Abstract
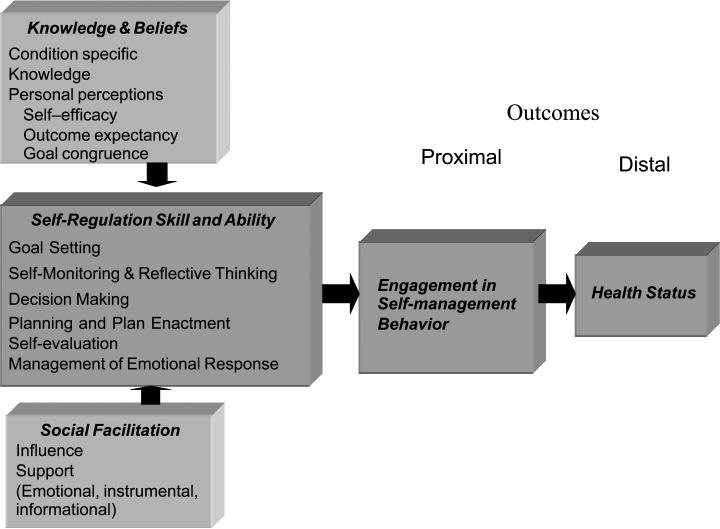
An essential characteristic of advanced practice nurses is the use of theory in practice. Clinical nurse specialists apply theory in providing or directing patient care, in their work as consultants to staff nurses, and as leaders influencing and facilitating system change. Knowledge of technology and pharmacology has far outpaced knowledge of how to facilitate health behavior change, and new theories are needed to better understand how practitioners can facilitate health behavior change. In this article, the Integrated Theory of Health Behavior Change is described, and an example of its use as foundation to intervention development is presented. The Integrated Theory of Health Behavior Change suggests that health behavior change can be enhanced by fostering knowledge and beliefs, increasing self-regulation skills and abilities, and enhancing social facilitation. Engagement in self-management behaviors is seen as the proximal outcome influencing the long-term distal outcome of improved health status. Person-centered interventions are directed to increasing knowledge and beliefs, self-regulation skills and abilities, and social facilitation. Using a theoretical framework improves clinical nurse specialist practice by focusing assessments, directing the use of best-practice interventions, and improving patient outcomes. Using theory fosters improved communication with other disciplines and enhances the management of complex clinical conditions by providing holistic, comprehensive care.
Keywords: clinical nurse specialists, health behavior change, Integrated Theory of Health Behavior Change, self-management
Personal behavior influences one's health.1,2 Many people can improve their health by managing their chronic condition or engaging in health promotion behaviors. Persons with chronic conditions improve their health by managing specific health behaviors, a process that requires behavior change. Healthy people, as well as persons with chronic conditions, have opportunities to improve their health by regularly engaging in health promotion activities, a behavior change process similar or identical to the process used to manage chronic conditions. For example, just as persons with pulmonary conditions who smoke need to change their behavior, healthy people who smoke may also need to change their behavior. Nurses and other healthcare professionals play a major role in identifying behaviors critical to health, assessing the needs of individuals and groups and recommending specific health behaviors, preparing and delivering interventions designed to enhance engagement in health behaviors, and evaluating the effectiveness of interventions for individuals, groups, communities, and the nation. To fulfill these role responsibilities, nurses and other healthcare professionals benefit from understanding the theory and science of health behavior change, what is known as well as the gaps and opportunities. Knowledge development and use are best when built on the success of the past.
The purpose of this article is to present a new midrange descriptive theory, the Integrated Theory of Health Behavior Change (ITHBC), and demonstrate the application of ITHBC in the development of an intervention. This article includes a discussion of select aspects of health behavior change; introduces the ITHBC, including concepts, definitions, and relationships among concepts; and provides an example of how the ITHBC was used to develop an intervention designed to facilitate a specific change.
HEALTH BEHAVIOR CHANGE
Chronic Conditions and Behavior Change
Researchers suggest that personal behaviors cause more than 50% of illnesses. Approximately 12% of children have special healthcare needs,3 7% of persons younger than 65 years have a serious life-altering chronic condition, and 37% of persons older than 65 years have 3 or more serious chronic conditions.4,5 Day-to-day management of these chronic conditions is the responsibility of the person and his/her family. However, persons and their families are often not prepared to assume this responsibility. Repeated readmission to acute care facilities,6,7 failure to reach targeted outcomes,8,9 and the continued need for unscheduled outpatient services10 are indicators that people need more help. Healthcare systems are being challenged to assume a greater role in assisting persons to better care for themselves.8,11 Successful management of chronic conditions benefits people as it improves their health status and well-being 4,11–14 Success enhances a family's cohesion and functioning.15,16 Improved outcomes also benefit the healthcare system and society.17
Health behaviors required to manage chronic conditions are numerous and varied.13,14,18 There is a growing body of evidence that there is a core group of behaviors common across the management of chronic conditions.8,9,19–23 For example, people with chronic conditions change their behaviors to manage symptoms such as pain, fatigue, or shortness of breath. Persons self-administer prescribed and over-the-counter medications. Health behaviors needed to manage medications include having and using resources to obtain the medications; accurately self-administering medications over time; and recognizing and reporting adverse effects, unintended outcomes, or failure to attain desired outcomes. Persons must know how to monitor and make decisions about disease indicators such as blood glucose, peak flow reading, or weight gain. People who successfully manage chronic conditions manage negative emotions associated with chronic conditions and fulfill responsibilities to their concomitant life roles.24,25
Health Promotion and Behavior Change
Health promotion also requires people to initiate and maintain health behavior changes. Commonly recognized behaviors such as activity and exercise, good nutrition, stress management, limited alcohol consumption, and smoking cessation positively affect health.1,17,26 Enactment of prevention behaviors is also needed. Prevention behaviors include things such as screening for breast cancer,27 applying preventative strategies for bone loss during menopausal transition and with age,28 or obtaining immunization for prevention of human papillomavirus infection.28 To improve or maintain their health status, people must have healthy lifestyles. Although the value of engaging in health-promoting activities is generally accepted, there is significant variability in how primary health promotion is incorporated into the healthcare system, schools, the work-place, and communities.
