Abstract
The limited efficacy of cytotoxic therapy for advanced biliary tract and gallbladder cancers emphasizes the need for novel and more effective medical treatment options. A better understanding of the specific biological features of these neoplasms led to the development of new targeted therapies, which take the abundant expression of several growth factors and cognate tyrosine kinase receptors into account. This review will briefly summarize the status and future perspectives of antiangiogenic and growth factor receptor-based pharmacological approaches for the treatment of biliary tract and gallbladder cancers. In view of multiple novel targeted approaches, the rationale for innovative therapies, such as combinations of growth factor (receptor)-targeting agents with cytotoxic drugs or with other novel anticancer drugs will be highlighted.
Keywords: Growth factor receptor, Biliary tract cancer, Small molecule inhibitor, Monoclonal antibody, Innovative cancer treatment, Sorafenib, Bevacizumab, Erlotinib
INTRODUCTION
Biliary tract cancers (BTC) originate from the intra- or extrahepatic bile duct epithelium[1]. They were first described by Durand-Fardel in 1840[2,3]. The extrahepatic type (cholangiocarcinoma), primarily cancers involving the confluence of the right and left hepatic ducts, accounts for 80%-90%, and the intrahepatic type (cholangiocellular carcinoma) for the remaining 10%-20% of all biliary tract cancers. Hilar BTC as a specific sub-entity was first reported by Klatskin in 1965, hence their designation as Klatskin tumors[4]. BTC have been considered rare malignancies comprising only 3% of gastrointestinal tumors. However, interest in BTC is growing due to a rising worldwide incidence and associated mortality especially in intrahepatic BTC[5-8].
BTC is notoriously difficult to diagnose and is usually fatal because of its late clinical presentation and the lack of effective non-surgical treatment modalities[9]. Surgical resection or liver transplantation remain the only potentially curative therapeutic options. Unfortunately, most patients have unresectable disease at presentation and die within 12 mo. Liver failure and recurrent sepsis, secondary to biliary obstruction, also contribute to the high mortality[10]. Overall survival rate is poor, with less than 5% of BTC patients surviving to 5 years, a rate which has not changed significantly over the past 30 years[11]. Similar to BTC, there is currently no standard chemotherapy regimen for patients with advanced gallbladder cancer.
Therefore, innovative drugs are urgently needed for effective medical treatment of biliary tract and gallbladder cancers. This review will provide a perspective overview of selected agents, which are currently in development, or under consideration or testing for a more effective, targeted treatment of BTC (Table 1; Figure 1)[12-24]. Moreover, we will discuss promising approaches, which have not yet been tested in BTC or gallbladder cancer, but warrant future evaluation.
Table 1.
Current status of clinical trials with agents that target growth factor receptors and related signaling pathways for treatment of biliary tract and gallbladder cancers
| Name | Target | Mechanism | Cotreatment | Status | Clinical trials |
| Bevacizumab | VEGF | VEGF-neutralizing antibody | Erlotinib | Phase II | NCT00350753[17] |
| Erlotinib | Phase II | NCT00356889[18] | |||
| Radiation | Phase I | NCT00426829[21] | |||
| Floxuridine, dexamethasone | Phase II | NCT00410956[20] | |||
| Gemcitabine, oxaliplatin | Phase II | NCT00361231[19] | |||
| Cediranib (AZD2171) | PAN-VEGFR, PDGFR, c-KIT | Tyrosine kinase inhibitor | AZD-0530 | Phase I | NCT00475956 |
| Cetuximab | EGFR | Monoclonal antibody | Gemcitabine, oxaliplatin | Phase II | NCT00552149 (BINGO)[22] |
| Erlotinib | EGFR | Tyrosine kinase inhibitor | Phase II | NCT00033462[12] | |
| Gemcitabine | Phase Ib | ||||
| Oxaliplatin, gemcitabine, radiation | Phase I | NCT00266097[16] | |||
| Lapatinib | EGFR, erbB2 | Tyrosine kinase inhibitor | Phase II | NCT00107536[14] | |
| Sorafenib | VEGFR, PDGFR, c-Raf, B-Raf | Tyrosine kinase inhibitor | Oxaliplatin, | Phase II | NCT00238212[15] |
| Capecitabine | Phase I/II | NCT00634751[23] | |||
| Gemcitabine | Phase I/II | NCT00661830 (GEMSO)[24] | |||
| Bortezomib | Proteasome | Proteasome inhibitor | Phase II | NCT00085410[13] | |
| Docetaxel | Phase I |
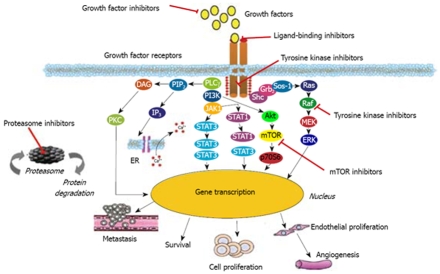
Figure 1.
Major growth factor receptor signaling pathways. TK: Tyrosine kinase; P: Phosphorylation; MEK: Mitogen-activated protein kinase; ERK: Extracellular signal-regulated kinase; PI3K: Phosphatidylinositol-3 kinase; mTOR: Mammalian target of rapamycin; JAK: Janus kinase; STAT: Signal transducer and activator of transcription.
ANTIANGIOGENIC TREATMENT STRATEGIES
Angiogenesis plays a central role in tumor growth and progression, and its implications have been extensively investigated and described in the literature for various cancers[25,26]. In the early 1970s, Folkman J[27] was the first to develop the concept of angiogenesis-dependent tumor growth and postulated that the specific blocking of blood flow to the tumor should be a promising strategy for cancer treatment.
Among the angiogenic factors/receptors described so far, the vascular endothelial growth factor (VEGF) and VEGF receptor family including the secreted glycoproteins VEGF-A, VEGF-B, VEGF-C, VEGF-D, VEGF-E, the placental growth factors (PlGF-1,-2), and their cognate receptors VEGFR-1 (Flt-1) and VEGFR-2 (Flk/KDR) play major roles in not only physiological but also in pathological angiogenesis. VEGF-A which binds to both VEGFR-1 and -2 is a key regulator of the development of the vascular system and is commonly overexpressed in a variety of solid tumors[28].
In addition, elevated levels of circulating VEGF-A are correlated with progression and metastasis of gastrointestinal cancers. A recent study confirmed that elevated VEGF expression correlated with increased metastasis of intrahepatic cholangiocarcinoma[29]. Here upregulated VEGF-C, which plays an important role in the lymph node metastasis of intrahepatic cholangiocarcinoma, was the best independent factor for a poor prognosis[30].
In this vein VEGF protein is overexpressed in cholangiocarcinomas[31], which is paralleled by VEGFR-1, -2 expression in the surrounding endothelial cells[32,33]. Therefore the VEGF/VEGFR system is an attractive target for the treatment of these almost chemoresistant cancers.
ANTIBODY-BASED ANTIANGIOGENIC THERAPY
Anti-VEGF treatment
Bevacizumab is a humanized murine monoclonal anti-VEGF antibody, which when combined with standard cytostatic treatment significantly increased survival in patients with metastatic colorectal cancer as compared to standard treatment alone[34]. This positive phase III clinical trial led to approval of bevacizumab for the treatment of advanced colorectal cancer in 2005. Comparable results were obtained in a recent phase III clinical trial of bevacizumab in non-small cell lung cancer. This study was interrupted prematurely because of an obvious survival advantage in the antibody treated patients[35].
The first clinical data on the successful treatment of cholangiocarcinoma with bevacizumab were reported in 2006, and described a patient whose metastasis from cholangiocarcinoma resolved after salvage therapy with 3 cycles of bevacizumab (5 mg/kg) combined with cisplatin (75 mg/kg) and high-dose fluorouracil and leucovorin over a period of 2 wk[36].
Currently, several studies using bevacizumab for combination therapy of cholangiocarcinoma are ongoing. An ongoing phase II trial explores the combination of systemic bevacizumab with floxuridine and dexamethasone given as a hepatic arterial infusion in patients with unresectable hepatocellular carcinoma or intrahepatic cholangiocarcinoma (NCT00410956). In this trial, patients undergo placement of the hepatic arterial infusion (HAI) pump and a cholecystectomy and receive floxuridine and dexamethasone by HAI continuously for 2 wk. Bevacizumab is concomitantly given for 30-90 min iv at the beginning and end of each cycle. Outcome measure of the study trial is to determine the antitumor efficacy (complete and partial response, stable and progressive disease) as well as toxicity as measured by Common Toxicity Criteria (CTC), which is a standard set by the National Cancer Institute to provide standard language for reporting adverse events which occur in cancer clinical trials[37].
Two other Phase II trials are currently determining the safety and efficacy of bevacizumab in combination with the EGFR tyrosine kinase inhibitor erlotinib in patients with metastatic or unresectable gall bladder or bile duct cancers and other advanced upper gastrointestinal carcinomas, which are refractory or intolerant to standard chemotherapy (NCT00350753[17]; NCT00033462[12]). This particular combination was chosen because dual targeting of cancer cells (EGFR) and their nutrient supply (anti-VEGF) will likely have synergistic antitumoral effects[38]. Synergy has been shown at the molecular level, since inhibition of the EGFR suppressed the release of VEGF from tumor cells in vitro[39,40]. Moreover, high levels of VEGF have been shown to promote resistance to anti-EGFR treatment in squamous cell carcinoma[41]. Recent clinical trials for refractory non-small-cell lung cancer and advanced renal cell carcinoma proved that this particular combination is highly effective[42-44].
The combination of bevacizumab with radiation therapy is currently being studied in inoperable hepatocellular carcinoma and cholangiocarcinoma in a non-randomized, open label phase I trial (NCT00426829[21]). In rectal cancer patients, bevacizumab was shown to enhance tumor blood flow, to reduce tumor interstitial pressure, and to decrease mean vessel density. These physiologic changes enhanced the efficacy of radiation therapy in a neoadjuvant setting[45]. It is most probable that antiangiogenic preconditioning to normalize the tumor vasculature in primary liver tumors will equally create a “therapeutic window” whereby improved blood flow with enhanced exposure to radiosensitizing oxygen is achieved.
