College Station, TX) using sample and nonresponse weights. Path analyses were estimated in Mplus (Muthén and Muthén, 1998-2006), again accounting for sample and nonresponse weights. Early adversity and early substance use were included as ordinal categorical variables and SUD as a binary categorical variable. Models were fit using a robust weighted least-squares estimator and Delta parameterization. Estimating the path analytic model in Figure 1 allowed us to explicitly test both the direct and indirect effects of tribe, gender, and early adversity on SUD. This method overcomes some of the limitations of Baron and Kenny's causal steps approach (Baron and Kenny, 1986), most notably in increasing power, directly estimating the indirect (mediated) effects, and simultaneously estimating multiple direct and indirect effects (Cheung and Lau, 2008; Mackinnon et al., 2002; Preacher and Hayes, 2004, 2008). It is important to note here that our data are cross-sectional and that, although we use retrospective reports of the timing of adverse experiences and substance use to put them in temporal order, these analyses cannot demonstrate causal relationships among these variables. Our use of the terms direct effects and indirect effects should not be taken to imply causality per se but rather to refer to different types of associations among variables.
Results
Prevalence of adversity, substance use, and substance-use disorder
Table 1 shows the prevalence of adversity, substance use, and SUD symptoms in the analytic sample. Adversity was common in these reservation communities, and the majority of participants were exposed to adversity before their 18th birthdays. Substance use was also common, and most often initiated before age 18. Of those who eventually met criteria for SUD, almost one half (46.3%) first had symptoms before age 18.
Table 1.
Distribution of first occurrences of adversity, substance use, and substance-use-disorder (SUD) symptoms in the American Indian Service Utilization, Psychiatric Epidemiology, Risk and Protective Factors Project sample
| Ever experienced (lifetime exposure) |
Experienced before age 18 |
||||
| Variable | n | % of sample | Mean age at first exposure | n | % of those with lifetime exposure |
| Any adversitya | 2,002 | 68.4 | 7.2 | 1,855 | 92.7 |
| Major childhood event | 1,493 | 51.0 | 7.3 | 1,445 | 96.8 |
| Trauma | 668 | 22.8 | 11.9 | 533 | 79.8 |
| Witnessed violence | 791 | 27.0 | 11.2 | 695 | 87.9 |
| Traumatic news | 325 | 11.1 | 15.8 | 232 | 71.4 |
| Death of significant otheb | 599 | 20.5 | 17.0 | 364 | 60.8 |
| Substance use | 2,503 | 85.5 | 15.2 | 1,921 | 76.7 |
| SUD | 1,061 | 36.2 | 19.7 | 491 | 46.3 |
For adversity, occurrence subsequent to onset of substance use was counted as no occurrence;
only deaths of immediate family members—parents and siblings—were included in this category; more normative experiences with significant deaths, such as those of aging grandparents, were excluded here.
Relationships among early adversity, early substance use, and substance-use disorder
Results from the path analysis depicted in Figure 1 are presented in Table 2. The first group of data columns shows the effects of the exogenous variables (gender, tribe, Gender × Tribe interaction, and early adversity) on early substance use (solid light arrows in Figure 1). As is evident, early adversity was significantly and positively related to early use; the earlier adversity was experienced, the earlier substance use was initiated. The magnitude of this relationship was small, however, particularly in comparison with the relationships of tribe and gender to early use. Being male and being from the Northern Plains tribe were associated with significantly greater risk of early substance use; a Gender × Tribe interaction indicated that the gender difference was less pronounced in the Northern Plains than in the Southwest.
Table 2.
Effect estimates from path analysis with early exposure to any type of adversity (Model 1)
| Outcome: | Early use |
Substance-use disorder |
||||||
| Predictor | B (95% Cl) | Std β | z | p | B (95% Cl) | Std β | z | p |
| Gender (male) | ||||||||
| Direct | 0.62 (0.51, 0.73) | .29 | 10.82 | <.001 | 0.70 (0.55, 0.85) | .32 | 8.99 | <.001 |
| Indirect (via early use) | — | — | — | — | 0.26 (0.21, 0.32) | .12 | 9.16 | <.001 |
| Tribe (Northern Plains) | ||||||||
| Direct | 0.55 (0.44, 0.67) | .26 | 9.45 | <.001 | 0.31 (0.16, 0.45) | .14 | 4.09 | <.001 |
| Indirect (via early use) | — | — | — | — | 0.23 (0.18, 0.29) | .11 | 8.21 | <.001 |
| G × T (Northern Plains male) | ||||||||
| Direct | −0.31 (−0.48, −0.15) | −.13 | −3.73 | <.001 | −0.42 (−0.62, −0.22) | −.17 | −4.07 | <.001 |
| Indirect (via early use) | — | — | — | — | −0.13 (−0.20, −0.06) | −.05 | −3.63 | <.001 |
| Early adversitya | ||||||||
| Direct | 0.10 (0.08, 0.12) | .16 | 8.06 | <.001 | 0.12 (0.09, 0.15) | .19 | 7.77 | <.001 |
| Indirect (via early use) | — | — | — | — | 0.04 (0.03, 0.05) | .06 | 7.26 | <.001 |
| Early useb | — | — | — | — | 0.42 (0.37, 0.47) | .40 | 16.83 | <.001 |
| R2 | .11 | .32 | ||||||
Notes: B = unstandardized estimate; 95% CI = lower and upper bounds of 95% confidence interval; Std β = standardized estimate; z = estimate/standard error; p = probability that true value is 0; G × T = Gender × Tribe.
