Abstract
Background
The effects of lifestyle changes and evolving treatment practices on coronary disease incidence rates, demographic and clinical profile, as well as the short-term outcomes of patients hospitalized with acute myocardial infarction (AMI) have not been well characterized. The purpose of this study was to examine multi-decade long trends (1975–2005) in the incidence rates, demographic and clinical characteristics, treatment practices, and hospital outcomes of patients hospitalized with an initial AMI from a population-based perspective.
Methods and Results
Residents of the Worcester (MA) metropolitan area (median age = 37 years; 89% Caucasian) hospitalized with an initial AMI (n=8,898) at all greater Worcester medical centers during 15 annual periods between 1975 and 2005 comprised the sample of interest.
The incidence rates of initial AMI were lower in 2005 (209/100,000 population) than in 1975 (277/100,000), though these trends varied inconsistently over time. Patients hospitalized during the most recent study years were significantly older (mean age = 64 years in 1975; 71 years in 2005), more likely to be women (38% in 1975; 48% in 2005), and have a greater prevalence of comorbidities. Hospitalized patients were increasingly more likely to receive effective cardiac medications and coronary interventional procedures over the period under investigation. Hospital survival rates improved significantly over time (81% survived in 1975; 91% survived in 2005) while varying trends were observed in the occurrence of clinically important complications.
Conclusions
The results of this community-wide investigation provide insights into the changing magnitude, characteristics, management practices, and outcomes of patients hospitalized with a first MI.
Keywords: acute myocardial infarction, community-wide trends, surveillance
Introduction
The death rates attributed to coronary heart disease (CHD) have declined on a consistent basis in the U.S. as well as in a number of other industrialized countries since the mid to late 1960’s1,2. The reasons for the ongoing decline in CHD related mortality are incompletely understood, however, and represent the multifactorial effects of a variety of changes in different lifestyle practices and treatment approaches to CHD and its predisposing factors. Remarkable advances in the primary prevention and treatment of acute myocardial infarction (AMI) have taken place during the past several decades.
Despite these encouraging trends, CHD remains the leading cause of death in American men and women. Moreover, data from varying sources suggests continuing increases in the prevalence of obesity, diabetes, and less than optimal awareness and control of heart healthy eating practices and other coronary risk factors that may be associated with future increases in the incidence rates of acute coronary disease2.
The Worcester Heart Attack Study has been conducting population-based surveillance of AMI in residents of a large central New England metropolitan area hospitalized at all greater Worcester (MA) medical centers since the mid-1970s3–5. This observational study offers a unique opportunity to examine recent, and 30 year long (1975–2005), trends in the contemporary landscape of AMI, highlighting areas in need of further improvement in the prevention and/or management of acute coronary disease.
Methods
Residents of the Worcester metropolitan area (2000 census = 478,000) who were hospitalized with a discharge diagnosis of AMI at all 16 Worcester Standard Metropolitan Statistical Area (SMSA) hospitals during 1975, 1978, 1981, 1984, 1986, 1988, 1990, 1991, 1993, 1995, 1997, 1999, 2001, 2003 and 2005 comprised the study population3–5. In 2000, the median age of residents of the Worcester SMSA was 37 years, 49% were men, 89% were Caucasian, and approximately one quarter had a bachelor’s degree or higher. The periods under study were selected due to the availability of grant funding and for purposes of examining changes in our principal study outcomes over an approximate alternate year basis. All hospitals in the Worcester SMSA participated in this study. Originally, there were 16 health care facilities that were canvassed; in more recent years, fewer hospitals (n=11) have been providing care to greater Worcester residents due to hospital closures, mergers, or conversion to long-term care or rehabilitation facilities. Of the current 11 hospitals, 3 are considered to be tertiary care/university based medical centers. Approximately three quarters of patients with confirmed AMI had been hospitalized at these tertiary care medical centers over the years under study with little change in this proportion noted over time.
The details of this study have been described elsewhere3–5. In brief, the medical records of residents of the Worcester SMSA who had been hospitalized for possible AMI were individually reviewed and validated according to predefined diagnostic criteria. These criteria included a clinical history of prolonged chest pain not relieved by rest or use of nitrates, serum levels of various biomarkers in excess of the upper limit of normal as specified by the laboratory at each greater Worcester hospital, and serial electrocardiographic tracings during hospitalization showing changes in the ST segment and/or Q waves typical of AMI. At least 2 of these 3 criteria needed to be satisfied for study inclusion. Cases of perioperative-associated AMI were not included. Persons hospitalized at any of the greater Worcester medical centers who did not reside in the Worcester metropolitan area were not included in the study sample.
The present sample was restricted to patients with an initial AMI since we were interested in describing the clinical features and epidemiology of acute coronary disease in patients with a first clinical manifestation of underlying coronary atherosclerosis. Patients with a first MI were defined as those in which either mention was made in the review of the hospital charts that this was the patient’s first admission for a MI or the review of prior medical records and electrocardiograms failed to indicate the occurrence of a previous MI.
Data collection
Sociodemographic, medical history, and clinical data were abstracted from the hospital medical records of geographic and diagnostically eligible patients by trained study physicians and nurses. Information was collected about patient’s age, sex, race, length of hospital stay, comorbidities, AMI type, occurrence of clinically significant hospital complications6–8, and hospital survival status. Information was collected about the prescribing of different cardiac medications and coronary interventional procedures as they became available to clinical practice9. Both nurse’s and physician’s progress notes, and medication administration records and test results, were reviewed to ascertain the use of cardiac medications and coronary interventional procedures during hospitalization. Medication prescribing rates were calculated in the total sample of patients with confirmed AMI and were not restricted to those who did not have contraindications to the receipt of these therapies. Since the hospital length of stay of patients with AMI has declined considerably over time, and may have confounded the interpretation of changing trends in hospital death rates, we also presented data about 30 day death rates after hospital admission for AMI. Some form of additional follow-up after hospital discharge was available for the vast majority (~99%) of hospitalized patients during the years under study.