The discovery of knowledge about diseases, technological assessments, and pharmacology has far outpaced the knowledge of how to help people incorporate healthcare advances into their daily lives.12,29 Abundant information about health promotion is available, but the quality and accuracy of information differ across sources.30,31 Relatively little is available to help people sort through information, let alone apply it to their lifestyles. Healthcare professionals need to better understand how health behavior change is made and their role in facilitating and supporting change. How do people make health behavior change that persists over time?
Changing Needs and Perspectives
In the distant past, many acutely ill persons were encouraged and expected to assume a passive sick role.32 Hospital stays then were longer than today's, nursing and nursing assistants provide the care during recovery, and expectations for self-care after discharge were relatively simple.33,34 An increasing number of persons are surviving acute illnesses and a greater number of people live with chronic illnesses subject to acute exacerbations.35,36 People are treated and rapidly discharged from hospitals.37,38 Expectations for at-home management of complex conditions and treatment regimens have become common. People and their families are taught how to manage chronic conditions. Some people and families successfully managed, but many did not.
Health promotion was viewed as optional. Encouragement to engage in healthy behaviors was not always included in routine care; some healthcare professionals and systems embraced it, many others did not. When included in care settings, health promotion efforts tended to focus on single behaviors for individuals. General health was a fragmented concept, and information was modular and condition specific. New approaches to health promotion39 are directed to both individuals and populations, focus on multiple behaviors simultaneously, are delivered by professionals and laypersons,40 are increasingly sensitive to issues of culture and age,41 and occur across a variety of settings including schools, churches, and worksites. Contemporary interest in health promotion ranges from optimization of an individual's genetic makeup42 to construction of the health-promoting community's physical environments.43
Health Behavior Change: Lessons Learned
Four decades of research related to health behavior produced a better understanding of health behavior change.12,17,44–52 Researchers have examined health behaviors across a wide variety of conditions, persons, and venues and have tested a variety of interventions and theories. Changing one's health behaviors is a more complex process than originally envisioned. New health behaviors often are not maintained. Outcomes that have been achieved in controlled research studies have not been realized clinically.12 These discrepancies have a significant impact on the health (actual or potential) of the individual and on the health of society.1,2
Healthcare providers overestimate the extent to which people change.5,11,47,53 All too often, it is assumed that people change their behavior because the evidence supporting the benefits of change is so compelling. Healthcare systems regularly monitor treatment (especially cost and appropriateness) and outcomes, but the relationships between people's use of prescribed treatment and outcomes are seldom included in cost-benefit analysis.7,54–56 Measurement of one's engagement in health behavior change continues to be challenging. Self-reports of behavior are the most extensively used measure of engagement in health behavior. Self-report is accessible and inexpensive; however, it presents the perspective of the individual, a critical but limited picture.57,58
There is a lack of support for a number of previously held assumptions about health behavior change. Socio-demographic characteristics are poor predictors of persons’ likelihood to engage in health behavior change.47 Imparting factual information alone often does not result in the maintenance of long-term behavior change.8,12,45,59,60 Understanding and enhancing persons’ health beliefs (eg, Health Belief Model,48,61 Health Promotion Model,62 and Theory of Reasoned Action63,64) seem to foster initiation but not long-term maintenance of a health behavior.65 There is evidence that the trajectory of health behavior change seems to have a common pattern. For example, regardless of the behavior, the highest rate of relapse is seen very early after the change, and this has been seen across dieting, smoking cessation, increasing calcium intake, and others.12 Social factors affect behavior, but social factors can have either a negative or a positive impact on initiation and maintenance of health behavior change.12,62,66,67 It is not yet known whether adding a behavior (such as initiating an exercise program) differs from substitution (such as altering food choices), each of which could differ from extinction of a behavior (eg, smoking cessation).12
According to Whitehead,68 there is strong consensus for health promotion among nurses. And although there is a general understanding of health promotion, nurses struggle with understanding theoretical perspective related to health behavior change, best approaches, and evaluation of outcomes. Theory, specifically midrange theory, is useful because it provides an explanation of various situations and phenomenon. Although a great deal has been learned about health behavior change, challenges to nurses and other healthcare professionals are increasing. New theories are needed, theories building on past conceptual and empirical work.
Descriptive Midrange Theory and Advanced Practice Nurses
In contrast to the grand theories of nursing, midrange or middle-range, theories are more concrete and more easily used to guide practice.69 Often synthesized from knowledge and derived from the work of nurses or persons in other disciplines, midrange theories focus on a specific phenomenon like pain or uncertainty. Midrange theories are designed to be used in practice. There are numerous opportunities for advanced practice nurses (APNs) to use midrange theory while providing and directing clinical care. Using midrange theory can assist with the transfer, application, and evaluation of knowledge across individual and groups of patients. “Descriptive theory provides a description of what is happening in a situation and reveals the components that exist in a situation.”69(p192)
An essential characteristic of APNs is use of theory in practice.70 Clinical nurse specialists (CNSs) use theory to provide or direct patient care, in their work as consultants to staff nurses, and as leaders influencing and facilitating system change.71 Clinical nurse specialists use midrange theories that address phenomena relevant to their specialty. Theory-based practice enhances achievement of positive patient outcomes. It provides an explanation for a person's response to his/her condition or treatment. Theory-based practice helps clinicians be faster as it focuses their assessment. It fosters a match between the theory and evidence-based interventions and outcomes with existing, sensitive measures. Using theory decreases distractions and reduces time obtaining and sorting irrelevant information. It facilitates clear and timely communication with other professionals and interested parties (eg, health plan or insurance). Using theory is smart practice. Clinicians are able to observe patterns more quickly, manage complexity, and provide or direct holistic care. Using theory enhances the development of “practice wisdom” because it fosters pattern recognition.. Using theory helps ensure that a CNS practice is holistic and comprehensive.
