Abstract
The replicative potential of human CD56+ CD3− natural killer (NK) cells is unknown. We found that by exposing NK cells to the leukemic cell line K562 genetically modified to express 4-1BB ligand and interleukin 15 (K562-mb15-41BBL), they expanded for up to 30 population doublings, achieving numbers that ranged from 1.6 × 105 to 1.2 × 1011 percent (median, 5.9 × 106 percent; n = 7) of those originally seeded. However, NK cells eventually became unresponsive to stimulation and died. Their demise could be suppressed by enforcing the expression of the human telomerase reverse transcriptase (TERT) gene. TERT-overexpressing NK cells continued to proliferate in response to K562-mb15-41BBL stimulation for more than 1 year of culture, while maintaining a normal karyotype and genotype. Long-lived NK cells had high cytotoxicity against myeloid and T-lineage leukemic cells. They remained susceptible to genetic manipulation, becoming highly cytotoxic to B-lineage leukemic cells after expression of anti-CD19 signaling receptors. Thus, human NK cells have a replicative potential similar to that of T lymphocytes and their lifespan can be significantly prolonged by an increase in TERT activity. We suggest that the methods described here should have many applications in studies of NK cell biology and NK cell-based therapies.
Keywords: natural killer cells, senescence, telomerase reverse transcriptase, immunotherapy
INTRODUCTION
Natural killer (NK) cells are a subset of peripheral blood lymphocytes that can kill a variety of target cells and are emerging as a powerful tool for cell therapy of hematologic malignancies and other cancers (Kiessling et al, 1975;Moretta & Moretta, 2004;Lanier, 2005;Farag et al, 2002;Passweg et al, 2004;Miller et al, 2005;Verheyden & Demanet, 2008). In addition to their direct antitumor activity, NK cells influence immune responses by interacting with dendritic cells, macrophages, T cells and endothelial cells (Vivier et al, 2008). Thus, many have proposed NK cell strategies as a means to improve cancer immuno-therapy, transplantation of solid organs and hematopoietic stem cells, and the control of inflammatory and autoimmune disorders (Terme et al, 2008).
Unlike T and B lymphocytes which readily respond to a variety of proliferative stimuli, NK cells are well known to be refractory to undergo sustained proliferation in vitro. Several cytokines (such as IL-2, IL-12 and IL-15) have been reported to stimulate NK cells (Trinchieri et al, 1984;Naume et al, 1992;Carson et al, 1997;Robertson et al, 1996;Perussia et al, 1987;Miller et al, 1992;Guven et al, 2003), as does contact with HLA class I-negative cells such as the K562 leukemia cell line or the HFWT Wilms' tumor cell line (Phillips & Lanier, 1985;Robertson et al, 1996;Harada et al, 2002). However, the capacity of these methods to induce long-term proliferation of CD56+ CD3− cells is generally modest and/or of short duration. Therefore, it is unclear how many cycles of cell division human NK cells can undergo while maintaining their function, and what factors limit their proliferation.
We devised a method that allows specific activation and expansion of human NK cells from peripheral blood cells (Imai et al, 2005). This method relies on co-culture with the K562 leukemia cell line transfected with two NK stimulatory molecules, membrane-bound interleukin 15 and 4-1BB ligand, termed K562-mb15-41BBL cells. In this study, we used this method to stimulate the long-term expansion of human NK cells. We determined their replicative potential, as well as genetic integrity and function after sustained proliferation.
MATERIALS AND METHODS
Cells
The myeloid cell lines K-562, KG-1 and U-937; the T-lineage ALL cell line Jurkat and the B-lineage ALL cell lines RS4;11 and 380 were available in our laboratory. Cells were maintained in RPMI-1640 (Gibco, Grand Island, NY) supplemented with 10% fetal bovine serum (FBS; BioWhittaker, Walkersville, MD) and antibiotics.
Peripheral blood was obtained from healthy adult donors (de-identified discarded material). Mononuclear cells collected from the samples by centrifugation on a Lymphoprep density step (Nycomed, Oslo, Norway) were washed twice in RPMI medium.
NK cells stimulation
To stimulate the expansion of NK cells, we cocultured peripheral blood mononuclear cells or NK cells with the K562-mb15-41BBL cell line (K562 cells transduced with constructs encoding the “membrane-bound” form of IL-15 and with 4-1BB ligand), previously described (Imai et al, 2005). Peripheral blood mononuclear cells (1.5 × 106) or NK cells (0.1 × 106) were incubated in a 24-well tissue culture plate with 106 K562-mb15-41BBL (irradiated with 100 Gray) cells in the presence of 10 IU/mL human IL-2 (National Cancer Institute BRB Preclinical Repository, Rockville, MD) in RPMI-1640 and 10% FBS. After 7 days of culture, residual T cells were removed using anti-CD3 Dynabeads (Invitrogen, Carlsbad, CA) and the concentration of IL-2 was increased to 100 IU/mL. Population doubling was defined as the log of the ratio of the final count to the baseline count divided by the log of 2.