Anti-PIGF treatment
The use of a neutralizing anti-PlGF monoclonal antibody in VEGF-inhibitor resistant tumors is an attractive alternative antiangiogenic strategy. A proof of concept study has been performed in an animal study with melanoma or pancreatic adenocarcinoma bearing mice[46]. The antibody specifically inhibits the binding of PlGF to its receptor VEGFR-1, present on tumor-associated endothelial cells and macrophages. The underlying idea of using this approach was derived from gene inactivation studies showing that endogenous PlGF is redundant in vascular development and physiological vessel maintenance, but an important contributor to the “angiogenic switch” in solid tumor growth. This led to the hypothesis that unlike VEGF inhibitors, PlGF inhibition might reduce pathological angiogenesis, without disturbing physiological blood vessel homeostasis and reduce concomitant unwanted side effects. Hence, anti-PlGF treatment could perhaps substitute for anti-VEGF therapy in the future. Moreover, as PlGF levels increase in the circulation of cancer patients receiving anti-VEGF treatment[47-49], anti-PlGF should also counteract this potential downside of anti-VEGF therapy. Accordingly, anti-PlGF-treatment inhibits angiogenesis, lymphangiogenesis, tumor growth and motility in anti-VEGF-resistant tumor bearing mice. Here, it blocks the so-called rescue-angiogenesis, a major problem in current antiangiogenic approaches, and showed excellent treatment tolerability. In addition, anti-PlGF treatment may permit long-term treatment of cancers in children, pregnant women, or patients at risk for thrombotic, cardiac or other complications for whom the adverse effects of other VEGF/VEGFR-inhibitors may be excessive and prohibitive.
ANTIANGIOGENIC THERAPY WITH SMALL MOLECULE INHIBITORS
Several agents which inhibit the tyrosine kinase activity of angiogenic growth factor receptors like the VEGFR or PDGFR, have been synthesized by combinatorial chemistry. These tyrosine kinase inhibitors are small molecules which occupy the ATP binding site of the tyrosine kinase domain of the intracellular portion of the receptor. Because of their effects on downstream signaling, these inhibitors interfere with a number of key biologic functions associated with VEGFR activation. Although drugs that are targeted to specific VEGFR kinases have shown clinical efficacy, the redundancy in the angiogenesis pathways necessitates broad spectrum inhibitors that address multiple (VEGFR) targets[50].
AZD2171
AZD2171 is a highly potent small molecule with pan-VEGFR-tyrosine kinase inhibiting activity (50% inhibitory concentration of < 0.002 μmol/L for VEGFR-2 and 0.005 μmol/L for VEGFR-1, respectively). AZD2171 also inhibits VEGFR-3, PDGFR-β and c-Kit at nanomolar concentrations[51]. The antineoplastic potency of AZD2171 has been demonstrated in several tumors, including lung, hepatocellular, colorectal and prostate cancer and in all cases the antitumor effect was associated with strong inhibition of VEGF signaling and angiogenesis[52-54]. A phase I dose-finding study was conducted in 83 patients with advanced solid tumors[52]. The study was divided into parts A and B, with 36 patients on a dose-escalation schema, in which 3 to 8 patients received a single oral dose of AZD2171 ranging from 0.5-60 mg. After a wash-out period of 2 to 7 d, the patients continued with daily treatment at the same dose level. AZD2171 was generally well tolerated at < 45 mg/d with common side effects of fatigue, nausea, diarrhea, and vomiting. In part B, an additional 47 patients were enrolled at 20, 30 or 45 mg orally daily. All patients had liver metastases and six patients had NSCLC. The major toxicities and side-effects included hypertension, headache, diarrhea, and voice hoarseness. Three patients in the 60 mg cohort each experienced one serious adverse event (grade 4 cerebral hemorrhage, grade 4 hypoglycemia, and grade 3 hypertension). Of the 83 patients enrolled, two partial responses were observed, while stable disease was seen in 23 patients.
At present AZD2171 is being evaluated in three different studies (Horizon I-III) in patients with advanced colorectal cancer. In Horizon III, which is a phase II/III study, AZD2171 is tested as a combination partner for FOLFOX compared to a combination of FOLFOX and bevacizumab in patients with previously untreated metastatic colorectal cancer. AZD2171 has shown encouraging signs of antitumor activity in a clinical development program, which has included over 700 patients to date. Based on the generally encouraging findings, AZD2171 is currently also being investigated in cholangiocarcinoma. A pending phase I trial (NCT00475956) explores the effects of AZD2171 in combination with AZD0530, a dual-specific inhibitor of Src and Abl. Src and Abl are protein tyrosine kinases which are overexpressed in malignancies such as chronic myeloid leukemia (CML), where AZD0530 has already been proved to be an effective anticancer agent[55]. The idea for using this particular combination for the treatment of cholangiocarcinoma may have arisen from observations that the Abl- and Src-inhibitor imatinib (Gleevec) showed apoptosis-inducing and growth-reducing effects in cholangiocarcinoma cells in vitro[56]. However, imatinib also inhibits other tyrosine kinases, such as c-kit and PDGFR-β. Thus it is not clear, whether the effects of imatinib on cholangiocarcinomas are related to Src-inhibition. This is doubtful as s-src expression, which is highly correlated with the indices of early stage hepatocellular carcinoma phenotype, is not likely to be involved in the cholangiocarcinoma phenotype, as no s-src activation could be detected in cholangiocarcinoma[57].
STRATEGIES TARGETING THE EGFR
The central role of the epidermal growth factor receptor (EGFR) in the proliferation of tumor epithelia and its overexpression in several solid tumors have provided the rationale for targeting this key signaling network. EGFR blockade with monoclonal antibodies and tyrosine kinase inhibitors has already translated into clinical benefit in gastrointestinal tumors, including primary liver cancer[58,59].
Over the past few years, three EGFR-specific agents have received regulatory approval: (1) The monoclonal anti-EGFR antibody cetuximab for metastatic colorectal cancer, and squamous cell carcinoma of the head and neck; (2) The tyrosine kinase inhibitor erlotinib for advanced or metastatic pancreatic cancer and NSCLC; and (3) The EGFR tyrosine kinase inhibitor gefitinib for advanced or metastatic NSCLC. However, the general FDA approval for NSCLC treatment with gefitinib was recently withdrawn after it failed to demonstrate a survival benefit either alone or with chemotherapy in three phase III trials[58,60].
Several reports indicate that the EGFR is frequently (over-)expressed in cholangiocarcinoma. Additionally, sustained EGFR activation due to defective receptor internalization has been reported for cholangiocarcinoma cells[61]. Of note, bile acids activate EGFR-signaling via a TGF-alpha-dependent mechanism, thereby contributing to the growth characteristics of cholangiocytes and cholangiocarcinoma cells[62]. Clinicopathologically, EGFR overexpression was shown to be associated with macroscopic tumor type, lymph node metastasis, tumor stage, lymphatic vessel invasion, and perineural invasion in extrahepatic cholangiocarcinoma. High levels of EGFR expression and activation increased the risk for tumor recurrence in intrahepatic cholangiocarcinoma[29]. EGFR-inhibitors inhibited cholangiocarcinoma cell growth in vitro and in vivo[33,61,63].
These encouraging preliminary findings on the general suitability of anti-EGFR-based-approaches for the treatment of cholangiocarcinoma spawned several clinical trials. In a cohort composed of 24 chemotherapy-refractory patients and 18 chemotherapy-naive patients administered oral erlotinib (150 mg/d) as monotherapy, the progression free survival at 6 mo was determined[64,65]. Seventeen percent of the patients achieved this primary end point, while disease control was obtained in 50% of patients with a median duration of 5.1 mo. Seven percent of the patients showed a partial response of 4 to 14 mo duration. The results suggest an astonishing therapeutic benefit for EGFR blockade with erlotinib in patients with advanced biliary cancer, however, this has to be confirmed in future larger controlled trials and in trials which use erlotinib in combination with other targeted agents.
An ongoing multicenter phase II trial in patients with advanced BTC (BINGO; NCT00552149) evaluates the efficacy of the EGFR-antibody cetuximab (Huether et al, 2006), combined with gemcitabine-oxaliplatin chemotherapy (GEMOX). Patients will be randomized 1:1 to receive GEMOX (1000 mg/m² gemcitabine; 100 mg/m² oxaliplatin) alone or GEMOX + cetuximab (500 mg/m²) every other week. The BINGO trial also comprises ancillary basic research and functional imaging studies, in order to identify markers that predict treatment efficacy of bile duct cancer. The primary outcome measure of the study is progression-free survival at 4 mo. Secondary outcome measures are the feasibility and toxicity of the treatments, and an evaluation of the degree and duration of objective tumor response or tumor control in a time frame of one year.
A third study used cetuximab in combination with GEMOX in a small number of nine GEMOX resistant patients with advanced, metastatic and unresectable intrahepatic cholangiocarcinoma[66]. Patients received cetuximab 400 mg/m² on day 1, then 250 mg/m² weekly, combined with gemcitabine 1000 mg/m² on day 1 and oxaliplatin 85 mg/m² on day 2, every 3 wk. Results of the study were encouraging. Cetuximab was well tolerated and provided good palliative effects in advanced cholangiocarcinoma. Moreover, adding cetuximab bypassed tumor resistance to GEMOX[67].
Taken together, anti-EGFR-based therapies for treating BTC appear to have their greatest potential when given in combination either with conventional cytostatics or with other targeted agents. The rationale for using combination therapies is the existence of multilevel receptor cross-stimulation or of redundant signaling pathways which lead to neoplasia. Blocking only one of these pathways allows others to act as salvage or escape mechanisms for cancer cells. Preclinical evidence of synergistic antitumor activity achievable by combining targeted agents that block multiple signaling pathways has recently emerged[68-70]. The multi-target approach can be accomplished by using either combinations of selective agents or single agents, which address various targets[71].
