Abstract
Introduction Depression is a common and debilitating condition. A body of evidence exists about improving depression outcomes in primary care, using collaborative care models. Such approaches, however, have not been routinely adopted within general practice settings. In this paper we outline the results of an audit of an enhanced care initiative that trained practice nurses to deliver such approaches.
Method An audit of symptom outcome and satisfaction was conducted in depression case-management clinics run by practice nurses. Results were then benchmarked against appropriate randomised trial data. The cost of practice nurse time devoted to the delivery of the service was estimated by multiplying time by unit cost.
Results A mean change of 9.07 (standard deviation (SD) 6.67, 95% confidence interval (CI) 7.93–10.22, P < 0.001) points on the Patient Health Questionnaire (PHQ9) score was observed in those who were using/had used the service. Clinical change demonstrated a shift from moderate-to-severe to mild depression. The results reflect the changes seen in randomised controlled trial data from similar interventions in similar samples, and are superior to expected treatment as usual outcomes. Overall, respondents were ‘very satisfied’ with the service on offer. The mean cost of practice nurse time was estimated at £45 per patient.
Discussion While acknowledging the limitations of audit data, practice nurses in general practice appear to be able to offer effective and acceptable case management to patients experiencing depression.
Keywords: depression, depression case management, practice nurses, primary care
Introduction
Depression is a common disorder which affects approximately 5–10% of the British population.1 It is the third most common reason for primary care consultation within the UK,2 and up to 95% of depression treatment in the UK is provided in primary care.3 Depression is a debilitating illness, resulting in significant distress and disability, 4 and the cost of depression treated by primary care practitioners has been estimated at nearly twice that of inpatient mental health services.5 Common mental health problems have large financial implications for the UK. Layard calculated a total economic cost of approximately £25 billion, which equates to over 2% of the gross domestic product; this figure includes lost output, lost tax, benefits and public expenditure on mental health services.6 The implementation of guidelines such as those of the National Institute for Health and Clinical Excellence (NICE) for depression management,7 and national enhanced services for depression under the new General Medical Services (GMS) contract (2003), aims to identify more cases at an earlier stage. High-volume quick-access services are advocated to meet the demands laid on services of such high-prevalence conditions.3
NICE guidelines recommend cognitive behavioural therapy (CBT) as the treatment of choice for mild-to-moderate depression; however, significant problems with access exist, and consequently antidepressant medication is the most common primary care intervention at a staggering cost to the NHS.8 There is a need for services to enhance this intervention in a way that is accessible to the primary care population.9,10
Collaborative care has a positive effect upon depression outcomes at 6 months, and at up to 18 months post-treatment in comparison to standard care, according to a meta-analysis of 37 randomised trials (12 355 subjects).11 It can include a range of interventions ranging from simple follow-up to more complex support.11 Collaborative care is based upon a chronic care model including a multiprofessional approach, with evidence-based protocols to organise patient management, enhance both pharmacological and psychological interventions, schedule follow-up and define interprofessional communication.12 Indications are that this is a cost-effective intervention.13 Central to the collaborative care approach is the case manager,11 who:
proactively follows up patients
assesses patient adherence to psychological and pharmacological treatments
monitors patient progress
takes action when treatment is unsuccessful
delivers psychological support.
