Abstract
Aims
Inflammation is pivotal in atherosclerosis and a key early step is endothelial dysfunction. C-reactive protein, the prototypic marker of inflammation, and cardiovascular risk marker have been shown to promote atherogenesis. Increased levels of C-reactive protein are associated with endothelial dysfunction. The glycocalyx decorates the luminal surface and affords critical protection of the endothelium. Thus, the aim of the study was to examine the effect of C-reactive protein on the endothelial glycocalyx.
Methods and results
Human aortic endothelial cells (HAECs) were incubated with C-reactive protein at different concentrations (0, 12.5, 25, and 50 µg/mL) with boiled C-reactive protein as a control. For in vivo experiments, human C-reactive protein was injected into rats and human serum albumin was used as a control. Endothelial glycocalyx thickness was examined by transmission electron microscopy. Hyaluronan (HA) was examined in the supernatant of HAECs and in plasma and surface expression of heparan sulfate (HS) was quantified. C-reactive protein dose-dependently increased HA release in vitro and in vivo (P < 0.01). Also, glycocalyx thickness was significantly decreased (P < 0.05). Western blotting for HS showed significant reduction in expression of HS, one of the main glycosaminoglycans in the glycocalyx, with C-reactive protein treatment. There was a significant positive correlation between HA release and monocyte–endothelial cell adhesion, plasminogen activator inhibitor-1, and intercellular adhesion molecule-1 release and a negative correlation with endothelial nitric oxide synthase activity.
Conclusion
Collectively, these data suggest that C-reactive protein impairs glycocalyx function, resulting in endothelial dysfunction.
Keywords: Endothelium, Dysfunction, C-reactive protein, eNOS, Inflammation, Glycocalyx, Hyaluronan
1. Introduction
Increasing evidence support the involvement of inflammation in the pathogenesis of atherosclerosis.1 C-reactive protein, the prototypic marker of inflammation, has been shown in numerous studies to predict cardiovascular events.2 In addition to being a risk marker, C-reactive protein by enhancing inflammation, oxidative stress, and pro-coagulant activity appears to mediate atherothrombosis.3,4
In endothelial cells (ECs), C-reactive protein increases the expression of cell adhesion molecules, intercellular adhesion molecule-1 (ICAM-1) and vascular cell adhesion molecule-1, increases monocyte-chemotactic protein-1 and endothelin-1, plasminogen activator inhibitor-1, and inflammatory cytokines, and decreases prostacyclin release as well as tissue plasminogen activator activity.3,4 C-reactive protein augments monocyte–EC adhesion under static and shear stress conditions. Increased C-reactive protein levels are associated with impaired endothelial vasoreactivity.3,4 In addition, we and others5,6 have shown that C-reactive protein causes down-regulation of endothelial nitric oxide synthase (eNOS) by decreasing eNOS activity and NO bioactivity as determined by the conversion of arginine to citrulline and cyclic GMP release, respectively. Furthermore, recent evidence in murine models has also shown that C-reactive protein administration impairs endothelial vasoreactivity and eNOS in vivo via uncoupling of the enzyme.7–10 Many groups have now confirmed that C-reactive protein administration in vivo impairs endothelial vasoreactivity.7–10
Recent studies have recognized that the endothelial glycocalyx, an intraluminal layer, consisting mainly of hyaluronan (HA) and heparan sulfate (HS), contributes to the vasculoprotective effects of the vessel wall.11,12 HA, in the EC glycocalyx, appears to serve as a mechano-shear sensor and regulates NO release and maintains vascular permeability.13–16 Recent data demonstrate that exposure of EC to oxidized low-density lipoprotein (ox-LDL) or tumour necrosis factor alpha (TNF-α) reduces thickness of the EC glycocalyx and decreases the amount of HS associated with the surface.16–19 Lewis et al.20 demonstrated that coronary artery endothelial glycocalyx of pigeons was thinnest in areas with high disease predilection and thickness was reduced even further on cholesterol challenge. Furthermore, in Type 1 diabetics, EC glycocalyx is profoundly reduced compared with matched healthy controls.21,22
Although several reports demonstrate that C-reactive protein induces endothelial activation/dysfunction, there is a paucity of data on the effects of C-reactive protein on the endothelial glycocalyx and its association with endothelial dysfunction. Thus, in this study, we examined the effect of C-reactive protein treatment in vitro and in vivo on the EC glycocalyx.
