Abstract
Objective
The scale of road traffic injuries (RTI) in India is uncertain because of limitations in the availability and reliability of incidence data. We report these data for Hyderabad city in southern India.
Methods
In a cross-sectional population-based survey, 10,459 participants aged 5-49 years (94.3% participation) selected using three-stage systematic cluster sampling were interviewed. Participants recalled RTI in the preceding 3 months, and RTI related death and disability in the household in the last 3 years. RTI was defined as an injury resulting from a road traffic crash irrespective of the severity.
Results
The age-sex-adjusted annual incidence of non-fatal RTI requiring recovery period of ≤7, >7-29 and ≥30 days was 13% (95% CI 12.6 to 13.4%), 5.8% (95% CI 5.5 to 6.0%) and 1.2% (95% CI 1.1 to 1.4%), respectively. The overall adjusted rate for non-fatal RTI was 20.7 (95% CI 20.0 to 21.3%). The relative risk of RTI requiring recovery period of >7 days was significantly higher in the third per capita monthly income quartile (p<0.05). The incidence of non-fatal RTI was highest as a pedestrian, motorized two-wheeled vehicle and cycle user, 6.4, 6.3 and 5.1/100 persons/year, respectively. Annual RTI mortality and disability rates were 38.2 (95% CI 17.5 to 58.8) and 35.1 (95% CI 12.4 to 57.7) per 100,000 population.
Conclusions
There is a high burden of RTI in this urban population. With recent focused attention on RTI by the Government of India, these findings could assist in planning appropriate initiatives to reduce the RTI burden.
Keywords: disability, epidemiology, India, mortality, road traffic injuries
INTRODUCTION
Road traffic injuries (RTI) are estimated to constitute a major global public health problem.[1-2] Globally, RTI fatalities are projected to increase by 66% between the years 2000 and 2020 with South Asia estimated to record the largest increase, and will be the third leading cause of death.[3] With incomplete, little or no data available from countries with higher RTI mortality rates, there is also a suggestion that the present global RTI burden is underestimated.[1, 4]
The Global Burden of Disease (GBD) Study has estimated an annual RTI mortality rate of 20.9/100,000 population for all ages for India in 2002; these are projected estimates due to incomplete death registration in India.[5] Though a 2.5 times increase in RTI fatalities is predicted for India by the year 2020,[3] RTI is not considered a serious public health issue yet by policy makers in India.[6-7] A major reason for this lack of appropriate policy and intervention response by policy makers is the non-availability of robust and comprehensive RTI data that can highlight the magnitude of RTI burden.[6]
A detailed assessment of the risk factors for RTI in the general population is needed to plan informed RTI prevention strategies. We conducted a population-based study to elucidate the incidence, risk factors and outcome of RTI in the Indian city of Hyderabad. In this paper, we report RTI incidence and burden of RTI in this urban population in India.
METHODS
This study was approved by the Ethics Committee of the Administrative Staff College of India, Hyderabad, India.
Hyderabad city in Andhra Pradesh state of India has a population of 3.8 million excluding the surrounding areas that make up Hyderabad agglomeration.[8] Hyderabad had 1.2 million registered motor-vehicles in 2001-2002, the majority being motorised two-wheeled vehicles (77%), followed by 11% cars, and the rest were other types of motor-vehicles including motorised three-wheeled vehicles, buses, trucks, and tempo/vans.[9]
The study population was selected using a three-stage systematic cluster sampling procedure with equal probability of selection. Based on census data,[10] we divided Hyderabad into 2,542 clusters of mostly 1,400-1,600 population and listed in sequence. We then selected 50 clusters starting with a random cluster and then every 51st cluster was chosen to obtain 50 clusters. These clusters were plotted on the Hyderabad map and each cluster was visited by the study team to broadly understand the socio-economic profile. Through discussions with personnel of the Revenue Department, Municipal Corporation of Hyderabad, it was estimated that 20% of Hyderabad’s population belonged to upper, 50% to middle and 30% to lower socioeconomic strata. In order to maintain a similar socioeconomic profile in the study sample, three lower socioeconomic status clusters from the original sample were replaced by two middle and one upper socioeconomic status clusters adjacent to them in their census wards. We also selected one cluster of 49 homeless persons to represent this group in the population.[11]
Within each cluster (other than the homeless cluster), we enumerated the households and residents starting from the north-east corner of the cluster and ending in south-west corner. A household was defined as persons eating from the same kitchen. Visitors, hostels, hotels, commercial establishments, and prisons were not included. All residents 5-49 years of age in the selected clusters were considered eligible. Systematic sampling, with the first number drawn randomly, was carried out to sample households with the aim of sampling 215-225 eligible people in each cluster. This usually required a sampling interval between 5 and 8 households depending on the total number of households and the eligible population in a cluster. All residents 5-49 years of age in the selected households formed the study population.
