Abstract
Two years after the introduction of free antiretroviral therapy (ART) in Tanzania and in spite of the logistical support provided to facilitate clinic attendance, a considerable level of attrition from the program was identified among clients from a semi-rural ward. Qualitative research on ART patients’ health-seeking behavior identified factors affecting sustained attendance at treatment clinics. A mix of methods was used for data collection including semi-structured interviews with 42 clients and 11 service providers and 4 participatory group activities conducted with members of a post-test group between October and December 2006. A socio-ecological framework guided data analysis to categorize facilitators and barriers into individual, social, programmatic, and structural level influences, and subsequently explored their interaction and relative significance in shaping ART clients’ behavior. Our findings suggest that personal motivation and self-efficacy contribute to program retention, and are affected by other individual-level experiences such as perceived health benefits or disease severity. However, these determinants are influenced by others’ opinions and beliefs in the community, and constrained by programmatic and structural barriers. Individuals can develop the requisite willingness to sustain strict treatment requirements in a challenging context, but are more likely to do so within supportive family and community environments. Effectiveness and sustainability of ART roll-out could be strengthened by strategic intervention at different levels, with particular attention to community-level factors such as social networks’ influence and support.
Introduction
Despite the international health community’s initial concerns over whether antiretroviral therapy (ART) programs could be feasibly introduced within the widespread poverty of much of sub-Saharan Africa, treatment compliance in the region has sometimes exceeded rates found in richer countries.1-3 Notwithstanding that, adherence to ART in Africa is often poor and there are fears it could decrease over time.4 A recent meta-analysis covering 13 African countries suggests that approximately 40% of all ART clients might have died or discontinued treatment within 2 years of having initiated it.5 Sustaining life-long treatment might be particularly challenging for rural residents who need to travel regularly to major hospitals to obtain pill refills and undergo follow-up checks.
In Kisesa, a semi-rural ward of North Tanzania, a longitudinal surveillance and monitoring project (TAZAMA) is documenting the implementation of the national ART program, including its clinical impact and broader epidemiologic, demographic, and socioeconomic outcomes. As ART is being scaled-up, a parallel process of research is mapping ongoing community-level responses in order to identify emerging problems and inform the timely development of policy recommendations. At the onset of ART roll-out, formative research was conducted to identify and mitigate perceived and experienced barriers to treatment initiation among Kisesa residents.6 This early community-based research identified concerns over sustaining long-term treatment, transportation costs, and the referral hospital’s reputation for being unfriendly as key factors hampering accessibility to the Care and Treatment Clinic (CTC). A series of measures were consequently introduced by the program to alleviate practical and financial barriers, including the provisions of a fare to cover transportation costs and an “escort” from a community-based organization who accompanied clients during their first visit to the clinic. Furthermore, two nurses were hired at the CTC specifically to “meet and greet” Kisesa referrals and assist with clinical assessments and subsequent visits. These measures facilitated registration procedures and relieved anxiety related to attending the clinic for the first time. However, in spite of the support provided, a considerable level of attrition from the program was identified among clients from this ward at a 2-year follow-up.
The observational cohort study in which this research is nested offers an opportunity to track how ART provision has moved from a “pilot” phase in which we were able to identify how barriers to treatment initiation could be overcome on a small scale through resource-intensive interventions, to a scaled-up version where we can longitudinally assess longer term challenges faced by national ART programs.
Theoretical Framework
This study applied a social-ecological framework to the exploration of barriers and facilitators to sustained treatment adherence experienced by ART patients. Social-ecological theories situate individuals in a dynamic “social ecology”7 in which individuals adapt their behavior to their social environment and take decisions based on information, influence, and interactions available through local social networks, relationships, and institutions. At the same time, social structures and processes are shaped by the collective behavior of individuals, which can shift over time.8 Social ecological approaches eschew polarized debates between proponents of “individualist” versus “structuralist” models and instead argue that health promotion requires interventions at both levels, and that they represent two ends of a continuum rather than dualistic opposites.9
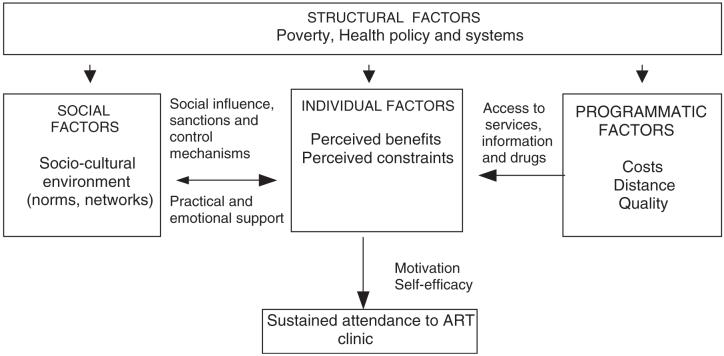
Drawing on formative research conducted in the same setting6 and the growing body of literature on ART programs in developing countries, the following social-ecological framework (Fig. 1) illustrates the factors underpinning treatment adherence at individual, community, programmatic and structural levels. The framework builds on existing theories to illustrate possible interactions between contextual and individual determinants and the pathways through which these affect health-seeking behavior. Data collection was subsequently guided by these categories in order to understand their relative importance and specific manifestations in the study setting.