2. Methods
Human C-reactive protein was purified from human ascitic/pleural fluids as described previously.23 These fluids were anonymized and the protocol of waived consent was approved by the UC Davis Medical Center Institutional Review Board. We have shown that our in-house purified, dialysed C-reactive protein mediates its inflammatory effects in toll-like receptor 4 knocked down cells providing further cogent data that C-reactive protein-mediated effects are not due to endotoxin or azide contamination.23
2.1. Cell culture and treatment
Human aortic endothelial cells (HAECs; Cambrex) were grown in endothelial medium containing growth supplements (EGM-MV) and used between passages 3 and 5. For the initial experiments, cells were grown in 12-well plates. Upon reaching 80% confluency, the cells were incubated with C-reactive protein (0, 25, and 50 µg/mL) or boiled C-reactive protein (25 µg/mL) for 12 h. The rationale for using doses of C-reactive protein up to 50 µg/mL is because plasma C-reactive protein levels, ranging 20–64 mg/L, have been reported in patients with acute coronary syndromes and levels appear to be higher in aortic sinus samples and predict poorer outcomes.24,25 Also, these doses of C-reactive protein did not result in significantly increased cell proliferation.
2.2. In vivo C-reactive protein treatment
This study conforms with the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication No. 85-23, revised 1996) and our institution is compliant with these guidelines (UC Davis Approval number#15232). Male hooded Wistar rats (weighing 125–150 g) were obtained from Charles River Lab. Animals were housed in a controlled environment at an ambient temperature of 21 ± 2°C on a 12 h light:dark cycle. Food and water were provided ad libitum. The rats were acclimatized to animal housing conditions for 1 week. The protocol was approved by the animal committee of University of California at Davis. Human C-reactive protein/human serum albumin (HuSA, 20 mg/kg body weight for 3 days, n = 5 in each group) was injected in the peritoneal cavity of the rats as described previously.26 The rats were sacrificed by overdose of pentobarbital. Aorta was obtained for en face staining and for isolation of rat, aortic ECs were obtained using anti-CD31 antibodies as described previously.10
2.3. Hyaluronan
HA release from C-reactive protein-treated HAECs and in circulation of rats treated with human C-reactive protein/HuSA was examined by ELISA (Echelon Biosciences), and the inter- and intra-assay coefficient of variation of the assay was <8%.
2.4. Western blotting for HS
Western blotting for HS was performed on membrane fractions of lysates from C-reactive protein-treated HAECs using anti-human monoclonal antibodies to HS (Calbiochem) as described previously.5 Densitometric ratios to β-actin as a loading control were calculated. Also, rat aortic sections were stained using mouse anti-rat antibodies to HS followed by secondary anti-mouse IgG-PE and images were obtained using a fluorescent microscope.
2.5. TEM for EC glycocalyx
Cells were cultured as above in eight-well Permanox® slide wells. Both C-reactive protein-treated HAECs and human C-reactive protein/HuSA-injected rat aortic ECs were used for these experiments. They were fixed and embedded using a modification of the protocol described previously.27 Protocol modifications for the cultured cells were as follows. One well in each treatment group was processed without Alcian Blue and lanthanum nitrate. Alcian Blue 8GX (AB) was added to a mixed aldehyde fix (2.5% glutaraldehyde and 2% paraformaldehyde in a 0.06% sodium phosphate buffer with a final concentration of 0.05%) immediately prior to fixation. Cells remained in the fixative/AB at 4°C until further processing. After rinsing three times in 0.01 M phosphate buffer, cells were incubated in 1% osmium tetroxide in 0.1 M buffer with 1% lanthanum nitrate for 1 h followed by washes and then incubated 90 min in 1% aqueous uranyl acetate. Dehydration was achieved in ascending concentrations of ethanol. All procedures before the 95% ethanol were carried out at 4°C. After the final 100% ethanol fresh epoxy resin was added to the wells and left at room temperature overnight, resin was exchanged and then polymerized at 70°C overnight. The Permanox® was stripped from the cultures and a jeweler's saw was utilized to select an area of cells for on face sectioning. Ultrathin sections were stained with uranyl acetate and lead citrate and then viewed with a Philips CM120 electron microscope (FEI Company, Hillsboro, OR, USA, made in Eindhoven, The Netherlands) equipped with a GATAN digital camera (Gatan MegaScan, model 794/20, Pleasanton, CA, USA). Semi-quantitative measurements of glycocalyx thickness were made utilizing the micron bar on the image of interest. A determination was made of where the actual cell membrane was and the glycocalyx was measured from the cell membrane to the outer edge of the glycocalyx. Briefly, for measurements of glycocalyx thickness, five cells were selected empirically for having thick vs. thin glycocalyx within the same sample. All micrographs were taken at the same magnification. Four sites were chosen across the length of the glycocalyx where the basal lamina was clear enough to make a perpendicular measurement possible. The four sites on each micrograph were measured and the thickness determined. Thicknesses within the thick or thin region were averaged to determine thickness range.