While most trials have been conducted in the USA, raising questions about its effectiveness in countries with better-resourced primary care systems,11,12 recent evidence suggests it can successfully transfer to a UK setting.14
Depression case-management service
As part of a collaborative, a telephone-based depression case-management service run by practice nurses was developed to support patients with moderate-to-severe depression, using evidence-based interventions. The service was located in a number of general practitioner (GP) practices in the North East of England. Each practice covered mixed rural and urban areas, with populations across a broad range of socio-economic status. The mean list size of practices using the service was 9200 (range 7400–10 400), with between five and seven GPs per practice. This collaborative care service uses a multidisciplinary team, including a practice nurse, GP and community psychiatric nurse (CPN). The proposed benefit of this service is the availability of structured support for a high volume of patients at a low intensity level-henceenhancing primary care depression treatment. GPs refer patients for practice nurse support during a depressive episode and to have progress/treatment carefully monitored. Practice nurses running this service attend a three-day skills-focused training programme. Training includes teaching on depression and its symptoms, structure and practice of contacts, assessing progress using a nine-item depression symptom scale (Patient Health Questionnaire, PHQ9),15 and psychological support approaches. The initial meeting between the practice nurse and the patient takes place face to face in the surgery, and the remaining sessions are conducted primarily via telephone. The practice nurse intervention has a specific structure and addresses the following:
medication management including discussion of difficulties with prescribed medications, education about response times, and side-effects and their management, and problem solving any concordance issues
behavioural activation, 16 which is a review of the relationship between activity and mood, the discussion of self-help information relating to this, and the patient's use of activity planning
the assessment of depression symptom level using the PHQ9, discussion of changes seen and review of any risk factors identified. The PHQ9 was considered a suitable tool for this purpose as it is a valid measure of depression,15 with excellent test–retest reliability and detail of minimal clinically important difference (MCID)17
the identification of those patients who are not responding (based upon MCID) for discussion in regular case review sessions with the attached CPN and/or GP if immediate action is required.
Further details of the structure and evaluation of training and the intervention are available elsewhere.18
This paper outlines the audit process used to examine the impact of interventions on symptom level outcomes and satisfaction delivered in routine primary care clinics, carried out by a group of practice nurses after their training as part of this collaborative.
Method
Treatment data collection
Practice nurses running depression case-management services within their practice were asked to collect routine data (depression symptom level scores, service response rate, number of failed planned phone calls, medication and basic demographic details) from the clinical records of all patients who had received or were current recipients of the service. All data were collected between April and July 2007 in an anonymous format. Data were then collated and entered into SPSS version 16 for windows (RW).
Patient satisfaction with the service was assessed using a questionnaire with fixed response options (very satisfied, satisfied, neither satisfied nor unsatisfied, unsatisfied) to provide categorical data with an option for free text comment. Respondents remained anonymous.
The audit was approved and requested by the local primary care trust, in line with UK national guidance.19
Audit data
Statistical analysis
Statistical analysis of PHQ9 depression symptom level scores was conducted using paired sample means testing to explore the within-group change observed over time. A second analysis was conducted, selecting only those individuals who had at this point received an adequate ‘dose’ of intervention, as defined by six or more contacts.
Clinical effectiveness
Estimation of the clinical effectiveness of the service was conducted using predefined severity categories, MCID and normative data of the PHQ9. Individual patient scores were categorised pre- and post-treatment, relating to severity and the number of patients in each category observed at each time point. The rate of MCID between observations was established by calculating the number of patients who had a reduction of five points or more in their PHQ9 score. The number of patients achieving clinically significant improvement was estimated by observing the relationship of the PHQ9 scores in our service to the PHQ9 scores seen in non-depressed samples (mean 3.3, standard deviation (SD) 3.8). Clinically significant change was assumed when a patient's PHQ9 score pre-treatment was greater than the normal population mean plus two standard deviations and reduced to within one standard deviation of that mean post-treatment. In addition the number of patients experiencing a 50% drop in PHQ9 scores was calculated, a measure of clinical improvement commonly found in primary care depression trials and audits.
Clinical audit standards
The standard was chosen from controlled trial evidence, which included usual-care controls in samples reflective of our service.13,14,20–22 To make comparisons between different tools measuring the same clinical observation (depression symptom level), data were converted to paired sample effect sizes. Mean change was divided by pre-treatment standard deviation to allow for effect sizes to be consistent with both parallel and crossover trial designs.
The direct costs of the practice nurse involvement were estimated by multiplying practice nurse unit costs,23 with mean contact and missed call rates, allowing for 15 minute call times and 5 minute missed call time. The worst case was calculated by taking mean plus standard deviation scores for both observations, and multiplying by unit costs.