FIG. 1.
Factors and pathways influencing sustained clinic attendance among antiretroviral therapy (ART) clients from a semi-rural area.
Theories that have focused on the individual’s behavioral decision-making consider how people determine whether they will engage in certain behavior.10,11 This process requires careful balancing of perceived benefits against constraints of adopting a particular course of action, and does not occur in a vacuum but rather reflects the availability of useful or accurate information and the wider social environment, including prevalent norms and the extent and supportiveness of social networks.8,9 Numerous studies have confirmed that the level of support received from family members and close social networks strongly influences individual behaviors and decisions regarding treatment.12-15 A South African study, for instance, found that receiving social support was instrumental in helping ART patients achieve compliance beyond the first 3 months of treatment.16
Program-level factors will also shape individuals’ cost-benefit analysis of seeking and sustaining treatment. The distance to medical services, financial and opportunity costs of travel, and quality of care such as waiting time, attitude of providers, and ease of following instructions for complex regimens have all been identified as determinants of treatment compliance.6,16-18 For example, in a study conducted in Uganda, Tanzania, and Botswana, the costs related to ART clinic attendance and long waiting times were identified as major obstacles to treatment adherence.19
Individuals thus formulate personal opinions and behavioural intentions while negotiating their social environment and the parameters of the ART program, and they do so against a broader structural background that, in much of sub-Saharan Africa, includes entrenched poverty, food insecurity, weakened health systems, and a lack of formalized social welfare mechanisms. One outcome of the interaction of all these social influences is individuals’ self-efficacy—confidence in being able to act on one’s decisions—that in the case of ART relates to the ability to identify a feasible treatment plan and remain compliant to it by persevering in the face of obstacles and integrating it into day-to-day routines.20 Evidence from several studies supports the central role played by self-efficacy in sustained treatment, as it has been found to be associated with decreased likelihood of missing scheduled appointments20 and higher levels of drug adherence.21-25
Methods
Part of a wider community-based cohort study monitoring Tanzania’s ART roll-out, this study used a qualitative approach to investigate the diversity and interplay of factors underlying attendance at ART clinics. A mix of methods was used including semi-structured interviews with 42 clients and 11 service providers and 4 participatory group activities conducted with members of a post-test group during routine monthly meetings. Research activities were recorded with permission, transcribed, and translated into English. Details on the study setting26 have been provided elsewhere. Ethical approval for the research was obtained from both the LSHTM Ethical Committee and the Tanzanian National Ethical Research Board.
Data were analyzed with the qualitative software package NVIVO-7 using the social-ecological framework as an initial coding guide, followed by detailed thematic content analysis to refine subthemes, make comparisons between cases, and identify contradictions and outliers. Relationship codes were created to analyze links between categories and respondents were classified by demographic variables to explore patterns by gender, residence, and age. Findings were triangulated through comparison across study participants as well as data collection method. Two researchers independently coded data and discussed emerging hypotheses, which were subsequently tested by rereading transcripts and fine-tuning the interpretation of coded themes to maximize rigor.
Results
Individual factors
In line with individual-level behavioral theories, perceptions of disease severity and susceptibility, as well as perceived benefits and barriers of staying on treatment, emerged as key determinants of clinic attendance. These were manifested as two primary psychological constructs: personal willingness (motivation) and perceived capacity (self-efficacy).
Most study participants reported having experienced positive physiologic outcomes from treatment, and this tended to increase motivation to stay on ART. Motivated patients trusted antiretroviral drugs, felt a sense of personal responsibility over their treatment, and perceived themselves to be capable of meeting its requirements despite difficulties encountered:
Because these drugs are giving me hope so that I may live, I have only to drag myself although it is far. (female, roadside area)
Even if you get a problem today, you will go there the following day and continue with the drugs because that medicine is your life. (Group activity, males from remote areas)
While some barriers to treatment were seen as beyond personal control, patients emphasized the need for individual persistence in the face of obstacles.
