Abstract
Objective To provide quantitative evaluations on the association between income inequality and health.
Design Random effects meta-analyses, calculating the overall relative risk for subsequent mortality among prospective cohort studies and the overall odds ratio for poor self rated health among cross sectional studies.
Data sources PubMed, the ISI Web of Science, and the National Bureau for Economic Research database.
Review methods Peer reviewed papers with multilevel data.
Results The meta-analysis included 59 509 857 subjects in nine cohort studies and 1 280 211 subjects in 19 cross sectional studies. The overall cohort relative risk and cross sectional odds ratio (95% confidence intervals) per 0.05 unit increase in Gini coefficient, a measure of income inequality, was 1.08 (1.06 to 1.10) and 1.04 (1.02 to 1.06), respectively. Meta-regressions showed stronger associations between income inequality and the health outcomes among studies with higher Gini (≥0.3), conducted with data after 1990, with longer duration of follow-up (>7 years), and incorporating time lags between income inequality and outcomes. By contrast, analyses accounting for unmeasured regional characteristics showed a weaker association between income inequality and health.
Conclusions The results suggest a modest adverse effect of income inequality on health, although the population impact might be larger if the association is truly causal. The results also support the threshold effect hypothesis, which posits the existence of a threshold of income inequality beyond which adverse impacts on health begin to emerge. The findings need to be interpreted with caution given the heterogeneity between studies, as well as the attenuation of the risk estimates in analyses that attempted to control for the unmeasured characteristics of areas with high levels of income inequality.
Introduction
Empirical studies have attempted to link income inequality with poor health, but recent systematic reviews have failed to reach a consensus because of mixed findings. The stakes in the debate are high because many developed countries have experienced a surge in income inequality during the era of globalisation, and if economic inequality is truly damaging to health, then even a “modest” association can amount to a considerable population burden. More than three quarters of the countries belonging to the Organisation for Economic Cooperation and Development (OECD) have in fact experienced a growing gap between rich and poor during the past two decades.1
Income inequality could damage health through two pathways. Firstly, a highly unequal society implies that a substantial segment of the population is impoverished, and poverty is bad for health. Secondly, and more contentiously, income inequality is thought to affect the health of not just the poor, but the better off in society as well. The so called spillover (or contextual) effects of inequality have in turn been attributed to the psychosocial stress resulting from invidious social comparisons,2 3 as well as the erosion of social cohesion.4 The public health importance and burden of income inequality are obviously broader under the second scenario.4 5 6 7 8
We sought to provide quantitative evaluations of the income inequality hypothesis by conducting a meta-analysis of prospective cohort studies and cross sectional studies on the association of income inequality with mortality and self rated health. We also quantitatively evaluated the potential factors explaining the differences between studies—for example, the “threshold effect” hypothesis posits the existence of a threshold of income inequality beyond which adverse impacts on health begin to emerge.4
Methods
Study selection
We followed published guidelines for meta-analyses of observational studies.9 Use of multilevel data (that is, simultaneous consideration of individual income as well as the distribution of income across area units within which individuals reside) is essential for testing the contextual effect of income inequality. As Subramanian and Kawachi have argued,4 only multilevel data can properly distinguish the contextual health effects of income inequality from the effect of individual income.10
In our meta-analysis we included cohort studies on the association between income inequality and mortality or cross sectional studies on the association between income inequality and self reported health. To be included studies had to use multilevel data—at least two levels including one or more region variable(s); address sample clustering caused by multilevel data structure; adjust for age, sex, and individual socioeconomic status; and be peer reviewed. We selected mortality and self rated health as health outcomes because these were the most commonly used validated indicators of health.11 In most cases self rated health was measured on a Likert scale with questions on respondents’ perceived health—for example, “Would you say that in general your health is: excellent, very good, good, fair, or poor?”w21 We also included in our sensitivity analysis two cohort analyses that did not address sample clustering.w11 w12
A researcher trained in online article searches (NK) searched papers written in any language published between January 1995 and July 2008, using PubMed, ISI Web of Science (Thomson Reuters), and the National Bureau of Economic Research database using the following keywords: “inequalit(y/ies)”, “income”, “Gini”, “mortality”, “death”, and “health”. The terms “dental”, “human right(s)”, and “screening” were used to exclude clearly irrelevant articles. We restricted the search period because a previous study found no multilevel study investigating the income inequality hypothesis published before 1996.4 We also reviewed all papers cited by the most recent systematic review by Wilkinson and Pickett,7 which covered all articles reviewed by other systematic reviews.4 6 12 We also reviewed expert suggestions.
Data extraction
Two investigators (NK and GS) independently extracted information on study design, data sources, country of data origin, sample size, number of cases, age, sex, estimations, response rate, follow-up rate, follow-up duration, measure of income inequality, outcome, outcome specifications (binary or ordinal/number of self rated health items), area unit over which income inequality was evaluated, adjustment variables, statistical modelling strategies, and methods for addressing data clustering. We resolved discrepancies between the data abstracted by the two investigators. If necessary, we contacted authors to obtain missing information on exact sample sizes,w3 signs of estimations,w7 distributions of income inequality measures,w30 and response rates.w14 If a cross sectional study pooled data from multiple years, we selected the models adjusted for years for which year adjusted models were available as we needed to have the estimate averaged throughout the period observed. When a paper reported multiple models with different income inequality measures, we selected the analyses using Gini coefficient, the most commonly used measure of income inequality (see box).
Gini coefficient
The Gini coefficient is formally defined as half of the arithmetic average of the absolute differences between all pairs of incomes within the sample, with the total then being normalised on mean income. If incomes are distributed completely equally, the value of the Gini will be zero. If one person has all the income (complete inequality) the Gini will assume a value of 1.
