“Cavities” is the common term for dental decay, more properly known as caries, which is Latin for rottenness. Caries is one of the most common of dental diseases in humans. Caries has been defined as “a disease of the calcified tissues of the teeth resulting from the action of micro-organisms on carbohydrates, characterized by decalcification of the inorganic portions of the tooth and accompanied or followed by disintegration of the organic portion” (1).
Caries results from bacterial decay of the tooth structure brought about by the release of acids from oral bacteria fermenting carbohydrates on the tooth surface. Therefore, a diet high in highly refined and easily fermentable carbohydrates will favor the development of caries.
As western civilization progressed, our diet changed to include the types of foods that would promote decay and so caries became a widespread and serious concern. It is only recently that the use of fluoride and improved oral hygiene practices has brought about a decline in the incidence of caries in human mouths.
Many owners are unaware that dogs may also be subject to caries. Though the incidence of caries in dogs is lower than it has been in humans, it does occur and we must watch for areas at risk or already undergoing decay and recommend such preventive or restorative treatments as are reasonable. In a review of the author’s records, it was found that 5.25% of adult canine patients had one or more caries lesion and in most cases, lesions were bilaterally symmetrical (2).
Factors which must be in place for caries to develop include: natural tooth structure with susceptible surface exposed to the oral environment, complex indigenous microflora, and food ingested by mouth. There are many modifying factors as well, which influence the location of the lesion.
Among the reasons proposed for the lower incidence of caries in dogs compared with historical rates in humans are: conical tooth shape and wider inter-dental spacing with less area for food impaction and stagnation; diets which include little fermentable carbohydrate; higher salivary pH (in dogs, mean pH of 7.5 compared with 6.5 in humans) to buffer acids produced by bacterial fermentation of carbohydrates; in dogs, a relatively low level of salivary amylase to break down starches which are retained in and around the teeth. When caries develops, it does so in the following manner.
As bacteria on the tooth surface ferment the carbohydrates, acids (lactic, acetic, propionic) are released. These acids diffuse into and demineralize the surface enamel. Loss of mineral exposes the organic (protein) matrix of the enamel, which is digested by enzymes from the oral bacteria and/or leukocytes. As the process penetrates deeper, microcavitations develop under the surface. As these expand, they coalesce and the undermined enamel collapses.
There is a constant exchange of minerals between the enamel and the oral fluid. If this exchange is balanced, no lesion develops, but if there is a net loss of mineral from the enamel, caries develops. In the very early stages, before the protein matrix collapses, the process can be reversed and the lesion can “heal.” Once the protein matrix collapses, the lesion is irreversible and treatment is aimed at preventing further progression and replacing the lost tissue with a suitable restorative material.
The rate of progression of caries depends more on factors external to the tooth such as the cariogenicity of microflora, the availability of acidogenic substrates, and the remineralizing capability of oral fluids. Intrinsic factors include the degree of tissue mineralization and the amount of matrix protein.
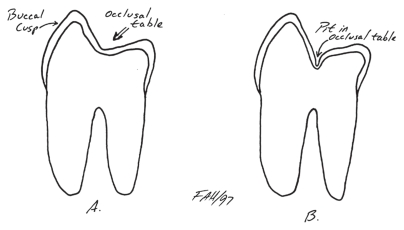
Caries can be classified by location as pit and fissure caries, smooth surface caries, or root surface caries. In the author’s experience, pit and fissure caries are the most common type in dogs. They can occur in the pits sometimes found on the occlusal tables of the maxillary molars. As Figure 1 shows, some teeth have a smooth transition from the palatal wall of the buccal cusps down on to the occlusal table. In other teeth, there is a pit at the base of the cusps and in these teeth, the enamel is thinner at the bottom of the pit. Figure 2 is a photograph of the left maxillary 1st molar in a young dog showing deep occlusal pits highlighted with a pink fluid. If food high in carbohydrates becomes trapped in these pits along with sufficient bacteria, caries is very likely to develop.
Figure 1.