The obstacle is that, maybe when you are very sick, you can’t even walk. To come to the road, to go to the bus stand (...). You arrive there and you stay for a long time. I mean you are hungry and sick (...) at four o’clock you are just still there. Then it is far from here, I mean we get problems, but as you are in search for life, you have only to persevere. (female, roadside area)
However, among clients who were not experiencing physical recovery, “losing hope” could lead to attrition from the program. As mentioned by a group of men brainstorming about a typical community member on ART:
He is ignoring these drugs. Maybe he has used them without any good results, and hence he decided to quit using them completely. Our friend wanted to get better immediately ... (Group activity, males from remote areas)
Regaining health does not automatically lead to strengthened motivation, as in some cases it was interpreted as a sign of declining HIV severity, reducing a patient’s commitment to treatment adherence or leading to interrupted treatment:
... she was in a bad condition, she has used these drugs and her condition became well ... she felt that she was cured, hence there was no need of going to the clinic. It will make her think that she is well, she is just healthy and sound, she doesn’t feel any pain, and from there she will see those things as useless. (Group activity, females from remote areas)
Social factors
At the community level, the study examined how social norms and support from personal networks affected treatment patterns. First, it emerged that prevailing beliefs around the causes and basic etiology of HIV could reduce motivation for biomedical treatment. Beliefs that HIV is caused by witchcraft, and that it can be cured through spiritual healing and/or traditional medicine are common in Kisesa and other semirural communities in sub-Saharan Africa27,28 and can weaken confidence in ART effectiveness:
God is really able, He can really heal even AIDS. There were rashes on my face but the bishop laid his hands upon me and said that these rashes will disappear, and really after one day, I woke up in the morning of the following day and those rashes had disappeared completely. I think it was just the power of that faith in God that this problem is finished. (male, roadside area)
S/he thinks that Jesus has healed him/her and won’t attend clinic again. (home-based care provider)
I checked the chest and they said it was okay, this one is bewitched .... there is medicine sold in Arusha. It’s called “Ngetwa” ... For HIV ... They said it’s traditional, it’s obtained from the Masai in Arusha ... Ngetwa, people used to talk ... perhaps if we assist this person with Masai medicines, because he is tired of injections .... they said let’s go now to Arusha. (male, roadside area)
Misconceptions and rumors related to the antiretroviral drugs themselves also generate mistrust and confusion, negatively influencing the motivation for initiating therapy among potential patients, as well as contributing to treatment interruption among those already enrolled in the program:
Those drugs make them ... They cut, they really cut ... I mean people are just dying. You just find yourself dying. You die while you are just fat. That is just the belief. (female, roadside area)
Those medicines were so confusing. Sometimes you hear that if you use those medicines you will die. So it used to confuse people so much ... we used to fear it so much that it means if you take these medicines you may die. (male, roadside area)
In some cases, misunderstanding about the incompatability of certain behaviours with treatment, such as drinking alcohol, smoking cigarettes, or engaging in sex, could dishearten patients and lead to decreased levels of self-efficacy.
The other obstacle is that ... you actually go to the clinic, you start by being given the conditions about those drugs and you have a husband at home. When you go to involve your husband, the husband shuns away, you see, he doesn’t like. Now you start thinking that, when I start taking those drugs, it means that I will be just destroying them, you see, I will be using the drugs while at the same time I will be having sex with my husband, therefore there is nothing that I will be doing, it is better by 20 times that I do what? I quit ... (Group activity, females from roadside areas)
Concerning alcohol we were forbidden to take alcohol, if you are using alcohol you should now stop, so perhaps if you break those conditions and take alcohol then those medicines shall be ineffective. So you are not supposed to take alcohol, you are not supposed to smoke cigarette. (male, roadside area)
You shouldn’t take those drugs while at the same time you continue with sexual matters. (male, remote area)
She will first be hesitating ... should she continue with the drugs or should she continue having sex? (Group activity, females from remote areas)
While ambivalence and apprehension toward ART were part of the social environment, a more explicit influence on individuals’ decision-making came from the opinions of sexual partners, family members, friends, and influential community members. Social networks created powerful conduits for both support and discouragement vis-à-vis sustained treatment. Some ART clients dropped out from the program even after having been provided with accurate information at the health facilities when confronted with skepticism from influential peers:
The other thing is that, maybe you get a friend, then s/he starts telling you many things, maybe about AIDS. Then you start thinking: so there isn’t even that need of going to the clinic. That is also an obstacle ... You can get a friend who will start telling you a lot of words ... for example, they may just cheat you that it is AIDS, very many are being told that “you are just being cheated, they are just liars, just quit going to the clinic, what are you going to do there? Just stay at home and maintain your condition.” There are many who are being told so, then actually someone does what? s/he just stays at home. You can be tempted because we hear just many things (...) if they tell her that this is not a disease to be treated at the hospital, it is a disease that can be treated by traditional healers, then she will decide to go to the traditional healers ... (Group activity, females from remote areas)
... but now our clients they understand. But when they return to the community ... some people lie to them: “Ah those drugs are not good. If you take ART you will die and so and so.” But when they come here we are trying to give them information about it that this is not correct (...) some people there at the community, they don’t know their serostatus so they are trying to give our clients some rumors which are not true. (ART clinic staff)
Similarly, other people’s positive perception about ART and in particular the opinions of those already on therapy, influenced individuals’ decisions to test and stay on treatment.