Immortalization, immunophenotyping and genetic manipulation of NK cells
NK cells expanded for 7 days were infected with an RD114-pseudotyped retroviral vector that contained genes encoding human telomerase reverse transcriptase (TERT) and GFP, separated by an internal ribosome entry site (IRES) and controlled by MSCV LTR. The plasmid was generated from a pCIneo-hEST2-HA construct provided by Dr. Jeffrey Dome (Children's National Medical Center, Washington, DC). We then sorted GFP+ NK cells with a fluorescence-activated cell sorter (MoFlo, Cytomation). TERT expression was detected by reverse transcriptase-polymerase chain reaction (RT-PCR). Telomerase activity was assayed according to a PCR-based TRAP (TRAPeze kit; Millipore, Billerica, MA).
Cell marker studies were performed using antibodies to CD3 (conjugated to peridin chlorophyll protein, PerCP); CD56, CD16, CD69, NKp44 (CD336), NKp30 (CD337) NKp46 (CD335), NKG2D, CD94, CD226, 2B4 (CD244), KIR2DL2/2DL3 (CD158b), KIR2DL3 (NKAT2), KIR3DL1 (CD158e), KIR2DS4 (CD158i), granzyme B and perforin (conjugated to phycoerythrin, PE); CD16 (conjugated to PE-cyanin 7); and KIR2DL1(CD158ah) conjugated to allophycocyanin. Antibodies were from Becton Dickinson (San Jose, CA), Beckman Coulter (Miami, FL), Miltenyi (Auburn, CA) and Invitrogen (Carlsbad, CA).
TERT-expressing NK cells were transduced with a construct encoding the anti-CD19-BB-ζ chimeric receptor as previously described (Imai et al, 2005). Expression of the receptor was detected with a goat anti-mouse (Fab)2 polyclonal antibody conjugated with biotin (Jackson ImmunoResearch Labs, West Grove, PA) followed by streptavidin conjugated to PerCP (Becton Dickinson) (Imai et al, 2004;Imai et al, 2005).
Colony formation of TERT-expressing NK cells was tested with a standard two-layer soft agar colony-forming assay (9 replicates) (de Larco & Todaro, 1978). Colonies were counted weekly for up to 3 weeks. The T-cell leukemia cell line Jurkat was cultured in parallel as a positive control. The growth of TERT-expressing NK cells in immunodeficient mice was determined in 8-14-week-old NOD.Cg-Prkdcscid IL2rgtm1Wjl/SzJ (NOD/scid IL2RGnull) mice (Jackson Laboratory, Bar Harbor, ME). Cells (1 × 107) were injected intravenously (3 mice per clone). After 4 weeks, mice were euthanized; cell suspensions from peripheral blood, bone marrow, spleen and liver were examined for the presence of cells expressing GFP and/or CD56.
Cytotoxicity assays
Target cells (1.5 × 105) were placed in 96-well U-bottomed tissue culture plates (Costar, Cambridge, MA) and incubated with TERT-expressing NK cells at various effector : target (E : T) ratios in RPMI-1640 supplemented with 10% FBS. The NK cells were cultured with 1000 U/mL IL-2 for 48 hours before the assay. After 4 hours, cells were harvested and assayed by flow cytometry as previously described (Imai et al, 2004;Imai et al, 2005).
Spectral karyotyping and single nucleotide polymorphism array analysis
Spectral karyotyping (SKY) was performed with the Applied Spectral Imaging (ASI, Vista, CA) SkyPaint kit for human chromosomes. Images were acquired with a fluorescence microscope equipped with an interferometer (Spectra Cube, ASI) and a custom-designed filter cube (Chroma Technologies, Rockingham, VT), and analyzed with SKY View version 2.1 software (ASI).
For single nucleotide polymorphism (SNP) array analysis, we hybridized DNA from NK cells to Affymetrix SNP 6.0 arrays (Affymetrix, Santa Clara, CA) according to the manufacturer's instructions. SNP genotyping was performed with the Birdseed v2 algorithm in the Affymetrix Genotyping Console v 2.1. SNP 6.0 CEL. CHP files were preprocessed with dChip (www.dchip.org), and signal intensities for both the SNP and copy number variation (CNV) probes were summarized with the PM-only model-based expression algorithm. Raw signal intensities were normalized with the reference normalization algorithm that accounts for chromosomal aneuploidy (Mullighan et al, 2007). Copy number changes were detected by circular binary segmentation (Olshen et al, 2004) using copy number thresholds of >2.3 and <1.7, and at least 5 consecutive markers. Putative somatic CNVs in the early-passage NK cells were compared with the SNP 6.0 copy number profiles of pooled cell samples from patients with leukemia in complete remission, and with a database of copy number variants (http://projects.tcag.ca/variation/). Copy number profiles of late-passage samples were compared directly with their corresponding early-passage sample to detect CNVs that might have developed during culture.
