ABSTRACT
OBJECTIVE
To describe the occurrence of mental health problems and cognitive impairment in a group of elderly homeless men and to demonstrate how clinical examination and screening tests used in a shelter setting might be helpful in identifying mental illness and cognitive impairment.
DESIGN
Cross-sectional study including face-to-face interviews and review of medical records.
SETTING
A community-based homeless shelter in an urban metropolitan centre (Toronto, Ont).
PARTICIPANTS
A total of 49 male participants 55 years of age or older. The average duration of homelessness was 8.8 (SD 10.2) years.
METHODS
Participants were admitted to a community-based shelter that offered access to regular meals, personal support and housing workers, nursing, and a primary care physician. Medical chart review was undertaken to identify mental illness or cognitive impairment diagnosed either before or after admission to the facility. The 15-item Geriatric Depression Scale (GDS-15) and the Folstein Mini-Mental State Examination (MMSE) were administered.
MAIN OUTCOME MEASURE
Previous or new diagnosis of mental illness or cognitive impairment.
RESULTS
Thirty-six of the participants (73.5%) had previous or new diagnoses. The most prevalent diagnosis was schizophrenia or psychotic disorders (n = 17), followed by depression (n = 11), anxiety disorders (n = 3), cognitive impairment (n = 8), and bipolar affective disorder (n = 1). A total of 37% of participants were given new mental health diagnoses during the study. The GDS-15 identified 9 people with depression and the MMSE uncovered 11 individuals with cognitive impairment who had not been previously diagnosed.
CONCLUSION
This study suggests that providing access to primary care physicians and other services in a community-based shelter program can assist in identification of mental illness and cognitive impairment in elderly homeless men. Use of brief screening tools for depression and cognitive impairment (like the GDS-15 and the MMSE) could be helpful in this highrisk group.
RÉSUMÉ
OBJECTIF
Établir l’incidence des problèmes de santé mentale et des déficits cognitifs chez un groupe d’hommes sans abri âgés et montrer comment l’examen clinique et certains tests de dépistage peuvent favoriser l’identification de ces problèmes.
TYPE D’ÉTUDE
Étude transversale incluant des entrevues individuelles et une revue de dossiers médicaux.
CONTEXTE
Un refuge communautaire pour sans abri de la région métropolitaine de Toronto, Ontario.
PARTICIPANTS
Un total de 49 sujets mâles d’au moins 55 ans qui étaient sans abri depuis en moyenne 8,8 ans (DS 10,2 ans).
MÉTHODES
Les participants ont été admis à un refuge communautaire qui offrait des repas quotidiens et l’accès à un support individuel, à des travailleurs du logement, à des infirmières et à un médecin de première ligne. Les dossiers médicaux ont été consultés pour déterminer les maladies mentales ou les troubles cognitifs diagnostiqués avant ou après l’admission au refuge. L’échelle gériatrique de dépression à 15 items (ÉGD-15) et le test de Folstein (MMSE) ont été administrés aux participants.
PRINCIPAL PARAMÈTRE À L’ÉTUDE
Diagnostics de maladie mentale ou de trouble cognitif antérieur ou nouveau.
RÉSULTATS
Des diagnostics antérieurs ou nouveaux ont été trouvés chez 36 participants (73,5 %). La schizophrénie ou les troubles psychotiques étaient les diagnostics les plus fréquents (n = 17), suivis des dépressions (n = 11), des troubles anxieux (n = 3), des déficits cognitifs (n = 8) et des maladies bipolaires (n = 1). Au total, 37 % des participants ont reçu un nouveau diagnostic de maladie mentale durant l’étude. L’ÉGD-15 a identifié 9 cas de dépression et le MMSE, 11 cas de troubles cognitifs qui n’avaient pas été diagnostiqués auparavant.
CONCLUSION
Cette étude suggère que l’accès à un médecin de première ligne et à d’autres services via un refuge au sein de la communauté peut faciliter la détection de maladies mentales et de troubles cognitifs chez des sans abri mâles âgés. L’utilisation d’outils simples pour dépister la dépression et les troubles cognitifs (comme l’ÉGD-15 et le MMSE) pourrait être avantageuse dans ce groupe à haut risque.
