What is primary healthcare?
Primary healthcare is about providing ‘essential healthcare’ which is universally accessible to individuals and families in the community and provided as close as possible to where people live and work. It refers to care which is based on the needs of the population. It is decentralised and requires the active participation of the community and family.1
Providing mental health services in primary healthcare involves diagnosing and treating people with mental disorders; putting in place strategies to prevent mental disorders and ensuring that primary heathcare workers are able to apply key psychosocial and behavioural science skills, for example, interviewing, counselling and interpersonal skills, in their day to day work in order to improve overall health outcomes in primary healthcare.
Integrated primary mental health services are complementary with tertiary and secondary level mental health services (see the ‘optimal mix of services’ information sheet), e.g. general hospital services (short stay wards, and consultation-liaison services to other medical departments), which can manage acute episodes of mental illness quite well but do not provide a solution for people with chronic disorders who end up in the admission–discharge–admission (revolving door syndrome) unless backed up by comprehensive primary healthcare services or community services.
Integrating specialised health services – such as mental health services – into PHC is one of WHO's most fundamental health care recommendations.2
Rationale for integrating mental health services into primary healthcare
There are many advantages for integrating mental health services into primary healthcare:
Reduced stigma for people with mental disorders and their families
Because primary healthcare services are not associated with any specific health conditions, stigma is reduced when seeking mental healthcare from a primary healthcare provider (compared to a stand-alone specialised service), making this level of care far more acceptable – and therefore accessible – for most users and families.
Improved access to care
Integrated care helps to improve access to mental health services and treatment of co-morbid physical conditions.
Comorbidity
Mental health is often comorbid with many physical health problems such as cancer, HIV/AIDS, diabetes and tuberculosis, among others. The presence of substantial comorbidity has serious implications for the identification, treatment and rehabilitation of affected individuals. When primary healthcare workers have received some mental health training they can attend to the physical health needs of people with mental disorders as well as the mental health needs of those suffering from infectious and chronic diseases. This will lead to better health outcomes.
Improved prevention and detection of mental disorders
Primary healthcare workers are frontline formal health professionals, ‘the first level of contact of individuals, the family and community with the national health system’.1 Equipping these workers with mental health skills promotes a more holistic approach to patient care and ensures both improved diction and prevention of mental disorders.
Treatment and follow-up of mental disorders
People who are diagnosed with a mental disorder are often unable to access any treatment for their mental health problems. By providing mental health services in primary healthcare, more people will be able to receive the mental healthcare they need because of:
better physical accessibility. Primary healthcare is ‘the first level of contact (the closest and the easiest to access) of individuals, the family and community with the national health system’1
better financial accessibility. When consulting in hospitals, indirect health expenditures (transportation, loss of productivity related to the time spent in accompanying the patient to hospital, etc) add to the cost of consultation and medications. If mental health services are integrated into primary healthcare, healthcare costs are greatly reduced/minimal
better acceptability. Linked to reduced stigma and easier communication with healthcare providers (e.g. reduced language and cultural barriers, better knowledge of the user's personality and personal and familial background/history).
Reduced chronicity and improved social integration, both for the people with mental disorders and his/her household
When people are treated far from their homes, it disrupts normal daily life, employment and family life; it removes individuals from their normal supports, essential to recovery, and it imposes more burden on families and care givers. By providing services in primary healthcare the burden on individuals, families and society will be reduced, household productivity and social integration will be maintained, resulting in better chances of recovery.
Human rights protection
Providing treatment at primary healthcare, backed by secondary health care and informal community care can prevent people from being admitted into psychiatric institutions often associated with human rights violations.
The reduced stigma associated with receiving care in primary healthcare settings can also mean people with mental disorders and their families are less likely to experience discrimination within society.
Better health outcomes for people treated in primary healthcare
In terms of clinical outcomes it has been found that, for most common mental disorders, primary health-care can deliver good care and certainly better care than that provided in psychiatric hospitals.
Improving human resource capacity for mental health
Integrating mental health services into primary healthcare can be an important solution to addressing human resource shortages to deliver mental health interventions.
Challenges to overcome for successful integration
Integration of mental health services requires a lot of careful planning and there are likely to be several issues and challenges that will need to be addressed.
