Abstract
Community-based interventions are an important component of obesity prevention efforts. The literature provides little guidance on priority-setting for obesity prevention in communities, especially for socially and culturally diverse populations. This paper reports on the process of developing prioritized, community-participatory action plans for obesity prevention projects in children and adolescents using the ANGELO (Analysis Grid for Elements Linked to Obesity) Framework. We combined stakeholder engagement processes, the ANGELO Framework (scans for environmental barriers, targeted behaviours, gaps in skills and knowledge) and workshops with key stakeholders to create action plans for six diverse obesity prevention projects in Australia (n = 3), New Zealand, Fiji and Tonga from 2002 to 2005. Some sites included sociocultural contextual analyses in the environmental scans. Target groups were under-5-year-olds (Australia), 4–12-year-olds (Australia) and 13–18-year-olds (all four countries). Over 120 potential behavioural, knowledge, skill and environmental elements were identified for prioritization leading into each 2-day workshop. Many elements were common across the diverse cultural communities; however, several unique sociocultural elements emerged in some cultural groups which informed their action plans. Youth were actively engaged in adolescent projects, allowing their needs to be incorporated into the action plans initiating the process of ownership. A common structure for the action plan promoted efficiencies in the process while allowing for community creativity and innovation. The ANGELO is a flexible and efficient way of achieving an agreed plan for obesity prevention with diverse communities. It is responsive to community needs, combines local and international knowledge and creates stakeholder ownership of the action plan.
Keywords: childhood, obesity prevention, action plan
INTRODUCTION
To control the burgeoning childhood obesity epidemic, long-term comprehensive programs have the greatest potential. These are programs that introduce settings-based policies, address underlying social and cultural contextual factors and use multiple strategies in multiple settings and sectors that are applied in a collaborative manner (Kumanyika et al., 2002; WHO, 2003; Doak et al., 2006). The need to address underlying sociocultural factors is often overlooked but important because they influence eating and physical activity behaviours (Kumanyika, 1993; Mavoa, 2006) as well as attitudes to body size (Becker, 1995; Ricciardelli and McCabe, 2003).
Much of the evidence for obesity prevention stems from a modest number of published intervention studies, most of which have not been comprehensive in their approach, rather, they have focused on single strategies (mainly education; increasing the level of physical activity in school) set in a single setting (mainly primary schools) and few have demonstrated an impact on target groups (Jain, 2005; Summerbell et al., 2005; Doak et al., 2006). Thus, there is little guidance in the literature on what concrete actions can be taken to prevent childhood obesity at a community level, especially for socially and culturally diverse populations. This lack of evidence and the complexity of implementing a comprehensive approach to obesity prevention makes priority setting for effective action to control the obesity epidemic an enormous challenge (Swinburn et al., 2005), although the processes used for prioritizing actions in other areas (Hawe et al., 1990; National Public Health Partnership, 2000; Bartholomew et al., 2001, Carter, 2001; Green and Kreuter, 2005) can be applied to obesity prevention.
The complex process of prioritizing strategies, implementing actions and evaluating impacts can be tested with demonstration communities where initial resources and research expertise can be focused into a defined sociocultural and geographical area. Based on this rationale, we have supported several whole-of-community demonstration projects for obesity prevention and assisted the communities to set priorities for action.
The planning process has been built around the ANGELO Framework (Analysis Grid for Environments Linked to Obesity) which was originally developed by Swinburn et al. (Swinburn et al., 1999) to categorize the various components of the obesogenic environment into two sizes of environment (micro/settings and macro/sectors) and four types of environments (physical, economic, policy and sociocultural). The framework has since been integrated into an environmental research framework for weight gain prevention (Kremers et al., 2006) and expanded as an assessment tool for environmental determinants of obesity (Swinburn et al., 1999; Swinburn, 2004). The framework has also been used as an assessment tool for potential interventions (WHO, 2002), a classification system for systematic reviews of the obesogenic environment (Ferreira et al., 2007; van der Horst et al., 2007; Wendel-Vos et al., 2007) and on urban health and healthy weights (Raine et al, 2008); and as a guide to scanning individual behaviours for action (Egger et al., 2007). In this paper, we describe the use of the framework as part of the priority setting process for obesity prevention action in communities. The widening use of the ANGELO Framework has, therefore, led us to swap the ‘E’ from ‘Environments’ to ‘Elements’ so that ANGELO now stands for Analysis Grids for Elements Linked to Obesity.
This priority-setting process (which we called the ANGELO Process because of the central use of the ANGELO Framework) is described here, drawing on our experiences across six whole-of-community obesity prevention projects for children and adolescents in four countries [Australia (3), New Zealand, Fiji and Tonga]. The ANGELO Process is evidence- and practice-based (Green, 2001; Rychetnik et al., 2004; Smith et al., 2006). It follows the principles and action areas of health promotion (Green and Kreuter, 2005; McKenzie et al.,2005; Keleher et al., 2007) and the processes of priority setting where ‘technical assessments’ (evidence from the literature, local evidence and experience, specific analyses or targeted research) are included in a due process (engagement with the key stakeholders, joint and transparent decision-making) so that agreed priorities are reached (Pickett and Hanlon, 1990; National Public Health Partnership, 2000; Carter, 2001; Green and Kreuter, 2005; Swinburn et al., 2006).