Scored to reflect the age at first adversity exposure: 0 = not before age 18 or subsequent to onset of substance use, 1 = 14–17 years of age, 2 = 10–13 years of age, 3 = 6–9 years of age, and 4 = before age 6;
0 if no substance use was reported before age 18, 1 if substance use was initiated after age 13 and before age 18, and 2 if it was initiated by age 13.
The second set of data columns in Table 2 shows relationships of gender, tribe, and early adversity with risk for SUD (solid dark arrows, Figure 1); also shown are the indirect effects of these factors on SUD via their relationship with early substance use (dashed arrows, Figure 1). Overall, close to one third of the variance in SUD was explained by this model. SUD was significantly related to early adversity, more strongly related to tribe, and most strongly related to gender (as with early use, a Gender × Tribe interaction qualified these effects). Much of the relationship of these factors to risk for SUD was indirect, through early initiation of substance use. It is notable that the relationship between tribe and SUD was considerably (although not quite significantly) smaller than the relationship between tribe and early use.
Examination of the indirect effects in Table 2 shows that early adversity had a small (β = .06) but significant relationship to SUD through its association with increased risk for earlier substance use. Likewise, both tribe and gender had significant indirect relationships with SUD (β = .11 and .12, respectively). These mediated effects support the hypothesis that some of the relationships of early adversity, tribe, and gender to SUD might be explained by the earlier initiation of substance use associated with these factors.
Despite this evidence of partial mediation, the direct effects remained strong. Early experiences of adversity were associated with increased risk for SUD not only because of earlier substance use but also because of other factors not captured in our model. Early adversity and early substance use had overlapping, but also independent, associations with subsequent SUD. The pattern was similar with regard to effects of tribe and gender; early use explained some of the association between these factors and SUD, but significant association remained when early use was accounted for in the model.
Differential associations between substance-use disorder and specific types of adversity
We tested another model in which we replaced the overall early adversity variable included in Model 1 with the five specific early adversity variables described earlier (Table 3). Three types of adversity emerged as significantly related to SUD in these models: major childhood events, traumas, and witnessed violence. Both direct and indirect relationships between each of these three adversity types and SUD were significant, suggesting partial mediation. Also, as was the case in the analysis of any exposure to adversity, these relationships were small.
Table 3.
Effect estimates from path analysis with specific types of adversity (Model 2)
| Outcome | Early use |
Substance-use disorder |
||||||
| Predictor | B (95% CI) | Std β | z | P | B (95% CI) | Std β | z | P |
| Gender (male) | ||||||||
| Direct | 0.63 (0.52, 0.74) | .30 | 10.89 | <.001 | 0.74 (0.59, 0.90) | .33 | 9.41 | <.001 |
| Indirect (via early use) | — | — | — | — | 0.26 (0.21, 0.32) | .12 | 9.15 | <.001 |
| Tribe (Northern Plains) | ||||||||
| Direct | 0.56 (0.44, 0.67) | .26 | 9.49 | <.001 | 0.32 (0.18, 0.47) | .14 | 4.28 | <.001 |
| Indirect (via early use) | — | — | — | — | 0.23 (0.18, 0.29) | .10 | 8.20 | <.001 |
| G × T (Northern Plains male) | ||||||||
| Direct | −0.32 (−0.49, −0.16) | −.13 | −3.84 | <.001 | −0.45 (−0.65, −0.24) | −.18 | −4.31 | <.001 |
| Indirect (via early use) | — | — | — | — | −0.13 (−0.21, −0.06) | −.05 | −3.73 | <.001 |
| Early adversitya | ||||||||
| Major childhood event | ||||||||
| Direct | 0.04 (0.01, 0.07) | .06 | 3.05 | .002 | 0.07 (0.04, 0.11) | .11 | 4.62 | <.001 |
| Indirect (via early use) | — | — | — | — | 0.02 (0.006, 0.03) | .03 | 3.00 | .003 |
| Trauma | ||||||||
| Direct | 0.06 (0.02, 0.11) | .07 | 3.08 | .002 | 0.08 (0.04, 0.13) | .09 | 3.77 | <.001 |
| Indirect (via early use) | — | — | — | — | 0.03 (0.01, 0.04) | .03 | 3.03 | .002 |
| Witnessed violence | ||||||||
| Direct | 0.06 (0.02, 0.10) | .07 | 2.91 | .004 | 0.08 (0.03, 0.12) | .09 | 3.48 | .001 |
| Indirect (via early use) | — | — | — | — | 0.03 (0.008, 0.04) | .03 | 2.87 | .004 |
| Traumatic news | ||||||||
| Direct | 0.02 (−0.04, 0.08) | .01 | 0.67 | .501 | 0.06 (−0.01, 0.13) | .04 | 1.66 | .098 |
| Indirect (via early use) | — | — | — | — | 0.008 (−0.02, 0.03) | .005 | 0.67 | .501 |