Results
Patient characteristics
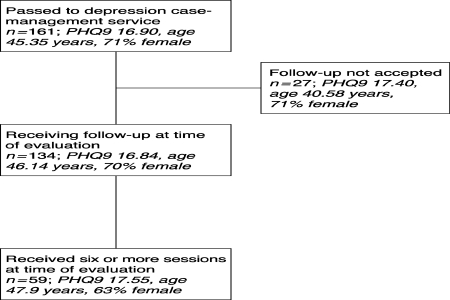
Treatment data were collected on 161 patients referred to the service with a new diagnosis of depression. One-hundred and thirty-four (83%) accepted case management (for patient flow see Figure 1). Demographic data were available on 121 (75%) patients. The mean age of patients was 45.35 years (SD 15.64, range 18–84), and 18 (15%) patients were over the age of 60 years; 86 (71%) were female. Employment status was available for 72 (43%) patients, of whom 38 (52%) were employed, nine (12.5%) were unemployed, 16 (22%) were retired, and of the remainder, eight were carers (11%) and there was one student (1.4%). The patient characteristics seen in this sample are reflective of the practice populations. The mean number of contacts was 5.51 (SD 3.17), with mean number of missed calls of 2.18 (SD 2.48). Patients were seen in four GP practices by six practice nurses. The mean time to first follow-up contact post-diagnosis and instigation of treatment was 5.83 (SD 4.41) days.
Figure 1.
Patient status at time of audit. Number in italics outline baseline PHQ9 score, age and proportion of females in each group
Data were available on medication prescriptions for 113 patients; 20 received no prescription (18%) and 93 (82%) were prescribed. Selective serotonin reuptake inhibitors were the most common medication used in 83 cases, tricyclic and related anti-depressants in five cases, other antidepressants in two cases and beta-blockers/benzodiazepines in three cases (see Table 1).
Table 1.
Baseline demographic data (presented as n (%) unless stated otherwise)
| All patients passed to service | Those not accepting service | Those accepting service | Those receiving six or more contacts | |
|---|---|---|---|---|
| Mean age (SD), years | 45.35 (15.64); n = 121 | 40.58 (15.73); n = 17 | 46.14 (15.57); n = 104 | 47.9 (15.9); n = 59 |
| Sex | 86 (71%) female, 35 (29%) male | 13 (76.5%) female, 4 (23.5%) male | 73 (70.2%) female, 31(29.8%) male | 37 (63%) female, 22 (37%) male |
| Employment status | 38 (53%) employed, 9 (12.5%) unemployed, 16 (22%) retired, 9 (12.5%) other | 3 (23%) employed, 3 (23%) unemployed, 5 (38%) retired, 2 (16%) other | 35 (59%) employed, 6 (10%) unemployed, 11 (19%) retired, 7 (12%) other | 15 (63%) employed, 2 (9%) unemployed, 5 (20%) retired, 2 (8%) other |
| Mean Baseline PHQ9 score (SD) | 16.90 (4.80), n = 161 | 17.40 (5.5), n = 27 | 16.84 (4.88), n = 134 | 17.55(4.88), n = 59 |
| Medication use | 24 (20%) no prescription, 97 (80%) prescribed | 3 (17%) no prescription, 14 (83%) prescribed | 20 (19%) no prescription, 84 (81%) prescribed | 20 (19%) no prescription, 84 (81%) prescribed |
Analysis of symptom level change during depression case management
Mean symptom level across the whole group identified at baseline (n = 161) was 16.90 (SD 4.80), and of those who accepted follow-up (n = 134) 16.84 (SD 4.88), which equates to the moderate-to-severe category for depression. Mean post-treatment PHQ9 score was 7.76 (SD 6.56, n = 134), indicating a mean positive change in depression symptom level of 9.07 (SD 6.67, 95% confidence interval (CI) 7.93–10.22, P < 0.001) points on the PHQ9 measure. Selecting those patients with six or more contacts, this difference was increased to 11.51 (n = 59, SD 7.20, 95% CI 9.63–13.39, P < 0.001).