METHODS
Obesity prevention demonstration projects
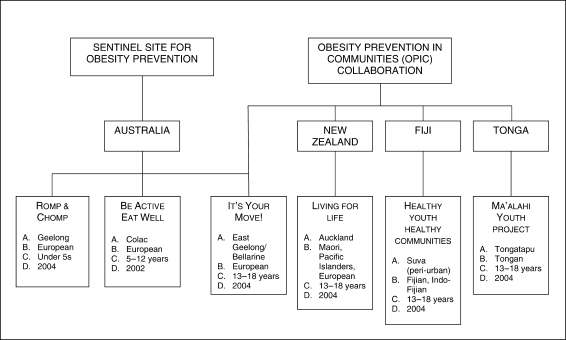
The structure of the six whole-of-community demonstration projects is outlined in Figure 1. Three projects are part of the Sentinel Site for Obesity Prevention (Barwon South-West region of Victoria, Australia). One Australian project and the three projects in New Zealand, Fiji and Tonga targeted 12–18-year-olds. These four adolescent projects are part of the Obesity Prevention in Communities (OPIC) collaboration. All projects were initiated from normative needs (Bradshaw, 1972), based on the opinion and experience of experts according to current research and findings.
Fig. 1:
Six whole-of-community demonstration projects for obesity prevention established in four countries, supported by the Sentinel Site for Obesity Prevention and Obesity Prevention in Communities Project (OPIC) Collaboration. (A) Location; (B) main cultural groups; (C) target age groups; (D) year commenced.
The demonstration projects, detailed elsewhere, were quasi-experimental and used a variety of designs to concurrently assess appropriate comparison groups (Schultz et al., 2007; Swinburn et al, 2007).
All intervention sites were purposively chosen. Projects incorporated a 1-year planning period including community engagement, the development of the action plan with the communities and the collection of baseline data; and a 3-year intervention period based on capacity building principles (New South Wales Health, 2001; Smith et al, 2006) before administering repeat measurements.
The priority setting process
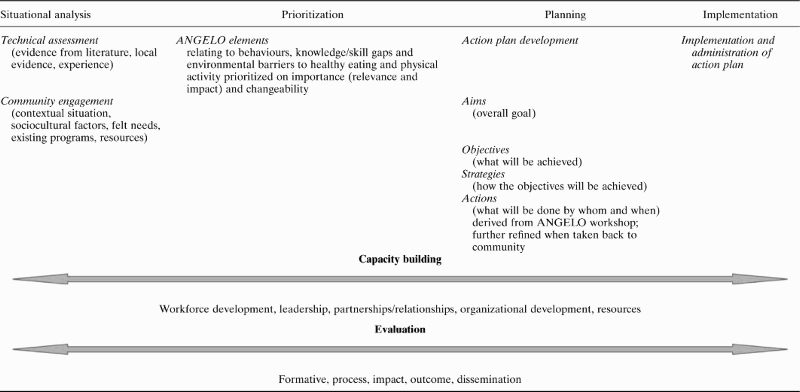
This process (hereafter referred to as the ANGELO Process) occurred in four phases: (i) sociocultural analyses (outside Australia); (ii) stakeholder engagement; (iii) a stakeholder workshop to confirm and assess the elements in the ANGELO Framework; and (iv) creation of the draft action plan. The ‘elements’ in the framework refer to a list of potential target behaviours, potential knowledge and skill gaps to address and potential environmental barriers to overcome. Together, these four phases made up the initial stages of the full health promotion process (Hawe et al., 1990; Green and Kreuter, 2005; McKenzie et al.,2005; Keleher et al., 2007) by incorporating needs assessments, prioritization, early planning stages as well as contributing to capacity building and formative evaluation (Table 1).
Table 1:
The overall health promotion process: the ANGELO Process covers the situational analysis, prioritization and planning phases and contributes to building capacity and formative evaluation
 |
Sociocultural analyses
Preliminary sociocultural studies were conducted in New Zealand, Fiji and Tonga to identify key sociocultural barriers to achieve healthy eating (such as traditions of over-eating on social occasions), regular physical activity (such as expectations on girls to do household tasks rather than play sport) and healthy body size (such as equating large body sizes with being cared for). Sociocultural interviews were not conducted in Australia because the sampling frame was primarily Australian European and there was considerable literature on which to draw (McCabe and Ricciardelli, 2001; Ricciardelli and McCabe, 2003; Brown and Trost, 2003; Burton et al., 2003; Bell and Swinburn, 2004; Hesketh et al., 2005; Franklin et al, 2006) and sociocultural factors were considered to be more dominant in the Pacific populations (Pollock, 1992; Coyne, 2000; Khaleghian, 2003). In Fiji and Tonga, semi-structured interviews were conducted with six females and six males aged 12–18 years per cultural group (Tongans in Tonga, Indo-Fijians and indigenous Fijians in Fiji). Interviews were conducted and audio-taped by an interviewer fluent in the first language of the participant, then transcribed and translated where necessary. Researchers representing each cultural group initially worked separately then together to identify sociocultural factors. In New Zealand, six focus groups were conducted with 79 adolescents, with the groups differentiated on the basis of gender and cultural group (Samoan, Tongan, Maori). Preliminary analysis from the interviews and focus groups identified elements that were incorporated into the respective ANGELO Framework and were presented back to communities before or during the stakeholder workshops.
Stakeholder engagement
The engagement component involved advocacy for the project through initial discussions with people in the organizations related to the target settings (schools), relevant government agencies (health and education departments) and other key local organizations (churches and local government). Discussions with ‘champions’ or people visible and influential in the communities also occurred through a ‘snowballing’ process. Additionally, the elements to be prioritized at the workshop were listed (potential behaviours, knowledge and skill gaps and environmental barriers) and discussed to obtain feedback on inclusiveness and language used.