In Canada’s large metropolitan cities, homelessness is an increasing concern, with approximately 5 out of every 10 000 people sleeping in shelters.1,2 Available estimates suggest that the number of homeless people is growing rapidly. For example, in the past decade the population of homeless individuals on any given night has nearly doubled in Toronto, Ont.3 While most homeless people tend to be young, single men, there is an increasing recognition of the demographic diversity of these individuals, which includes children, families, and the elderly.1,2,4–6
Homelessness is an important determinant of health status and has been shown to be associated with increased risk of a range of physical and mental health problems compared with the general population.4,6–10 Homeless individuals develop chronic health problems many years earlier than their housed counterparts, and the mortality rate among homeless men in Toronto is twice that of the general population.5,6 Increasingly, mental health disorders are being recognized as important health-related risk factors for and outcomes of homelessness. 11 Estimates of the prevalence of mental illness consistently show that approximately half of all homeless individuals have had mental illnesses at some time in their lives. Alcohol use disorders are widespread, affecting 60% of homeless men, followed by affective disorders (20% to 40%), schizophrenia (6% to 14%), and dementia (3%).4,8,12 Whether compromised mental health is a precipitant of homelessness or an end result of daily stress and isolation, its effects are often long-standing and result in moderate to severe disability.5,13
Access to health care has been shown to protect against the negative health effects of homelessness and poverty.5,14–17 Even in Canada, however, access to primary health care is often suboptimal. Although homeless individuals use health services frequently, it is often in the form of emergency department visits, hospitalizations, or brief contacts with health buses.9,18,19 Some studies reported that as few as half of respondents had access to primary care.11,20 Potential reasons for poor access to health care include physicians’ refusal to provide care to those with lost health insurance cards and patients’ difficulties keeping appointments, limited financial or psychological resources, and competing priorities in daily life.9,21,22 These barriers are often accentuated in those with mental illness, making them among the most vulnerable of the homeless.
Despite the recognition of the demographic diversity of homelessness in Canada, little is known about the health status of elderly homeless individuals in large metropolitan areas. Available research on mental illness in the homeless has been conducted outside of Canada and has focused on a relatively young cohort.8,11,23–27 This study aimed to describe the occurrence of mental health problems and cognitive impairment in a group of elderly homeless men living in a community-based shelter in a Canadian urban metropolitan centre. It also aimed to investigate the effect of providing access to regular primary health care, including the use of screening tests to facilitate identification of mental health disorders and cognitive impairment.
METHODS
The study was conducted in a community-based shelter in Toronto, Ont. The shelter was a satellite of a larger shelter, designed to meet the needs of the increasingly diverse homeless population. Staff at the larger shelter or other shelters in the city would contact intake staff at the community-based shelter for those clients they thought would be appropriate for admission. All clients considered for admission were men aged 55 and older who agreed to live in a community setting and who had no active “severe” behavioural or substance abuse problems. Severity of behavioural problems or substance abuse was assessed by the intake worker and the hostel manager on a case-by-case basis; this was intended to minimize disruption of the surrounding community and the other residents in the hostel. Interested clients would be interviewed by an intake worker and receive a tour of the hostel before admission.
Basic health care services at the shelter were provided by a full-time registered practical nurse and a family physician who provided service 1 full day per week. The nurse had regular contact with most of the shelter clients and was responsible for administering medications and monitoring medical conditions (eg, diabetes, blood pressure, vital signs in acute illnesses). All residents were encouraged, but not required, to see the family physician for a complete history and physical examination and for ongoing care. Appointments were encouraged but not necessary for contact with the physician. The family physician would regularly reach out to clients who did not attend appointments in order to develop rapport and encourage them to obtain medical follow-up. This outreach included socializing or conducting interviews or assessments with clients in the hallway, cafeteria, or their bedrooms. The primary care physician had timely access to a staff psychiatrist who attended the larger hostel 1 or 2 days per week and conducted consultations when requested.