2.6. Monocyte-EC adhesion
Monocyte-EC adhesion under static conditions was performed after treatment of HAECs with C-reactive protein or boiled C-reactive protein for 12 h as described previously using CFDA-labelled monocytes.28
2.7. eNOS bioactivity
eNOS enzymatic activity was assessed by measuring the conversion of 14C-l-arginine to 14C-l-citrulline in HAEC lysates as reported previously.7
2.8. Plasminogen activator inhibitor-1 activity
Plasminogen activator inhibitor-1 (PAI-1) activity in the supernatants of C-reactive protein-treated HAECs was examined by ELISA using the Spectrolyse reagents from American Diagnostica as reported previously.29
2.9. Intercellular adhesion molecule-1
ICAM-1 release from C-reactive protein-treated HAECs was examined using a high sensitivity ELISA from R&D Systems as described previously.28
2.10. Statistical analysis
All experiments were performed at least three times in duplicate. The dose–response comparisons were analysed using ANOVA followed by post hoc tests. The experimental results are presented as means ± SD. Paired t-tests were used to compute differences in the variables, and the level of significance was set at P < 0.05.
3. Results
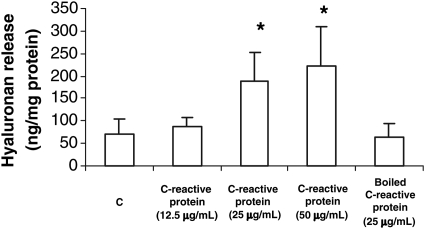
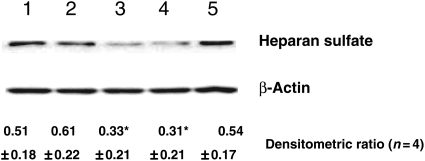
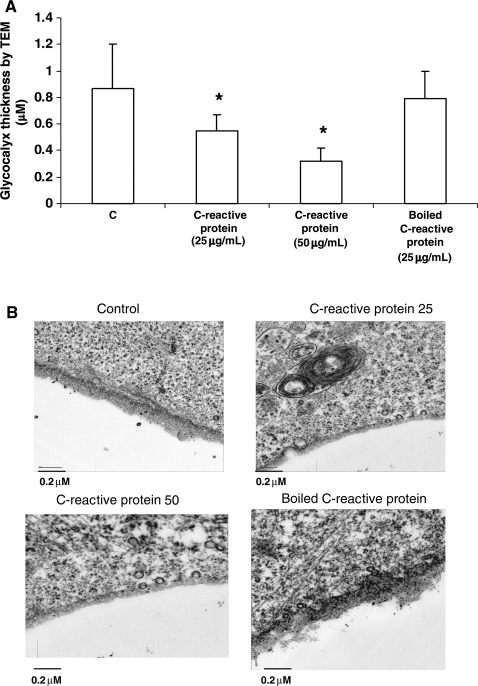
C-reactive protein dose-dependently increased HA release from HAECs (Figure 1), whereas boiled C-reactive protein failed to have any effect (C: 72 ± 33 ng/mg protein; C-reactive protein 12.5: 87 ± 21 ng/mg protein; C-reactive protein 25: 188 ± 66 ng/mg protein; C-reactive protein 50: 222 ± 87 ng/mg protein; boiled C-reactive protein: 65 ± 29 ng/mg protein; P < 0.01 compared with C and boiled C-reactive protein). Also, western blotting for membrane-associated HS showed significant reduction in expression of HS, one of the main glycosaminoglycans (GAGs) in the glycocalyx following C-reactive protein treatment (Figure 2). We then examined glycocalyx thickness by transmission electron microscopy (TEM). As depicted in Figure 3A and B (representative TE micrographs), C-reactive protein treatment significantly decreased thickness of the EC glycocalyx, again boiled C-reactive protein had no effect.
Figure 1.
Effect of C-reactive protein on HA release from HAECs. HAECs were treated with different concentrations of C-reactive protein (0, 12.5, 25, and 50 µg/mL) or boiled C-reactive protein (25 µg/mL) overnight at 37°C and HA release in the media was assessed by ELISA as described in Section 2. Data are mean ± S.D of eight experiments. *P < 0.01 compared with C.
Figure 2.