Prioritization workshop
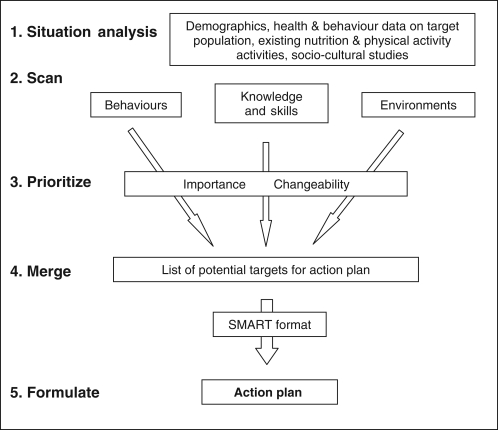
A 2-day stakeholder workshop was conducted to finalize and prioritize the ANGELO elements and develop a draft action plan. The workshops were facilitated by researchers with community-based obesity prevention expertise and occurred in five stages (Figure 2). Participants were representatives from key stakeholder organizations and included student representatives for the four adolescent projects, who for some of the workshops, were in the majority.
Fig. 2:
The ANGELO Process to identify priority elements for inclusion into an agreed action plan. SMART stands for Specific, Measurable, Achievable, Relevant, and Time-bound (as attributes of good objectives).
The situational analysis involved presenting and discussing data collected from the technical assessments and community consultations (e.g. what programs are already operating). In the scanning phase (stage two), workshop participants were asked to consider key behaviours to target, knowledge and skill gaps related to the behaviours to be addressed (e.g. misunderstandings about the role of breakfast in maintaining a healthy weight), and environmental barriers (including sociocultural elements) to be considered. These elements, presented in worksheets, had been modified for each community according to available evidence and feedback from the community (described above) and were subsequently checked with workshop participants. The scanning then involved briefly discussing each element to ensure a common understanding and to identify any new elements that were relevant to each community.
The prioritization process (stage three) involved a scoring process that used a five-point scale where potential elements were scored for importance (what is the relevance and impact of this in our situation?; 1=‘not important’ to 5=‘extremely important’) and changeability (how easy or hard is this element to change in our situation?; 1=‘very hard to change’ to 5=‘very easy to change’). Rating scores for importance and changeability were multiplied to give a total score for each of the elements, and then ranked giving five points for the highest ranked to one point for the fifth ranked (no ties were allowed). Collated scores prioritized the elements for incorporation into the action plan.
Within settings relevant to the community (e.g. homes, schools, neighbourhoods and churches), environmental barriers were scanned (as above) and prioritized in terms of food, physical activity and body size preferences under the following environment type: physical (what is/is not available?), economic (what are the financial factors?), policy (what are the rules?) and sociocultural (what are the attitudes, beliefs, perceptions, values, expectations, practices?) (Swinburn et al., 1999).
Drafting the action plan
The merge (stage four) pulled together the highest ranked behavioural, knowledge, skill and environmental elements in the key settings (about 6–8 for each) as top targets for action. These were discussed by participants, and in the final step, the agreed priority elements were moulded into a structured action plan (stage five). The behaviours were generally used to create the objectives, and the associated knowledge gaps and environmental barriers were used to identify the strategies.
When formulating the action plan, guidance was provided by the facilitator around developing an overall aim or goal (a statement that explains the project and states the target group; measured as the project's outcome); writing SMART [Specific, Measurable, Achievable, Relevant, Time-bound, (Round et al., 2005)] objectives and developing strategies. Participants were encouraged to brainstorm a name for their project if time permitted, otherwise a name was chosen later by the community.
RESULTS
Sociocultural analyses
The key sociocultural findings that informed the relevant ANGELO worksheets were presented at their workshops. Table 2 shows an overview of the key findings from the one-on-one interviews conducted with three cultural groups in Fiji (indigenous Fijians and IndoFijians) and Tonga. It is not possible to compare these with the focus group findings conducted in Auckland, given the different methodology. Many key factors were common to all three cultural groups; for example, family members provided important messages about food, physical activity and body size that both supported and inhibited a healthy lifestyle. Culturally specific sociocultural factors included the perceived influence of the media on body-size preferences (greater for IndoFijians) and the prioritization of study over recreation (IndoFijians) (Cama, 2006, unpublished report; Mavoa et al., 2007).