Clinical effectiveness
The majority of patients in the pre-treatment group suffered from moderate-to-severe depression pre-treatment (n = 85, 64%). This decreased at post-treatment assessment (n = 24, 18%). The majority of patients fell below 10 points on the PHQ9, post-intervention (n = 95, 71%), indicating they were experiencing minimal symptoms. Of the 85 patients in the moderate-to-severe or severe group pre-treatment, 63 (74%) moved post-treatment to the ‘not depressed’ group. Fifteen patients (11%) using the service had no change or deterioration at the time of audit. We observed improvement of five points on the PHQ9 in 98 (73%) patients. Of those patients with six or more contacts, 49 (83%) improved five or more points on the PHQ9 (see Table 2).
Table 2.
Change across diagnostic category
| PHQ9 (score range) | Pre-treatment n (%) | Post-treatment n (%) |
|---|---|---|
| 0–10 (not depressed) | 11(8) | 95 (71) |
| 10–15 (mild-to-moderate depression) | 38 (28) | 15 (11) |
| 15–20 (moderate-to-severe depression) | 56 (42) | 17 (13) |
| 20+ (severe depression) | 29 (22) | 7 (5) |
Clinical significance of change
When we adopted a more stringent test of ‘clinically significant change’, we found that pre-treatment, four (3%) patients were within one standard deviation of the normal population score, while 123 (92%) were above two standard deviations from the norm. Post-treatment, 70 (52%) were within one standard deviation of the norm, with the mean of our post-treatment group falling just outside of that range (7.76), while 39 (29%) were above two standard deviations. Sixty patients (45%) moved from a group more than two standard deviations from the normal population pre-treatment to within one standard deviation post-treatment. Of those patients receiving six or more sessions, 37 (63%) achieved this level of clinically significant change.
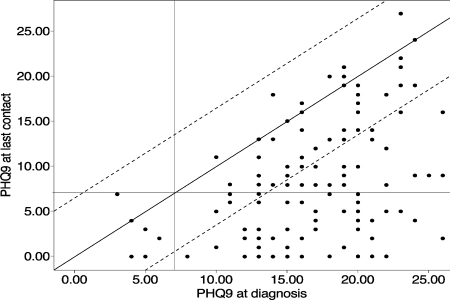
Seventy (55%) people entering the service had a 50% reduction in symptoms measured by the PHQ9 at time of audit. Of those with six or more contacts (n = 59), a drop of 50% or more in depression symptoms was observed in 40 (68%) patients. Figure 2 outlines change of patients across pre–post-treatment, with reference to MCID and clinical significance.
Figure 2.
Scatterplot of PHQ9 score pre-post intervention. Horizontal and vertical reference lines indicate mean of non-clinical sample plus one standard deviation. Diagonal reference line shows no change. Diagonal tram lines show minimal clinically important difference (MCID)
Benchmarking against standards of clinical change
Data were then benchmarked against published evidence of collaborative care. Table 3 outlines results from selected studies and our local treatment outcomes. Depression symptom level was measured in selected studies using the Hopkins Symptom Checklist (SCL20),24 the Hamilton Rating Scale for Depression,25 and the PHQ9. The estimates of change observed in this audit of service delivery appear to reflect positively in relation to expectations from controlled research data. When observed against usual care, the effect size seen is markedly greater, indicating that outcomes are superior to what would be expected. In addition, the change seen is reflective of trial interventions enhancing depression management. In order to balance any potential over-estimation, we conducted an additional analysis of the pre-post effect size taking the lower estimate of change from the 95% CI in our statistical analysis – giving a result of 1.62. Such a cautious approach indicates our results remain reflective of randomised control trial data.
Table 3.