Standardisation of income inequality measures and effect size
Some studies used other measures of income inequality; as alternative measures are all highly correlated (Pearson’s r >0.94), according to Kawachi et al,13 we transformed all measures to Gini coefficients. The alternative measures included median share, the percentages of the total area income received by residents with incomes below the median, and the decile ratio—the ratio of incomes of people at the 90th and 10th centiles of an income distribution. The data for converting the effect sizes by median share and decile ratio into those comparable with Gini were the following: US state Gini by US Census Bureau14 for Fiscella and Peterw7 w8 and Backlund et al,w10 the ratio of standard deviations between Gini and median share reported by Kawachi and Kennedy13 for Mcleod et al,w29 and Norway region Gini by Dahl et al15 for Osler et alw1 (given similar Ginis between Denmark and Norway reported by the Luxembourg Income Study).16
As the specifications of effect estimates varied across studies (based on categories or per unit increase in Gini), we standardised them so that they represented effects per 0.05 unit increase in Gini (about equivalent to 2.0-2.5 SD of the US state Gini).14 For studies providing estimates according to Gini categories, we calculated the standardised estimates using generalised least squares.17 We estimated the midpoints of open ended top and bottom Gini categories, adopting the ratios of intervals among the categories that were reported by other articles using the same or similar data from the same country. When such reference articles were not available, we alternatively estimated the midpoints using regression equations created by the multiple Gini centiles reported in the same article.
Statistical analysis
We estimated the overall relative risk for subsequent mortality among cohort studies and the overall odds ratio for poor self rated health among cross sectional studies per 0.05 unit increase in Gini coefficient. Because our preliminary meta-analyses found significant heterogeneity between studies, we used a random effects approach with a restricted maximum likelihood estimate, incorporating an estimate of variation between studies into the calculation of the common effect.18 I2 statistics and Cochran Q test evaluated the heterogeneity.19 20
Then, using a meta-regression approach with random effects models we evaluated potential factors hypothesised to account for the heterogeneity between studies—that is, potential thresholds of the Gini coefficient (dichotomised at the median 0.3),4 study region (the United States versus other countries),4 6 the length of follow-up (<7 versus ≥7 years, dichotomised at the median), the incorporation of time lags between income inequality and health outcomes,21 22 23 the age range of the subjects (<60 versus ≥60),w1024 and whether the study was between countries versus within one country. We further examined the differences in statistical modelling approaches—that is, the models controlling for regional dummies to adjust for unobserved confounding factors, as well as the adjustment for average area income.22 25 26 27 Additional potential sources of heterogeneity evaluated included data period (<1990 versus 1990 or later), alternative income inequality measures (Gini versus median share), and adjustment for area income. We separately conducted a meta-analysis for the four cross sectional studies using ordinal regressionw8 w29-31 because effect estimates based on dichotomous and ordinal models were not directly comparable. An estimate using an ordinal probit regressionw31 was converted into values comparable with logistic estimates, according to Lipsey and Wilson.28
Next, to evaluate if the result of our meta-analysis was consistent regardless of the inclusion of specific models that have potential problems in being synthesised, we conducted a sensitivity analysis. For example, we compared the models that included and excluded the papers not considering sample clustering.w11 w12 We also examined alternative sets of models—for example, those controlling for area income (six studies)w1-4 w6 w9 and those controlling for unmeasured regional characteristics through fixed effects (three studies).w3 w6 w10
A meta-analysis substituting three modelsw3 w6 w10 with their region adjusted alternatives further evaluated the effect of adjusting for unmeasured regional characteristics. In addition, we used funnel plots to detect publication bias and Begg’s and Egger’s tests to measure funnel plot asymmetry.29 30
Finally, we estimated the potential national impacts of income inequalities on mortality in every OECD country based on thresholds suggested. We used Stata release 10 (Statacorp, TX, USA) for all analyses.
Results
From the 2839 potentially relevant articles identified, we excluded 2679 because they were outside the scope of this review. Among the 160 remaining papers, 54 articles had multilevel data on income inequality and mortality or self rated health. We excluded five papers without sufficient statistical information,22 25 31 32 33 12 with duplicate data,21 23 34 35 36 37 38 39 40 41 42 43 eight with non-comparable modelling strategies (such as using continuous outcomes or alternative statistical approaches),22 25 44 45 46 47 48 49 and one article not controlling for individual socioeconomic status.50 Finally, nine cohort and 19 cross sectional data matched our inclusion criteria, covering 59 509 857 cohort and 1 280 211 cross sectional individuals (tables 1, 2, and 3 ). The cohort studies included six countries: Denmark, Finland, Norway, New Zealand, and the US,w1-10 and the cross sectional studies included six countries: Canada, Chile, China, Japan, the United Kingdom and the USw8 w13-31 with the three using multiple country data.w26-27 Sixteen cross sectional studies used binary logistic regressions, dichotomising five self rated health items into poor versus better health,w13-19 w21-28 while four studiesw8 w29-31 used ordinal and one used a multinomial logistic model.w20 All studies used sample or census data representative of their target populations (country/countries or regions) and all cohort studies identified mortality using death registers. Response rates were 64% or higher.
Table 1.