Effect of C-reactive protein on HS levels in HAECs. HAECs were treated with different concentrations of C-reactive protein (0, 12.5, 25, and 50 µg/mL) or boiled C-reactive protein (25 µg/mL) overnight at 37°C and HS on cells was quantified by western blotting, using specific anti-human antibodies and using β-actin as a loading control as described in Section 2. Representative western blot and densitometric ratio for four different experiments are provided: 1, C; 2, C-reactive protein (12.5 µg/mL); 3, C-reactive protein (25 µg/mL); 4, C-reactive protein (50 µg/mL); 5, boiled C-reactive protein (25 µg/mL); *P < 0.05 compared with control and boiled C-reactive protein. Data are mean ± SD. *P < 0.05 compared with C.
Figure 3.
Effect of C-reactive protein on glycocalyx thickness of HAECs. HAECs were treated with different concentrations of C-reactive protein (0, 25, and 50 µg/mL) or boiled C-reactive protein (25 µg/mL) overnight at 37°C and glycocalyx thickness was assessed by TEM as described in Section 2. (A) Mean ± SD of four experiments. *P < 0.01 compared with C. Representative micrographs are shown in (B).
We also examined the effect of C-reactive protein treatment on eNOS activity, PAI-1 activity, ICAM-1 release, and monocyte–EC adhesion. As reported previously8,10 and in Table 1, C-reactive protein dose-dependently decreased eNOS activity and up-regulated PAI-1, ICAM-1, and adhesion (P < 0.05). Furthermore, there was a significant negative correlation between HA release from EC and eNOS (r = −0.71, P < 0.01), and positive correlation with PAI-1 (r = 0.49, P < 0.05), ICAM-1 (r = 0.63, P < 0.05), and monocyte adhesion (r = 0.77, P < 0.01) (n = 8).
Table 1.
Biological effects of C-reactive protein in HAECs
| C | C-reactive protein |
|||
|---|---|---|---|---|
| 12.5 µg/mL | 25 µg/mL | 50 µg/mL | ||
| eNOS activity (pmol/mg protein) | 624 ± 236 | 601 ± 231 | 324 ± 105* | 214 ± 99* |
| PAI-1 activity (pg/mg protein) | 21 ± 11 | 26 ± 13 | 59 ± 18* | 66 ± 22* |
| ICAM-1 release (ng/mg protein) | 4.1 ± 1.9 | 5.1 ± 2.7 | 9.4 ± 2.5* | 10.6 ± 1.9* |
| Monocyte–EC adhesion (%bound) | 29 ± 18 | 33 ± 19 | 56 ± 19* | 64 ± 24* |
Data are provided as mean ± SD of eight different experiments.
*P < 0.05 by ANOVA followed by paired t-tests.
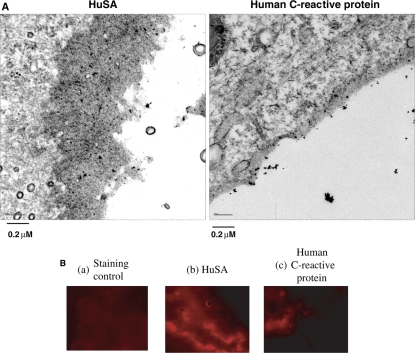
To confirm the in vitro effects of C-reactive protein in vivo, rats were treated ip with human C-reactive protein/HuSA. In C-reactive protein-treated rats (average C-reactive protein: 18.4 ± 5.9 mg/L), there was increased circulating levels of HA (HuSA: 29.2 ± 10.9 ng/mL vs. human C-reactive protein: 42.7 ± 15.5 ng/mL; P < 0.05). TEM confirmed that C-reactive protein impairs endothelial glycocalyx thickness in vivo (Figure 4A; average thickness: HuSA: 0.53 ± 0.15 µM vs. human C-reactive protein: 0.41 ± 0.11 µM; P < 0.05). Also, there was decreased staining of C-reactive protein-treated rat aortic endothelium with HS compared with HuSA (Figure 4B).
Figure 4.
Effect of C-reactive protein on glycocalyx in vivo. Wistar rats were treated with HuSA or human C-reactive protein (20 mg/kg body weight ip for 3 days) and aorta was removed for en face staining and for isolation of ECs as described in Section 2. Glycocalyx thickness was assessed by TEM as described in Section 2. Representative micrographs are shown in (A). Aorta was stained with antibodies to HS as described in Section 2 (B). (B,a) Negative control-no antibody, only PE; (B,b) HS staining with HuSA and (B,c) HS staining with human C-reactive protein.