At the time of planning of this study, the most recent RTI fatalities data available with the Government of India were for the year 2001.[12] Using these data and assuming the number of people with non-fatal RTI to be 20-50 times of those with fatal RTI, an annual RTI incidence between 0.16 and 0.39% was estimated for India’s population.[8] For obtaining data on RTI for the last 3 years in the study, the RTI incidence over 3 years was estimated as 0.81% for Hyderabad (assuming an average annual incidence of 0.27%). Using Poisson distribution and assuming a design effect (DE) of 1.5 due to cluster sampling strategy,[13] a sample size of 9,000 people aged 5-49 years was estimated such that RTI incidence estimates over 3 years would be between 0.59 to1.02% at the 95% confidence level (CI). Assuming 85% participation rate, we aimed at sampling 10,600 people aged 5-49 years.
Interview
Data were collected from October 2005 to December 2006. Trained interviewers obtained written informed consent from eligible people for participation in the study (from the parent/guardian for those aged 5-15 years), followed by confidential interview using a questionnaire designed for this study. Questionnaire was developed by the study team through review of worldwide literature and focus group discussions with randomly selected members of the population. The questionnaire was developed in English, was translated in Telugu and Hindi, the two local languages, following which it was back-translated into English in order to ensure accurate and relevant meaning and intent of the questions. Pilot testing of the questionnaire was done and modifications made as necessary.
Detailed demographic data were obtained for all participants aged 5-49 years (information collected from parent/guardian for participants <11 years of age, and in the presence of parent/guardian for those aged 11-15 years). The participants were asked to recall if they were involved in road traffic crash (RTC) at different time periods - preceding three and twelve months - resulting in an injury irrespective of the severity. Detailed data including duration of RTI, vehicles involved and days of recovery/disability were documented. If a participant reported more than one RTI during the recall periods, all RTI were documented. For participants with RTI related disability in the last 3 years, data on RTI that resulted in disability were also obtained. Data on death of a household member in the last 3 years due to RTI were documented by interviewing the head/lady of the household who also provided data on the household income.
Definition of road traffic injury
RTI was defined as any injury resulting from RTC irrespective of severity and outcome. RTC was explained to the respondent as any crash on a road involving at least one moving vehicle irrespective of it resulting in an injury. This could include collision with a vehicle or any non-moving object while driving/riding a vehicle, skidding/ slipping/ overturning of a moving vehicle while driving/riding a vehicle, collision with a moving vehicle while walking/running/standing/sitting on road, or fall from a moving vehicle. These explanations were given to each participant before asking questions on RTC and RTI.
Data management and statistical analysis
Data were entered in an MS Access database and data entered by one data entry operator were checked by another. SPSS was used for statistical analysis. Annual non-fatal RTI rates were calculated using three-month recall period for overall non-fatal RTI and for RTI requiring recovery period of ≤7, >7-29 and ≥30 days. For this analysis, recovery period was defined as days taken to return to normal daily activities as prior to RTI. For participants who were still recovering at the time of interview and those who had not recovered, recovery period was taken to be the length of time since sustaining RTI. Annual incidence rates for non-fatal RTI for which medical treatment outside home was sought as an out-patient (excluding self-medication through purchase of medicines from pharmacy) or as in-patient are also presented. Relative risk of non-fatal RTI is presented, and estimates for non-fatal RTI burden for Hyderabad were calculated using the incidence rates from this study. Type of road user categories included pedestrian, cycle, motorised two-wheeled vehicle (MTV), motorised three-wheeled vehicle (commercial passenger vehicles: auto-rickshaw and seven-seater), car/jeep, and other vehicles (bus/tempo/truck/lorry).
Annual RTI mortality and disability rates per 100,000 population for the 5-49 years age group are presented based on deaths and disabilities reported in the last 3 years. Annual RTI incidence rates were adjusted for the age and sex distribution of Hyderabad population, and the 95% CI included the DE for the cluster sampling strategy.[14] The incidence rates were not adjusted for exposure. Per capita monthly income (PCMI) was considered in four quartiles based on the distribution in the study population. Chi-square and one-tailed tests for significance are reported where appropriate.
RESULTS
Of the 11,097 eligible participants, 10,459 (94.3%) participated, and 447 (4%) were not available/could not be contacted for interview and 191 (1.7%) refused participation. Of the participants, 5,376 (51.4%) were males. The participation rate was 93.1% and 95.5% for males and females, respectively.