Benchmarking of practice nurse data against published randomised trial data
| Unutzer et al, 200220,a | Hunkeler et al, 200021,b | Katon et al, 200413,a | Dietrich et al, 200422,a | Richards et al, 200814,c | PN datac intervention | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention (n = 906) | Tau (n = 895) | Intervention (n = 179) | Tau (n = 123) | Intervention (n = 164) | Tau (n = 165) | Intervention (n = 224) | Cluster control tau (n = 181) | Intervention (n = 41) | Cluster control tau (n = 35) | |||
| Pre | 1.67 (0.61) | 1.68 (0.61) | 16.6 (6.2) | 17.4 (6.6) | 1.7 (0.51) | 1.6 (0.45) | 2.04 (0.66) | 1.98 (0.65) | 17.51 (4.9) | 18.17 (5.56) | 16.83 (4.88) | |
| Post | 0.93 (0.67) | 1.21 (0.72) | 8.12 (na) | 10.38 (na) | 1.14 (na) | 1.21 (na) | 0.97 (0.80) | 1.09 (0.74) | 8.80 (7.02) | 13.82 (8.37) | 7.76 (6.56) | |
| Pre–post effect size | 1.21 | 0.77 | 1.37 | 1.06 | 1.1 | 0.87 | 1.62 | 1.36 | 1.77 | 0.78 | 1.86 | (1.62d) |
Numbers in parentheses are SD.
aSCL20 depression symptom level assessment
bHamilton Rating Scale for Depression symptom level assessment
cPatient Health Questionnaire depression symptom level assessment
dPre–post effect size based upon lower estimate of change from 95% CI
Satisfaction with service
Patient satisfaction
Fifty-six (44%) patients returned satisfaction questionnaires for the audit; 35 (64%) patients were ‘very satisfied’ with the service, 18 (32%) were ‘satisfied’, and one was ‘unsatisfied’ (n = 54). Thirty-seven (66%) found the service ‘very helpful’, 15 (27%) found the service ‘helpful’, and three (5%) found it ‘a little helpful’ (n = 55). None reported the service being ‘unhelpful'; 45 (80%) reported a better understanding of their depression, seven (12.5%) did not (n = 52). The majority of respondents (n = 53, 94.6%) indicated they would recommend this service to others they knew with similar problems.
GP satisfaction
Eighteen GPs responded to our request for feedback; 17 (95%) used the service and considered that the service enhanced medication concordance, and supported the continuation of the service.
Estimation of practice nurse cost
Mean contact time was 82 minutes per patient per intervention. Based upon unit costs of practice nurse time at £30 per hour, each patient received £41 worth of nurse time. This increased to £45 when missed calls were included, assuming each took approximately 5 minutes. When we used the increased assumption of contact time (contacts per patient = mean + standard deviation and missed contact = mean + standard deviation), nurse costs increased to £76.75 per patient.
Discussion
This audit describes clinical cost and satisfaction outcomes after the introduction of a depression case-management service in primary care settings. It is an intervention delivered by staff with very limited formal training in mental health, who are, however, experts in the management of chronic health conditions.
It has been suggested that sufficient randomised evidence base for collaborative care already exists, and the main challenge now is the implementation in routine care.9,10 We found clinical outcomes that suggest practice nurses are well placed to deliver these interventions at a modest manpower cost. Our observed improvement in depression symptom levels appears comparable to results seen in similar interventions in controlled trials from both the USA and Europe. Our audit suggests that a depression case-management service, run by trained practice nurses, facilitates an effective clinical outcome that may be superior to usual care.
Our use of practice nurses was based upon the fact that they have significant contact with depressed individuals, especially because of increased prevalence in other chronic conditions they manage as a staff group.26 Their ability to adopt structured mental health approaches has been reported.27,28 The training was well received by all staff post-training, increasing confidence in addressing issues that are pertinent to depression management.29
Like others examining the dissemination of such approaches into routine care, we have observed major hurdles. The maintenance of leadership for such service redesign has been difficult to maintain once staff return to their usual primary care practices. Such leadership has been seen as essential in transferring evidence-based interventions into routine care.30 Clearly, the use of local enhanced service finance to support the scheme provides incentives; however, if structures are not in place to monitor performance against objectives, such schemes may fail. This may explain the limited uptake of depression case management post-training, with only four practices contributing data to this audit. The Quality Outcome Framework (QOF), in use in the UK, provides incentives for depression recognition; however, its focus on baseline assessment of depression may fail to provide sufficient incentive for meaningful system redesign that enhances treatment outcomes.
