Abstract
Background
We propose evaluation of a multi-component home automated telemanagement (HAT) system providing integrated support to both clinicians and patients in implementing hypertension treatment guidelines.
Methods
In a randomized clinical study 550 African Americans with hypertension are followed for 18 months. The major components of the intervention and control groups are identical and are based on the current standard of care. For the purpose of this study, we define “standard of care” as the expected evidence-based care provided according to the current hypertension treatment guidelines. While intervention and control groups are similar in terms of their care components, they differ in the mode of care delivery. For the control group the best attempt is made to deliver all components of a guideline-concordant care in a routine clinical environment whereas for the intervention group the routine clinical environment is enhanced with Health Information Technology (IT) that assists clinicians and patients in working together in implementing treatment guidelines. The HAT system guides patients in following their individualized treatment plans and helps care coordination team in monitoring the patient progress. The study design is aimed at addressing the main question of this trial: whether the addition of the IT-enhanced care coordination in the routine primary care setting can improve delivery of evidence-based hypertension care in African Americans. The outcome parameters include quality of life, medical care utilization, treatment compliance, psychosocial variables and improvement in blood pressure control rates.
Conclusions
The trial will provide insight on the potential impact of IT-enhanced care coordination in African Americans with poorly controlled hypertension.
Keywords: hypertension, telemedicine, self-management
Background
Recent studies demonstrated that successful chronic disease management requires a coordinated effort that includes health care providers who follow current clinical guidelines in their every day practice, educated patients who are adherent to their prescribed treatment plans and comprehensive patient-provider communication (1). Previous studies have been successful in affecting the major components of hypertension care including physician practice patterns, patient adherence to therapy, and patient-provider communication (2). These studies focused mainly on an improvement of a single component of the clinical care process (2). To date there have been a limited number of studies evaluating the coordinated approach that concurrently employs all of the above mentioned components in an integrated framework linked to primary care. In this study we propose evaluating a multi-component telemanagement system that provides integrated support to both clinicians and patients in implementing hypertension treatment guidelines in accordance with the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) (3).
Several studies explored the possibilities of home telecare programs for patients with hypertension. A study of effects of home telemonitoring on blood pressure (BP) control in urban African Americans demonstrated a more pronounced improvement in BP control as compared to a community-based intervention (4). A home telemonitoring service was particularly efficacious among African American patients in a randomized clinical trial conducted to determine the efficacy of a telecommunication service in reducing BP (5). A care management program delivered through secure patient Web communications improved BP control in patients with hypertension (6). A nutrition education program delivered via the Internet was associated with significant weight loss and with the lowering of BP (7). However, none of these programs studied the impact of a multi-component telemanagement system that provides integrated support to both clinicians and patients in implementing JNC 7 guidelines to improve hypertension control rates in African Americans.
The Home Automated Telemanagement (HAT) system (8) was designed to facilitate the Chronic Care Model (9) by supporting an informed, activated patient interacting with a prepared, proactive practice team. The HAT system helps to implement patient self-care, clinical decision support and care coordination, enhanced patient-provider communication, disease education, control of patient adherence with their individualized treatment plans, healthy lifestyle counseling, and social support. In previous studies we have demonstrated: 1) a high level of acceptance of the HAT system by patients with limited education and no previous computer experience (10), 2) acceptance of the system by physician and nurses taking care of their patients (11), 3) validity of the self-testing results in adult patients who used HAT (12). The system has been successfully implemented for home telemanagement in patients with asthma (10), chronic obstructive pulmonary disease (13), inflammatory bowel disease (14), and multiple sclerosis (15).
In this study, we seek to advance our understanding of the applicability and utility of home telemanagement by focusing on its impact on African-Americans with hypertension. Routine care delivery of a guideline-concordant hypertension care including both pharmacological and non-pharmacological components is frequently hampered by multiple barriers at system, clinic, and patient levels (2). The major components of the intervention and control groups in this study are identical and are based on the current standard of care. For the purpose of this study, we define “standard of care” as the expected evidence-based care provided according to the JNC 7 guidelines (3). While intervention and control groups are similar in terms of their care components, they differ in the mode of care delivery. For the control group the best attempt is made to deliver all components of a guideline-concordant care in a routine clinical environment whereas for the intervention group the routine clinical environment is enhanced with Health Information Technology (IT) that assists clinicians and patients in working together in implementing treatment guidelines. This design is aimed to address the main question of this trial: whether the addition of the IT-enhanced care coordination in the routine primary care setting can improve delivery of evidence-based hypertension care in African Americans.