There is a neighbor who told me that had been using them for a long period. Therefore he also told me that I should also go there to check my health. She took me there. I told her let’s go ... I started using these drugs and until now I am continuing using them. (female, roadside area)
Because of my health, I have taken four guys to the VCT center. I tell them “just go and check, sometimes you may think that it’s witches, but actually you are bewitching yourself” (...) they go ... they have started (ART). (male, road-side area)
The experience of directly observing improved health among other ART patients within one’s social network also positively influenced attitudes to treatment:
... when I saw my husband using them (ART) I decided to come to check too. (female, remote area)
... other patients who used to hide themselves have seen their fellows who come to these services are getting relief so they now turn up too. (ART clinic staff)
The level and source of interpersonal support, therefore, emerged as a significant catalyst for self-efficacy and sustained motivation. Treatment supporters (selected by patients as a prerequisite for enrollment in the national ART programme) and family members, including children, were often reported to be important sources of hope and courage and to help individuals integrate therapy into daily life by providing practical support such as reminding of appointments, cooking, bringing medicines home, etc.
I was there with my sister. They kept on giving me courage ... At present I know I can do everything, I am able. I just decided to choose them ... because in case I have problems they can help me. (female, roadside area)
While I was still serious he used to come daily ... He would help me even to look at my card. He would look at my return appointment date and say ‘ahaa, it’s not yet due.’ So when the date approaches he comes to remind me: “don’t forget to go.” I said “I won’t forget.” That’s how he was helping me, insisting to me: “the date is on the card. You can’t forget it.” We kept reciting it: “it’s a certain date.” (male, remote area)
... at home there is my child studying. If you have forgotten it (date of clinic appointment) you just ask him/her: what is today’s date?’ S/he’ll say “it is a certain date.” It’s not difficult; it’s just easy to me. (female, remote area)
It was that guy, that friend of mine ... he told me: “just continue taking the drugs, you shouldn’t have any worries, you will be just cultivating without any problem.” (male, roadside area)
She can be advised, she gets someone to encourage her to continue using those drugs ... Hope will come for one reason: she will get counseling. After getting counseling ... she will be committed, she will understand and she will continue ... (Group activity, females from remote areas)
Resource flows between network members serve as an important marker of social support in a context of entrenched rural poverty, and the ability to obtain financial assistance from a family member or close contact played a key role in individuals’ confidence that they could maintain a treatment program:
You will struggle to get that money, you will even go to your relative to ask him/her for money so that you may go to the clinic, you will go there and s/he will give you. (female, roadside area)
In addition to family members, the level of support received by other CTC clients, post-test club members and health professionals also emerged a factor contributing to retain clients in the ART program.
When I arrived there the doctor told me, “ooh you have been infected with the disease” ... after I received good instructions it encouraged me, I stopped worrying. It’s when I got courage. (female, roadside area)
So we enlightened each other, we met those using it and they said “I used to be in a very bad condition but right now I feel better, you come here walking so you are better.” I was satisfied because if you go to clinic you meet your fellow there so you exchange ideas. (male, roadside area).
While many study participants reported receiving family support, those that did not clearly suffered negative outcomes in their physical and psychological well-being. Perceived lack of family support led some individuals to drop-out from treatment altogether despite high levels of personal motivations to continue and evidence of physical recovery. When family members discouraged ART or suggested alternatives such as visiting religious preachers or traditional healers, patients were reluctant to pursue a biomedical solution further. Some could not sustain participation in the program without sufficient emotional or economic support:
Once you are segregated by your parents, where will you go? If you are being insulted scolded at home you can’t go everyday to the clinic. (Group activity, females from remote areas)
... there are others who are actually giving up hope, we see them even in their families ... they don’t have people to help them. (female, roadside area)
I had asked father for some money in the morning and he told me that we are tired of your diseases. (female, roadside area)
In extreme cases, the social influence of family members was so significant that relatives such as parents or husbands actually made the choices regarding treatment, including taking the decision to interrupt ART.