RESULTS
Replicative potential of human NK cells and immortalization by TERT overexpression
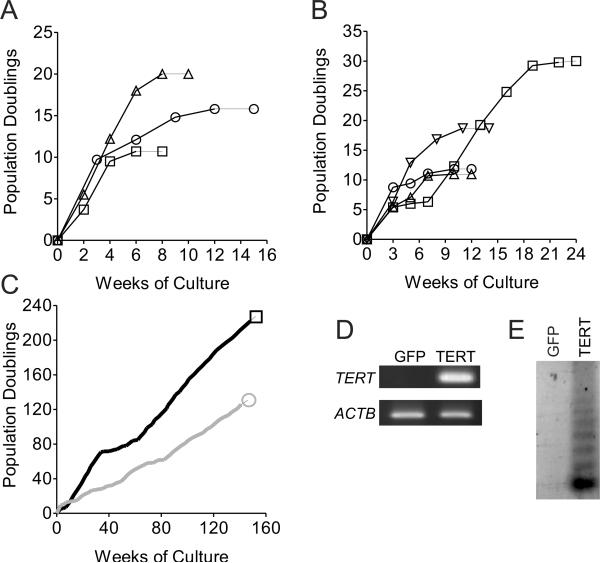
We stimulated peripheral blood mononuclear cells from 3 healthy donors by adding irradiated K562-mb15-41BBL cells to the cultures (1 to 1.5 peripheral blood mononuclear cells). Cultures were then replenished with irradiated K562-mb15-41BBL cells (10 to 1 CD56+ CD3−) every 2 weeks. Using this method, NK cells continually expanded reaching numbers that were up to 108 percent of the number of CD56+ CD3− cells originally seeded. The expanded NK cells maintained the heterogeneous expression of KIR molecules seen in primary cells (not shown), indicating that no particular subset was preferentially expanded. However, NK cells in these cultures eventually became unresponsive to stimulation and progressively died at 11, 16, and 20 population doublings and 8, 10 and 15 weeks of culture (Fig. 1A) after expanding to 1.6 × 105, 5.9 × 106 and 1.0 × 108 percent of the input cells. Thus, human NK cells have a high but not unlimited replicative capacity.
Figure 1. Replicative potential of human NK cells and their immortalization.
(A) NK cells for 3 healthy donors were stimulated with K562-mb15-41BBL cells every 2–3 weeks. Eventually, proliferation ceased and cells died. (B) Cells from 4 healthy donors were stimulated for 1 week with K562-mb15-41BBL cells and then transduced with a retrovirus containing GFP only. GFP-positive cells were stimulated the addition of irradiated K562-mb15-41BBL cells every 2–3 weeks. Proliferation eventually ceased and cells died. (C) Cells from 2 donors transduced as in B but with a vector containing the TERT gene continued to expand more than 150 weeks. (D) TERT mRNA expression by RT-PCR and (E) telomerase activity by TRAP assay in TERT-transduced NK cells.
If the demise of NK cells after prolonged stimulation was caused by erosion of telomere ends and replicative senescence, we reasoned that it should be possible to overcome this restriction by enforcing the expression of TERT. Thus, we stimulated NK cells for 1 week using the K562-mb15-41BBL cells and then transfected them with an MSCV-retroviral vector containing both human TERT and GFP genes or GFP alone. TERT transduction efficiency in the 4 donor, as measured by the percentage of cells expressing GFP, was 51%, 58%, 60% and 65%. GFP-positive cells were sorted and then stimulated with periodic pulses of K562-mb15-41BBL cells every 2–3 weeks. The GFP vector-transduced cells from all 4 donors tested underwent senescence after 11 to 30 (median, 16) population doublings, and 84 to 168 (median, 91) days of continuous culture (Fig. 1B) after expanding to a median of 2.2 × 107 (range, 2.0 × 105 to 1.2 × 1011) percent of input cells. By contrast, TERT/GFP-transduced cells from 2 donors continued to expand (Fig. 1C). TERT expression and telomerase activity was demonstrated by RT-PCR analysis and telomeric repeat amplification protocol (TRAP) (Fig. 1D and 1E). Despite transduction with the TERT gene, cells from 2 of the 4 donors entered senescence during culture, although at later times than their TERT-negative counterparts: day 112 and 154 versus 84 and 98 (not shown). Periodic addition of K562-mb15-41BBL cells to the cultures remained a requirement to sustain TERT-NK cell growth. These results indicate that replicative senescence is the chief factor limiting the expansion of human NK cells.
