ABSTRACT
OBJECTIVE
To examine childhood immunization levels relative to the number of family physicians, pediatricians, and public health nurses in Ontario.
DESIGN
Retrospective comparative analysis of publicly available data on immunization coverage levels and the relative number of family physicians, pediatricians, and public health nurses.
SETTING
Ontario.
PARTICIPANTS
Seven-year-old children, family physicians, pediatricians, and public health nurses in Ontario.
MAIN OUTCOME MEASURES
The association between immunization coverage levels and the relative number of family physicians, pediatricians, and public health nurses.
RESULTS
We found correlations between immunization coverage levels and the relative number (ie, per 1000 Ontario residents) of family physicians (ρ = 0.60) and pediatricians (ρ = 0.70) and a lower correlation with the relative number of public health nurses (ρ = 0.40), although none of these correlations was significant. A comparison of temporal trends illustrated that variation in the relative number of family physicians and pediatricians in Ontario was associated with similar variation in immunization coverage levels.
CONCLUSION
Increasing the number of family physicians and pediatricians might help to boost access to immunizations and perhaps other components of cost-saving childhood preventive care.
RÉSUMÉ
OBJECTIF
Examiner les niveaux de vaccination des enfants par rapport au nombre de médecins de famille, de pédiatres et d’infirmières de santé publique en Ontario.
TYPE D’ÉTUDE
Analyse comparative rétrospective des données disponibles au public sur les niveaux de couverture vaccinale, et du nombre relatif de médecins de famille, de pédiatres et d’infirmières de santé publique.
CONTEXTE
Ontario.
PARTICIPANTS
Enfants âgés de 7 ans, médecins de famille, pédiatres et infirmières de santé publique de l’Ontario.
PRINCIPAUX PARAMÈTRES À L’ÉTUDE
Association entre les niveaux de couverture vaccinale et le nombre relatif de médecins de famille, de pédiatres et d’infirmières de santé publique.
RÉSULTATS
Des corrélations ont été observées entre les niveaux de couverture vaccinale et le nombre relatif (c.-à-d. par 1000 résidents de l’Ontario) de médecins de famille (ρ= 0.60), de pédiatres (ρ= 0.70) et, à un moindre degré, d’infirmières de santé publique (ρ= 0.40), quoique aucune de ces corrélations ne soit significative. Une comparaison des tendances temporelles a montré qu’une variation du nombre relatif de médecins de famille et de pédiatres en Ontario s’accompagne d’une variation semblable de la couverture vaccinale.
CONCLUSION
Une augmentation du nombre de médecins de famille et de pédiatres pourrait améliorer l’accès à la vaccination et peut-être à d’autres types de soins préventifs économiquement rentables orientés vers l’enfance.
There are current concerns regarding the number of family physicians in Canada and how persistent shortfalls might affect the level of health care. A collaborative survey conducted by the College of Family Physicians of Canada, the Canadian Medical Association, and the Royal College of Physicians and Surgeons of Canada1 revealed that in 2007 about 14% of Canadians did not have family physicians. Only 30.8% of physicians reported that they were taking new patients. With only about 17% of Ontario’s physicians serving patients in small towns or rural settings,1 the situation is likely even worse in rural areas of the province.2 The results from the 2007 survey suggest, therefore, that some Canadians might have trouble accessing preventive primary health care. This is a cause for concern given the importance of primary care for improving population health and controlling health care costs. The survey results can also be considered surprising given the importance Canadians place on their universal health care system as a societal value and as a cornerstone of national identity.
Similar concerns have been raised about the number of public health nurses (PHNs) in Ontario. A recent assessment by the Nursing Health Services Research Unit of McMaster University in Hamilton, Ont, and the University of Toronto in Ontario concluded that the total number of nurses employed in public health has been remarkably stable despite population growth and increased demand for services.3 The potential shortfall of PHNs in Ontario has implications not only for the province’s ability to respond to public health emergencies, such as pandemics, but also for essential preventive care services like childhood immunizations.