Data analysis
The age adjusted incidence rates of initial AMI were calculated using indirect adjustment to the age distribution of the 2000 greater Worcester population. Census data were derived from both statewide and national sources and estimates of the greater Worcester population were constructed based on extrapolated estimates during intercensal years. Confidence intervals (95%) were calculated on our hospital incidence rates of initial AMI using the Poisson error distribution10. The significance of changing trends in the incidence rates of initial AMI was examined using Poisson regression. Differences in the distribution of demographic and clinical factors in patients who had been hospitalized with an initial AMI over time were examined with the chi-square test for trends and analysis of variance for discrete and continuous variables, respectively.
The short-term prognosis in each period was examined by calculating in-hospital case-fatality rates (CFRs). This term was used instead of a mortality rate since it more appropriately describes the lethality associated with a particular disease in a patient population (e.g., AMI). For the calculation of the CFR’s associated with a particular clinical condition, the denominator consists of those with the condition (e.g. patients who developed cardiogenic shock) while the numerator refers to the number of those who died as a result of this complication.
A logistic multivariable regression analysis was used to examine changes over time in hospital CFRs, and occurrence of clinically significant hospital complications, while controlling for potentially confounding demographic (e.g., age, sex) and clinical prognostic factors (e.g., prior comorbidities, AMI type). These variables were considered as potential confounders since this study, as well as prior investigations, have shown that these factors can affect hospital death and complication rates after AMI and need to be analytically controlled for. The Hosmer-Lemeshow goodness of fit test was utilized to examine the adequacy of the logistic regression model for each clinical outcome. Given the nonrandomized nature of the present study, and the caveats and difficulties involved in the interpretation of any multivariable adjusted estimates of association, we did not control for the hospital use of cardiac treatment strategies in our regression analyses in which hospital survival status, or development of important clinical complications, were our key study outcomes. The SAS Institute Statistical Analysis System was utilized for all statistical analyses. Human subjects approval for this study was obtained from the Committee for the Protection of Human Subjects at the University of Massachusetts Medical School.
The authors had full access to, and take full responsibility for, the integrity of the data. All authors have read and agree to the manuscript as written.
Results
A total of 8,898 residents of the Worcester metropolitan area were hospitalized with an initial AMI during the period under study. Overall, the average age of study patients was approximately 71 years, 48% were women, and 95% were Caucasian.
Incidence Rates of Initial MI
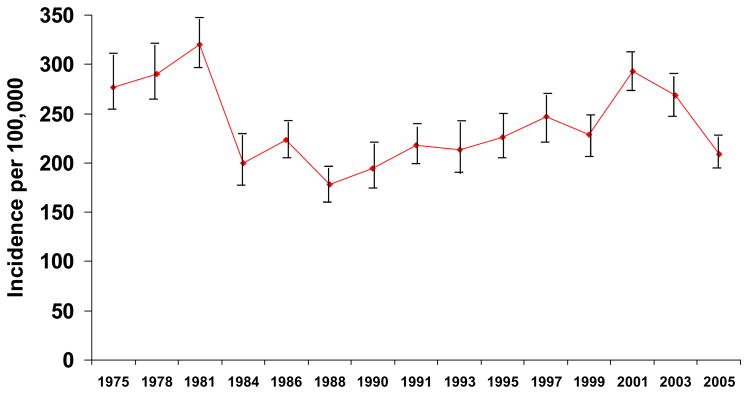
The age-adjusted hospital incidence rates (per 100,000 population) of initial MI’s in greater Worcester residents increased from 277 in 1975 to a peak of 320 in 1981 (Figure 1). There was a gradual increase in the incidence rates of AMI between 1988 and 2001 after which time these incidence rates declined to 209 in our most recent study year of 2005 (P=0.42 for overall trends) (Figure 1).
Figure 1.
Trends in the incidence rates of initial acute myocardial infarction
Patient Characteristics Associated with Initial AMI
Patients who were admitted to greater Worcester hospitals with an initial AMI during recent, as compared to earlier, study years were significantly older (mean age = 63.5 years in 1975; mean age = 70.8 years in 2005), more likely to be women, to be obese, and to have a prior history of diabetes, hypertension, stroke, or heart failure (Table 1). The average hospital stay has declined markedly over time from an average of 17 days in the mid-1970’s to approximately 5 days in 2005. Duration of prehospital delay after the onset of acute coronary symptoms to the seeking of medical care remained essentially unchanged over time (Table 1).
Table 1.