Table 2:
Key sociocultural findings that informed the ANGELO workshops in Fiji and Tonga (the dots identify elements noted by at least 50% of interviewees)
| List of sociocultural elements | Fijians | Indo-Fijians | Tongans |
|---|---|---|---|
| Food and eating | |||
| Knew about healthy and unhealthy food and drinks | • | • | • |
| Favourite foods and drinks high in fat and/or sugar | • | • | |
| Often skipped breakfast, especially females | • | • | |
| Mothers and grandmothers provided most messages about food at home | • | • | • |
| Peers influenced school food by sharing | • | • | • |
| Unmonitored spending money to purchase junk food | • | • | |
| Physical activity | |||
| More males exercised than females | • | • | • |
| Males perceived to have more freedom for recreational activities | • | • | |
| Safety seen as a barrier for females’ recreational activities | • | • | |
| Chores limited females’ recreational activities | • | • | |
| Study (school) seen as a barrier to recreational activities | • | • | |
| Families provided messages about physical activity (PA), especially fathers | • | • | |
| Older siblings and cousins encouraged PA | • | ||
| Peers provided messages about PA | • | • | |
| Sports and sports stars provided messages about PA, especially for males | • | • | |
| Body size preferences | |||
| Body size preference ‘not too skinny, not too fat’ | • | • | |
| Males wanted to increase weight or muscle | • | • | |
| Parents provided messages about ideal weight | • | • | |
| Older siblings and cousins provided messages about ideal weight | • | • | |
| Peers provided messages about ideal weight | • | • | |
| The media provided messages about ideal weight | • | • | |
Stakeholder engagement
This period of advocacy and engagement took about 6–12 months and was critical for ensuring key stakeholder organizations were engaged in the proposed projects and were able to work collaboratively to develop an action plan. (In the Pacific, once project staff are accepted, strong long-term stakeholder relationships are developed.) Community members provided valuable information on the context of their community and key settings, and about existing programs, networks and resources to support the project. In some instances, Members of Parliament and religious leaders (particularly in Fiji and Tonga) were engaged. Key champions (e.g. teachers, local sporting champions) were identified by key stakeholders as those who were visible or influential in communities. In general, stakeholders were enthusiastic about the projects’ objectives to improve healthy eating and physical activity and readily engaged in the consultation processes. Some concerns, however, were raised by communities and schools during this consultation stage. These included funding of implementation activities, fitting the action into the crowded school timetables, the added burdens to teacher workloads, the sensitive nature of weighing and measuring children and the sustainability of activities once project funding finished. During this time, the process also involved employment of project staff and setting up of interim project structures.
ANGELO workshops
Workshops participants were updated on international evidence on obesity prevention, relevant data for the target age group and local contextual information. They then worked through pre-prepared worksheets to score priority behaviours to target, knowledge and skill gaps, and environmental barriers to address. In total, there were over 120 elements listed for prioritization. Table 3 shows an example of the list of 15 potential behaviours and the two additional behaviours (added by participants on the day of the workshop) for the Australian adolescent community and the results from the prioritization stage (highest ranked scores).
Table 3:
List of the potential behaviours and the prioritized behaviours to target in interventions, from the Australian adolescent community project (It's Your Move!)
| List of elements for potential behaviours to target | Top rankings |
|---|---|
| Increase the amount of fruit eaten | 3 |
| Increase the amount of vegetables eaten | |
| Increase water intake and decrease high sugar drinks | 1 |
| Have a complete breakfast more often | 2 |
| Decrease junk food (high fat, high sugar) before or after school | |
| Have healthier lunches more often | 4 |
| Have dinners that are lower in fatty foods (e.g. fried foods, takeaways) | |
| Decrease serving sizes | |
| Increase participation in organized sport | 6 |
| Increase participation in other organized activities that involve being active (e.g. dance, martial arts) | 7 |
| Increase informal activities that involve being active (e.g. skateboarding, shooting basketball hoops) | |
| Increase walking/cycling (and less car use) | 5 |
| Increase physical education (PE) in schools | |
| Decrease TV viewing time | |
| Decrease electronic games time | |
| Additional | |
| Increase activities at lunch/recess | |
| Decrease dieting behaviours |
Similar elements were listed with the other non-Australian communities with a maximum of 18 elements, most being common across all communities. Several behaviours were worded differently between communities, but essentially had the same meaning, with culturally specific examples given for most elements. For example ‘have healthier lunches more often’ was worded for Tonga as ‘increase the healthiness of school lunch with less high-fat, high-sugar food for lunch (e.g. keke [cake]) and more healthy choices (e.g. manioka [tapioca], rice, fruit, vegetables, fo'i moa [hen's egg])’.
Specific behaviours relating to sociocultural factors that emerged from Fiji and Tonga were included on their respective worksheets. Those that emerged from Fiji included decreasing high fat/high sugar foods after school and decreasing the purchase of high fat/high sugar snacks; balancing food quantities across the day; reducing starchy vegetables e.g. taro; and the notion of ‘early to bed, early to rise’. Behaviours unique to Tonga included replacing butter and dripping with healthier oils, learning to fish and making a home garden.
Table 4 shows an example of the potential knowledge and skill gaps to target for the Fijian community and the results from the prioritization stage. Environmental barriers to change were identified for relevant settings and included homes/families, schools, neighbourhoods (community organizations, sports clubs and shops), churches and villages where appropriate. For brevity, the identified barriers in the home/family setting for the four adolescent projects have been combined and shown in Table 5. In the worksheets, the elements were grouped according to type of environment (physical, economic, policy or sociocultural).
Table 4:
List of potential knowledge and skill gaps for prioritization, showing the prioritized results for Fijian adolescent community project (Healthy Youth, Healthy Communities)
| List of elements for knowledge and skill gaps | Top rankings |
|---|---|
| To know that takeaways are fattening | |
| To know that snacks like chips/crisps, vara (germinated coconut) and bhajiah (deep fried savoury snack) are fattening | |
| To understand appropriate serve sizes | |
| To know the importance of eating breakfast each morning | 1 |
| To understand what a healthy body size looks like | |
| To know that fruit juices and cordials are high in sugar | |
| To know what healthy school food choices are | 2 |
| To know what healthy after-school food choices are | |
| To understand that ghee, butter and oils are fattening | |
| To know that dalo (taro; starchy root crop) and rice is not very fattening | |
| To get a taste for lots of different types of vegetables (F)a | |
| To have the cooking skills to make tasty healthy meals (i.e. using less fat) | 5 |
| To have good sports skills, e.g. ball skills (I, girls)a | |
| To know what is a good amount of physical activity to do each day | |
| To know where sports and activities are offered | |
| To understand that walking is good exercise | 3 |
| To know that being overweight causes diabetes and heart disease | 3 |
| Additional | |
| To know the importance of adequate sleep |
aElements that the socio-cultural studies found to be particularly important for particular gender or ethnic groups (F=Fijians, I=IndoFijians).