IGF/IGFR-BASED STRATEGIES
Activation of the insulin-like growth factor (IGF) receptor 1 (IGF-1R) by IGF-I and IGF-II plays a pivotal role in tumor cell proliferation and spread, by promoting cell cycle progression, preventing apoptosis, and by regulating and maintaining the metastatic tumor phenotype[70,72-75]. A wide variety of tumors show abnormal or enhanced expression of IGFs and IGF-1R, which leads to auto- and paracrine growth stimulation, and which has been correlated with enhanced proliferation, tumor de-differentiation, disease stage, development of metastases and reduced patient survival. Enhanced expression of IGF-1R has also been demonstrated in BTC, and the IGF/IGFR system was shown to be centrally involved in proliferation and suppression of apoptosis of cholangiocarcinoma cells[76], making the IGF/IGFR-signaling system an attractive target for the treatment of BTC. Thus IGF-1R blocking antibodies, IGF-1R antisense oligonucleotides, or IGF-1R siRNA have all been shown to effectively interfere with IGF-1R mediated signaling in vitro and with tumor growth and spread in vivo[76-80].
We and others validated the selective IGF-1R tyrosine kinase inhibitor NVP-AEW541 as a promising novel agent for the therapy of several cancers[81-85]. Moreover, we showed that a combination of IGF-1R inhibitors together with the multi-kinase inhibitor sorafenib, offer additive antitumoral efficacy for cholangiocarcinoma in vitro[86]. The antineoplastic properties of NVP-AEW541 and related compounds such as NVP-ADW742 have been demonstrated in preclinical studies on Ewing’s sarcoma-bearing mice, fibrosarcoma, breast cancer and musculoskeletal sarcoma[81-83].
Specific IGFR-antibodies potently suppressed prostate and breast cancer cell growth in vitro[87]. The clinically most advanced anti-IGFR antibody is CP-751871, which is currently being tested in three phase II trials for advanced breast cancer, NSCLC and prostate cancer (www.clinical-trials.gov). Importantly, the preliminary clinical data indicate that IGFR-inhibition is well-tolerated[88-90]. Safety is important, since IGFR-based inhibition has long been regarded as a high-risk intervention, because of the high homology of the IGF-1R receptor with the related insulin-receptor, and the fear that IGF-1R tyrosine kinase inhibitors may lead to insulin resistance and overt diabetes[91]. However, the current in vivo data do not support this assumption, resulting in a growing interest in anti-IGFR-based therapies[92].
Crosstalk between the signaling of the IGF/IGFR system and other growth factor receptors will likely attenuate the antineoplastic effect of monotherapeutic approaches, necessitating combinations of IGF/IGFR-targeting therapies with other therapies to enhance efficacy[93,94]. This can be achieved by dual-targeting the IGF-1R and the EGFR, since the EGFR is activated by the IGF/IGFR-system leading to mito-oncogenic EGFR-tyrosine kinase activity without ligand stimulation of the EGFR[95]. In this line IGFR- combined with EGFR-inhibition can over-additively enhance the antineoplastic effect of the respective monotherapies in gastrointestinal cancers[96-98].
DUAL-TARGETING SMALL MOLECULE INHIBITORS
The use of dual-targeting small molecule inhibitors, simultaneously blocking less related kinases such as VEGFR and EGFR tyrosine kinases, may also be promising for the future treatment of BTC. These agents inhibit both tumor cell proliferation/survival by blocking mito-oncogenic EGFR signaling of the tumor cells and angiogenesis by inhibiting endothelial VEGFRs. Recent in vivo studies of non-cholangiocarcinoma models (colon, prostate, NSCLC) demonstrated that the dual-targeting tyrosine kinase inhibitor NVP-AEE788 displayed significant antineoplastic efficacy[99-101]. NVP-AEE788 was recently also shown to be a potent inhibitor of cholangiocarcinoma cell growth[33], further emphasizing the possible suitability of EGFR/VEGFR-dual targeting agents for the treatment of cholangiocarcinoma.
ZD6474 (Zactima) is another EGFR/VEGFR tyrosine kinase inhibitor with potent antineoplastic properties in phase II/III trials on NSCLC and thyroid cancer. In these trials response rates of 30% in patients with locally advanced medullary thyroid cancer[102] as well as significant prolongation in the progression-free survival of NSCLC patients[103,104] were observed.
Clinical studies on BTC using these dual target kinase inhibitors have not yet been conducted. Nevertheless, the idea of simultaneously inhibiting these two growth factor receptor systems is currently under clinical investigation using a combination of EGFR-inhibiting erlotinib together with VEGF-neutralizing bevacizumab (see before). Indeed, the University of Colorado together with Astra Zeneca only recently started a phase I trial (NCT00551096) to determine the highest dose of Zactima that can be safely given as a single agent or in combination with gemcitabine and capecitabine in advanced solid tumors. This study is explicitly planned with an expanded cohort of patients with biliary cancers (BTC and gallbladder cancer), who will be treated at the highest determined dose in further studies.
OTHER STRATEGIES
Targeting the AKT/mTOR pathway
The activated PI3K/AKT/mTOR pathway has emerged as a novel contributor to BTC development[105]. PI3K associates with the intracellular domain of several growth factor receptors. Upon receptor activation, PI3K triggers the generation of phosphatidylinositol 3,4,5-trisphosphate (PIP3), which provokes the subsequent activation of AKT, a serine/threonine kinase that activates multiple cellular target proteins, such as the mammalian target of rapamycin (mTOR) subfamily. mTOR is a serine-threonine kinase that downregulates apoptosis, and via stimulation of cell cycle progression enhances proliferation and cell growth. Specifically, mTOR is involved in the activation of mRNA-translation into proteins, which are necessary for cell cycle progression from G1 to S-phase, including the E4-binding protein (E4-BP1), and p70S6 kinase[106]. In nontransformed cells the PI3K/AKT/mTOR pathway is controlled by the phosphatase and tensin homolog deleted on chromosome ten (PTEN), a tumor suppressor which inhibits this pathway by reversing PI3K and subsequent AKT activation. Mutation or silencing of the PTEN gene leads to activation of the mTOR pathway and promotion of carcinogenesis.
AKT-inhibition
The tricyclic nucleoside VQD-002 (triciribine phosphate monohydrate, TCN-P, Vioquest Pharmaceuticals) is a small molecule inhibitor of AKT signaling. Identified by the Moffitt Cancer Center through screening the NCI diversity set, VQD-002 was shown to be highly selective for Akt without affecting the activation of other related kinases, such as PI3K, PKC, phosphoinositide-dependent kinase-1, serum and glucocorticoid-inducible kinase, PKA, STAT-3 or ERK1/2. Accordingly, AKT-inhibition by VQD-002 resulted in suppression of cell growth and induction of apoptosis in human cancer cells and in tumor xenograft mouse models, with high selectivity for those tumors with aberrant Akt[107]. An ongoing phase I/IIa trial (NCT00363454) on metastatic solid tumors overexpressing AKT, such as pancreatic, breast, ovarian and colorectal cancer is promising, as preliminary results indicate that VQD-002 was well tolerated and prolonged the stable disease period of patients (http:www.vioquestpharm.com). VQD-002 is already earmarked for combination with the EGFR antagonist erlotinib, since preclinical studies showed that coadministration of VQD-002 can help to overcome resistance to EGFR-antibody therapy in breast cancer patients with PTEN-deficiency[108].
mTOR-inhibition
The natural antibiotic rapamycin (sirolimus) is a potent inhibitor of mTOR[109]. Recently, three analogues of rapamycin with superior pharmacokinetic and biological properties have emerged. The cell cycle inhibitor-779 (CCI-779, temsirolimus) is a soluble ester analogue. RAD001 [40-O-(2-hydroxyethyl)-rapamycin, everolimus] is a derivative of rapamycin with high oral bioavailability, and AP23573 is a non-pro-drug analogue of rapamycin. These agents have been successfully tested for their antineoplastic potency and/or tolerability in various malignancies in early clinical trials (e.g. CCI-779 in renal, breast and lung cancers), or are currently being studied in open clinical trials for the treatment of colorectal, endometrial, and brain tumors (RAD001, everolimus)[110-112]. AP23573 has been successfully tested in a phase II trial in sarcomas[113], and two phase I studies in patients with refractory or advanced solid tumors showed partial responses and disease stabilization in individual patients[114]. In preclinical investigations, the antiproliferative, antimigratory and anti-invasive potency of rapamycin in cholangiocarcinoma cells has recently been described[115]. Activated mTOR was also demonstrated to be a negative prognostic factor for patients with BTC, and patients with activated mTOR are likely to benefit from targeted therapy with mTOR inhibitors in the future[116]. However, so far no trials exploring mTOR-inhibitors for BTC have been initiated.
Targeting the Ras/Raf/MARK pathway
The proliferative Ras/Raf/MEK/ERK pathway is one the key signaling cascades that underlies the development and maintenance of cancers. This pathway transduces extracellular signals from the various growth factor receptor tyrosine kinases (e.g. EGFR, IGFR, VEGFR and PDGFR) to the nucleus with a series of specific phosphorylation events, resulting in the expression of proteins for cell cycle progression, apoptosis resistance, extracellular matrix remodeling, cellular motility, angiogenesis or drug resistance[117]. Dysregulation of this crucial pathway occurs due to oncogenic transformation of Ras and Raf isoforms, or to overexpression and/or overactivation (via phosphorylation) of the Ras and Raf genes[118,119]. Activating B-Raf mutations are relatively common in cholangiocarcinomas and disruption of the Raf/MEK/ERK (MAPK) kinase pathway, either by B-Raf or Ras mutations, is detected in more than 60% of all BTC, which is therefore one of the most frequent defects in cholangiocellular carcinogenesis[120].
Sorafenib
The bi-aryl urea derivative sorafenib (NexavarTM) is an oral multi-kinase inhibitor, which targets kinases of wild-type B-Raf, mutantV559E B-Raf and C-Raf, and importantly receptor tyrosine kinases involved in angiogenesis, including VEGFR-2, and -3, and PDGFR[121]. Sorafenib has been approved by the FDA for the treatment of advanced renal cell carcinoma and of inoperable hepatocellular cancer.
The effect of sorafenib on several molecular targets in addition to the Raf isoforms makes it difficult to determine which of its targets contributes most to its antitumor activity in a given tumor type. For instance, a recent HCC trial suggested that inhibition of the Raf/MEK/ERK pathway was central to sorafenib’s mode of antitumor action[122], whereas in other cancers, such as renal cell carcinoma or NSCLC, the antineoplastic activity was attributed mainly to its antiangiogenic activity[121,123].
