Abstract
Purinoceptors are rapidly becoming recognised as important regulators of tissue and organ function. Renal expression of P2 receptors is broad and diverse, as reflected by the fact that P2 receptors have been identified in virtually every major tubular/vascular element. While P2 receptor expression by these renal structures is recognised, the physiological functions that they serve remains to be clarified. Renal vascular P2 receptor expression is complex and poorly understood. Evidence suggests that different complements of P2 receptors are expressed by individual renal vascular segments. This unique distribution has given rise to the postulate that P2 receptors are important for renal vascular function, including regulation of preglomerular resistance and autoregulatory behaviour. More recent studies have also uncovered evidence that hypertension reduces renal vascular reactivity to P2 receptor stimulation in concert with compromised autoregulatory capability. This review will consolidate findings related to the role of P2 receptors in regulating renal microvascular function and will present areas of controversy related to the respective roles of ATP and adenosine in autoregulatory resistance adjustments.
Keywords: Afferent arteriole, Autoregulation, Adenosine, P2X receptors, Hypertension, Tubuloglomerular feedback
Introduction
Understanding the physiology of renal purinoceptors has become a rapidly developing area of investigation. It is now recognised that extracellular ATP and adenosine are important signalling molecules regulating the renal microcirculation and tubular function and influencing renin secretion [1–20]. This review will summarise information defining the roles of extracellular ATP in regulating renal microvascular function and renal haemodynamics.
P2 receptors and their expression in the renal vasculature and glomeruli
P2 receptors are expressed by renal vascular, glomerular, mesangial and tubular epithelial cells [1–15]. P2X1 receptors are expressed by vascular smooth muscle of arcuate and interlobular arteries and afferent arterioles but do not appear to be expressed by glomeruli or efferent arterioles [4, 12, 21]. P2X1 receptor expression by afferent arteriole vascular smooth muscle has been confirmed by immunostaining and by western blot analysis [4, 11]. P2Y1 receptors are found on afferent and efferent arterioles and P2X2 receptor expression has been detected in larger intrarenal arteries and veins [6]. P2Y1, P2Y2 and P2X7 receptors are expressed in rat mesangial cells [22, 23] and P2Y2 receptors are found in podocytes [3, 6]. Mouse mesangial cells express P2X2, P2X4, P2X7, P2Y2 and P2Y4 receptors. mRNA is detected for P2X1 and P2X3 receptors in murine mesangial cells but protein is not found by western blot analysis [9]. Considering the wide distribution of renal P2 receptor subtypes, it seems likely that purinoceptors play diverse roles in regulating renal vascular and tubular function.
Purinoceptors and renal haemodynamics
The modulation of renal vascular resistance by nucleotides and nucleosides has been recognised since the 1920s, but only received widespread attention in recent decades [24–42]. The renal vascular response to infused ATP or other P2 agonists depends on many factors including the species, the type of agonist infused, ambient vascular tone and the experimental conditions. Intrarenal infusion of ATP into canine kidneys produces vasodilation by stimulating endothelial release of nitric oxide [43, 44]. Vasoconstriction is observed in isolated perfused rat kidneys under basal tone, and either vasoconstriction or vasodilation when renal vascular resistance is elevated [45–48]. Infusion of ATP or α β-methylene ATP (an effective P2X1 receptor agonist, which also has some influence on P2X3 and P2X5 receptors) into the isolated perfused rat kidney induces a sustained concentration-dependent vasoconstriction under normal conditions [45–49], but ATP-mediated responses are less consistent under high-tone conditions [45, 48].
Suprarenal aortic infusion of ATP into anaesthetised rats that had been fed on a low salt diet led to nitric oxide-dependent vasodilation in the medullary circulation, whereas in rats fed a high salt diet, medullary blood flow decreased in response to ATP [50]. P2Y receptor agonists, such as 2-methylthio ATP, UTP or ATP-γ-S, produce nitric oxide-dependent vasodilation when infused at low concentrations but vasoconstriction at higher concentrations [45, 49]. Thus, endothelial P2Y receptors may mediate vasodilation due to nitric oxide-dependent relaxation of the renal microvasculature, which reverts to a pronounced vasoconstriction during inhibition of nitric oxide synthase [45]. P2X receptor-mediated vasoconstrictor responses are also augmented by inhibition of nitric oxide production [45].
P2 receptors and the renal microcirculation: single vessel studies
Extracellular ATP is an important autocrine and paracrine regulator of preglomerular vascular responses, mediated by P2X and P2Y receptor activation [21, 33, 41, 51–55]. Infusion of relatively low doses of α β-methylene ATP into the rabbit renal artery produces renal cortical and medullary vasoconstriction as indicated by decreases in regional blood flow [56, 57]. Exposure of microperfused rabbit afferent arterioles (with attached glomeruli) to ATP or β γ-methylene ATP reduced arteriolar diameter [41]. Afferent arterioles also express adenosine-sensitive A1 receptors, raising the question of whether the vasoconstriction is induced by ATP-dependent activation of P2 receptors, or whether the ATP is hydrolyzed to adenosine which vasoconstricts arterioles by activating A1 receptors. The fact that ATP vasoconstricts afferent arterioles directly was established by demonstrating that ATP-mediated vasoconstriction persists even during adenosine receptor blockade and that the sustained vasoconstriction to ATP is eliminated during P2 receptor blockade [21, 33, 51].
Renal vascular resistance is regulated primarily by adjusting afferent arteriolar resistance, with only lesser resistance contributions being made by the upstream arterial segments [58]. Of the three preglomerular vascular segments evaluated for responsiveness to P2 receptor activation by ATP, only the afferent arteriole exhibits sustained ATP-mediated vasoconstriction at concentrations as low as 100 nM (Fig. 1) [21]. Arcuate arteries respond to 10 and 100 µM ATP with a transient vasoconstriction that quickly subsides [21]. Interlobular arteries respond to 100 µM ATP with a sustained vasoconstriction, but lower concentrations produce no significant response [21]. Importantly, efferent arterioles are completely unresponsive to ATP concentrations as high as 100 µM [21]. These observations support the hypothesis that extracellular ATP could serve as a paracrine regulator whose actions primarily influence afferent arteriolar vascular smooth muscle and thus arteriolar diameter [8, 12, 55, 59].
Fig. 1.
ATP concentration–response relationship for the intrarenal pre- and postglomerular vascular segments. Average segmental diameter responses evoked by ATP applied to the adventitial surface of arcuate arteries (top panel), interlobular arteries (second panel), afferent arterioles (third panel) and efferent arterioles (bottom panel). After the control period (Con), increasing concentrations of ATP (0.1, 1.0, 10 and 100 µM) were applied at 5-min intervals as indicated by the dotted lines. Each protocol ended with a 5-min recovery period (Rec) while bathed with control solution. Each data point represents diameter measurements taken at 12-s intervals and normalised as a percentage of the control diameter. Data were modified from an earlier report [21]
As indicated above, P2Y receptors modulate vascular resistance by stimulating the synthesis and release of endothelium-derived relaxing factors [45, 49, 60]. Direct assessment of the contribution of endogenous nitric oxide in single intrarenal arteries reveals that the transient ATP-mediated vasoconstriction of rat arcuate arteries reverts to a sustained vasoconstriction in kidneys pretreated with l-NAME [60]. This observation is consistent with whole-kidney studies where inhibition of nitric oxide synthase with L-NAME greatly reduces the renal vasodilation evoked by ATP or P2Y receptor agonists such as 2-methylthio ATP or UTP [46, 61]. Futhermore, intrarenal infusion of ATP into the canine kidney in vivo produces a rapid vasodilation under basal conditions; whereas during inhibition of nitric oxide synthase, ATP produces sustained renal vasoconstriction [43]. Thus, nitric oxide is responsible for P2 receptor-mediated renal vasodilation, suggesting that regulation of renal vascular tone by ATP may involve a complex interplay between segmental vasoconstrictor and vasodilatory signals arising from selective, paracrine activation of P2 receptors on renal vascular smooth muscle cells and endothelial cells. This idea is supported by observations in other renal and nonrenal vascular beds demonstrating that nitric oxide and endothelium-derived hyperpolarizing factor(s) contribute to the vasodilation produced by P2Y receptor activation [61–66].
P2 receptor-mediated second messenger systems in the renal microcirculation
Preglomerular vascular smooth muscle cells and glomerular mesangial cells respond to α β-methylene ATP, or ATP, with a rapid, biphasic increase in intracellular calcium concentration. This calcium response involves calcium release from intracellular stores and/or influx of calcium from the extracellular fluid (see example traces shown in Fig. 2 and Fig. 5b) [9, 11, 59, 67–74]. Low concentrations of ATP (≤1.0 µM) vasoconstrict afferent arterioles by activation of L-type Ca2+ channels. Higher concentrations of ATP (>1.0 µM) vasoconstrict afferent arterioles by combining calcium influx and calcium release to increase the intracellular calcium concentration [11, 59, 73–76]. Calcium influx, and afferent arteriolar vasoconstriction, induced by ATP is markedly attenuated by blockade of voltage-gated L-type Ca2+ channels [59, 72–76]. Removal of extracellular calcium merely blunts the peak increase in calcium induced by 10 µM ATP, while the sustained elevation of calcium is abolished (Fig. 2b vs. d) [59, 73, 74]. Thus, release of calcium from intracellular stores is a major contributor to the peak calcium response to ATP, while calcium influx supports the sustained increase in intracellular calcium concentration [59, 72–76]. Interestingly, the sustained concentration-dependent afferent arteriolar vasoconstriction by ATP is attenuated, or eliminated, by superfusion with calcium-free medium or blockade of L-type Ca2+ channels [75, 76].
Fig. 2.
The effect of α β-methylene ATP and ATP on intracellular calcium concentration in preglomerular smooth muscle cells. Response of intracellular calcium concentration evoked by α β-methylene ATP or ATP (each 10 µM) in the presence of 1.8 mM extracellular calcium (a and b), in the absence of extracellular calcium (c and d) and during P2X1 receptor blockade with NF-279 (e). The periods of exposure to α β-methylene ATP or ATP administration are indicated by the black bars. The periods of exposure to calcium-free medium or NF-279 are shown by a second set of black bars. Calcium measurements were performed using fura 2. Data were modified from an earlier report [74]
Fig. 5.