Characteristics of selected cohort studies on association between income inequality and mortality
| Details of study | Age (years) | Follow-up (years) | Outcome (No of events) | Measure of income inequality | Area level variable | Adjusted variables in primary models other than age and sex | |
|---|---|---|---|---|---|---|---|
| Eligible papers | |||||||
| Osler et al, 2002w1 | Copenhagen City Heart Study, Glostrup Population Study (CCHS/GPS) 1976-8/1964-92 (n=28 131), Copenhagen, Denmark | ≥20 | 3-28 | All cause mortality, confirmed by national population register (n=7567) | Median share* | 149 parishes | Income |
| Blomgren et al, 2004w2 | Census 1990 (n=1.08 million men),* Finland | 25-64 | 6 | Alcohol related disease mortality, confirmed by death register (n=9820) | Gini | 84 NUT4 regions | Income, education, occupational status, and mother tongue |
| Kravdal, 2008w3 | Census 1980-2002 (n=54.31 million), Norway | 30-79 | 1-22 | All cause mortality, confirmed by population database (n=513 746) | Gini | 431 municipalities | Income, education, mean area income, and data year |
| Blakely et al, 2003w4 | Census 1991 (n=1 391 118), New Zealand | 25-64 | 3 | All cause mortality, confirmed by mortality record (n=19 128) | Gini | 35 sub-regions | Income, mean area income, and rural residency |
| Henriksson et al, 2006w5 | Census 1990 (n=1 578 186), Sweden | 40-64 | 2-7 | All cause mortality, confirmed by national cause of death register (n=49 782) | Gini | 170 parities/municipalities | Occupational position |
| Gerdtham and Johannesson, 2004w6 | Survey of Living Conditions 1980-6 (n=41 006), Sweden | 20-84 | 10-16 | All cause mortality, confirmed by national cause of death register (n=6725, 16.4% of total) | Gini | 24 counties/284 municipalities | No of children, immigrant, marital status, income, education, employment status, functional limitations, self rated health, high blood pressure, data year, urbanisation, and mean area income |
| Fiscella and Peter, 1997 w7/2000w8 | NHANES I Epidemiologic Follow-up Study (NHEFS) 1971-5 (n=13 280), US | 25-74 | 2-16 | All cause mortality, confirmed by medical records and death certificates (n=1992, 15% of total) | Median share* | 105 primary sampling units | Income and family size. Morbidity, depression, and baseline self rated health are adjusted only in primary model |
| Lochner et al, 2001w9 | National Health Interview Survey (NHIS) 1987-94 (n=546 888), US | 18-74 | 1-6 | All cause mortality, confirmed by the National Death Index (n=19 379) | Gini | 48 states | Race/ethnicity, marital status, income, and poverty rate |
| Backlund et al, 2007w10 | National Longitudinal Mortality Study (NLMS) 1979-85 (n=521 248), US | ≥25 | 4.75-10.75 | All cause mortality, confirmed by the National Death Index (n=19 049) | Median share* | 50 states | Household size, marital status, race, Hispanic origin, family income, education, employment status, and urbanisation |
| Studies not addressing data clustering (for sensitivity analysis only) | |||||||
| Daly et al, 1998w11 | Panel Study of Income Dynamics 1978-88 (sample size not reported), US | ≥25 | 5 | All cause mortality, reported by the next year survey (n=716) | Median share* | 50 states | Race, family size, and median area income |
| Kahn et al, 1999w12 | Cancer Prevention Study II 1982 (n=76 628 men),‡ US | 30-74 | 14 | All cause mortality, confirmed by the death certificates (n=15 439) | 90/10 ratio | 318 standard metro areas | Education |
*Median share—that is, % of income sum below median in total area income.
Table 2.
Characteristics of selected cross sectional studies on association between income inequality and self rated health (SRH) in studies with binary or multinomial outcome
| Details of study | Age (years) | Outcome (No of cases) | Measure of income inequality | Area level variable | Lag (years)* | Adjusted variables in primary models other than age and sex | |
|---|---|---|---|---|---|---|---|
| Xi and McDowell, 2005w13 | Ontario Health Survey (OHS), 1996-7 (n=30 820), Ontario, Canada | ≥25 | Lower 2 of 5 SRH items (n=3945) | Gini | 42 public health units | 0 | Marital status, income, education, smoking, and regular exercise |
| Subramanian et al, 2003w14 | National Socioeconomic Characterization Survey (NSCS), 2000 (n=98 344), Chile | 15-99 | Lower 2 of 5 SRH items (n=8513) | Gini | 68 communities | 0 | Marital status, ethnicity, income, education, type of health insurance, employment status, urban residency, median area income. |
| Pey and Rodriduez, 2006w15 | China Health and Nutrition Survey (CHNS), 1991/1993/1997 (n=9594), China | ≥18 | Lower 2 of 4 SRH items (n=2753) | Gini | 9 provinces | 5 | Marital status, income, education, rural residency, health insurance |
| Ichida et al, 2005w16 | Aichi Gerontological Evaluation Study, 2003 (n=12 775), Aichi, Japan | ≥65 | Lower 2 of 5 SRH items (n=3628) | Gini | 25 communities | 0 | Income, education, marital status, mean area income |
| Shibuya et al, 2002w17 | Comprehensive survey of living conditions of people on health and welfare (LCPHW), 1995 (n=80 899), Japan | ≥16 | Lower 2 of 5 SRH items (n=7928) | Gini | 46 prefectures | 0 | Marital status, income, health check up, median area income, regional block dummies |
| Craig, 2005w18 | Scottish Household Survey (SHS), 1999-2000 (n=18 466), Scotland | 16-64 | Lower 2 of 3 SRH items (n=8126) | Gini | 32 local authorities | 0 | Income, employment status, education, mean area income |
| Weich et al, 2002w19 | British Household Panel Survey (BHPS), 1991 (n=8366), UK | 16-75 | Lower 2 of 5 SRH items (n=653) | Gini | 18 regions | 0 | Ethnicity, income, education, employment status, housing tenure, social class by head of household |
| Lopez, 2004w20 | Behavioural risk factor surveillance system (BRFSS), 1993-4 (n=108 661), US | ≥18 | Lower 2 of 5 SRH items v higher 2 items (n=15 669)† | Gini | Metro areas | 0 | Race/ethnicity, income, education, smoking, area per capita income |
| Kennedy et al, 1998w21 | Behavioural risk factor surveillance system (BRFSS), 2000 (n=205 245), US | ≥18 | Lower 2 of 5 SRH items (n=29 679) | Gini | 50 states | 2-4 | Race, income |
| Subramanian and Kawachi, 2003 w22/ Blakely and Kawachi, 2001w23 | Current Population Survey (CPS), 1995/1997 (n=213 965 or 185 479), US | ≥18 | Lower 2 of 5 SRH items (n=30 009 or 16 281) | Gini | 50 states or 232 metro areas | 6-10 or 6-8 | Race, income, mean area income |
| Shi and Starfield, 2000w24 | Community Tracking Study (CTS), 1995 (n=58 885), US | 17-65 | Lower 2 of 5 SRH items (n=7699) | Gini | 50 states | 0 | Race, hourly wage, education, paid work, employment type, poverty level, health insurance, physical health status, smoking habits, area primary care resource level |
| Kahn et al, 2000w25 | National Maternal Infant Health Survey (NMIHS), 1988 (n=7889 women), US | ≥15 | Lower 2 of 5 SRH items (n=781) | Gini | 50 states | 3 | Marital status, race/ethnicity, household size, income, education |
| Bobak et al, 2000w26 | New Democracies Barometer, New Baltic Barometer, New Russia Barometer, 1996/1998 (n=5330), East Europe | 20-60 | Lower 2 of 5 SRH items (n=713) | Gini | 7 nations | 0 | Marital status, education |
| Bobak et al, 2007w27 | New Europe Barometer (NEB), 2004 (n=15 331), Middle and East Europe | ≥18 | Lower 2 of 5 SRH items (n=1836) | Gini | 13 nations | 0 | Marital status, income, education, number of household items |
| Torshemi et al, 2006w28 | WHO collaborative health behaviour in school aged children (CHBSAC), 1997-8 (n=120 381 children), Multiple countries | 6,8, 10 | Lowest 1 of 3 SRH items (n=7258) | Gini | 27 nations | 0 | Family affluence, parental emotional support, parental school involvement, family structure |
*Time lags between data on income inequality and health outcome.