Cross section through the maxillary 1st molar of a dog. The tooth on the left has no occlusal pit and would be resistant to caries. The tooth on the right has a deep occlusal pit and would be anatomically at risk for the development of caries.
Figure 2.
The occlusal surface of the left maxillary 1st molar in a dog. Pink liquid has been applied to the crown to highlight the occlusal pits that put this tooth at risk for the development of caries. As this tooth has just erupted and has not yet developed any decay, a Pit and Fissure sealant is indicated to prevent caries development.
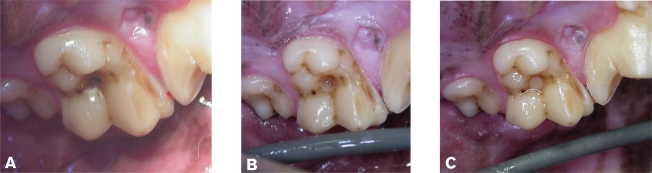
Other locations at risk are the deep developmental grooves on the buccal surface of the maxillary 4th premolars and on the lingual side of the mandibular 1st molars between the mesial and central cusps. These grooves are often filled with calculus, but on deeper exploration, there may be soft, carious dentin at the base. Figure 3 is a series of photographs of the right maxillary 4th premolar, first with calculus and caries in the developmental groove (Figure 3a), then after debridement of the groove (Figure 3b), and finally after restoration with a bonded composite resin material (Figure 3c).
Figure 3.
A — A caries lesion in the developmental groove of the right upper 4th premolar tooth in a dog. B — The lesion following removal of calculus and necrotic dentin. C — The lesion following restoration with a bonded composite filling material.
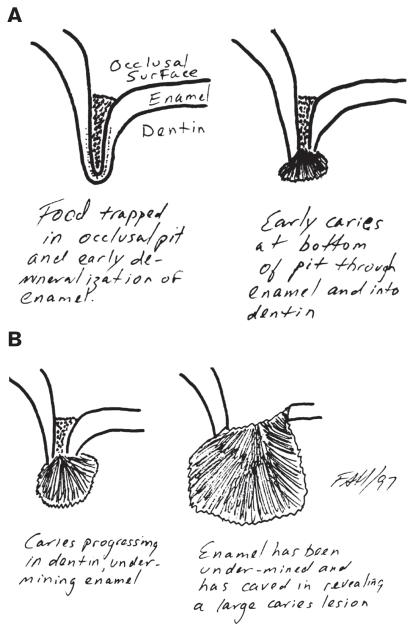
The series of diagrams in Figure 4 shows the progression of pit caries. Initially, food becomes trapped in an occlusal pit. As the bacteria ferment the carbohydrates, acids diffuse into the enamel and start to remove minerals from the surface. The food packed in the pit prevents oral fluids from reaching the demineralized surface and so remineralization is not possible. In time, the enamel is completely demineralized and the protein matrix digested. Now the caries has reached the dentin, which has a lower mineral content and a higher protein content. The decay progresses more rapidly in the dentin. Though the entrance to the lesions is the same size, the caries grows larger, undermining the overlying enamel.
Figure 4.
A and B — Progression of the development of a caries in the occlusal pit of the maxillary 1st molar from left to right.
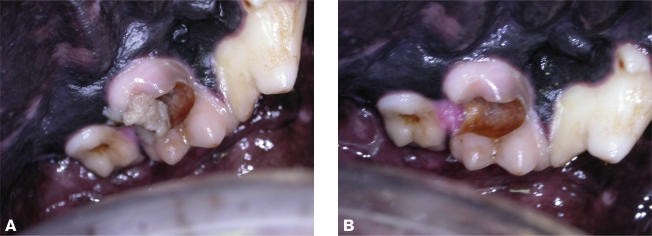
Only when the caries is quite large does the overlying enamel cave in at which point the large caries becomes readily detectable. Unfortunately, by the time the lesion is large enough to be easily seen, it has usually extended into the endodontic system of the tooth and there is such extensive loss of tooth structure that extraction is the only option. Figure 5 is of a medium-sized and treatable caries in the occlusal surface of the left maxillary 1st molar in a dog. The first image (Figure 5a) shows the dark spot over the pit. A dental explorer would easily sink into this dark area indicating decay. The second image (Figure 5b) is following preparation of the cavity to receive its restoration and the final image (Figure 5c) shows the restoration in place. Figure 6 is of a much more advanced caries of the left maxillary 1st molar in a dog. In the first image (Figure 6a), we can see food debris trapped in the lesion. The second image (Figure 6b) is after removal of gross, loose debris and shows the color of the carious dentin within the lesion. These caries involved the pulp and had removed a significant amount of the physical structure of the crown, and so the tooth was extracted.