The specific goals of this study include: 1) refining the HAT program according to the JNC 7 Report and implementing the multidisciplinary model for hypertension telemanagement in African Americans as an adjunct to ambulatory care, 2) evaluating in a randomized clinical trial the impact of telemangement on hypertension care delivery and on patients' clinical outcomes using both clinic- and patient-level variables. The comparison will be made with the standard of hypertension care recommended by JNC 7 Report.
The following primary hypothesis related to clinic-level outcomes will be tested: Use of telemanagement will be associated: 1) with improved proportion of treated patients that achieve blood pressure goals meeting JNC 7 recommendations, and 2) with a significant reduction in systolic and diastolic blood pressure. We will also explore the impact of HAT on physician awareness and on the use of the hypertension treatment guidelines promulgated by the JNC 7 Report.
The following secondary exploratory hypothesis related to patient-level outcomes will be evaluated: The HAT program will have positive impact on behavioral and cognitive factors that play an important role in the process of patient self-management, including hypertension treatment self-efficacy, health locus of control, health beliefs, and knowledge of hypertension. We will also investigate the impact of HAT on patients’ compliance with multi-component treatment plans (including adherence to medication regimens and therapeutic life style changes) and explore the effect of the HAT system on a patient’s ability to reach dietary, physical activity, weight control, and sodium consumption goals recommended by the JNC 7 Report.
During this study we will explore the impact of HAT on patient satisfaction with medical care, health-related quality of life and health services utilization. We will also assess acceptance of the HAT system by both patients and providers.
Conceptual Framework Model
The Chronic Care Model (CCM), described by Wagner et al (9), provides a conceptual framework for effective patient-centered disease management. The HAT system is designed to support the major components of this model on patient and physician levels including 1) an informed, activated patient; 2) self-management support; 3) productive patient-provider interactions; 4) a prepared, proactive practice team; 5) decision support; 6) clinical information systems.
The healthy lifestyle support provided by the HAT system utilizes behavioral constructs from Social Cognitive Theory (SCT), Transtheoretical Model and Consumer Information Processing Model as its major theoretical behavioral foundation. SCT synthesizes concepts and processes from cognitive, behavioral and emotional models of behavioral change (16). SCT constructs relevant to the HAT design include behavioral capability, self-efficacy, outcome expectation and reinforcement.
Behavioral capability includes knowledge of “what to do” and “how to do it” as well as the skills needed to perform it. Behavioral capability is considered a necessary prerequisite for performing a behavior, but is insufficient to guarantee performance. Self-efficacy expectations are a person’s beliefs about one’s capability to perform a specific behavior. Self-efficacy beliefs have been found to be related to whether or not a person will attempt a task and also to how long a person will persevere in completing the task. Outcome expectations are a person’s beliefs concerning the effects of engaging in certain actions. Realistic outcome expectations can enhance self-efficacy. Reinforcement is defined as response to a person’s behavior that increases or decreases the chances of recurrences. Table 1 highlights how the constructs of SCT apply to the HAT design.
Table 1.
Application of Concepts from SCT to the HAT Design
| Concept | Application |
|---|---|
| 1. Behavioral Capability | Users/patients are given information about specific behavioral actions (healthy diet, stress avoidance, regular exercise, etc), and stepwise training and suggestions for how to incorporate desirable behavioral patterns into their daily lives |
| 2. Self-efficacy | The use of praise, feedback, and setting achievable goals are used to increase patients’ perceptions of their self-efficacy |
| 3. Outcome Expectations | HAT repeatedly informs the patients that following their HTN self-care plan will improve BP control, decrease CVD risk, and increase quality of life |
| 4. Reinforcement | User/patient receives praise and encouragement for following HTN self-care plans. The HAT nurse contacts patients in case of non-adherence to educate and reinforce patient adherence |
The HAT components utilizing SCT concepts provide support and reinforcement while making an attempt to enhance patient self-efficacy by creating mastery. This approach includes the following strategies: 1) Identifying barriers by providing the patient with a list of potentially remediable factors, 2) Helping patients set intermediate, small, and easily achievable goals, and 3) Offering vignettes for modeling appropriate behavior.
The Transtheoretical Model (TTM) provides a theoretical framework which is used in interventions aimed to help patients adopt healthy behaviors (17). The model comprises four constructs: stages of change (precontemplation, contemplation, preparation, action, maintenance and relapse), decisional balance, situational self-efficacy, and processes of change (18).
The tailored messages that are delivered to the patient by the HAT system are based on patient self-reported data. For each patient, behavioral constructs such as stage of change and self-efficacy are collected during a self-testing session and are sent to the HAT central server. A tailored message corresponding to the behavioral construct is then chosen from the message library and sent back to the patient.