Sorafenib alone or in combination with conventional cytostatics (5-fluorouracil, gemcitabine, doxorubicin) or IGF-1R inhibition induces a potent growth suppression of cholangiocarcinoma cells in vitro[86]. Antitumor efficacy was even higher when sorafenib was combined with the histone deacetylase inhibitor MS-275[124,125]. These encouraging findings have resulted in an ongoing phase II trial which evaluates sorafenib monotherapy in patients with unresectable or metastatic gallbladder cancer or BTC (NCT00238212). In an intermediate evaluation of this study, sorafenib was well tolerated, but as a single agent it did not lead to a clinically significant response rate in these patients, while its impact on survival was comparable to commonly used chemotherapy regimens. These promising results of sorafenib monotherapy will likely facilitate novel therapeutic strategies which will combine multikinase inhibition with conventional cytostatic therapy or with unrelated pathway inhibitors, such as histone deacetylase or proteasome inhibitors (see below) for enhanced and well tolerated medical treatment of advanced BTC[126].
Targeting the proteasome
Another interesting therapeutic approach for innovative cancer treatment is the inhibition of the 26S proteasome, which is a large protease that is present in both the nucleus and the cytoplasm of eukaryotic cells. The proteasome functions as an identifier and proteolytic graveyard for proteins branded for destruction by the ubiquitin system. The so-called ubiquitin-proteasome pathway (UPP) is the major non-lysosomal proteolytic system in eukaryotic cells and triggers degradation of proteins involved in cell cycle progression, apoptosis, nuclear factor kappa B (NF-κB) activation, and angiogenesis. UPP also degrades mutant, damaged, and misfolded proteins[127]. Since these signaling pathways are critical for cell survival and proliferation, especially in cancer cells, inhibition of the proteasome has emerged as an attractive target for cancer therapy.
Bortezomib
Bortezomib (VelcadeTM) is a proteasome inhibitor, which blocks multi-ubiquitinated protein degradation by reversibly and competitively inhibiting the active site threonine residue of the 26S proteasome[128]. Antineoplastic activity of bortezomib has already been shown in several in vitro and in vivo studies[129,130]. Only recently we and others showed the potent apoptosis inducing and growth inhibiting features of bortezomib in cholangiocarcinoma cells[125,131]. Bortezomib is the first proteasome inhibitor to be approved for cancer therapy and based on the results of a phase II trial[127] has recently been approved by the FDA for the treatment of mantle cell lymphoma[132,133]. Other cancers, including neuroendocrine tumors, RCC, NSCLC, or metastatic sarcomas have also been evaluated in recent phase II clinical trials. In some of these studies a significant antineoplastic effect with bortezomib monotherapy was observed, while in other studies no or only marginal responses were found[134-136]. However, in the latter cases further investigation on the role of bortezomib in combination with other antitumoral drugs was recommended, since proteasome inhibition will likely sensitize cancer cells to other therapeutic agents. Combinations with encouraging results have been reported in two studies of lung cancer and lymphoma[137,138]. In another phase I trial, bortezomib was tested in combination with the cytotoxic agent docetaxel in advanced solid tumors, including cholangiocarcinoma, where it showed generally good tolerability[13]. A phase II trial exploring bortezomib as first-line systemic therapy of patients with unresectable or metastatic adenocarcinoma of the bile duct or gallbladder is currently ongoing (NCT00085410). A comparable study in HCC was recently reported to have resulted in disease stabilization in some patients, with generally good tolerability. Here it was again suggested that the focus should next be on combinations of bortezomib with HCC-relevant cytostatics such as doxorubicin[139]. In the in vitro studies on cholangiocellular carcinoma cells we found that bortezomib shows over-additive antitumoral effects when combined with multikinase inhibitors like sorafenib or histone deacetylase inhibitors, such as MS-275[125].
CONCLUSION
Targeted-therapies, which specifically inhibit growth factor receptors and their related signaling pathways, are promising approaches for the innovative medical treatment of biliary tract and gallbladder cancers. In particular, antiangiogenic strategies as well as combination treatments with cytostatics have proved particularly efficient, as they leave fewer mechanisms of escape for the tumor cells. Combinations of these targeted drugs are especially intriguing, and in the future multi-kinase inhibitors such as sorafenib will be combined with other growth factor receptor inhibitors, proteasome inhibitors, histone deacetylase inhibitors, farnesyltransferase inhibitors or cytostatics to effectively control advanced biliary tract or gallbladder cancers. The advantage of such novel combination therapies is their higher tumor cell specificity and higher efficacy, combined with acceptable toxicity and side effects. These novel combination treatments will widen the therapeutic spectrum for biliary tract and gallbladder cancers; the results of (ongoing) clinical studies are eagerly awaited.
Footnotes
Peer reviewer: Ignacio Gil-Bazo, MD, PhD, Cancer Biology and Genetics Program, Memorial-Sloan Kettering Cancer Center, 1275 York Avenue Box 241, New York 10021, United States
S- Editor Tian L L- Editor Webster JR E- Editor Yin DH
References
- 1.de Groen PC, Gores GJ, LaRusso NF, Gunderson LL, Nagorney DM. Biliary tract cancers. N Engl J Med. 1999;341:1368–1378. doi: 10.1056/NEJM199910283411807. [DOI] [PubMed] [Google Scholar]
- 2.Renshaw K. Malignant neoplasms of the extrahepatic biliary ducts. Ann Surg. 1922;76:205–221. doi: 10.1097/00000658-192208000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldzieher M, von Bókay Z. Der primäre Leberkrebs. Virchows Arch. 1911;203:75–131. [Google Scholar]
- 4.Klatskin G. Adenocarcinoma of the hepatic duct at its bifurcation within the porta hepatis: an unusual tumor with distinctive clinical and pathological features. Am J Med. 1965;38:241–256. doi: 10.1016/0002-9343(65)90178-6. [DOI] [PubMed] [Google Scholar]
- 5.Khan SA, Taylor-Robinson SD, Toledano MB, Beck A, Elliott P, Thomas HC. Changing international trends in mortality rates for liver, biliary and pancreatic tumours. J Hepatol. 2002;37:806–813. doi: 10.1016/s0168-8278(02)00297-0. [DOI] [PubMed] [Google Scholar]
- 6.Patel T. Increasing incidence and mortality of primary intrahepatic cholangiocarcinoma in the United States. Hepatology. 2001;33:1353–1357. doi: 10.1053/jhep.2001.25087. [DOI] [PubMed] [Google Scholar]
- 7.Patel T. Worldwide trends in mortality from biliary tract malignancies. BMC Cancer. 2002;2:10. doi: 10.1186/1471-2407-2-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Taylor-Robinson SD, Toledano MB, Arora S, Keegan TJ, Hargreaves S, Beck A, Khan SA, Elliott P, Thomas HC. Increase in mortality rates from intrahepatic cholangiocarcinoma in England and Wales 1968-1998. Gut. 2001;48:816–820. doi: 10.1136/gut.48.6.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ishak KG, Anthony PP, Sobin LH. Histological typing of tumours of the liver. World Health Organization International Histological Typing of Tumours. 2nd ed. Vol. 48. Berlin: Springer-Verlag; 2007. [Google Scholar]
- 10.Carriaga MT, Henson DE. Liver, gallbladder, extrahepatic bile ducts, and pancreas. Cancer. 1995;75:171–190. doi: 10.1002/1097-0142(19950101)75:1+<171::aid-cncr2820751306>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 11.Shaib Y, El-Serag HB. The epidemiology of cholangiocarcinoma. Semin Liver Dis. 2004;24:115–125. doi: 10.1055/s-2004-828889. [DOI] [PubMed] [Google Scholar]
- 12.Dragovich T, Huberman M, Von Hoff DD, Rowinsky EK, Nadler P, Wood D, Hamilton M, Hage G, Wolf J, Patnaik A. Erlotinib plus gemcitabine in patients with unresectable pancreatic cancer and other solid tumors: phase IB trial. Cancer Chemother Pharmacol. 2007;60:295–303. doi: 10.1007/s00280-006-0389-0. [DOI] [PubMed] [Google Scholar]
- 13.Messersmith WA, Baker SD, Lassiter L, Sullivan RA, Dinh K, Almuete VI, Wright JJ, Donehower RC, Carducci MA, Armstrong DK. Phase I trial of bortezomib in combination with docetaxel in patients with advanced solid tumors. Clin Cancer Res. 2006;12:1270–1275. doi: 10.1158/1078-0432.CCR-05-1942. [DOI] [PubMed] [Google Scholar]
- 14.Lapatinib in treating patients with unresectable liver or biliary tract cancer. ClinicalTrials.gov Identifier: NCT00107536. Available from: URL: http://clinicaltrials.gov/show/ NCT00107536.
- 15.Sorafenib in treating patients with unresectable or metastatic gallbladder cancer or cholangiocarcinoma. ClinicalTrials.gov Identifier: NCT00238212. Available from: URL: http://clinicaltrials.gov/show/ NCT00238212.
- 16.Oxaliplatin, gemcitabine, erlotinib, and radiation therapy in treating patients with unresectable and/or metastatic pancreatic cancer or biliary tract cancer. ClinicalTrials.gov Identifier: NCT00266097. Available from: URL: http://clinicaltrials.gov/show/ NCT00266097.
- 17.Avastin and tarceva for upper gastrointestinal cancers. ClinicalTrials.gov Identifier: NCT00350753. Available from: URL: http://clinicaltrials.gov/show/ NCT00350753.
- 18.Bevacizumab and erlotinib in treating patients with metastatic or unresectable biliary tumors. ClinicalTrials.gov Identifier: NCT00356889. Available from: URL: http://clinicaltrials.gov/show/ NCT00356889.
- 19.Gemcitabine, oxaliplatin in combination with bevacizumab in biliary tract and gallbladder cancer. ClinicalTrials.gov Identifier: NCT00361231. Available from: URL: http://clinicaltrials.gov/show/ NCT00361231.
- 20.Floxuridine and dexamethasone as a hepatic arterial infusion and bevacizumab in treating patients with primary liver cancer that cannot be removed by surgery. ClinicalTrials.gov Identifier: NCT00410956. Available from: URL: http://clinicaltrials.gov/show/ NCT00410956.
- 21.Proton therapy and bevacizumab for primary liver tumors. ClinicalTrials.gov Identifier: NCT00426829. Available from: URL: http://clinicaltrials.gov/show/ NCT00426829.