| Untimely significant deaths | ||||||||
| Direct | 0.03 (−0.01, 0.08) | .03 | 1.52 | .129 | 0.03 (−0.03, 0.08) | .02 | 0.92 | .356 |
| Indirect (via early use) | — | — | — | — | 0.01 (−0.004, 0.03) | .01 | 1.51 | .131 |
| Early useb | — | — | — | — | 0.42 (0.37, 0.47) | .40 | 16.56 | <.001 |
| R2 | .11 | .34 | ||||||
Notes: B = unstandardized estimate; 95% CI=lower and upper bounds of 95% confidence interval; Std β = standardized estimate; z = estimate/ standard error; p = probability that true value is 0; G × T = Gender × tribe.
Scored to reflect the age of first adversity exposure: 0 = not before age 18 or subsequent to onset of substance use, 1 = 14–17 years of age, 2 = 10–13 years of age, 3 = 6–9 years of age, and 4 = before age 6;
0 if no substance use was reported before age 18, 1 if substance use was initiated after age 13 and before age 18, 2 if it was initiated between 10 and 13, and 3 if initiation was before age 9.
Discussion
Attempts to account for disparities in SUD between members of American Indian communities and others in the United States have often referenced established links between adversity and SUD, speculating that the high rates of adversity in American Indian communities might explain high rates of SUD. Childhood exposure to adversity has been proposed as a particularly potent risk factor for SUD. We found reports of childhood adversity to be associated with elevated risk of subsequent development of SUD and risk for developing SUD to be inversely related to age at first exposure. These findings are consistent with what we know about child development. Young children have not yet developed the extensive repertoire of personal resources facilitative of coping with critical challenges, and adversities are likely to be more disorganizing for them than they would be for older, more developmentally advanced individuals. Such disorganization may have long-term consequences to the extent that it disrupts basic developmental processes and hampers the emergence of normative cognitive, social, and emotional skills. In addition, the onset of adversity in childhood is likely associated with more prolonged exposure to adversity (e.g., ongoing exposure to family violence) that may also contribute to elevated risk.
We also tested the hypothesis that increased risk for long-term substance-use problems associated with early adversity might be explained by earlier initiation of substance use as a short-term response to such adversity. Our findings suggest that early use explains some, but not all, of the link between early adversity and SUD. Early experiences of adversity were related to early substance use, and early substance use was related to greater risk of SUD. However, although the inclusion of early use in the model attenuated the effects of adversities, it did not eclipse those effects. Other processes were clearly at work in linking early adversity to SUD. Further research is needed—in particular, careful investigation of the developmental processes potentially disrupted by exposure to trauma and their relationship to susceptibility to SUD.
It is important to note here that the size of the effects of early use on SUD are markedly greater (total standardized β = .42) than the size of the effects attributable to early adversity (total standardized β = .25). It is clear, then, that early onset of substance use is a primary target for SUD prevention efforts and that it is important to direct resources toward delaying substance initiation. But knowing that delaying initiation is an important short-term goal does not tell us the best way to accomplish that goal. Our finding that early adversity is one factor associated with greater risk for early initiation becomes important as we consider the targets of and mechanisms for prevention efforts. It provides one piece of the puzzle as to why young adolescents begin using substances too early and suggests that prevention efforts ought to include helping children weather adversity, perhaps providing support and teaching coping skills that will help them deal with stress and trauma in ways that circumvent substance use.
The tribe and gender effects we found were consistent with earlier reports of differential risk for SUD. The significant indirect effects of both of these factors through early use suggests that earlier substance use among those in the Northern Plains tribe and among males accounts for some of the observed disparities in rates of disorder. Future studies will need to focus on cultural and gender differences in susceptibility to both early use and SUD and identify critical targets for intervention.