The Consumer Information Processing Model (CIP) is based on two central postulates (19). First, the amount of information that can be processed by individuals is limited. Second, the usability of information can be maximized by splitting and providing it in “chunks.” These claims have been supported by previous findings (20) that short term memory is limited to seven (or 5 to 9) chunks of information. These CIP concepts have been utilized in our user interface and in the design of the interactive multimedia education module. The user interface for this study was designed to represent a limited amount of information on each screen so that patients can easily grasp all the presented information in an unambiguous way. For the interactive education module, we divided the educational curriculum into small educational tips, and organized the tips into consecutive sections.
Study Design
Overview of the Clinical Trial
To evaluate the efficacy of the HAT System as an adjunct to the current standard of medical care for African American patients with hypertension, we propose to conduct a randomized clinical trial. The study is conducted in primary care clinics located in the Baltimore/Washington DC Metropolitan Area.
All candidate clinics (N=50) have been classified (stratified) as university, Veteran Affairs, HMO/private and non-private/other sites. This classification resulted in a total of 4 categories. Our choice of the stratification factor was based on the results of the ALLHAT study that showed statistical differences in BP control rates between university or Veteran Affairs sites compared with private or HMO sites (22). Stratified randomization was performed at the clinic level with patients sequentially selected within each clinic (11 patients from each clinic). Overall 550 patients have been enrolled into this study.
Research Model
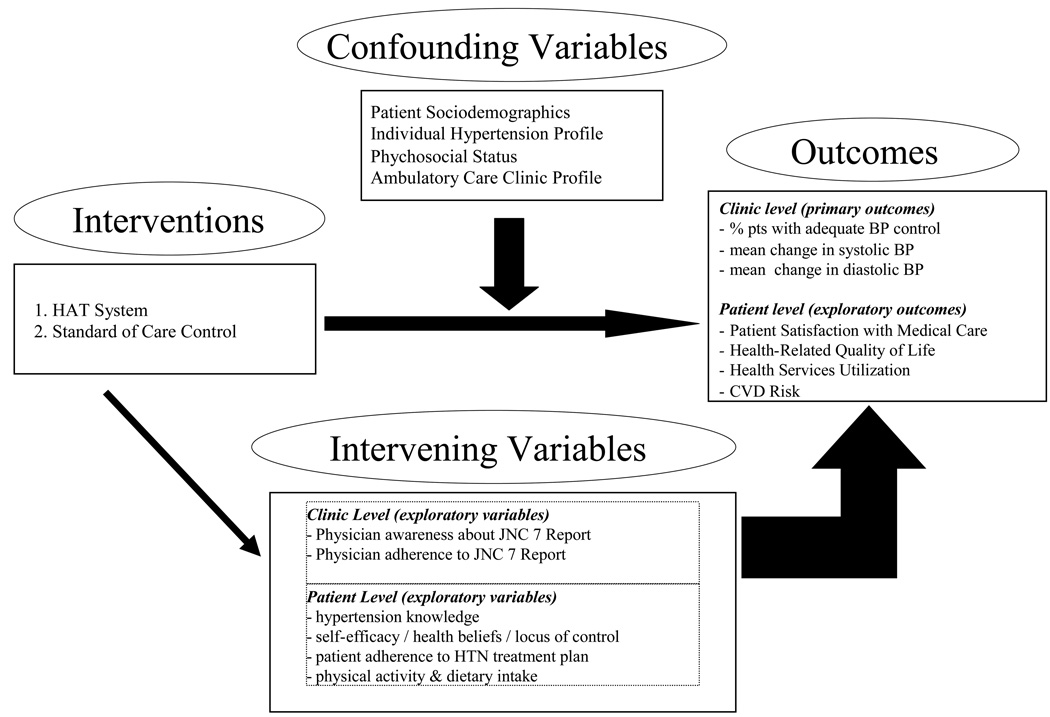
The research model (Figure 1) defines the variables to be measured and their hypothesized associations. Fifty primary care clinics will be randomly assigned to one of two study groups: the HAT intervention (Group 1) or the current standard of care (as recommended by JNC 7) control (Group 2). The individual primary care clinic will be the unit of analysis. For each clinic we will assess the effect of HTN HAT on hypertension control rates and mean change in systolic and diastolic blood pressure. We will also explore the HAT impact on behavioral and cognitive factors affecting patient-centered care, patient satisfaction with care, physician awareness and acceptance of JNC 7 guidelines, and related outcomes. Patient satisfaction with medical care is an exploratory outcome (see Figure 1) measured by a Client Satisfaction Questionnaire (22). The relevant study variables include the 1) independent variables, 2) dependent variables, 3) potential confounding variables and 4) intervening variables. The study variables under each category are listed in the Figure 1.
