Abstract
Low socioeconomic status (SES) is associated with poor health outcomes in patients who have coronary heart disease (CHD). Inflammation is a potential mechanism by which low SES may lead to adverse cardiovascular outcomes, but it is not known whether low SES is associated with inflammation in patients who have CHD. We measured high-sensitivity C-reactive protein (CRP) levels in a cross-sectional study of 985 adults who had CHD. Income and education were determined by self-report. We used ordinal logistic regression to examine the association of income and education with CRP. Of the 985 participants, 390 had high CRP levels (>3 mg/dl). The proportion of participants who had high CRP levels ranged from 30% (103 of 340) in those who had a college degree to 51% (65 of 127) in those who had less than a high school degree (p <0.0001). The proportion of subjects who had a high CRP level ranged from 28% (52 of 183) in those who had annual income >$50,000 to 42% (199 of 974) in those who had an annual income <$20,000 (p <0.001). After adjustment for traditional cardiovascular risk factors and other potential confounding variables, lower income and education remained associated with higher CRP levels. In conclusion, low SES is associated with high CRP levels in patients who have CHD. This observation raises the possibility that inflammation may contribute to the adverse cardiovascular outcomes associated with low SES.
To determine the relation between socioeconomic status (SES) and level of C-reactive protein (CRP), we assessed income and education and measured CRP in a cross-sectional study of 985 adults who had coronary heart disease (CHD). We hypothesized that lower income and education would be associated with higher CRP levels after adjusting for demographic characteristics, traditional CHD risk factors, medical co-morbidities, medication use, and other clinical indicators.
Methods
Participants
The Heart and Soul Study is a prospective cohort study that examines the influence of psychosocial factors on health outcomes in patients who have coronary artery disease. Methods have been described previously.1,2 Patients who had coronary artery disease were recruited by using administrative databases from 2 Departments of Veterans Affairs Medical Centers (Veterans Affairs Medical Center, San Francisco, and the Veterans Affairs Palo Alto Health Care System, Palo Alto, California), 1 university-based medical center (University of California, San Francisco), and 9 public health clinics in the Community Health Network of San Francisco. Eligibility requirements included a history of any of the following: myocardial infarction, angiographic evidence of ≥50% stenosis in ≥1 coronary vessel, coronary revascularization, a diagnosis of coronary disease that was documented by an internist or cardiologist, or evidence of exercise-induced ischemia by treadmill or nuclear testing.
A total of 15,438 eligible patients was mailed an invitation to participate, and 2,495 responded that they would be interested. Of the 2,495 patients whom we attempted to contact by telephone to schedule a study appointment, 505 could not be reached and 596 declined to participate. An additional 370 patients were excluded because they had a history of myocardial infarction in the previous 6 months, deemed themselves unable to walk 1 block, or were planning to move out of the local area within 3 years.
Between September 2000 and December 2002, 1,024 participants enrolled and attended a day-long appointment at the Veterans Affairs Medical Center in San Francisco. For this cross-sectional study, we excluded 39 subjects from whom we could not obtain serum samples, leaving 985 participants for analysis. This study protocol was approved by the appropriate institutional review boards, and all participants provided written, informed consent.
Predictor variable: SES
We evaluated SES by measuring education and income. To assess education, we asked participants, “What is the highest level of education that you have completed?” Multiple-choice responses were grade ≤8, grades 9 to 11, high school graduate or equivalent, some college or vocational school, college degree, or graduate or professional degree. For analysis purposes, we categorized participants as having less than a high school education, a high school diploma, or a college or graduate degree.