Effect of ANG-II hypertension on the afferent arteriolar diameter and calcium signalling responses to ATP. Panel a presents the changes in afferent arteriolar diameter in kidneys from normotensive rats (black symbols) and from Ang-II hypertensive rats (grey symbols). Data are expressed as a percentage of the control diameter. ATP was administered in concentrations of 0.1–100 μM. Values represent average diameters measured over the last 2 min of each treatment period and plotted as means ± SE. *P < 0.05, significant difference from control diameter; #P < 0.05 significant difference from normotensive controls. b Presents the change in intracellular calcium concentration (detected by fura 2) induced by 10 µM ATP in single preglomerular smooth muscle cells taken from normotensive (black trace) and ANG II hypertensive rats (grey trace). The period of ATP administration is depicted by the black bar. Data are modified from an earlier report [11]
P2X receptors are ligand-gated channels that allow influx of extracellular Ca2+ and Na+ ions. Activation of P2X receptors on afferent arterioles leads to calcium influx, whereas calcium mobilisation from intracellular stores occurs in response to P2Y receptor activation (Fig. 2) [59, 74]. Thus, P2X1 receptor-mediated vasoconstriction and calcium signalling responses are eliminated in calcium-free bathing solutions (Fig. 2a vs. c) and during blockade of voltage-gated, L-type Ca2+ channels [59, 72–76]. In contrast, P2Y receptor-mediated vasoconstriction and calcium signalling responses persist during calcium channel blockade or in calcium-free conditions (Fig. 2d), indicating differing signalling mechanisms between the two receptor families [59, 72–76]. In summary, activation of voltage-dependent calcium channels and calcium influx are important signalling elements for ATP-mediated vasoconstriction of afferent arterioles through P2X1 receptor activation, whereas calcium release mechanisms predominate in vascular responses evoked by P2Y receptor activation.
Studies also indicate that cytochrome P450 metabolites, such as 20-hydroxyeicosatetraenoic acid (20-HETE), may play an important role as second messengers facilitating P2 receptor activation in renal microvascular smooth muscle. 20-HETE is an important modulator of L-type Ca2+ channel function, K+ channel function and renal vascular autoregulatory responses [77–80]. In one study, afferent arteriolar responses to ATP, α β-methylene ATP and UTP were determined before and after treatment with the selective CYP450 hydroxylase inhibitor, N-methylsulfonyl-12,12-dibromododec-11-enamide (DDMS), or the 20-HETE antagonist, 20-hydroxyeicosa-6(Z),15(Z)-dienoic acid (20-HEDE) [81]. The sustained vasoconstriction normally observed in response to α β-methylene ATP under control conditions was eliminated during 20-HETE inhibition with DDMS or 20-HEDE [81]. In contrast, afferent arteriolar vasoconstriction induced by P2Y2 receptor activation with UTP was unaffected by inhibition of 20-HETE [81]. The ATP-induced increase in intracellular calcium concentration in preglomerular microvascular smooth muscle cells was significantly attenuated by 20-HEDE [82]. Similarly, 20-HETE inhibition attenuated the increase in intracellular calcium concentration induced by α β-methylene ATP, but responses evoked by UTP were unchanged [82]. These results demonstrate that 20-HETE plays a significant role in the renal vascular vasoconstrictor response and the elevation of intracellular calcium concentration in response to P2X1 receptor activation.
Rho-kinase and its multiple co-factors modulate vascular tone, purportedly by increasing calcium sensitivity and thus smooth muscle contractility [83–85]. The Rho-kinase system also influences P2 receptor-mediated vasoconstriction, 20-HETE-dependent intracellular signalling, renal microvascular function and myogenic autoregulatory behaviour [86–93]. Inhibition of Rho-kinase in hydronephrotic kidneys vasodilates virtually every pre- and postglomerular artery/arteriole and attenuates endothelin- or adenosine-induced renal microvascular vasoconstriction [87]. Similarly, preliminary in vitro studies revealed that Rho-kinase inhibition with Y-27632 produced a rapid, concentration-dependent afferent arteriolar vasodilation and inhibited renal autoregulatory responses [88]. In addition, vasoconstrictor responses induced by angiotensin II or ATP were markedly attenuated [88]. Interestingly, the afferent arteriolar vasoconstriction elicited by α β-methylene ATP was completely eliminated [88]. Thus, P2 receptor activation involves induction of a number of second messenger systems that also play major roles in regulating pressure-dependent renal perfusion.
P2 receptors and their roles in renal autoregulation and tubuloglomerular feedback
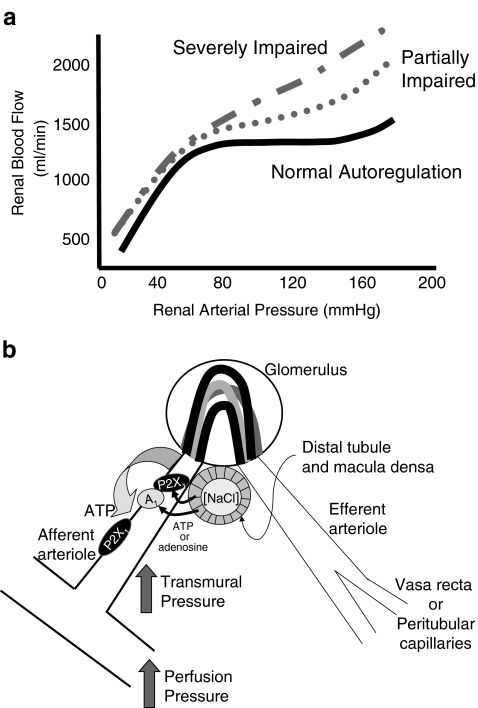
The phenomenon of autoregulation is a critical renal microvascular control mechanism that serves to assure and protect normal renal function [55, 94–98]. The autoregulatory mechanism maintains a stable renal blood flow (Fig. 3a), glomerular capillary pressure and glomerular filtration rate by buffering acute changes in renal perfusion pressure with precise adjustments in preglomerular vascular resistance [36, 55, 94–98]. Whole-kidney autoregulation integrates the combined influences of two major regulatory systems. They include an intrinsic myogenic mechanism operating along the preglomerular vascular tree, and the tubuloglomerular feedback mechanism, which regulates tone in the distal afferent arteriole through an interaction between the arteriole and the macula densa region in the thick ascending limb of the loop of Henle of the same nephron [55, 95, 97–101]. The signalling mechanism(s) by which changes in transmural pressure and/or stimulation of tubuloglomerular feedback produce precise adjustments in afferent arteriolar resistance remain somewhat controversial and are under intensive study. This section of the review will try to highlight the important controversies in the area but will not go into exhaustive detail. The interested reader is referred to some excellent reviews, which devote more attention to the subject [8, 12, 28, 95, 97, 98, 102–106] (plus, see article by Bell et al [107] in this Special Issue). Instead, this review will focus on the critical data leading to the postulate that ATP transduces haemodynamic and tubular information into autoregulatory adjustments in afferent arteriolar diameter by stimulating P2 receptors.
Fig. 3.
Postulated signalling mechanisms for ATP-mediated autoregulatory adjustments in afferent arteriolar diameter. Panel a illustrates a normal profile for autoregulation of renal blood flow (solid black line) and the autoregulatory profiles that might be observed under conditions of moderate and severe autoregulatory dysfunction (modified from [171]). b ATP might be released from afferent arteriole smooth muscle cells in response to an increase in renal perfusion pressure. This ATP released into the perivascular interstitial fluid could act upon P2X1 receptors to evoke autoregulatory vasoconstrictor responses. ATP released from the macula densa, in response to an increase in distal tubular fluid NaCl concentration, can traverse the interstitial fluid of the juxtaglomerular apparatus to act on afferent arterioles and induce tubuloglomerular feedback-mediated vasoconstriction. Alternatively, released ATP could be degraded to adenosine in the interstitial fluid prior to activating afferent arteriolar adenosine A1 receptors to regulate afferent arteriolar resistance
It is generally agreed that autoregulation is mediated by a locally generated paracrine messenger molecule, or molecules, linking myogenic and tubuloglomerular feedback signals from the macula densa with highly precise adjustments in afferent arteriolar resistance to modulate glomerular capillary pressure and glomerular filtration rate [36, 55, 95, 97, 98]. Recently, most attention has focused on the respective roles of adenosine versus its precursor, ATP, as direct effectors of autoregulatory vascular responses [33, 55, 95, 97, 98, 101]. The evidence for adenosine in modulating tubuloglomerular feedback arises mainly from micropuncture studies in rat kidneys. Pharmacological blockade of A1 receptors blunts tubuloglomerular feedback-dependent changes in proximal tubule stop-flow pressure stimulated by increasing distal tubular NaCl concentration [108–110]. Tubuloglomerular feedback responses are also inhibited by suppression of adenosine formation from ATP using an antagonist of ecto-5′nucleotidase (the enzyme that catalyses the final reaction in the formation of adenosine), either alone or in combination with continuous administration of an A1 receptor agonist (cyclohexyladenosine) to “clamp” endogenous adenosine levels [109, 111]. Furthermore, mice deficient in ecto-5′-nucleotidase have attenuated tubuloglomerular feedback responses [111, 112]. These observations support a primary role for A1 receptors in mediating tubuloglomerular feedback responses (Fig. 3b). Alternatively, the activation of vasodilatory A2 receptors on afferent arterioles could blunt autoregulatory and tubuloglomerular feedback responses under conditions where A1 receptors are genetically deleted/inactivated or they are blocked pharmacologically [54, 102, 113]. Nevertheless, renal blood flow autoregulation is inhibited by approximately 40% in adenosine A1 receptor-deficient mice and tubuloglomerular feedback responses are attenuated [114, 115]. Interestingly, glomerular filtration rate is normal in these mice. Collectively, these data support the hypothesis that adenosine is an important paracrine signalling molecule for transmitting tubuloglomerular feedback and contribute to whole-kidney autoregulatory responses [114–118].