Figure 1.
HAT Research Model
The major components of ambulatory care practice to be received in the two study groups are presented in Table 2 and described in the text below. The components are subdivided into two sets depending on whether they are delivered on a clinic or a patient level. Clinicians in both study groups undergo a comprehensive education of the JNC 7 guidelines. Patient e-kiosks for hypertension education are installed in waiting rooms in all clinics. Patients in both study groups undergo structured hypertension education and receive the standard of care for hypertension recommended by JNC 7 guidelines. The only difference between the two groups is that in the intervention group both clinicians and patients are assisted by the HAT system.
Table 2.
Comparison of the HTN care to be received by the two study groups.
| HTN Care Component | HTN Standard of Care Control | Intervention (HAT) Group |
|---|---|---|
| Clinic-level | ||
| Academic detailing | X | X |
| JNC 7 materials | X | X |
| Pt. educational e-kiosks | X | X |
| HTN HAT system | X | |
| Patient-level | ||
| Structured HTN education | X | X |
| HTN educational materials | X | X |
| Regular care and follow-up | X | X |
| HTN HAT system | X | |
Clinic-Level Components
Academic detailing has been shown to successfully affect clinician practice patterns (23). In this study, academic detailing of JNC 7 Report is conducted in small groups in all participating clinics by local hypertension care opinion leaders. The academic detailing is supplemented by the distribution of the JNC 7 printed materials to clinicians. In addition, clinicians in the Intervention Clinics receive access to the HAT system to assist them in following the JNC 7 guidelines.
Patient-level Components
All patients enrolled in the study receive structured computer-assisted hypertension education during their baseline study visit. The patients also receive printed materials explaining hypertension treatment and therapeutic lifestyles. We choose to use the computer-assisted education because our studies (24–26) showed that computer-assisted education can be a feasible education alternative in a general patient population regardless of the level of computer literacy and could be at least as effective as one-on-one education. In addition, the patients enrolled at the intervention clinics have the HAT system installed at their homes which assists them in following their individualized hypertension treatment plans.
Hypertension HAT System
Physicians in the intervention clinics receive access to the HAT system from their office desktops. The clinician HAT units provide continuous support in following the JNC 7 guidelines. The HAT functionality includes structured computer-assisted JNC 7 training, interactive clinical decision support for JNC 7 algorithms for pharmacological treatment, multi-component individualized hypertension treatment plans, monthly patient status reports, clinical alerts and reminders.
A nurse case manager (HAT nurse) for this project is responsible for setting up an individualized treatment plan in coordination with the patient primary care provider. The information on each patient’s self-care plan and any following change in the self-care plan is kept in a formalized structured format in the study database. The HAT system uses the information on the self-care plans from the database to assess the patient’s adherence to self-management. In the case of patient non-adherence the HAT system sends corresponding alert message. The alerts are also generated in response to certain clinical criteria that are individually set up for each patient from the HAT website. The HAT nurse reviews the alert messages on daily basis. She responds to the qualifying alerts by calling the patient and by providing case-specific education and counseling in order to reinforce patient self-management. If it is necessary, the alert is forwarded to the patient’s doctor immediately by the nurse. The HAT nurse is responsible for the continuous update of the information in the self-care plan database. The database is available from any Web browser using secure protocol so that all eligible staff is able to easily access the data.
A personal self-care plan consists of a set of self-management guidelines which are individualized for each patient and are presented in a clear and understandable format. In addition to pharmacological treatment section the self-care plan includes components to enforce therapeutic life styles suggested by the JNC 7 Report that are individualized for a particular patient. All patients enrolled from the intervention clinics receive self-care plans that are based on the initial patient evaluation. The self-care plans are coordinated with the patients’ primary care physicians and are given to the patients only after they are approved by their physicians. The self-care plan includes patient’s personal treatment goals, daily medication regimen, self-assessment guidelines including actions that should be undertaken in response to certain symptoms or objective measurements, information on follow-up visits, personalized instructions for the implementation of therapeutic lifestyle changes such as weight reduction, adoption of the DASH (4, 7) eating plan, dietary sodium reduction, physical activity, and moderation of alcohol consumption. The self-care plan is designed as an agreement between the patient and the clinician based on the patient’s needs and preferences for the care of their hypertension management. The self-care plan includes pharmacological and non-pharmacological components. The extent of the patient’s involvement in their care is reflected in three specific behaviors which the patient identified as most important for him or her and for which mutually acceptable goals were set up. The self-care plan is setup by the case manager in collaboration with the patient and can be dynamically updated on the HAT case management portal.