To determine income, we asked participants, “Which of the following categories best describes your total combined household income for the previous 12 months?” (<$10,000, $10,000 to $19,000, $20,000 to $29,000, $30,000 to $39,999, $40,000 to $50,000, or >$50,000). For analysis purposes, we categorized participants into 1 of 4 income groups (<$20,000, $20,000 to $29,999, $30,000 to $50,000, or ≥$50,000).3
Outcome variable: CRP
Participants were instructed to fast for 12 hours (except for medication, which they were to take with water), not to take aspirin for 1 week, and not to smoke for 5 hours. Fasting venous blood samples were obtained, and serum was frozen at –70°C until the time of the CRP assay. We used the Roche Integra high-sensitivity assay (Roche, Indianapolis, Indiana) to measure CRP in 229 participants and (due to a change in the laboratory) the Beckman Extended Range high-sensitivity CRP assay (Beckman, Galway, Ireland) to measure CRP in the remaining 756 participants. We categorized participants by CRP levels <1,1 to 3, and >3 mg/L, which corresponded to low, moderate, and high levels of cardiovascular risk, respectively.4
The Roche Integra high-sensitivity CRP assay is an immunoturbidimetric assay that uses latex particles that are coated with monoclonal anti-CRP antibody. When the CRP of the sample agglutinates with these particles, a precipitate is formed and the amount is determined turbidimetrically at 522 nm. This assay has been standardized against the World Health Organization reference and compared with the Dade nephelometric method, with a correlation coefficient of 0.997. The interassay coefficient of variation is 3.2%, and the lowest detectable measurement of this assay is 0.025 mg/dl.
The Beckman Extended Range CRP assay is also an immunoturbidimetric assay that uses latex particles and a near-infrared particle immunoassay that is measured with a laser diode at 940 nm, with a detection limit of 0.20 mg/L and a measuring range of 0.20 to 1440 mg/L. This assay is highly correlated with the Roche Integra assay (r = 0.99 in a sample of 185 patients). The interassay (between-run) coefficient of variation is ≤6.7%, and the intraassay (with-in-run) coefficient of variation is <6.2%.
Other measurements
Age, gender, ethnicity, smoking, marital status, alcohol use, medical history, angina frequency, and physical activity were determined by a self-report questionnaire. We used the Computerized Diagnostic Interview Schedule, Fourth Edition, to determine the presence of current major depression according to criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.5,6 Alcohol use was evaluated by using alcohol consumption from the Alcohol Use Disorders Identification Test, with a score ≥4 to define regular alcohol use.7
Participants were instructed to bring all medication bottles to their study appointment, and the research team recorded all current medications. All participants completed echocardiography at rest for measurement of left ventricular ejection fraction and an exercise treadmill test with stress echocardiography. We calculated the wall motion score index at peak exercise as our measurement of ischemia.8 Body mass index was calculated as weight in kilograms divided by the square of height in meters. We measured systolic and diastolic blood pressures, fasting total cholesterol level, high-density lipoprotein, low-density lipoprotein, and triglycerides (milligrams per deciliter). Creatinine clearance (milliliter per minute) was calculated from 24-hour urine excretion.
Statistical analysis
This study examined the association of education and income with levels of C-reactive protein. Differences in characteristics of participants by level of CRP (<1,1 to 3, and >3 mg/L) were compared using analysis of variance for continuous variables and chi-square test for dichotomous variables. We used analysis of covariance to compare mean log CRP by categories of income and education. We also compared the unadjusted frequency of low, moderate, and high CRP levels by categories of education and income by using Cochran-Armitage chi-square test for trend.
To further evaluate the association between low SES and CRP, we used polytomous (ordinal) logistic regression, with category of income or education as the predictor variable and category of CRP (<1, 1 to 2, >3 mg/L) as the ordinal outcome variable. To obtain adjusted risk estimates, we entered all variables listed in Table 1 into a backward elimination logistic regression models that included different levels of education and income as indicator variables. Variables that were associated with high CRP levels (at p <0.05) were retained in the models. We verified the proportional odds assumption for all models. Results are reported as odds ratios with 95% confidence intervals. Analyses were performed with SAS 8 (SAS Institute, Cary, North Carolina).
Table 1.