Table 5:
List of potential environmental barriers in the home/family setting, separated by environment type, from the four communities targeting the adolescent age group
| Environment type | Identified elements in home/family setting (articulated as barriers) |
|---|---|
|
Physical What is/is not available? |
Food:
|
Physical activity:
| |
|
Economic What are the financial factors? |
Food:
|
Physical activity:
| |
|
Policy What are the rules? |
Food:
|
Physical activity:
| |
|
Sociocultural What are the attitudes, beliefs, perceptions, values, practices? |
Food:
|
Physical activity:
| |
Body size:
|
The highest ranked barriers to target emerging from the prioritization of home environments for the New Zealand community were no fruit at home, too many of high fat snacks at home, few home rules about eating junk food, mainly high fat low vegetable meals, family practices not supportive of reducing fatty foods, junk food for lunchboxes and few home rules about TV viewing.
The action plans
For each community, consensus was reached from discussions on an overall goal for their project and these included both a capacity building and obesity prevention component. For example, the goal in Fiji was ‘to increase the capacity of the Nasinu community to promote healthy eating and regular physical activity and to reduce the development of overweight and obesity in the youth in the community’. In other communities, the terms ‘overweight’ and ‘obesity’ were deemed inappropriate and were replaced by ‘maintaining healthy weight’.
Eight to 10 objectives were developed for each action plan. Three of these were common across all plans: building community capacity (workforce development, leadership, partnerships/relationships, organizational development and resources), communicating the project messages (social marketing) and evaluating the project. The latter two usually required their own sub-plans. Four or five objectives stemmed from the priority behavioural elements obtained from the ANGELO Framework. Fijian youth identified ‘early to bed, early to rise’ as an element for action and although this was not identified by other groups present (including the Indo-Fijian youth), it was not rejected. Instead, the ANGELO Framework allowed for this specifically identified element as it was subsequently incorporated into the first behavioural objective, i.e. ‘to significantly reduce the proportion of adolescents who skip breakfast on school days’, after discussion around time management and the issue of skipping breakfast. The final one or two objectives in each action plan allowed for innovative or exploratory interventions. In Australia, key stakeholders of the adolescent group wanted to focus on healthy body size and shape and decided, ‘to create an acceptance of different healthy body sizes/shapes and decrease episodes of inappropriate dieting’ as an objective, demonstrating how the process responds to felt needs (the areas that the adolescents think needed addressing).
Knowledge and skill gaps and the list of environmental barriers were scored and ranked in the same way as behaviours and then used to inform strategies of action for the behavioural objectives. Strategies typically consisted of social marketing, policy or program actions.
Once agreement had been reached on the draft action plan at the end of each workshop, each plan was further refined by taking it back to the community and seeking input from other stakeholders who were unable to participate in the workshop. Also, timelines, processes and accountability by project coordinators were assigned to the action plan as it evolved. Evaluation measures were assigned once baseline data were analysed. The action plan was designed to be a ‘living’ document, which guided implementation and evolved through several versions (up to 15) during the life of the project.
DISCUSSION
Obesity prevention action plans were successfully developed in Australia, New Zealand, Fiji and Tonga using the ANGELO Process. Stakeholders were facilitated to develop their own action plans for healthy eating and physical activity, appropriate for the target age group, culture/s and local contexts.
Priority setting is a vital step in achieving action on obesity prevention. Indeed, the International Obesity Prevention Task Force (IOTF) identified priority setting as the fifth stage of translating evidence into action (Swinburn et al., 2005). Selecting a portfolio of specific policies, programs and other actions require the input of evidence from a variety of sources and a process to analyse and incorporate that evidence into specific conclusions. This is precisely what the ANGELO Process, as described here, was able to achieve at a community level. It proved to be an effective and efficient way of incorporating literature evidence, local evidence and stakeholder/community input into judgements for identifying priority interventions. It also served the important process of giving the local stakeholders a central role in the development of the plan so that they would be empowered to deliver a multi-strategy, multi-setting intervention dose appropriate for their community. As one of the principles of health promotion, stakeholder engagement and participatory planning are critical for developing a collaborative planning partnership and consensus on the way forward (National Public Health Partnership, 2000; Green and Kreuter, 2005; Flemming and Parker, 2007;). Moreover, the process proved to be applicable across diverse communities.
In Fiji, Tonga and New Zealand, the preliminary qualitative research provided critical contextual information, including the identification of culturally specific practices that were important to incorporate into the action plan. This is particularly important if there is little published information about the culturally shaped attitudes, beliefs, perceptions and expectations in relation to food, physical activity and body size of the target population.