The Study Sample
To be eligible for entry into the study, potential study subjects must satisfy the following inclusion criteria: 1) be a patient with a primary care provider at one of the clinics participating in the study; 2) have a physician diagnosis of hypertension; 3) be 21 years of age or older at the time of randomization; 4) be African-American by self-report; 5) be prescribed at least one medication for hypertension; 6) have poorly controlled blood pressure defined as the average of two, seated BP measurements at each of two consecutive baseline evaluation visits; 7) understand spoken English; 8) have a home telephone; 9) have no other member of the household enrolled in the study.
Patients are ineligible for entry into the study if any of the following exclusionary criteria are met: 1) an identified secondary cause of hypertension; 2) symptomatic myocardial infarction or stroke within the past 6 months; 3) congestive heart failure (NYHA class III or greater); 3) significant renal impairment; 4) diseases likely to lead to noncardiovascular death over the course of the study; 5) evidence that the patient may move from the study area before the completion of the study; 6) presence of any health condition, that would preclude participation (e.g., psychiatric diagnosis or physical disability); 7) any type of chemical dependency.
After completion of each study visit, the patients receive $25 to compensate for their time spent filling out questionnaires and answering interviewers’ questions.
Description of Intervention
General Considerations for Design of HTN HAT System
The HTN HAT system has three major objectives: 1) to help patients in following their self-management plans; 2) to help health care practitioners to follow their patients’ self-management process; 3) to facilitate clinical practices implementing multi-component hypertension management based on the JNC 7 guidelines.
In this randomized clinical trial, patients in the intervention group have the HAT home units (Internet-enabled computer connected to a blood pressure monitor and weight scale) installed in their homes and are instructed on how to use it. They are asked to do self-testing on a regular basis. During self-testing they measure objective parameters and answer questions regarding their symptoms, side effects, medication use, and other self-care actions. Based on the self-testing results the patients receive advice according to the treatment plan prescribed by their provider. Using self-reported data the system determines patient Stage of Change according to the Transtheoretical Model with the respect to a certain activity (i.e., dietary sodium reduction) which is identified in individualized treatment plan. The patients receive short multimedia message according to the current Stage of Change. All patient data is automatically sent by the computer to the HAT Server, where the information is analyzed by the HAT System in real time. For patients who fail to do self-testing regularly, who are non-adherent to their medication regimen (based on self-report), or who consistently fail to answer correctly the educational quizzes, the HAT system will send multimedia education and brief counseling messages that reinforce adherence with their self-care plans. The HAT System also automatically generates alerts each time patients: 1) do not perform self-testing as scheduled, 2) do not take their medications as prescribed, or 3) exceed specified thresholds for clinical parameters. The alerts are checked on a daily basis by the HAT nurse working for the project. The nurse decides whether a particular alert is clinically significant. If necessary, the patients for whom alerts are generated is contacted by phone for individual case management by the nurse. Physicians and patients receive monthly computer-generated reports that summarize the patient’s status and adherence with self-care plan. They are notified immediately by the nurse if a clinically significant event which requires urgent physician’s attention occurs. In addition, physicians have access to the HAT system at their offices and use it for computerized decision support of the JNC 7 guidelines. A general outline for the interactions between HTN HAT and a patient is shown in Table 3, which is annotated in the text below.
Table 3.
Model of HTN HAT-Patient Interaction during the HAT Session
| 1. | Regular patient assessment (symptoms, side effects, medication use, self-care adherence, objective parameters - SBP, DBP, weight) |
| 2. | Help in following an individualized hypertension treatment plan (evaluation of self-testing results, BP goals assessment, feedback according to the individualized self-care plan) |
| 3. | Structured hypertension education |
| 4. | Control of treatment adherence (medications, lifestyles, PCP follow-up visits) |
| 5. | Evaluation of behavioral constructs (such self-efficacy, stage of change) tailored to therapeutic lifestyles |
| 6. | Lifestyle modification counseling (weight control, DASH eating plan, dietary sodium reduction, physical activity, moderation of alcohol consumption) |
| 7. | Social support (virtual patient groups, chat room, message board, e-mail list) |
Structure of a HAT-Patient Session
Each HTN HAT-patient session includes monitoring, analysis and educational components. The patients are guided by the system through each telecommunication session. During the HAT session the patients perform following tasks (1) answer questions on a disease diary, (2) use blood pressure monitor or weight scale when prompted by the system, (3) obtain interpretation of self-testing results and advice according to their self-care plan, (4) receive tailored messages from one or several counseling modules, (5) receive knowledge reinforcement from hypertension education module, (6) use social support and healthy lifestyle promotion modules. The HAT monitoring component interacts with the patient to collect self-testing data. The HAT analysis component interprets the received data according to the patient’s treatment plan and detects clinically significant events and patient non-adherence. The analysis component identifies which part of a patient's treatment plan that patient should follow and which alerts, if any, should be generated. The educational component includes two parts. The first part is based on the results of the analysis component and provides the patient with immediate interpretation of the self-testing. The patient is educated on how to follow the individualized hypertension treatment plan according to the interpretation results and receives information tailored to the current disease status. The second part of the educational component does not depend on the self-testing results and is aimed at providing general disease education. This part is organized in the form of multi-choice questions and “Tips of the day.”
