Abstract
Background
The aim of this prospective study was to determine whether a level of positive airway pressure was generated in participants receiving nasal high flow (NHF) delivered by the Optiflow™ system (Fisher and Paykel Healthcare Ltd, Auckland, New Zealand) in a cardiothoracic and vascular intensive care unit (ICU).
Methods
Nasopharyngeal airway pressure was measured in 15 postoperative cardiac surgery adult patients who received both NHF and standard facemask therapy at a flow rate of 35 litre min−1. Measurements were repeated in the open mouth and closed mouth positions. Mean airway pressure was determined by averaging the pressures at the peak of inspiration of each breath within a 1 min period, allowing the entire pressure profile of each breath to be included within the calculation.
Results
Low level positive pressure was demonstrated with NHF at 35 litre min−1 with mouth closed when compared with a facemask. NHF generated a mean nasopharyngeal airway pressure of mean (sd) 2.7 (1.04) cm H2O with the mouth closed. Airway pressure was significantly higher when breathing with mouth closed compared with mouth open (P≤0.0001).
Conclusions
This study demonstrated that a low level of positive pressure was generated with NHF at 35 litre min−1 of gas flow. This is consistent with results obtained in healthy volunteers.
Australian Clinical Trials Registry www.actr.org.au ACTRN012606000139572.
Keywords: airway pressure, nasal high-flow therapy, Optiflow™, oxygen
Patients with respiratory failure are typically treated with three main respiratory support strategies, depending on the severity of their illness. These are traditional oxygen therapy, non-invasive ventilation, and invasive mechanical ventilation.1 A new respiratory support therapy has recently been introduced into the adult arena. NHF allows the delivery of up to 60 litre min−1 of heated and humidified gas via a wide bore nasal cannula. However, the effect of delivering such high-flow rates into the nasopharynx remains unclear.
In neonatal care, the delivery of relatively high flows of heated and humidified gas via a nasal cannula has gained increasing acceptance in the treatment of respiratory conditions.2–4 Studies of NHF in this patient population have demonstrated an effect comparable with nasal continuous positive airway pressure (CPAP).4–6 In adults, there have been reports that NHF may be beneficial in the treatment of obstructive sleep apnoea, attributable to a flow-related pressure effect.7 There has been a similar pressure effect reported in healthy adult volunteers8–9 where a positive relationship between flow and airway pressure has also been described. However, to date there have been no published reports evaluating pressure effects in the adult ICU population.
The aim of this study was to quantify the airway pressure effect associated with NHF in an adult patient cohort.
Methods
A prospective study was conducted in a 16-bed cardiothoracic and vascular ICU to test the hypothesis that a positive airway pressure is generated. The study was approved by the regional Ethics Committee. Written informed consent was obtained from the participants before operation.
Participants who were undergoing elective cardiac surgery were eligible for inclusion in this study. They were excluded if they had a history of sinus problems, nasal trauma, or a markedly deviated septum. In total, 20 participants were recruited, of which 15 completed the study. Five participants were excluded before data collection: one participant was excluded from all study procedures as they returned from theatre in a critical condition; one participant was excluded as it was not possible to insert the pressure measuring catheter; and three were excluded after the pressure measuring catheter became dislodged before data collection.
On return from theatre, while sedated and ventilated, a 10 F catheter was inserted into the nasopharynx via the nose. The catheter was secured in place and remained in situ overnight. Participants received all standard ICU care. The morning after surgery, once awake and extubated, participants were routinely mobilized to a chair and their pain levels assessed. Analgesia was provided where necessary, as per unit protocol, to ensure that each participant was able to breathe deeply and comfortably. For consistency, all measurements were performed by one of the researchers trained in this technique.
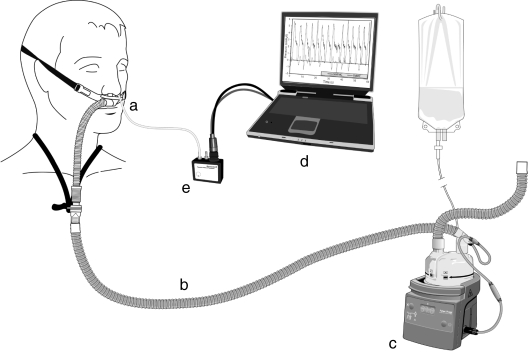
Before performing measurements, correct placement of the catheter was confirmed using end-tidal carbon dioxide (CO2) monitoring. If necessary, the catheter was suctioned and manipulated until a clear respiratory trace was achieved. A visual check was also performed to locate the tip of the catheter behind the uvula. The catheter was then connected to the Honeywell precision pressure transducer (PPT-0001 DWWW2VA-B, Honeywell International Ltd, NJ, USA) using a laptop computer interface (Figs 1 and 2). The Optiflow™ system (MR880 heated humidifier, RT241 heated delivery tube, Fisher and Paykel Healthcare Ltd, Auckland, New Zealand) with an air/oxygen blender (Bird high-flow blenders, Cardinal Healthcare, IL, USA) was used for all measurements.