4. Discussion
Inflammation plays a critical role in atherogenesis. C-reactive protein is a prototypic marker of inflammation and has been shown in numerous prospective studies to predict cardiovascular events.2 Much data are evolving to suggest that C-reactive protein also promotes endothelial dysfunction.3,4 Several studies have shown that high C-reactive protein levels are associated with impaired endothelial vasoreactivity.3,4 Also, three groups have independently shown that the human C-reactive protein transgenic (Tg) mice exhibit decreased eNOS activity in vivo, 8,30,31 corroborating the inverse correlation between C-reactive protein and endothelium vasoreactivity in human subjects. C-reactive protein has also been shown to induce hypertension in CF1 Tg mice expressing rabbit C-reactive protein attributable to C-reactive protein-induced decline in bioavailable NO.31 Furthermore, injection of adeno-associated virus vector with C-reactive protein in rats compared with control vector results in impaired endothelial vasoreactivity in vivo.32 In addition, we have shown that in vitro that C-reactive protein inhibits eNOS by uncoupling the enzyme.7 We have confirmed these in vitro findings in vivo in Sprague–Dawley rats, where we demonstrated that compared with HuSA, C-reactive protein significantly impaired endothelium-dependent vasodilation. Furthermore, this was accompanied by significant reduction in eNOS activity, eNOS dimer/monomer ratio, tetrahydrobiopterin levels, and protein expression of GTPCH1 in C-reactive protein-treated than HuSA-treated rats. Thus, C-reactive protein impaired endothelial function in vivo via uncoupling of eNOS.10 Using purified C-reactive protein, we have previously shown in vivo effects on up-regulating superoxide, myeloperoxidase, MMP-9, tissue factor, and promoting ox-LDL uptake.33–35 Also, the Stroes group36 has shown that infusion of C-reactive protein in humans resulted in impaired endothelium-dependent vasodilation.
The glycocalyx of the EC decorates the luminal surface of the endothelium and serves as a barrier to transvascular exchange of macromolecules and blood cell adhesion to the endothelium and may affect the resistance to blood flow within the microcirculation proper. Within the microvasculature, observations by electron microscopy using cationic markers reveal that the glycocalyx is composed of a highly sulfated layer of GAGs bound to a variety of proteins (proteoglycans).11,12 In vivo microvascular studies of enzymatic degradation of specific GAGs have revealed dramatic increases in capillary haematocrit, increased capillary permeability, enhanced leucocyte (white blood cell) adhesion, and diminished resistance to blood flow within the microcirculation.11,12 It has also been shown that the composition of the glycocalyx changes in microvessels during angiogenesis and with the onset of atherosclerosis in macrovessels. HS, a glucosaminoglycan and the most common GAG on the EC glycocalyx, is associated with ∼50–90% of endothelial proteoglycans.11,12 Also, the GAG HA may play a role in permeation of the glycocalyx by macromolecules and contribute to the structural integrity of the GAG protein matrix and play a critical role in EC dysfunction. Recent studies have recognized that the endothelial glycocalyx, an intraluminal layer, consisting mainly of HA and HS, contributes to the vasculoprotective effects of the vessel wall.11 HA, in the EC glycocalyx, appears to serve as a mechano-shear sensor and regulates NO release and maintains vascular permeability.12 The glycocalyx also appears to serve as a barrier for leucocyte adhesion and inflammatory states are associated with increased shedding of the endothelial glycocalyx.12 The thickness of the glycocalyx is reduced at high- compared with low-risk regions of the murine carotid artery.18 Also, hyaluronidase activity and plasma HA have been shown to be correlated with increased carotid intimal medial thickness.22 Exposure to ox-LDL or TNF-α in vivo reduces thickness of the EC glycocalyx.37,38 Furthermore, in Type 1 diabetics, EC glycocalyx is profoundly reduced compared with matched healthy controls.22 Plasma HA levels are increased in Type 1 diabetics and correlates significantly and inversely to systemic glycocalyx volume.21
In this study, we have used three biomarkers of the integrity of the glycocalyx. Previously, HA levels have been shown to correlate with in vivo measures of glycocalyx.21,22 HS is a significant GAG comprising the glycocalyx. Also, we examined the glycocalyx directly using TEM. Using all three valid measures, we show that C-reactive protein impairs the functional integrity of the glycocalyx. In this manuscript, we demonstrate that C-reactive protein impairs endothelial glycocalyx as evidenced by increased shedding of HA from EC glycocalyx, decreased cell-associated HS, and decreased glycocalyx thickness by TEM. Previously, Nieuwdorp et al.21 have shown that hyperglycaemia resulted in endothelial dysfunction and this was strongly correlated to glycocalyx volume and shedding of HA. In order to examine whether this reduction in glycocalyx by C-reactive protein results in impaired endothelial function, we also examined other biomarkers of endothelial activity such as eNOS, PAI-1, ICAM, and monocyte–EC adhesion. We and others have previously reported that C-reactive protein treatment of EC dose-dependently decreased eNOS activity and up-regulated PAI-1, ICAM-1, and adhesion and provided mechanistic insights.9 In this manuscript, we show that C-reactive protein-induced endothelial dysfunction/activation (decreased eNOS, increased PAI-1, ICAM-1, and adhesion) correlated significantly to impairment in glycocalyx (HA release). We also provide additional evidence in vivo of C-reactive protein impairing glycocalyx as demonstrated by increased HA in circulation, decreased HS staining in rat aortic endothelium, and impaired thickness of EC glycocalyx—these results are in support of our recent data in vivo demonstrating that C-reactive protein impairs endothelial vasoreactivity.10
Thus, in this study, we make the novel observation that C-reactive protein impairs the functional integrity of the glycocalyx in vitro and in vivo and this correlates with endothelial dysfunction/activation. Future studies will examine mechanisms by which EC glycocalyx is impaired in disease states such as in diabetes and hypertension and the role of the elevated C-reactive protein present in these conditions.