Characteristics of Patients With Initial Acute Myocardial Infarction According to Time Period of Hospitalization
| Characteristics | 1975/1978 (n=1,077) |
1981/1984 (n=1,098) |
1986/1988 (n=973) |
1990/1991 (n=1,069) |
1993/1995 (n=1,187) |
1997/1999 (n=1,351) |
2001/2003 (n=1,553) |
2005 (n=590) |
|---|---|---|---|---|---|---|---|---|
| Age (yrs) (%)*** | ||||||||
| <55 | 24.2 | 20.3 | 17.4 | 18.3 | 20.6 | 18.7 | 17.8 | 17.4 |
| 55–64 | 26.3 | 24.2 | 22.9 | 19.1 | 17.4 | 18.4 | 17.4 | 15.8 |
| 65–74 | 25.9 | 25.5 | 30.5 | 28.5 | 26.0 | 21.9 | 20.9 | 20.9 |
| 75–84 | 17.4 | 20.5 | 19.7 | 24.5 | 25.3 | 27.5 | 27.2 | 25.9 |
| ≥85 | 6.2 | 9.5 | 9.6 | 9.5 | 10.9 | 13.5 | 16.7 | 20.1 |
| Age (mean, yrs)*** | 64.2 (+13.1) | 65.7 (+15.3) | 67.0 (+13.6) | 67.5 (+14.1) | 67.5 (+14.0) | 68.9 (+14.4) | 69.9 (+14.6) | 70.8 (+14.6) |
| Male sex (%)*** | 62.2 | 60.8 | 59.5 | 56.2 | 57.7 | 57.9 | 56.7 | 51.7 |
| White race (%)*** | 96.2 | 98.5 | 98.4 | 96.1 | 95.7 | 94.9 | 89.9 | 91.9 |
| Body mass index (%, ≥30) | --† | -- | -- | -- | 25.4 | 24.6 | 29.5 | 31.7 |
| Prehospital delay (median, hours) | -- | -- | 2.1 | 2.2 | 2.3 | 2.0 | 2.0 | 1.9 |
| Length of hospital stay (mean, days)*** | 17.0 (+10.1) | 14.4 (+12.8) | 11.7 (+9.7) | 10.5 (+10.0) | 7.9 (+5.9) | 6.1 (+5.3) | 5.9 (+5.9) | 5.3 (+5.0) |
| Cardiac rehabilitation (%) | -- | -- | 15.5 | 18.4 | 20.7 | 18.5 | 19.9 | 6.9 |
| Medical History (%) | ||||||||
| Angina** | 16.2 | 20.6 | 19.4 | 19.0 | 18.4 | 17.8 | 16.9 | 10.7 |
| Diabetes*** | 19.3 | 18.7 | 23.2 | 21.8 | 23.9 | 25.7 | 28.1 | 28.3 |
| Hypertension*** | 39.9 | 48.6 | 48.2 | 50.6 | 54.8 | 56.6 | 64.8 | 72.0 |
| Stroke*** | 4.0 | 6.7 | 8.2 | 7.0 | 7.8 | 8.2 | 9.3 | 9.2 |
| Heart failure*** | 6.9 | 8.9 | 7.1 | 8.2 | 9.9 | 13.6 | 15.0 | 19.7 |
| Current smoker*** | -- | -- | -- | -- | -- | 23.4 | 24.9 | 23.1 |
| Physiologic Findings | ||||||||
| Initial heart rate (mean, bpm) | -- | -- | 83.4 (+22.9) | 84.9 (+24.0) | 85.0 (+24.4) | 85.3 (+23.9) | 86.7 (+24.4) | 86.6 (+22.8) |
| Systolic BP (mean, mmHg) | -- | -- | -- | -- | -- | 143.5 (+33.3) | 142.4 (+35.3) | 142.3 (+32.2) |
| Diastolic BP (mean, mmHg)** | -- | -- | -- | -- | -- | 80.2 (+21.2) | 78.4 (+21.3) | 76.7 (+20.3) |
| Initial cholesterol (mean, mg/dl)*** | 233.6 (+57.7) | 228.1 (+56.9) | 222.1 (+54.6) | 216.7 (+54.0) | 204.3 (+52.6) | 193.6 (+46.1) | 183.8 (+55.9) | 174.4 (+48.6) |
| Initial HDL cholesterol (mean, mg/dl) | -- | -- | -- | -- | 40.8 (+11.7) | 42.3 (+11.1) | 43.2 (+13.2) | 41.4 (+12.2) |
| Initial LDL cholesterol (mean, mg/dl)*** | -- | -- | -- | -- | 122.1 (+39.2) | 122.0 (+51.3) | 112.3 (+39.8) | 106.6 (+42.1) |
| Creatinine (mean, mg/dl)** | -- | -- | -- | -- | 1.2 (+0.8) | 1.3 (+1.0) | 1.4 (+1.1) | 1.4 (+1.1) |
| Glucose (mean, mg/dl) | -- | -- | -- | -- | 184.5 (+112.5) | 175.0 (+94.5) | 180.9 (+158.8) | 172.9 (+99.8) |
| Hemoglobin (mean, mg/dl) | -- | -- | -- | -- | 13.8 (+2.0) | 13.7 (+2.4) | 13.8 (+5.6) | 13.5 (+2.0) |
| Q wave AMI*** | 70.9 | 63.7 | 57.8 | 55.0 | 48.5 | 42.3 | 25.7 | 22.7 |
| ST segment elevation AMI (%) | -- | -- | -- | -- | -- | 52.6 | 38.4 | 36.1 |
p<.001;
p<.01;
p<.05;
information not collected during specified period
During the most recent years under study, hospitalized patients had a higher heart rate and serum creatinine levels at the time of hospital admission compared with earlier study years. Patients hospitalized during the 2000’s had lower initial total serum cholesterol levels than patients hospitalized during earlier study years.
The proportion of patients with a Q-wave MI declined from approximately 70% in 1975 to less than 25% in 2005 (Table 1). In 1997, we began collecting information on whether the patient’s ECG showed ST segment elevation changes or otherwise. In 1997, 49.2% of patients were diagnosed with an ST segment elevation AMI; this percentage was 40.0% in 2001 and 36.1% in 2005.