Annual non-fatal RTI incidence
During the last 3 months, 536 non-fatal RTI were reported by 520 participants. The overall age-sex-adjusted rate for non-fatal RTI was 20.7 (95% CI 20.0 to 21.3; DE 2.24)/100 persons/year. The adjusted rate for RTI requiring recovery period of ≤7 days, >7-29 days and ≥30 days was 13.0 (95% CI 12.6 to 13.4; DE 1.70), 5.8 (95% CI 5.6 to 6.0; DE 1.25) and 1.2 (95% CI 1.1 to 1.4; DE 1.36), respectively (Table 1). The overall rate for non-fatal RTI peaked in the15-19 years age group (Table 1). Males had twice or more incidence rate for RTI requiring recovery period of ≤7 and >7-29 days as compared with females, however, RTI incidence for recovery period of ≥30 days was nearly twice in females as compared with males (Table 1). The incidence rate for RTI requiring recovery period of ≤7 days and >7-29 days was the least in the first PCMI quartile and was fairly similar for the other three PCMI quartiles. The rate for RTI requiring recovery period of ≥30 days was highest in the third PCMI quartile, nearly 2.5 and 4 times the rate in the first and last quartiles, respectively (Table 1). The decline in RTI incidence from 3-months to 12-months recall period was 44.9%.
Table 1.
Estimated annual non-fatal road traffic injury (RTI) incidence rate per 100 persons for three-months recall period in population aged 5-49 years in Hyderabad. CI denotes confidence interval.
| Variable | Total (10,459) |
Number with RTI (% of total) |
Annual non-fatal RTI incidence per 100 persons (95% CI) |
|||
|---|---|---|---|---|---|---|
| Recovery period of ≤7days** |
Recovery period of >7-29 days** |
Recovery period of ≥30 days** |
Overall | |||
|
Age group
(years) * # |
||||||
| 5-9 | 1,425 | 56 (3.9) | 10.0 (9.6-10.4) | 4.2 (3.9-4.4) | 0.6 (0.5-0.7) | 15.6 (15.0-16.2) |
| 10-14 | 1,384 | 73 (5.3) | 14.8 (14.4-15.3) | 6.1 (5.9-6.4) | 1.3 (1.2-1.4) | 23.5 (22.9-24.1) |
| 15-19 | 1,372 | 91 (6.6) | 18.9 (18.4-19.3) | 8.9 (8.7-9.2) | 1.3 (1.2-1.4) | 30.1 (29.5-30.8) |
| 20-29 | 2,825 | 158 (5.6) | 13.4 (13.0-13.9) | 5.8 (5.5-6.0) | 1.6 (1.5-1.7) | 20.9 (20.3-21.6) |
| 30-39 | 1,972 | 103 (5.2) | 13.1 (12.7-13.6) | 5.6 (5.3-5.8) | 1.0 (0.9-1.1) | 20.5 (19.8-21.1) |
| 40-49 | 1,481 | 56 (3.8) | 7.7 (7.3-8.2) | 4.2 (4.0-4.5) | 1.5 (1.3-1.6) | 13.8 (13.2-14.4) |
| Sex † # | ||||||
| Male | 5,376 | 381 (7.1) | 17.8 (17.1-18.4) | 8.5 (8.1-8.9) | 1.6 (1.4-1.7) | 28.7 (27.8-29.6) |
| Female | 5,083 | 156 (3.1) | 7.9 (7.5-8.4) | 2.9 (2.7-3.1) | 0.9 (0.7-1.1) | 12.2 (11.4-12.9) |
|
PCMI quartiles in
Indian Rupees ‡ |
||||||
| ≤625 | 2,635 | 124 (4.7) | 12.3 (11.9-12.7) | 5.3 (5.1-5.6) | 0.9 (0.8-1.0) | 18.8 (18.2-19.5) |
| >625-1,100 | 2,483 | 135 (5.4) | 13.7 (13.2-14.1) | 5.8 (5.5-6.1) | 1.4 (1.3-1.6) | 21.7 (21.1-22.4) |
| >1,100-2,136 | 2,477 | 140 (5.7) | 13.4 (12.9-13.8) | 6.0 (5.7-6.2) | 2.3 (2.1-2.4) | 22.6 (22.0-23.2) |
| >2,136 | 2,522 | 132 (5.2) | 13.6 (13.2-14.1) | 6.0 (5.8-6.3) | 0.6 (0.5-0.7) | 20.9 (20.3-21.6) |
| Overall § | 10,459 | 537 (5.1) | 13.0 (12.6-13.4) | 5.8 (5.5-6.0) | 1.2 (1.1-1.4) | 20.7 (20.0-21.3) |
Sex-adjusted incidence
Age-adjusted incidence
Per capita monthly income; 1 US$ was approximately 44 Indian Rupees during the study period; data not available for 342 participants including 6 with RTI
Age-sex-adjusted incidence
p<0.001 for age and PCMI, and p<0.0079 for sex; Chi-square test
Data on recovery period missing for 17 participants
Data on treatment were available for 520 (97%) of the non-fatal RTI in the last 3 months. Of these 520 non-fatal RTI, medical treatment outside home was sought for 274 (52.7%) RTI of which 265 (96.7%) was as an out-patient. The overall annual incidence of non-fatal RTI for which medical treatment outside home was sought was 10.5 (95% CI 9.7 to 11.3; DE 1.83)/100 persons/year, and that as out-patient and in-patient was 10.1 (95% CI 9.4 to 10.9; DE 1.73) and 0.3 (95% CI 0.2 to 0.5; DE 1.02)/100 persons/year, respectively. Among the 9 people who were treated as in-patient, 5 (55.6%) were pedestrians and 4 (44.4%) were MTV users. The mean length of stay in the hospital was 4.67 days (median 3 days, range 1 to 15 days).