In response to these surveys, we examined childhood immunization levels relative to the number of family physicians, pediatricians, and PHNs in Ontario. Immunizations play an important role in reducing many causes of morbidity and mortality among children. As such, immunizations are an important component of pediatric primary care. Recent research has suggested that changes in immunization coverage levels can serve as a rough indicator, or sentinel event, for the level of early childhood preventive care.4,5
METHODS
We reviewed immunization coverage levels between 2000 and 2004 for 7-year-olds for the province of Ontario. These data were provided by the Ontario Ministry of Health and Long-Term Care. We focused on coverage levels for vaccines for the diphtheria and tetanus toxoids and acellular pertussis (DTaP) series; polio; and measles, mumps, and rubella (MMR). At the time of the study, survey results for 2005 to 2007 had not yet been generated by the Ontario Ministry of Health and Long-Term Care, and were thus not available. Data on the number of family physicians and pediatricians registered in Ontario were provided by the Ontario Physician Human Resources Data Centre. In Ontario, pediatricians provide primary preventive care, in addition to referral services. Data on the number of PHNs in Ontario between 1993 and 2006 were taken from a recent report provided by the Nursing Health Services Research Unit.3 We considered PHNs to be primary care providers for this study, given their role in providing childhood vaccinations. Population estimates for Ontario were obtained from Statistics Canada.6 We used nonparametric Spearman correlations to estimate the association between immunization levels and the number of family physicians per 1000 residents in the province of Ontario. Because we used publicly available data, we were not required by the University of Toronto to submit our research protocol for institutional ethics review.
RESULTS
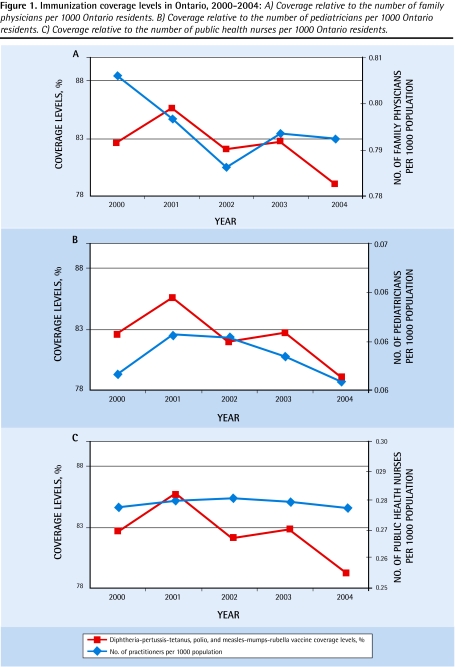
Table 1 summarizes the DTaP-polio-MMR vaccination coverage levels; population estimates; the number of family physicians, pediatricians, and PHNs; and the relative number of providers per 1000 residents, for Ontario for 2000 to 2004. A comparison of temporal trends in the relative number of primary care providers with immunization coverage levels among 7-yearold children suggests that increases and decreases in the relative number of family physicians (Figure 1A) and pediatricians (Figure 1B) in Ontario were generally associated with similar variation in immunization coverage levels. The temporal trend in the relative number of PHNs (Figure 1C), however, did not correspond to variation in immunization coverage levels. We found high, although nonsignificant, correlations between the number of family physicians (ρ = 0.60, P = .28) and pediatricians (ρ = 0.70, P = .19) per 1000 Ontario residents and coverage levels for the DTaP-polio-MMR vaccine combination between 2000 and 2004. A substantially lower correlation was found between immunization levels and the relative number of PHNs (ρ = 0.40, P = .50) during that same time period. The correlation between immunization coverage levels and the sum of the relative numbers of family physicians and pediatricians was also high (ρ = 0.60, P = .29). A post-hoc analysis revealed that small sample sizes (N = 5) resulted in low statistical power (range 10% to 27%) for correlation significance tests.
Table 1.