A cross-sectional study design was used and consisted of reviewing medical records and conducting face-to-face interviews between September 2002 and August 2004. A research assistant approached clients of the hostel, described the study, and received informed consent for participation. The study received ethics approval from the St Michael’s Hospital Research Ethics Board in Toronto.
The 15-item Geriatric Depression Scale (GDS-15) and the Folstein Mini-Mental State Examination (MMSE) were administered to consenting participants by a single interviewer.28–31 The purpose was to obtain complementary information on the prevalence of depression and cognitive impairment in this population using brief, valid measures that could easily be applied in a primary care setting. The GDS-15 is a measure of depression that takes 5 to 7 minutes to complete; it can be completed by patients themselves or administered by a health care provider. The GDS-15 has been validated as a screening measure for depression in primary care and psychiatric settings, with reported sensitivity between 79% and 100% and specificity between 67% and 82%.32,33 It is valid for elderly patients, including those who have concurrent cognitive impairment.33,34
Patients’ medical records were reviewed to obtain information on diagnoses made before admission and within 6 months of admission to the hostel. The medical records held by the hostel medical and nursing staff were reviewed in detail. On admission to the hostel, all clients who were seen by the medical doctor were encouraged to provide consent for obtaining medical records from previous physicians in the community, hostels, and hospitals and from other health care providers that they had previously been in contact with. All investigations, past medical records, medication prescriptions, and consultant reports were reviewed. Thus, the definition of a diagnosis of a mental health problem or cognitive impairment used for the purpose of this study was based on the clinical judgment of the treating physicians. Participants were determined to have previous diagnoses of mental illness if the diagnoses were listed in their past medical histories, on the cumulative patient profile with a date earlier than their date of admission to the shelter, or in their medical records or consultant reports as being identified before their admission to the shelter. Participants were determined to have new diagnoses of mental illness if diagnoses were listed in their medical records at the time of or within the first 6 months of their admission or diagnoses were listed on their cumulative patient profiles with dates on or after their first visit with the physician, and they had no record of a mental health diagnosis or prescription for a psychotropic medication (ie, an antidepressant, antipsychotic, or mood-stabilizing drug that was not prescribed for a clear indication other than a mental illness) in the previous medical records or consultant reports. Careful review of available records was conducted to ensure that any recording of a new mental health diagnosis was based on the current assessments and not simply on review of old records. A period of 6 months after admission was chosen as the time point for chart review to allow for the client to be assessed by the hostel physician, to capture diagnoses that were likely present at the time of admission but not yet identified or diagnosed, and to minimize detection of new conditions that might have developed since being admitted to the hostel.
Most charts had insufficient information to determine a detailed history of alcohol use or to determine if clients met strict criteria for diagnosis of alcohol abuse or dependence. A client was said to abuse alcohol if alcohol abuse, alcohol dependence, or alcoholic was listed as a diagnosis in the medical record or if consumption of more than 2 alcoholic beverages per day or more than 14 alcoholic beverages per week was recorded in the medical record.
Secondary calculations of rates of mental illness are reported, which add findings of the GDS-15 and MMSE to the findings of the medical record review. A score on the MMSE of 22 or less was classified as dementia; a score of 23 to 27 was considered indicative of mild cognitive impairment.35 A score on the GDS-15 between 5 and 9 was classified as mild depression and a score of 10 or more was classified as severe depression.28,29
Analyses
Demographic variables and mental health diagnoses are reported as absolute numbers and proportions of the entire group (N = 49) or as means and standard deviations. Proportions of those with a diagnosis identified by the GDS-15 and MMSE are reported as proportions of those who were tested. To determine if there was a difference between those who participated in the interviews and those who did not, we compared mean age and years of homelessness using the Student t test. Results were considered significant at P < .05.
RESULTS
Demographic characteristics
A total of 49 participants’ charts were reviewed. The participants ranged in age from 55 to 89 years, with a mean of 66.4 (SD 8.6) years. The average number of years of homelessness was 8.8 (SD 10.2). Forty-six participants were white and 3 were black.
The refusal rate for participation in the interview portion of the study was 40.8%, with a total of 29 individuals completing both the GDS-15 and the MMSE. There was no significant difference in the mean age or years of homelessness between those who completed the interviews and those who did not (P > .05).