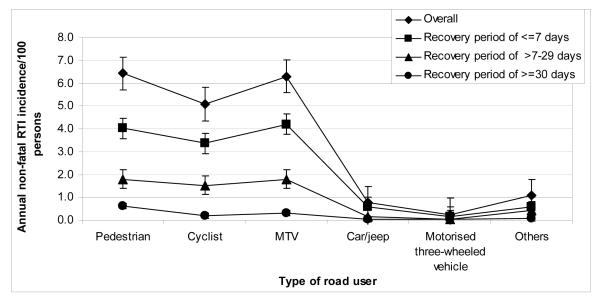
As shown in Figure 1, the overall estimated incidence rate for non-fatal RTI/100 persons/year was similar for pedestrian (6.4, 95% CI 5.7 to 7.2) and MTV users (6.3, 95% CI 5.6 to 7.0) and was slightly lower for cycle users (5.1, 95% CI 4.4 to 5.8). RTI as road users other than pedestrian, cycle or MTV users accounted for 10.4% of the overall RTI. Among the non-fatal RTI requiring recovery period of ≤7 and >7-29 days, the proportion of RTI as a pedestrian (31.2%) and MTV user (32.6%) was similar, and the proportion of RTI as a pedestrian was twice (48.5%) compared with MTV user (24.6%) among RTI requiring recovery period of ≥30 days.
Figure 1.
Estimated annual non-fatal road traffic injury incidence rate per 100 persons based on three-month recall period for the different types of road users. Bars represent 95% confidence interval. MTV stands for motorised two-wheeled vehicle and includes moped, luna, scooter, scooterette and motorcycle; Motorised three-wheeled vehicle are commercial passenger vehicles and include auto-rickshaw and seven-seater; Others include bus, tempo, van, lorry and truck.
The relative risk of overall RTI or that requiring recovery period of >7 days was significantly higher in the younger age groups with the highest in the 15-19 years age group, and was more than twice in males as compared with females (Table 2). The relative risk of overall RTI and of that requiring recovery period of >7 days was significantly higher in the third PCMI quartile as compared with the fourth (Table 2). The number of people with non-fatal RTI annually in Hyderabad aged 5-49 years was estimated to be 628,136 (95% CI 608,973 to 647,300) of whom an estimated 212,928 (33.9%) would need a recovery period of >7 days and 450,897 (71.8%) would be males (Table 2).
Table 2.
The relative risk of non-fatal RTI and the estimated burden in Hyderabad by age groups, sex and per capita monthly income (PCMI) among population aged 5-49 years in Hyderabad. CI denotes confidence interval.
| Variable | Relative risk of non-fatal RTI (95% CI)* |
Population of Hyderabad† |
Estimated number of people in Hyderabad with non- fatal RTI annually‡ (95% CI) |
||
|---|---|---|---|---|---|
| Overall | Recovery period of >7 days |
Overall | Recovery period of >7 days |
||
|
Age group
(years) |
|||||
| 5-9 | 1.13 (1.03-1.23) | 0.84 (0.72-0.99) | 412,581 | 64,363 (61,021-66,962) | 19,598 (18,277-20,918) |
| 10-14 | 1.70 (1.56-1.84) | 1.30 (1.13-1.50) | 451,834 | 106,181 (103,334-109,028) | 33,481 (32,035-34,927) |
| 15-19 | 2.17 (2.01-2.35) | 1.81 (1.59-2.07) | 446,968 | 134,671 (131,856-137,487) | 45,904 (44,473-47,334) |
| 20-29 | 1.51 (1.40-1.63) | 1.30 (1.15-1.47) | 783,387 | 163,885 (158,949-168,820) | 57,579 (55,072-60,086) |
| 30-39 | 1.48 (1.37-1.60) | 1.15 (1.01-1.32) | 558,585 | 114,286 (110,767-117,806) | 36,643 (34,856-38,431) |
| 40-49 | 1.00 | 1.00 | 388,468 | 53,686 (51,239-56,134) | 22,026 (20,783-23,269) |
| Sex | |||||
| Males | 2.36 (2.26-2.46) | 2.64 (2.43-2.86) | 1,571,619 | 450,897 (436,753-465,042) | 157,633 (149,775-165,491) |
| Females | 1.00 | 1.00 | 1,470,204 | 178,777 (168,044-189,509) | 55,721 (51,604-59,837) |
|
PCMI quartiles
in Indian Rupees § |
|||||
| ≤625 | 0.90 (0.85-0.95) | 0.93 (0.84-1.04) | |||
| >625-1,100 | 1.04 (0.98-1.10) | 1.09 (0.98-1.21) | |||
| >1,100-2,136 | 1.08 (1.02-1.14) | 1.24 (1.12-1.37) | |||
| >2,136 | 1.00 | 1.00 | |||
|
Total
(5-49 years) |
Not applicable | Not applicable | 3,041,823 | 628,136 (608,973-647,300) | 212,928 (203,194-222,661) |
40-49 years and females used as reference categories for age, sex and PCMI, respectively
Census Bureau of India[8]
Calculated from annual non-fatal RTI incidence based on three-months recall period
1 US$ was approximately 44 Indian Rupees during the study period; income distribution data for the Hyderabad population not available and therefore estimates not made for RTI numbers in Hyderabad for the PCMI quartiles.