However, other results suggest that adenosine and A1 receptors are less important for overall autoregulatory resistance adjustments in both in vivo and in vitro settings [30, 54, 113, 119]. Only modest inhibition of tubuloglomerular feedback responses was observed during peritubular perfusion with adenosine receptor antagonists or saturating concentrations of adenosine [54], and autoregulation of renal blood flow and glomerular filtration rate remains normal in the canine kidney during adenosine receptor blockade [30, 119]. Micropuncture studies revealed that blockade of adenosine A1 receptors dilated rat afferent arterioles and their upstream arterial segments, but tubuloglomerular feedback responses remained intact [34, 54]. Pressure-mediated vasoconstriction of rat juxtamedullary afferent arterioles is unaffected by blockade of A1 receptors [33, 120]. During saturation of adenosine receptors with high doses of adenosine, marked vasodilation and loss of afferent autoregulatory responses occurred via an A2 receptor mechanism [113]. Blockade of A2 receptors alone or combined A2 and A1 receptor antagonism restored afferent arteriolar autoregulatory capability [113]. Collectively, these studies suggest that adenosine modulates autoregulatory responses via selective activation of A1 and A2 receptors, but is not essential for the manifestation of autoregulatory responses.
An alternative hypothesis is that extracellular ATP serves as the primary signalling molecule mediating renal autoregulatory and tubuloglomerular feedback responses (Fig. 3b) [33, 43, 51, 54, 95, 97, 120–125]. Microdialysis of the renal cortical interstitium reveals that the concentration of ATP in the cortical interstitial fluid increases as renal arterial pressure increases and as autoregulatory adjustments in renal vascular resistance occur. Interstitial adenosine concentrations do not change during this period [36, 120, 124, 125]. Renal cortical interstitial ATP concentration also increases when tubuloglomerular feedback responses are induced by increasing distal volume delivery by means of acetazolamide treatment [120, 125]. Conversely, interstitial ATP concentration decreases when tubuloglomerular feedback responses are inhibited with furosemide [120, 125]. These manipulations of tubuloglomerular feedback signals do not alter renal interstitial adenosine concentrations. In addition, pressure- and tubular flow-mediated increases in renal cortical interstitial ATP concentration were maintained in kidneys treated with the L-type Ca2+ channel blocker, nifedipine, which completely prevented autoregulatory adjustments in renal vascular resistance, indicating that changes in interstitial ATP concentrations precede changes in renal vascular resistance [124]. Thus, interstitial ATP concentrations are directly correlated with conditions that evoke tubuloglomerular feedback and myogenic autoregulatory responses, consistent with extracellular ATP mediating autoregulatory adjustments in preglomerular vascular resistance (Fig. 3b).
As indicated above, afferent arterioles represent the primary preglomerular renal microvascular element that sets and regulates renal vascular resistance. Traditionally, direct assessment of afferent arteriolar responses to vasoactive stimuli has been accomplished either using isolated, cannulated arterioles held on perfusion pipettes in vitro or using hydronephrotic kidneys in vitro or in vivo. The in vitro blood-perfused juxtamedullary nephron preparation presents a unique opportunity to directly observe renal microvascular function without separating the vascular element from upstream or downstream vascular segments and while maintaining the association of the blood vessel with the tubular structures it serves [126–129]. Accordingly, this preparation provides a useful tool for observing myogenic and tubuloglomerular feedback contributions to renal autoregulation [99, 130]. With this preparation, pressure-mediated afferent arteriolar vasoconstriction is markedly attenuated by P2 purinoceptor desensitisation, by pharmacological blockade of P2 receptors or by genetic deletion of P2X receptors [12, 33, 51, 131]. As shown in Fig. 4, pressure-mediated afferent arteriolar autoregulatory vasoconstriction was inhibited by non-selective P2 receptor blockade with suramin or PPADS or by more selective P2X receptor blockade with NF-279 [33, 51]. Furthermore, mice lacking P2X1 receptors exhibit impaired pressure-mediated afferent arteriolar vasoconstriction [33]. While it was clear that deletion or inactivation of P2X1 receptors inhibited autoregulatory behaviour, it was not clear if this inhibition reflected loss of myogenic behaviour or tubuloglomerular feedback influences. In order to try to identify which component of autoregulation was influenced by P2X1 receptor inactivation, experiments were performed to delete the tubuloglomerular feedback component. The rationale was that if tubuloglomerular feedback responses were already absent in the P2X1 knockout mice, then interventions designed to inhibit tubuloglomerular feedback responses would have no effect on the autoregulatory response in these mice, whereas the same interventions would attenuate overall autoregulatory responses in normal wild-type mice by subtracting the tubuloglomerular feedback contribution from the overall autoregulatory response. Accordingly, tubuloglomerular feedback responses were inhibited by either by resection of the loops of Henle (papillectomy) or by exogenous administration of furosemide. Acute papillectomy interrupts the flow of distal tubular fluid past the macula densa and minimises tubuloglomerular feedback-dependent influences on afferent arteriolar function [33, 99, 132–134], while furosemide administration has been used to inhibit tubuloglomerular feedback responses by inhibiting the NKCC-2 transporter in the apical membrane of the macula densa cells [33, 125, 132, 133, 135–141]. Using these strategies, it was clear that pressure-mediated autoregulatory responses were significantly blunted in wild-type mice, whereas furosemide or papillectomy had no effect on the autoregulatory response observed in P2X1 receptor knockout mice [33]. This observation suggests that the tubuloglomerular feedback component of the autoregulatory response is already absent in mice lacking P2X1 receptors. Further support for the P2X1 receptor hypothesis arises from the observation that afferent arterioles from P2X1 knockout mice vasoconstrict during A1 receptor stimulation with the A1 receptor agonist, N6-cyclopentyl adenosine, and A1 receptor-mediated vasoconstriction of rat afferent arterioles was not affected by P2X1 receptor blockade with NF-279 [33]. Thus, P2X1 receptor knockout mice exhibit blunted autoregulatory behaviour despite retaining a functional adenosine receptor system. These data suggest that ATP-sensitive P2X1 receptors are essential signalling components of pressure-mediated autoregulatory behaviour and for translating macula densa signals into tubuloglomerular feedback-mediated vasoconstriction of afferent arterioles.
Fig. 4.
Effect of P2 receptor blockade on the afferent arteriolar autoregulatory response induced by an increase in perfusion pressure. Pressure-mediated afferent arteriolar autoregulatory responses are depicted before and during P2 receptor blockade with NF-279 (top panel), PPADS (centre panel) and suramin (bottom panel). Autoregulatory responses were induced by increasing perfusion pressure in 30 mmHg increments at 5-min intervals. The data are expressed as a percentage of the control diameter and each data point represents the average diameter response over the last 2 min of each period. Control responses are shown by the black symbols and the response during P2 receptor blockade are shown by the grey symbols. At the end of each protocol, perfusion pressure was returned to 100 mmHg to determine recovery for the pressure stimulus. Data are modified from earlier reports [33, 51]
That ATP is a mediator of tubuloglomerular feedback signals is supported by recent studies showing that macula densa cells release ATP in response to conditions known to evoke tubuloglomerular feedback responses [121–123]. Using a microdissected glomerular preparation with an attached macula densa, Bell et al [121] determined that ATP was released from the basolateral aspect of the macula densa in response to a tubuloglomerular feedback stimulus. They used biosensor cells overexpressing P2X receptors to monitor cellular responses by whole-cell patch clamp. When the biosensor was placed in close proximity to the basolateral surface of the macula densa, a tubuloglomerular feedback stimulus stimulated an increase in the intracellular calcium concentration in the biosensor cell. The calcium concentration in the biosensor cell also increased when exposed to ATP directly, or when the NaCl concentration in the distal tubular fluid was increased. The calcium response was prevented if the biosensor was moved away from the macula densa. These data argue that ATP, or another purinergic substance, is released from the basolateral aspect of the macula densa into the surrounding fluid.
Studies using the isolated perfused rabbit juxtaglomerular apparatus, combined with confocal fluorescence imaging, demonstrate propagation of a calcium signal from the macula densa toward the proximal afferent arteriole, the adjacent glomerulus and intraglomerular cells, in response to increasing tubular flow past the macula densa [142]. Propagation of the calcium signal and afferent arteriolar vasoconstriction are inhibited by P2 receptor blockade but not by P1 receptor blockade. Accordingly, ATP appears to represent a key signalling molecule linking the macula densa with tubuloglomerular feedback-mediated afferent arteriolar vasoconstriction [143].
Interestingly, increases in tubular fluid flow rate in isolated perfused mouse thick ascending loops of Henle result in P2 receptor-mediated increases in epithelial cell cytosolic calcium concentration [144]. This flow-induced elevation of intracellular calcium concentration was almost completely blocked when the non-selective P2 receptor antagonist, suramin, or the ATP scavenger, apyrase, was added to the bath solution. These data suggest that increasing tubular fluid flow and/or tubular distention stimulate ATP release from the basolateral aspect of the renal tubule into the adjacent bathing medium. Addition of suramin or apyrase to the luminal perfusate also significantly blunted the perfusion-induced increase in intracellular calcium concentration in the tubular epithelial cells. The change in fluid flow is postulated to be detected by mechanical stimulation of a primary cilium extending into the tubular lumen from the apical membrane of the epithelium. This study suggests that mouse thick ascending loop of Henle tubular epithelial cells are capable of detecting changes in tubular distention and/or tubular fluid flow rate and respond by releasing ATP into the tubular fluid and into the “interstitial fluid” adjacent to the basolateral surface of the tubule. Interestingly, similar observations have also been made for other renal tubular epithelia. Mechanical stimulation of apical monocilia has been found to regulate ATP release from cultured mouse collecting duct principal cells [145]. Flow-induced ATP release was robust in cilium-competent monolayers of epithelial cells but significantly blunted in cilium-deficient monolayers [145]. This may represent an important sensory system used by macula densa cells to monitor tubular fluid flow and thereby influence macula densa ATP release. Macula densa cells extend a single cilium from the apical membrane into the tubular lumen [146]. Thus, to extrapolate from observations made in other renal epithelia to the macula densa, mechanical stimulation of the macula densa cilia may trigger ATP release from the basolateral membrane into the interstitial fluid adjacent to the basolateral surface of the macula densa plaque and initiate tubuloglomerular signals to the afferent arteriole.