Use of Cardiac Medications and Coronary Interventional Procedures
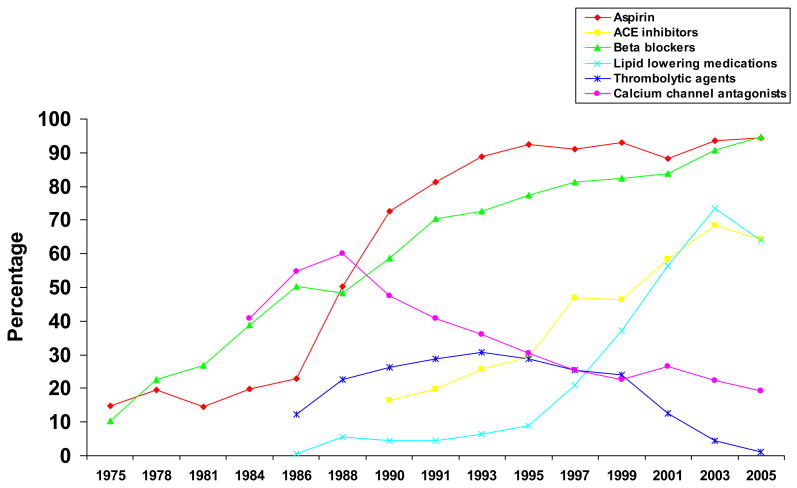
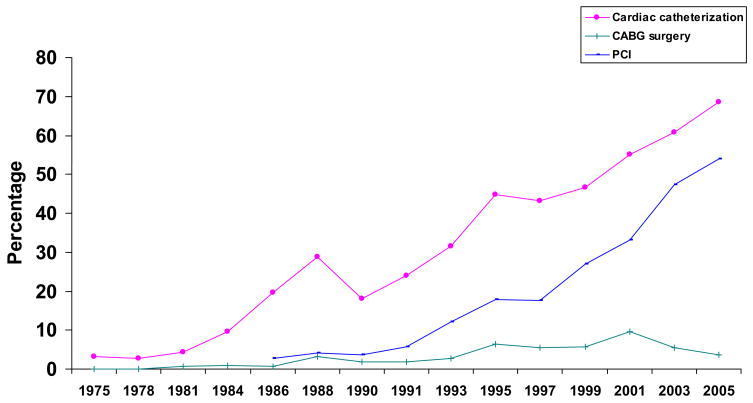
Marked increases in the use of aspirin, angiotensin converting enzyme inhibitors, beta blockers, and lipid lowering medications were observed during the years under study (Figure 2). On the other hand, use of thrombolytic therapy has declined markedly during recent years, such that only 1.2% of patients hospitalized in 2005 received thrombolytic therapy. Hospital use of calcium antagonist agents also declined. Use of cardiac catheterization and percutaneous coronary interventions (PCI) has increased markedly over time whereas the use of CABG surgery during hospitalization has increased during the 1990’s and declined in the 2000’s (Figure 2). Cardiac catheterization, PCI, and CABG surgery were respectively utilized in 68.5%, 53.9%, and 3.7% of patients hospitalized with an initial AMI during 2005 (Figure 3). (double check)
Figure 2.
Use of cardiac medications according to time period of hospitalization
Figure 3.
Use of cardiac procedures and coronary reperfusion strategies according to time period of hospitalization
Frequency and Death Rates of Acute Clinical Complications
Patients hospitalized with AMI during the most recent study years were more likely to develop atrial fibrillation compared with patients hospitalized in the early study years (Table 2). Patients hospitalized during recent study years were slightly less likely to develop cardiogenic shock with inconsistent trends noted in the occurrence of heart failure. Encouragingly, the hospital CFR’s associated with each of these important clinical complications have declined appreciably over time despite the advanced age and greater prevalence of comorbidities in patients hospitalized with AMI during our most recent study years (Table 2).
Table 2.
Risk of Developing Selected Hospital Complications and Hospital Case-Fatality Rates (CFR) in Patients Hospitalized With Initial Acute Myocardial Infarction According to Time Period of Hospitalization
| Heart Failure (HF) |
Atrial Fibrillation (AF) |
Cardiogenic Shock |
Hospital Death |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Crude Frequency (%) |
Adjusted Risk of HF* |
CFR (%) |
Multivariate Odds of Death* |
Crude Frequency (%) |
Adjusted Risk of AF* |
CFR (%) |
Multivariate Odds of Death* |
Crude Frequency (%) |
Adjusted Risk of Shock* |
CFR (%) |
Multivariate Odds of Death* |
CFR (%) |
Multivariate Odds of Dying |
|
| 1975 | 33.1 | 1.0 | 34.3 | 1.0 | 11.4 | 1.0 | 32.2 | 1.0 | 6.6 | 1.0 | 73.5 | 1.0 | 19.1 | 1.0 |
| 1978 | 36.0 | 1.16 (0.88,1.52) | 28.4 | 0.61 (0.36,1.03) | 13.6 | 1.24 (0.85,1.81) | 27.6 | 0.65 (0.27,1.52) | 5.9 | 0.88 (0.54,1.46) | 78.8 | 1.39 (0.35,5.50) | 16.7 | 0.62 (0.43,0.92) |
| 1981 | 34.0 | 0.97 (0.74,1.26) | 27.2 | 0.43 (0.26,0.73) | 15.3 | 1.29 (0.90,1.85) | 22.5 | 0.33 (0.14,0.78) | 7.0 | 1.08 (0.67,1.72) | 77.8 | 0.97 (0.29,3.27) | 16.0 | 0.43 (0.30,0.63) |
| 1984 | 46.8 | 2.28 (1.71,3.03) | 20.5 | 0.33 (0.19,0.57) | 21.6 | 2.46 (1.70,3.56) | 21.2 | 0.37 (0.16,0.86) | 4.8 | 0.73 (0.42,1.27) | 68.2 | 0.51 (0.13,2.03) | 13.3 | 0.35 (0.23,0.53) |
| 1986 | 37.6 | 1.42 (1.07,1.87) | 28.3 | 0.38 (0.23,0.66) | 17.1 | 1.78 (1.22,2.57) | 24.4 | 0.37 (0.16,0.87) | 7.6 | 1.19 (0.71,1.86) | 87.5 | 2.81 (0.63,12.47) | 16.9 | 0.38 (0.26,0.57) |
| 1988 | 33.6 | 1.15 (0.85,1.55) | 30.0 | 0.45 (0.25,0.78) | 18.2 | 1.87 (1.27,2.74) | 38.3 | 0.74 (0.32,1.68) | 7.2 | 1.17 (0.70,1.95) | 84.4 | 2.70 (0.57,12.82) | 17.0 | 0.40 (0.26,0.60) |