Different types of adverse experiences had differential relationships to risk for both early substance use and for subsequent SUD. Three categories of events (major childhood events, traumas, and witnessed violence) were consistently associated with increased odds of both early substance use and SUD; two other categories (traumatic news and deaths of immediate family members) were generally not associated with either. It makes sense that major childhood events, traumas, and witnessed violence were associated with increased risk, given the intensity, immediacy, and importance of many of these events. More difficult to explain is the lack of relationship between traumatic news and deaths of parents or siblings and increased risk. We cannot say why traumatic news was not related to increased risk in this American Indian sample although it has been reported to be related in a multiethnic sample (Turner and Lloyd, 2003); it will be important to replicate this finding and to more carefully explore factors related to it.
We did not expect the lack of relationship between loss of parents or siblings during childhood and increased risk for substance use. We expected that, by limiting the category of deaths of significant others to only untimely deaths of parents or siblings (i.e., excluding more normative experiences of grandparent deaths), we might find relationships to risk where Turner and Lloyd did not. This was not the case, however; although such experiences were nonnormative in our sample (reported by 20% of participants, about the same as traumas and much less often than major childhood events, as shown in Table 1), they did not predict increased risk for SUD. One explanation is that this particular kind of adversity may be associated with mental health problems other than SUD (e.g., depression), a possibility we will explore in further analyses of the AI-SUPERPFP data. Alternatively, cultural traditions around deaths may offer support that buffers the effects of this kind of trauma. Such rituals are generally lacking for other traumatic experiences, and comparable support may, in fact, be particularly absent following adverse experiences that are stigmatized (e.g., sexual abuse and family violence). Another explanation is that when either traumatic news or deaths of significant others were reported in childhood (before age 18), the average age at first exposure was later than for major childhood events, traumas, or witnessed violence; later exposure, thus, may help explain the lower risk related to these kinds of events. Clearly, it is important to pay attention to the kinds of stresses faced by children and the resources available for helping children cope with these events. All adversities do not appear to be created equal in terms of their relationship to risk for SUD.
One final finding deserves note, namely that different types of adversities had additive relationships with SUD. The experience of a trauma increased the risk of SUD over and above the risk associated with a major childhood event or with witnessed violence and vice versa. Children exposed to all three types of events were at substantially greater risk of SUD than were children exposed to only one type. Multiple adversities, common in these American Indian communities, appear to be particularly burdensome.
Limitations
The findings presented here contribute substantially to our understanding of the relationship between childhood adversity and subsequent SUD in American Indian populations. Nevertheless, they must be considered in light of their limitations. Limitations in the AI-SUPERPFP sample, study design, and instrumentation have been discussed at length elsewhere (Beals et al., 2003a). Most importantly, although the samples were well defined and justified, they were restricted in cultural representation, age range, and residence. In addition, the cross-sectional design and reliance on retrospective self-reports make these data susceptible to errors associated with the filters of both time and response bias.
Another limitation lies in the fact that the models we tested did not incorporate the number of adversities encountered within each category (e.g., illness and parental divorce), the duration of exposure (e.g., repeated episodes of witnessing family violence throughout childhood), or participants' subjective reports of the significance of experiences. Thus, although our findings suggest an important role of early adversity in subsequent substance-use problems, they likely underestimate the true extent of the association.
Implications
These findings have implications for efforts to reduce SUD disparities among American Indians. First, intervention efforts are likely to be most effective if they focus on delaying initiation of substance use. Second, one potential way to delay initiation is to deal with children's exposure to adversity. A primary goal of public health efforts should be the reduction in children's exposure to adverse events, but such exposure is likely to be somewhat resistant to change. Thus, we must also design interventions to help children to cope with the adversity they will almost inevitably encounter. Prevention efforts should include work with young children—before they are exposed to adversity, if possible—to help shore up their capability for dealing with adverse events and support their successful development despite the challenges presented by such events.
Because early substance use alone did not account for the increased risk of SUD after adversity, it is evident that more research is needed to identify other factors that explain the link. The relationship we found between the timing of adversity and SUD suggests a need to focus on how specific developmental processes are disrupted and how failed development relates to increased risk. The identification of critical developmental problems engendered by adversity and linked to SUD can help direct prevention efforts and ensure brighter futures for children.