Metabolism of extracellular ATP involves ectonucleotidases that are highly expressed in the kidney [7, 147–153] (plus see article by Shirley, Vekaria & Sévigny [154] in this Special Issue). Ectonucleotidases cleave ATP to AMP and 5′-nucleotidase hydrolyzes AMP to adenosine. These ecto-enzymes may represent a mechanism by which the interstitial adenosine concentration is regulated through systematic degradation of ATP in the renal interstitial fluid. Thus, ectonucleotidases may catabolize ATP released from the macula densa to yield adenosine that can activate P1 receptors. To distinguish P2 receptor-mediated effects from P1 receptor effects, various pharmacological, biochemical and molecular tools have been used, including metabolically stable P2 receptor agonists, P1 and P2 receptor antagonists, adenosine uptake inhibitors and ectonucleotidase-deficient mice. In isolated perfused rat kidneys, the vascular response to ATP is unaltered by the adenosine receptor antagonist, 8-phenyltheophylline or the adenosine uptake inhibitor, S-(p-nitrobenzyl)-6-thioinosine [45]; indicating that P2 receptors are directly activated by ATP. In juxtamedullary nephrons, ATP-mediated vasoconstriction of afferent arterioles is enhanced during adenosine receptor blockade [21]. However, Takenaka et al reported that enhanced production of adenosine from AMP by intrarenal infusion of 5′-nucleotidase improved autoregulation in Thy-1 nephritic rats, which are a model of mesangial cell ablation pathology associated with impaired autoregulation [153]. Moreover, tubuloglomerular feedback stop-flow pressure responses are attenuated by inhibition of adenosine formation with the 5′-nucleotidase blocker, α β-methylene ADP [109], and by deletion of the gene coding for ecto-5′-nucleotidase (CD73) expression [111, 112]. However, if ATP is not metabolised and its concentration increases in the interstitial fluid, it is possible that it could desensitize P2 receptors and thereby lead to reduced tubuloglomerular feedback reactivity.
Studies were recently performed to assess the ability of the cells making up the glomeruli to catabolize ATP to its main degradation products: ADP, AMP and adenosine [151]. Incubation of isolated glomeruli under control conditions revealed that basal extracellular ATP concentrations in the bathing medium reached 1.0 nM and increased approximately 6.5-fold when ecto-ATPase activity was inhibited with 6-N, N-diethyl-β-γ-dibromomethylene-d-adenosine-5-triphosphate (ARL67156) [151]. In the absence of ecto-ATPase inhibitor, exogenous ATP added to these isolated glomeruli was almost completely hydrolyzed within 20 min, with AMP being the major catabolic product. AMP has little effect on afferent arteriole diameter [151]. Mechanical perturbation of isolated glomeruli during inhibition of ecto-ATPase activity increases the ATP concentration in the bathing medium by approximately 35%. These data demonstrate that ATP is constitutively released from isolated rat glomeruli and that this release is enhanced by mechanical stimulation or glomerular deformation. Glomeruli express detectable ecto-5′-nucleotidase activity which can be modulated by dietary salt [152].
A recent report suggests a potential interaction between ATP- and adenosine-mediated autoregulatory influences and connexins 37 and 40 [155]. Blockade of connexins 37 and 40 attenuated autoregulatory behaviour by approximately 50%. Blunting of the autoregulatory response with connexin blockers was augmented by A1 receptor blockade but not by P2 receptor blockade. However, when A1 and P2 receptor blockers were used together, the impact of connexin inhibitors was significantly enhanced. These data suggest that A1 receptors and P2 receptors may interact with each other and with connexins 37 and 40 to transduce purinergic autoregulatory signals intended to regulate preglomerular resistance. The authors concluded that A1 and P2 receptors are needed to achieve complete whole-kidney autoregulatory behaviour and suggested that A1 and P2 receptors interact in that response.
Purinoceptors in hypertension
Hypertension is frequently associated with progressive renal injury that develops through a number of poorly understood factors [156, 157]. Compromised renal autoregulatory efficiency can be a contributing factor that results in chronic elevation of glomerular capillary pressure and subsequent glomerular injury [96]. Renal autoregulation is impaired in many experimental models of hypertension [106, 158–165]. Given that purinoceptors are important for regulation of renal microvascular function and autoregulation, and for modulation of haemodynamic function and tubular transport, it is reasonable to examine the relationship between purinoceptor function and hypertension-related renal injury. Studies indicate that purinoceptors contribute to the functional adaptations in the development of hypertension and may contribute to the renal pathophysiology of hypertension [162, 166, 167]. P2X7 receptor immunoreactivity is increased in mesangial cells from Ren-2 transgenic hypertensive rats [166]. Renal injury in Ang-II-infused hypertensive rats is ameliorated by treatment with the P2Y12 receptor antagonist, clopidogrel, as well as the non-selective P2 receptor blocker, PPADS, without reducing arterial pressure [168]. Pressure-mediated afferent arteriolar autoregulatory responses are attenuated in Ang-II-infused hypertensive rats [162, 169]. Consistent with impaired autoregulatory behaviour, afferent arteriolar vasoconstrictor responses to ATP and β γ-methylene ATP are markedly attenuated compared with those seen in normotensive controls (Fig. 5a), supporting the hypothesis that P2 receptors are essential elements in the autoregulatory response. Interestingly, afferent arteriolar responses to the P1 receptor agonist, adenosine, were unchanged [11]. P2X1 receptor-mediated impairment of afferent arteriolar vasoconstriction is associated with impaired calcium signalling responses to ATP or β γ-methylene ATP in freshly isolated preglomerular smooth muscle cells from hypertensive rats compared to normotensive controls (Fig. 5b) [11]. Reduction of the calcium signalling response could account for the impaired afferent arteriolar autoregulatory efficiency and thus contribute to hypertension-induced renal and glomerular injury. Attenuated responsiveness to P2 receptor stimulation in this model of hypertension is counter to responses observed with other vasoconstrictor agonists. For example, afferent arteriolar responses to angiotensin II are enhanced in Ang-II-infused hypertensive rats whereas the response to noradrenaline and adenosine are unchanged [160, 170]. Simultaneous loss of autoregulatory responsiveness and responsiveness to P2X1 receptor activation is interesting and supports the argument that normally functioning P2X1 receptors are essential for normal autoregulatory behaviour to occur.
Perspectives
P2 receptors in the control of renal tubular and haemodynamic function remain an emerging and exciting field of study. Evidence that P2 receptors are ubiquitously expressed throughout the kidney but that the receptor expression profile is different between different nephron segments and structures argues that each serves an important physiological function. Studies have not progressed far enough to definitively assign function to receptors expressed in each kidney region. However, compelling data are accumulating that implicate P2 receptors as contributing importantly to both physiological and pathophysiological processes. There is much to be learned about this class of receptors and there is much excitement ahead as their respective roles are defined.
It is clear that P1 and P2 receptors are effective modulators of renal microvascular function. P2X1 receptors are important for pressure-dependent autoregulatory adjustments in renal vascular resistance. The debate continues on whether or not they are important for tubuloglomerular feedback adjustments in afferent arteriole resistance. Many other questions remain to be answered. What is(are) the actual messenger molecule(s) responsible for autoregulatory changes in renal vascular resistance? Is it ATP, adenosine or another yet unidentified substance? Are the myogenic and the tubuloglomerular feedback components of the whole-kidney autoregulatory response mediated by the same messenger molecule? What is the role of renal ectonucleotidases in the physiology of the purine signalling pathways described in this review? Is autoregulatory impairment directly responsible for hypertension-related kidney injury or are there other more important intermediates involved? If failure of the renal vascular purinoceptor system is responsible for some aspects of hypertensive renal injury, could it also be involved in renal injury in other conditions such as diabetes, obesity or immunosuppressive therapies? Answers to these and other questions will help push development of this field and will contribute greatly to our understanding of why these tissue-specific renal purinoceptor receptor systems are distributed the way they are. Time and better investigational tools will help to clarify the physiology of these receptors. Nevertheless, the data generated to date clearly establish the renal P2 receptor system as an important regulatory system for maintaining renal vascular and tubular function.
Acknowledgements
The author wishes to thank Dr. Zhengrong Guan for her assistance in preparing this manuscript. Some of the work described in this review was supported by grants from the American Heart Association and by NIH (DK44628 and HL 074167).