| 1990 | 34.9 | 1.24 (0.93,1.66) | 24.1 | 0.29 (0.16,0.50) | 22.4 | 2.46 (1.71,3.54) | 22.3 | 0.34 (0.15,0.77) | 4.6 | 0.68 (0.39,1.18) | 82.6 | 0.76 (0.17,3.49) | 15.2 | 0.30 (0.20,0.46) |
| 1991 | 33.0 | 1.15 (0.87,1.52) | 16.0 | 0.22 (0.12,0.39) | 14.4 | 1.44 (0.99,2.10) | 22.0 | 0.28 (0.12,0.67) | 4.7 | 0.72 (0.42,1.22) | 51.9 | 0.38 (0.10,1.49) | 10.7 | 0.22 (0.14,0.33) |
| 1993 | 30.7 | 1.09 (0.82,1.45) | 18.3 | 0.17 (0.10,0.31) | 11.7 | 1.21 (0.81,1.79) | 19.4 | 0.22 (0.09,0.55) | 5.8 | 0.92 (0.55,1.53) | 72.7 | 0.70 (0.19,2.58) | 11.0 | 0.17 (0.11,0.26) |
| 1995 | 35.6 | 1.48 (1.12,1.96) | 17.4 | 0.13 (0.08,0.23) | 13.5 | 1.49 (1.02,2.18) | 20.5 | 0.19 (0.08,0.47) | 8.9 | 1.50 (0.94,2.39) | 45.5 | 0.22 (0.07,0.69) | 11.7 | 0.15 (0.10,0.23) |
| 1997 | 27.2 | 0.90 (0.68,1.20) | 18.5 | 0.14 (0.08,0.25) | 12.4 | 1.30 (0.89,1.90) | 22.1 | 0.18 (0.07,0.44) | 7.8 | 1.28 (0.80,2.04) | 55.6 | 0.23 (0.08,0.73) | 11.5 | 0.14 (0.10,0.22) |
| 1999 | 32.8 | 1.22 (0.92,1.61) | 17.7 | 0.13 (0.07,0.23) | 16.5 | 1.83 (1.26,2.64) | 16.7 | 0.15 (0.06,0.35) | 6.1 | 1.02 (0.62,1.67) | 65.0 | 0.33 (0.10,1.08) | 11.1 | 0.13 (0.08,0.19) |
| 2001 | 34.1 | 1.22 (0.93,1.60) | 17.0 | 0.14 (0.08,0.24) | 21.1 | 2.36 (1.66,3.36) | 21.6 | 0.21 (0.10,0.48) | 6.1 | 1.10 (0.68,1.78) | 34.7 | 0.12 (0.04,0.40) | 11.1 | 0.14 (0.09,0.21) |
| 2003 | 34.7 | 1.41 (1.06,1.86) | 11.2 | 0.08 (0.04,0.14) | 22.2 | 2.73 (1.91,3.90) | 13.3 | 0.10 (0.04,0.23) | 3.5 | 0.65 (0.37,1.13) | 46.2 | 0.12 (0.03,0.45) | 7.8 | 0.08 (0.05,0.13) |
| 2005 | 31.5 | 1.02 (0.76,1.37) | 17.2 | 0.11 (0.06,0.19) | 22.9 | 2.67 (1.85,3.85) | 18.5 | 0.14 (0.06,0.33) | 5.1 | 0.93 (0.54,1.60) | 43.3 | 0.12 (0.03,0.44) | 9.5 | 0.09 (0.06,0.15) |
Controlling for age, sex, length of hospital stay, prior history of angina, hypertension, diabetes, stroke, heart failure and MI type.
Controlling for age, sex, length of hospital stay, prior history of angina, hypertension, diabetes, stroke, heart failure, MI type, and complicated AMI.
We carried out a series of multivariable adjusted regression analyses for purposes of examining changing trends in the risk of, and mortality associated with, these hospital outcomes while controlling for several demographic and clinical factors of prognostic importance (Table 2). The results of these analyses showed inconsistent trends in the risk of developing atrial fibrillation, heart failure, and cardiogenic shock over the period under study. Declines over time in the hospital death rates associated with each of these clinical complications were observed.
Declines in hospital death rates occurred over the period under study. In 1975, the hospital CFR was 19.1% compared to 9.5% in 2005 (Table 2). Since the average stay for patients hospitalized with AMI has declined markedly over time, we also examined changing trends in 30 day CFR’s from the time of hospital admission during the years under study. The results of this analysis confirmed previously observed declines in hospital death rates associated with AMI. In 1975/78, the 30 day death rates after hospital admission were 17.6% while these death rates were 11.9% in 2003/05.
Discussion
The results of this community-wide study suggest declines in the incidence rates of initial AMI during the most recent years under study. There have been considerable changes in the demographic, clinical, and treatment profile of greater Worcester residents hospitalized with a first AMI at all area medical centers. Encouraging declines in short-term death rates were observed between 1975 and 2005 as were declines in the hospital death rates of several important clinical complications.