ITHBC: A DESCRIPTIVE MIDRANGE THEORY
Development
The ITHBC was developed by the author and emerged from a systematic review of the literature.72 Ten years’ of peer-reviewed published research on interventions designed to facilitate health behavior change was reviewed. Rather than focusing on any single behavior or theory, components of interventions or programs were selected because of their efficacy (defined as statistically significant differences between groups).
During her postdoctoral fellowship (T32NR07102), Ryan developed the ITHBC by integrating those concepts that had been foundational to interventions previously identified. The interventions that resulted in changing health behaviors were influenced by a number of theories, including theories of health behavior change,12,18,44–49,51,61–65,73–78 self-regulation theories,79–85 social support theory,12,53,63,64,67,73,75,76,86–88 and research related to self-management of chronic illnesses.11,18,20,24,59,83,84,89–98 The descriptive theory reflected the observation that behavior was associated with interventions that addressed condition-specific knowledge and health beliefs, foster an increase in self-regulation skills and abilities, and enhanced social facilitation. The ITHBC is a blending of concepts from multiple theories and numerous empirical studies. There is strong empirical evidence for the inclusion of each of the concepts, and it is the proposed relationship among the concepts that is new in this descriptive midrange theory.
ITHBC Assumptions
New theories are needed to better understand health behavior change. The ITHBC is based on the assumption that behavior change is a dynamic, iterative process. Desire and motivation are prerequisites to change, and self-reflection facilitates progress. Positive social influences sway one's interest and willingness just as positive relationships help to support and sustain change. There is growing evidence that person-centered interventions are more effective than standardized interventions in facilitating health behavior change.99–101 Engagement in healthy behavior is an outcome that can be realized in the short-term (a proximal outcome), and engagement in health behavior influences and leads to improvement in health status, the distal outcome realized over time.
Description of ITHBC
The ITHBC (Figure 1) purports health behavior change can be enhanced by fostering knowledge and beliefs, increasing self-regulation skills and abilities, and enhancing social facilitation. Engagement in self-management behaviors is seen as the proximal outcome, and this, in turn, influences the long-term outcome of improved health status. Person-centered interventions are directed to increasing knowledge and beliefs, self-regulation skills and abilities, and social facilitation. According to this theory, persons will be more likely to engage in the recommended health behaviors if they have information about and embrace health beliefs consistent with behavior, if they develop self-regulation abilities to change their health behaviors, and if they experience social facilitation that positively influences and supports them to engage in preventative health behaviors.19,20,102,103 Knowledge and beliefs impact behavior-specific self-efficacy,74–76 outcome expectancy,75,76 and goal congruence.104 Self-regulation is the process used to change health behavior and includes activities such as goal setting, self-monitoring and reflective thinking, decision making, planning for and engaging in specific behaviors, and self-evaluating and self-managing physical, emotional, and cognitive responses associated with health behavior change.81,82,84 Social facilitation includes the concepts of social influence, social support, and negotiated collaboration between individuals and families and healthcare professionals.67
Figure 1.
Integrated Theory of Health Behavior Change.
Outcomes in this theory are both proximal and distal. The proximal outcome is actual engagement in self-management behaviors specific to a condition or health behavior. Distal outcomes refer to the long-term impact of personal behavior on health status. Failure to engage in healthy behaviors may result in premature onset of disease conditions. Distal outcomes are related, in part, to successful achievement of proximal outcomes. Although achievement of distal outcomes provides data about the effectiveness of the intervention, these outcomes are generally slow to be realized. Measurement of proximal outcomes is critical to evaluate whether people have made and are maintaining change in their health behavior.
The constructs of knowledge and beliefs, self-regulation, and social facilitation are related to each other and to the proximal and distal outcomes. Knowledge and beliefs are the first construct. Knowledge is defined as condition-specific factual information, and beliefs are defined as personal perceptions about the specific health condition or health behavior. Enhancement of knowledge and beliefs results in increased understanding of a specific condition or behavior, increased behavior-specific self-efficacy (confidence in one's ability to successfully engage in a change in normal and stressful situations), outcome expectancy (one's belief that engagement in a behavior will result in desired results), and goal congruence (resolution of confusion and anxiety occurring from apparent contradictory and competing demands associated with health goals). The second major construct is self-regulation. Self-regulation is a process that people use as they incorporate a behavior change into their daily routines and lifestyles. Self-regulation requires goal setting, self-monitoring and reflective thinking, decision making, planning and plan enactment, self-evaluation, and management of emotions occurring with the change. The third major construct is social facilitation. Social facilitation includes social influence and social support. People experience social influence when a knowledgeable person in a position of perceived authority sways their thinking and motivation, leading to engagement in behavior. Social influence comes from numerous sources, for example, healthcare providers, television and radio, family and neighbors, coworkers, or printed or electronic communication. Social support consists of emotional, instrumental, or informational support, which facilitates engagement in a health behavior.