Functional features of immortalized NK cells
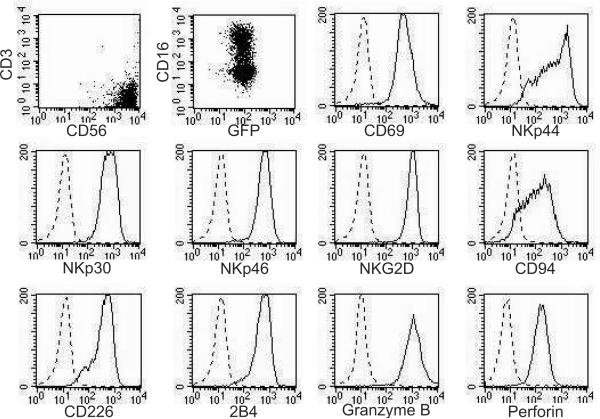
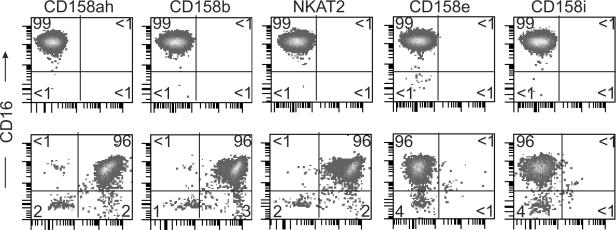
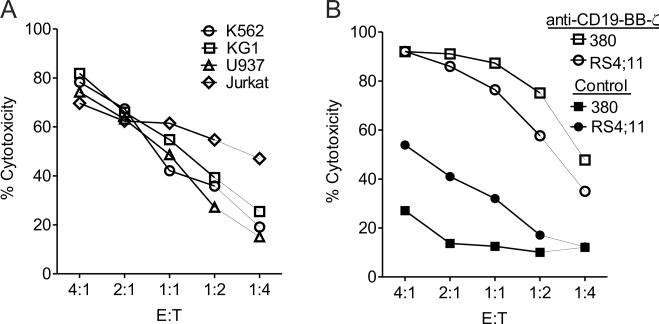
TERT-NK cells maintained an immunophenotype characteristic of activated NK cells. Besides high expression of CD56, lack of CD3 and heterogeneous expression of CD16, these cells expressed the activation marker CD69, the natural cytotoxicity receptors NKp44 (CD336), NKp30 (CD337) and NKp46 (CD335), the C-type lectin-activating receptor NKG2D, the C-type lectin inhibitory receptor CD94, and the NK-associated molecules CD226 and 2B4 (CD244), as well as granzyme B and perforin (Fig. 2). Although NK cells stimulated with K562-mb15-41BBL cells maintained an heterogeneous KIR expression profile even after 45 days of culture, when we examined the KIR profile of TERT-NK cells after prolonged cultures (day 141 and 172) we observed a predominantly homogeneous KIR expression profile (Fig. 3). This was clearly distinct in the cells of the 2 donors, indicating that NK cells with different KIR expression are equally susceptible to TERT-driven life extension. TERT-NK cells remained functionally intact, maintaining their cytotoxicity against the NK-sensitive leukemic cell lines K562, KG1, U937 and Jurkat (Fig. 4A). TERT-NK cells from the 2 donors continued to require stimulation with K562-mb15-41BBL cells to grow, and did not form colonies in soft agar (in the same assays, the median colony formation of Jurkat cells was 563/100 mm2 [range, 463–613/100 mm2]). Moreover, after injection in NOD/scid IL2RGnull mice, no TERT-NK cells could be detected in blood, marrow, spleen and liver by flow cytometry using GFP and/or CD56 as a marker (sensitivity, 1 in 10,000 mononuclear cells). Therefore, TERT-NK cells did not acquire the capacity to grow autonomously.
Figure 2. Immunophenotypic features of TERT-immortalized NK cells.
Immortalized NK cells by TERT transduction were analyzed by flow cytometry after 189 days of culture. Broken line histograms represent isotype-matched antibody staining; solid line histograms represent staining with specific PE-conjugated antibodies.
Figure 3. KIR profile of TERT-immortalized NK cells.
Immortalized NK cells from 2 donors were analyzed by flow cytometry after 179 days (top row) and 141 days of culture (bottom row). Biexponential density plots show expression of CD16 and of various KIR molecules. Percentage of cells in each quadrant is indicated.
Figure 4. TERT-immortalized NK cells retain their cytotoxicity against NK-sensitive leukemia cell line cells and susceptibility to genetic manipulation.
(A) TERT-immortalized NK cells expanded for 24–37 weeks were incubated for 4 hours with myeloid (K562, KG1 and U937) and T lymphoid (Jurkat) leukemia cell lines at the indicated E:T ratios. Each data point represents the mean percentage of duplicate measurements of leukemia cell killing after culture as compared to that of parallel cultures without NK cells. Each assay was done at least twice; representative data is shown. (B) TERT-immortalized NK cells expanded for 45 weeks were transduced anti-CD19-BB-ζ or control vector and incubated with the B-lineage ALL cell lines 380 and RS4;11 as in A. Expression of anti-CD19-BB-ζ expressing cells markedly enhanced cytotoxicity, as previously observed for freshly stimulated primary NK cells.(Imai et al, 2005)
To determine whether the cells remained susceptible to genetic manipulation, we transduced TERT-NK cells (cultured for 315 and 399 days) with a previously described retroviral vector expressing a chimeric receptor that recognizes CD19 and delivers two stimulatory signals through CD3ζ and 4-1BB (anti-CD19-BB-ζ) (Imai et al, 2004;Imai et al, 2005). The efficiency of anti-CD19 receptor expression in immortalized NK cells (45% and 72%) was well within the 43% to 93% range (median, 69%) that we previously reported for freshly expanded NK cells (Imai et al, 2005). TERT-NK cells expressing anti-CD19-BB-ζ receptors exerted potent cytotoxicity against NK-resistant CD19+ B-lineage leukemic cells (Fig. 4B). Collectively, these results indicate the TERT-NK cells essentially maintain the functional properties of newly activated NK cells.