Ontario data from 2000 to 2004 on childhood complete-for-age immunization coverage levels for DTaP, polio, and MMR antigens; the number of family physicians, pediatricians, and PHNs; population estimates; and the relative number of family physicians, pediatricians, and PHNs per 1000 Ontario residents.
| VARIABLE |
YEAR |
||||
|---|---|---|---|---|---|
| 2000 | 2001 | 2002 | 2003 | 2004 | |
| Immunization coverage for 7-year-olds, % | 82.64 | 85.64 | 82.03 | 82.75 | 79.09 |
| No. of family physicians | 9418 | 9478 | 9515 | 9730 | 9842 |
| No. of pediatricians | 709 | 741 | 752 | 753 | 750 |
| No. of PHNs | 3242 | 3327 | 3396 | 3423 | 3443 |
| Population (in millions) | 11.685 | 11.897 | 12.102 | 12.262 | 12.420 |
| Relative no. of family physicians | 0.8060 | 0.7966 | 0.7862 | 0.7935 | 0.7924 |
| Relative no. of pediatricians | 0.0607 | 0.0623 | 0.0621 | 0.0614 | 0.0604 |
| Relative no. of PHNs | 0.2774 | 0.2796 | 0.2806 | 0.2791 | 0.2772 |
DTaP—diphtheria and tetanus toxoids and acellular pertussis, MMR—measles, mumps, and rubella, PHN—public health nurse.
Figure 1.
Immunization coverage levels in Ontario, 2000–2004: A) Coverage relative to the number of family physicians per 1000 Ontario residents. B) Coverage relative to the number of pediatricians per 1000 Ontario residents. C) Coverage relative to the number of public health nurses per 1000 Ontario residents.
DISCUSSION
Our study is the first to compare childhood immunization rates and the relative number of family physicians, pediatricians, or PHNs in Ontario or elsewhere in Canada. Our results indicate that fluctuations in immunization coverage levels are correlated with changes in the relative number of family physicians and pediatricians. Although the observed correlation does not indicate a causal relationship, our results suggest that the apparent shortfall of these primary care providers might have been a contributing factor affecting immunization coverage levels. Although immunizations are, for the most part, tied to well-child visits to family physicians or pediatricians, children without family physicians or pediatricians must seek immunizations elsewhere, such as local public health offices. Our results, however, indicate that the relative number of PHNs likely does not affect immunization levels.
Our study suggests that reductions in the relative number of family physicians and pediatricians might result in reduced access to some forms of pediatric primary care, such as immunizations. Research indicates residents of the United States are one-third less likely than Canadians to have regular doctors and that they are one-fourth more likely to have unmet health care needs.7–9 Unlike the situation in the United States, where insurance status influences accessibility to immunizations and childhood preventive care,5 the availability of primary care physicians might influence accessibility in Ontario.
Limitations
The results of our study are subject to certain limitations and potentially confounding factors. For example, there are other factors that could substantially affect immunization coverage levels, such as the perceived association between childhood vaccines and autism, a concern recently covered in the press.10 Also, it is important to recognize that the number of family physicians, pediatricians, and PHNs is not equivalent to the number of patients seen by those providers. In addition, the validity of our results is dependent on the accuracy of the population estimates and estimates of immunization coverage used in the study. Finally, because our study is ecological in nature, it cannot demonstrate causation, but rather the correlation among factors at the population level.
Conclusion
The results of our study indicate that there is a correlation between immunization coverage levels and the number of family physicians and pediatricians in Ontario. Our results suggest that increasing the number of family physicians and pediatricians in Ontario might boost access to immunizations. The need for more family physicians and pediatricians could be particularly acute among rural populations of Canada.2 As has been observed in the United States, diminished accessibility to immunizations and other components of preventive care might contribute to greater long-term health care spending. Our study suggests, therefore, that underimmunization of the population might reflect underservice. Increasing the number of family physicians and pediatricians could be essential to the long-term effectiveness and viability of Canada’s universal health care system. Further study of immunizations and the availability of primary care providers in Ontario should examine the consequences of physician shortfalls on immunization coverage levels in rural settings.