Incidence Rates of Initial AMI
The age-adjusted incidence rates of AMI in residents of the Worcester metropolitan area increased during the initial study years, declined for several years thereafter, increased steadily until 2001, and then declined through 2005. To the best of our knowledge, ours is the first of the few ongoing community-based coronary disease surveillance projects in the U.S. or overseas to provide data about changing trends in the incidence rates of AMI in the 21st century.
Although we can only speculate about the reasons for the declining incidence rates of MI observed during the most recent years under study, it is not unreasonable to suggest that reductions in the magnitude of AMI are related to declines in the population rates of cigarette smoking and increased awareness and treatment of hyperlipidemia, hypertension, and other risk factors for AMI that have been noted in other studies2,11. It is possible, however, that there may have been concomitant changes in out-of-hospital deaths due to AMI in this population over time, increases in the prevalence of unrecognized MI’s, and changes in patient’s care seeking behavior over the 30 year period under study, though the latter factor has not changed appreciably in patients hospitalized with AMI during the years under study.
In the Minnesota Heart Survey, the age-adjusted rates of hospitalizations for incident events of MI in Minneapolis-St. Paul residents declined by approximately 5% between the single study years of 1985 and 1990 and by an additional 10% between 1990 and 199512. In the Olmsted County (MN) surveillance project, the incidence rates of AMI declined between 1979 and 1998, though a total of less than 2,000 incident events of AMI occurred in this population during the 2 decade long period under study13. In the NHANES-I Epidemiologic Follow-up Study, the age-adjusted incidence rates of initial AMI were unchanged over the period 1971–199214. In the Atherosclerosis Risk in Communities (ARIC) study, relatively stable incidence rates of AMI were observed between 1987 and 199615.
Differences in the magnitude and changing patterns of acute coronary disease observed in the U.S. may be partially explained by the definitions of AMI utilized, years under study, and by the size, representativeness, and characteristics of the populations under study. Assessing secular changes in the incidence rates of AMI is challenging given the reliance on hospital administrative systems, extent and quality of information recorded in patient’s hospital charts, the validation process, and comprehensiveness of the coronary disease surveillance system.
There have been marked changes over time in the type of AMI patients present with. The increasing proportion of patients hospitalized with a non-ST segment elevation AMI may represent the increasing sensitivity of diagnostic tests utilized over time, from the creatine kinase assays used during the early study years to the currently utilized troponin assays. In 2005, 89% of patients with AMI had positive troponin findings. These changing patterns of AMI may also be due to the older age and greater prevalence of comorbidities in hospitalized patients and greater use of effective cardiac medications both prior to, and during, the acute hospitalization. More contemporary data in different population settings are needed to characterize the changing epidemiology of AMI16.
Changing Profile of Patients Hospitalized with AMI
Residents of the Worcester metropolitan area hospitalized with AMI during the most recent years under study were significantly older and were more likely to be women than patients who were hospitalized during earlier study years. This shift in delaying the onset of AMI to an older age, while reflective of the aging of the U.S. population and improvements in the care of patients with pre-existing coronary disease, is likely also to be due to the increasing adoption of healthy lifestyle practices and other primary preventive modalities in the general population and in various at risk groups. There have also been marked increases over time in the proportion of our patient population presenting with other clinically important chronic diseases. This shifting patient profile towards the admission of increasingly older patients with a greater prevalence of serious comorbidities has important implications for the management of these increasingly complex patients.
While detailed evidence-based guidelines for the management of patients with AMI are available to assist clinicians, it is important to recognize that a substantial proportion of hospitalized patients may have selected medication contraindications, and/or require modifications, to routine treatment plans. It was of interest to note that patients hospitalized during recent study years were much more likely to be obese and/or have diabetes previously diagnosed. These trends likely reflect the ongoing epidemic of obesity and diabetes in North America. If declines in the incidence rates of AMI are to continue, improvements in the primary prevention and management of patients with these metabolic disorders, similar to what has been achieved for the control of hypercholesterolemia, will be necessary.
The changing baseline characteristics of our patient population are similar to those observed in the National Registry of Myocardial Infarction (NRMI)17, but in contrast to those noted in the Minnesota Heart Survey in which there was little change in the age profile of patients hospitalized with an incident AMI between 1985 and 199512. The findings of our study, as well as the collective results of the NRMI studies, demonstrate that patients currently hospitalized with AMI are more likely to be older, women, and have various comorbidities present including hypertension, diabetes, and cerebrovascular disease.
The increasing age and prevalence of comorbidities in patients currently hospitalized with AMI present significant challenges to health care providers. Data from a number of community-based investigations have documented increased hospital complication rates, more prolonged hospital stays, and worse hospital survival for elderly as compared with middle-aged and younger patients presenting with AMI. Surprisingly, despite the fact that patients in our most recently hospitalized study years were older and sicker, our study suggests no increases in the risk of developing several major clinical complications as well as considerable improvements in hospital prognosis during the period under study. These improving trends likely reflect advances in coronary reperfusion techniques, development of more effective adjunctive cardiac therapies, and increased utilization of these treatment modalities across all age strata12,18,19.
Changes in Hospital Management Practices
Increases in the prescribing of a number of evidence-based cardiac therapies in greater Worcester residents hospitalized with AMI over time have taken place. Other population-based studies and coronary disease registries have noted similar increases in the use of effective cardiac therapies (e.g., aspirin, beta blockers, lipid lowering agents) as they have been introduced into practice guidelines, suggesting the more optimal management of patients hospitalized with AMI12,17–19. These encouraging trends need continued monitoring, however, as contemporary practice patterns further evolve as well as identification of the characteristics of patients less likely to be treated with these proven therapeutic strategies.