Funding
This work was supported by National Institutes of Health Grant [RO1 HL074360 and K24 AT00596] to I.J.
Acknowledgements
We thank Lydia Howell for providing us the information with regards to the transmission electron microscopy, and Samuel Park and Catherine Duncan-Staley for their technical assistance.
Conflicts of interest: none declared.
References
- 1.Hansson GK, Libby P. The immune response in atherosclerosis: a double-edged sword. Nat Rev Immunol. 2006;6:508–519. doi: 10.1038/nri1882. [DOI] [PubMed] [Google Scholar]
- 2.Ridker PM. C-reactive protein and the prediction of cardiovascular events among those at intermediate risk: moving an inflammatory hypothesis toward consensus. J Am Coll Cardiol. 2007;49:2129–2138. doi: 10.1016/j.jacc.2007.02.052. [DOI] [PubMed] [Google Scholar]
- 3.Verma S, Devaraj S, Jialal I. Is C-reactive protein an innocent bystander or proatherogenic culprit? C-reactive protein promotes atherothrombosis. Circulation. 2006;113:2135–2150. [PubMed] [Google Scholar]
- 4.Devaraj S, Singh U, Jialal I. The evolving role of C-reactive protein in atherothrombosis. Clin Chem. 2009;52:229–238. doi: 10.1373/clinchem.2008.108886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Venugopal SK, Devaraj S, Yuhanna I, Shaul P, Jialal I. Demonstration that C-reactive protein decreases eNOS expression and bioactivity in human aortic endothelial cells. Circulation. 2002;106:1439–1441. doi: 10.1161/01.cir.0000033116.22237.f9. [DOI] [PubMed] [Google Scholar]
- 6.Verma S, Wang CH, Li SH, Dumont AS, Fedak PW, Badiwala MV, et al. A self-fulfilling prophecy: C-reactive protein attenuates nitric oxide production and inhibits angiogenesis. Circulation. 2002;106:913–919. doi: 10.1161/01.cir.0000029802.88087.5e. [DOI] [PubMed] [Google Scholar]
- 7.Singh U, Devaraj S, Vasquez-Vivar J, Jialal I. C-reactive protein decreases endothelial nitric oxide synthase activity via uncoupling. J Mol Cell Cardiol. 2007;43:780–791. doi: 10.1016/j.yjmcc.2007.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Teoh H, Quan A, Lovren F, Wang G, Tirgari S, Szmitko PE, et al. Impaired endothelial function in C-reactive protein overexpressing mice. Atherosclerosis. 2008;201:318–325. doi: 10.1016/j.atherosclerosis.2008.02.034. [DOI] [PubMed] [Google Scholar]
- 9.Jialal I, Verma S, Devaraj S. Inhibition of endothelial nitric oxide synthase by C-reactive protein. Clin Chem. 2009;55:206–208. doi: 10.1373/clinchem.2008.119206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hein TW, Singh U, Vasquez-Vivar J, Devaraj S, Kuo L, Jialal I. Human C-reactive protein induces endothelial dysfunction and uncoupling of eNOS in vivo. Atherosclerosis. 2009 doi: 10.1016/j.atherosclerosis.2009.02.002. doi:10.1016/j.atherosclerosis.2009.02.002, Published online ahead of print February 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weinbaum S, Tarbell JM, Damiano ER. The structure and function of the endothelial glycocalyx layer. Annu Rev Biomed Eng. 2007;9:121–167. doi: 10.1146/annurev.bioeng.9.060906.151959. [DOI] [PubMed] [Google Scholar]
- 12.Nieuwdorp M, Meuwese MC, Vink H, Hoekstra JB, Kastelein JJ, Stroes ES. The endothelial glycocalyx: a potential barrier between health and vascular disease. Curr Opin Lipidol. 2005;16:507–511. doi: 10.1097/01.mol.0000181325.08926.9c. [DOI] [PubMed] [Google Scholar]