Alcohol and substance abuse
A history of alcohol use was documented in 42 of the medical records reviewed. Fourteen participants (33.3%) were current alcohol abusers and 9 (21.4%) had previously abused alcohol. Because of the difficulties in establishing firm criteria for alcohol abuse or dependence, figures on alcohol abuse are not included in the calculations for mental illness.
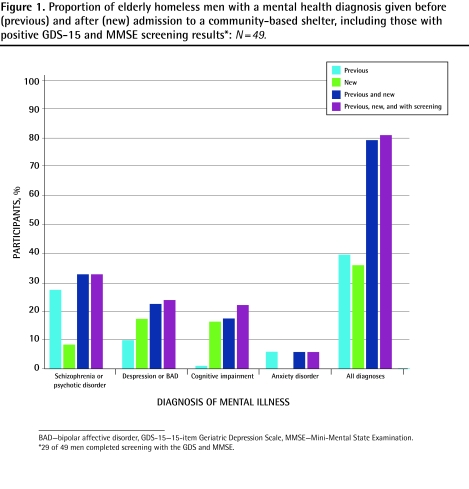
Previous and new clinical diagnosis of mental illness
The previous and new diagnoses of mental illness (excluding alcohol abuse) are summarized in Figure 1. Twenty-one men (42.9%) had previous diagnoses of mental illness. The most prevalent diagnosis was schizophrenia (n = 14), followed by depression (n = 3), anxiety disorders (n = 3), dementia (n = 1), and bipolar affective disorder (n = 1). Six months after admission, 18 participants (36.7%) had received new diagnoses of mental illness. Depression was the most common new diagnosis (n = 8, 16.3%), followed by cognitive impairment (n = 7, 14.3%) and psychotic disorders that were not otherwise specified (n = 3, 6.1%). Three participants who were given new mental health diagnoses had other previously diagnosed mental illnesses. Of these, 2 had previous diagnoses of schizophrenia; 1 was given a new clinical diagnosis of depression and the other was given a new diagnosis of dementia. One individual with a previously diagnosed anxiety disorder was given a new diagnosis of depression. Thus, the total number of participants with any previous or new diagnosis was 36 (73.5%).
Figure 1.
Proportion of elderly homeless men with a mental health diagnosis given before (previous) and after (new) admission to a community-based shelter, including those with positive GDS-15 and MMSE screening results*: N=49.
Depression as measured by the GDS-15
The GDS-15 was administered to a total of 29 participants, with a mean score of 4.39 (SD 3.4). As seen in Table 1, 9 men (31.0%) had scores indicating depression. Of these, 6 participants (20.7%) had scores suggesting mild depression and 3 (10.3%) had scores suggesting severe depression. Most participants with a GDS-15 score indicating depression had previous (n = 3) or new (n = 5) clinical diagnoses of depression.
Table 1.
Scores on the GDS-15 and MMSE in 29 elderly homeless participants
| SCREENING TEST | N | PROPORTION OF TESTED PARTICIPANTS (N = 29) | PROPORTION OF TOTAL PARTICIPANTS (N = 49) |
|---|---|---|---|
| GDS-15 (score) | |||
| • Mild depression (5–9) | 6 | 20.7 | 12.2 |
| • Severe depression (≥ 10) | 3 | 10.3 | 6.1 |
| • All depression (≥ 5) | 9 | 31.0 | 18.4 |
| MMSE (score) | |||
| • Mild impairment (23–27) | 6 | 20.7 | 12.2 |
| • Dementia (≤ 22) | 5 | 17.2 | 10.2 |
| • All cognitive impairment | 11 | 37.9 | 22.4 |
GDS-15—15-item Geriatric Depression Scale, MMSE—Mini-Mental State Examination.
Cognitive impairment
Only 1 participant had a diagnosis of dementia before admission to the shelter. Within 6 months of admission, another 7 participants (14.3%) had been diagnosed with cognitive impairment or dementia.