Hospital Death Rates
Despite differences in the years under study, demographic and clinical characteristics of the patient samples included, and availability and use of different cardiac therapies, studies carried out in hospitalized patients in Rochester13,20 and Minneapolis-St. Paul, Minnesota12 have shown improvements over time in hospital survival after AMI. In the NRMI studies, hospital CFR’s declined from 11.2% in 1990 to 9.4% in 199917. In the NHANES Epidemiologic Follow-up Study, declines in the age-adjusted 28 day CFR’s for AMI were observed between the early 1970’s and early 1990’s14. In the Minnesota Heart Survey, 28 day death rates after hospitalization for MI declined by more than one half in men and by more than one-third in women between 1985, 1990, and 199512.
Although a causal relationship cannot be established, the declines in hospital death rates observed in the current and prior studies have occurred in the setting of a marked increase in the hospital use of evidence-based cardiac therapies and percutaneous revascularization9,12,17. In a systematic review of the literature, as well as data from several national sources, a more than one-third reduction in AMI associated mortality has been estimated to have occurred between 1975 and 1995 with increases in the use of effective cardiac therapies accounting for the majority of the decline in mortality observed during this period21.
Despite favorable declines over time in hospital death rates, as well as in the major clinical complications associated with AMI, short-term associated mortality rates appear to have leveled off during the last several years of our study. Continued improvements and refinement in the appropriate use of evidence-based therapies may further help to improve the short-term survival of these patients. Increased study of existing and novel treatment strategies in increasingly prevalent and unique subsets of patients with AMI including the obese, diabetics, and the elderly may be necessary to achieve larger declines in AMI associated mortality.
Study strengths and limitations
The strengths of our study include the large community-based sample of patients with confirmed AMI from all central Massachusetts hospitals and the ability to examine 3 decade long trends in a variety of AMI associated clinical and demographic characteristics and hospital outcomes. The study was carried out in men and women of all ages from a well-defined metropolitan area with demographic characteristics similar to U.S. residents. However, this study has several limitations which must be kept in mind when interpreting our study results. Our study cohorts are comprised largely of Caucasians and thus may lack generalizablity to other race/ethnic groups. In addition, the present study only included patients hospitalized with AMI. The influence of possible changes over time in the magnitude of out-of-hospital deaths due to cardiac disease on the characteristics of patients hospitalized with AMI remains unknown. We were unable to collect data on changes in patient’s smoking status after hospital discharge which may have affected some of the long-term survival findings observed22. We were also unable to collect information on the role of biomarkers indicative of inflammation or changes in, and adherence to, the use of cardiac medications by patients on a long-term basis.
Conclusions
The results of this community-wide investigation demonstrate continuing changes in the contemporary demographic, clinical, and therapeutic landscape of patients hospitalized with an initial AMI. Improvements in the utilization of effective cardiac therapies have been accompanied by recent declines in AMI hospital incidence rates and short-term mortality as well as improvements in the hospital prognosis of patients developing major clinical complications of AMI. Recognition of the changing profile of patients hospitalized with AMI, and further studies exploring the optimal management of increasingly older patients with serious comorbidities, will contribute to further improvements in these and other important endpoints in patients with acute coronary disease.
Acknowledgments
We wish to express our appreciation to all persons involved in the review of data for this project during the years under study.
Sources of Funding: Grant support for this project was provided by the National Heart, Lung, and Blood Institute (RO1 HL35434).
Footnotes
Conflict of Interest Disclosures: There are no conflicts of interest to report by any of the authors.
References
- 1.American Heart Association. 2008 Heart Disease and Stroke Statistics Update. Dallas, Texas: American Heart Association; 2008. [Google Scholar]
- 2.National Institutes for Health, National Heart, Lung, and Blood Institute. Morbidity and Mortality: 2007 Chartbook on Cardiovascular, Lung, and Blood Disease. Available at http://www.nhlbi.nih.gov/resources/docs/07-chtbk.pdf.