They tell him/her, aha, this disease has no cure so you are just wasting your time going to hospital. S/he comes to tell you again that “I was told at home ... that I should not go to hospital but I should go to church and I have answered them that I want to go to hospital.” That’s a problem too ... sometimes he/she wants to go and check CD4 but you find that the family takes him/her to traditional healers ... They say “these people just deceive you, you must be bewitched.” So when you return to that family you find that s/he is not there ... Most of such people we get them from a family that has got so many doubts so they have decided to take him/her to traditional healers. (home-based care provider)
You may find that perhaps a woman is forbiden by her husband. You might find that a woman is ready to go there but her husband tells her “but I don’t have that disease perhaps it’s you who has got it. And if you want to continue going there you should leave my place,” so the woman stops to go there for her CD4 results and there is no way of telling that woman to go for CD4 test again. (home-based care provider)
Maybe she may be having her partner at home who will prevent her, what are you going to do there? (Group activity, females from remote areas)
On the positive side, however, local home-based care providers were able to step in and provide a replacement social support network which contributed to client’s self-efficacy. In addition to providing direct assistance with travel or subsistence, home-based care staff was described by clients as providing a considerable level of encouragement both to ART patients themselves and also to their affected families, helping increase empathy.
... we arrived to a place (ART clinic) ... that woman (home-based care provider) was familiar with the place ... after getting that experience, I am now going alone. (male, roadside area)
The attendants will be coming at home to visit from time to time ... they will go to your parents and discuss with them and eventually it will come a stage when your parents will understand. (Group activity, females from remote areas)
She was telling the people at home: ‘you shouldn’t segregate this person because she is suffering from this and this, you should just be close to her’. Every time she was going there at home until her relatives became close. (Group activity, females from roadside areas)
Programmatic factors
The free provision of ART by the national Aids Control Program was mentioned as a factor contributing to increased self-efficacy:
When I heard that the drugs were available and that were being given for free, honestly I felt very pleased, I was very happy. That is why I wasn’t ashamed neither did I have a grudge of continuing to receive the drugs. (female, roadside area)
On the other hand, the distance to the clinic regularly came up as a barrier to clinic attendance, related to the inconvenience of travel, or the necessity of making the journey to the referral hospital during severe illness:
I was carried on a bicycle by father, I was serious, I was wearing a gown, I tied myself with a khanga, I was vomiting. After reaching the town I took a taxi to the clinic, after arriving to the clinic I fell down. (female, roadside area)
Almost all study participants suggested, without any prompting, that the service should be brought closer to the clients.
We would like the institutions to think of us, that they should build us hospitals nearby here so that we could get medicine. (female, remote area)
Access to information during the “adherence training” sessions conducted as part of the enrolment procedure seemed important to retention of clients. Mandatory participation of a “treatment partner” in the program often proactively addressed some of the community-level barriers, including skepticism and misconceptions about HIV and ART among family members:
At the beginning I felt that even if I ... maybe I can talk and be stigmatized at home. That is why I felt aah, it is better I just remain quiet. But when I started going to the clinic, when I attended classes, they knew everything, they were also educated, and my mother too ... now all of them know that I go to the clinic in town, they know that I have my clinic. (female, roadside area)
Structural factors
In the context of severe poverty of rural Tanzania, structural factors ultimately constrain individuals’ ability to sustain treatment. Difficulties in procuring transport fares, conflicting priorities on how to use any cash assistance provided through the programme, and inadequate nutrition levels all emerged as factors leading to delayed or missed appointments.
During all the participatory group discussions, structural factors were consistently ranked as posing the most intractable barriers to clinic attendance. Compared to these, social or behavioral determinants were listed as of lesser importance and more easily resolved.
From that ranking they said unanimously that the biggest problems they face at the time of going to the clinic are food and fare. Those are the leading obstacles that they mentioned. They further added that the other obstacles are normal, and they can solve them by working and collaborating with their relatives and friends. (notes from group activity with males from roadside areas).
When considering what might lead a “typical ART client” to drop-out from the ART program, study participants presented a clear analysis of how individual level facilitators, such as “regaining health” could be stymied by barriers at the social level through lack of family support or prevailing beliefs among relevant social networks that HIV could be cured through other means. This tension played out against a backdrop of structural constraints, further mitigating against successful achievement of individual behavioral intentions:
And when she goes to the clinic she uses her own ways, she goes to the clinic and she gets those drugs, and when she brings them at home, she has to take them secretly. Now she starts asking herself, “there is a day when I will be discovered here,” now when she regains her health somehow, she thinks that she is cured, she decides to quit taking the drugs. She actually quits. (Group activity, females from road-side areas)
Discussion
Many studies have focused on structural barriers to successful treatment compliance, highlighting how inadequate nutrition, costly transport options, and the opportunity costs of spending time seeking care pose insurmountable obstacles to many HIV-positive people in a range of developing countries, including Tanzania.19,29-31 Such findings have led some to suggest that structural, rather than behavioral, interventions may be the most useful to ensure optimal treatment program.32
Our findings suggest, however, that while structural factors do significantly restrict individuals’ ability to comply with treatment, even when some of these barriers are alleviated (through free provision of ART and transport costs) important challenges to sustained clinic attendance persist. While removing structural obstacles is essential, addressing sociocultural and psychosocial factors is also required.