Hypertension education is divided into consecutive sections reflecting following topics: 1) How your body controls blood pressure / A cardiovascular primer, 2) Understanding hypertension, 3) How hypertension hurts your body, 4) Diagnosing and monitoring blood pressure, 5) Therapeutic lifestyles, 6) Medication for hypertension, 7) Emergency situations, 8) Hypertension and other disease, 9) Hypertension in special groups.
Each section is broken into a sequence of simple educational messages that is presented to the patients one-by-one as a “tip of the day.” During each telecommunication session a patient receives a multiple choice question aimed to assess the patient’s understanding of the educational message received by the patient during a previous session. If the patient answers correctly, the next educational message is presented by HAT. If the patient answer is incorrect the educational message from previous session will be presented again. If the patient answers the same question incorrectly several times the HAT system generates an educational alert so that the HAT nurse can discuss a particular topic with the patient. At the end of each section, patients receive a short quiz consisting of 3–5 questions representing topics which are particularly important for hypertension patients to understand. If patients pass the quiz they move to the next section, otherwise they return to the beginning of the current session and repeat it again. Patient progress with educational curriculum is monitored by the HAT system. HAT generates textual and audio messages to reinforce patient education.
Each self-testing session consists of mandatory and optional components. Mandatory components take 10–15 min for the majority of patients to complete. In addition, once a week the mandatory part is broadened to assess diet, physical activity, alcohol consumption, anxiety and depression. This additional component may take 5–7 minutes to complete. The optional components include interactive education, structured lifestyle modification counseling, social support, secure patient-provider messaging, and review of personal goals and achievements. There are no time limits for these activities. A maximal number of consecutive days without self-testing is setup by a case manager for each patient in the HAT case management portal. The case manager receives an alert when this maximum is reached and then contacts patients to mitigate possible self-care issues.
The Role of the HAT Nurse
The HAT nurse is an integral part of the HAT intervention. The nurse acts as a case manager and checks alerts generated by the HAT system on a daily basis. She has to respond to the alerts according to the established guidelines and contacts the patients to counsel and educate them. The non-compliance alerts are usually resolved by the responsible nurse without physician intervention. The patient’s physician is notified of these events in the monthly reports. However, the physician is notified about alerts immediately if serious clinical deterioration occurs in patients who do not comply with their self-care plans.
Considerations for computer interface design for HTN HAT patient unit
The design of HTN HAT interface for patient units was based on our previous experience in successfully introducing this technology to patients with various chronic conditions. The evaluation of home telemonitoring acceptance has been conducted in a group of asthma patients enrolled from low income inner city areas (Washington Heights and Harlem in New York City). The patient population was comprised mostly of African Americans or Hispanics (78%); 45% were employed; 58% never used ATM, and 71 % never used computer before. Our results showed that 74% of the patients perceived self-monitoring as “not complicated at all” and 87% expressed interest in using such a system in the future (12). Similar results were obtained in patients with inflammatory bowel disease. Though 20% of these patients had never used a computer at home, 80% of them believed that the self-testing would not interfere with usual activities and that the self-testing was not complicated (14). High acceptance of the HAT user interface was shown among methadone users using multimedia smoking cessation module. Though 60% of the participants have never used a computer before, 79% of them rated the computer interface as “not complicated at all” (26).
Following steps have been undertaken to ensure successful acceptance of the HAT system by the African American patients with hypertension: 1) recommendations from current literature for development of computer interfaces for this population were incorporated in the HAT design, 2) additional adaptability to personal user preferences were provided by the development of three modifications of the HAT user interface: mouse-, keyboard-, and voice-driven versions, and 3) we implemented a thorough iterative process for the HAT system pre-testing in laboratory environment, in focus groups, and in patient homes. The following specific recommendations have been implemented to improve acceptance of the computer interface: text/background contrast, color-coded content, small number of navigation buttons, increased size of navigation buttons, clearer graphics for menu options, large fonts, simple language, friendly encouraging messages, minimizing amount of information per screen (dividing large messages between several screens), keyboard- or voice driven interfaces.