Late passage TERT-NK cells undergo genetic alterations
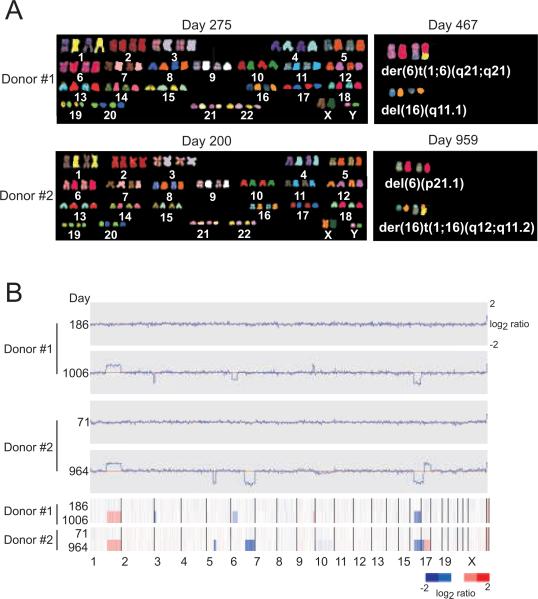
TERT-NK cells maintained a normal karyotype as demonstrated by SKY analysis on days 200 and 275 (Fig. 5A). They had only a few gene copy number changes apparent on SNP array analysis on days 71 and 186 (Fig. 5B); the majority were focal (<100 kb in size) and were located in regions of previously described inherited copy number variations (http://projects.tcag.ca/variation/).
Figure 5. Karyotypic and genetic features of TERT-transduced NK cells.
(A) SKY was done for TERT-transduced NK cells from 2 donors. Each panel shows the spectral (RGB) color image (left) and the classified (pseudocolor) chromosome after per-pixel classification of the spectral data (right). Cells maintained a normal karyotype on days 275 and 200, whereas cells collected from late passages had gross genetic changes. Thus, der(6)t(1;6)(q21;q21) and del(16)(q11.1) were found in 15/15 metaphase cells of donor 1 (5 of them had random changes); del(6)(p21.1) and der(16)t(1;16)(q12;q11.2) were found in 15/15 metaphase cells of donor 2. (B) SNP array analysis performed on genomic DNA of early (day 71 and 186) passage TERT-transduced NK cells (day 186 for donor 1 and day 71 for donor 2) did not detect any genomic alteration. Late-passage cells (day 1006 for donor 1 and day 964 for donor 2), had substantial changes (listed in Table 1).
Although TERT-NK cells continued to expand for more than 1000 days of K562-mb15-41BBL-stimulated culture (130 and 227 population doublings), we noticed a decrease in the intensity of CD56 and CD16 expression beginning on days 395 and 471 of culture (population doublings, 47 and 94, respectively), while NK-associated markers such as NKp30, NKp44, NKp46 and NKG2D were maintained. These phenotypic alterations corresponded to genetic changes as demonstrated by SKY on days 467 and 959 (Fig. 5A). SNP array copy number analysis (on days 964 and 1006) also revealed gross genetic abnormalities (Fig. 5B) including common gains in genes on chromosome 1 and losses on chromosome 16 plus other alterations summarized in Table 1. Thus, enforced expression of TERT appreciably extends K562-mb15-41BBL-driven NK cell expansion but ultimately this effect is superseded by the accumulation of genetic changes.
Table 1.
Genomic abnormalities detected in late-passage NK cells by SNP array
| Locus | Copy number | Segment size | First genes in segment |
|---|---|---|---|
| Donor #1 | |||
| chr1:142693888-247190999 | 3.28 | 104374.557 | /PPIAL4/NBPF20/PDE4DIP/SEC22B/NOTCH2NL/HFE2/TXNIP/POLR3GL/ANKRD34/LIX1L/RBM8A/PEX11B/ITGA10/ANKRD35 |
| chr3:35333-8194195 | 0.96 | 8153.311 | /CHL1/CNTN6/CNTN4/IL5RA/TRNT1/CRBN/LRRN1/SETMAR/SUMF1/ITPR1/BHLHB2/ARL8B/EDEM1/GRM7 |
| chr6:6377363-40914908 | 1.29 | 34519.036 | /LY86/RREB1/SSR1/CAGE1/RIOK1/DSP/C6orf151/BMP6/TXNDC5/MUTED |
| chr7:86651910-86685111 | 0.85 | 33.201 | /DMTF1/C7orf23 |
| chr9:127616284-139572457 | 3.21 | 11956.173 | /PBX3/C9orf28/LMX1B/ZNF297B/RALGPS1/ANGPTL2/GARNL3/SLC2A8/ZNF79/RPL12 |
| chr9:139578217-139653235 | 5.29 | 75.018 | /C9orf112/ZMYND19/ARRDC1/C9orf37 |
| chr9:139653450-140211203 | 3.23 | 557.753 | /EHMT1/FLJ40292/CACNA1B |
| chr10: 15970976-15971048 | 4.43 | 0.072 | |
| chr12:111424307-111424462 | 4.13 | 0.155 | /PTPN11 |
| chr14:41309290-41351861 | 3.13 | 42.571 | /LRFN5 |
| chr14:47452995-47477520 | 3.31 | 24.525 | |
| chr16:45021271-69399598 | 0.98 | 24366.13 | /FLJ43980/SHCBP1/VPS35/ORC6L/MLCK/LOC388272/GPT2/DNAJA2/NETO2/ITFG1 |
| chr16:69760286-88690249 | 1.01 | 18916.04 | /HYDIN/FLJ11171/CALB2/ZNF23/ZNF19/CHST4/TAT/MARVELD3/PHLPPL/AP1G1 |
| Donor #2 | |||