The concept of goal congruence, one of the health belief concepts, is new to this work. It has been conceptually integrated from the works of Bandura75 and Carver and Scheier.81 Bandura discusses stress resulting from difficult or competing life events and the need for persons to ameliorate this stress by using secondary cognitive strategies. Carver and Scheier suggest that goals are hierarchical, ranging from abstract goals or general values to actual behaviors. Applied to osteoporosis prevention, a woman could have health promotion as an abstract principle or a “goal to be healthy,” but she could experience conflict among behaviors needed to promote health. Competing goals result in stress, and cognitive strategies such as reframing can help women identify how to achieve higher levels of goals by altering behaviors. For example, many women have a goal to reduce or maintain their weight and a goal to increase their calcium intake. It could be problematic to increase one's calcium intake by increasing caloric consumption with high-calorie dairy foods. To make these goals congruent, women need to find ways to both manage their weight and increase their calcium intake.
Relationships Among Constructs of the Theory
It is proposed that knowledge, in and of itself, does not lead to behavior change; however, knowledge and health beliefs are linked to engagement in self-regulation.59,98,105–112 Engagement in self-regulation skills and abilities enhances self-management behaviors. Positive social facilitation enhances self-regulation and engagement in self-management behaviors. Engagement in self-management behaviors has a direct and positive effect on health status.14,20,94,97,109,113–117
Additions of and Empirical Support for ITHBC
This new, descriptive theory adds several elements to the discussion of health behavior change. Concepts included in the theory have strong empirical base. Proposed relationships among constructs are new. All major constructs contain defining concepts. The process components have been clearly articulated. The concept of social facilitation has been expanded and developed. Outcomes have been conceptualized as proximal and distal. The ITHBC is intended to facilitate health behavior change related to management of chronic conditions and to health promotion.
Initial testing has provided evidence that the concepts within the theory explain approximately 25% of the variation for a specific health behavior change and up to 45% of the variance when select characteristics of the participants (race/ethnicity and body mass index) are used as moderators (P. Ryan et al, unpublished manuscript, 2005).38,118 The ITHBC is being tested in a number of studies funded by the National Institute of Nursing Research (1R15NR009021-01A2 and 1P20NR0010674-01).
ITHBC AS FOUNDATIONAL TO THE DEVELOPMENT OF AN INTERVENTION
Concepts from the ITHBC were used to develop an intervention related to the prevention or attenuation of osteoporosis (1R15NR009021). A description of the intervention is provided as an example of a theory-based intervention. The intervention was designed to foster health behavior change, specifically osteoporosis prevention, by enhancing knowledge and beliefs, facilitating development of self-regulation skills and beliefs, and enriching social facilitation. The intervention is delivered electronically and enhances, not eliminates, individualized care.
Prevention of osteoporosis and fractures associated with low bone density requires women to regularly engage in a number of health behaviors, such as consuming an adequate intake of calcium and vitamin D, engaging in weight-bearing activities, enhancing balance during the middle-age years to prevent falls associated with fragile fractures, monitoring bone density, and taking prescribed medications.28,119–123 Although there is a genetic component to the development of osteoporosis, hormonal changes occurring during menopausal transition cause a decrease in bone density. During this life transition, women may have an opportunity to attenuate or slow the development of osteoporosis by ensuring an adequate intake of calcium and vitamin D, regularly engaging in weight-bearing exercise, maintaining or enhancing their balance, and collaborating with healthcare professionals to ensure they obtain recommended bone density scans as recommended.
Women begin the intervention by completing a focused assessment. Congruent with the ITHBC, women are assessed for their knowledge about osteoporosis and factors associated with prevention, their perceived risk factors, and their health beliefs related to osteoporosis. Women's calcium intake is determined, as well as their behavior-specific self-efficacy, outcome expectancy, and factors affecting their goal congruence. On the basis of the results of this assessment, women receive information specifically tailored to match their responses.124 The content of the intervention is evidence based and has been prepared to increase their knowledge and enhance their self-efficacy, outcome expectations, and goal congruence.
Women learn the skills and abilities of self-regulation to understand how to apply knowledge and beliefs to their lives. Learning and using self-regulation skills occur via a computer program developed specifically for this intervention. With the assistance of the computer, women are guided to identify specific goals.104 Extensive arrays of goals are available for selection, and women select 1 or more goals based on their understanding, preferences, and current behaviors. Goals are further individualized as women create a plan on how to enact their goal. For example, they can choose to focus on 1 or more behaviors. They can begin confidently by taking big steps or begin slowly by making small incremental changes. They can choose to increase their calcium intake via foods, supplements, or a combination of foods and supplements. They can choose the type or types of weight-bearing exercise they are interested in and the frequency, intensity, and duration for the exercise. They can choose among alternative methods of enhancing balance such as a specially developed sequence of exercises or engagement in select Thai Chi movements.
Once the woman has determined her goal(s), she is assisted in monitoring her current behaviors related to this goal. For example, when a woman chooses to increase her calcium intake, she is able to choose how frequently she wants to monitor her progress and which assessment tools she wants to use (choice of self-monitoring tool can be changed daily based on individual preference and eating habits). Over time, the woman is provided graphic feedback displaying the extent to which she is meeting her personal goal, comparing her previous behaviors to national recommendations (normative feedback) or to her current behaviors (ipsitative feedback). The computer assists women to reflect on their goals, specific plans, and relative success via journaling exercises. Progress is recognized and the computer program provides built-in suggestions to aid in managing common challenges faced when changing these specific behaviors. Women are encouraged to use the computer program at least 3 to 5 times per week over an 8-week period or until they are able to meet their goals regularly without engaging in the steps of the self-regulation process.
The intervention is designed to influence women in a number of ways. Electronic information has been prepared so women are able to receive information from a virtual person with informational authority, such as a recommendation from a health provider, the Surgeon General, or the National Osteoporosis Foundation. “Stories” are embedded in the context of the intervention. These stories role model how other women have managed. The intervention contain personal feedback and numerous messages of encouragement. Women are able to communicate electronically or by telephone with a healthcare provider (a CNS in this case).