- 13.Weinbaum S, Zhang X, Han Y, Vink H, Cowin SC. Mechanotransduction and flow across the endothelial glycocalyx. Proc Natl Acad Sci USA. 2003;100:7988–7995. doi: 10.1073/pnas.1332808100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Florian JA, Kosky JR, Ainslie K, Pang Z, Dull RO, Tarbell JM. Heparan sulfate proteoglycan is a mechanosensor on endothelial cells. Circ Res. 2003;93:e136–e142. doi: 10.1161/01.RES.0000101744.47866.D5. [DOI] [PubMed] [Google Scholar]
- 15.Thi MM, Tarbell JM, Weinbaum S, Spray DC. The role of the glycocalyx in reorganization of the actin cytoskeleton under fluid shear stress: a ‘bumper-car’ model. Proc Natl Acad Sci USA. 2004;101:16483–16488. doi: 10.1073/pnas.0407474101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Henry CB, Duling BR. Permeation of the luminal capillary glycocalyx is determined by hyaluronan. Am J Physiol. 1999;277:H508–H514. doi: 10.1152/ajpheart.1999.277.2.H508. [DOI] [PubMed] [Google Scholar]
- 17.Constantinescu AA, Vink H, Spaan JA. Endothelial cell glycocalyx modulates immobilization of leukocytes at the endothelial surface. Arterioscler Thromb Vasc Biol. 2003;23:1541–1547. doi: 10.1161/01.ATV.0000085630.24353.3D. [DOI] [PubMed] [Google Scholar]
- 18.van den Berg BM, Spaan JA, Rolf TM, Vink H. Atherogenic region and diet diminish glycocalyx dimension and increase intima-to-media ratios at murine carotid artery bifurcation. Am J Physiol Heart Circ Physiol. 2006;290:H915–H920. doi: 10.1152/ajpheart.00051.2005. [DOI] [PubMed] [Google Scholar]
- 19.Pillarisetti S, Paka L, Obunike JC, Berglund L, Goldberg IJ. Subendothelial retention of lipoprotein (a). Evidence that reduced heparan sulfate promotes lipoprotein binding to subendothelial matrix. J Clin Invest. 1997;100:867–874. doi: 10.1172/JCI119602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lewis JC, Taylor RG, Jones ND, St Clair RW, Cornhill JF. Endothelial surface characteristics in pigeon coronary artery atherosclerosis. I. Cellular alterations during the initial stages of dietary cholesterol challenge. Lab Invest. 1982;46:123–138. [PubMed] [Google Scholar]
- 21.Nieuwdorp M, Mooij HL, Kroon J, Atasever B, Spaan JA, Ince C, et al. Endothelial glycocalyx damage coincides with microalbuminuria in type 1 diabetes. Diabetes. 2006;55:1127–1132. doi: 10.2337/diabetes.55.04.06.db05-1619. [DOI] [PubMed] [Google Scholar]
- 22.Nieuwdorp M, Holleman F, de Groot E, Vink H, Gort J, Kontush A, et al. Perturbation of hyaluronan metabolism predisposes patients with type 1 diabetes mellitus to atherosclerosis. Diabetologia. 2007;50:1288–1293. doi: 10.1007/s00125-007-0666-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dasu MR, Devaraj S, Du Clos TW, Jialal I. The biological effects of CRP are not attributable to endotoxin contamination: evidence from TLR4 knockdown human aortic endothelial cells. J Lipid Res. 2007;48:509–512. doi: 10.1194/jlr.C600020-JLR200. [DOI] [PubMed] [Google Scholar]
- 24.van den Berg BM, Vink H, Spaan JA. The endothelial glycocalyx protects against myocardial edema. Circ Res. 2003;92:592–594. doi: 10.1161/01.RES.0000065917.53950.75. [DOI] [PubMed] [Google Scholar]
- 25.Biasucci LM, Liuzzo G, Grillo RL, Caligiuri G, Rebuzzi AG, Buffon A, et al. Elevated levels of C-reactive protein at discharge in patients with unstable angina predict recurrent instability. Circulation. 1999;99:855–860. doi: 10.1161/01.cir.99.7.855. [DOI] [PubMed] [Google Scholar]
- 26.Ridker PM, Cannon CP, Morrow D, Rifai N, Rose LM, McCabe CH, et al. Pravastatin or Atorvastatin Evaluation, Infection Therapy-Thrombolysis in Myocardial Infarction 22 (PROVE IT-TIMI 22) Investigators. C-reactive protein levels and outcomes after statin therapy. N Engl J Med. 2005;352:20–28. doi: 10.1056/NEJMoa042378. [DOI] [PubMed] [Google Scholar]