Annual RTI mortality and disability rates
A total of 12 deaths due to RTI were reported in 5-49 years age group in the last 3 years, representing an estimated annual RTI mortality rate of 38.2/100,000 (95% CI 17.5 to 58.8; DE 1.00). Among these 12 deaths, 6 (50%) were on MTV, 4 (33.3%) were pedestrian, 1 (8.3%) in car/jeep, and 1 (8.3%) on cycle. Seven (26.9%) belonged to the first and second PCMI quartiles each, 9 (34.6%) to the third, 2 (7.7%) to the fourth PCMI quartile and PCMI data were not available for 1 death.
A total of 11 participants aged 5-49 years reported RTI related disability in the last 3 years representing an estimated annual RTI disability rate of 35.1/100,000 population (95% CI 12.4 to 57.7; DE 1.2). Eight (72.7%) were aged 30-49 years, 6 (54.5%) were males, and 3 (27.3%) belonged to the first and second PCMI quartiles each, 1 (9.1%) to the third, and 4 (36.4%) to the fourth PCMI quartile. Of them, 3 (27.3%) each were MTV user and pedestrian, 2 (18.2%) each were cycle and motorised three-wheeled vehicle user and 1 (9.1%) was car/jeep user. Four (36.4%) participants reported body structure related disabilities and 7 (63.6%) reported body function related disabilities.
DISCUSSION
This population-based study representative of the 5-49 years age group in Hyderabad city in India showed that nearly 1 in 14 people reported non-fatal RTI annually requiring a recovery period of >7 days, and an estimated 38 and 35 per 100,000 people die and are disabled due to RTI each year, respectively.
The annual incidence of RTI requiring more than 7 days of recovery was 6% and that requiring 30 or more days of recovery was 1.2% in this population. These rates are 184 and 32 times the annual deaths due to RTI in this population, respectively. These findings suggest that the magnitude of RTI is high, and is higher than that reported from developing countries.[15-21] We examined some possible reasons for this. The majority of the previously published population-based studies on incidence assessment of all types of injuries including RTI from other countries have reported data on RTI that had resulted in at least half/one day of loss of activities using 12-months recall period, and most of these had reported proxy data.[15-21] In order to get a more comprehensive picture of RTI, we documented all RTI irrespective of the severity or the number of days of loss of activity. We did not use proxy data for household members but collected data directly from all eligible household members except those 5-11 years old. We used a recall period of three-months to estimate the annual incidence of non-fatal RTI as recall bias is a major limitation for data on non-fatal injuries, and less severe injuries in particular are underestimated with longer recall periods.[22,23] Our data show that the decline in RTI incidence from 3- to 12-months recall period was nearly 50%. We also documented multiple RTI during the recall period in the same participant. It is known that injuries may be clustered in some individuals.[24] In addition, during the development and testing of the study questionnaire, it was observed that some events (such as fall/slip while alighting from a moving bus, crash between a pedestrian and a moving cycle) were not considered RTC by participants. Therefore, each participant was explained the definition of RTC and RTI to ensure that the information on these were not missed. This, we believe, has resulted in better RTI estimates.