The MMSE was administered to 29 residents, with a mean score of 27.1 (SD 2.6). As shown in Table 1, the MMSE identified 11 individuals (37.9%) with cognitive impairment: 6 (20.7%) had mild cognitive impairment and 5 (17.2%) had dementia. Of the 6 participants who had been clinically diagnosed with dementia and who completed the MMSE, 4 received scores indicating dementia and 2 received scores indicating mild cognitive impairment. The MMSE identified 4 participants with mild cognitive impairment and 1 with dementia among those who had not previously been given a clinical diagnosis of cognitive impairment.
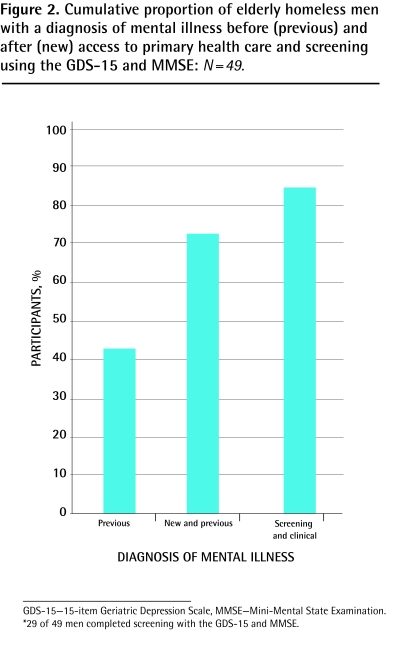
Overall frequency of mental illness
To give an estimate of the overall frequency of mental illness among the participants, we combined previous and new clinical diagnoses of mental illness with diagnoses detected on the MMSE and GDS-15, controlling for those individuals who received more than 1 diagnosis. As can be seen in Figure 2, an additional 5 participants with mental illnesses that had not previously been diagnosed were identified using the GDS-15 (n = 1) and MMSE (n = 4). In total, 41 participants (83.7%) met the study criteria for mental illness or cognitive impairment.
Figure 2.
Cumulative proportion of elderly homeless men with a diagnosis of mental illness before (previous) and after (new) access to primary health care and screening using the GDS-15 and MMSE: N=49.
DISCUSSION
This survey found that major mental health disorders and cognitive impairment were very common in this sample of elderly homeless men. The findings mirror previous studies conducted outside of Canada on mostly nonelderly populations, demonstrating that just under half of all participants had previous diagnoses of mental illness or dementia. The most common diagnoses before admission included psychotic disorders (29%), affective disorders (14%), and dementia (2%), but only accounted for about half of the total number of participants found to have mental illnesses. There are similarities between this sample and other reports on the general population of homeless individuals in terms of the high frequency of current (28%) or past (18%) alcohol abuse in this study. These findings suggest that elderly men in Canada are extremely vulnerable to the adverse health effects of homelessness and are at considerable risk of morbidity.
Perhaps the most striking finding of this study is the large proportion of participants who had mental illnesses that were unrecognized or that had not been treated in the past. Despite the high baseline rate of mental illness, 37% of participants had previously undiagnosed mental illnesses. Providing access to regular primary health care was effective in that it was associated with the identification of 8 men (16%) with depression and 7 (14%) with dementia. This finding suggests that the use of simple screening measures for depression and cognitive impairment can be effective in uncovering previously unrecognized mental health disorders in a homeless population. In particular, use of the MMSE showed that more than one-third of those tested had mild or moderate cognitive impairment. This study demonstrates that the use of screening and facilitation of access to primary care can benefit this vulnerable population.
This study adds to recent research demonstrating benefits of removing barriers and providing access to primary mental health care in the community.26,27,36 Although this study assesses the effects of improving access to primary health care as the primary intervention, the shelter actually has several components in common with outreach programs that have been proven to be effective. These components include stable shelter, assistance with achieving stable housing, case management, and outreach by social workers, nurses, and shelter employees. It is likely that all of these components function together to facilitate access to primary care and to achieve benefits in health status.