In order to successfully implement a comprehensive obesity prevention action plan, a capacity building approach is recognized as a promising approach to enable actions across multiple-settings using multiple strategies for physical activity and healthy eating interventions (Pate et al., 2000; Kumanyika et al., 2002; Swinburn and Egger, 2002). The ANGELO workshops contributed to building community capacity (New South Wales Health, 2001) in terms of workforce development (increasing skills in project planning and knowledge about obesity prevention); in leadership (identifying champions) and in partnerships (by building on or creating new relationships between key stakeholders, sharing a common goal and creating ownership of the project). Participating youth in Australia became ‘Student Ambassadors’ for the project. In Fiji, Tonga and New Zealand, some of the adolescent participants in the ANGELO workshops became members of student health committees. In their roles, these youth were active in informing the intervention strategies and being champions (role models) for their peers and their families (Caltabiano and Sarafino, 2002; Sanderson, 2004). This active engagement of youth has contributed to the adolescents’ sense of ownership and thus uptake of the interventions (Green and Kreuter, 2005).
Across the four adolescent targeted communities, the number of common potential behaviours to target for intervention that emerged outnumbered those that were unique to a community. This was despite clear ethnic and cultural differences across the four countries, suggesting that the ANGELO Process could be considered for wider application. At the workshop, the scoring process determines the ranking of the elements; however, these are open to consensus to determine how they are incorporated into the action plan ensuring the process is a flexible one, responding to felt needs (Bradshaw, 1972). For example, Fijian youth prioritized balancing food quantities across the day, while Indo-Fijian youth and school and religious representatives did not. However, the need for a regular and healthy breakfast was ranked high by all groups. It was agreed to combine these two priorities into one objective (i.e. to reduce the proportion of youth who skip breakfast and lunch on school days). This flexible integration of opinions from one or more community sectors also contributed to the sense of community ownership (Green and Kreuter, 2005). Similarly, fruit, vegetable, high fat foods and drink consumption rated highly among the church group in Fiji, but not necessarily by the other groups. It was then agreed that as an innovative/experimental objective, to include a program for promoting healthy eating and physical activity within churches, mosques and temples which could also potentially encompass all these behaviours and in a range of contexts that reflected the cultural and religious diversity of the Fijian population.
The three standard objectives incorporated into the action plan for capacity building, social marketing and evaluation, we would recommend for any obesity prevention program as good practice (Hawe et al., 1990; New South Wales Health, 2001; Donovan and Henley, 2003; Victorian Government Department of Human Services, 2003; Smith et al., 2006; Stead et al., 2007).
Limitations
The ANGELO Process may not suit all communities, as to date it has only been applied in relatively small discrete towns or communities. A pathway needs to be found for scaling this up, or a similar process, across larger areas including metropolitan areas or whole states or nations. Also, the ANGELO Process has a focus on obesity prevention; however, the principles could still be applied if the scope of the intervention is broadened. The process did require expert facilitation and therefore training programs for facilitators would be needed for a more widespread adoption of this process. Other approaches such as a focus group methodology across the community could also be effective and efficient, but this possibility was not tested here.
CONCLUSIONS
The ANGELO Process produced a comprehensive action plan for community-level obesity prevention and demonstrated a flexible and effective practical application of evidence-based priority-setting. Its application in cultures where the evidence is limited and the cultural determinants of obesity are likely to be strong requires preliminary assessment of sociocultural elements to ensure that sociocultural barriers are incorporated into the action plan. While the ANGELO Process starts to create community ownership of the potential solutions for childhood obesity, the challenge will come with scaling the process up for application across many communities.
FUNDING
Funding for the OPIC study was provided by the Wellcome Trust in Fiji and Tonga and the National Medical Research Council in Australia and the Health Research Council in New Zealand. Funding for the It's Your Move! project in Australia was provided by the Victorian Government Department of Human Services.
ACKNOWLEDGEMENTS
We are grateful to the participants for their generous contributions during the interviews and focus groups, and to their families, schools and churches for facilitating these activities. We acknowledge the contributions of the Healthy Youth Healthy Community team in Fiji, the Màalahi Youth team in Tonga, especially Dr Viliami Puloka, the Tonga Health Promotion team and the Living4Life team in New Zealand. We are especially grateful to Dr Iris Wainiqolo, Dr Kitioni Rawalai, Seini Kurusiga and Shakila Naidu for co-piloting, conducting, translating and transcribing the interviews in Fiji and Ms Lupe Savou and Dr Vakaola Mafi for conducting, transcribing and translating the interviews in Tonga. We are grateful to Dr Robyn Dixon, Dr Deborah Widdowson and Dr Unaise Baba for conducting and transcribing the focus groups in New Zealand. We are also grateful to Dr Peter Kremer for comments on earlier drafts of this paper.