- 22.Biliary cancers: egfr inhibitor, gemcitabine and oxaliplatin. ClinicalTrials.gov Identifier: NCT00552149. Available from: URL: http://clinicaltrials.gov/show/ NCT00552149.
- 23.CO07204-Phase I/II of oxaliplatin, capecitabine & sorafenib for Advanced Pancreatic & Biliary Carcinoma. ClinicalTrials.gov Identifier: NCT00634751. Available from: URL: http://clinicaltrials.gov/show/ NCT00634751.
- 24.Gemcitabine and Sorafenib in Advanced Biliary Tract Cancer (GEMSO) ClinicalTrials.gov Identifier: NCT00661830. Available from: URL: http://clinicaltrials.gov/show/ NCT00661830.
- 25.Carmeliet P. Angiogenesis in health and disease. Nat Med. 2003;9:653–660. doi: 10.1038/nm0603-653. [DOI] [PubMed] [Google Scholar]
- 26.Folkman J. Role of angiogenesis in tumor growth and metastasis. Semin Oncol. 2002;29:15–18. doi: 10.1053/sonc.2002.37263. [DOI] [PubMed] [Google Scholar]
- 27.Folkman J. Tumor angiogenesis: therapeutic implications. N Engl J Med. 1971;285:1182–1186. doi: 10.1056/NEJM197111182852108. [DOI] [PubMed] [Google Scholar]
- 28.Shibuya M. Vascular endothelial growth factor receptor-1 (VEGFR-1/Flt-1): a dual regulator for angiogenesis. Angiogenesis. 2006;9:225–230; discussion 231. doi: 10.1007/s10456-006-9055-8. [DOI] [PubMed] [Google Scholar]
- 29.Yoshikawa D, Ojima H, Iwasaki M, Hiraoka N, Kosuge T, Kasai S, Hirohashi S, Shibata T. Clinicopathological and prognostic significance of EGFR, VEGF, and HER2 expression in cholangiocarcinoma. Br J Cancer. 2008;98:418–425. doi: 10.1038/sj.bjc.6604129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Park BK, Paik YH, Park JY, Park KH, Bang S, Park SW, Chung JB, Park YN, Song SY. The clinicopathologic significance of the expression of vascular endothelial growth factor-C in intrahepatic cholangiocarcinoma. Am J Clin Oncol. 2006;29:138–142. doi: 10.1097/01.coc.0000204402.29830.08. [DOI] [PubMed] [Google Scholar]
- 31.Hida Y, Morita T, Fujita M, Miyasaka Y, Horita S, Fujioka Y, Nagashima K, Katoh H. Vascular endothelial growth factor expression is an independent negative predictor in extrahepatic biliary tract carcinomas. Anticancer Res. 1999;19:2257–2260. [PubMed] [Google Scholar]
- 32.Benckert C, Jonas S, Cramer T, Von Marschall Z, Schafer G, Peters M, Wagner K, Radke C, Wiedenmann B, Neuhaus P, et al. Transforming growth factor beta 1 stimulates vascular endothelial growth factor gene transcription in human cholangiocellular carcinoma cells. Cancer Res. 2003;63:1083–1092. [PubMed] [Google Scholar]
- 33.Wiedmann M, Feisthammel J, Bluthner T, Tannapfel A, Kamenz T, Kluge A, Mossner J, Caca K. Novel targeted approaches to treating biliary tract cancer: the dual epidermal growth factor receptor and ErbB-2 tyrosine kinase inhibitor NVP-AEE788 is more efficient than the epidermal growth factor receptor inhibitors gefitinib and erlotinib. Anticancer Drugs. 2006;17:783–795. doi: 10.1097/01.cad.0000217433.48870.37. [DOI] [PubMed] [Google Scholar]
- 34.Hurwitz H, Fehrenbacher L, Novotny W, Cartwright T, Hainsworth J, Heim W, Berlin J, Baron A, Griffing S, Holmgren E, et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med. 2004;350:2335–2342. doi: 10.1056/NEJMoa032691. [DOI] [PubMed] [Google Scholar]
- 35.Sandler A, Gray R, Perry MC, Brahmer J, Schiller JH, Dowlati A, Lilenbaum R, Johnson DH. Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med. 2006;355:2542–2550. doi: 10.1056/NEJMoa061884. [DOI] [PubMed] [Google Scholar]
- 36.Tai CJ, Chiou HY, Wu CH, Pan S, Liu JD. Rapid resolution of liver metastasis from cholangiocarcinoma after bevacizumab with cisplatin and high-dose fluorouracil plus leucovorin. Onkologie. 2006;29:179–180. doi: 10.1159/000091751. [DOI] [PubMed] [Google Scholar]
- 37.Müller RP, Seegenschmiedt MH, Höffken K, Junginger T, Sauer H. Common Toxicity Criteria (CTC): Dokumentation von Nebenwirkungen in der Onkologie. Dtsch Ärztebl. 1999;96:A489–A495. [Google Scholar]
- 38.Greten TF. [Molecular therapy for HCC?] Z Gastroenterol. 2006;44:205–206. doi: 10.1055/s-2005-859031. [DOI] [PubMed] [Google Scholar]
- 39.Riedel F, Gotte K, Li M, Hormann K, Grandis JR. EGFR antisense treatment of human HNSCC cell lines down-regulates VEGF expression and endothelial cell migration. Int J Oncol. 2002;21:11–16. [PubMed] [Google Scholar]
- 40.Ciardiello F, Caputo R, Bianco R, Damiano V, Fontanini G, Cuccato S, De Placido S, Bianco AR, Tortora G. Inhibition of growth factor production and angiogenesis in human cancer cells by ZD1839 (Iressa), a selective epidermal growth factor receptor tyrosine kinase inhibitor. Clin Cancer Res. 2001;7:1459–1465. [PubMed] [Google Scholar]
- 41.Viloria-Petit A, Crombet T, Jothy S, Hicklin D, Bohlen P, Schlaeppi JM, Rak J, Kerbel RS. Acquired resistance to the antitumor effect of epidermal growth factor receptor-blocking antibodies in vivo: a role for altered tumor angiogenesis. Cancer Res. 2001;61:5090–5101. [PubMed] [Google Scholar]
- 42.Gridelli C, Maione P, Rossi A, De Marinis F. The role of bevacizumab in the treatment of non-small cell lung cancer: current indications and future developments. Oncologist. 2007;12:1183–1193. doi: 10.1634/theoncologist.12-10-1183. [DOI] [PubMed] [Google Scholar]
- 43.Hainsworth JD, Sosman JA, Spigel DR, Edwards DL, Baughman C, Greco A. Treatment of metastatic renal cell carcinoma with a combination of bevacizumab and erlotinib. J Clin Oncol. 2005;23:7889–7896. doi: 10.1200/JCO.2005.01.8234. [DOI] [PubMed] [Google Scholar]
- 44.Herbst RS, Johnson DH, Mininberg E, Carbone DP, Henderson T, Kim ES, Blumenschein G Jr, Lee JJ, Liu DD, Truong MT, et al. Phase I/II trial evaluating the anti-vascular endothelial growth factor monoclonal antibody bevacizumab in combination with the HER-1/epidermal growth factor receptor tyrosine kinase inhibitor erlotinib for patients with recurrent non-small-cell lung cancer. J Clin Oncol. 2005;23:2544–2555. doi: 10.1200/JCO.2005.02.477. [DOI] [PubMed] [Google Scholar]
- 45.Czito BG, Bendell JC, Willett CG, Morse MA, Blobe GC, Tyler DS, Thomas J, Ludwig KA, Mantyh CR, Ashton J, et al. Bevacizumab, oxaliplatin, and capecitabine with radiation therapy in rectal cancer: Phase I trial results. Int J Radiat Oncol Biol Phys. 2007;68:472–478. doi: 10.1016/j.ijrobp.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 46.Fischer C, Jonckx B, Mazzone M, Zacchigna S, Loges S, Pattarini L, Chorianopoulos E, Liesenborghs L, Koch M, De Mol M, et al. Anti-PlGF inhibits growth of VEGF(R)-inhibitor-resistant tumors without affecting healthy vessels. Cell. 2007;131:463–475. doi: 10.1016/j.cell.2007.08.038. [DOI] [PubMed] [Google Scholar]
- 47.Willett CG, Boucher Y, Duda DG, di Tomaso E, Munn LL, Tong RT, Kozin SV, Petit L, Jain RK, Chung DC, et al. Surrogate markers for antiangiogenic therapy and dose-limiting toxicities for bevacizumab with radiation and chemotherapy: continued experience of a phase I trial in rectal cancer patients. J Clin Oncol. 2005;23:8136–8139. doi: 10.1200/JCO.2005.02.5635. [DOI] [PubMed] [Google Scholar]
- 48.Motzer RJ, Michaelson MD, Redman BG, Hudes GR, Wilding G, Figlin RA, Ginsberg MS, Kim ST, Baum CM, DePrimo SE, et al. Activity of SU11248, a multitargeted inhibitor of vascular endothelial growth factor receptor and platelet-derived growth factor receptor, in patients with metastatic renal cell carcinoma. J Clin Oncol. 2006;24:16–24. doi: 10.1200/JCO.2005.02.2574. [DOI] [PubMed] [Google Scholar]
- 49.Rosen LS, Kurzrock R, Mulay M, Van Vugt A, Purdom M, Ng C, Silverman J, Koutsoukos A, Sun YN, Bass MB, et al. Safety, pharmacokinetics, and efficacy of AMG 706, an oral multikinase inhibitor, in patients with advanced solid tumors. J Clin Oncol. 2007;25:2369–2376. doi: 10.1200/JCO.2006.07.8170. [DOI] [PubMed] [Google Scholar]
- 50.Cabebe E, Wakelee H. Role of anti-angiogenesis agents in treating NSCLC: focus on bevacizumab and VEGFR tyrosine kinase inhibitors. Curr Treat Options Oncol. 2007;8:15–27. doi: 10.1007/s11864-007-0022-4. [DOI] [PubMed] [Google Scholar]
- 51.Zhu AX. Development of sorafenib and other molecularly targeted agents in hepatocellular carcinoma. Cancer. 2008;112:250–259. doi: 10.1002/cncr.23175. [DOI] [PubMed] [Google Scholar]