Challenges and Lessons Learned
The main challenge of the study was to introduce an interactive health communication technology which can be successfully used by our target population at home. To address this challenge we employed an iterative step-wise process of the HAT home unit development that accounted for major principles of user-friendly interface design (27) and for the requirements of development of culturally sensitive content (28). The user interface design issues are described in the previous section. Focus groups were used for the content development. The results of the focus groups have been described (28).
At the beginning of the study, we conducted and analyzed four focus groups with 32 African American participants diagnosed with hypertension to develop a culturally tailored content for a home-based telecare program aimed at improving hypertension care in African Americans. The discussion about the use of technology was well accepted, it identified culturally and gender specific barriers in hypertension care, and generated a comprehensive list of concepts and features to be included in a home-based computerized hypertension telemanagement system. Several categories emerged across the groups, including Barriers, Facilitators, Consumer Suggestions and Technology. The patients identified key health care components and indicated the skills and tasks they perceived as steps towards managing their hypertension which were subsequently included into the home telemanagement program.
Based on the preferences expressed by the focus group participants, the following topics in the interactive hypertension education curriculum were significantly enhanced: stress management, effective communication with providers, navigation of health care system, alternative medicine, social support, community resources.
Results of the focus groups conducted with patients who used this technology, indicated that majority of participants enthusiastically endorsed the notion of using telecare technology to facilitate hypertension management. Based on our previous experience described above, we hypothesize that the hypertension telemanagement will be well accepted by study population.
What We Know?
Routine care delivery of guideline-concordant hypertension care is frequently hampered by multiple barriers at system, clinic, and patient levels
Home telemonitoring programs for patients with hypertension showed improvement in hypertension control rates
Impact of home telemanagement in African Americans with poorly controlled hypertension has not been studied systematically
What This Article Adds?
The proposed clinical trial will evaluate whether the addition of the IT-enhanced care coordination in the routine primary care setting can improve delivery of evidence-based hypertension care in African Americans
Home Automated Telemanagement (HAT) is a telecare system aimed at supporting an informed, activated patient interacting with a prepared, proactive care management team.
Acknowledgments
Funding Sources:
Research grant R01 HL078579 from the NIH
Footnotes
Journal Subject Codes: hypertension, telemedicine, self-management
Clinical Trial Registration Information: NCT00224861
Conflict of Interest Disclosures:
None
References
- 1.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288:1775–1779. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- 2.Walsh JM, McDonald KM, Shojania KG, Sundaram V, Nayak S, Lewis R, Owens DK, Goldstein MK. Quality improvement strategies for hypertension management: a systematic review. Med Care. 2006;44:646–657. doi: 10.1097/01.mlr.0000220260.30768.32. [DOI] [PubMed] [Google Scholar]
- 3.The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. 2003 May; doi: 10.1161/01.HYP.0000107251.49515.c2. NIH Publication No. 03-5233. [DOI] [PubMed]
- 4.Artinian NT, Washington OGM, Templin TN. Effects of home telemonitoring and community-based monitoring on blood pressure control in urban African Americans: A pilot study. Heart & Lung. 2001;30:191–199. doi: 10.1067/mhl.2001.112684. [DOI] [PubMed] [Google Scholar]
- 5.Rogers MAM, Small D, Buchan DA, Butch CA, Stewart CM, Krenzer BE, Husovsky HL. Home monitoring service improves mean arterial pressure in patients with essential hypertension. Ann Intern Med. 2001;134:1024–1032. doi: 10.7326/0003-4819-134-11-200106050-00008. [DOI] [PubMed] [Google Scholar]