We used the recovery status from RTI as an indicator of the severity of RTI. With 1 in 14 people aged 5-49 years requiring a recovery period of more than 7 days due to non-fatal RTI annually and half seeking treatment as an out-patient, the burden of RTI in this urban population is enormous. This burden was highest in young males. The over representation of young adults and males has been documented previously and is possibly related to their differential exposure to risk and in risk-taking.[1, 26-29] Interestingly, the non-fatal RTI incidence was similar across the PCMI quartiles for RTI requiring recovery period of less than 30 days. However, the two middle PCMI quartiles had higher incidence for RTI requiring recovery period of 30 days or more as compared with the lowest and highest PCMI quartiles. Socioeconomic status is known to be a risk factor for injury including RTI, and mortality and morbidity rates in vulnerable road users have been reported to be higher in the lower social classes.[1, 27, 30-31] However, a cohort study from rural Vietnam did not find poverty either as a risk or protective factor for RTI and the middle income group was exposed to the highest risk of RTI.[24] We used per capita monthly income as a measure of socioeconomic status; other indicators such as education, occupation and household expenditure have also been used previously. Further research is needed to better understand the seemingly complex association of socioeconomic status with RTI.
Eighty five percent of non-fatal RTI were accounted for by the pedestrians, MTV and cycle users. The predominance of these road users correlates with the previously published data which show that these groups are over-represented in RTI at the global level.[1] In Hyderabad, there has been a phenomenal increase in vehicles on the road in the last three decades, 90.7% from 1981 to 2001, respectively.[9] Such an increase would be expected to result in increased risk of RTI for the vulnerable road users. MTV account for the majority of vehicles in Hyderabad.[9] An interesting finding was that RTI incidence as MTV user increased with increasing per capita income. In our population, MTV ownership increased with increasing PCMI (p<0.001; unpublished data). The cost of MTV in India ranges from US$ 750 to 1500 and is higher than the annual per capita gross domestic product for India (US$ 736).[32] The higher ownership of MTV with increasing income can explain the higher RTI incidence as MTV user with increasing income in our population.
The annual RTI mortality rate per 100,000 in the 5-49 years age group was 38.2 (95% CI 17.5 to 58.8). This study was not powered to measure RTI mortality rate as the required sample size for such an assessment would be very large, and the wide confidence intervals highlight the importance of a reasonable sample size to arrive at reliable RTI mortality estimates. The point estimate of RTI mortality in our urban population aged 5-49 years is nearly twice that reported by the GBD Study.[5] The GBD estimates are for all ages and the entire country including rural areas where the RTI mortality rate is estimated to be lower, and are projected estimates due to non-availability of complete death registration data.[5] Our mortality rate is comparable to a previous assessment for all ages carried out in south India (34/100,000 population) which included rural and urban populations; this sample had over-representation of the poor population.[33] The burden of disability due to RTI was similar to that of mortality in our population. It is estimated that 2.1% of the Indian population has some form of disability of which 69% is in the 5-49 years age group, [34] and that injuries are responsible for one-third of these disabilities with RTI contributing nearly half to injury disability.[35]
RTI are responsible for significant loss of life, disability, and economic loss in this population as the young and economically productive age group is affected. However, limited research on RTI is available from India.[36-37] The lack of an appropriate response and resources for RTI prevention is further highlighted when compared with HIV/AIDS, another disease affecting the young and economically productive age group that has a mortality rate (37.5/100,000) similar to that of RTI in India.[5] The resource allocation for HIV/AIDS was 13.5 times more (US$ 469.2 million) as compared with that for road safety (US$ 34.7 million) in the last 5 years in India.[38-39] There is nearly a four-fold increase in the funds allocated for HIV/AIDS over the next 5 years.[38] Clearly, the low allocation of funds for research and evidence-based road safety interventions needs to be enhanced to reduce the RTI burden in India.
As reliable estimation of the RTI burden is a critical first step for informing RTI prevention, data from well-designed population-based studies are needed to provide better understanding of this burden. This study has demonstrated that there is a high burden of RTI in this urban population. In the background of the recent interest by the Government of India to address RTI,[40] these findings could assist in raising the profile of RTI as a public health problem which needs to be addressed as a preventable cause of mortality and morbidity, and to plan appropriate interventions for it.
KEY MESSAGES.
What is already known?
Road traffic injuries are an increasing problem in India
Limited data available on the magnitude of road traffic injuries
Data mainly available from hospital records
What this study adds?
1 in 14 people in the 5-49 years age group reported road traffic injuries annually requiring a recovery period of more than 7 days in this urban population
Incidence of non-fatal road traffic injuries similar across per capita income quartiles
An estimated 38 per 100,000 people die and a similar number are disabled annually due to road traffic injuries in this urban Indian population
ACKNOWLEDGMENTS
The authors acknowledge the contribution of N Balaji Rao, D Ram Babu, K Bhagawan Babu and YRK Satya Prasad in the implementation of this study.
FUNDING This study was supported by the Wellcome Trust, UK (077002/Z/05/Z). R Dandona is supported in part by the National Health and Medical Research Council Capacity Building Grant in Injury Prevention and Trauma Care, Australia.