- 52.Drevs J, Siegert P, Medinger M, Mross K, Strecker R, Zirrgiebel U, Harder J, Blum H, Robertson J, Jurgensmeier JM, et al. Phase I clinical study of AZD2171, an oral vascular endothelial growth factor signaling inhibitor, in patients with advanced solid tumors. J Clin Oncol. 2007;25:3045–3054. doi: 10.1200/JCO.2006.07.2066. [DOI] [PubMed] [Google Scholar]
- 53.Aragon-Ching JB, Dahut WL. The role of angiogenesis inhibitors in prostate cancer. Cancer J. 2008;14:20–25. doi: 10.1097/PPO.0b013e318161c014. [DOI] [PubMed] [Google Scholar]
- 54.Wedge SR, Kendrew J, Hennequin LF, Valentine PJ, Barry ST, Brave SR, Smith NR, James NH, Dukes M, Curwen JO, et al. AZD2171: a highly potent, orally bioavailable, vascular endothelial growth factor receptor-2 tyrosine kinase inhibitor for the treatment of cancer. Cancer Res. 2005;65:4389–4400. doi: 10.1158/0008-5472.CAN-04-4409. [DOI] [PubMed] [Google Scholar]
- 55.Nowak D, Boehrer S, Hochmuth S, Trepohl B, Hofmann W, Hoelzer D, Hofmann WK, Mitrou PS, Ruthardt M, Chow KU. Src kinase inhibitors induce apoptosis and mediate cell cycle arrest in lymphoma cells. Anticancer Drugs. 2007;18:981–995. doi: 10.1097/CAD.0b013e3281721ff6. [DOI] [PubMed] [Google Scholar]
- 56.Chiorean MV, Guicciardi ME, Yoon JH, Bronk SF, Kaufmanns SH, Gores GJ. Imatinib mesylate induces apoptosis in human cholangiocarcinoma cells. Liver Int. 2004;24:687–695. doi: 10.1111/j.1478-3231.2004.0984.x. [DOI] [PubMed] [Google Scholar]
- 57.Ito Y, Kawakatsu H, Takeda T, Sakon M, Nagano H, Sakai T, Miyoshi E, Noda K, Tsujimoto M, Wakasa K, et al. Activation of c-Src gene product in hepatocellular carcinoma is highly correlated with the indices of early stage phenotype. J Hepatol. 2001;35:68–73. doi: 10.1016/s0168-8278(01)00077-0. [DOI] [PubMed] [Google Scholar]
- 58.Rocha-Lima CM, Soares HP, Raez LE, Singal R. EGFR targeting of solid tumors. Cancer Control. 2007;14:295–304. doi: 10.1177/107327480701400313. [DOI] [PubMed] [Google Scholar]
- 59.Sangro B, Mazzollini G, Prieto J. Future therapies for hepatocellular carcinoma. Eur J Gastroenterol Hepatol. 2005;17:515–521. doi: 10.1097/00042737-200505000-00007. [DOI] [PubMed] [Google Scholar]
- 60.Thatcher N, Chang A, Parikh P, Rodrigues Pereira J, Ciuleanu T, von Pawel J, Thongprasert S, Tan EH, Pemberton K, Archer V, et al. Gefitinib plus best supportive care in previously treated patients with refractory advanced non-small-cell lung cancer: results from a randomised, placebo-controlled, multicentre study (Iressa Survival Evaluation in Lung Cancer) Lancet. 2005;366:1527–1537. doi: 10.1016/S0140-6736(05)67625-8. [DOI] [PubMed] [Google Scholar]
- 61.Yoon JH, Gwak GY, Lee HS, Bronk SF, Werneburg NW, Gores GJ. Enhanced epidermal growth factor receptor activation in human cholangiocarcinoma cells. J Hepatol. 2004;41:808–814. doi: 10.1016/j.jhep.2004.07.016. [DOI] [PubMed] [Google Scholar]
- 62.Werneburg NW, Yoon JH, Higuchi H, Gores GJ. Bile acids activate EGF receptor via a TGF-alpha-dependent mechanism in human cholangiocyte cell lines. Am J Physiol Gastrointest Liver Physiol. 2003;285:G31–G36. doi: 10.1152/ajpgi.00536.2002. [DOI] [PubMed] [Google Scholar]
- 63.Jimeno A, Rubio-Viqueira B, Amador ML, Oppenheimer D, Bouraoud N, Kulesza P, Sebastiani V, Maitra A, Hidalgo M. Epidermal growth factor receptor dynamics influences response to epidermal growth factor receptor targeted agents. Cancer Res. 2005;65:3003–3010. doi: 10.1158/0008-5472.CAN-04-3586. [DOI] [PubMed] [Google Scholar]
- 64.Philip PA, Mahoney MR, Allmer C, Thomas J, Pitot HC, Kim G, Donehower RC, Fitch T, Picus J, Erlichman C. Phase II study of erlotinib in patients with advanced biliary cancer. J Clin Oncol. 2006;24:3069–3074. doi: 10.1200/JCO.2005.05.3579. [DOI] [PubMed] [Google Scholar]
- 65.Leone F, Pignochino Y, Cavalloni G, Aglietta M. Targeting of epidermal growth factor receptor in patients affected by biliary tract carcinoma. J Clin Oncol. 2007;25:1145; author reply 1145–1145; author reply 1146. doi: 10.1200/JCO.2006.09.3427. [DOI] [PubMed] [Google Scholar]
- 66.Paule B, Bralet M, Herelle M, Rage E, Ducreux M, Guettier C, Adam R. Cetuximab plus gemcitabine/oxaliplatin (GEMOX) for patients with unresectable/recurrent intrahepatic cholangiocarcinoma refractory to GEMOX. J Clin Oncol. 2007;24 Suppl 18:14084. doi: 10.1159/000111117. [DOI] [PubMed] [Google Scholar]
- 67.Paule B, Herelle MO, Rage E, Ducreux M, Adam R, Guettier C, Bralet MP. Cetuximab plus gemcitabine-oxaliplatin (GEMOX) in patients with refractory advanced intrahepatic cholangiocarcinomas. Oncology. 2007;72:105–110. doi: 10.1159/000111117. [DOI] [PubMed] [Google Scholar]
- 68.Ganslmayer M, Ocker M, Kraemer G, Zopf S, Hahn EG, Schuppan D, Herold C. The combination of tamoxifen and 9cis retinoic acid exerts overadditive anti-tumoral efficacy in rat hepatocellular carcinoma. J Hepatol. 2004;40:952–956. doi: 10.1016/j.jhep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 69.Ciardiello F, Troiani T, Bianco R, Orditura M, Morgillo F, Martinelli E, Morelli MP, Cascone T, Tortora G. Interaction between the epidermal growth factor receptor (EGFR) and the vascular endothelial growth factor (VEGF) pathways: a rational approach for multi-target anticancer therapy. Ann Oncol. 2006;17 Suppl 7:vii109–vii114. doi: 10.1093/annonc/mdl962. [DOI] [PubMed] [Google Scholar]
- 70.Sachdev D, Yee D. Disrupting insulin-like growth factor signaling as a potential cancer therapy. Mol Cancer Ther. 2007;6:1–12. doi: 10.1158/1535-7163.MCT-06-0080. [DOI] [PubMed] [Google Scholar]
- 71.Maione P, Gridelli C, Troiani T, Ciardiello F. Combining targeted therapies and drugs with multiple targets in the treatment of NSCLC. Oncologist. 2006;11:274–284. doi: 10.1634/theoncologist.11-3-274. [DOI] [PubMed] [Google Scholar]
- 72.Zhang H, Yee D. The therapeutic potential of agents targeting the type I insulin-like growth factor receptor. Expert Opin Investig Drugs. 2004;13:1569–1577. doi: 10.1517/13543784.13.12.1569. [DOI] [PubMed] [Google Scholar]
- 73.Wang Z, Ruan YB, Guan Y, Liu SH. Expression of IGF-II in early experimental hepatocellular carcinomas and its significance in early diagnosis. World J Gastroenterol. 2003;9:267–270. doi: 10.3748/wjg.v9.i2.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wang Y, Sun Y. Insulin-like growth factor receptor-1 as an anti-cancer target: blocking transformation and inducing apoptosis. Curr Cancer Drug Targets. 2002;2:191–207. doi: 10.2174/1568009023333863. [DOI] [PubMed] [Google Scholar]
- 75.Hofmann F, Garcia-Echeverria C. Blocking the insulin-like growth factor-I receptor as a strategy for targeting cancer. Drug Discov Today. 2005;10:1041–1047. doi: 10.1016/S1359-6446(05)03512-9. [DOI] [PubMed] [Google Scholar]
- 76.Alvaro D, Barbaro B, Franchitto A, Onori P, Glaser SS, Alpini G, Francis H, Marucci L, Sterpetti P, Ginanni-Corradini S, et al. Estrogens and insulin-like growth factor 1 modulate neoplastic cell growth in human cholangiocarcinoma. Am J Pathol. 2006;169:877–888. doi: 10.2353/ajpath.2006.050464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Scotlandi K, Benini S, Nanni P, Lollini PL, Nicoletti G, Landuzzi L, Serra M, Manara MC, Picci P, Baldini N. Blockage of insulin-like growth factor-I receptor inhibits the growth of Ewing's sarcoma in athymic mice. Cancer Res. 1998;58:4127–4131. [PubMed] [Google Scholar]
- 78.Shapiro DN, Jones BG, Shapiro LH, Dias P, Houghton PJ. Antisense-mediated reduction in insulin-like growth factor-I receptor expression suppresses the malignant phenotype of a human alveolar rhabdomyosarcoma. J Clin Invest. 1994;94:1235–1242. doi: 10.1172/JCI117441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Salisbury AJ, Macaulay VM. Development of molecular agents for IGF receptor targeting. Horm Metab Res. 2003;35:843–849. doi: 10.1055/s-2004-814158. [DOI] [PubMed] [Google Scholar]
- 80.Ellouk-Achard S, Djenabi S, De Oliveira GA, Desauty G, Duc HT, Zohair M, Trojan J, Claude JR, Sarasin A, Lafarge-Frayssinet C. Induction of apoptosis in rat hepatocarcinoma cells by expression of IGF-I antisense c-DNA. J Hepatol. 1998;29:807–818. doi: 10.1016/s0168-8278(98)80263-8. [DOI] [PubMed] [Google Scholar]