Characteristics of 985 participants by level of C-reactive protein (CRP)
| Variable | CRP |
p Value | ||
|---|---|---|---|---|
| <1 mg/L (n = 262) | 1–3 mg/L (n = 333) | >3 mg/L (n = 390) | ||
| Age (yrs) | 66 ± 11 | 68 ± 11 | 66 ± 11 | 0.02 |
| Men | 224 (86%) | 283 (85%) | 295 (76%) | 0.001 |
| White | 151 (58%) | 208 (62%) | 236 (61%) | 0.52 |
| Married | 131 (50%) | 137 (41%) | 153 (39%) | 0.02 |
| Current smoking | 38 (15%) | 50 (15%) | 107 (27%) | <0.0001 |
| Regular alcohol use | 77 (30%) | 100 (30%) | 108 (28%) | 0.78 |
| Hypertension | 176 (68%) | 234 (70%) | 284 (73%) | 0.36 |
| Diabetes mellitus | 55 (21%) | 95 (29%) | 110 (28%) | 0.07 |
| Congestive heart failure | 33 (13%) | 53 (16%) | 87 (22%) | 0.004 |
| Angina weekly or more | 94 (36%) | 114 (34%) | 146 (38%) | 0.65 |
| Previous myocardial infarction | 136 (52%) | 188 (57%) | 203 (52%) | 0.37 |
| Previous stroke | 34 (13%) | 49 (15%) | 55 (14%) | 0.85 |
| Previous coronary artery bypass grafting | 101 (39%) | 123 (37%) | 125 (32%) | 0.18 |
| Previous coronary angioplasty | 106 (41%) | 133 (40%) | 146 (38%) | 0.67 |
| Current depression | 58 (22%) | 75 (23%) | 84 (22%) | 0.94 |
| Not at all or a little physically active | 63 (24%) | 112 (34%) | 185 (48%) | <0.0001 |
| β-Blocker use | 160 (61%) | 191 (57%) | 214 (55%) | 0.29 |
| Renin-angiotensin system inhibitor use | 136 (52%) | 180 (54%) | 189 (48%) | 0.31 |
| Diuretics (loop or thiazide) use | 57 (22%) | 90 (27%) | 143 (37%) | 0.0001 |
| Statin use | 177 (68%) | 230 (69%) | 226 (58%) | 0.003 |
| Aspirin use | 216 (82%) | 257 (77%) | 288 (74%) | 0.03 |
| Hormone replacement therapy use | 7 (3%) | 9 (3%) | 30 (8%) | 0.001 |
| Ejection fraction (%) | 0.62 ± 0.09 | 0.62 ± 0.10 | 0.61 ± 0.10 | 0.33 |
| Wall motion score index | 1.14 ± .31 | 1.17 ± .34 | 1.19 ± .39 | 0.22 |
| Systolic blood pressure (mm Hg) | 129 ± 20 | 132 ± 20 | 136 ± 22 | <0.0001 |
| Diastolic blood pressure (mm Hg) | 73 ± 12 | 75 ± 11 | 76 ± 11 | 0.005 |
| Total cholesterol (mg/dl) | 171 ± 37 | 177 ± 43 | 183 ± 46 | 0.001 |
| High-density lipoprotein (mg/dl) | 47.8 ± 15 | 46 ± 14 | 44 ± 13 | 0.004 |
| Low-density lipoprotein (mg/dl) | 96.5 ± 26 | 104 ± 33 | 110 ± 38 | <0.0001 |
| Creatinine clearance (ml/min) | 86 ± 28 | 81 ± 28 | 78 ± 29 | 0.001 |
| Body mass index (kg/m2) | 27 ± 4.1 | 28 ± 5 | 30 ± 6 | <0.0001 |
| Triglycerides (mg/dl) | 136 ± 157 | 137 ± 120 | 147 ± 113 | 0.47 |
Values are means ± SD or numbers of patients (percentages).
Results
Among the 985 study participants, 262 had CRP levels <1 mg/L, 333 had CRP levels 1 to 3 mg/L, and 390 had CRP levels >3 mg/L (Table 1). Compared with participants who had low CRP levels, those who had higher CRP levels were older, less likely to be men or married, and more likely to smoke, to have diabetes, to have congestive heart failure, and to be physically inactive. Participants who had higher CRP levels were also more likely to be taking diuretics, less likely to be taking statins or aspirin, and more likely to be using hormone replacement therapy. They had higher values for blood pressure, low-density lipoprotein, and body mass index and lower values for high-density lipoprotein and creatinine clearance compared with those who had low CRP levels.