The ITHBC was foundational to the development of the intervention.104 The intervention contained the required constructs of knowledge and beliefs, self-regulation skills and abilities, and social facilitation. The intervention begins with assessing each woman in terms of these dimensions and is designed to focus on and enhance these 3 dimensions. The ITHBC provided direction for selection of meaningful and sensitive outcomes. The proximal outcome, engagement in self-management behaviors of calcium and vitamin D intake, weight-bearing exercise, balance enhancement, and collaboration for appropriate monitoring are assessed. Achievement of these outcomes provides a measure of the effectiveness of the intervention, and engagement in these behaviors is congruent with long-term bone health.
IMPLICATIONS: ISSUES RELATED TO USE OF THEORY IN PRACTICE
Many people enjoy leisurely shopping. They get to see what is new and what is on sale and generate ideas about what is available and possible. It can be fun, relaxing, and social. But when time is limited and expectations for results are high, structured shopping has better results than leisure shopping does, especially when items are categorized by store and organized geographically and individual items are clearly specified. Shopping without a plan is similar to developing an intervention without a theory. Developing an intervention without a theory puts one in a position where any information, content, or delivery method could be included or excluded for unspecified reasons. Using theory to develop an intervention makes a CNS better, faster, and smarter. Using concepts from multiple unrelated theories is better than not having any structure, but using unrelated concepts is like going shopping with an unorganized list. One has a much higher likelihood of finding what is needed, but it requires more time and backtracking. Clinical time is precious, and expectations for patient satisfaction and outcomes are high. Use of the ITHBC creates the structure identifying those factors essential to the development of an intervention fostering health behavior change. Using the ITHBC makes it clear that enhancing knowledge and beliefs, self-regulation skills and abilities, and social facilitation leads to engagement in self-management behaviors and is associated with greater likelihood of desired outcomes.
As a midrange theory, the ITHBC has been developed to increase a person's ability to engage in behavior change to increase his/her self-management behaviors. The success and utility of the theory depend, in part, on the ability of the CNS to correctly match the theory to the clinical problem. For example, the ITHBC will not provide the foundation of clinical concepts helpful to providing care to persons with dementia or in an emergency or crisis situation, but it does provide the foundation for structuring interventions for an wide array of persons and populations needing health behavior change. With the complexity of patient conditions, it may be necessary for the CNS to rely on more than 1 midrange theory when providing care or providing consultation for the care of a single patient or patient population.
Advanced practice nurses and graduate nursing students often express uncertainty about how to use theory in practice. Ideally, theory informs research and practice, and research and practice inform and shape theory, a process termed praxis. Praxis is this iterative and integrative process that produces reciprocal influence and change between clinical practice and theory.125–127 Assessment components, selection of interventions, and choice of clinical outcome measures are influenced by theory. Clinical successes and struggles support or provide data to question the relative helpfulness of components of the theory in specific clinical conditions and situations. Schwartz-Barcott and colleagues128 propose the use of a systematic approach, “fieldwork,” to actually engage in the work of praxis. A specific midrange theory in practice is mindfully chosen for use by APNs engaging in fieldwork. They engage in evaluating theimpactofamidrange theory within specific settings or for particular conditions. Fieldwork improves the link between theory and practice; hence, the author advocate a systematic approach to alteration of theory relevant to practice. Im and Meleis129 propose a different but related process in which the midrange theory is adapted to become a situation-specific theory, or the alteration of theory to meet the specific needs of a group of patients. For example, the midrange theory of self-efficacy is adapted to meet the specific needs and concerns of persons with chronic heart failure or diabetes.130
CONCLUSION
Engagement in healthy behavior is essential to improvement of health and management of chronic conditions. Nurses and other healthcare providers benefit from knowing how to support the initiation and maintenance of health behavior change by individuals. Significant progress has been made in understanding behavior change, but additional knowledge is needed to meet the health goals of individuals and society. New theories are needed to provide internally logical and coherent perspective to achieve these goals. The ITHBC presented in this article is an integration of past successes and makes substantive contributions to understanding health behavior by combining knowledge and beliefs, self-regulation processes, and social facilitation. It is purported that the behavior changes necessary to manage chronic conditions are more similar than different than behavior changes necessary for health promotion. Measurement of behavior occurs proximally to ensure that behavior change has actually occurred, as well as distally to ensure attainment of improved health status. Advanced practice nurses benefit directly from using and sharing midrange theories and are educated and positioned to provide the continual iterative and integrative processes that make practice better because of theory and theory better because of practice.
Acknowledgments
Funding sources for this study were the following: Patient Centered Informational Interventions (Brennan, Ryan Postdoctoral Fellowship, T32NR07102), Tailored Computerized Intervention for Behavior Change (Ryan, 1R15NR009021-01A2), and Center for Enhancement of Self-management in Individuals and Families (Marek, 1P20NR0010674-01, Ryan CO and Center Scientist).
Footnotes
Editor's Note: In 2009, we will publish 6 articles for which 1 to 3 credit hours may be earned as part of a CNS's learning activities. Examination questions are provided at the end of this article for your consideration. See the answer/enrollment form after the article for additional information regarding the program.
- Identify concepts of health behavior change.
- Describe the ITHBC and how it can be used to facilitate health behavior changes.