Figure 5.
A — A caries lesion in the occlusal pit of the left maxillary 1st molar of a dog. B — The lesion following removal of debris and necrotic dentin. C — The lesion restored with a bonded composite filling material.
Figure 6.
A — A large caries lesion affecting most of the occlusal table of the left maxillary 1st molar of a dog. Note the remnants of the dog’s most recent meal within the lesion. B — Following removal of the loose debris, the extent of tissue loss is evident. The dark dentin is also necrotic and would need to be removed. This tooth was extracted due to the severity of tissue loss and exposure of the pulp.
An observation worth noting is that in the author’s experience, pit caries in the occlusal tables of the maxillary 1st molars teeth seems to be more common in large-breed dogs such as Labrador retrievers and German shepherd dogs.
Whenever performing an oral examination or hygiene procedure, watch for small caries lesions that are still treatable, as well as areas that might be particularly prone to caries development.
Prevention of caries is based on a thorough oral examination of the recently erupted permanent teeth at the time of spay/neuter. If deep occlusal pits such as those seen in Figure 2 or other anatomically compromised areas are found but there is not yet any sign of decay, then the application of a pit and fissure sealant is indicated. These products flow into the occlusal pits to occlude them and exclude food impaction.
In examining the teeth of a mature animal with your dental explorer, check for pits and fissures. If caries has started to develop, you will be able to force the tip of the explorer into the decaying surface. As you withdraw the instrument, the tip will stick and then let go, resulting in a metallic “ping” from the explorer tip and the sensation of “tugback.” Sound enamel and dentin are too hard to allow the explorer to penetrate so if you can get your instrument to sink in at all, you have found a caries lesion.
For established caries, the decayed enamel and dentin and all debris are removed from the lesion. Intra-oral dental radiographs are required to determine if there are any signs of endodontic (pulp) disease. The depth of the lesion needs to be examined and explored to determine if there is pulp exposure or near-pulp exposure. Endodontic (root canal) therapy is performed if indicated and then the prepared cavity is filled with a bonded dental restorative material (a filling).
Advanced caries will often involve both pulp exposure/necrosis and dramatic loss of coronal structure. In these cases, extraction of the remnants of the tooth is indicated.
Suggested reading
Hale, FA. Dental caries (cavities) In: Lobpriese HB, ed. Blackwell’s Five-minute Veterinary Consultant, Clinical Companion, Small Animal Dentistry. Iowa: Blackwell Publ, 2007:212–224.
McComb, D. Caries-detector dyes — How accurate and useful are they? J Can Dent Assoc 2000;66:195–198, Available from http://www.cda-adc.ca/jcda/vol-66/issue-4/195.html Last accessed October 13, 2009.
Footnotes
Use of this article is limited to a single copy for personal study. Anyone interested in obtaining reprints should contact the CVMA office ( hbroughton@cvma-acmv.org) for additional copies or permission to use this material elsewhere.
References
- 1.Dorland WA. Dorland’s Illustrated Medical Dictionary. 25th ed. Philadelphia: WB Saunders; 1974. [Google Scholar]
- 2.Hale FA. Dental caries in the dog. J Vet Dent. 1998;15:79–83. doi: 10.1177/089875649801500203. [DOI] [PubMed] [Google Scholar]