- 81.Tanno B, Mancini C, Vitali R, Mancuso M, McDowell HP, Dominici C, Raschella G. Down-regulation of insulin-like growth factor I receptor activity by NVP-AEW541 has an antitumor effect on neuroblastoma cells in vitro and in vivo. Clin Cancer Res. 2006;12:6772–6780. doi: 10.1158/1078-0432.CCR-06-1479. [DOI] [PubMed] [Google Scholar]
- 82.Höpfner M, Sutter AP, Huether A, Baradari V, Scherubl H. Tyrosine kinase of insulin-like growth factor receptor as target for novel treatment and prevention strategies of colorectal cancer. World J Gastroenterol. 2006;12:5635–5643. doi: 10.3748/wjg.v12.i35.5635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Höpfner M, Huether A, Sutter AP, Baradari V, Schuppan D, Scherubl H. Blockade of IGF-1 receptor tyrosine kinase has antineoplastic effects in hepatocellular carcinoma cells. Biochem Pharmacol. 2006;71:1435–1448. doi: 10.1016/j.bcp.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 84.Garcia-Echeverria C, Pearson MA, Marti A, Meyer T, Mestan J, Zimmermann J, Gao J, Brueggen J, Capraro HG, Cozens R, et al. In vivo antitumor activity of NVP-AEW541-A novel, potent, and selective inhibitor of the IGF-IR kinase. Cancer Cell. 2004;5:231–239. doi: 10.1016/s1535-6108(04)00051-0. [DOI] [PubMed] [Google Scholar]
- 85.Scotlandi K, Manara MC, Nicoletti G, Lollini PL, Lukas S, Benini S, Croci S, Perdichizzi S, Zambelli D, Serra M, et al. Antitumor activity of the insulin-like growth factor-I receptor kinase inhibitor NVP-AEW541 in musculoskeletal tumors. Cancer Res. 2005;65:3868–3876. doi: 10.1158/0008-5472.CAN-04-3192. [DOI] [PubMed] [Google Scholar]
- 86.Huether A, Höpfner M, Baradari V, Schuppan D, Scherubl H. Sorafenib alone or as combination therapy for growth control of cholangiocarcinoma. Biochem Pharmacol. 2007;73:1308–1317. doi: 10.1016/j.bcp.2006.12.031. [DOI] [PubMed] [Google Scholar]
- 87.Feng Y, Zhu Z, Xiao X, Choudhry V, Barrett JC, Dimitrov DS. Novel human monoclonal antibodies to insulin-like growth factor (IGF)-II that potently inhibit the IGF receptor type I signal transduction function. Mol Cancer Ther. 2006;5:114–120. doi: 10.1158/1535-7163.MCT-05-0252. [DOI] [PubMed] [Google Scholar]
- 88.Manara MC, Landuzzi L, Nanni P, Nicoletti G, Zambelli D, Lollini PL, Nanni C, Hofmann F, Garcia-Echeverria C, Picci P, et al. Preclinical in vivo study of new insulin-like growth factor-I receptor--specific inhibitor in Ewing's sarcoma. Clin Cancer Res. 2007;13:1322–1330. doi: 10.1158/1078-0432.CCR-06-1518. [DOI] [PubMed] [Google Scholar]
- 89.Hofmann F, Brueggen J, Capraro H-G, Cozens R, Evans DB, Fabbro D, Ferrari S, Furet P, Garcia-Echeverria C, Geiger T, et al. In vitro and in vivo profiling of selective and potent IGF-IR kinase inhibitors. Proc AACR. 2003;44:3798. [Google Scholar]
- 90.Burtrum D, Zhu Z, Lu D, Anderson DM, Prewett M, Pereira DS, Bassi R, Abdullah R, Hooper AT, Koo H, et al. A fully human monoclonal antibody to the insulin-like growth factor I receptor blocks ligand-dependent signaling and inhibits human tumor growth in vivo. Cancer Res. 2003;63:8912–8921. [PubMed] [Google Scholar]
- 91.Garber K. IGF-1: old growth factor shines as new drug target. J Natl Cancer Inst. 2005;97:790–792. doi: 10.1093/jnci/97.11.790. [DOI] [PubMed] [Google Scholar]
- 92.Leary A, Johnston SR. Small molecule signal transduction inhibitors for the treatment of solid tumors. Cancer Invest. 2007;25:347–365. doi: 10.1080/07357900701259694. [DOI] [PubMed] [Google Scholar]
- 93.Desbois-Mouthon C, Cacheux W, Blivet-Van Eggelpoel MJ, Barbu V, Fartoux L, Poupon R, Housset C, Rosmorduc O. Impact of IGF-1R/EGFR cross-talks on hepatoma cell sensitivity to gefitinib. Int J Cancer. 2006;119:2557–2566. doi: 10.1002/ijc.22221. [DOI] [PubMed] [Google Scholar]
- 94.Tao Y, Pinzi V, Bourhis J, Deutsch E. Mechanisms of disease: signaling of the insulin-like growth factor 1 receptor pathway--therapeutic perspectives in cancer. Nat Clin Pract Oncol. 2007;4:591–602. doi: 10.1038/ncponc0934. [DOI] [PubMed] [Google Scholar]
- 95.Gilmore AP, Valentijn AJ, Wang P, Ranger AM, Bundred N, O'Hare MJ, Wakeling A, Korsmeyer SJ, Streuli CH. Activation of BAD by therapeutic inhibition of epidermal growth factor receptor and transactivation by insulin-like growth factor receptor. J Biol Chem. 2002;277:27643–27650. doi: 10.1074/jbc.M108863200. [DOI] [PubMed] [Google Scholar]
- 96.Höpfner M, Sutter AP, Huether A, Baradari V, Scherubl H. Tyrosine kinase of insulin-like growth factor receptor as target for novel treatment and prevention strategies of colorectal cancer. World J Gastroenterol. 2006;12:5635–5643. doi: 10.3748/wjg.v12.i35.5635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Huether A, Höpfner M, Baradari V, Schuppan D, Scherubl H. EGFR blockade by cetuximab alone or as combination therapy for growth control of hepatocellular cancer. Biochem Pharmacol. 2005;70:1568–1578. doi: 10.1016/j.bcp.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 98.Huether A, Hopfner M, Sutter AP, Schuppan D, Scherubl H. Erlotinib induces cell cycle arrest and apoptosis in hepatocellular cancer cells and enhances chemosensitivity towards cytostatics. J Hepatol. 2005;43:661–669. doi: 10.1016/j.jhep.2005.02.040. [DOI] [PubMed] [Google Scholar]
- 99.Heymach JV. ZD6474-clinical experience to date. Br J Cancer. 2005;92 Suppl 1:S14–S20. doi: 10.1038/sj.bjc.6602604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Busby JE, Kim SJ, Yazici S, Nakamura T, Kim JS, He J, Maya M, Wang X, Do KA, Fan D, et al. Therapy of multidrug resistant human prostate tumors in the prostate of nude mice by simultaneous targeting of the epidermal growth factor receptor and vascular endothelial growth factor receptor on tumor-associated endothelial cells. Prostate. 2006;66:1788–1798. doi: 10.1002/pros.20519. [DOI] [PubMed] [Google Scholar]
- 101.Younes MN, Park YW, Yazici YD, Gu M, Santillan AA, Nong X, Kim S, Jasser SA, El-Naggar AK, Myers JN. Concomitant inhibition of epidermal growth factor and vascular endothelial growth factor receptor tyrosine kinases reduces growth and metastasis of human salivary adenoid cystic carcinoma in an orthotopic nude mouse model. Mol Cancer Ther. 2006;5:2696–2705. doi: 10.1158/1535-7163.MCT-05-0228. [DOI] [PubMed] [Google Scholar]
- 102.Lakhani VT, You YN, Wells SA. The multiple endocrine neoplasia syndromes. Annu Rev Med. 2007;58:253–265. doi: 10.1146/annurev.med.58.100305.115303. [DOI] [PubMed] [Google Scholar]
- 103.Natale RB, Bodkin D, Govindan R, Sleckman B, Rizvi N, Capo A, Germonpré P, Stockman P, Kennedy S, Ranson M. ZD6474 versus gefitinib in patients with advanced NSCLC: Final results from a two-part, double-blind, randomized phase II trial. J Clin Oncol. 2006;24(18S):7000. doi: 10.1200/JCO.2008.18.6015. [DOI] [PubMed] [Google Scholar]
- 104.Wells S, You YN, Lakhani V, Hou J, Langmuir P, Headley D, Skinner M, Morse M, Burch W, Schlumberger M. A phase II trial of ZD6474 in patients with hereditary metastatic medullary thyroid cancer. J Clin Oncol. 2006;24(20S):5533. [Google Scholar]
- 105.Schmitz KJ, Lang H, Wohlschlaeger J, Sotiropoulos GC, Reis H, Schmid KW, Baba HA. AKT and ERK1/2 signaling in intrahepatic cholangiocarcinoma. World J Gastroenterol. 2007;13:6470–6477. doi: 10.3748/wjg.v13.i48.6470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Duran I, Salazar R, Casanovas O, Arrazubi V, Vilar E, Siu LL, Yao J, Tabernero J. New drug development in digestive neuroendocrine tumors. Ann Oncol. 2007;18:1307–1313. doi: 10.1093/annonc/mdm009. [DOI] [PubMed] [Google Scholar]
- 107.Yang L, Dan HC, Sun M, Liu Q, Kaneko S, Sun XM, Feldman RI, Nicosia SV, Sebti SM, Cheng JQ. Discovery of a small molecule Akt inhibitor with antitumor activity in cancer cells overexpressing Akt. Proc Amer Assoc Cancer Res (meeting abstract) 2004;45(suppl):893. doi: 10.1158/0008-5472.CAN-04-0343. [DOI] [PubMed] [Google Scholar]
- 108.Yu D, Esteva F, Lu CH, Wyszomierski S, Sahin A, Mills G, Hung MC, Hortobagyi G. Strategies for overcoming trastuzumab resistance caused by PTEN deficiency. Proceedings of the 99th Annual Meeting of the American Association for Cancer Research. Pro AACR. 2008:675. doi: 10.1158/1078-0432.CCR-06-2837. [DOI] [PubMed] [Google Scholar]