- 6.Green BB, Cook AJ, Ralston JD, Fishman PA, Catz SL, Carlson J, Carrell D, Tyll L, Larson EB, Thompson RS. Effectiveness of home blood pressure monitoring, Web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA. 2008;299:2857–2867. doi: 10.1001/jama.299.24.2857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moore TJ, Alsabeeh N, Apovian CM, Murphy MC, Coffman GA, Cullum-Dugan D, Jenkins M, Cabral H. Weight, blood pressure, and dietary benefits after 12 months of a Web-based Nutrition Education Program (DASH for health): longitudinal observational study. J Med Internet Res. 2008;10:e52. doi: 10.2196/jmir.1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Finkelstein J, Khare R, Vora D. Home Automated Telemanagement (HAT) system to facilitate self-care of patients with chronic diseases. J Systemics, Cybernetics Informat. 2003;1:78–82. [Google Scholar]
- 9.Wagner EH. Chronic Disease Management: What will it take to improve care for chronic illness? Effective Clinical Practice. 1998;1:2–4. [PubMed] [Google Scholar]
- 10.Finkelstein J, O'Connor G, Friedman RH. Development and implementation of the home asthma telemonitoring (HAT) system to facilitate asthma self-care. Stud Health Technol Inform. 2001;84:810–814. [PubMed] [Google Scholar]
- 11.Cross RK, Finkelstein J. Feasibility and Acceptance of a Home Telemanagement System in Patients with Inflammatory Bowel Disease: A 6-Month Pilot Study. Digestive Diseases and Sciences. 2007;52:357–364. doi: 10.1007/s10620-006-9523-4. [DOI] [PubMed] [Google Scholar]
- 12.Finkelstein J, Cabrera M, Hripcsak G. Internet-based Home Asthma Telemonitoring: Can patients handle the technology? Chest. 2000;117:148–155. doi: 10.1378/chest.117.1.148. [DOI] [PubMed] [Google Scholar]
- 13.Finkelstein J, O'Connor GT, Galichina N. Feasibility of Internet-based Home Automated Telemanagement in patients with Chronic Obstructive Pulmonary Disease. Chest. 2001;120:253S. [Google Scholar]
- 14.Cross RK, Arora M, Finkelstein J. Acceptance of telemanagement is high in patients with inflammatory bowel disease. J Clin Gastroenterol. 2006;40:200–208. doi: 10.1097/00004836-200603000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Finkelstein J, Lapshin O, Castro C, Cha E, Provance PG. Home-based physical telerehabilitation in patients with multiple sclerosis: A pilot study. J Rehab Res Develop. 2008;45:1361–1373. [PubMed] [Google Scholar]
- 16.Bandura A. Social Learning Theory. Englewood Cliffs. NJ: Prentice Hall; 1977. [Google Scholar]
- 17.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 18.Rhodes F, Fishbein M, Reis J. Using behavioral theory in computer-based health promotion and appraisal. Health Education & Behavior. 1997;24:20–34. doi: 10.1177/109019819702400105. [DOI] [PubMed] [Google Scholar]
- 19.Theory at Glance. A Guide for Health Promotion Practice. 2005 September; NIH Publication No. 05-3896.
- 20.Massaro DW, Cowan N. Information processing models: microscopes of the mind. Annu Rev Psychol. 1993;44:383–425. doi: 10.1146/annurev.ps.44.020193.002123. [DOI] [PubMed] [Google Scholar]
- 21.Cushman WC, Ford CE, Cutler JA, Margolis KL, Davis BR, Grimm RH, Black HR, Hamilton BP, Holland J, Nwachuku C, Papademetriou V, Probstfield J, Wright JT, Alderman MH, Weiss RJ, Piller L, Bettencourt J, Walsh SM. Success and predictors of blood pressure control in diverse North American settings: The antihypertensive and lipid-lowering treatment to prevent heart attack trial. Journal of Clinical Hypertension. 2002;4:393–404. doi: 10.1111/j.1524-6175.2002.02045.x. [DOI] [PubMed] [Google Scholar]
- 22.Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: Development of a general scale. Evaluation and Program Planning. 1979;2:197–207. doi: 10.1016/0149-7189(79)90094-6. [DOI] [PubMed] [Google Scholar]
- 23.Solomon DH, Houten L, Glynn RJ, Baden L, Curtis K, Schrager H, Avorn J. Academic detailing to improve use of broad-spectrum antibiotics at an academic medical center. Arch Intern Med. 2001;161:1897–1902. doi: 10.1001/archinte.161.15.1897. [DOI] [PubMed] [Google Scholar]
- 24.Finkelstein J, Lapshin O. Reducing depression stigma using a web-based program. International J Medical Informatics. 2007;76:726–734. doi: 10.1016/j.ijmedinf.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 25.Finkelstein J, Lapshin O, Wasserman E. Randomized Study of Different Anti-Stigma Media. Patient Educ Couns. 2008;71:204–214. doi: 10.1016/j.pec.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 26.Finkelstein J, Lapshin O, Cha E. Feasibility of Promoting Smoking Cessation Among Methadone Users Using Multimedia Computer-Assisted Education. Journal of Medical Internet Research. 2008;10:e33. doi: 10.2196/jmir.1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nielsen J. Usability Engineering. San Diego, CA: Academic Press; 1993. [Google Scholar]
- 28.Li J, Garcia S, Castro HK, DeForge BR, Hise MK, Finkelstein J. Acceptance and expectations of information technology to support hypertension self-care in African Americans: a qualitative inquiry. AMIA Annu Symp Proc. 2007:1032. [PubMed] [Google Scholar]