| chr1:97730342-97980161 | 1.12 | 249.819 | /DPYD |
| chr1:142693888-247190999 | 2.81 | 104320.302 | /PPIAL4/NBPF20/PDE4DIP/SEC22B/NOTCH2NL/HFE2/TXNIP/POLR3GL/ANKRD34/LIX1L/RBM8A/PEX11B/ITGA10/ANKRD35/PIAS3 |
| chr5:51190359-69110735 | 0.89 | 17920.376 | /PELO/ITGA1/ITGA2/MOCS2/FST/NDUFS4/ARL15/HSPB3/SNAG1/ESM1/GZMK/GZMA/FLJ37927/LOC493869/UNG2/DHX29 |
| chr6:100934555-170761408 | 0.95 | 69744.702 | /SIM1/ASCC3/GRIK2/HACE1/LIN28B/BVES/POPDC3/PREP/PRDM1/ATG5/AIM1/RTN4IP1/QRSL1 |
| chr16:45021271-69399598 | 0.96 | 24326.995 | /FLJ43980/SHCBP1/VPS35/ORC6L/MLCK/LOC388272/GPT2/DNAJA2/NETO2/ITFG1 |
| chr16:69760286-88815024 | 0.97 | 19042.966 | /HYDIN/FLJ11171/CALB2/ZNF23/ZNF19/CHST4/TAT/MARVELD3/PHLPPL/AP1G1 |
| chr17:514-22294526 | 1 | 22259.939 | /RPH3AL/LOC400566/FAM101B/VPS53/FAM57A/GEMIN4/C17orf25/RNMTL1/NXN/TIMM22 |
| chr17:22294632-78643088 | 3.32 | 56348.456 | /WSB1/KSR1/LGALS9/NOS2A/LOC201229/NLK/FLJ40504/TMEM97/IFT20/TNFAIP1 |
| chr21:allchr | 2.5 | ||
DISCUSSION
In this study, we applied a culture system that allows the continuous expansion of human NK cells to determine their replicative potential. This culture system relies on the unique properties of a genetically modified leukemia cell line, K562-mb15-41BBL (Imai et al, 2005). Results of this study show that pulses of K562-mb15-41BBL cells can maintain continuous long-term expansion of human NK cells. We found that the replicative potential of NK cells from healthy adult donors (3 untransduced and 4 transduced with a GFP only vector), ranged from 11 to 30 population doublings and was most likely limited by telomere attrition. Indeed, TERT overexpression allowed the continuous growth and preservation of NK function well beyond the senescence-imposed turning point. Ectopic expression of TERT did not affect the growth rate, phenotype, cytotoxic capacity (spontaneous or after redirection with chimeric receptors) of the transduced NK cells, which continued to depend on contact with K562-mb15-41BBL cells for proliferation.
Early studies showed that T cells can typically expand for approximately 20 to 40 population doublings before entering senescence (Effros & Pawelec, 1997;Hooijberg et al, 2000;Luiten et al, 2003), with CD4 cells from some individuals expanding for up to 60 population doublings (Roth et al, 2005), and CD8 subclones for over 100 (Rufer et al, 2001). Thus, the overall proliferative potential of NK cells is in the lower range of findings for T lymphocytes. Although NK cells forced to express TERT could expand for at least 130 population doublings and more than 1000 days in K562-mb15-41BBL-stimulated cultures, they eventually acquired gross genetic abnormalities that were strikingly similar for both donors, suggesting common mechanisms leading to genetic instability. Likewise, Roth et al.(Roth et al, 2005) observed tetraploid cells in late-passage cultures of TERT-transduced CD4+ T lymphocytes, suggesting that genetic instability is a limiting factor in immortalization of both NK cells and T lymphocytes. In our study, TERT-NK cells examined after 4–6 months of culture expressed a predominantly homogeneous KIR profile, suggesting the preferential expansion of some cell subsets. Although we did not examine retroviral integration sites to determine clonality of the long-lived cell populations, the cells had not acquired capacity for autonomous growth as shown by their absolute requirement for K562-mb15-41BBL stimulation, and their failure to form colonies in soft agar and to grow in immunodeficient mice. Notably, the KIR profile was different in the TERT-NK cells of the two donors indicating that NK cell expansion is not limited to a particular subset of cells.