Limitations
There are several limitations to this study. The diagnosis of a new or previous mental illness was obtained through a review of medical records, which is less desirable than the use of objective interview techniques by a mental health professional. The medical care of homeless individuals is often not linear, and as such it is very possible that an individual could have received care or treatment for a condition that was not listed on the medical records. This might have overestimated the number of conditions determined to be undiagnosed. It is also important to note, however, that it was the usual practice of the shelter’s medical staff to make all attempts to request medical information from as many sources as possible.
Another limitation is that neither the use of screening measures (ie, GDS-15, MMSE) nor the clinical impression of a family physician is the criterion standard for diagnosing mental illness. It is also important to note that the group studied might not be representative of typical homeless men, as the individuals referred to the hostel would have had to be stable enough to have made initial contact with the hostel system. Furthermore, those individuals with substantial behavioural and substance abuse problems were not admitted. With these factors in mind, the true extent of mental illness is probably underestimated in our study relative to the larger population of homeless men. Finally, this study was conducted in Canada, where universal health insurance is provided, and participants could therefore differ substantially from other countries in terms of their current health status and access to previous health care.14,15 The comparison of the rates of mental illness between our study and others, however, suggests more similarities than differences between this group and the general population of homeless individuals.4
Conclusion
This study suggests that providing access to primary care physicians and other services in a community-based shelter program can assist in identification of mental illness and cognitive impairment in elderly homeless men. The use of brief screening tools for depression and cognitive impairment (like the GDS-15 and the MMSE) could be helpful in this high-risk group.
Acknowledgment
The study was funded in part by a grant from the College of Family Physicians of Canada’s Research and Education Foundation.
EDITOR ’S KEY POINTS
Despite the recognition of the demographic diversity of homelessness in Canada, little is known about the health status of elderly homeless individuals in large metropolitan areas.
This study’s findings indicated that major mental health disorders and cognitive impairment were very common in this sample of elderly homeless men; 83.7% of participants met the study criteria for diagnoses of mental illness or cognitive impairment. A large proportion of participants had mental illnesses that were previously unrecognized or that had not been treated in the past.
This study demonstrates that the use of screening tools and facilitation of access to primary care can benefit this vulnerable population.
POINTS DE REPÈRE DU RÉDACTEUR
Même si la diversité démographique des sans abri du Canada est bien connue, on sait peu de chose sur l’état de santé des sans abri âgés des grandes régions métropolitaines.
Les observations de cette étude indiquent que les problèmes de maladie mentale et les déficits cognitifs majeurs sont fréquents chez les sans abri mâles âgés; 83,7 % des participants répondaient aux critères de l’étude pour un diagnostic de maladie mentale ou de déficit cognitif. Une importante proportion des participants présentaient une maladie mentale qui n’avait pas été découverte ni traitée auparavant.
L’étude démontre qu’en utilisant des outils de dépistage et en favorisant l’accès à des soins primaires, on peut rendre service à ce groupe vulnérable.
Footnotes
*Full text is available in English at www.cfp.ca.
This article has been peer reviewed.
Contributors
Both authors were responsible for designing all aspects of the study, as well as for collection and analysis of the data. The first draft of the manuscript was written by Dr Limbos; Dr Joyce reviewed and revised the manuscript. Both authors approved the final manuscript submitted for publication.