Acknowledgments
AI-SUPERPFP would not have been possible without the significant contributions of many people. The following interviewers and computer/data management and administrative staff supplied energy and enthusiasm for an often difficult job: Anna E. Barón, Antonita Begay, Amelia I. Begay, Cathy A.E. Bell, Phyllis Brewer, Nelson Chee, Mary Cook, Helen J. Curley, Mary C. Davenport, Rhonda Wiegman Dick, Marvine D. Douville, Pearl Dull Knife, Geneva Emhoolah, Fay Flame, Roslyn Green, Billie K. Greene, Jack Herman, Tamara Holmes, Shelly Hubing, Cameron Joe, Louise F. Joe, Cheryl L. Martin, Jeff Miller, Robert H. Moran, Natalie K. Murphy, Melissa Nixon, Ralph L. Roanhorse, Margo Schwab, Jennifer Desserich, Donna M. Shangreaux, Matilda J. Shorty, Selena S. S. Simmons, Wileen Smith, Tina Standing Soldier, Jennifer Truel, Lori Trullinger, Arnold Tsinajinnie, Jennifer M. Warren, Intriga Wounded Head, Theresa (Dawn) Wright, Jenny J. Yazzie, and Sheila A. Young. We also acknowledge the contributions of the Methods Advisory Group: Margarita Alegria, Evelyn I. Bromet, Dedra Buchwald, Peter Guarnaccia, Steve G. Heeringa, Ron Kessler, R. Jay Turner, and William A. Vega. Finally, we thank the tribal members who so generously answered all the questions asked of them.
Footnotes
This research was supported by National Institute of Mental Health grants R01 MH48174 (to Spero M. Manson and Janette Beals, principal investigators) and P01 MH42473 (to Spero M. Manson, principal investigator). Analyses for and writing of the article were also supported by the National Institute on Drug Abuse grants R01 DA14817 and R01 DA17803 (to Janette Beals, principal investigator).
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) Washington, DC: 1994. [Google Scholar]
- Aneshensel CS. Outcomes of the stress process. In: Horwitz AV, Scheid TL, editors. A Handbook for the Study of Mental Health: Social Contexts, Theories, and Systems. New York: Cambridge Univ. Press; 1999. pp. 211–227. [Google Scholar]
- Anthony JC, Petronis KR. Early-onset drug use and risk of later drug problems. Drug Alcohol Depend. 1995;40:9–15. doi: 10.1016/0376-8716(95)01194-3. [DOI] [PubMed] [Google Scholar]
- Bachman JG, Johnston LD, O'Malley PM. Monitoring the Future: Questionnaire Responses From the Nation's High School Seniors, 1998. Ann Arbor, MI: Institute of Social Research, University of Michigan; 2001. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Pers. Social Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beals J, Manson SM, Mitchell CM, Spicer P the AI-SUPERPFP Team. Cultural specificity and comparison in psychiatric epidemiology: Walking the tightrope in American Indian research. Cult. Med. Psychiat. 2003a;27:259–289. doi: 10.1023/a:1025347130953. [DOI] [PubMed] [Google Scholar]
- Beals J, Manson SM, Shore JH, Friedman M, Ashcraft M, Fairbank JA, Schlenger WE. The prevalence of posttraumatic stress disorder among American Indian Vietnam veterans: Disparities and context. J. Traumat. Stress. 2002;15:89–97. doi: 10.1023/A:1014894506325. [DOI] [PubMed] [Google Scholar]
- Beals J, Novins DK, Whitesell NR, Spicer P, Mitchell CM, Man-son SM the AI-SUPERPFP Team. Prevalence of mental disorders and utilization of mental health services in two American Indian reservation populations: Mental health disparities in a national context. Amer. J. Psychiat. 2005;162:1723–1732. doi: 10.1176/appi.ajp.162.9.1723. [DOI] [PubMed] [Google Scholar]
- Beals J, Spicer P, Mitchell CM, Novins DK, Manson SM the AI-SUPERPFP Team. Racial disparities in alcohol use: Comparison of 2 American Indian reservation populations with national data. Amer. J. Publ. Hlth. 2003b;93:1683–1685. doi: 10.2105/ajph.93.10.1683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauvais F. American Indians and alcohol. Alcohol Hlth Res. World. 1998;22:253–259. [PMC free article] [PubMed] [Google Scholar]
- Brennan PL, Schutte KK, Moos RH. Reciprocal relations between stressors and drinking behavior: A three-wave panel study of late middle-aged and older women and men. Addiction. 1999;94:737–749. doi: 10.1046/j.1360-0443.1999.94573712.x. [DOI] [PubMed] [Google Scholar]
- Center for Mental Health Services. Mental Health: Culture, Race, and Ethnicity. A Supplement to Mental Health: A Report of the surgeon general, DHHS Publication No. (SMA) 01-3613. Rockville, MD: Substance Abuse and Mental Health Services Administration, Public Health Service, Department of Health and Human Services; 2001. [PubMed] [Google Scholar]