Mean ± SE log CRP values were 0.48 ± 0.07 mg/dl in the 340 participants who had a college degree, 0.80 ± 0.06 mg/dl in the 516 participants who had a high school degree, and 0.98 ± 0.12 in the 127 participants who had less than a high school degree (p <0.0001). Mean ± SE log CRP values were 0.33 ± 0.10 mg/dl in the 183 participants who had an annual income >$50,000, 0.75 ± 0.09 in the 189 participants who had an annual income from $30,000 to $50,000, 0.81 ± 0.11 in the 133 participants who had an annual income from $20,000 to $29,999, and 0.82 ± 0.06 in the 474 participants who had an annual income <$20,000 (p = 0.0002).
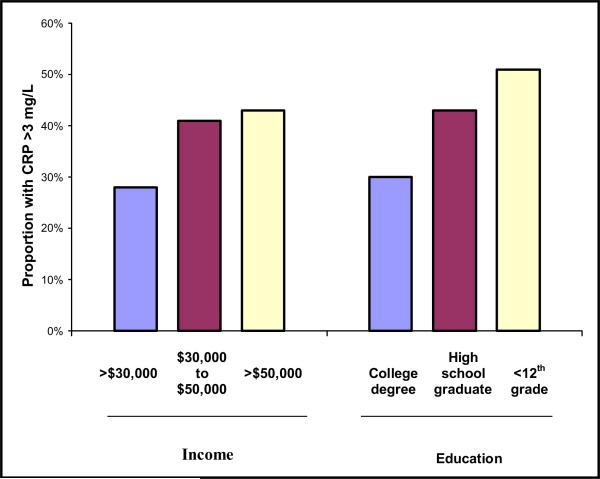
When we divided CRP into categories (<1, 1 to 3, >3 mg/dl), lower income and education levels were associated with higher CRP levels (Figure 1, Table 2). The proportion of participants who had high CRP levels (>3 mg/dl) ranged from 30% in those who had a college degree to 51% in those who had less than a high school education (p <0.0001) and from 28% in those who had an annual income ≥$50,000 to 42% in those who had an annual income <$20,000 (p <0.001). After adjustment for potential confounding variables, lower income and education levels remained associated with higher CRP levels (Table 3).
Figure 1.
Proportion of participants who had high CRP levels according to income and education level (p for trend <0.01).
Table 2.
Socioeconomic status and level of C-reactive protein (CRP) in 985 participants with coronary heart disease
| CRP |
p Value | |||
|---|---|---|---|---|
| <1 mg/L | 1–3 mg/L | >3 mg/L | ||
| Education | ||||
| Grade ≤8 | 11 | 19 | 22 | 0.0002 |
| Grades 9–11 | 12 | 20 | 43 | |
| High school graduate | 36 | 55 | 85 | |
| Some college or vocational school | 85 | 118 | 137 | |
| College degree | 63 | 57 | 54 | |
| Graduate or professional degree | 54 | 63 | 49 | |
| Annual income (United States dollars) | ||||
| <$10,000 | 58 | 87 | 100 | 0.002 |
| $10,000–$19,000 | 53 | 77 | 99 | |
| $20,000–$29,999 | 27 | 45 | 61 | |
| $30,000–$39,999 | 22 | 31 | 40 | |
| $40,000–$50,000 | 25 | 33 | 38 | |
| >$50,000 | 75 | 56 | 52 | |
Values are numbers of subjects.
Table 3.