References
- 1.Bailey MA, Hillman KA, Unwin RJ (2000) P2 receptors in the kidney. J Auton Nerv Syst 81:264–270 [DOI] [PubMed]
- 2.Bailey MA, Imbert-Teboul M, Turner C, Marsy S, Srai K, Burnstock G, Unwin RJ (2000) Axial distribution and characterization of basolateral P2Y receptors along the rat renal tubule. Kidney Int 58:1893–1901 [DOI] [PubMed]
- 3.Bailey MA, Turner CM, Hus-Citharel A, Marchetti J, Imbert-Teboul M, Milner P, Burnstock G, Unwin R (2004) P2Y receptors present in the native and isolated rat glomerulus. Nephron Physiol 96:79–90 [DOI] [PubMed]
- 4.Chan CM, Unwin RJ, Bardini M, Oglesby IB, Ford APDW, Townsend-Nicholson A, Burnstock G (1998) Localization of the P2X1 purinoceptors by autoradiography and immunohistochemistry in the rat kidney. Am J Physiol Renal Physiol 274:F799–F804 [DOI] [PubMed]
- 5.Chan CM, Unwin RJ, Burnstock G (1998) Potential functional roles of extracellular ATP in kidney and urinary tract. Exp Nephrol 6:200–207 [DOI] [PubMed]
- 6.Turner CM, Vonend O, Chan C, Burnstock G, Unwin RJ (2003) The pattern of distribution of selected ATP-sensitive P2 receptor subtypes in normal rat kidney: an immunohistological study. Cells Tissues Organs 175:105–117 [DOI] [PubMed]
- 7.Unwin RJ, Bailey MA, Burnstock G (2003) Purinergic signaling along the renal tubule: the current state of play. News Physiol Sci 18:237–241 [DOI] [PubMed]
- 8.Guan Z, Osmond DA, Inscho EW (2007) Purinoceptors in the kidney. Exp Biol Med 232:715–726 [PubMed]
- 9.Rivera I, Zhang S, Fuller BS, Edwards B, Seki T, Wang MH, Marrero MB, Inscho EW (2007) P2 receptor regulation of [Ca2+]i in cultured mouse mesangial cells. Am J Physiol Renal Physiol 292:F1380–F1389 [DOI] [PubMed]
- 10.Leipziger J (2003) Control of epithelial transport via luminal P2 receptors. Am J Physiol Renal Physiol 284:F419–F432 [DOI] [PubMed]
- 11.Zhao X, Cook AK, Field M, Edwards B, Zhang S, Zhang Z, Pollock JS, Imig JD, Inscho EW (2005) Impaired Ca2+ signaling attenuates P2X receptor-mediated vasoconstriction of afferent arterioles in angiotensin II hypertension. Hypertension 46:562–568 [DOI] [PubMed]
- 12.Inscho EW (2001) P2 receptors in the regulation of renal microvascular function. Am J Physiol Renal Physiol 280:F927–F944 [DOI] [PubMed]
- 13.Schwiebert EM, Kishore BK (2001) Extracellular nucleotide signaling along the renal epithelium. Am J Physiol Renal Physiol 280:F945–F963 [DOI] [PubMed]
- 14.Schwiebert EM (2001) ATP release mechanisms, ATP receptors and purinergic signalling along the nephron. Clin Exp Pharmacol Physiol 28:340–350 [DOI] [PubMed]
- 15.Schwiebert EM, Zsembery A (2003) Extracellular ATP as a signaling molecule for epithelial cells. Biochim Biophys Acta 1615:7–32 [DOI] [PubMed]
- 16.Churchill PC, Ellis VR (1993) Purinergic P2Y receptors stimulate renin secretion by rat renal cortical slices. J Pharmacol Exp Ther 266:160–163 [PubMed]
- 17.Yao J, Suwa M, Li B, Kawamura K, Morioka T, Oite T (2003) ATP-dependent mechanism for coordination of intercellular Ca2+ signaling and renin secretion in rat juxtaglomerular cells. Circ Res 93:338–345 [DOI] [PubMed]
- 18.Churchill PC, Churchill MC (1988) Effects of adenosine on renin secretion. Atlas of science. Pharmacology 2:367–373
- 19.Churchill PC, Churchill MC (1985) A1 and A2 adenosine receptor stimulation inhibits and stimulates renin secretion of rat cortical slices. J Pharmacol Exp Ther 232:589–594 [PubMed]
- 20.Schnermann J (1998) Juxtaglomerular cell complex in the regulation of renal salt excretion. Am J Physiol Regul Integr Comp Physiol 274:R263–R279 [DOI] [PubMed]
- 21.Inscho EW, Ohishi K, Navar LG (1992) Effects of ATP on pre- and postglomerular juxtamedullary microvasculature. Am J Physiol Renal, Fluid Electrolyte Physiol 263:F886–F893 [DOI] [PubMed]
- 22.Harada H, Chan CM, Loesch A, Unwin R, Burnstock G (2000) Induction of proliferation and apoptotic cell death via P2Y and P2X receptors, respectively, in rat glomerular mesangial cells. Kidney Int 57:949–958 [DOI] [PubMed]
- 23.Mohaupt MG, Fischer T, Schwöbel J, Sterzel RB, Schulze-Lohoff E (1998) Activation of purinergic P2Y2 receptors inhibits inducible NO synthase in cultured rat mesangial cells. Am J Physiol Renal Physiol 275:F103–F110 [DOI] [PubMed]
- 24.Carmines PK, Inscho EW (1994) Renal arteriolar angiotensin responses during varied adenosine receptor activation. Hypertension 23:I114–I119 [DOI] [PubMed]
- 25.Drury AN, Szent-Györgyi A (1929) The physiological activity of adenine compounds with special reference to their action upon the mammalian heart. J Physiol (Lond) 68:213–237 [DOI] [PMC free article] [PubMed]
- 26.Hansen PB, Castrop H, Briggs J, Schnermann J (2003) Adenosine induces vasoconstriction through Gi-dependent activation of phospholipase C in isolated perfused afferent arterioles of mice. J Am Soc Nephrol 14:2457–2465 [DOI] [PubMed]
- 27.Hansen PB, Hashimoto S, Oppermann M, Huang Y, Briggs J, Schnermann J (2005) Vasoconstrictor and vasodilator effects of adenosine in the mouse kidney due to preferential activation of A1 or A2 adenosine receptors. J Pharmacol Exp Ther 315:1150–1157 [DOI] [PubMed]
- 28.Hansen PB, Schnermann J (2003) Vasoconstrictor and vasodilator effects of adenosine in the kidney. Am J Physiol Renal Physiol 285:F590–F599 [DOI] [PubMed]
- 29.Holz FG, Steinhausen M (1987) Renovascular effects of adenosine receptor agonists. Ren Physiol 10:272–282 [DOI] [PubMed]
- 30.Ibarrola AM, Inscho EW, Vari RC, Navar LG (1991) Influence of adenosine receptor blockade on renal function and autoregulation. J Am Soc Nephrol 2:991–999 [DOI] [PubMed]
- 31.Inscho EW, Carmines PK, Navar LG (1991) Juxtamedullary afferent arteriolar responses to P1 and P2 purinergic stimulation. Hypertension 17:1033–1037 [DOI] [PubMed]
- 32.Inscho EW, Mitchell KD, Navar LG (1994) Extracellular ATP in the regulation of renal microvascular function. FASEB J 8:319–328 [DOI] [PubMed]
- 33.Inscho EW, Cook AK, Imig JD, Vial C, Evans RJ (2003) Physiological role for P2X1 receptors in renal microvascular autoregulatory behavior. J Clin Invest 112:1895–1905 [DOI] [PMC free article] [PubMed]
- 34.Kawabata M, Ogawa T, Takabatake T (1998) Control of rat glomerular microcirculation by juxtaglomerular adenosine A1 receptors. Kidney Int 54:S228–S230 [DOI] [PubMed]
- 35.Nishiyama A, Inscho EW, Navar LG (2001) Interactions of adenosine A1 and A2a receptors on renal microvascular reactivity. Am J Physiol Renal Physiol 280:F406–F414 [DOI] [PubMed]
- 36.Nishiyama A, Rahman M, Inscho EW (2004) Role of interstitial ATP and adenosine in the regulation of renal hemodynamics and microvascular function. Hypertension Research 27:791–804 [DOI] [PubMed]
- 37.Osswald H, Spielman WS, Knox FG (1978) Mechanism of adenosine-mediated decreases in glomerular filtration rate in dogs. Circ Res 43:465–469 [DOI] [PubMed]
- 38.Schnermann J, Traynor T, Yang TX, Arend L, Huang YNG, Smart A, Briggs JP (1998) Tubuloglomerular feedback: new concepts and developments. Kidney Int 54:S40–S45 [DOI] [PubMed]
- 39.Eppel GA, Malpas SC, Denton KM, Evans RG (2004) Neural control of renal medullary perfusion. Clin Exp Pharmacol Physiol 31:387–396 [DOI] [PubMed]
- 40.Traynor T, Yang TX, Huang YG, Arend L, Oliverio MI, Coffman T, Briggs JP, Schnermann J (1998) Inhibition of adenosine-1 receptor-mediated preglomerular vasoconstriction in AT1A receptor-deficient mice. Am J Physiol Renal Physiol 275:F922–F927 [DOI] [PubMed]
- 41.Weihprecht H, Lorenz JN, Briggs JP, Schnermann J (1992) Vasomotor effects of purinergic agonists in isolated rabbit afferent arterioles. Am J Physiol Renal Fluid Electrolyte Physiol 263:F1026–F1033 [DOI] [PubMed]
- 42.Weihprecht H, Lorenz JN, Briggs JP, Schnermann J (1994) Synergistic effects of angiotensin and adenosine in the renal microvasculature. Am J Physiol 266:F227–F239 [DOI] [PubMed]
- 43.Majid DSA, Inscho EW, Navar LG (1999) P2 purinoceptor saturation by adenosine triphosphate impairs renal autoregulation in dogs. J Am Soc Nephrol 10:492–498 [DOI] [PubMed]
- 44.Majid DSA, Navar LG (1992) Suppression of blood flow autoregulation plateau during nitric oxide blockade in canine kidney. Am J Physiol Renal Fluid Electrolyte Physiol 262:F40–F46 [DOI] [PubMed]
- 45.Eltze M, Ullrich B (1996) Characterization of vascular P2 purinoceptors in the rat isolated perfused kidney. Pflügers Arch 306:139–152 [DOI] [PubMed]