LIST OF ABBREVIATIONS USED
- CI
Confidence interval
- DE
Design effect
- MTV
Motorised two-wheeled vehicle
- PCMI
Per capita monthly income
- RTC
Road traffic crash
- RTI
Road traffic injuries
Footnotes
COMPETING INTERESTS None.
REFERENCES
- 1.Peden M, Scurfield R, Sleet D, et al. World report on road traffic injury prevention. World Health Organization; Geneva: 2004. [Google Scholar]
- 2.World Health Organization Global Burden of Disease Project Revised Global Burden of Disease 2002 Estimates. [Accessed 29 April 2008]. ( http://www.who.int/healthinfo/statistics/gbdwhoregionmortality2002.xls)
- 3.Kopits E, Cropper ML. Traffic Fatalities and Economic Growth. 2003. World Bank Policy Research Working Paper No. 3035. [DOI] [PubMed]
- 4.Ameratunga S, Hijar M, Norton R. Road traffic injuries: confronting disparities to address a global-health problem. Lancet. 2006;367:1533–40. doi: 10.1016/S0140-6736(06)68654-6. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization Cause of death and burden of disease estimates by country. [Accessed 29 April 2008]. 2002. ( http://www.who.int/healthinfo/statistics/bodgbddeathdalyestimates.xls)
- 6.Dandona R. Making road safety a public health concern with policy makers in India. Natl Med J India. 2006;19:126–33. [PubMed] [Google Scholar]
- 7.Dandona R, Mishra A. Deaths due to road traffic crashes in Hyderabad city in India: need for strengthening surveillance. Natl Med J India. 2004;17:74–9. [PubMed] [Google Scholar]
- 8.Registrar General of India . Population Totals: India, Census of India 2001. Ministry of Home Affairs, Government of India; New Delhi: [Accessed 20 April 2008]. ( http://www.censusindia.gov.in/Census_Data_2001/Census_Data_Online/Population/Total_Population.aspx) [Google Scholar]
- 9.Category-wise vehicular strength in twin cities. Government of Andhra Pradesh; Hyderabad: [Accessed 3 May 2008]. ( http://www.aptransport.org/html/veh_strength.htm) [Google Scholar]
- 10.Registrar General of India . Andhra Pradesh, Census of India 2001, Primary Census Abstract. Ministry of Home Affairs, Government of India; New Delhi: 2005. Data Product No. 00-63-2001-Cen-CD. [Google Scholar]
- 11.Director of Census Andhra Pradesh . Andhra Pradesh, Census of India 2001, Primary Census Abstract. Directorate of Census Operations, Government of Andhra Pradesh; Hyderabad: 2005. p. 671. [Google Scholar]
- 12.National Crimes Records Bureau . Accidental deaths and suicides in India – 2001. Ministry of Home Affairs, Government of India; New Delhi: 2001. [Google Scholar]
- 13.Rosner B. Fundamentals of Biostatistics. 2nd edition PWS Publishers; Boston: 1986. pp. 84–92.pp. 302–68.pp. 404–8. [Google Scholar]
- 14.Bennett S, Woods T, Liyanage WM, et al. A simplified general method of cluster-sample surveys of health in developing countries. World Health Stat Quart. 1991;44:98–106. [PubMed] [Google Scholar]
- 15.Mock CN, Abantanga F, Cummings P, et al. Incidence and outcome of injury in Ghana: a community-based survey. Bull World Health Organ. 1999;77:955–64. [PMC free article] [PubMed] [Google Scholar]
- 16.Nordberg E, Kimani V, Diwan V. Household survey of injuries in a Kenyan district. East Afr Med J. 2000;77:240–4. doi: 10.4314/eamj.v77i5.46626. [DOI] [PubMed] [Google Scholar]
- 17.Ghaffar A, Hyder AA, Masud TI. The burden of road traffic injuries in developing countries: the 1st national injury survey of Pakistan. Public Health. 2004;118:211–7. doi: 10.1016/j.puhe.2003.05.003. [DOI] [PubMed] [Google Scholar]
- 18.Kobusingye O, Guwatudde D, Lett R. Injury patterns in rural and urban Uganda. Inj Prev. 2001;7:46–50. doi: 10.1136/ip.7.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moshiro C, Heuch I, Astrøm AN, et al. Injury morbidity in an urban and a rural area in Tanzania: an epidemiological survey. BMC Public Health. 2005;28(5):11. doi: 10.1186/1471-2458-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fatmi Z, Hadden WC, Razzak J, et al. Incidence, patterns and severity of reported unintentional injuries in Pakistan for persons 5 years and older: results from the National Health Survey of Pakistan 1990-94. BMC Public Health. 2007;7:152. doi: 10.1186/1471-2458-7-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hang HM, Bach TT, Byass P. Unintentional injuries over a 1-year period in a rural Vietnamese community: describing an iceberg. Public Health. 2005;119:466–73. doi: 10.1016/j.puhe.2004.08.022. [DOI] [PubMed] [Google Scholar]