Although this study focused on peripheral blood NK cells from adult healthy donors, it is likely that the culture system we describe would be suitable for expanding NK cell populations from other sources, such as cord blood or peripheral blood from patients, or perhaps circulating NK cell subsets, such as those expressing specific activating or inhibitory receptors (Moretta & Moretta, 2004;Lanier, 2005;Yu et al, 2007). An emerging concept in NK cell biology is that different developmental sites and microenvironmental niches determine the generation of NK cell populations with distinct properties (Di Santo, 2008). Using the same method that we applied for to CD56+ CD3− cells from peripheral blood it should be possible to expand NK cell subsets obtained from different tissues by modifying the culture conditions to mimic those of environmental stimuli, thus facilitating their study.
Acknowledgments
This work was supported by grants CA113482 and CA21765 from the National Cancer Institute, and by the American Lebanese Syrian Associated Charities (ALSAC)
REFERENCES
- Carson WE, Fehniger TA, Haldar S, Eckhert K, Lindemann MJ, Lai CF, Croce CM, Baumann H, Caligiuri MA. A potential role for interleukin-15 in the regulation of human natural killer cell survival. Journal of Clinical Investigation. 1997;99:937–943. doi: 10.1172/JCI119258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Larco JE, Todaro GJ. Growth factors from murine sarcoma virus-transformed cells. Proceeding of the National Academy of Science U.S.A. 1978;75:4001–4005. doi: 10.1073/pnas.75.8.4001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Santo JP. Natural killer cells: diversity in search of a niche. Nature Immunology. 2008;9:473–475. doi: 10.1038/ni.f.201. [DOI] [PubMed] [Google Scholar]
- Effros RB, Pawelec G. Replicative senescence of T cells: does the Hayflick Limit lead to immune exhaustion? Immunology.Today. 1997;18:450–454. doi: 10.1016/s0167-5699(97)01079-7. [DOI] [PubMed] [Google Scholar]
- Farag SS, Fehniger TA, Ruggeri L, Velardi A, Caligiuri MA. Natural killer cell receptors: new biology and insights into the graft-versus-leukemia effect. Blood. 2002;100:1935–1947. doi: 10.1182/blood-2002-02-0350. [DOI] [PubMed] [Google Scholar]
- Guven H, Gilljam M, Chambers BJ, Ljunggren HG, Christensson B, Kimby E, Dilber MS. Expansion of natural killer (NK) and natural killer-like T (NKT)-cell populations derived from patients with B-chronic lymphocytic leukemia (B-CLL): a potential source for cellular immunotherapy. Leukemia. 2003;17:1973–1980. doi: 10.1038/sj.leu.2403083. [DOI] [PubMed] [Google Scholar]
- Harada H, Saijo K, Watanabe S, Tsuboi K, Nose T, Ishiwata I, Ohno T. Selective expansion of human natural killer cells from peripheral blood mononuclear cells by the cell line, HFWT. Japanese Journal of Cancer Research. 2002;93:313–319. doi: 10.1111/j.1349-7006.2002.tb02174.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooijberg E, Ruizendaal JJ, Snijders PJ, Kueter EW, Walboomers JM, Spits H. Immortalization of human CD8+ T cell clones by ectopic expression of telomerase reverse transcriptase. Journal of Immunology. 2000;165:4239–4245. doi: 10.4049/jimmunol.165.8.4239. [DOI] [PubMed] [Google Scholar]
- Imai C, Iwamoto S, Campana D. Genetic modification of primary natural killer cells overcomes inhibitory signals and induces specific killing of leukemic cells. Blood. 2005;106:376–383. doi: 10.1182/blood-2004-12-4797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai C, Mihara K, Andreansky M, Nicholson IC, Pui CH, Campana D. Chimeric receptors with 4-1BB signaling capacity provoke potent cytotoxicity against acute lymphoblastic leukemia. Leukemia. 2004;18:676–684. doi: 10.1038/sj.leu.2403302. [DOI] [PubMed] [Google Scholar]
- Kiessling R, Klein E, Wigzell H. “Natural” killer cells in the mouse. I. Cytotoxic cells with specificity for mouse Moloney leukemia cells. Specificity and distribution according to genotype. European Journal of Immunology. 1975;5:112–117. doi: 10.1002/eji.1830050208. [DOI] [PubMed] [Google Scholar]
- Lanier LL. NK cell recognition. Annual Review of Immunology. 2005;23:225–74. 225–274. doi: 10.1146/annurev.immunol.23.021704.115526. [DOI] [PubMed] [Google Scholar]
- Luiten RM, Pene J, Yssel H, Spits H. Ectopic hTERT expression extends the life span of human CD4+ helper and regulatory T-cell clones and confers resistance to oxidative stress-induced apoptosis. Blood. 2003;101:4512–4519. doi: 10.1182/blood-2002-07-2018. [DOI] [PubMed] [Google Scholar]