References
- 1.National Center for Health Statistics . Healthy People 2000 Final Review. Public Health Service; Hyattsville, MD: 2001. [Google Scholar]
- 2.U.S. Department of Health and Human Services . Healthy People 2010: Understanding and Improving Health. 2nd ed. U.S. Government Printing Office; Washington, DC: 2000. [Google Scholar]
- 3.van Dyck PC, Kogan MD, McPherson MG, Weissman GR, Newacheck PW. Prevalence and characteristics of children with special health care needs. Arch Pediatr Adolesc Med. 2004;158:884–890. doi: 10.1001/archpedi.158.9.884. [DOI] [PubMed] [Google Scholar]
- 4.Center for Disease Control [March 28, 2008];Chronic Disease Program. Chronic disease overview. http://www.cdc.gov/print.do?url=http://www.cdc.gov/nccdphp/overview.htm.
- 5.Committee on Communication for Behavior Change in the 21st Century . Speaking of Health: Assessing Health Communication Strategies for Diverse Populations. The National Academies Press; Washington, DC: 2002. p. 1. [Executive summary] [PubMed] [Google Scholar]
- 6.Naylor M. Transitional care of older adults. Annu Rev Nurs Res. 2002;20:127–147. [PubMed] [Google Scholar]
- 7.Doran D, editor. Nursing-Sensitive Outcomes: State of the Science. Jones & Bartlett; Sandbury, MA: 2003. [Google Scholar]
- 8.Bodenheimer T. Helping patient improve their health-related behaviors: what system changes do we need? Dis Manag. 2005;8(5):319–330. doi: 10.1089/dis.2005.8.319. [DOI] [PubMed] [Google Scholar]
- 9.Bodenheimer T. Interventions to improve chronic illness care: evaluating their effectiveness. Dis Manag. 2003;6(2):63–71. doi: 10.1089/109350703321908441. [DOI] [PubMed] [Google Scholar]
- 10.Marek KD, Popejoy L, Petroski G, Mehr D, Rantz M, Lin WC. Clinical outcomes of aging in place. Nurs Res. 2005;54(3):202–211. doi: 10.1097/00006199-200505000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Center for the Advancement of Health [January 2008];Health behavior change in managed care: a status report executive summary. http://www.cfah.org/pdfs/health_execsumm.pdf.
- 12.Institute of Medicine . Health and Behavior: The Interplay of Biological, Behavioral, and Societal Influences: Committee on Health and Behavior: Research, Practice and Policy Board on Neuroscience and Behavioral Health. National Academy Press; Washington, DC: 2001. [Google Scholar]
- 13.Lorig K, Sobel DS, Stewart AL, et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization. Med Care. 1999;37:5–14. doi: 10.1097/00005650-199901000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Lorig KR, Sobel DS, Ritter PL, Laurent DD, Hobbs M. Effect of a self-management program on patients with chronic disease. Eff Clin Pract. 2001;4(6):256–262. [PubMed] [Google Scholar]
- 15.Feetham SL, Thomson EJ. Keeping the individual and family in focus. In: Miller SM, MCDaniel SH, Rolland JS, Feetham SL, editors. Individual, Families, and the New Era of Genetics: Biopsychosocial Perspectives. WW Norton; New York, NY: 2006. pp. 102–110. [Google Scholar]
- 16.Grey M, Knafl K, McCorkle R. A framework for the study of self- and family management of chronic conditions. Nurs Outlook. 2006;54(5):278–286. doi: 10.1016/j.outlook.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 17.US Department of Health and Human Services . Healthy People 2010: Understanding and Improving Health. 2nd ed. US Government Printing Office; Washington, DC: 2000. [Google Scholar]
- 18.Clark NM, Becker MH, Janz NK, Lorig KR, Bakowski W, Andereson L. Self-management of chronic disease by older adults: a review and questions for research. J Aging Health. 1991;3(1):3–27. [Google Scholar]
- 19.Lorig K, Ritter PL, Plant K. A disease-specific self-help program compared with a generalized chronic disease self-help program for arthritis patients. Arthritis Rheum. 2005;53(6):950–957. doi: 10.1002/art.21604. [DOI] [PubMed] [Google Scholar]
- 20.Barlow J, Sturt J, Hearnshaw H. Self-management interventions for people with chronic conditions in primary care: examples from arthritis, asthma and diabetes. Health Educ J. 2002;61(4):365–378. [Google Scholar]
- 21.Parry C, Kramer HM, Coleman EA. A qualitative exploration of a patient-centered coaching intervention to improve care transitions in chronically ill older adults. Home Health Care Serv Q. 2006;25:39–53. doi: 10.1300/J027v25n03_03. [DOI] [PubMed] [Google Scholar]
- 22.Schreurs KMG, Colland VT, Kuijer RG, de Ridder DTD, van Elderen T. Development, content, and process evaluation of a short self-management intervention in patients with chronic disease require self-care behaviors. Patient Educ Couns. 2003;51:133–141. doi: 10.1016/s0738-3991(02)00197-0. [DOI] [PubMed] [Google Scholar]
- 23.Tsai AC, Morton SC, Mangione CM, Keeler EB. A meta-analysis of interventions to improve care for chronic illnesses. Am J Manag Care. 2005;11:478–488. [PMC free article] [PubMed] [Google Scholar]
- 24.Lorig KR. Chronic disease self-management. Am Behav Sci. 1996;39(6):676–683. [Google Scholar]
- 25.Miller JF, editor. Coping With Chronic Illness: Overcomming Powerlesness. 3rd ed. FA Davis; Philadelphia, PA: 2000. [Google Scholar]
- 26.USDHHS . Steps to a Healthier US: A Program and Policy Perspective: Prevention Strategies That Work. USDHHS; Washington, DC: 2003. [Google Scholar]
- 27.US Preventative Task Force [January 5, 2009];Screening for breast cancer. 2008 http://www.ahrq.gov/clinic/3rduspstf/breastcancer/brcanrr.htm.