Through the application of a social-ecological framework to piece together the multiplicity of levels at which facilitators and barriers to health-seeking interact, our study demonstrates how individuals adjust their behavior to their immediate social environment. The process through which other’s people’s behaviors, advice, and beliefs determine health behavior (social influence) emerges as a main pathway for individual decision-making and reflects localized norms and levels of support within individuals’ social networks. The strength of social influence could act as a powerful motivator and strengthen an ART patient’s self-efficacy to overcome other barriers, or could severely undermine capacity to follow through an intention to remain on treatment, leading to dropping out from the program. This finding reinforces similar results regarding the role of family and community social support on adherence from a range of studies conducted in both developed and developing countries.33-36
As such, proactive efforts to engage with patients’ social networks could be a useful strategy for improving retention rates. In highly family-centered, yet resource-poor, settings, social capital assets are central to survival and thus families and other network members are likely to play a much greater role in health-seeking decisions than in more individualistic societies with solid institutional safety nets. Activities that already appear successful such as educating and sensitizing family members through home based care workers could be expanded, as could capitalizing on ART patients’ own ability to influence beliefs and social norms within their social networks, and to offer referrals to the program as well as practical advice on overcoming barriers to treatment.
At programmatic level, other possible implications from the research include experimenting with community based ART distribution approaches to limit the physical exertion, inconvenience, and financial and time costs of regular travel to the CTC clinic. In South Africa, trials are underway of ART provision through community lay health workers (F.P. Lewin, personal communication). It might also be worth taking a harm reduction approach to alcohol and tobacco use rather than conveying strong disapproval during medical advice and training sessions given by CTC staff in adherence training; similarly, acknowledging ART patients’ sexuality and local sexual norms may improve acceptability of risk reduction messages; these, in turn, should take into consideration that most people on ART will neither wish nor be in a position to give up regular sexual relations.
To conclude, individual psychosocial attributes, including motivation and self-efficacy, affect sustained adherence to ART programs over a prolonged period of time, but are dependent on the interaction of other determinants that operate at different levels. Using a social-ecological framework to investigate and analyze the links and relative roles of individual, social, programmatic and ultimately structural factors can help identify feasible “entry points” for interventions to improve program retention and compliance in a specific context. Similar approaches have been used in developing multi-level interventions for HIV prevention programs, and this study demonstrates its useful application to seeking and sustaining ART.
Acknowledgments
We wish to thank the directors of the National Institute for Medical Research, Mwanza, and the ART clinic at Bugando Medical Centre for the support provided to conduct this study. We also want to thank the VCT counselors Rose Manyala and Esther Mwinuka for facilitating the recruitment of participants as well as all the respondents participating in this research for their time and the valuable information provided. Funded by the Global Fund for Aids, Tuberculosis and Malaria (GFATM) and the Wellcome Trust.
Footnotes
Author Disclosure Statement
No competing interests exist.