Competing interests
None declared
References
- 1.Hwang SW. Homelessness and health. CMAJ. 2001;164(2):229–33. [PMC free article] [PubMed] [Google Scholar]
- 2.Statistics Canada 2001 Census analysis series: collective dwellings Ottawa, ON: Statistics Canada; 2002. Available from: www12.statcan.ca/English/census01/Products/Analytic/companion/coll/pdf/96F0030X1E2001004/pdf Accessed 2007 Oct 15. [Google Scholar]
- 3.Golden A, Currie WH, Greaves E, Latimer EJ.Taking responsibility for homelessness: an action plan for Toronto. Report of the Mayor’s Homelessness Action Task Force Toronto, ON: City of Toronto; 1999. Available from: www.city.toronto.on.ca/mayor/homelessness.htm. Accessed 2007 Oct 15. [Google Scholar]
- 4.Fischer PJ, Breakey WR. The epidemiology of alcohol, drug and mental disorders among homeless persons. Am Psychol. 1991;46(11):1115–28. doi: 10.1037//0003-066x.46.11.1115. [DOI] [PubMed] [Google Scholar]
- 5.Hwang SW. Mortality among men using homeless shelters in Toronto, Ontario. JAMA. 2000;283(16):2152–7. doi: 10.1001/jama.283.16.2152. [DOI] [PubMed] [Google Scholar]
- 6.Gelberg L, Linn LS, Mayer-Oakes SA. Differences in health status between older and younger homeless adults. J Am Geriatr Soc. 1990;38(11):1220–9. doi: 10.1111/j.1532-5415.1990.tb01503.x. [DOI] [PubMed] [Google Scholar]
- 7.Ferenchick GS. Medical problems of homeless and nonhomeless persons attending an inner-city health clinic. Am J Med Sci. 1991;301(6):379–82. doi: 10.1097/00000441-199106000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Acorn S. Mental and physical health of homeless persons who use emergency shelters in Vancouver. Hosp Community Psychiatry. 1993;44(9):854–7. doi: 10.1176/ps.44.9.854. [DOI] [PubMed] [Google Scholar]
- 9.Wood D. Delivering health care to homeless persons. The diagnosis and management of medical and mental health conditions. New York, NY: Springer Publishing; 1992. [Google Scholar]
- 10.Crowe C, Hardill K. Nursing research and political change: the street health report. Can Nurse. 1993;89(1):21–4. [PubMed] [Google Scholar]
- 11.Wojtusik L, White MC. Health status, needs, and health care barriers among the homeless. J Health Care Poor Underserved. 1998;9(2):140–52. doi: 10.1353/hpu.2010.0379. [DOI] [PubMed] [Google Scholar]
- 12.Mental Health Policy Research Group . Mental illness and pathways into homelessness: proceedings and recommendations. Toronto, ON: Canadian Mental Health Association; 1998. [Google Scholar]
- 13.Wright JD, Weber E. Homelessness and health. New York, NY: McGraw-Hill; 1987. [Google Scholar]
- 14.Stark LR. Barriers to health care for homeless people. In: Jahiel RI, editor. Homelessness: a prevention-oriented approach. Baltimore, MD: Johns Hopkins University Press; 1992. [Google Scholar]
- 15.Katz SJ, Hofer TP, Manning WG. Physician use in Ontario and the United States: the impact of socioeconomic status and health status. Am J Public Health. 1996;86(4):520–4. doi: 10.2105/ajph.86.4.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gorey KM, Holowary EJ, Fehringer G, Laukkanen E, Moskowitz A, Webster DJ, et al. An international comparison of cancer survival: Toronto, Ontario, and Detroit, Michigan, metropolitan areas. Am J Public Health. 1997;87(7):1156–63. doi: 10.2105/ajph.87.7.1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kessler RC, Frank RG, Edlund M, Katz SJ, Lin E, Leaf PJ. Differences in the use of psychiatric services between the United States and Ontario. N Engl J Med. 1997;336(8):551–7. doi: 10.1056/NEJM199702203360806. [DOI] [PubMed] [Google Scholar]
- 18.Padgett DK, Struening EL, Andrews H, Pittman J. Predictors of emergency room use by homeless adults in New York City: the influence of predisposing, enabling and need factors. Soc Sci Med. 1995;41(4):547–56. doi: 10.1016/0277-9536(94)00364-y. [DOI] [PubMed] [Google Scholar]
- 19.Padgett D, Struening EL, Andrews H. Factors affecting the use of medical, mental health, alcohol, and drug treatment services by homeless adults. Med Care. 1990;28(9):805–21. doi: 10.1097/00005650-199009000-00010. [DOI] [PubMed] [Google Scholar]