EDITOR’S KEY POINTS
Currently there are concerns about the number of family physicians in Canada and how persistent shortfalls might affect the level of health care. This study aimed to examine whether the relative number of primary care providers (including family physicians, pediatricians, and public health nurses) was related to childhood immunization levels.
The authors did identify correlations between immunization coverage levels and the numbers of family physicians, pediatricians, and to a lesser extent public health nurses. The correlations were not significant, owing to low test power as a result of the small sample size, but these results do suggest that the relative number of practitioners might affect levels of care.
POINTS DE REPÈRE DU RÉDACTEUR
On s’inquiète actuellement du nombre insuffisant de médecins de famille au Canada et des conséquences éventuelles de cette situation qui perdure sur la qualité des soins primaires. Cette étude voulait déterminer si on pouvait associer le nombre relatif de soignants de première ligne (incluant médecins de famille, pédiatres et, à un moindre degré, infirmières de santé publique) au niveau de vaccination des enfants.
Les auteurs ont observé des corrélations entre les niveaux de couverture vaccinale et le nombre de médecins de famille, de pédiatres et, à un moindre degré, d’infirmières de santé publique. Ces corrélations n’étaient pas significatives, à cause du faible niveau de puissance des tests résultant de la petite taille des échantillons, mais les résultats donnent néanmoins à croire que le nombre relatif de médecins pourrait affecter le niveau de soins.
Footnotes
*Full text is available in English at www.cfp.ca.
This article has been peer reviewed.
Contributors
Dr Schillaci and Ms Romain contributed to concept and design of the study; data gathering, analysis, and interpretation; and preparing the manuscript for submission.
Competing interests
None declared
References
- 1.College of Family Physicians of Canada, Canadian Medical Association, Royal College of Physicians and Surgeons of Canada 2007 National Physician Survey Mississauga, ON: College of Family Physicians of Canada; 2007. Available from: www.nationalphysiciansurvey.ca/nps/2007_Survey/2007nps-e.asp. Accessed 2009 Sep 11. [Google Scholar]
- 2.Rourke J. Increasing the number of rural physicians. CMAJ. 2008;178(3):322–5. doi: 10.1503/cmaj.070293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Underwood J, Alameddine M, Baumann A, Deber R, Laporte A, Dragan A. Fact sheet: nurses in public health in Ontario. Hamilton, ON: Nursing Health Services Research Unit, McMaster University; 2007. [Google Scholar]
- 4.Roohan PJ, Butch JM, Anarella JP, Gesten F, Shure K. Quality measurement in Medicaid managed care and fee-for-service, the New York State experience. Am J Med Qual. 2006;21(3):185–91. doi: 10.1177/1062860606287199. [DOI] [PubMed] [Google Scholar]
- 5.Schillaci MA, Waitzkin H, Carson EA, Lopez CM, Boehm DA, Lopez LA, et al. Immunization coverage and Medicaid managed care in New Mexico: a multi-method assessment. Ann Fam Med. 2004;2(1):13–21. doi: 10.1370/afm.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Statistics Canada Population by year, by province and territory Ottawa, ON: Statistics Canada; 2007. Available from: www.statcan.gc.ca/start-debuteng.html Accessed 2007 May 21. [Google Scholar]
- 7.Lasser E, Himmelstein DU, Wollhandler S.Access to care, health status, and health disparities in the United States and Canada: results of a cross-national population-based survey Am J Public Health 20069671300–7. Epub 2006 May 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Deber RB. Health care reform: lesson from Canada. Am J Public Health. 2003;93(1):20–4. doi: 10.2105/ajph.93.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guyatt GH, Devereaux PJ, Lexchin J, Stone SB, Yalnizyan A, Himmelstein D, et al. A systematic review of studies comparing health outcomes in Canada and the United States. Open Med. 2007;1(1):e27–36. [PMC free article] [PubMed] [Google Scholar]
- 10.Lett D. Vaccine-autism link discounted, but effect of “study” is unknown. CMAJ. 2007;177(8):841. doi: 10.1503/cmaj.071199. [DOI] [PMC free article] [PubMed] [Google Scholar]