- Cheung GW, Lau RS. Testing mediation and suppression effects of latent variables: Bootstrapping with structural equation models. Organ. Res. Meth. 2008;11:296–325. [Google Scholar]
- Chilcoat HD, Menard C. Epidemiological investigations: Comorbidity of posttraumatic stress disorder and substance use disorder. In: Ouimette P, Brown PJ, editors. Trauma and Substance Abuse: Causes, Consequences and Treatment of Comorbid Disorders. Washington, DC: American Psychological Assn; 2003. pp. 9–28. [Google Scholar]
- Conger JJ. Alcoholism: Theory, problem and challenge: II. Reinforcement theory and the dynamics of alcoholism. Q.J. Stud. Alcohol. 1956;17:296–305. [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Ruan WJ. The association between stress and drinking: Modfiying effects of gender and vulnerability. Alcohol Alcsm. 2005;40:453–460. doi: 10.1093/alcalc/agh176. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP. The role of adversity and stress in psychopathology: Some evidence and its implications for theory and research. J. Hlth Social Behav. 2000;41:1–19. [PubMed] [Google Scholar]
- Foshee VA, Ennett ST, Bauman KE, Granger DA, Benefield T, Suchindran C, Hussong AM, Karriker-Jaffe KJ, DuRant RH. A test of biosocial models of adolescent cigarette and alcohol involvment. J. Early Adolesc. 2007;27:4–39. doi: 10.1177/0272431606294830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins EH, Cummins LH, Marlatt GA. Preventing substance abuse in American Indian and Alaska Native youth: Promising strategies for healthier communities. Psychol. Bull. 2004;130:304–323. doi: 10.1037/0033-2909.130.2.304. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: Implications for substance use prevention. Psychol. Bull. 1992;112:64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- Hingson RW, Heeren T, Edwards EM. Age at drinking onset, alcohol dependence, and their relation to drug use and dependence, driving under the influence of drugs, and motor-vehicle crash involvement because of drugs. J. Stud. Alcohol Drugs. 2008;69:192–201. doi: 10.15288/jsad.2008.69.192. [DOI] [PubMed] [Google Scholar]
- Hisnanick JJ. The prevalence of alcohol abuse among American Indians and Alaska Natives. Hlth Values: J. Hlth Behav. Educ. Promot. 1992;16:32–37. [Google Scholar]
- Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychol. Med. 1997;27:1101–1119. doi: 10.1017/s0033291797005588. [DOI] [PubMed] [Google Scholar]
- Koss MP, Yuan NP, Dightman D, Prince RJ, Polacca M, Sanderson B, Goldman D. Adverse childhood exposures and alcohol dependence among seven Native American Tribes. Amer. J. Prev. Med. 2003;25:238–244. doi: 10.1016/s0749-3797(03)00195-8. [DOI] [PubMed] [Google Scholar]
- Kunitz SJ. Risk factors for polydrug use in a Native American population. Subst. Use Misuse. 2008;43:331–339. doi: 10.1080/10826080701202783. [DOI] [PubMed] [Google Scholar]
- Kunitz SJ, Gabriel KR, Levy JE, Henderson E, Lampert K, McCloskey J, Quintero G, Russell S, Vince A. Alcohol dependence and conduct disorder among Navajo Indians. J. Stud. Alcohol. 1999;60:159–167. doi: 10.15288/jsa.1999.60.159. [DOI] [PubMed] [Google Scholar]
- Kunitz SJ, Levy JE. Drinking Careers: A twenty-Five-Year Study of Three Navajo populations. New Haven, CT: Yale Univ. Press; 1994. [Google Scholar]
- LeMaster PL, Connell CM, Mitchell CM, Manson SM. Tobacco use among American Indian adolescents: Protective and risk factors. J. Adolesc. Hlth. 2002;30:426–432. doi: 10.1016/s1054-139x(01)00411-6. [DOI] [PubMed] [Google Scholar]
- Libby AM, Orton HD, Novins DK, Spicer P, Buchwald D, Beals J, Manson SM the AI-SUPERPFP Team. Childhood physical and sexual abuse and subsequent alcohol and drug use disorders in two American-Indian tribes. J. Stud. Alcohol. 2004;65:74–83. doi: 10.15288/jsa.2004.65.74. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol. Meth. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manson SM, Beals J, Klein SA, Croy CD. Social epidemiology of trauma among 2 American Indian reservation populations. Amer. J. Publ. Hlth. 2005;95:851–859. doi: 10.2105/AJPH.2004.054171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May PA. Overview of alcohol abuse epidemiology for American Indian populations. In: Sandefur GD, Rindfuss RR, Cohen B, editors. Changing Numbers, Changing Needs: American Indian Demography and Public Health. Washington, DC: National Academies Press; 1996. pp. 235–261. [PubMed] [Google Scholar]