References
- 1.Coetzee D, Boulle A, Hildebrand K, Asselman V, Van Cutsem G, Goemaere E. Promoting adherence to antiretroviral therapy: the experience from a primary care setting in Khayelitsha, South Africa. AIDS. 2004;18(Suppl 3):S27–31. doi: 10.1097/00002030-200406003-00006. [DOI] [PubMed] [Google Scholar]
- 2.Mills EJ, Nachega JB, Buchan I, et al. Adherence to antiretroviral therapy in sub-Saharan Africa and North America: A meta-analysis. JAMA. 2006;296:679–690. doi: 10.1001/jama.296.6.679. [DOI] [PubMed] [Google Scholar]
- 3.Orrell C, Bangsberg DR, Badri M, Wood R. Adherence is not a barrier to successful antiretroviral therapy in South Africa. AIDS. 2003;17:1369–1375. doi: 10.1097/00002030-200306130-00011. [DOI] [PubMed] [Google Scholar]
- 4.Gill CJ, Hamer DH, Simon JL, Thea DM, Sabin LL. No room for complacency about adherence to antiretroviral therapy in sub-Saharan Africa. AIDS. 2005;19:1243–1249. doi: 10.1097/01.aids.0000180094.04652.3b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rosen S, Fox MP, Gill CJ. Patient retention in antiretroviral therapy programs in sub-Saharan Africa: A systematic review. PLoS Med. 2007;4:e298. doi: 10.1371/journal.pmed.0040298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mshana GH, Wamoyi J, Busza J, et al. Barriers to accessing antiretroviral therapy in Kisesa, Tanzania: A qualitative study of early rural referrals to the national program. AIDS Patient Care STDs. 2006;20:649–657. doi: 10.1089/apc.2006.20.649. [DOI] [PubMed] [Google Scholar]
- 7.Murphy E. Promoting Healthy Behavior. Population. Reference Bureau; Washington, D.C.: 2005. (Health Bulletin, 2). [Google Scholar]
- 8.Latkin CA, Knowlton AR. Micro-social structural approaches to HIV prevention: A social ecological perspective. AIDS Care. 2005;17:S102–113. doi: 10.1080/09540120500121185. [DOI] [PubMed] [Google Scholar]
- 9.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31:143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 10.Fishbein M. The role of theory in HIV prevention. AIDS Care. 2000;12:273–278. doi: 10.1080/09540120050042918. [DOI] [PubMed] [Google Scholar]
- 11.Noar SM. An interventionist’s guide to AIDS behavioral theories. AIDS Care. 2007;19:392–402. doi: 10.1080/09540120600708469. [DOI] [PubMed] [Google Scholar]
- 12.Alfonso V, Geller J, Bermbach N, Drummond A, Montaner JS. Becoming a “treatment success”: What helps and what hinders patients from achieving and sustaining undetectable viral loads. AIDS Patient Care STDs. 2006;20:326–334. doi: 10.1089/apc.2006.20.326. [DOI] [PubMed] [Google Scholar]
- 13.Ammassari A, Trotta MP, Murri R, et al. Correlates and predictors of adherence to highly active antiretroviral therapy: Overview of published literature. J Acquir Immune Defic Syndr. 2002;31:S123–127. doi: 10.1097/00126334-200212153-00007. [DOI] [PubMed] [Google Scholar]
- 14.Remien RH, Bastos FI, Jnr VT, et al. Adherence to antiretroviral therapy in a context of universal access, in Rio de Janeiro, Brazil. AIDS Care. 2007;19:740–748. doi: 10.1080/09540120600842516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van Servellen G, Lombardi E. Supportive relationships and medication adherence in HIV-infected, low-income Latinos. West J Nurs Res. 2005;27:1023–1039. doi: 10.1177/0193945905279446. [DOI] [PubMed] [Google Scholar]
- 16.Nachega JB, Knowlton AR, Deluca A, et al. Treatment supporter to improve adherence to antiretroviral therapy in HIV-infected South African adults. A qualitative study. J Acquir Immune Defic Syndr. 2006;43(Suppl 1):S127–133. doi: 10.1097/01.qai.0000248349.25630.3d. [DOI] [PubMed] [Google Scholar]
- 17.Monreal MT, da Cunha RV, Trinca LA. Compliance to antiretroviral medication as reported by AIDS patients assisted at the University Hospital of the Federal University of Mato Grosso do Sul. Braz J Infect Dis. 2002;6:8–14. doi: 10.1590/s1413-86702002000100002. [DOI] [PubMed] [Google Scholar]
- 18.Stout BD, Leon MP, Niccolai LM. Nonadherence to antiretroviral therapy in HIV-positive patients in Costa Rica. AIDS Patient Care STDs. 2004;18:297–304. doi: 10.1089/108729104323076034. [DOI] [PubMed] [Google Scholar]
- 19.Hardon AP, Akurut D, Comoro C, et al. Hunger, waiting time and transport costs: Time to confront challenges to ART adherence in Africa. AIDS Care. 2007;19:658–665. doi: 10.1080/09540120701244943. [DOI] [PubMed] [Google Scholar]