Association between socioeconomic status and level of C-reactive protein (CRP) (<1, 1 to 3, >3 mg/L)
| Proportion With CRP >3 mg/L | Unadjusted OR (95% CI) | p Value | Adjusted OR (95% CI)* | p Value | Adjusted OR (95% CI)† | p Value | |
|---|---|---|---|---|---|---|---|
| Education | |||||||
| ≤11 yrs | 51% (65/127) | 2.4 (1.6–3.5) | <0.0001 | 2.2 (1.4–3.5) | 0.001 | 2.2 (1.3–3.6) | 0.002 |
| High school degree | 43% (222/516) | 1.7 (1.3–2.2) | <0.0001 | 1.4 (1.0–1.9) | 0.03 | 1.5 (1.1–2) | 0.02 |
| College degree or higher | 30% (103/340) | 1 | — | 1 | — | ||
| Annual income | |||||||
| <$20,000 | 42% (199/474) | 2.1 (1.5–2.8) | <0.0001 | 1.4 (.96–2.1) | 0.08 | 1.2 (0.8–1.9) | 0.34 |
| $20,000–29,999 | 46% (61/133) | 2.4 (1.6–3.7) | <0.0001 | 2.2 (1.4–3.6) | 0.001 | 2.1 (1.2–3.5) | 0.006 |
| $30,000–50,000 | 41% (78/189) | 2.0 (1.3–2.9) | 0.0005 | 1.8 (1.2–2.8) | 0.007 | 1.7 (1.1–2.7) | 0.02 |
| ≥$50,000 | 28% (52/183) | 1 | — | 1 | — | 1 | — |
All variables were entered into a backward elimination ordinal logistic regression model with a p value <0.05 for retention. Other variables associated with high CRP level (at p <0.05) in the education model were white ethnicity, smoker, history of congestive heart failure, not currently depressed, little or no physical activity, not using a β blocker, using hormone therapy, increased systolic blood pressure, high cholesterol level, low high-density lipoprotein level, low creatinine clearance and high body mass index. Other variables associated with high CRP level (at p <0.05) in the income model were white ethnicity, smokers, history of congestive heart failure, not currently depressed, little or not physically activity, not using a β blocker, using hormone therapy, increased systolic blood pressure, low cholesterol level, high low-density lipoprotein level, high triglyceride level, low creatinine clearance, and high body mass index.
Further adjusted for other socioeconomic variable (education or income).
CI = confidence interval; OR = odds ratio.
Discussion
Our cross-sectional study of outpatients who had CHD associated low SES with higher levels of CRP. Associations of lower education and income were independent of each other and persisted after adjustment for traditional cardiovascular risk factors, marital status, and depression. The observed relation between low SES and CRP raises the intriguing possibility that inflammation may contribute to the adverse cardiovascular outcomes associated with low SES.
Low SES is associated with an increased risk of CHD and with greater morbidity and mortality among patients who have CHD.9–17 However, the mechanisms by which low SES leads to adverse cardiovascular outcomes are not known. Patients who have low SES are more likely to smoke, to be obese, to have hypertension or diabetes, and to be physically inactive.18–21 However, even after adjusting for traditional CHD factors, low SES is independently associated with excess morbidity and mortality among patients who had CHD.22–24 The effect of low SES on mortality after myocardial infarction is equivalent to the effect of many traditional risk factors.25
CRP level, a measurement of inflammation, is a well-established and independent predictor of cardiovascular events.26–29 Previous studies of healthy adults have associated high CRP levels with low social class in childhood,30,31 low occupational grade,3 low educational level,32–34 and low income level.34 Our findings demonstrate that the association between low SES and CRP that was observed in healthy adults is also present in patients who have CHD. Because high levels of CRP predict CHD events,26–28 inflammation may be a mechanism by which SES leads to adverse health outcomes.
Other possible pathways by which SES may influence cardiovascular outcomes include the effects of chronic stress,3 dysregulation of the parasympathetic nervous system,35 greater insulin resistance,36 and differences in dietary, lifestyle, and behavior patterns.37 Limited education and lack of financial resources may also affect access to quality medical care38 and decrease adherence to medication.39 Whatever the mechanism, our findings suggest that patients who have a low income or education level may benefit from more aggressive management of CHD, including treatment of dyslipidemia, hypertension, diabetes, smoking, obesity, and physical inactivity.
Our study has several limitations that should be considered. Income and education were measured by self-report, thus leaving room for inaccuracies in our analysis. Further, our measurement of “overall household income” may not reflect the participants’ personal income. However, it is likely a reasonable reflection of participants’ SES. Although the 2 CRP assays were highly correlated (r = 0.99), use of 2 different assays still poses a potential limitation. Moreover, stepwise analysis uses a purely statistical method to select significant variables without necessarily considering biologic confounding. In addition, the investigation involved only a minority of female participants, so our results may not generalize to all populations.