†Multinomial logistic regression with contrast of fair/poor v excellent/very good health (items: excellent, very good, good, fair, poor).
Table 3.
Characteristics of selected cross sectional studies on association between income inequality and self rated health (SRH) in studies with ordinal outcomes
| Details of study | Age (years) | Outcome (No of cases) | Measure of income inequality | Area level variable | Lag (years)* | Adjusted variables in primary models other than age and sex | |
|---|---|---|---|---|---|---|---|
| Fiscella and Franks, 2000w8 | NHANES I epidemiologic Follow-up Study (NHEFS), 1971-5 (n=13 280), US | 25-74 | 5 SRH items (No of cases not reported) | Median share† | 105 primary sampling units | 0 | Income |
| Mcleod et al, 2003w29 | National Population Health Survey (NPHS), 1994 (n=6180 or 5911), Canada | ≥18 | 5 SRH items (No of cases not reported) | Median share† | 53 metro areas | 3 or 7 | Age squared, marital status, household size, income, educational status, mean area income, city size |
| Hou and John, 2005w30 | National Population Health Survey (NPHS), 1996-7 (n=34 592), Canada | ≥12 | 5 SRH items (n=3576 in lower 2 categories) |
Gini | Census tracts | 0 | Income, immigrants, race, education |
| Gravelle and Sutton, 2008w31 | British General Household Survey (BGHS), 1979-2000 (n=231 208),‡ UK | 16-69 | 3 SRH items (n=24 554 in lowest and 58 704 in second lowest) | Gini | 19 regions | 0 | Income, education, occupation (social class), data year |
*Time lags between data on income inequality and health outcome.
†Median share: % of income sum below median in total area income.
‡Ordinal probit.
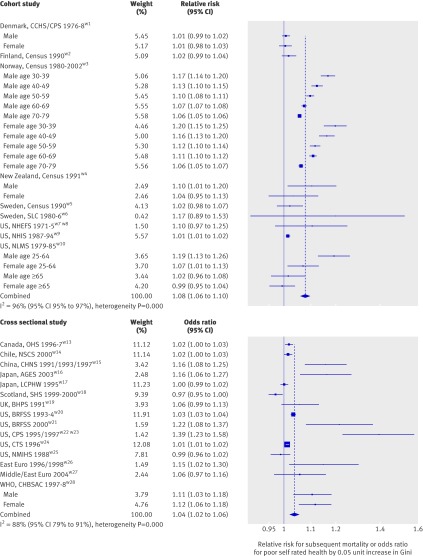
The overall cohort relative risk (95% confidence interval) for mortality adjusted for sociodemographic characteristics (including individual socioeconomic status) was 1.08 (1.06 to 1.10) per 0.05 unit increase in Gini (fig 1). The overall cross sectional odds ratio for poor self rated health was 1.04 (1.02 to 1.06) in binary logistic regressions (fig 1) and 1.08 (1.01 to 1.14) in ordinal regressions (see fig A on bmj.com). The effect sizes among studies were heterogeneous (P<0.001 for heterogeneity for all meta-analyses).
Fig 1 Result of primary meta-analysis of cohort and cross sectional studies: relative risks for subsequent mortality and odds ratios for poor self rated health per 0.05 unit increase in Gini coefficient. Combined relative risks and odds ratios based on weights for individual studies calculated with random effects models with restricted maximum likelihood estimate
Meta-regression analyses showed a significantly higher cohort relative risk among studies with higher average Ginis, later baseline data (>1990), and adjustment for area income compared with their counterparts; while the length of follow-up (>7 years) showed a marginally higher relative risk (table 4). For example, the overall cohort relative risk increased by 1.01 (95% confidence interval 1.00 to 1.05) per 0.05 unit increase in average Gini (data not shown). When we dichotomised average Gini at the median, the overall cohort relative risk for studies with average Gini of 0.30 or higher was 1.09 (1.07 to 1.12), while the relative risk was 1.02 (0.97 to 1.07) for those lower than 0.30. Heterogeneity between studies was not explained by the choice of income inequality measure (Gini or median share), adjustment for other contextual factors, whether the study was done in the US or not, or age range (<60 v ≥60). Cross sectional meta-regressions showed similar trends in terms of average Gini, incorporation of time lag, and study regions (table 5). In addition, between country studies showed significantly higher overall odds ratios (1.11) than within country studies (1.02). In the meta-regression by average Gini, we excluded the study by Pei et al,w15 which reported very low Gini (0.20) despite general reports of a high Chinese Gini (for example, 0.47 by the United Nations51).
Table 4.