- 20.Johnson MO, Neilands TB, Dilworth SE, Morin SF, Remien RH, Chesney MA. The role of self-efficacy in HIV treatment adherence: validation of the HIV Treatment Adherence Self-Efficacy Scale (HIV-ASES) J Behav Med. 2007;30:359–370. doi: 10.1007/s10865-007-9118-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Catz SL, Kelly JA, Bogart LM, Benotsch EG, McAuliffe TL. Patterns, correlates, and barriers to medication adherence among persons prescribed new treatments for HIV disease. Health Psychol. 2000;19:124–133. [PubMed] [Google Scholar]
- 22.Gifford AL, Bormann JE, Shively MJ, Wright BC, Richman DD, Bozzette SA. Predictors of self-reported adherence and plasma HIV concentrations in patients on multidrug antiretroviral regimens. J Acquir Immune Defic Syndr. 2000;23:386–395. doi: 10.1097/00126334-200004150-00005. [DOI] [PubMed] [Google Scholar]
- 23.Johnson MO, Catz SL, Remien RH, et al. Theory-guided, empirically supported avenues for intervention on HIV medication nonadherence: Findings from the Healthy Living Project. AIDS Patient Care STDs. 2003;17:645–656. doi: 10.1089/108729103771928708. [DOI] [PubMed] [Google Scholar]
- 24.Kalichman SC, Rompa D, DiFonzo K, et al. HIV treatment adherence in women living with HIV/AIDS: Research based on the Information-Motivation-Behavioral Skills model of health behavior. J Assoc Nurses AIDS Care. 2001;12:58–67. doi: 10.1016/S1055-3290(06)60217-3. [DOI] [PubMed] [Google Scholar]
- 25.Seidl EM, Melchiades A, Farias V, Brito A. Persons living with HIV/AIDS: factors associated with adherence to antiretroviral treatment. Cad Saude Publica. 2007;23:2305–2316. doi: 10.1590/s0102-311x2007001000006. [DOI] [PubMed] [Google Scholar]
- 26.Boerma JT, Urassa M, Senkoro K, Klokke A, Ngweshemi JZ. Spread of HIV infection in a rural area of Tanzania. AIDS. 1999;13:1233–1240. doi: 10.1097/00002030-199907090-00013. [DOI] [PubMed] [Google Scholar]
- 27.Plummer ML, Mshana G, Wamoyi J, et al. ‘The man who believed he had AIDS was cured’: AIDS and sexually-transmitted infection treatment-seeking behaviour in rural Mwanza, Tanzania. AIDS Care. 2006;18:460–466. doi: 10.1080/09540120500220367. [DOI] [PubMed] [Google Scholar]
- 28.Wanyama J, Castelnuovo B, Wandera B, et al. Belief in divine healing can be a barrier to antiretroviral therapy adherence in Uganda. AIDS. 2007;21:1486–1487. doi: 10.1097/QAD.0b013e32823ecf7f. [DOI] [PubMed] [Google Scholar]
- 29.Au JT, Kayitenkore K, Shutes E, et al. Access to adequate nutrition is a major potential obstacle to antiretroviral adherence among HIV-infected individuals in Rwanda. AIDS. 2006;20:2116–2118. doi: 10.1097/01.aids.0000247580.16073.1b. [DOI] [PubMed] [Google Scholar]
- 30.Byakika-Tusiime J, Oyugi JH, Tumwikirize WA, Katabira ET, Mugyenyi PN, Bangsberg DR. Adherence to HIV antiretroviral therapy in HIV+Ugandan patients purchasing therapy. Int J STD AIDS. 2005;16:38–41. doi: 10.1258/0956462052932548. [DOI] [PubMed] [Google Scholar]
- 31.Weiser S, Wolfe W, Bangsberg D, et al. Barriers to antiretroviral adherence for patients living with HIV infection and AIDS in Botswana. J Acquir Immune Defic Syndr. 2003;34:281–288. doi: 10.1097/00126334-200311010-00004. [DOI] [PubMed] [Google Scholar]
- 32.Crane JT, Kawuma A, Oyugi JH, et al. The price of adherence: qualitative findings from HIV positive individuals purchasing fixed-dose combination generic HIV antiretroviral therapy in Kampala, Uganda. AIDS Behav. 2006;10:437–442. doi: 10.1007/s10461-006-9080-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Campero L, Herrera C, Kendall T, Caballero M. Bridging the gap between antiretroviral access and adherence in Mexico. Qual Health Res. 2007;17:599–611. doi: 10.1177/1049732307301335. [DOI] [PubMed] [Google Scholar]
- 34.Davies G, Koenig LJ, Stratford D, et al. Overview and implementation of an intervention to prevent adherence failure among HIV-infected adults initiating antiretroviral therapy: Lessons learned from Project HEART. AIDS Care. 2006;18:895–903. doi: 10.1080/09540120500329556. [DOI] [PubMed] [Google Scholar]
- 35.Diabate S, Alary M, Koffi CK. Determinants of adherence to highly active antiretroviral therapy among HIV-1-infected patients in Cote d’Ivoire. AIDS. 2007;21:1799–1803. doi: 10.1097/QAD.0b013e3282a5667b. [DOI] [PubMed] [Google Scholar]
- 36.Kumarasamy N, Safren SA, Raminani SR, et al. Barriers and facilitators to antiretroviral medication adherence among patients with HIV in Chennai, India: A qualitative study. AIDS Patient Care STDs. 2005;19:526–537. doi: 10.1089/apc.2005.19.526. [DOI] [PubMed] [Google Scholar]