Acknowledgments
This work was supported by grants from the Department of Veterans Affairs, Washington, DC; the American Federation for Aging Research (Paul Beeson Scholars Program), New York, New York; the Robert Wood Johnson Foundation (Faculty Scholars Program), Princeton, New Jersey; and the Nancy Kirwan Heart Research Fund, San Francisco, California.
References
- 1.Ruo B, Rumsfeld JS, Hlatky MA, Liu H, Browner WS, Whooley MA. Depressive symptoms and health-related quality of life: the Heart and Soul Study. JAMA. 2003;290:215–221. doi: 10.1001/jama.290.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beattie MS, Shlipak MG, Liu H, Browner WS, Schiller NB, Whooley MA. C-reactive protein and ischemia in users and nonusers of beta-blockers and statins: data from the Heart and Soul Study. Circulation. 2003;107:245–250. doi: 10.1161/01.cir.0000044387.23578.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Owen N, Poulton T, Hay FC, Mohamed-Ali V, Steptoe A. Socioeconomic status, CRP, immune factors, and responses to acute mental stress. Brain Behav Immun. 2003;17:286–295. doi: 10.1016/s0889-1591(03)00058-8. [DOI] [PubMed] [Google Scholar]
- 4.Ridker PM. Inflammation in atherothrombosis: how to use high-sensitivity C-reactive protein (hsCRP) in clinical practice. Am Heart Hosp J. 2004;2:4–9. [PubMed] [Google Scholar]
- 5.Blouin AG, Perez EL, Blouin JH. Computerized administration of the Diagnostic Interview Schedule. Psychiatry Res. 1988;23:335–344. doi: 10.1016/0165-1781(88)90024-8. [DOI] [PubMed] [Google Scholar]
- 6.Levitan RD, Blouin AG, Navarro JR, Hill J. Validity of the computerized DIS for diagnosing psychiatric inpatients. Can J Psychiatry. 1991;36:728–731. [PubMed] [Google Scholar]
- 7.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158:1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- 8.Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, Gutgesell H, Reichek N, Sahn D, Schnittger I, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr. 1989;2:358–367. doi: 10.1016/s0894-7317(89)80014-8. [DOI] [PubMed] [Google Scholar]
- 9.Williams RB, Barefoot JC, Califf RM, Haney TL, Saunders WB, Pryor DB, Hlatky MA, Siegler IC, Mark DB. Prognostic importance of social and economic resources among medically treated patients with angiographically documented coronary artery disease. JAMA. 1992;267:520–524. (erratum JAMA 1992;268:2652) [PubMed] [Google Scholar]
- 10.Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993;88:1973–1998. doi: 10.1161/01.cir.88.4.1973. [DOI] [PubMed] [Google Scholar]
- 11.Smith GD, Hart C, Blane D, Gillis C, Hawthorne V. Lifetime socioeconomic position and mortality: prospective observational study. BMJ. 1997;314:547–552. doi: 10.1136/bmj.314.7080.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davey Smith G, Neaton JD, Wentworth D, Stamler R, Stamler J. Mortality differences between black and white men in the USA: contribution of income and other risk factors among men screened for the MRFIT. MRFIT Research Group. Multiple Risk Factor Intervention Trial. Lancet. 1998;351:934–939. doi: 10.1016/s0140-6736(00)80010-0. [DOI] [PubMed] [Google Scholar]
- 13.Salomaa V, Niemela M, Miettinen H, Ketonen M, Immonen-Raiha P, Koskinen S, Mahonen M, Lehto S, Vuorenmaa T, Palomaki P, et al. Relationship of socioeconomic status to the incidence and prehospital, 28-day, and 1-year mortality rates of acute coronary events in the FINMONICA myocardial infarction register study. Circulation. 2000;101:1913–1918. doi: 10.1161/01.cir.101.16.1913. [DOI] [PubMed] [Google Scholar]
- 14.Alboni P, Amadei A, Scarfo S, Bettiol K, Ippolito F, Baggioni G. In industrialized nations, a low socioeconomic status represents an independent predictor of mortality in patients with acute myocardial infarction. Ital Heart J. 2003;4:551–558. [PubMed] [Google Scholar]