For example:
integration into primary healthcare requires investment in the training of staff to detect and treat mental disorders
within the context of training, primary health-care workers may be uncomfortable in dealing with mental disorders and may also question their role in managing disorders. Therefore, in addition to imparting skills, training also needs to address the overall reluctance of primary healthcare workers to work with people with mental disorders
the issue of availability of time also needs to be addressed. In many countries primary health-care staff are overburdened with work as they are expected to deliver multiple healthcare programmes. Governments can not ignore the need to increase the numbers of primary healthcare staff if they are to take on additional mental health work
adequate supervision of primary care staff is another key issue which needs to be addressed if integration is to succeed. Mental health professionals should be available regularly to primary care staff to give advice as well as guidance on management and treatment of people with mental disorders. Furthermore the absence of a good referral system between primary and secondary care can severely undermine the effectiveness of mental healthcare delivered at primary health-care level
finally, governments must pay attention to key human resource management issues in primary healthcare – adequate working conditions, payment, resources and support to carry out demanding work.
WHO key recommendations for integration
Preliminary situational analysis
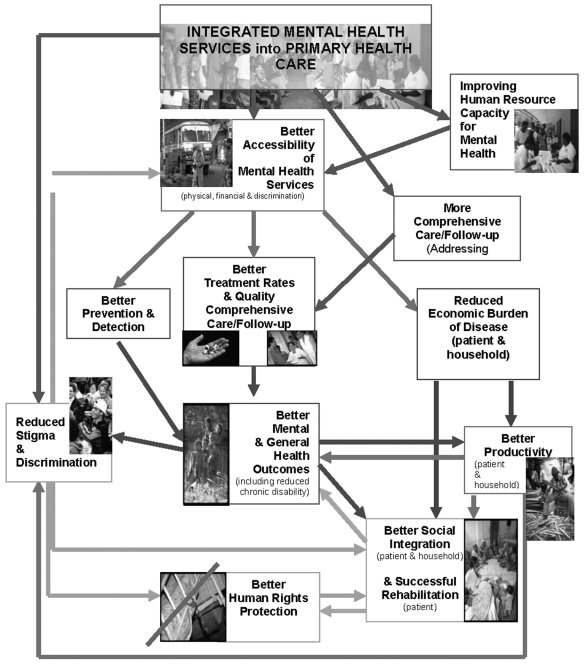
Integration requires a careful analysis of the best options for the treatment and care of mental disorders at different levels of care (see Figure 1). The specific ways in which mental health should be integrated into primary healthcare will be influenced by the current function, status and strengths of primary, secondary and tertiary care levels within countries' existing health systems as well as the community context.
Figure 1.
Rationale for integrating mental health services into primary healthcare
Build one existing networks/structures and human resources
As far as possible, and as long as consistent with the international standards of good practices, countries must look at using and strengthening existing networks of services, including those in primary health-care, to provide mental health services.
Funding
Funds must be shifted/redistributed from tertiary to secondary and primary levels of care (and/or community oriented mental health services), or new funds must be made available.
Clear delineation of mental disorders
The delineation of a few targeted mental disorders to be treated at the primary care level in some contexts can be desirable. It simplifies both the requirements for types of medicine (limited list of psychotropic medications) and the training of primary care workers who then need to be proficient and skilled in the use of a few selected drugs. The range of disorders can be increased in a stepped manner according to capacity and needs.
Human resource training and competencies
Integration into primary healthcare requires training of primary care staff in identification and treatment of mental disorders. The training of established primary care teams should occur in service settings and should involve programmes in diagnosis, management, and follow-up consultations as well as human rights and family intervention.
General health staff must have the knowledge, skills and motivation to treat and manage patients suffering from mental disorders. A mental health component should be included in the educational curriculum of all social and health workers and ongoing training and support provided on site.
Recruitment/education of new PHC staff
In some countries, primary care staff are already overburdened with work and integration of mental healthcare into primary healthcare will require and increase in the absolute numbers of primary care staff. There need to be sufficient numbers of staff with the knowledge and authority to prescribe psychotropic medicines at primary and secondary levels.