- 109.Tsang CK, Qi H, Liu LF, Zheng XF. Targeting mammalian target of rapamycin (mTOR) for health and diseases. Drug Discov Today. 2007;12:112–124. doi: 10.1016/j.drudis.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 110.Dudkin L, Dilling MB, Cheshire PJ, Harwood FC, Hollingshead M, Arbuck SG, Travis R, Sausville EA, Houghton PJ. Biochemical correlates of mTOR inhibition by the rapamycin ester CCI-779 and tumor growth inhibition. Clin Cancer Res. 2001;7:1758–1764. [PubMed] [Google Scholar]
- 111.Easton JB, Houghton PJ. mTOR and cancer therapy. Oncogene. 2006;25:6436–6446. doi: 10.1038/sj.onc.1209886. [DOI] [PubMed] [Google Scholar]
- 112.Wullschleger S, Loewith R, Hall MN. TOR signaling in growth and metabolism. Cell. 2006;124:471–484. doi: 10.1016/j.cell.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 113.Okuno S. Mammalian target of rapamycin inhibitors in sarcomas. Curr Opin Oncol. 2006;18:360–362. doi: 10.1097/01.cco.0000228742.72165.cf. [DOI] [PubMed] [Google Scholar]
- 114.Smolewski P. Recent developments in targeting the mammalian target of rapamycin (mTOR) kinase pathway. Anticancer Drugs. 2006;17:487–494. doi: 10.1097/00001813-200606000-00001. [DOI] [PubMed] [Google Scholar]
- 115.Sawada T, Okada T, Kubota K. Rapamycin inhibits the growth of cholangiocarcinoma cells in vitro. J Clin Oncol. 2007;25(Suppl 18):15153. [Google Scholar]
- 116.Herberger B, Puhalla H, Lehnert M, Wrba F, Novak S, Brandstetter A, Gruenberger B, Gruenberger T, Pirker R, Filipits M. Activated mammalian target of rapamycin is an adverse prognostic factor in patients with biliary tract adenocarcinoma. Clin Cancer Res. 2007;13:4795–4799. doi: 10.1158/1078-0432.CCR-07-0738. [DOI] [PubMed] [Google Scholar]
- 117.Sridhar SS, Hedley D, Siu LL. Raf kinase as a target for anticancer therapeutics. Mol Cancer Ther. 2005;4:677–685. doi: 10.1158/1535-7163.MCT-04-0297. [DOI] [PubMed] [Google Scholar]
- 118.Fukushima T, Suzuki S, Mashiko M, Ohtake T, Endo Y, Takebayashi Y, Sekikawa K, Hagiwara K, Takenoshita S. BRAF mutations in papillary carcinomas of the thyroid. Oncogene. 2003;22:6455–6457. doi: 10.1038/sj.onc.1206739. [DOI] [PubMed] [Google Scholar]
- 119.Davies H, Bignell GR, Cox C, Stephens P, Edkins S, Clegg S, Teague J, Woffendin H, Garnett MJ, Bottomley W, et al. Mutations of the BRAF gene in human cancer. Nature. 2002;417:949–954. doi: 10.1038/nature00766. [DOI] [PubMed] [Google Scholar]
- 120.Tannapfel A, Sommerer F, Benicke M, Katalinic A, Uhlmann D, Witzigmann H, Hauss J, Wittekind C. Mutations of the BRAF gene in cholangiocarcinoma but not in hepatocellular carcinoma. Gut. 2003;52:706–712. doi: 10.1136/gut.52.5.706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Wilhelm SM, Carter C, Tang L, Wilkie D, McNabola A, Rong H, Chen C, Zhang X, Vincent P, McHugh M, et al. BAY 43-9006 exhibits broad spectrum oral antitumor activity and targets the RAF/MEK/ERK pathway and receptor tyrosine kinases involved in tumor progression and angiogenesis. Cancer Res. 2004;64:7099–7109. doi: 10.1158/0008-5472.CAN-04-1443. [DOI] [PubMed] [Google Scholar]
- 122.Gollob JA, Wilhelm S, Carter C, Kelley SL. Role of Raf kinase in cancer: therapeutic potential of targeting the Raf/MEK/ERK signal transduction pathway. Semin Oncol. 2006;33:392–406. doi: 10.1053/j.seminoncol.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 123.Liu L, Cao Y, Chen C, Zhang X, McNabola A, Wilkie D, Wilhelm S, Lynch M, Carter C. Sorafenib blocks the RAF/MEK/ERK pathway, inhibits tumor angiogenesis, and induces tumor cell apoptosis in hepatocellular carcinoma model PLC/PRF/5. Cancer Res. 2006;66:11851–11858. doi: 10.1158/0008-5472.CAN-06-1377. [DOI] [PubMed] [Google Scholar]
- 124.Höpfner M, Baradari V, Huether A, Scherübl H. Growth inhibition of human cholangiocarcinoma by sorafenib-based mono- and combination treatment. FASEB J. 2008;22:1136–1139. [Google Scholar]
- 125.Baradari V, Hopfner M, Huether A, Schuppan D, Scherubl H. Histone deacetylase inhibitor MS-275 alone or combined with bortezomib or sorafenib exhibits strong antiproliferative action in human cholangiocarcinoma cells. World J Gastroenterol. 2007;13:4458–4466. doi: 10.3748/wjg.v13.i33.4458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.El-Khoueiry AB, Rankin C, Lenz HJ, Philip P, Rivkin SE, Blanke CD. SWOG 0514: a phase II study of sorafenib (BAY 43-9006) as single agent in patients (pts) with unresectable or metastatic gallbladder cancer or cholangiocarcinomas. J Clin Oncol. 2007;25(20S):4639. [Google Scholar]
- 127.Roccaro AM, Hideshima T, Richardson PG, Russo D, Ribatti D, Vacca A, Dammacco F, Anderson KC. Bortezomib as an antitumor agent. Curr Pharm Biotechnol. 2006;7:441–448. doi: 10.2174/138920106779116865. [DOI] [PubMed] [Google Scholar]
- 128.Mitsiades CS, Mitsiades N, Hideshima T, Richardson PG, Anderson KC. Proteasome inhibitors as therapeutics. Essays Biochem. 2005;41:205–218. doi: 10.1042/EB0410205. [DOI] [PubMed] [Google Scholar]
- 129.Schwartz R, Davidson T. Pharmacology, pharmacokinetics, and practical applications of bortezomib. Oncology (Williston Park) 2004;18:14–21. [PubMed] [Google Scholar]
- 130.Brignole C, Marimpietri D, Pastorino F, Nico B, Di Paolo D, Cioni M, Piccardi F, Cilli M, Pezzolo A, Corrias MV, et al. Effect of bortezomib on human neuroblastoma cell growth, apoptosis, and angiogenesis. J Natl Cancer Inst. 2006;98:1142–1157. doi: 10.1093/jnci/djj309. [DOI] [PubMed] [Google Scholar]
- 131.Ustundag Y, Bronk SF, Gores GJ. Proteasome inhibition-induces endoplasmic reticulum dysfunction and cell death of human cholangiocarcinoma cells. World J Gastroenterol. 2007;13:851–857. doi: 10.3748/wjg.v13.i6.851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Fisher RI, Bernstein SH, Kahl BS, Djulbegovic B, Robertson MJ, de Vos S, Epner E, Krishnan A, Leonard JP, Lonial S, et al. Multicenter phase II study of bortezomib in patients with relapsed or refractory mantle cell lymphoma. J Clin Oncol. 2006;24:4867–4874. doi: 10.1200/JCO.2006.07.9665. [DOI] [PubMed] [Google Scholar]
- 133.Kane RC, Dagher R, Farrell A, Ko CW, Sridhara R, Justice R, Pazdur R. Bortezomib for the treatment of mantle cell lymphoma. Clin Cancer Res. 2007;13:5291–5294. doi: 10.1158/1078-0432.CCR-07-0871. [DOI] [PubMed] [Google Scholar]
- 134.Maki RG, Kraft AS, Scheu K, Yamada J, Wadler S, Antonescu CR, Wright JJ, Schwartz GK. A multicenter Phase II study of bortezomib in recurrent or metastatic sarcomas. Cancer. 2005;103:1431–1438. doi: 10.1002/cncr.20968. [DOI] [PubMed] [Google Scholar]
- 135.Kondagunta GV, Drucker B, Schwartz L, Bacik J, Marion S, Russo P, Mazumdar M, Motzer RJ. Phase II trial of bortezomib for patients with advanced renal cell carcinoma. J Clin Oncol. 2004;22:3720–3725. doi: 10.1200/JCO.2004.10.155. [DOI] [PubMed] [Google Scholar]
- 136.Shah MH, Young D, Kindler HL, Webb I, Kleiber B, Wright J, Grever M. Phase II study of the proteasome inhibitor bortezomib (PS-341) in patients with metastatic neuroendocrine tumors. Clin Cancer Res. 2004;10:6111–6118. doi: 10.1158/1078-0432.CCR-04-0422. [DOI] [PubMed] [Google Scholar]
- 137.Fanucchi MP, Fossella FV, Belt R, Natale R, Fidias P, Carbone DP, Govindan R, Raez LE, Robert F, Ribeiro M, et al. Randomized phase II study of bortezomib alone and bortezomib in combination with docetaxel in previously treated advanced non-small-cell lung cancer. J Clin Oncol. 2006;24:5025–5033. doi: 10.1200/JCO.2006.06.1853. [DOI] [PubMed] [Google Scholar]
- 138.O'Connor OA. Marked clinical activity of the proteasome inhibitor bortezomib in patients with follicular and mantle-cell lymphoma. Clin Lymphoma Myeloma. 2005;6:191–199. doi: 10.3816/CLM.2005.n.046. [DOI] [PubMed] [Google Scholar]
- 139.Hegewisch-Becker S, Sterneck M, Schubert U, Rogiers X, Guerciolini R, Pierce JE, Hossfeld DK. Phase I/II trial of botrezomib in patients with unresectable hepatocellular carcinoma. ASCO annual meeting proceedings. J Clin Oncol. 2004;22 Suppl 15:4089. [Google Scholar]