REFERENCES
- Bartholomew L. K., Parcel G. S., Kok G., Gottlieb N. H. Intervention Mapping: Designing Theory- and Evidence-Based Health Promotion Programs. California: Mayfield; 2001. [Google Scholar]
- Becker A. E. Body, Self and Society. The View from Fiji. Philadelphia: University of Pennsylvania Press; 1995. [Google Scholar]
- Bell A. C., Swinburn B. What are the key food groups to target for preventing obesity and improving nutrition in schools? European Journal of Clinical Nutrition. 2004;58:258–263. doi: 10.1038/sj.ejcn.1601775. [DOI] [PubMed] [Google Scholar]
- Bradshaw J. The concept of social need. New Society. 1972;30:640–643. [Google Scholar]
- Brown W. J., Trost S. G. Life transitions and changing physical activity patterns in young women. American Journal of Preventive Medicine. 2003;25:140–143. doi: 10.1016/s0749-3797(03)00119-3. [DOI] [PubMed] [Google Scholar]
- Burton N. W., Turrell G., Oldenburg B. Participation in recreational physical activity: why do socioeconomic groups differ? Health Education and Behaviour. 2003;30:225–244. doi: 10.1177/1090198102251036. [DOI] [PubMed] [Google Scholar]
- Caltabiano M. L., Sarafino E. P. Health Psychology: Biosocial Interactions. An Australian Perspective. Brisbane: Wiley; 2002. [Google Scholar]
- Carter R. Priority Setting in Health: Processes and Mechanisms; Expert Paper prepared on invitation from the Commonwealth Secretariat for the 13th Commonwealth Health Ministers Meeting; November 25–29; Christchurch. New Zealand: 2001. [Google Scholar]
- Coyne T. Lifestyle diseases in pacific communities. In: Hughes R., Langi S., editors. Technical Paper/Secretariat of the Pacific Community No 219. Noumea: Secretariat of the Pacific Community; 2000. [Google Scholar]
- Doak C. M., Visscher T. L., Renders C. M., Seidell J. C. The prevention of overweight and obesity in children and adolescents: a review of interventions and programmes. Obesity Reviews. 2006;7:111–136. doi: 10.1111/j.1467-789X.2006.00234.x. [DOI] [PubMed] [Google Scholar]
- Donovan R., Henley N. Social Marketing: Principles and Practice. Melbourne: IP Communications; 2003. [Google Scholar]
- Egger G., Pearson S., Pal S., Swinburn B. Dissecting obesogenic behaviours: the development and application of a test battery for targeting prescription for weight loss. Obesity Reviews. 2007;8:481–486. doi: 10.1111/j.1467-789X.2007.00395.x. [DOI] [PubMed] [Google Scholar]
- Ferreira I., van der Horst K., Wendel-Vos W., Kremers S., van Lenthe F. J., Brug J. Environmental correlates of physical activity in youth—a review and update. Obesity Reviews. 2007;18:129–154. doi: 10.1111/j.1467-789X.2006.00264.x. [DOI] [PubMed] [Google Scholar]
- Flemming M. L., Parker E. Health Promotion. Principles and Practice in the Australian Context. 3rd edititon. Sydney: Allen & Unwin; 2007. [Google Scholar]
- Franklin J., Denyer G., Steinbeck K. S., Caterson I. D., Hill A. J. Obesity and risk of low self-esteem: a statewide survey of Australian children. Pediatrics. 2006;118:2481–2487. doi: 10.1542/peds.2006-0511. [DOI] [PubMed] [Google Scholar]
- Green L. From research to ‘best practices’ in other settings and populations. American Journal of Health Behavior. 2001;25:165–178. doi: 10.5993/ajhb.25.3.2. [DOI] [PubMed] [Google Scholar]
- Green L., Kreuter M. Health Promotion Planning: An Educational and Ecological Approach. 4th edition. New York: McGraw-Hill; 2005. [Google Scholar]
- Hawe P., Degeling D., Hall J. Evaluating Health Promotion: A Health Workers Guide. Sydney: MacLennan and Petty; 1990. [Google Scholar]
- Hesketh K., Waters E., Green J., Salmon L., Williams J. Healthy eating, activity and obesity prevention: a qualitative study of parent and child perceptions in Australia. Health Promotion International. 2005;20:19–26. doi: 10.1093/heapro/dah503. [DOI] [PubMed] [Google Scholar]
- Jain A. Treating obesity in individuals and populations. British Medical Journal. 2005;331:1387–1390. doi: 10.1136/bmj.331.7529.1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keleher H., MacDougall C., Murphy B. Understanding Health Promotion. Melbourne: Oxford University Press; 2007. [Google Scholar]
- Khaleghian P. Noncommunicable Disease in Pacific Island Countries: Disease Burden, Economic Costs and Policy Options. A Report prepared for the South Pacific Commission and the World Bank. South Pacific Commission, Noumea. 2003 [Google Scholar]
- Kremers S. P., de Bruijn G. J., Visscher T. L., van Mechelen W., de Vries N. K., Brug J. Environmental influences on energy balance-related behaviours: a dual-process view. International Journal of Behavioral Nutrition and Physical Activity. 2006;3:9–18. doi: 10.1186/1479-5868-3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumanyika S. K. Special issues regarding obesity in minority populations. Annals of Internal Medicine. 1993;119:650–654. doi: 10.7326/0003-4819-119-7_part_2-199310011-00005. [DOI] [PubMed] [Google Scholar]
- Kumanyika S., Jeffery R. W., Morabia A., Ritenbaugh C., Antipatis V. J. Obesity prevention: the case for action. International Journal of Obesity and Related Metabolic Disorders. 2002;26:425–436. doi: 10.1038/sj.ijo.0801938. [DOI] [PubMed] [Google Scholar]
- Mavoa H. The ‘C’ Factor: Cultural underpinnings of food, eating and body size. Progress in Obesity Research 10; Proceedings of the 10th International Congress on Obesity; 3–8 September; Sydney. 2006. [Google Scholar]