- 3.Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Recent changes in the attack rates and survival rates of acute myocardial infarction (1975–1981): The Worcester Heart Attack Study. JAMA. 1986;255:2774–2779. [PubMed] [Google Scholar]
- 4.Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Incidence and case fatality rates of acute myocardial infarction (1975–1984): the Worcester Heart Attack Study. Am Heart J. 1988;115:761–767. doi: 10.1016/0002-8703(88)90876-9. [DOI] [PubMed] [Google Scholar]
- 5.Goldberg RJ, Yarzebski J, Lessard D, Gore JM. A two-decades (1975 to 1995) long experience in the incidence, in-hospital and long-term case-fatality rates of acute myocardial infarction: a community-wide perspective. J Am Coll Cardiol. 1999;33:1533–1539. doi: 10.1016/s0735-1097(99)00040-6. [DOI] [PubMed] [Google Scholar]
- 6.Goldberg RJ, Yarzebski J, Lessard D, Wu J, Gore JM. Recent trends in the incidence rates of and death rates from atrial fibrillation complicating initial acute myocardial infarction: A community-wide perspective. Am Heart J. 2002;143:519–527. doi: 10.1067/mhj.2002.120410. [DOI] [PubMed] [Google Scholar]
- 7.Spencer FA, Meyer TE, Goldberg RJ, Yarzebski J, Hatton M, Lessard D, Gore JM. Twenty year trends (1975–1995) in the incidence, in-hospital and long-term death rates associated with heart failure complicating acute myocardial infarction: a community-wide perspective. J Am Coll Cardiol. 1999;34:1378–1387. doi: 10.1016/s0735-1097(99)00390-3. [DOI] [PubMed] [Google Scholar]
- 8.Goldberg RJ, Samad NA, Yarzebski J, Gurwitz J, Bigelow C, Gore JM. Temporal trends in cardiogenic shock complicating acute myocardial infarction. N Engl J Med. 1999;340:1162–1168. doi: 10.1056/NEJM199904153401504. [DOI] [PubMed] [Google Scholar]
- 9.Spencer FA, Lessard D, Yarzebski J, Gore JM, Goldberg RJ. Decade long changes in the increasingly effective medical management of patients surviving hospitalization for acute myocardial infarction. Am Heart J. 2005;150:838–844. doi: 10.1016/j.ahj.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Brewslow NE, Day NE. The design and analysis of cohort studies. 2. Lyon, France: International Agency for Research on Cancer; 1987. Statistical Methods in Cancer Research; pp. 61–73. [Google Scholar]
- 11.Arnett DK, McGovern PG, Jacobs DR, Jr, Shahar E, Duval S, Blackburn H, Luepker RV. Fifteen-year trends in cardiovascular risk factors (1980–1982 through 1995–1997): the Minnesota Heart Survey. Am J Epidemiol. 2002;156:929–935. doi: 10.1093/aje/kwf133. [DOI] [PubMed] [Google Scholar]
- 12.McGovern PG, Jacobs DR, Jr, Shahar E, Arnett DK, Folsom AR, Blackburn H, Luepker RV. Trends in acute coronary heart disease mortality, morbidity and medical care from 1985 through 1997: the Minnesota Heart Survey. Circulation. 2001;104:19–24. doi: 10.1161/01.cir.104.1.19. [DOI] [PubMed] [Google Scholar]
- 13.Roger VL, Jacobsen SJ, Weston SA, Goraya TY, Killian J, Reeder GS, Kottke TE, Yawn BP, Frye RL. Trends in the incidence and survival of patients with hospitalized myocardial infarction. Olmsted County, Minnesota, 1979 to 1994. Ann Intern Med. 2002;136:341–348. doi: 10.7326/0003-4819-136-5-200203050-00005. [DOI] [PubMed] [Google Scholar]
- 14.Ergin A, Muntner P, Sherwin H, He J. Secular trends in cardiovascular disease mortality, incidence, and case fatality rates in adults in the United States. Am J Med. 2004;117:219–227. doi: 10.1016/j.amjmed.2004.03.017. [DOI] [PubMed] [Google Scholar]
- 15.Rosamond WD, Folsom AR, Chambless LE, Wang CH. Coronary heart disease trends in four United State communities. The Atherosclerosis Risk in Communities (ARIC) Study 1987–1996. Int J Epidemiol. 2001;30:S17–S22. doi: 10.1093/ije/30.suppl_1.s17. [DOI] [PubMed] [Google Scholar]
- 16.Goff DC, Jr, Brass L, Braun LT, Croft JB, Flesch JD, Fowkes FG, Hong Y, Howard V, Huston S, Jencks SF, Luepker R, Manolio T, O’Donnell C, Robertson RM, Rosamond W, Rumsfeld J, Sidney S, Zheng ZJ. American Heart Association Council on Epidemiology and Prevention; American Heart Association Council on Stroke; American Heart Association Council on Cardiovascular Nursing; American Heart Association Working Group on Quality of Care and Outcomes Research; American Heart Association Working Group on Atherosclerotic Peripheral Vascular Disease. Essential features of a surveillance system to support the prevention and management of heart disease and stroke. Circulation. 2007;115:127–155. doi: 10.1161/CIRCULATIONAHA.106.179904. [DOI] [PubMed] [Google Scholar]
- 17.Rogers WJ, Canto JG, Lambrew CT, Tiefenbrunn AJ, Kinkaid B, Shoultz DA, Frederick PD, Every N. Temporal trends in the treatment of over 1.5 million patients with myocardial infarction in the U.S. from 1990 through 1999. J Am Coll Cardiol. 2000;36:2056–2063. doi: 10.1016/s0735-1097(00)00996-7. [DOI] [PubMed] [Google Scholar]
- 18.Lucas FL, DeLorenzo MA, Siewers AE, Wennberg DE. Temporal trends in the utilization of diagnostic testing and treatments for cardiovascular disease in the United States, 1993–2001. Circulation. 2006;113:380–387. doi: 10.1161/CIRCULATIONAHA.105.560433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gerber Y, Rihal CS, Sundt TM, 3rd, Killian JM, Weston SA, Therneau TM, Roger VL. Coronary revascularization in the community. J Am Coll Cardiol. 2007;50:1223–1229. doi: 10.1016/j.jacc.2007.06.022. [DOI] [PubMed] [Google Scholar]
- 20.Gerber Y, Jacobsen SJ, Frye RL, Weston SA, Killian JM, Roger VL. Secular trends in deaths from cardiovascular diseases: A 25-year community study. Circulation. 2006;113:2285–2292. doi: 10.1161/CIRCULATIONAHA.105.590463. [DOI] [PubMed] [Google Scholar]
- 21.Heidenreich PA, McClellan M. Trends in treatment and outcomes for acute myocardial infarction: 1975–1995. Am J Med. 2001;110:165–174. doi: 10.1016/s0002-9343(00)00712-9. [DOI] [PubMed] [Google Scholar]
- 22.Critchley JA, Capewell S. Mortality risk reduction associated with smoking cessation in patients with coronary heart disease: a systematic review. JAMA. 2003;290:86–97. doi: 10.1001/jama.290.1.86. [DOI] [PubMed] [Google Scholar]