- May PA, Gossage JP. New data on the epidemiology of adult drinking and substance use among American Indians of the northern states: Male and female data on prevalence, patterns, and consequences. Amer. Indian Alaska Nat. Ment. Hlth Res. 2001;10:1–26. doi: 10.5820/aian.1002.2001.1. [DOI] [PubMed] [Google Scholar]
- Mitchell CM, Beals J, Novins DK, Spicer P the AI-SUPERPFP Team. Drug use among two American Indian populations: Prevalence of lifetime use and DSM-IV substance disorders. Drug Alcohol Depend. 2003;69:29–41. doi: 10.1016/s0376-8716(02)00253-3. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User's Guide, Version 4th. Los Angeles, CA: Muthén & Muthén; 1998–2006. [Google Scholar]
- National Institutes of Health. Strategic Research Plan and Budget to Reduce and Ultimately Eliminate Health Disparities, Fiscal Years 2002–2006. Bethesda, MD: National Institutes of Health, Department of Health and Human Services; 2002. [Google Scholar]
- Norton IM, Manson SM. Research in American Indian and Alaska Native communities: Navigating the cultural universe of values and process. J. Cons. Clin. Psychol. 1996;64:856–860. doi: 10.1037//0022-006x.64.5.856. [DOI] [PubMed] [Google Scholar]
- Novins DK, Barón AE. American Indian adolescent substance use: The hazards for substance use initiation and progression for adolescents aged 14 to 20. J. Amer. Acad. Child Adolesc. Psychiat. 2004;43:316–324. doi: 10.1097/00004583-200403000-00013. [DOI] [PubMed] [Google Scholar]
- Oetting ER, Beauvais F. Epidemiology and correlates of alcohol use among Indian adolescents living on reservations. In: Spiegler DL, Tate DA, Aitken SS, Christian CM, editors. Alcohol Use Among U.S. Ethnic Minorities. NIAAA Research Monograph No. 18, DHHS Publication No. ADM 89–1435. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 1989. pp. 239–267. [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav. Res. Meth. Instr. Comput. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Meth. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Robin RW, Chester B, Rasmussen JK, Jaranson JM, Goldman D. Prevalence and characteristics of trauma and posttraumatic stress disorder in a southwestern American Indian community. Amer. J. Psychiat. 1997a;154:1582–1588. doi: 10.1176/ajp.154.11.1582. [DOI] [PubMed] [Google Scholar]
- Robin RW, Chester B, Rasmussen JK, Jaranson JM, Goldman D. Prevalence, characteristics, and impact of childhood sexual abuse in a Southwestern American Indian tribe. Child Abuse Negl. 1997b;21:769–787. doi: 10.1016/s0145-2134(97)00038-0. [DOI] [PubMed] [Google Scholar]
- Robin RW, Rasmussen JK, Gonzalez-Santin E. Impact of childhood out-of-home placement on a Southwestern American Indian Tribe. J. Human Behav. Social Environ. 1999;2:69–89. [Google Scholar]
- Robins LN, Przybeck TR. Age of onset of drug use as a factor in drug and other disorders. In: Jones CL, Battjes RJ, editors. Etiology of Drug Abuse: Implications For Prevention: NIDA Research Monograph No. 56, DHHS Publication No. (ADM) 85–1335. Washington: Government Printing Office; 1985. pp. 178–192. [PubMed] [Google Scholar]
- Rodgers KB, Fleming WM. Individual, family, and community factors related to Alcohol use among Native American adolescents. Adolesc. Fam. Hlth. 2003;3:140–147. [Google Scholar]
- Spooner C. Causes and correlates of adolescent drug abuse and implications for treatment. Drug Alcohol Rev. 1999;18:453–475. [Google Scholar]
- Stewart SH, Conrod PJ. Psychosocial models of functional associations between posttraumatic stress disorder and substance use disorder. In: Ouimette P, Brown PJ, editors. Trauma and Substance Abuse: Causes, Consequences and Treatment of Comorbid Disorders. Washington, DC: American Psychological Assn; 2002. pp. 29–55. [Google Scholar]
- Stueve A, O'Donnell LN. Early alcohol initiation and subsequent sexual and alcohol risk behaviors among urban youths. Amer. J. Publ. Hlth. 2005;95:887–893. doi: 10.2105/AJPH.2003.026567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tschann JM, Adler NE, Irwin CE, Millstein SG, Turner RA, Kegeles SM. Initiation of substance use in early adolescence: The roles of pubertal timing and emotional distress. Hlth Psychol. 1994;13:326–333. doi: 10.1037//0278-6133.13.4.326. [DOI] [PubMed] [Google Scholar]
- Turner RJ, Lloyd DA. Lifetime traumas and mental health: The significance of cumulative adversity. J. Hlth Social Behav. 1995;36:360–376. [PubMed] [Google Scholar]