- 28.US Department of Health and Human Services . Bone Health and Osteoporosis: A Report of the Surgeon General. US Department of Health and Human Services, Office of the Surgeon General; Rockville, MD: 2004. [Google Scholar]
- 29.Wagner ED. The role of patient care teams in chronic disease management. Br Med J. 2000;320:567–572. doi: 10.1136/bmj.320.7234.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Institute of Medicine. Committee on Health Literacy. Board on Neuroscience and Behavioral Health . Health Literacy: A Prescription to End Confusion. The National Academies Press; Washington, DC: 2004. [Google Scholar]
- 31.US Department of Health and Human Services Office of Disease Prevention and Health Promotion (ODPHP) [September 22, 2008];Improved healthfinder.gov makes health information quicker and easier to use: DHHS. 2008 http://www.hhs.gov/ophs/news/20080922.html.
- 32.Parsons T. The Social System. Free Press; Glencoe, IL: 1951. [Google Scholar]
- 33.Bayliss EA. Supporting self-management for patients with complex medical needs: recommendations of a working group. Chron Illn. 2007;3(2):167–175. doi: 10.1177/1742395307081501. [DOI] [PubMed] [Google Scholar]
- 34.Sevick MA, Trauth JM, Ling BS, et al. Patients with complex chronic diseases: perspectives on supporting self-management. J Gen Intern Med. 2007;22(suppl 3):438–444. doi: 10.1007/s11606-007-0316-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Destache CJ, Dewan N, O'Donohue WJ, Campbell JC, Angelillo VA. Clinical and economic considerations in the treatment of acute exacerbation of chronic bronchitis. J Antimicrob Chemother. 1999;43(suppl A):107–113. doi: 10.1093/jac/43.suppl_1.107. [DOI] [PubMed] [Google Scholar]
- 36.Seneff MG, Wagner DP, Wagner JE, Zimmerman JE, Knaus WA. Hospital and 1-year survival of patients admitted to intensive care units with acute exacerbation of chronic obstructive pulmonary disease. JAMA. 1995;274(23):1852–1857. [PubMed] [Google Scholar]
- 37.Weiss M, Piacentine LB, Lokken A, et al. Perceived readiness of hospital discharge in adult medical-surgical patients. Clin Nurse Spec. 2007;21(3):31–42. doi: 10.1097/00002800-200701000-00008. [DOI] [PubMed] [Google Scholar]
- 38.Weiss M, Ryan P, Lokken A, Nelson E. Length of stay after vaginal birth: socio-demographics and readiness-for-discharge. Birth. 2004;31(2):93–101. doi: 10.1111/j.0730-7659.2004.00286.x. [DOI] [PubMed] [Google Scholar]
- 39.Prochaska JO. Multiple health behavior research represents the future of preventive medicine. Prev Med. 2008;46:281–285. doi: 10.1016/j.ypmed.2008.01.015. [DOI] [PubMed] [Google Scholar]
- 40.Tessaro IA, Taylor S, Belton L, et al. Adapting a natural (lay) helpers model of change for worksite health promotion for women. Health Educ Res. 2008;15(5):603–614. doi: 10.1093/her/15.5.603. [DOI] [PubMed] [Google Scholar]
- 41.Gordon C. Live Well Live Long: Health Promotion and Disease Prevention for Older Adults. American Society on Aging; Cal State, LA: 2006. American Society on Aging, Edward R. Roybal, Institute for Applied Gerontology. [Google Scholar]
- 42.Chen LS, Kowok OM, Goodson P. US health educators’ likelihood of adopting genomic competencies into health promotion. Am J Public Health. 2008;98(9):1651–1657. doi: 10.2105/AJPH.2007.122663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bassett EM, Glandon RP. Influencing design, promoting health. J Public Health Manag Pract. 2008;14(3):244–254. doi: 10.1097/01.PHH.0000316483.65135.a1. [DOI] [PubMed] [Google Scholar]
- 44.DiClemente C, Kegler MC. Emerging Theories in Health Promotion Practice and Research. Jossey-Bass; San Francisco, CA: 2002. [Google Scholar]
- 45.Glanz K, Lewis FM, Rimer BK. Health Behavior and Health Education: Theory, Research and Practice. Jossey-Bass; San Francisco, CA: 1997. [Google Scholar]
- 46.Gochman DS, editor. Handbook of Health Behavior Research II: Provider Determinants. Plenum; New York, NY: 1997. [Google Scholar]
- 47.Haynes B, Taylor DW, Sackett DL. Compliance in Health Care. Johns Hopkins University Press; Baltimore, MD: 1979. [Google Scholar]
- 48.Janz NK, Becker MH. The health belief model: a decade later. Health Educ Behav. 1984;11(1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 49.Marlatt GA, Gordon JR, editors. Prevention: Maintenance Strategies in the Treatment of Addictive Behaviors. Guilford Press; New York, NY: 1985. [Google Scholar]
- 50.Norman P. Predicting Health Behavior. Open University Press; Philadelphia, PA: 1998. [Google Scholar]
- 51.Shumaker SA, Schron EB, Ockene JK, McBee WL, editors. The Handbook of Health Behavior Change. 2nd ed. Springer; New York, NY: 1998. [Google Scholar]
- 52.Glanz K, Rimer B, Su S. Theory at a Glance: A Guide for Health Promotion Practice. Vol. 2. National Cancer Institute; Bethesda, MD: 2005. [Google Scholar]
- 53.Greene J, Yedidia MJ, The Take Care to Learn Evaluation Collaborative Provider behaviors contributing to patient self-management of chronic illness among underserved populations. J Health Care Poor Underserved. 2005;16:808–824. doi: 10.1353/hpu.2005.0097. [DOI] [PubMed] [Google Scholar]
- 54.Given B, Beck S, Etland C, Holmes Gobel B, Lamkin L, Marsee VD. Nursing-Sensitive Patient Outcomes. Oncology Nursing Society; Pittsburg, PA: 2004. [Google Scholar]
- 55.McCauley KM, Bixby MB, Naylor MD. Advanced practice nurse strategies to improve outcomes and reduce costs in elders with health failure. Dis Manag. 2006;9(5):302–310. doi: 10.1089/dis.2006.9.302. [DOI] [PubMed] [Google Scholar]
- 56.International Council of Nurses [September 28, 2008];Position statement: promoting the value and cost-effectiveness of nursing. 2001 http://icn.ch/psvalue.htm.