Results of meta-regressions stratified by study characteristics: overall relative risks (95% confidence intervals) for mortality (cohort studies)
| No of studies | RR (95% CI)* | P value for difference† | Residual heterogeneity (τ2) | |
|---|---|---|---|---|
| Mean income inequality: | ||||
| Gini <median(0.3)w1 w2 w5 w6 | 4 | 1.02 (0.97 to 1.07) | 0.006 | 2.1×0−3 |
| Gini ≥median(0.3)w3 w4 w7-w10 | 5 | 1.09 (1.07 to 1.12) | ||
| Study region: | ||||
| USw7-w10 | 3 | 1.06 (1.01 to 1.11) | 0.37 | 3.0×0−3 |
| Non-USw1-w6 | 6 | 1.09 (1.06 to 1.12) | ||
| Baseline data: | ||||
| ≤1990w1 w2 w5-w8 w10 | 6 | 1.04 (1.01 to 1.08) | 0.01 | 2.2×0−3 |
| >1990w3 w4 w9 | 3 | 1.10 (1.07 to 1.13) | ||
| Follow-up duration: | ||||
| ≤Median (7 years)w2 w4 w5 w9 | 4 | 1.03 (0.98 to 1.09) | 0.06 | 2.6×0−3 |
| >Median (7 years)w1 w3 w6-w8 w10 | 5 | 1.09 (1.06 to 1.12) | ||
| Income inequality measure: | ||||
| Giniw2-w6 w9 | 6 | 1.09 (1.06 to 1.12) | 0.11 | 2.7×0−3 |
| Median sharew1 w7 w8 w10 | 3 | 1.05 (1.00 to 1.09) | ||
| Adjustment for area income/poverty: | ||||
| Now1 w2 w5 w7 w8 w10 | 5 | 1.04 (1.00 to 1.08) | 0.009 | 2.2×0−3 |
| Yesw3 w4 w6 w9 | 4 | 1.10 (1.07 to 1.13) | ||
| Age (years): | ||||
| <60w1-w9 | 9 | 1.06 (1.01 to 1.10) | 0.26 | 3.0×0−3 |
| ≥60w3 w10 | 2 | 1.09 (1.06 to 1.12) | ||
*From random effects models with restricted maximum likelihood estimate.
†Calculated by interaction analyses.
Table 5.
Results of meta-regressions stratified by study characteristics*: overall odds ratios (95% confidence intervals) for poor self rated health (cross sectional studies) per 0.05 unit increase in Gini coefficient
| No of studies | OR (95% CI)† | P value for difference‡ | Residual heterogeneity (τ2) | |
|---|---|---|---|---|
| Mean income inequality§: | ||||
| Gini <0.3w18 w19 | 2 | 0.99 (0.96 to 1.01) | 0.01 | 7.6×10−5 |
| Gini ≥0.3w13 w14 w16 w17 w20-w28 | 12 | 1.02 (1.02 to 1.03) | ||
| Study region: | ||||
| USw20-w25 | 5 | 1.02 (1.01 to 1.04) | — | — |
| Non-US, within country studiesw13-w19 | 7 | 1.01 (1.00 to 1.02) | 0.21 | 8.0×10−5 |
| All non-US studiesw13-w19 w26-w28 | 10 | 1.02 (1.01 to 1.03) | 0.67 | 8.4×10−5 |
| Time lag: | ||||
| Now13 w14 w16-w20 w24 w26-w28 | 11 | 1.01 (1.01 to 1.02) | <0.001 | 0.0×10−5 |
| Yesw15 w21-w23 w25 | 4 | 1.03 (1.03 to 1.04) | ||
| Adjustment for area income/poverty: | ||||
| Now13 w15 w17 w19 w22-w28 | 10 | 1.02 (1.01 to 1.03) | 0.28 | 8.0×10−5 |
| Yesw14 w16 w18 w20 w21 | 5 | 1.01 (0.99 to 1.03) | ||
| Within or between country: | ||||
| Within countryw13-w25 | 12 | 1.02 (1.01 to 1.03) | <0.001 | 7.2×10−5 |
| Between countryw26-w28 | 3 | 1.11 (1.07 to 1.15) | ||
| Self rated health items: | ||||
| 5 itemsw13 w14 w16 w17 w19-w27 | 12 | 1.02 (1.01 to 1.03) | 0.64 | 7.6×10−5 |
| 3 or 4 itemsw15 w18 w28 | 3 | 1.03 (1.00 to 1.05) | ||
*Not stratified by age as there was only one study with young subjects and all others used adult subjects (including some with wider age ranges).
†From random effects models with restricted maximum likelihood estimate.
‡Calculated by interaction analyses.
§CHNS dataw15 omitted because of wide gap between Chinese Gini coefficients reported by article (mean Gini=0.20) and other statistics (for example, 0.47 by United Nations43).
In our sensitivity analyses, none of the inclusions and exclusions of specific studies (see table A on bmj.com) nor one by one exclusions of each study (data not shown) materially changed the results of the primary meta-analyses. One exception is the alternative meta-analysis replacing three modelsw3 w6 w10 with those adjusted for regions, which attenuated the overall relative risk from 1.08 (1.06 to 1.10) to 1.02 (1.00 to 1.04). This is similar to the overall relative risk when we used the models adjusted for three regions only (1.02, 0.99 to 1.05).
We did not find a significant publication bias among cohort studies (Begg’s P=0.60), although there was a suggestion of publication bias among the cross sectional studies (P=0.03) (see fig B on bmj.com). When we removed the three smallest cross sectional studies (whose weights were also small as less than two)w21-23 w26 the bias was not significant (P=0.13).