While outcomes were positive, consideration must be given to the numerous weaknesses of our data. They are based upon a non-randomised sample that accepted the intervention when offered, and uses samples from practices that embraced service redesign for the treatment of depression. A proportion of our improvement is likely to be due to natural remission and usual care; beyond considering the outcomes in usual care arms of controlled trials, to what degree this explains our observed improvement is unclear. We report incomplete data regarding age, sex and employment status of patients. Following up this gap in information and collecting additional details in relation to depression history, duration and other demographic factors was beyond our remit. While little difference can be noted between those accepting follow-up and those refusing it, it is unclear if such a picture would maintain with a complete data set. In addition we have no independent verification as to how closely the practice nurses adhered to protocols outlined in training, nor of data quality. As the service provides a chronic care-management approach to depression, no confines are placed upon the number of sessions or duration of contact. Hence, by using the most recent recorded PHQ9 score as our post score, we are capturing a ‘snapshot’ of clinical status of individuals at varying stages in recovery. To try to provide analysis of a ‘standard dose’ we conducted an additional analysis on those receiving six or more sessions, observing increased improvement. While satisfaction data appear positive, we received feedback from approximately 41% of patients, using locally designed non-validated measures. This response rate may be reasonable in routine care; however, the views of those not responding may have tempered the high levels of support for the intervention we found. Those that did respond found the additional support helpful and informative. Comments often indicated that the relationship already established within the practice facilitated delivery of the intervention. This may suggest that practice nurses, due to their contact with patients over a wide range of health problems, are ideally placed to normalise the treatment of depression. Such considerations are tentative, and further detailed qualitative research may add a depth of understanding to this area, which at present is lacking.
In conclusion, we found depression case management can be effectively delivered by practice nurses, following brief training, with results that are similar to those seen in randomised controlled trials.
Contributor Information
David Ekers, Nurse Consultant Primary Care Mental Health, Tees Esk and Wear Valleys NHS Trust, and Honorary Clinical Lecturer, Mental Health Research Centre, Durham University, UK.
Rea Wilson, Primary Care Graduate Mental Health Worker, Tees Esk and Wear Valleys NHS Trust, UK.
REFERENCES
- 1.Singleton N, Bumpstead R, O'Brien M, et al. Office of National Statistics. Psychiatric Morbidity Among Adults Living in Private Households London: HMSO, 2001 [DOI] [PubMed] [Google Scholar]
- 2.Gilbody S, Whitty P. Improving the recognition and management of depression in primary care. Effective Health Care 2002;7(5):1–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fletcher J, Bower P, Gask L, et al. Primary Care Services for Depression: a guide to best practice. Hyde, Cheshire: Services Improvement Partnership, 2006 [Google Scholar]
- 4.Henderson S, Andrews G, Hall W. Australia's mental health: an overview of the general population survey. Australian and New Zealand Journal of Psychiatry 2001;34(2):197–205 [DOI] [PubMed] [Google Scholar]
- 5.Pincus H, Pettit A. The societal costs of chronic major depression. Journal of Clinical Psychiatry 2001;62(6):5–9 [PubMed] [Google Scholar]
- 6.Layard R. Mental Health: Britain's biggest social problem? Strategy Unit Seminar Paper: RL414c, 2004. www.strategy.gov.uk/downloads/files/mh_layard.pdf [Google Scholar]
- 7.National Institute for Health and Clinical Excellence Management of Depression in Primary and Secondary Care. London: National Institute for Health and Clinical Excellence, 2004 [Google Scholar]
- 8.Bird A. We Need to Talk. The case for psychological therapy on the NHS. London: Mental Health Foundation, 2006 [Google Scholar]