- 22.Mock C, Acheampong F, Adjei S, et al. The effect of recall on estimation of incidence rates for injury in Ghana. Int J Epidemiol. 1999;28:750–5. doi: 10.1093/ije/28.4.750. [DOI] [PubMed] [Google Scholar]
- 23.Moshiro C, Heuch I, Astrøm AN, et al. Effect of recall on estimation of non-fatal injury rates: a community based study in Tanzania. Inj Prev. 2005;11:48–52. doi: 10.1136/ip.2004.005645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thanh NX, Hang HM, Chuc NT, et al. Does poverty lead to non-fatal unintentional injuries in rural Vietnam? Int J Inj Contr Saf Promot. 2005;12:31–7. doi: 10.1080/17457300512331342207. [DOI] [PubMed] [Google Scholar]
- 25.Peden M, McGee K, Sharma G. The injury chart book: a graphical overview of the global burden of injuries. World Health Organization; Geneva: 2002. [Google Scholar]
- 26.Odero W, Garner P, Zwi A. Road traffic injuries in developing countries: a comprehensive review of epidemiological studies. Trop Med Int Health. 1997;2:445–60. [PubMed] [Google Scholar]
- 27.Nantulya VM, Reich M. The neglected epidemic: road traffic injuries in developing countries. BMJ. 2002;324:1139–41. doi: 10.1136/bmj.324.7346.1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dandona R, Kumar GA, Dandona L. Risky behaviour of drivers of motorised two wheeled vehicles in India. Journal Saf Res. 2006;37:149–58. doi: 10.1016/j.jsr.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 29.Dandona R, Kumar GA, Dandona L. Traffic law enforcement in Hyderabad, India. Int J Inj Control Saf Promot. 2005;12:167–76. doi: 10.1080/17457300500088840. [DOI] [PubMed] [Google Scholar]
- 30.Nantulya V, Reich M. Equity dimensions of road traffic injuries in low- and middle-income countries. Inj Control Saf Promot. 2003;10:13–20. doi: 10.1076/icsp.10.1.13.14116. [DOI] [PubMed] [Google Scholar]
- 31.Laflamme L, Diderichsend F. Social differences in traffic injury risks in childhood and youth – a literature review and a research agenda. Inj Prev. 2000;6:293–8. doi: 10.1136/ip.6.4.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Human Development Report 2007-8. Fighting climate change: human solidarity in a divided world. [Accessed 15 May 2008]. ( http://hdrstats.undp.org/countries/data_sheets/cty_ds_IND.html)
- 33.Aeron-Thomas A, Jacobs GD, Sexton B, et al. The involvement and impact of road crashes on the poor: Bangladesh and India case studies. Transport Research Laboratory (TRL); Crowthrone: 2004. TRL Published Project Report 010. [Google Scholar]
- 34.Registrar General of India . C-20: Disabled population by type of disability, age and sex, Census of India 2001. Ministry of Home Affairs, Government of India; New Delhi: [Accessed 3 April 2008]. 2001. ( http://www.censusindia.gov.in/Tables_Published/C-Series/c_series_tables_2001.aspx) [Google Scholar]
- 35.Gururaj G. Injuries in India: a national perspective. National Commission on Macroeconomics and Health. Ministry of Health & Family Welfare, Government of India; New Delhi: [Accessed 3 April 2008]. ( www.whoindia.org/LinkFiles/Commision_on_Macroeconomic_and_Health_Bg_P2__Injury_in_India.pdf) [Google Scholar]
- 36.Dandona L, Sivan YS, Jyothi MN, et al. The lack of public health research output from India. BMC Public Health. 2004;4:55. doi: 10.1186/1471-2458-4-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Garg N, Hyder AA. Road traffic injuries in India: a review of the literature. Scan J Pub Health. 2006;34:100–9. doi: 10.1080/14034940510032149. [DOI] [PubMed] [Google Scholar]
- 38.National AIDS Control Organisation Source of Funding of NACP III. [Accessed 2 May 2008]. ( http://www.nacoonline.org/About_NACO/Funds_and_Expenditures/)
- 39.Planning Commission of India The working group report on road transport for the Eleventh Five Year Plan. [Accessed 2 May 2008]. ( http://planningcommission.gov.in/aboutus/committee/wrkgrp11/wg11_roadtpt.doc)
- 40.Indian Council of Medical Research Publications. [Accessed 20 May 2008]. ( http://www.icmr.nic.in/publication.html)