Availability of medicines
Basic psychotropic medicines must be available at primary and secondary care levels. Governments need to ensure that sufficient funds are allocated to purchase the basic essential psychotropic medicines and make sure they are available in primary care settings, in accordance with the policy adopted. Medicines may be purchased under generic names from non-profit organisations, allowing access to drugs of good quality at low prices.
Supervision and support of primary healthcare staff
Primary healthcare staff have to be adequately supervised, monitored and supported by mental health specialists (professional at/of secondary level) if integration is to succeed. The mental health professional should be available to discuss difficulties in management and to provide advice on interventions to be carried out by primary care staff.
Effective referral system and coordination of a collaborative network
Effective referral links between primary, secondary and tertiary levels of care need to be in place. It is recommended to develop and coordinate a collaborative network in order to provide mental health services.
Intersectoral approach and links with community services, both formal and informal
An intersectoral approach and collaboration will enhance the success of a primary healthcare approach – collaboration with non-health sectors such as education, social welfare, justice or employment/labour both at the policy, the planning and the implementation/service levels will be required.
Many mental disorders require psychosocial solutions. Thus, links need to be established between mental health services and various community agencies at the local level so that appropriate housing, income support, disability benefits, employment, and other social service supports are mobilised for people with mental disorders and in order that prevention and rehabilitation strategies can be more effectively implemented.
Close links with the informal community services is also fundamental – NGOs, religious leaders and other systems of support – and will lead to better outcomes and rationalisation of resources.
Recording systems for evaluation and monitoring
Recording systems need to be set up to allow for continuous monitoring, evaluation and updating of mental health activities: mental health data need to be routinely recorded in patients' files and integrated in the overall general health information system at primary healthcare level, in order to be used for monitoring, evaluation and planning and service improvements.
Biography
This document is reproduced with the kind permission of WHO and WONCA
The authors are staff members of the World Health Organization. The authors alone are responsible for the views expressed in this publication and they do not necessarily represent the decisions, policy or views of the World Health Organization.
REFERENCES
- 1.WHO Declaration of Alma-Ata International Conference on Primary Health Care, Alma-Ata, USSR, 6–12 September, 1978. www.who.int/hpr/NPH/docs/declaration_almaata.pdf(accessed 25 April 2007) [PubMed] [Google Scholar]
- 2.WHO The World Health Report 2001. Mental Health: New Understanding, New Hope Geneva: World Health Organization, 2001www.who.int/whr/2001/en/whr01_en.pdf(accessed 23 April 2007). [Google Scholar]
FURTHER READING
The WHO Mental Health Policy & Service Development Guidance Package. WHO Mental Health Policy and Service Guidance Package (13 modules). www.who.int/mental_health/policy/en (accessed 23 April 2007)
Mental health policy, plans and programme (updated version). Geneva, World Health Organization, 2005 (Mental Health Policy and Service Guidance Package).
Monitoring and Evaluation of Mental Health Policies and Plans. Geneva, World Health Organization, 2007 (Mental Health Policy and Service Guidance Package).
Organization of Services. Geneva, World Health Organization, 2003 (Mental Health Policy and Service Guidance Package).
USEFUL LINKS
Mental Health Policy & Service Development Guidance Package
www.who.int/mental_health/policy/essential package1/en/index.html
Wonca
The WHO MIND Project
www.who.int/mental_health/policy/WHO% 20MIND%20Brochure_English.pdf
Best Practices examples, a selection of Country Summaries and official documents
www.who.int/mental_health/policy/country/countrysummary/en/index.html.
KEY CONTACTS
Mental Health Policy and Service Development Team, Department of Mental Health and Substance Abuse, WHO Geneva
Dr Michelle Funk (Coordinator)
Email: funkm@who.int
Ms Natalie Drew and Dr Edwige Faydi (Technical Officers)
Email: drewn@who.int/faydie@who.int; tel: +41 (22) 791 38 55; fax: +41 (22) 791 38 40.
Wonca Working Party on Mental Health
Dr Gabriel Ivbijaro (Chair)
Email: gabriel.ivbijaro@gmail.com
Yvonne Chung (Wonca Secretariat)
Email: admin@wonca.com.sg; tel +(65) 6224 2886; fax: + (65) 6324 2029.