Fig 1.
Optiflow™ system set-up. a, Optiflow™ RT034 cannula; b, heater delivery tube RT241; c, MR880 heated humidifier; d, laptop interface; e, pressure transducer.
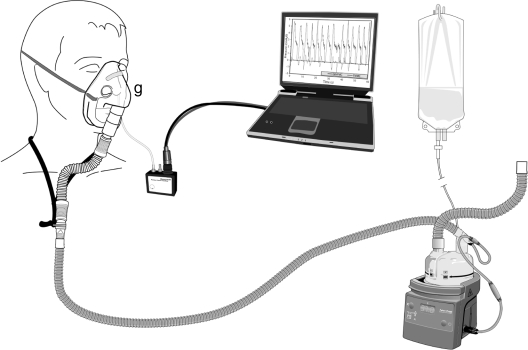
Fig 2.
Standard facemask set-up. g, Mask adapter (commercially unavailable).
Once the system temperature stabilized (target; 37°C with an absolute humidity of 44 mg H2O litre−1), therapy was commenced at 35 litre min−1 using the Optiflow™ wide bore nasal cannula (Fig. 1; RT034 nasal cannula, Fisher and Paykel Healthcare Ltd). As per the manufacturer's recommendations, the investigators ensured that no more than half the internal diameter of the nares was taken up by the cannula. Participants were given ∼15 min on the system to become accustomed to the feeling of increased flow and to allow breathing patterns to settle before measurements were commenced. Measurements were then repeated with a standard facemask (Fig. 2; Medium Adult SEE-THRU® Oxygen Mask, Hudson Respiratory Care Inc., NC, USA) at 35 litre min−1 (target; 37°C with an absolute humidity of 44 mg H2O litre−1) connected by way of an adapter to the heated delivery tube. This ensured that all equipment and conditions were standardized with the exception of the interface. Oxygen concentrations were titrated to meet participants' requirements. Measurements were recorded with the participant's mouth open and mouth closed for each interface. Each recording was taken over 1 min of quiet breathing. A washout period of 5 min was allowed between each of the measurements to ensure no carry-over effect between therapies. During this time, the patency and position of the catheter was re-checked.
At the end of the procedure, the nasopharyngeal catheter was removed and the participant returned to their original oxygen delivery device.
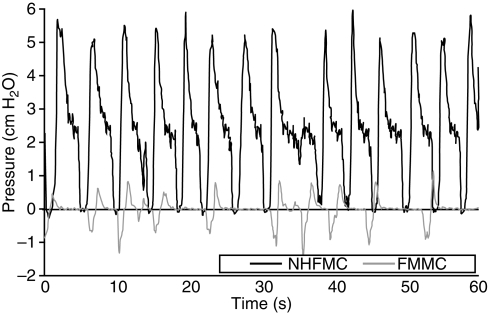
Nasopharyngeal pressure profiles were recorded for each participant over 1 min. An example of one participant's trace is shown in Figure 3. Data analysis determined the mean nasopharyngeal airway pressure. This required averaging the pressure from the peak of inspiration of the first breath to the peak of inspiration of the last breath within a 1 min recording. This allowed the entire pressure profile of each breath within that 1 min period to be included in the pressure calculation. All data analysis was performed using Microsoft® Office Excel 2003. Data are presented as mean (sd). Paired t-test was used to compare mean differences between NHF and standard facemask, and between the mouth open and mouth closed measurements for each interface.
Fig 3.
Breathing pressure profile of one participant over 1 min. Nasopharyngeal pressure (cm H2O) generated at 35 litre min−1 using NHF with the mouth closed (NHFMC) is shown in black. Nasopharyngeal pressure (cm H2O) generated at 35 litre min−1 using a facemask with the mouth closed (FMMC) is shown in grey.