- 46.Fernández O, Wangensteen R, Osuna A, Vargas F (2000) Renal vascular reactivity to P2-purinoceptor activation in spontaneously hypertensive rats. Pharmacol 60:47–50 [DOI] [PubMed]
- 47.Vargas F, Moreno MRR, Osuna A (1996) Renal vascular reactivity to ATP in ageing rats. Med Sci Res 24:263–265
- 48.Vargas F, Osuna A, Fernández-Rivas A (1996) Renal vascular reactivity to ATP in hyper- and hypothyroid rats. Experientia 52:225–229 [DOI] [PubMed]
- 49.Churchill PC, Ellis VR (1993) Pharmacological characterization of the renovascular P2 purinergic receptors. J Pharmacol Exp Ther 265:334–338 [PubMed]
- 50.Dobrowolski L, Walkowska A, Kompanowska-Jezierska E, Kuczeriszka M, Sadowski J (2007) Effects of ATP on rat renal haemodynamics and excretion: role of sodium intake, nitric oxide and cytochrome P450. Acta Physiologica 189:77–85 [DOI] [PubMed]
- 51.Inscho EW, Cook AK, Navar LG (1996) Pressure-mediated vasoconstriction of juxtamedullary afferent arterioles involves P2-purinoceptor activation. Am J Physiol Renal, Fluid Electrolyte Physiol 271:F1077–F1085 [DOI] [PubMed]
- 52.Gutierrez AM, Kornfeld M, Persson AE (1999) Calcium response to adenosine and ATP in rabbit afferent arterioles. Acta Physiol Scand 166:175–181 [DOI] [PubMed]
- 53.Inscho EW (2001) Renal microvascular effects of P2 receptor stimulation. Clin Exp Pharmacol Physiol 28:332–339 [DOI] [PubMed]
- 54.Mitchell KD, Navar LG (1993) Modulation of tubuloglomerular feedback responsiveness by extracellular ATP. Am J Physiol Renal Fluid Electrolyte Physiol 264:F458–F466 [DOI] [PubMed]
- 55.Navar LG, Inscho EW, Majid DSA, Imig JD, Harrison-Bernard LM, Mitchell KD (1996) Paracrine regulation of the renal microcirculation. Physiol Rev 76:425–536 [DOI] [PubMed]
- 56.Eppel GA, Ventura S, Denton KM, Evans RG (2006) Lack of contribution of P2X receptors to neurally mediated vasoconstriction in the rabbit kidney in vivo. Acta Physiologica 186:197–207 [DOI] [PubMed]
- 57.Eppel GA, Ventura S, Evans RG (2007) Regional vascular responses to ATP and ATP analogues in the rabbit kidney in vivo: roles for adenosine receptors and prostanoids. Br J Pharmacol 149:523–531 [DOI] [PMC free article] [PubMed]
- 58.Carmines PK, Inscho EW, Gensure RC (1990) Arterial pressure effects on preglomerular microvasculature of juxtamedullary nephrons. Am J Physiol 258:F94–F102 [DOI] [PubMed]
- 59.Inscho EW, LeBlanc EA, Pham BT, White SM, Imig JD (1999) Purinoceptor-mediated calcium signaling in preglomerular smooth muscle cells. Hypertension 33:195–200 [DOI] [PubMed]
- 60.Inscho EW, Cook AK, Mui V, Miller J (1998) Direct assessment of renal microvascular responses to P2-purinoceptor agonists. Am J Physiol Renal Physiol 274:F718–F727 [DOI] [PubMed]
- 61.Wangensteen R, Fernandez O, Sainz J, Quesada A, Vargas F, Osuna A (2000) Contribution of endothelium-derived relaxing factors to P2Y-purinoceptor-induced vasodilation in the isolated rat kidney. General Pharmacology: The Vascular System 35:129–133 [DOI] [PubMed]
- 62.Keef KD, Pasco JS, Eckman DM (1992) Purinrgic relaxation and hyperpolarization in guinea pig and rabbit coronary artery: Role of endothelium. J Pharmacol Exp Ther 260:592–600 [PubMed]
- 63.Malmsjö M, Edvinsson L, Erlinge D (1998) P2U-receptor mediated endothelium-dependent but nitric oxide- independent vascular relaxation. Br J Pharmacol 123:719–729 [DOI] [PMC free article] [PubMed]
- 64.Malmsjö M, Erlinge D, Högestätt ED, Zygmunt PM (1999) Endothelial P2Y receptors induce hyperpolarisation of vascular smooth muscle by release of endothelium-derived hyperpolarising factor. Eur J Pharmacol 364:169–173 [DOI] [PubMed]
- 65.Malmsjö M, ZM Chu, Croft K, Erlinge D, Edvinsson L, Beilin LJ (2002) P2Y receptor-induced EDHF vasodilatation is of primary importance for the regulation of perfusion pressure in the peripheral circulation of the rat. Acta Physiol Scand 174:301–309 [DOI] [PubMed]
- 66.Wihlborg AK, Malmsjö M, Eyjolfsson A, Gustafsson R, Jacobson K, Erlinge D (2003) Extracellular nucleotides induce vasodilatation in human arteries via prostaglandins, nitric oxide and endothelium-derived hyperpolarising factor. Br J Pharmacol 138:1451–1458 [DOI] [PMC free article] [PubMed]
- 67.Pfeilschifter J (1990) Comparison of extracellular ATP and UTP signalling in rat renal mesangial cells. Biochem J 272:469–472 [DOI] [PMC free article] [PubMed]
- 68.Gutierrez AM, Lou XF, Persson AEG, Ring A (1999) Ca2+ response of rat mesangial cells to ATP analogues. Eur J Pharmacol 369:107–112 [DOI] [PubMed]
- 69.Takeda M, Kawamura T, Kobayashi M, Endou H (1996) ATP-induced calcium mobilization in glomerular mesangial cells is mediated by P2u purinoceptor. Biochem Mol Biol Int 39:1193–1200 [DOI] [PubMed]
- 70.Pavenstädt H, Gloy J, Leipziger J, Klär B, Pfeilschifter J, Schollmeyer P, Greger R (1993) Effect of extracellular ATP on contraction, cytosolic calcium activity, membrane voltage, and ion currents of rat mesangial cells in primary culture. Br J Pharmacol 109:953–959 [DOI] [PMC free article] [PubMed]
- 71.Pfeilschifter J, Huwiler A, Briner VA (1995) Proliferative mechanisms in kidney cells. Curr Opin Nephrol Hypertension 4:98–103 [DOI] [PubMed]
- 72.Inscho EW, Belott TP, Mason MJ, Smith JB, Navar LG (1996) Extracellular ATP increases cytosolic calcium in cultured renal arterial smooth muscle cells. Clin Exp Pharmacol Physiol 23:503–507 [DOI] [PubMed]
- 73.Inscho EW, Schroeder AC, Deichmann PC, Imig JD (1999) ATP-mediated Ca2+ signaling in preglomerular smooth muscle cells. Am J Physiol Renal Physiol 276:F450–F456 [DOI] [PubMed]
- 74.White SM, Imig JD, Inscho EW (2001) Calcium signaling pathways utilized by P2X receptors in preglomerular vascular smooth muscle cells. Am J Physiol Renal Physiol 280:F1054–F1061 [DOI] [PubMed]
- 75.Inscho EW, Cook AK (2002) P2 receptor-mediated afferent arteriolar vasoconstriction during calcium channel blockade. Am J Physiol Renal Physiol 282:F245–F255 [DOI] [PubMed]
- 76.Inscho EW, Ohishi K, Cook AK, Belott TP, Navar LG (1995) Calcium activation mechanisms in the renal microvascular response to extracellular ATP. Am J Physiol Renal, Fluid Electrolyte Physiol 268:F876–F884 [DOI] [PubMed]
- 77.Yiu SS, Zhao X, Inscho EW, Imig JD (2003) 12-Hydroxyeicosatetraenoic acid participates in angiotensin II afferent arteriolar vasoconstriction by activating L-type calcium channels. J Lipid Res 44:2391–2399 [DOI] [PubMed]
- 78.Miyata N, Roman RJ (2005) Role of 20-hydroxyeicosatetraenoic acid (20-HETE) in vascular system. J Smooth Muscle Res 41:175–193 [DOI] [PubMed]
- 79.Roman RJ (2002) P-450 metabolites of arachidonic acid in the control of cardiovascular function. Physiol Rev 82:131–185 [DOI] [PubMed]
- 80.Maier KG, Roman RJ (2001) Cytochrome P450 metabolites of arachidionic acid in the control of renal function. Curr Opin Nephrol Hypertens 10:81–87 [DOI] [PubMed]
- 81.Zhao XY, Inscho EW, Bondlela M, Falck JR, Imig JD (2001) The CYP450 hydroxylase pathway contributes to P2X receptor-mediated afferent arteriolar vasoconstriction. Am J Physiol Heart Circ Physiol 281:H2089–H2096 [DOI] [PubMed]
- 82.Zhao X, Falck JR, Gopal VR, Inscho EW, Imig JD (2004) P2X receptor-stimulated calcium responses in preglomerular vascular smooth muscle cells involves 20-hydroxyeicosatetraenoic acid. J Pharmacol Exp Ther 311:1211–1217 [DOI] [PubMed]
- 83.Somlyo AP, Somlyo AV (2003) Ca2+ sensitivity of smooth muscle and nonmuscle myosin II: modulated by G proteins, kinases, and myosin phosphatase. Physiol Rev 83:1325–1358 [DOI] [PubMed]
- 84.Hirano K (2007) Current topics in the regulatory mechanism underlying the Ca2+ sensitization of the contractile apparatus in vascular smooth muscle. J Pharmacol Sci 109:109–115 [DOI] [PubMed]
- 85.Chitaley K, Weber D, Webb RC (2001) RhoA/Rho-kinase, vascular changes, and hypertension. Curr Hypertension Rep 3:139–144 [DOI] [PubMed]
- 86.Cavarape A, Bauer J, Bartoli E, Endlich K, Parekh N (2003) Effects of angiotensin II, arginine vasopressin and tromboxane A2 in renal vascular bed: role of rho-kinase. Nephrol Dial Transplant 18:1764–1769 [DOI] [PubMed]
- 87.Cavarape A, Endlich N, Assaloni R, Bartoli E, Steinhausen M, Parekh N, Endlich K (2003) Rho-kinase inhibition blunts renal vasoconstriction induced by distinct signaling pathways in vivo. J Am Soc Nephrol 14:37–45 [DOI] [PubMed]