- 20.Ball FL, Havassy BE. A survey of the problems and needs of homeless consumers of acute psychiatric services. Hosp Community Psychiatry. 1984;35(9):917–21. doi: 10.1176/ps.35.9.917. [DOI] [PubMed] [Google Scholar]
- 21.Hwang SW, Windrim PM, Svoboda TJ, Sullivan WF. Physician payment for the care of homeless people. CMAJ. 2000;163(2):170–1. [PMC free article] [PubMed] [Google Scholar]
- 22.Gelberg L, Gallagher TC, Andersen RM, Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am J Public Health. 1997;87(2):217–20. doi: 10.2105/ajph.87.2.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adams CE, Pantelis C, Duke PJ, Barnes TR. Psychopathology, social and cognitive functioning in a hostel for homeless women. Br J Psychiatry. 1996;168(1):82–6. doi: 10.1192/bjp.168.1.82. [DOI] [PubMed] [Google Scholar]
- 24.Fichter MM, Quadflieg N. Prevalence of mental illness in homeless men in Munich, Germany: results from a representative sample. Acta Psychiatr Scand. 2001;103(2):94–104. doi: 10.1034/j.1600-0447.2001.00217.x. [DOI] [PubMed] [Google Scholar]
- 25.Teesson M, Hodder T, Buhrich N. Psychiatric disorders in homeless men and women in inner Sydney. Aust N Z J Psychiatry. 2004;38(3):162–8. doi: 10.1080/j.1440-1614.2004.01322.x. [DOI] [PubMed] [Google Scholar]
- 26.Lehman AF, Dixon LB, Kernan E, DeForge BR, Postrado LT. A randomized trial of assertive community treatment for homeless persons with severe mental illness. Arch Gen Psychiatry. 1997;54(11):1038–43. doi: 10.1001/archpsyc.1997.01830230076011. [DOI] [PubMed] [Google Scholar]
- 27.Wasylenki DA, Goering PN, Lemire D, Lindsey S, Lancee W. The hostel outreach program: assertive case management for homeless mentally ill persons. Hosp Community Psychiatry. 1993;44(9):848–53. doi: 10.1176/ps.44.9.848. [DOI] [PubMed] [Google Scholar]
- 28.Shah A, Herbert R, Lewis S, Mahendran R, Platt J, Bhattacharyya B. Screening for depression among acutely ill geriatric inpatients with a short Geriatric Depression Scale. Age Ageing. 1997;26(3):217–21. doi: 10.1093/ageing/26.3.217. [DOI] [PubMed] [Google Scholar]
- 29.D’Ath P, Katona P, Mullan E, Evans S, Katona C. Screening, detection and management of depression in elderly primary care attenders. I: the acceptability and performance of the 15 item Geriatric Depression Scale (GDS15) and the development of short versions. Fam Pract. 1994;11(3):260–6. doi: 10.1093/fampra/11.3.260. [DOI] [PubMed] [Google Scholar]
- 30.Crum RM, Anthony JC, Bassett SS, Folstein MF. Population-based norms for the Mini-Mental State Examination by age and educational level. JAMA. 1993;269(18):2386–91. [PubMed] [Google Scholar]
- 31.Anthony JC, LeResche L, Niaz U, von Korff MR, Folstein MF. Limits of the “Mini-Mental State” as a screening test for dementia and delirium among hospital patients. Psychol Med. 1982;12(2):397–408. doi: 10.1017/s0033291700046730. [DOI] [PubMed] [Google Scholar]
- 32.Watson LC, Pignone MP. Screening accuracy for late-life depression in primary care: a systematic review. J Fam Pract. 2003;52(12):956–64. [PubMed] [Google Scholar]
- 33.Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982–1983;17(1):37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 34.Katz IR. Diagnosis and treatment of depression in patients with Alzheimer’s disease and other dementias. J Clin Psychiatry. 1998;59(Suppl 9):38–44. [PubMed] [Google Scholar]
- 35.Zaudig M. A new systematic method of measurement and diagnosis of “mild cognitive impairment” and dementia according to ICD-10 and DSM-III-R criteria. Int Psychogeriatr. 1992;4(2):203–19. doi: 10.1017/s1041610292001273. [DOI] [PubMed] [Google Scholar]
- 36.Goering P, Wasylenki D, Lindsay S, Lemire D, Rhodes A. Process and outcome in a hostel outreach program for homeless clients with severe mental illness. Am J Orthopsychiatry. 1997;67(4):607–17. doi: 10.1037/h0080258. [DOI] [PubMed] [Google Scholar]