Results
Data from 15 participants were analysed. The participants were 17 males and two females of mean (range) age 63 (41–79) yr, weight 86 (67–107) kg, and height 175 (156–186) cm.
Significantly higher nasopharyngeal airway pressures were recorded with NHF in the mouth closed position when compared with mouth open [2.7 (1.04) vs 1.2 (0.76) cm H2O (P=0.001)] (Table 1). There was no significant difference in nasopharyngeal airway pressure generated with facemask mouth open [0.11 (0.39) cm H2O] and facemask mouth closed [0.2 (0.63) cm H2O] (P=0.5). The corresponding values of nasopharyngeal pressures with NHF, during mouth open or mouth closed, were significantly higher than those with a facemask (P=0.001).
Table 1.
Measurements from the 15 participants showing individual nasopharyngeal pressures (cm H2O) and mean nasopharyngeal pressures (cm H2O) with sd generated with NHF and facemask at 35 litre min−1 with the open mouth (NHFMO and FMMO) and closed mouth positions (NHFMC and FMMC)
| Participant | Mean nasopharyngeal pressure (cm H2O) |
|||
|---|---|---|---|---|
| NHFMC | NHFMO | FMMC | FMMO | |
| 1 | 1.7 | 1.6 | 1.3 | 0.3 |
| 2 | 2.7 | 1.7 | — | 1.3 |
| 3 | — | — | — | — |
| 4 | 1.5 | 0.9 | −0.2 | −0.5 |
| 5 | 1.6 | 0.2 | −0.01 | 0.02 |
| 6 | 2.2 | 0.5 | 0.005 | −0.01 |
| 7 | 3.4 | 2.1 | 0.02 | 0.06 |
| 8 | 2.7 | 1.6 | −0.003 | 0.04 |
| 9 | 3.4 | 0.7 | −0.09 | 0.02 |
| 10 | 2.2 | 0.9 | 0.02 | −0.04 |
| 11 | 5.3 | 2.3 | 1.7 | 0.4 |
| 12 | 1.7 | 0.1 | −0.5 | 0.02 |
| 13 | 2.5 | 2.4 | 0.6 | −0.06 |
| 14 | 3.0 | 0.7 | 0.006 | 0.04 |
| 15 | 3.7 | 1.5 | −0.1 | 0.03 |
| Mean airway pressure at 35 litre min−1 | 2.7 | 1.2 | 0.2 | 0.1 |
| sd | 1.04 | 0.76 | 0.63 | 0.39 |
Discussion
This study demonstrates that a significant positive airway pressure effect is delivered with NHF using the Optiflow™ system and a wide bore nasal cannula. The pressure effect was shown to be most evident with the participant's mouth closed, but was still significant with the mouth open, when compared with a facemask interface at the same gas flow rate.
The mean nasopharyngeal airway pressure rather than the end-expiratory airway pressure was analysed. This was considered to be a more accurate assessment of overall therapy effect. The terms CPAP and PEEP have been avoided as it is not clear to us how these terms relate to NHF.
For the purposes of this study, a nasopharyngeal catheter was used rather than an oesophageal balloon catheter, due to the perceived patient risks and discomfort associated with the latter technique. Nasopharyngeal pressure has been taken as the most feasible surrogate measure of transpulmonary pressure. It should be noted that during analysis, the pressure profiles from the first four participants (Table 1) were noted to be dampened. Indeed, participant number 3 had no analysable pressure traces. These errors were assumed to be technique-related, but mean data have been reported where possible. To assess for difference, analysis was carried out including, and excluding, data belonging to the participants 1–4. Results showed that the difference in treatment effect remained similar whether these participants were included or not.
Previous research has shown comparable results with those obtained in this study.8,9
An overall effect on airway pressure was observed when individual pressure profiles recorded in this study were examined. As can be seen in Figure 3, the pressure tracing recorded with a facemask tends to rotate around zero (atmospheric pressure). With NHF, the entire pressure profile of the breath is elevated. Visual analysis of these profiles would also seem to suggest that the expiratory phase is prolonged when using NHF. This could be explained by the effect of breathing out against the incoming gas flow.