- Mavoa H., Schultz J., Goundar R. Looking to the Future: Indigenous Fijian and IndoFijian adolescents; 15th European Congress on Obesity: Final Programme; UK: Obesity International Trading Ltd; 2007. [Google Scholar]
- McCabe M. P., Ricciardelli L. A. Parent, peer and media influences on body image and strategies to both increase and decrease body size among adolescent boys and girls. Adolescence. 2001;36:225–240. [PubMed] [Google Scholar]
- McKenzie J. F., Neiger B. L., Smeltzer J. L. Planning, Implementing and Evaluating Health Promotion Programs: A Primer. 4th edition. San Francisco: Benjamin Cummings; 2005. [Google Scholar]
- National Public Health Partnership. Deciding and Specifying an Intervention Portfolio. Melbourne: National Public Health Partnership; 2000. [Google Scholar]
- New South Wales Health. A Framework for Building Capacity to Improve Health. Sydney: Better Health Centre; 2001. [Google Scholar]
- Pate R. R., Trost S. G., Mullis R., Sallis J. F., Wechsler H., Brown D. Community interventions to promote proper nutrition and physical activity among youth. Preventive Medicine. 2000;31:S138–S149. [Google Scholar]
- Pickett G. E., Hanlon J. J. Public Health: Administration and Practice. St Louis: Mosby-Year Book, Inc; 1990. [Google Scholar]
- Pollock N. These Roots Remain: Food Habits in Islands of the Central and Eastern Pacific. Laie, Hawaii: Institute of Polynesian Studies; 1992. [Google Scholar]
- Raine K., Spence J. C., Church J., Boule N., Slater L., Marko J., et al. State of the Evidence Review on Urban Health and Healthy Weights. Ottawa: CIHI; 2008. [Google Scholar]
- Ricciardelli L. A., McCabe M. P. A biopsychosocial model for understanding body image and body change strategies among children. Journal of Applied Developmental Psychology. 2003;24:475–495. [Google Scholar]
- Round R., Marshall B., Horton K. Planning for Effective Health Promotion Evaluation. Melbourne: Victorian Department of Human Services; 2005. [Google Scholar]
- Rychetnik L., Hawe P., Waters E., Barratt A., Frommer M. A glossary for evidence based public health. Journal of Epidemiology and Community Health. 2004;58:538–545. doi: 10.1136/jech.2003.011585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanderson C. A. Health Psychology. New Jersey: Wiley; 2004. [Google Scholar]
- Schultz J., Utter J., Mathews L., Cama T., Mavoa H., Swinburn B. The Pacific OPIC Project (Obesity Prevention in Communities): action plans and interventions. Pacific Health Dialogue. 2007;14:147–153. [PubMed] [Google Scholar]
- Smith B., Tang K., Nutbeam D. WHO Health Promotion Glossary: new terms. Health Promotion International. 2006;21:340–345. doi: 10.1093/heapro/dal033. [DOI] [PubMed] [Google Scholar]
- Stead M., Hastings G., McDermott L. The meaning, effectiveness and future of social marketing. Obesity Reviews. 2007;8:S189–S193. doi: 10.1111/j.1467-789X.2007.00340.x. [DOI] [PubMed] [Google Scholar]
- Summerbell C. D., Waters E., Edmunds L. D., Kelly S., Brown T., Campbell K. J. Interventions for preventing obesity in children. Cochrane Database Systematic Review. 2005;3 doi: 10.1002/14651858.CD001871.pub2. CD001871. [DOI] [PubMed] [Google Scholar]
- Swinburn B., Egger G. Preventive strategies against weight gain and obesity. Obesity Reviews. 2002;3:289–301. doi: 10.1046/j.1467-789x.2002.00082.x. [DOI] [PubMed] [Google Scholar]
- Swinburn B., Egger G., Raza F. Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Preventive Medicine. 1999;29:563–570. doi: 10.1006/pmed.1999.0585. [DOI] [PubMed] [Google Scholar]
- Swinburn B., Egger G. Influence of obesity-producing environments. In: Bray G. A., Bouchard C., editors. Handbook of Obesity - Clinical Applications. New York, NY: Marcel Dekker, Inc.; 2004. pp. 97–114. [Google Scholar]
- Swinburn B., Gill T., Kumanyika S. Obesity prevention: a proposed framework for translating evidence into action. Obesity Reviews. 2005;6:23–33. doi: 10.1111/j.1467-789X.2005.00184.x. [DOI] [PubMed] [Google Scholar]
- Swinburn B. A., Carter R., Haby M., Moodie M., Bell A. C., Simmons A. Obesity prevention—selecting the best investments. 2006 WHO Europe – Technical Review Paper, The obesity issues in Europe: status, challenges, prospects. [Google Scholar]
- Swinburn B. A., Pryor J., McCabe M., Carter R., de Courten M., Schaaf D., et al. The Pacific OPIC Project (Obesity Prevention in Communities)—objectives and design. Pacific Health Dialogue. 2007;14:139–146. [PubMed] [Google Scholar]
- van der Horst K., Oenema A., Ferreira I., Wendel-Vos W., Giskes K., van Lenthe F., et al. A systematic review of environmental correlates of obesity-related dietary behaviors in youth. Health Education Research. 2007;22:203–226. doi: 10.1093/her/cyl069. [DOI] [PubMed] [Google Scholar]
- Victorian Government Department of Human Services. Integrated Health Promotion: A Practice Guide for Service Providers. Australia: Victorian Government; 2003. [Google Scholar]
- Wendel-Vos W., Droomers M., Kremers S., Brug J., van Lenthe F. Potential environmental determinants of physical activity in adults: a systematic review. Obesity Reviews. 2007;8:425–440. doi: 10.1111/j.1467-789X.2007.00370.x. [DOI] [PubMed] [Google Scholar]
- WHO. Food and Health in Europe: A New Basis for Action. Denmark: Copenhagen, World Health Organization, Regional Office for Europe; 2002. [Google Scholar]
- WHO. WHO Technical Report Series 916. Geneva: Joint FAO/WHO expert consultation; 2003. Diet, nutrition and the prevention of chronic diseases. [PubMed] [Google Scholar]