- 9.Katon W, Unutzer J. Collaborative care models for depression: time to move from evidence to practice. Archives of Internal Medicine 2006;166:2304–6 [DOI] [PubMed] [Google Scholar]
- 10.Simon G. Collaborative care for depression is effective in older people, as the IMPACT trial shows. BMJ 2006;332:249–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gilbody S, Bower P, Fletcher J, et al. Collaborative care for depression. A cumulative meta-analysis and review of longer-term outcomes. Archives of Internal Medicine 2006;166:2314–21 [DOI] [PubMed] [Google Scholar]
- 12.Gunn J, Diggens J, Hegarty K, et al. A systematic review of complex system interventions designed to increase recovery from depression in primary care. BMC Health Services Research 2006;6:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Katon W, Schoenbaum M, Fan M, et al. Cost-effectiveness of improving primary care treatment of late life depression. Archives of General Psychiatry 2005;62:1313–20 [DOI] [PubMed] [Google Scholar]
- 14.Richards D, Lovell K, Gilbody S, et al. Collaborative care for depression in UK primary care: a randomised controlled trial. Psychological Medicine 2008;38(2):279–88 [DOI] [PubMed] [Google Scholar]
- 15.Kroenke K, Spitzer R, Williams J. PHQ9: Validity of a brief depression measure. Journal of General Internal Medicine 2001;16(9):606–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ekers D, Richards D, Gilbody S. A meta-analysis of randomised trials of behavioural treatment of depression. Psychological Medicine 2008;38(5):611–23 [DOI] [PubMed] [Google Scholar]
- 17.Lowe B, Unutzer J, Callahan C, et al. Monitoring depression treatment outcomes with the Patient Health Questionnaire-9. Medical Care 2004;42(12):1194–201 [DOI] [PubMed] [Google Scholar]
- 18.Ekers D, Richards D. Anxiety and depression in primary care. Primary Health Care 2007;14(4):36–9 [Google Scholar]
- 19.National Research Ethics Service Defining Research. London: National Patient Safety Agency, 2008 [Google Scholar]
- 20.Unutzer J, Katon W, Callahan C, et al. Improving mood-promoting access to collaborative treatment: collaborative care management of late-life depression in the primary care setting. A randomized controlled trial. JAMA 2002;288:2826. –45. [DOI] [PubMed] [Google Scholar]
- 21.Hunkeler E, Meresman J, Hargreaves W, et al. Efficacy of nurse telehealth care and peer support in augmenting treatment of depression in primary care. Archives of Internal Medicine 2000;9:700–8 [DOI] [PubMed] [Google Scholar]
- 22.Dietrich A, Oxman T, Williams J, et al. Re-engineering systems for the treatment of depression in primary care: cluster randomised controlled trial. BMJ 2004;329:602–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Netten A, Curtis L. Unit Costs of Health and Social Care. Canterbury: PSSRU, 2007 [Google Scholar]
- 24.Lipman R, Covi L, Shapiro A. The Hopkins symptom checklist (HSCL)–factors derived from the HSCL-90. Journal of Affective Disorders 1979;1:9–24 [DOI] [PubMed] [Google Scholar]
- 25.Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry 1960;23:56–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cole M, Bellavance F, Mansour A. Prognosis of depression in elderly community and primary care populations: a systematic review and meta-analysis. American Journal of Psychiatry 1999;156:1182–9 [DOI] [PubMed] [Google Scholar]
- 27.Mynors-Wallis L, Davies I, Gray A, et al. A randomized controlled trial and cost analysis of problem-solving treatment for emotional disorders given by community nurses in primary care. British Journal of Psychiatry 1997;170:113–19 [DOI] [PubMed] [Google Scholar]
- 28.Richards A, Barkham M, Cahill J, et al. PHASE: a randomised, controlled trial of supervised self-help cognitive behaviour therapy in primary care. British Journal of General Practice 2003;53:764–70 [PMC free article] [PubMed] [Google Scholar]
- 29.Ekers D, Richards D, Grant H. Developing depression management in primary care. Primary Health Care 2007;17(8):31–3 [Google Scholar]
- 30.Meredith L, Mendel P, Pearson M, et al. Implementation and maintenance of quality improvement for treating depression in primary care. Psychiatric Services 2006;57(1):48–55 [DOI] [PubMed] [Google Scholar]
CONFLICTS OF INTEREST
None.