- 88.Inscho EW, Cook AK, Webb RC (2009) Rho-kinase inhibition reduces pressure-mediated autoregulatory adjustments in afferent arteriolar diameter. Am J Renal Physiol 296:F590–F597 [DOI] [PMC free article] [PubMed]
- 89.Jankowski M, Szczepanska-Konkel K, Kalinowski L, Angielski S (2003) Involvement of rho-kinase in P2Y-receptor-mediated contraction of renal glomeruli. Biochem Biophys Res Commun 302:855–859 [DOI] [PubMed]
- 90.Sakurada S, Okamoto H, Takuwa N, Sugimoto N, Takuwa Y (2001) Rho activation in excitatory agonist-stimulated vascular smooth muscle. Am J Physiol Cell Physiol 281:C571–C578 [DOI] [PubMed]
- 91.Randriamboavonjy V, Busse R, Fleming I (2003) 20-HETE-induced contraction of small coronary arteries depends on the activation of rho-kinase. Hypertension 41:801 [DOI] [PubMed]
- 92.Sauzeau V, Le Jeune H, Cario-Toumaniantz C, Vaillant N, Gadeau AP, Desgranges C, Scalbert E, Chardin P, Pacaud P, Loirand G (2000) P2Y1, P2Y2, P2Y4, and P2Y6 receptors are coupled to Rho and Rho kinase activation in vascular myocytes. Am J Physiol Heart Circ Physiol 278:H1751 [DOI] [PubMed]
- 93.Schubert R, Kalentchuk VU, Krien U (2002) Rho kinase inhibition partly weakens myogenic reactivity in rat small arteries by changing calcium sensitivity. Am J Physiol Heart Circ Physiol 283:H2288 [DOI] [PubMed]
- 94.Arendshorst WJ, Navar LG (1993) Renal circulation and glomerular hemodynamics. In: Schrier RW, Gottschalk C (eds) Diseases of the kidney. Little, Brown and Co, Boston, pp 65–117
- 95.Just A (2007) Mechanisms of renal blood flow autoregulation: dynamics and contributions. Am J Physiol Regul Integr Comp Physiol 292:R1–R17 [DOI] [PubMed]
- 96.Loutzenhiser R, Griffin K, Williamson G, Bidani A (2006) Renal autoregulation: new perspectives regarding the protective and regulatory roles of the underlying mechanisms. Am J Physiol Regul Integr Comp Physiol 290:R1153–R1167 [DOI] [PMC free article] [PubMed]
- 97.Castrop H (2007) Mediators of tubuloglomerular feedback regulation of glomerular filtration: ATP and adenosine. Acta Physiologica 189:3–14 [DOI] [PubMed]
- 98.Schnermann J, Levine DZ (2003) Paracrine factors in tubuloglomerular feedback: adenosine, ATP and nitric oxide. Ann Rev Physiol 65:501–529 [DOI] [PubMed]
- 99.Takenaka T, Harrison-Bernard LM, Inscho EW, Carmines PK, Navar LG (1994) Autoregulation of afferent arteriolar blood flow in juxtamedullary nephrons. Am J Physiol 267:F879–F887 [DOI] [PubMed]
- 100.Vallon V (2003) Tubuloglomerular feedback and the control of glomerular filtration rate. News Physiol Sci 18:169–174 [DOI] [PubMed]
- 101.Vallon V, Muhlbauer B, Osswald H (2006) Adenosine and kidney function. Physiol Rev 86:901–940 [DOI] [PubMed]
- 102.Nishiyama A, Navar LG (2002) ATP mediates tubuloglomerular feedback. Am J Physiol Regul Integr Comp Physiol 283:R273–R275 [DOI] [PubMed]
- 103.Schnermann J (2002) Adenosine mediates tubuloglomerular feedback. Am J Physiol Regul Integr Comp Physiol 283:R276–R277 [DOI] [PubMed]
- 104.Bell PD, Lapointe JY, Peti-Peterdi J (2003) Macula densa cell signaling. Ann Rev Physiol 65:481–500 [DOI] [PubMed]
- 105.Komlosi P, Fintha A, Bell PD (2004) Current mechanisms of macula densa cell signalling. Acta Physiol Scand 181:463–469 [DOI] [PubMed]
- 106.Persson PB (2002) Renal blood flow autoregulation in blood pressure control. Curr Opin Nephrol Hypertension 11:67–72 [DOI] [PubMed]
- 107.Bell PD, Komlosi P, Zhang Z (2008) ATP as a mediator of macula densa cell signalling. Pur Sig (in press) [DOI] [PMC free article] [PubMed]
- 108.Schnermann J, Weihprecht H, Briggs JP (1990) Inhibition of tubuloglomerular feedback during adenosine1 receptor blockade. Am J Physiol 258:F553–F561 [DOI] [PubMed]
- 109.Thomson S, Bao DJ, Deng A, Vallon V (2000) Adenosine formed by 5'-nucleotidase mediates tubuloglomerular feedback. J Clin Invest 106:289–298 [DOI] [PMC free article] [PubMed]
- 110.Ren Y, Arima S, Carretero OA, Ito S (2002) Possible role of adenosine in macula densa control of glomerular hemodynamics. Kidney Int 61:169–176 [DOI] [PubMed]
- 111.Castrop H, Huang Y, Hashimoto S, Mizel D, Hansen P, Theilig F, Bachmann S, Deng C, Briggs J, Schnermann J (2004) Impairment of tubuloglomerular feedback regulation of GFR in ecto-5'-nucleotidase/CD73–deficient mice. J Clin Invest 114:634–642 [DOI] [PMC free article] [PubMed]
- 112.Huang DY, Vallon V, Zimmermann H, Koszalka P, Schrader J, Osswald H (2006) Ecto-5'-nucleotidase (cd73)-dependent and -independent generation of adenosine participates in the mediation of tubuloglomerular feedback in vivo. Am J Physiol Renal Physiol 291:F282–F288 [DOI] [PubMed]
- 113.Feng MG, Navar LG (2007) Adenosine A2 receptor activation attenuates afferent arteriolar autoregulation during adenosine receptor saturation in rats. Hypertension 50:744–749 [DOI] [PubMed]
- 114.Hashimoto S, Huang Y, Briggs J, Schnermann J (2006) Reduced autoregulatory effectiveness in adenosine 1 receptor-deficient mice. Am J Physiol Renal Physiol 290:F888–F891 [DOI] [PubMed]
- 115.Just A, Arendshorst WJ (2007) A novel mechanism of renal blood flow autoregulation and the autoregulatory role of A1 adenosine receptors in mice. Am J Physiol Renal Physiol 293:F1489–F1500 [DOI] [PubMed]
- 116.Brown R, Ollerstam A, Johansson B, Skott O, Gebre-Medhin S, Fredholm B, Persson AEG (2001) Abolished tubuloglomerular feedback and increased plasma renin in adenosine A1 receptor-deficient mice. Am J Physiol Regul Integr Comp Physiol 281:R1362–R1367 [DOI] [PubMed]
- 117.Sun D, Samuelson LC, Yang T, Huang Y, Paliege A, Saunders T, Briggs J, Schnermann J (2001) Mediation of tubuloglomerular feedback by adenosine: Evidence from mice lacking adenosine A1 receptors. Proc Natl Acad Sci USA 98:9983–9988 [DOI] [PMC free article] [PubMed]
- 118.Vallon V, Richter K, Huang DY, Rieg T, Schnermann J (2004) Functional consequences at the single-nephron level of the lack of adenosine A1 receptors and tubuloglomerular feedback in mice. Pflugers Arch V448:214–221 [DOI] [PubMed]
- 119.Premen AJ, Hall JE, Mizelle HL, Cornell JE (1985) Maintenance of renal autoregulation during infusion of aminophylline or adenosine. Am J Physiol Renal Physiol 248:F366–F373 [DOI] [PubMed]
- 120.Nishiyama A, Majid DSA, Walker MIII, Miyatake A, Navar LG (2001) Renal interstitial ATP responses to changes in arterial pressure during alterations in tubuloglomerular feedback activity. Hypertension 37:753–759 [DOI] [PubMed]
- 121.Bell PD, Lapointe J-Y, Sabirov R, Hayashi S, Peti-Peterdi J, Manabe K, Kovacs G, Okada Y (2003) Macula densa cell signaling involves ATP release through a maxi anion channel. Proc Natl Acad Sci USA 100:4322–4327 [DOI] [PMC free article] [PubMed]
- 122.Komlosi P, Peti-Peterdi J, Fuson AL, Fintha A, Rosivall L, Bell PD (2004) Macula densa basolateral ATP release is regulated by luminal [NaCl] and dietary salt intake. Am J Physiol Renal Physiol 286:F1054–F1058 [DOI] [PubMed]
- 123.Liu R, Bell PD, Peti-Peterdi J, Kovacs G, Johansson A, Persson AEG (2002) Purinergic receptor signaling at the basolateral membrane of macula densa cells. J Am Soc Nephrol 13:1145–1151 [DOI] [PubMed]
- 124.Nishiyama A, Jackson KE, Majid DSA, Rahman M, Navar LG (2006) Renal interstitial fluid ATP responses to arterial pressure and tubuloglomerular feedback activation during calcium channel blockade. Am J Physiol Heart Circ Physiol 290:H772–H777 [DOI] [PubMed]
- 125.Nishiyama A, Majid DSA, Taher KA, Miyatake A, Navar LG (2000) Relation between renal interstitial ATP concentrations and autoregulation-mediated changes in renal vascular resistance. Circ Res 86:656–662 [DOI] [PubMed]
- 126.Casellas D, Navar LG (1984) In vitro perfusion of juxtamedullary nephrons in rats. Am J Physiol Renal, Fluid Electrolyte Physiol 246:F349–F358 [DOI] [PubMed]
- 127.Casellas D, Carmines PK, Navar LG (1985) Microvascular reactivity of in vitro blood perfused juxtamedullary nephrons from rats. Kidney Int 28:752–759 [DOI] [PubMed]
- 128.Casellas D, Taugner R (1986) Renin status of the afferent arteriole and ultrastructure of the juxtaglomerular apparatus in "superficial" juxtamedullary nephrons from rats. Ren Physiol 9:348–356 [DOI] [PubMed]