- 15.Horne BD, Muhlestein JB, Lappe DL, Renlund DG, Bair TL, Bunch TJ, Anderson JL. Less affluent area of residence and lesser-insured status predict an increased risk of death or myocardial infarction after angiographic diagnosis of coronary disease. Ann Epidemiol. 2004;14:143–150. doi: 10.1016/S1047-2797(03)00125-X. [DOI] [PubMed] [Google Scholar]
- 16.Galobardes B, Lynch JW, Davey Smith G. Childhood SES and cause-specific mortality in adulthood: systematic review and interpretation. Epidemiol Rev. 2004;26:7–21. doi: 10.1093/epirev/mxh008. [DOI] [PubMed] [Google Scholar]
- 17.Lawlor DA, Davey Smith G, Patel R, Ebrahim S. Life-course socioeconomic position, area deprivation, and coronary heart disease: findings from the British Women's Heart and Health Study. Am J Public Health. 2005;95:91–97. doi: 10.2105/AJPH.2003.035592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Luepker RV, Rosamond WD, Murphy R, Sprafka JM, Folsom AR, McGovern PG, Blackburn H. Socioeconomic status and coronary heart disease risk factor trends. The Minnesota Heart Survey. Circulation. 1993;88:2172–2179. doi: 10.1161/01.cir.88.5.2172. [DOI] [PubMed] [Google Scholar]
- 19.Winkleby MA, Kraemer HC, Ahn DK, Varady AN. Ethnic and socioeconomic differences in cardiovascular disease risk factors: findings for women from the Third National Health and Nutrition Examination Survey, 1988–1994. JAMA. 1998;280:356–362. doi: 10.1001/jama.280.4.356. [DOI] [PubMed] [Google Scholar]
- 20.Rutledge T, Reis SE, Olson M, Owens J, Kelsey SF, Pepine CJ, Reichek N, Rogers WJ, Bairey-Merz CN, Sopko G, et al. Socioeconomic status variables predict cardiovascular disease risk factors and prospective mortality risk among women with chest pain. The WISE Study. Behav Modif. 2003;27:54–67. doi: 10.1177/0145445502238693. [DOI] [PubMed] [Google Scholar]
- 21.Nordstrom CK, Diez Roux AV, Jackson SA, Gardin JM. The association of personal and neighborhood socioeconomic indicators with subclinical cardiovascular disease in an elderly cohort. The Cardiovascular Health Study. Soc Sci Med. 2004;59:2139–2147. doi: 10.1016/j.socscimed.2004.03.017. [DOI] [PubMed] [Google Scholar]
- 22.Lantz PM, House JS, Lepkowski JM, Williams DR, Mero RP, Chen J. Socioeconomic factors, health behaviors, and mortality: results from a nationally representative prospective study of US adults. JAMA. 1998;279:1703–1708. doi: 10.1001/jama.279.21.1703. [DOI] [PubMed] [Google Scholar]
- 23.Alter DA, Iron K, Austin PC, Naylor CD. Influence of education and income on atherogenic risk factor profiles among patients hospitalized with acute myocardial infarction. Can J Cardiol. 2004;20:1219–1228. [PubMed] [Google Scholar]
- 24.Rutledge T, Reis SE, Olson M, Owens J, Kelsey SF, Pepine CJ, Mankad S, Rogers WJ, Bairey Merz CN, Sopko G, et al. Social networks are associated with lower mortality rates among women with suspected coronary disease: the National Heart, Lung, and Blood Institute–sponsored Women's Ischemia Syndrome Evaluation study. Psychosom Med. 2004;66:882–888. doi: 10.1097/01.psy.0000145819.94041.52. [DOI] [PubMed] [Google Scholar]
- 25.Mookadam F, Arthur HM. Social support and its relationship to morbidity and mortality after acute myocardial infarction: systematic overview. Arch Intern Med. 2004;164:1514–1518. doi: 10.1001/archinte.164.14.1514. [DOI] [PubMed] [Google Scholar]
- 26.Ridker PM, Buring JE, Shih J, Matias M, Hennekens CH. Prospective study of CRP and risk of future cardiovascular events among apparently healthy women. Circulation. 1998;98:731–733. doi: 10.1161/01.cir.98.8.731. [DOI] [PubMed] [Google Scholar]