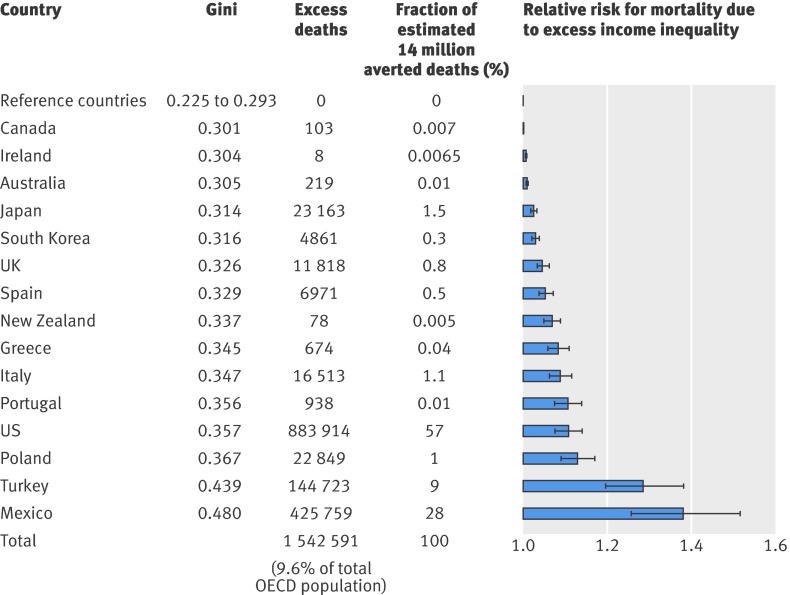
We predicted the potential excess risks of premature mortality for each OECD country, multiplying the unit effect estimates by the gap between each nation’s Gini reported52 and the Gini threshold suggested in the present study (Gini 0.3). The excess risks for selected countries were 3% in Japan, 11% in the US, and 38% in Mexico compared with the countries having Ginis lower than 0.3 (fig 2, see the figure footnotes for detailed information on our estimation).
Fig 2 Relative risks for subsequent mortality by 30 OECD member countries and estimated number of deaths avoided by levelling Gini to <0.3. Risks predicted on basis of Gini threshold (0.3) suggested by meta-regression, assuming that countries with Gini lower than threshold had no excess mortality risks (RR=1). Excess deaths estimated for only half of 30 countries because Gini coefficient is already <0.3 in remainder. Reference countries include Denmark (Gini=0.225), Sweden (0.243), Iceland (0.250), Netherlands (0.251), Austria (0.252), Slovakia (0.258), Czech Republic (0.260), Luxembourg (0.261), Finland (0.261), Norway (0.261), Switzerland (0.277), Belgium (0.272), France (0.273), Germany (0.277), and Hungary (0.293). Predicted relative risk for each country calculated by: RR=exp{[G−0.3]×ln(1.09/0.05)}, where G represents Gini coefficient of each country. Combined relative risk per 0.05 unit increase in Gini, as shown in table 4, was 1.09, estimated from data from Norway,w3 New Zealand,w4 and US.w7-10 Error bars represent 95% confidence intervals. Gini of each country derived from OECD,1 United Nations (for Slovakia and South Korea),51 and Statistics Iceland52
Discussion
Principal findings
Our meta-analysis of cohort studies including around 60 million participants found that people living in regions with high income inequality have an excess risk for premature mortality independent of their socioeconomic status, age, and sex. A similar conclusion was supported by our meta-analysis of cross sectional studies with poor self rated health as the outcome. The estimated excess mortality risk was 8% per 0.05 unit increase in the Gini coefficient. Although the size of the excess risk seems relatively “modest,” it has potentially important policy implications for population health as income inequality is an exposure that applies to society as a whole. For instance, if the inequality-mortality relation is truly causal then the population attributable fraction suggests that upwards of 1.5 million deaths (9.6% of total adult mortality in the 15-60 age group) could be averted in 30 OECD countries by levelling the Gini coefficient below the threshold value of 0.3 (based on 2007 population).53
Sources of heterogeneity between studies
The combined cohort relative risk and cross sectional odds ratio should be interpreted with caution, given the substantial heterogeneity detected between studies. Several local factors seem to account for this heterogeneity, including the possibility of a “threshold” effect of income inequality on health (with Gini values ≥0.3 indicating a more consistent association with adverse health effects), the time period in which the analyses were carried out (with studies after 1990 indicating a more consistent association), and the length of follow-up in the cohort studies. Consideration of these factors might help to improve our understanding of the specific circumstances under which income inequality is damaging to population health.
A further source of heterogeneity is the spatial unit across which income inequality indices are evaluated. Among the cross sectional studies, between country studies showed a significantly stronger association between income inequality and self rated health than within country studies. This observation is consistent with the conclusion of a recent systematic review suggesting that studies with smaller reference groups are less likely to show an association with health because the spatial scale does not reflect the social stratification of societies.7
Although not evaluated in this study, other contextual characteristics such as social security policies, labour markets, and immigration could also explain the heterogeneity between studies.
Study limitations
Several limitations need to be borne in mind in interpreting our findings. First and foremost, all meta-analysis of observational studies are prone to biases in the original studies.54 For example, although we evaluated multiple models using alternative sets of covariates, the estimates from the original studies might have been prone to residual confounding. Secondly, five cross sectional analyses did not report the necessary information to permit us to include them in the meta-analysis.22 25 31 32 33 Their omission might have influenced our conclusions. On the other hand, our findings rely more on the cohort studies reviewed, which involved larger samples and had no evidence of a publication bias. Thirdly, we cannot discount the possibility that income inequality is a marker of broader societal characteristics such as political ideology or race relations.55 56 57 58 Fourthly, the Gini coefficient is an overall summary measure of income distribution that is insensitive to the shape of the distribution (that is, a high Gini value could be produced by either a high number of extremely affluent individuals or a high number of extremely poor individuals). Lastly, although the subgroup analysis of studies with Gini values ≥0.3 is consistent with a “threshold” effect of income inequality on health, an alternative explanation is that a small incremental effect is easier to detect when the Gini is higher.