- Turner RJ, Lloyd DA. Cumulative adversity and drug dependence in young adults: Racial/ethnic contrasts. Addiction. 2003;98:305–315. doi: 10.1046/j.1360-0443.2003.00312.x. [DOI] [PubMed] [Google Scholar]
- Vega WA, Aguilar-Gaxiola S, Andrade L, Bijl R, Borges G, Cara-veo-Anduaga JJ, DeWit DJ, Heeringa SG, Kessler RC, Kolody B, Merikangas KR, Molnar BE, Walters EE, Warner LA, Wittchen H-U. Prevalence and age of onset for drug use in seven international sites: Results from the international consortium of psychiatric epidemiology. Drug Alcohol Depend. 2002;68:285–297. doi: 10.1016/s0376-8716(02)00224-7. [DOI] [PubMed] [Google Scholar]
- Wallace JM, Jr, Bachman JG, O'Malley PM, Johnston LD, Schulenberg JE, Cooper SM. Tobacco, alcohol, and illicit drug use: Racial and ethnic differences among U.S. high school seniors, 1976–2000. Publ. Hlth Rep. 2002;117(Suppl. No. 1):S67–S75. [PMC free article] [PubMed] [Google Scholar]
- Walters KL, Simoni JM, Evans-Campbell T. Substance use among American Indians and Alaska Natives: Incorporating culture in an "in-digenist" stress-coping paradigm. Publ. Hlth Rep. 2002;117(Suppl. No. 1):S104–S117. [PMC free article] [PubMed] [Google Scholar]
- Warner LA, White HR, Johnson V. Alcohol initiation experiences and family history of alcoholism as predictors of problem-drinking trajectories. J. Stud. Alcohol Drugs. 2007;68:56–65. doi: 10.15288/jsad.2007.68.56. [DOI] [PubMed] [Google Scholar]
- Westling E, Andrews JA, Hampson SE, Peterson M. Pubertal timing and substance use: The effects of gender, parental monitoring, and deviant peers. J. Adolesc. Hlth. 2008;42:555–563. doi: 10.1016/j.jadohealth.2007.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitbeck LB, Yu M, Johnson KD, Hoyt DR, Walls ML. Diagnostic prevalence rates from early to mid-adolescence among indigenous adolescents: First results from a longitudinal study. J. Amer. Acad. Child adolesc. Psychiat. 2008;47:890–900. doi: 10.1097/CHI.0b013e3181799609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitesell NR, Beals J, Mitchell CM, Keane EM, Spicer P, Turner RJ the AI-SUPERPFP Team. The relationship of cumulative and proximal adversity to onset of substance dependence symptoms in two American Indian communities. Drug Alcohol Depend. 2007a;91:279–288. doi: 10.1016/j.drugalcdep.2007.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitesell NR, Beals J, Mitchell CM, Novins DK, Spicer P, Manson SM the AI-SUPERPFP Team. Latent class analysis of substance use: Comparison of two American Indian reservation populations and a national sample. J. Stud. Alcohol. 2006;67:32–43. doi: 10.15288/jsa.2006.67.32. [DOI] [PubMed] [Google Scholar]
- Whitesell NR, Beals J, Mitchell CM, Novins DK, Spicer P, O'Connell J, Manson SM. Marijuana initiation in 2 American Indian reservation communities: Comparison to a national sample. Amer. J. Publ. Hlth. 2007b;97:1311–1318. doi: 10.2105/AJPH.2005.071266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitesell NR, Beals J, Mitchell CM, Spicer P, Novins DK, Manson SM the AI-SUPERPFP Team. Disparities in drug use and disorder: Comparison of two American Indian reservation communities and a national sample. Amer. J. Orthopsychiat. 2007c;77:131–141. doi: 10.1037/0002-9432.77.1.131. [DOI] [PubMed] [Google Scholar]
- Wichstrom L. The impact of pubertal timing on adolescents' alcohol use. J. Res. Adolesc. 2001;11:131–150. [Google Scholar]
- Widom CS, Weiler BL, Cottler LB. Childhood victimization and drug abuse: A comparison of prospective and retrospective findings. J. Cons. Clin. Psychol. 1999;67:867–880. doi: 10.1037//0022-006x.67.6.867. [DOI] [PubMed] [Google Scholar]
- Windle M, Spear LP, Fuligni AJ, Angold A, Brown JD, Pine D, Smith GT, Giedd J, Dahl RE. Transitions into underage and problem drinking: Developmental processes and mechanisms between 10 and 15 years of age. Pediatrics. 2008;121(Suppl. No. 4):S273–S289. doi: 10.1542/peds.2007-2243C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witt ED. Puberty, hormones, and sex differences in alcohol abuse and dependence. Neurotoxicol. Teratol. 2007;29:81–95. doi: 10.1016/j.ntt.2006.10.013. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Composite International Diagnostic Interview (CIDI), Version 1.0. Geneva, Switzerland: World Health Organization; 1990. [Google Scholar]
- York JL, Welte J, Hirsch J, Hoffman JH, Barnes G. Association of age at first drink with current alcohol drinking variables in a national general population sample. Alcsm Clin. Exp. Res. 2004;28:1379–1387. doi: 10.1097/01.alc.0000139812.98173.a4. [DOI] [PubMed] [Google Scholar]