- 27.Nitert MD, Chisalita SI, Olsson K, Bornfeldt KE, Arnqvist HJ. IGF-I/insulin hybrid receptors in human endothelial cells. Mol Cell Endocrinol. 2005;229:31–37. doi: 10.1016/j.mce.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 28.Devaraj S, Davis B, Simon SI, Jialal I. CRP promotes monocyte-endothelial cell adhesion via Fcgamma receptors in human aortic endothelial cells under static and shear flow conditions. Am J Physiol Heart Circ Physiol. 2006;291:H1170–H1176. doi: 10.1152/ajpheart.00150.2006. [DOI] [PubMed] [Google Scholar]
- 29.Devaraj S, Xu DY, Jialal I. C-reactive protein increases plasminogen activator inhibitor-1 expression and activity in human aortic endothelial cells: implications for the metabolic syndrome and atherothrombosis. Circulation. 2003;107:398–404. doi: 10.1161/01.cir.0000052617.91920.fd. [DOI] [PubMed] [Google Scholar]
- 30.Schwedler SB, Kuhlencordt PJ, Ponnuswamy PP, Hatiboglu G, Quaschning T, Widder J, et al. Native C-reactive protein induces endothelial dysfunction in ApoE−/− mice: implications for iNOS and reactive oxygen species. Atherosclerosis. 2007;195:e76–e84. doi: 10.1016/j.atherosclerosis.2007.06.013. [DOI] [PubMed] [Google Scholar]
- 31.Schwartz R, Osborne-Lawrence S, Hahner L, Gibson LL, Gormley AK, Vongpatanasin W, et al. C-reactive protein downregulates endothelial NO synthase and attenuates reendothelialization in vivo in mice. Circ Res. 2007;100:1452–1459. doi: 10.1161/01.RES.0000267745.03488.47. [DOI] [PubMed] [Google Scholar]
- 32.Guan H, Wang P, Hui R, Edin ML, Zeldin DC, Wang DW. Adeno-associated virus-mediated human C-reactive protein gene delivery causes endothelial dysfunction and hypertension in rats. Clin Chem. 2009;55:274–284. doi: 10.1373/clinchem.2008.115857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Singh U, Devaraj S, Jialal I. C-reactive protein stimulates myeloperoxidase release from polymorphonuclear cells and monocytes: implications for acute coronary syndromes. Clin Chem. 2009;55:361–364. doi: 10.1373/clinchem.2008.109207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Devaraj S, Dasu MR, Singh U, Rao LV, Jialal I. C-reactive protein stimulates superoxide anion release and tissue factor activity in vivo. Atherosclerosis. 2009;203:67–74. doi: 10.1016/j.atherosclerosis.2008.05.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Singh U, Dasu MR, Yancey PG, Afify A, Devaraj S, Jialal I. Human C-reactive protein promotes oxidized low density lipoprotein uptake and matrix metalloproteinase-9 release in Wistar rats. J Lipid Res. 2008;49:1015–1023. doi: 10.1194/jlr.M700535-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bisoendial RJ, Kastelein JJ, Peters SL, Levels JH, Birjmohun R, Rotmans JI, et al. Effects of CRP infusion on endothelial function and coagulation in normocholesterolemic and hypercholesterolemic subjects. J Lipid Res. 2007;48:952–960. doi: 10.1194/jlr.P600014-JLR200. [DOI] [PubMed] [Google Scholar]
- 37.Vink H, Constantinescu A, Spaan J. Oxidized lipoproteins degrade the endothelial surface layer. Circulation. 2000;101:1500–1502. doi: 10.1161/01.cir.101.13.1500. [DOI] [PubMed] [Google Scholar]
- 38.Henry C, Duling B. TNF-alpha increases entry of macromolecules into luminal endothelial cell glycocalyx. Am J Physiol Heart Circ Physiol. 2000;279:H2815–H2823. doi: 10.1152/ajpheart.2000.279.6.H2815. [DOI] [PubMed] [Google Scholar]