Conclusions
Although our study suggests that there is an association between higher income inequality and worse health outcomes, further investigations are needed because of the lack of empirical evidence from many parts of the world, including developing countries. Factors accounting for the heterogeneity between studies warrant further study. One policy implication of the present study is consistent with the recently released report of the WHO Commission on Social Determinants of Health, which said that local, domestic, and international communities should recognise the link between macro-economic conditions mirrored by income inequality and individual health.59
What is already known on this topic
Dozens of studies have examined the association between income inequality and population health, but consensus remains elusive because of inconsistent findings
Researchers have suggested several factors—such as a threshold effect of income inequality on health—that could account for heterogeneity between studies
What this paper adds
Our meta-analysis found that income inequality was associated with a modest excess risk of premature mortality and poor self rated health
The studies reviewed were highly heterogeneous, one potential explanation being the existence of a threshold effect of income inequality (Gini ≥0.3) on population health
If the inequality-mortality relation is truly causal then the population attributable fraction suggests that upwards of 1.5 million deaths (9.6% of adult mortality) could be averted in 30 OECD countries by levelling the Gini coefficient below the threshold value of 0.3
Contributors: NK conceived the study, gathered data, completed the analysis, drafted the initial manuscript, and conceptualised ideas. GS participated in the data acquisition, data extraction, and drafting of the manuscript. IK helped in the conceptualisation of the study and drafting of the manuscript. RMvD contributed to the supervision of the statistical analysis and drafting of the manuscript. SVS participated in the conceptualisation of ideas and the supervision of the analysis. ZY supervised the research project and analysis. All authors, external and internal, had full access to all of the data in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis. NK is guarantor.
Funding: This study is supported by the Pfizer Health Research Foundation. NK is a recipient of the fellowship award by the Abe Fellowship Program administered by the Social Science Research Council and the American Council of Learned Societies in cooperation with and funded by the Japan Foundation Center for Global Partnership. SVS is supported by the National Institute of Health Career Development Award (NHLBI 1k25 HL081275). These sponsors were not involved in study design and the collection, analysis, and interpretation of data and the writing of the article and the decision to submit it for publication.
Competing interest: None declared.
Ethical approval: Not required.
Data sharing: No additional data available.
Cite this as: BMJ 2009;339:b4471
References
- 1.OECD Rights and Translation Unit. Growing unequal? Income distribution and poverty in OECD countries. OECD publications, 2008.
- 2.Kondo N, Kawachi I, Subramanian SV, Takeda Y, Yamagata Z. Do social comparisons explain the association between income inequality and health? Relative deprivation and perceived health among male and female Japanese individuals. Soc Sci Med 2008;67:982-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kondo N, Kawachi I, Hirai H, Kondo K, Subramanian SV, Hanibuchi T, et al. Relative deprivation and incident functional disability among older Japanese women and men: prospective cohort study. J Epidemiol Community Health 2009;63:461-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Subramanian SV, Kawachi I. Income inequality and health: What have we learned so far? Epidemiol Rev 2004;26:78-91. [DOI] [PubMed] [Google Scholar]
- 5.Wagstaff A, van Doorslaer E. Income inequality and health: What does the literature tell us? Annu Rev Public Health 2000;21:543-67. [DOI] [PubMed] [Google Scholar]
- 6.Lynch J, Smith GD, Harper S, Hillemeier M, Ross N, Kaplan GA, et al. Is income inequality a determinant of population health? Part 1. A systematic review. Milbank Q 2004;82:5-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wilkinson RG, Pickett KE. Income inequality and population health: a review and explanation of the evidence. Soc Sci Med 2006;62:1768-84. [DOI] [PubMed] [Google Scholar]
- 8.Wilkinson RG, Pickett KE. The spirit level: why more equal societies almost always do better. Penguin Books, 2009.
- 9.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 2000;283:2008-12. [DOI] [PubMed] [Google Scholar]
- 10.Subramanian SV, Ichiro K. Being well and ng well on the importance of income for health. Int J Soc Welfare 2006;15:S13-22. [Google Scholar]
- 11.Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav 1997;38:21-37. [PubMed] [Google Scholar]
- 12.Hsieh C-C, Pugh MD. Poverty, income inequality, and violent crime: a meta-analysis of recent aggregate data studies. Crim Justice Rev 1993;18:182-202. [Google Scholar]
- 13.Kawachi I, Kennedy BP. The relationship of income inequality to mortality: Does the choice of indicator matter? Soc Sci Med 1997;45:1121-7. [DOI] [PubMed] [Google Scholar]
- 14.US Census Bureau. Table S4. Gini Ratios by State: 1969, 1979, 1989, 1999, 2008. www.census.gov/hhes/www/income/histinc/state/state4.html
- 15.Dahl E, Ivar Elstad J, Hofoss D, Martin-Mollard M. For whom is income inequality most harmful? A multi-level analysis of income inequality and mortality in Norway. Soc Sci Med 2006;63:2562-74. [DOI] [PubMed] [Google Scholar]
- 16.Luxembourg Income Study database, 2008. www.lisproject.org/
- 17.Orsini N, Bellocco R, Greenland S. Generalized least squares for trend estimation of summarized dose-response data. Stata J 2006;6:40-57. [Google Scholar]
- 18.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-88. [DOI] [PubMed] [Google Scholar]
- 19.Julian P. T. Higgins SGT. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539-58. [DOI] [PubMed] [Google Scholar]
- 20.Cochran WG. The combination of estimates from different experiments. Biometrics 1954;10:101-29. [Google Scholar]
- 21.Blakely TA, Kennedy BP, Glass R, Kawachi I. What is the lag time between income inequality and health status? J Epidemiol Community Health 2000;54:318-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mellor JM, Milyo J. Is exposure to income inequality a public health concern? Lagged effects of income inequality on individual and population health. Health Serv Res 2003;38:137-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Subramanian SV, Kawachi I. Whose health is affected by income inequality? A multilevel interaction analysis of contemporaneous and lagged effects of state income inequality on individual self-rated health in the United States. Health Place 2006;12:141-56. [DOI] [PubMed] [Google Scholar]
- 24.Subramanian SV, Kawachi I. Chasing the elusive null the story of income inequality and health. Int J Epidemiol 2007;36:596-9. [DOI] [PubMed] [Google Scholar]
- 25.Mellor JM, Milyo J. Income inequality and health status in the United States. Evidence from the current population survey. J Hum Resour 2002;37:510-39. [Google Scholar]
- 26.Subramanian SV, Blakely T, Kawachi I. Income inequality as a public health concern: where do we stand? Commentary on “Is exposure to income inequality a public health concern?” Health Serv Res 2003;38:153-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blakely TA, Kawachi I. What is the difference between controlling for mean versus median income in analyses of income inequality? J Epidemiol Community Health 2001;55:352-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lipsey MW, Wilson DB. Selecting, computing, and coding the effect size statistic. Practical meta-analysis. SAGE Publications, 2000:34-71.