- 27.Ridker PM, Hennekens CH, Buring JE, Rifai N. CRP and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med. 2000;342:836–843. doi: 10.1056/NEJM200003233421202. [DOI] [PubMed] [Google Scholar]
- 28.Danesh J, Wheeler JG, Hirschfield GM, Eda S, Eiriksdottir G, Rumley A, Lowe GD, Pepys MB, Gudnason V. C-reactive protein and other circulating markers of inflammation in the prediction of coronary heart disease. N Engl J Med. 2004;350:1387–1397. doi: 10.1056/NEJMoa032804. [DOI] [PubMed] [Google Scholar]
- 29.Pai JK, Pischon T, Ma J, Manson JE, Hankinson SE, Joshipura K, Curhan GC, Rifai N, Cannuscio CC, Stampfer MJ, Rimm EB. Inflammatory markers and the risk of coronary heart disease in men and women. N Engl J Med. 2004;351:2599–2610. doi: 10.1056/NEJMoa040967. [DOI] [PubMed] [Google Scholar]
- 30.Mendall MA, Patel P, Ballam L, Strachan D, Northfield TC. C reactive protein and its relation to cardiovascular risk factors: a population based cross sectional study. BMJ. 1996;312:1061–1065. doi: 10.1136/bmj.312.7038.1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mendall MA, Strachan DP, Butland BK, Ballam L, Morris J, Sweet-nam PM, Elwood PC. C-reactive protein: relation to total mortality, cardiovascular mortality and cardiovascular risk factors in men. Eur Heart J. 2000;21:1584–1590. doi: 10.1053/euhj.1999.1982. [DOI] [PubMed] [Google Scholar]
- 32.Wu T, Dorn JP, Donahue RP, Sempos CT, Trevisan M. Associations of serum C-reactive protein with fasting insulin, glucose, and glycosylated hemoglobin: the Third National Health and Nutrition Examination Survey, 1988–1994. Am J Epidemiol. 2002;155:65–71. doi: 10.1093/aje/155.1.65. [DOI] [PubMed] [Google Scholar]
- 33.Panagiotakos DB, Pitsavos CE, Chrysohoou CA, Skoumas J, Toutouza M, Belegrinos D, Toutouzas PK, Stefanadis C. The association between educational status and risk factors related to cardiovascular disease in healthy individuals: the ATTICA study. Ann Epidemiol. 2004;14:188–194. doi: 10.1016/S1047-2797(03)00117-0. [DOI] [PubMed] [Google Scholar]
- 34.Jousilahti P, Salomaa V, Rasi V, Vahtera E, Palosuo T. Association of markers of systemic inflammation, C reactive protein, serum amyloid A, and fibrinogen, with socioeconomic status. J Epidemiol Community Health. 2003;57:730–733. doi: 10.1136/jech.57.9.730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sloan RP, Huang MH, Sidney S, Liu K, Williams OD, Seeman T. SES and health: is parasympathetic nervous system activity an intervening mechanism? Int J Epidemiol. 2005;34:309–315. doi: 10.1093/ije/dyh381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lawlor DA, Smith GD, Ebrahim S. Association between childhood socioeconomic status and coronary heart disease risk among post-menopausal women: findings from the British Women's Heart and Health Study. Am J Public Health. 2004;94:1386–1392. doi: 10.2105/ajph.94.8.1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pickering T. Cardiovascular pathways: socioeconomic status and stress effects on hypertension and cardiovascular function. Ann NY Acad Sci. 1999;896:262–277. doi: 10.1111/j.1749-6632.1999.tb08121.x. [DOI] [PubMed] [Google Scholar]
- 38.Ancona C, Arca M, Saitto C, Agabiti N, Fusco D, Tancioni V, Perucci CA. Differences in access to coronary care unit among patients with acute myocardial infarction in Rome: old, ill, and poor people hold the burden of inefficiency. BMC Health Serv Res. 2004;4:34. doi: 10.1186/1472-6963-4-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Goldman DP, Smith JP. Can patient self-management help explain the SES health gradient? Proc Natl Acad Sci USA. 2002;99:10929–10934. doi: 10.1073/pnas.162086599. [DOI] [PMC free article] [PubMed] [Google Scholar]