- Miller JS, Oelkers S, Verfaillie C, McGlave P. Role of monocytes in the expansion of human activated natural killer cells. Blood. 1992;80:2221–2229. [PubMed] [Google Scholar]
- Miller JS, Soignier Y, Panoskaltsis-Mortari A, McNearney SA, Yun GH, Fautsch SK, McKenna D, Le C, Defor TE, Burns LJ, Orchard PJ, Blazar BR, Wagner JE, Slungaard A, Weisdorf DJ, Okazaki IJ, McGlave PB. Successful adoptive transfer and in vivo expansion of human haploidentical NK cells in cancer patients. Blood. 2005;105:3051–3057. doi: 10.1182/blood-2004-07-2974. [DOI] [PubMed] [Google Scholar]
- Moretta L, Moretta A. Unravelling natural killer cell function: triggering and inhibitory human NK receptors. EMBO Journal. 2004;23:255–259. doi: 10.1038/sj.emboj.7600019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullighan CG, Goorha S, Radtke I, Miller CB, Coustan-Smith E, Dalton JD, Girtman K, Mathew S, Ma J, Pounds SB, Su X, Pui CH, Relling MV, Evans WE, Shurtleff SA, Downing JR. Genome-wide analysis of genetic alterations in acute lymphoblastic leukaemia. Nature. 2007;446:758–764. doi: 10.1038/nature05690. [DOI] [PubMed] [Google Scholar]
- Naume B, Gately M, Espevik T. A comparative study of IL-12 (cytotoxic lymphocyte maturation factor)-, IL-2-, and IL-7-induced effects on immunomagnetically purified CD56+ NK cells. Journal of Immunology. 1992;148:2429–2436. [PubMed] [Google Scholar]
- Olshen AB, Venkatraman ES, Lucito R, Wigler M. Circular binary segmentation for the analysis of array-based DNA copy number data. Biostatistics. 2004;5:557–572. doi: 10.1093/biostatistics/kxh008. [DOI] [PubMed] [Google Scholar]
- Passweg JR, Tichelli A, Meyer-Monard S, Heim D, Stern M, Kuhne T, Favre G, Gratwohl A. Purified donor NK-lymphocyte infusion to consolidate engraftment after haploidentical stem cell transplantation. Leukemia. 2004;18:1835–1838. doi: 10.1038/sj.leu.2403524. [DOI] [PubMed] [Google Scholar]
- Perussia B, Ramoni C, Anegon I, Cuturi MC, Faust J, Trinchieri G. Preferential proliferation of natural killer cells among peripheral blood mononuclear cells cocultured with B lymphoblastoid cell lines. Natural Immunity and Cell Growth Regulation. 1987;6:171–188. [PubMed] [Google Scholar]
- Phillips JH, Lanier LL. A model for the differentiation of human natural killer cells. Studies on the in vitro activation of Leu-11+ granular lymphocytes with a natural killer-sensitive tumor cell, K562. Journal of Experimental Medicine. 1985;161:1464–1482. doi: 10.1084/jem.161.6.1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson MJ, Cameron C, Lazo S, Cochran KJ, Voss SD, Ritz J. Costimulation of human natural killer cell proliferation: role of accessory cytokines and cell contact-dependent signals. Natural Immunity. 1996;15:213–226. [PubMed] [Google Scholar]
- Roth A, Baerlocher GM, Schertzer M, Chavez E, Duhrsen U, Lansdorp PM. Telomere loss, senescence, and genetic instability in CD4+ T lymphocytes overexpressing hTERT. Blood. 2005;106:43–50. doi: 10.1182/blood-2004-10-4144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rufer N, Migliaccio M, Antonchuk J, Humphries RK, Roosnek E, Lansdorp PM. Transfer of the human telomerase reverse transcriptase (TERT) gene into T lymphocytes results in extension of replicative potential. Blood. 2001;98:597–603. doi: 10.1182/blood.v98.3.597. [DOI] [PubMed] [Google Scholar]
- Terme M, Ullrich E, Delahaye NF, Chaput N, Zitvogel L. Natural killer cell-directed therapies: moving from unexpected results to successful strategies. Nature Immunology. 2008;9:486–494. doi: 10.1038/ni1580. [DOI] [PubMed] [Google Scholar]
- Trinchieri G, Matsumoto-Kobayashi M, Clark SC, Seehra J, London L, Perussia B. Response of resting human peripheral blood natural killer cells to interleukin 2. Journal of Experimental Medicine. 1984;160:1147–1169. doi: 10.1084/jem.160.4.1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verheyden S, Demanet C. NK cell receptors and their ligands in leukemia. Leukemia. 2008;22:249–257. doi: 10.1038/sj.leu.2405040. [DOI] [PubMed] [Google Scholar]
- Vivier E, Tomasello E, Baratin M, Walzer T, Ugolini S. Functions of natural killer cells. Nature Immunology. 2008;9:503–510. doi: 10.1038/ni1582. [DOI] [PubMed] [Google Scholar]
- Yu J, Heller G, Chewning J, Kim S, Yokoyama WM, Hsu KC. Hierarchy of the human natural killer cell response is determined by class and quantity of inhibitory receptors for self-HLA-B and HLA-C ligands. Journal of Immunology. 2007;179:5977–5989. doi: 10.4049/jimmunol.179.9.5977. [DOI] [PubMed] [Google Scholar]