- 29.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sterne JA, Egger M, Smith GD. Systematic reviews in health care: Investigating and dealing with publication and other biases in meta-analysis. BMJ 2001;323:101-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.LeClere FB, Soobader MJ. The effect of income inequality on the health of selected US demographic groups. Am J Public Health 2000;90:1892-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Soobader MJ, LeClere FB. Aggregation and the measurement of income inequality: effects on morbidity. Soc Sci Med 1999;48:733-44. [DOI] [PubMed] [Google Scholar]
- 33.Wen M, Browning CR, Cagney KA. Poverty, affluence, and income inequality: neighborhood economic structure and its implications for health. Soc Sci Med 2003;57:843-60. [DOI] [PubMed] [Google Scholar]
- 34.Subramanian SV, Kawachi I, Kennedy BP. Does the state you live in make a difference? Multilevel analysis of self-rated health in the US. Soc Sci Med 2001;53:9-19. [DOI] [PubMed] [Google Scholar]
- 35.Blakely TA, Lochner K, Kawachi I. Metropolitan area income inequality and self-rated health—a multi-level study. Soc Sci Med 2002;54:65-77. [DOI] [PubMed] [Google Scholar]
- 36.Henriksson G, Allebeck P, Weitoft GR, Thelle D. Income distribution and mortality: implications from a comparison of individual-level analysis and multilevel analysis with Swedish data. Scand J Public Health 2006;34:287-94. [DOI] [PubMed] [Google Scholar]
- 37.Hou F, Myles J. Neighbourhood inequality, neighbourhood affluence and population health. Soc Sci Med 2005;60:1557-69. [DOI] [PubMed] [Google Scholar]
- 38.Lorgelly PK, Lindley J. What is the relationship between income inequality and health? Evidence from the BHPS. Health Econ 2008;17:249-65. [DOI] [PubMed] [Google Scholar]
- 39.Osler M, Christensen U, Due P, Lund R, Andersen I, Diderichsen F, et al. Income inequality and ischaemic heart disease in Danish men and women. Int J Epidemiol 2003;32:375-80. [DOI] [PubMed] [Google Scholar]
- 40.Shi L, Starfield B. Primary care, income inequality, and self-rated health in the United States: a mixed-level analysis. Int J Health Serv 2000;30:541-55. [DOI] [PubMed] [Google Scholar]
- 41.Jones AM, Wildman J. Health, income and relative deprivation: evidence from the BHPS. J Health Econ 2008;27:308-24. [DOI] [PubMed] [Google Scholar]
- 42.Blakely TA, Kennedy BP, Kawachi I. Socioeconomic inequality in voting participation and self-rated health. Am J Public Health 2001;91:99-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Blakely TA, Kawachi I. Education does not explain association between income inequality and health. BMJ 2002;324:1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Charafeddine R, Boden LI. Does income inequality modify the association between air pollution and health? Environ Res 2008;106:81-8. [DOI] [PubMed] [Google Scholar]
- 45.Gravelle H, Sutton M. Income related inequalities in self assessed health in Britain: 1979-1995. J Epidemiol Community Health 2003;57:125-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Li H, Zhu Y. Income, income inequality, and health: Evidence from China. J Comp Econ 2006;34:668-93. [Google Scholar]
- 47.Mansyur C, Amick BC, Harrist RB, Franzini L. Social capital, income inequality, and self-rated health in 45 countries. Soc Sci Med 2008;66:43-56. [DOI] [PubMed] [Google Scholar]
- 48.Deaton A. Inequalities in income and Inequalities in health. NBER Working Paper Series 1999 (Working Paper 7141).
- 49.Deaton A, Paxson C. Mortality, education, income, and inequality among American cohorts. NBER Working Paper Series 1999 (Working Paper 7140).
- 50.Mayer SE, Sarin A. Some mechanisms linking economic inequality and infant mortality. Soc Sci Med 2005;60:439-55. [DOI] [PubMed] [Google Scholar]
- 51.United Nations Development Programme. Inequality in income and expenditure. In: Human Development Report 2007/2008. Palgrave Macmillan, 2007:281-4.
- 52.Risk of poverty and income distribution 2003-2004. Statistic Iceland, 2008.
- 53.Förster M, d’Ercole MM. Income distribution and poverty in OECD countries in the second half of the 1990s. OECD Social Employment and Migration Working Papers 2005;22.
- 54.Egger M, Schneider M, Davey Smith G. Spurious precision? Meta-analysis of observational studies. BMJ 1998;316:140-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zimmerman FJ. A commentary on “Neo-materialist theory and the temporal relationship between income inequality and longevity change”. Soc Sci Med 2008;66:1882-94; discussion 903-8. [DOI] [PubMed] [Google Scholar]
- 56.Deaton A, Lubotsky D. Mortality, inequality and race in American cities and states. NBER Working Papers 2001;No 8370. [DOI] [PubMed]
- 57.Coburn D. Beyond the income inequality hypothesis: class, neo-liberalism, and health inequalities. Soc Sci Med 2004;58:41-56. [DOI] [PubMed] [Google Scholar]
- 58.Kunitz SJ. The health of populations: general theories and particular realities. Oxford University Press, 2006.
- 59.CSDH. Closing the gap in a generation: health equity through action on the social determinants of health. Final Report of the Commission on Social Determinants of Health. World Health Organization, 2008. [DOI] [PubMed]