A large interpatient variability was observed in this study. When participants using NHF breathed with mouth closed, the mean nasopharyngeal pressure generated ranged from 1.54 to 5.34 cm H2O (Table 1). We hypothesize that this variability may be due to differences in leak around the outside of the nasal cannula and the wide variability in nare size among the study population. A smaller leak may create an increased resistance to expiration resulting in higher nasopharyngeal pressure. Previous studies support this theory.5,10 Physiological differences in airway anatomy may also explain some of the variability. It is uncertain whether the presence of a nasopharyngeal catheter to measure airway pressure as used in this and other studies8,9 has an effect on the pressure generated in the upper airway.
In spite of these limitations, it is evident that a positive airway pressure is generated using NHF and this may have important clinical implications. A number of clinical benefits are associated with conventional pressure-generating devices, including improved oxygenation; improved ventilation perfusion matching; reduced airways resistance; reduced work of breathing; and the balancing of intrinsic PEEP.11 Studies to assess the extent to which NHF is associated with these clinical benefits are required.
In conclusion, NHF is a new respiratory support modality into which little clinical research has been conducted. We have shown that NHF can significantly increase mean nasopharyngeal airway pressure in an adult patient population. This may be an important factor in determining the most appropriate respiratory support therapy for a particular patient.
Areas for future research would include the investigation of airway pressure measurements at differing flow rates, clinical applications, and the influence of NHF on patient outcomes.
Funding
Research in the Cardiothoracic and Vascular Intensive Care Unit is supported in part by Fisher and Paykel Healthcare Ltd.
Acknowledgement
Special thanks to Steven Korner, Fisher and Paykel Healthcare Ltd, for assistance in refining the measurement technique.
References
- 1.Kallstrom TJ. AARC clinical practice guideline: oxygen therapy for adults in the acute care facility—2002 revision & update. Respiratory Care. 2002;47:717–20. [PubMed] [Google Scholar]
- 2.de Klerk A. Humidified high-flow nasal cannula: is it the new and improved CPAP? Adv Neonatal Care. 2008;8:98–106. doi: 10.1097/01.ANC.0000317258.53330.18. [DOI] [PubMed] [Google Scholar]
- 3.Shoemaker MT, Pierce MR, Yoder BA, Digeronimo RJ. High flow nasal cannula versus nasal CPAP for neonatal respiratory disease: a retrospective study. J Perinatol. 2007;27:85–91. doi: 10.1038/sj.jp.7211647. [DOI] [PubMed] [Google Scholar]
- 4.Saslow JG, Aghai ZH, Nakhla TA, et al. Work of breathing using high-flow nasal cannula in preterm infants. J Perinatol. 2006;26:476–80. doi: 10.1038/sj.jp.7211530. [DOI] [PubMed] [Google Scholar]
- 5.Lampland AL, Plumm B, Meyers PA, Worwa CT, Mammel MC. Observational study of humidified high-flow nasal cannula compared with nasal continuous positive airway pressure. J Pediatr. 2009;154:177–82. doi: 10.1016/j.jpeds.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 6.Kubicka ZJ, Limauro J, Darnall RA. Heated, humidified high-flow nasal cannula therapy: yet another way to deliver continuous positive airway pressure? Pediatrics. 2008;121:82–8. doi: 10.1542/peds.2007-0957. [DOI] [PubMed] [Google Scholar]
- 7.McGinley BM, Patil SP, Kirkness JP, Smith PL, Schwartz AR, Schneider H. A nasal cannula can be used to treat obstructive sleep apnea. Am J Respir Crit Care Med. 2007;176:194–200. doi: 10.1164/rccm.200609-1336OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Groves N, Tobin A. High flow nasal oxygen generates positive airway pressure in adult volunteers. Aust Crit Care. 2007;20:126–31. doi: 10.1016/j.aucc.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 9.Ritchie JE, Williams AB, Gerard C. Evaluation of a high flow nasal oxygenation system: gas analysis and pharyngeal pressures. Intensive Care Med. 2006;32:S219. [Google Scholar]
- 10.Locke RG, Wolfson MR, Shaffer TH, Rubenstein SD, Greenspan JS. Inadvertent administration of positive end-distending pressure during nasal cannula flow. Pediatrics. 1993;91:135–8. [PubMed] [Google Scholar]
- 11.Keenan SP, Kernerman PD, Cook DJ. Effect of noninvasive positive pressure ventilation on mortality in patients admitted with acute respiratory failure: a meta-analysis. Crit Care Med. 1997;25:1685–92. doi: 10.1097/00003246-199710000-00018. [DOI] [PubMed] [Google Scholar]