- 129.Inscho EW (2000) The in vitro blood perfused juxtamedullary nephron technique. In: Wang DH (ed) Methods in Molecular Medicine. Humana Press, Totowa, pp 435–449 [DOI] [PubMed]
- 130.Walker MIII, Harrison-Bernard LM, Cook AK, Navar LG (2000) Dynamic interaction between myogenic and TGF mechanisms in afferent arteriolar blood flow autoregulation. Am J Physiol Renal Physiol 279:F858–F865 [DOI] [PubMed]
- 131.Inscho EW, Cook AK, Imig JD, Vial C, Evans RJ (2004) Renal autoregulation in P2X1 knockout mice. Acta Physiol Scand 181:445–453 [DOI] [PubMed]
- 132.Ikenaga H, Fallet RW, Carmines PK (1996) Contribution of tubuloglomerular feedback to renal arteriolar angiotensin II responsiveness. Kidney Int 49:34–39 [DOI] [PubMed]
- 133.Sanchez-Ferrer CF, Roman RJ, Harder DR (1989) Pressure-dependent contraction of rat juxtamedullary afferent arterioles. Circ Res 64:790–798 [DOI] [PubMed]
- 134.Ichihara A, Inscho EW, Imig JD, Navar LG (1998) Neuronal nitric oxide synthase modulates rat renal microvascular function. Am J Physiol Renal Physiol 274:F516–F524 [DOI] [PubMed]
- 135.Duchin KL, Peterson LN, Burke TJ (1977) Effect of furosemide on renal autoregulation. Kidney Int 12:379–386 [DOI] [PubMed]
- 136.Wright FS, Briggs P (1977) Feedback regulation of glomerular filtration rate. Am J Physiol Renal Physiol 233:F1–F7 [DOI] [PubMed]
- 137.Moore LC, Schnermann J, Yarimizu S (1979) Feedback mediation of SNGFR autoregulation in hydropenic and DOCA- and salt-loaded rats. Am J Physiol Renal Physiol 237:F63–F74 [DOI] [PubMed]
- 138.Schnermann J, Briggs J (1982) Concentration-dependent sodium choride transport as the signal in feedback control of glomerular filtration rate. Kidney Int 22:S82–S89 [PubMed]
- 139.Casellas D, Moore LC (1990) Autoregulation and tubuloglomerular feedback in juxtamedullary glomerular arterioles. Am J Physiol Renal Physiol 258:F660–F669 [DOI] [PubMed]
- 140.Moore LC, Casellas D (1990) Tubuloglomerular feedback dependence of autoregulation in rat juxtamedullary afferent arterioles. Kidney Int 37:1402–1408 [DOI] [PubMed]
- 141.Schnermann J (1988) Effect of adenosine analogues on tubuloglomerular feedback responses. Am J Physiol 255:F33–F42 [DOI] [PubMed]
- 142.Peti-Peterdi J (2006) Calcium wave of tubuloglomerular feedback. Am J Physiol Renal Physiol 291:F473–F480 [DOI] [PubMed]
- 143.Komlosi P, Fintha A, Bell PD (2005) Renal cell-to-cell communication via extracellular ATP. Physiology 20:86–90 [DOI] [PubMed]
- 144.Jensen MEJ, Odgaard E, Christensen MH, Praetorius HA, Leipziger J (2007) Flow-induced [Ca2+]i increase depends on nucleotide release and subsequent purinergic signaling in the intact nephron. J Am Soc Nephrol 18:2062–2070 [DOI] [PubMed]
- 145.Hovater MB, Olteanu D, Hanson EL, Cheng NL, Siroky B, Fintha A, Komlosi P, Liu W, Satlin LM, Bell PD, Yoder BK, Schwiebert EM (2008) Loss of apical monocilia on collecting duct principal cells impairs ATP secretion across the apical cell surface and ATP-dependent and flow-induced calcium signals. Purinergic Signalling 4:155–170 [DOI] [PMC free article] [PubMed]
- 146.Webber WA, Lee J (1975) Fine structure of mammalian renal cilia. Anat Rec 182:339–343 [DOI] [PubMed]
- 147.Kishore BK, Isaac J, Fausther M, Tripp SR, Shi H, Gill PS, Braun N, Zimmermann H, Sevigny J, Robson SC (2005) Expression of NTPDase1 and NTPDase2 in murine kidney: relevance to regulation of P2 receptor signaling. Am J Physiol Renal Physiol 288:F1032–F1043 [DOI] [PubMed]
- 148.Sabolic I, Culic O, Lin S-H, Brown D (1992) Localization of ecto-ATPase in rat kidney and isolated renal cortical membrane vesicles. Am J Physiol Renal Physiol 262:F217–F228 [DOI] [PubMed]
- 149.Solini A, Iacobini C, Ricci C, Chiozzi P, Amadio L, Pricci F, Di Mario U, Di Virgilio F, Pugliese G (2005) Purinergic modulation of mesangial extracellular matrix production: role in diabetic and other glomerular diseases. Kidney Int 67:875–885 [DOI] [PubMed]
- 150.Vekaria RM, Shirley DG, Sevigny J, Unwin RJ (2006) Immunolocalization of ectonucleotidases along the rat nephron. Am J Physiol Renal Physiol 290:F550–F560 [DOI] [PubMed]
- 151.Karczewska J, Martyniec L, Dzierzko G, Stepinski J, Angielski S (2007) The relationship between constitutive ATP release and its extracellular metabolism in isolated rat kidney glomeruli. J Physiol Pharmacol 58:321–333 [PubMed]
- 152.Satriano J, Wead L, Cardus A, Deng A, Boss GR, Thomson SC, Blantz RC (2006) Regulation of ecto-5'-nucleotidase by NaCl and nitric oxide: potential roles in tubuloglomerular feedback and adaptation. Am J Physiol Renal Physiol 291:F1078–F1082 [DOI] [PubMed]
- 153.Takenaka T, Okada H, Kanno Y, Inoue T, Ryuzaki M, Nakamoto H, Kawachi H, Shimizu F, Suzuki H (2006) Exogenous 5'-nucleotidase improves glomerular autoregulation in Thy-1 nephritic rats. Am J Physiol Renal Physiol 290:F844–F853 [DOI] [PubMed]
- 154.Shirley DG, Vekaria RM, Sevigny J (2009) Ectonucleotidases and the kidney. Purinergic Signalling in press [DOI] [PMC free article] [PubMed]
- 155.Takenaka T, Inoue T, Kanno Y, Okada H, Hill CE, Suzuki H (2008) Connexins 37 and 40 transduce purinergic signals mediating renal autoregulation. Am J Physiol Reg Integr Comp Physiol 294:R1–R11 [DOI] [PubMed]
- 156.Rüster C, Wolf G (2006) Renin-angiotensin-aldosterone system and progression of renal disease. J Am Soc Nephrol 17:2985–2991 [DOI] [PubMed]
- 157.Wolf G (2006) Renal injury due to renin-angiotensin-aldosterone system activation of the transforming growth factor-[beta] pathway. Kidney Int 70:1914–1919 [DOI] [PubMed]
- 158.Anderson WP, Kett MM, Stevenson KM, Edgley AJ, Denton KM, Fitzgerald SM (2000) Renovascular hypertension: Structural changes in the renal vasculature. Hypertension 36:648–652 [DOI] [PubMed]
- 159.Fitzgerald SM, Evans RG, Bergström G, Anderson WP (1999) Renal hemodynamic responses to intrarenal infusion of ligands for the putative angiotensin IV receptor in anesthetized rats. J Cardiovasc Pharmacol 34:206–211 [DOI] [PubMed]
- 160.Imig JD, Inscho EW (2002) Adaptations of the renal microcirculation to hypertension. Microcirculation 9:315–328 [DOI] [PubMed]
- 161.Inscho EW, Carmines PK, Cook AK, Navar LG (1990) Afferent arteriolar responsiveness to altered perfusion pressure in renal hypertension. Hypertension 15:748–752 [DOI] [PubMed]
- 162.Inscho EW, Imig JD, Deichmann PC, Cook AK (1999) Candesartan-Cilexetil protects against loss of autoregulatory efficiency in angiotensin II infused rats. J Am Soc Nephrol 10:S178–S183 [PubMed]
- 163.Ploth DW (1983) Angiotensin II-dependent renal mechanisms in two-kidney, one-clip renal vascular hypertension. Am J Physiol Renal, Fluid Electrolyte Physiol 245:F131–F141 [DOI] [PubMed]
- 164.Ploth DW, Roy RN, Huang WC, Navar LG (1981) Impaired renal blood flow and cortical pressure autoregulation in the contralateral kidney of Goldblatt hypertensive rats. Hypertension 3:67–74 [DOI] [PubMed]
- 165.Racasan S, Joles JA, Boer P, Koomans HA, Braam B (2003) NO dependency of RBF and autoregulation in the spontaneously hypertensive rat. Am J Physiol Renal Physiol 285:F105–F112 [DOI] [PubMed]
- 166.Vonend O, Turner CM, Chan CM, Loesch A, Dell'Anna GC, Srai KS, Burnstock G, Unwin RJ (2004) Glomerular expression of the ATP-sensitive P2X receptor in diabetic and hypertensive rat models. Kidney Int 66:157–166 [DOI] [PubMed]
- 167.Welch WJ (2002) Adenosine type 1 receptor antagonists in fluid retaining disorders. Expert Opinion on Investigational Drugs 11:1553–1562 [DOI] [PubMed]
- 168.Graciano ML, Nishiyama A, Jackson K, Seth DM, Ortiz RM, Prieto-Carrasquero MC, Kobori H, Navar LG (2007) Purinergic receptors contribute to early mesangial cell transformation and renal vessel hypertrophy during angiotensin II-induced hypertension. Am J Physiol Renal Physiol 294:F161–F169 [DOI] [PMC free article] [PubMed]
- 169.Wang CT, Chin SY, Navar LG (2000) Impairment of pressure—natriuresis and renal autoregulation in ANG II-infused hypertensive rats. Am J Physiol Renal Physiol 279:F319–F325 [DOI] [PubMed]
- 170.Imig JD (2000) Afferent arteriolar reactivity to angiotensin II is enhanced during the early phase of angiotensin II hypertension. Am J Hypertens 13:810–818 [DOI] [PubMed]
- 171.Bidani AK, Griffin KA (2004) Pathophysiology of hypertensive renal damage: implications for therapy. Hypertension 44:595–601 [DOI] [PubMed]