- 57.Donaldson SI, Grant-Vallone EJ. Understanding self-report bias in organizational behavior research. J Bus Psychol. 2002;17(2):245–260. [Google Scholar]
- 58.Fernandez-Ballesteros R, Botella J. Self-report measures. In: Nezu AM, Nezu CM, editors. Evidence-Based Outcome Research: A Practical Guide to Conducting Randomized Controlled Trials for Psychosocial Interventions. Oxford; New York, NY: 2008. pp. 95–120. [Google Scholar]
- 59.Lorig KR, Holman HR. Self-management and education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26(1):1–7. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- 60.Sin MK, Kang DH, Weaver M. Relationships of asthma knowledge, self-management, and social support in African American adolescents with asthma. Int J Nurs Stud. 2005;42:307–313. doi: 10.1016/j.ijnurstu.2004.06.013. [DOI] [PubMed] [Google Scholar]
- 61.Becker MH. The Health Belief Model and Personal Health Behaviors. Charles B Slack Inc; Thorofare, NJ: 1974. [Google Scholar]
- 62.Pender NJ, Murdaugh C, Parsons MA. Health Promotion in Nursing Practice. Vol. 4. Appleton & Lang; Norwalk, CT: 2002. [Google Scholar]
- 63.Ajzen I, Albarracin D, Hornick . Predicting and Change of Health Behavior: Applying the Reasoned Action Approach. Lawrence Erlbaum Associates; Mahwah, NJ: 2007. [Google Scholar]
- 64.Ajzen I, Fishbein M. Understanding Attitudes and Predicting Social Behavior. Prentice Hall; Englewood Cliffs, NJ: 1980. [Google Scholar]
- 65.Nigg CR, Allegrante JJP, Ory M. Theory-comparison and multiple-behavior research: common themes advancing health behavior research. Health Educ Res. 2002;17(5):670–679. doi: 10.1093/her/17.5.670. [DOI] [PubMed] [Google Scholar]
- 66.Skinner TC, John M, Hampson SE. Social support and personal models of diabetes as predictors of self-care and well-being: a longitudinal study of adolescents with diabetes. J Pediatr Psychol. 2000;25(4):257–267. doi: 10.1093/jpepsy/25.4.257. [DOI] [PubMed] [Google Scholar]
- 67.Cohen S, Underwood LG, Gottlieb BH. Social Support Measurement and Intervention. Oxford University Press; New York, NY: 2000. [Google Scholar]
- 68.Whitehead D. An international Delphi study examining health promotion and health education in nursing practice, education and policy. J Clin Nurs. 2008;17:891–900. doi: 10.1111/j.1365-2702.2007.02079.x. [DOI] [PubMed] [Google Scholar]
- 69.Rodgers BL. Developing Nursing Knowledge: Philosophical Traditions and Influences. Lippincott Williams & Wilkins; Philadelphia, PA: 2005. [Google Scholar]
- 70.American Association of Colleges of Nursing [April 28, 2008];The essential of master's education for advance practice nursing. http://www.aacnnche.edu/Education/pdf/MasEssentials96.pdf.
- 71.National Association of Clinical Nurse Specialists 2004 Statement Development Task Force . Statement on Clinical Nurse Specialist Practice and Education. National Association of Clinical Nurse Specialists; Harrisburg, PA: 2004. [Google Scholar]
- 72.Ryan P. Interventions to Facilitate Behavior Change. Marquette University College of Nursing; Milwaukee, WI: 1998. [Google Scholar]
- 73.Ajzen I. Understanding attitudes and predicting social behavior. Prentice Hall; Englewood Cliffs, NJ: 1980. [Google Scholar]
- 74.Bandura A. Self-efficacy: The Exercise of Control. WH Freeman & Company; New York, NY: 1997. [Google Scholar]
- 75.Bandura A. Social Foundations of Thoughts & Action: A Social Cognitive Theory. Prentice Hall; Englewood Cliffs, NJ: 1986. [Google Scholar]
- 76.Bandura A. Social Learning Theory. Prentice Hall; Englewood Cliffs, NJ: 1977. [Google Scholar]
- 77.Glasgow RE, Funnell MM, Bonomi AE, Diavis C, Beckham V, Wagner EH. Self-management aspects of the improving chronic illness care breakthrough series: implementation with diabetes and heart failure teams. Ann Behav Med. 2002;24(2):80–87. doi: 10.1207/S15324796ABM2402_04. [DOI] [PubMed] [Google Scholar]
- 78.Gochman DS. Health Behavior: Emerging Research Perspectives. Plenum Press; New York, NY: 1988. [Google Scholar]
- 79.Baumeister RF, Vohs KD. Handbook of Self-regulation: Research, Theory, and Applications. Guilford Press; New York, NY: 2004. [Google Scholar]
- 80.Boekaerts M, Pintrich PR, Zeidner M. Handbook of Self-regulation. Academic Press; San Diego, CA: 2000. [Google Scholar]
- 81.Carver CS, Scheier MF. On the Self-regulation of Behavior. Cambridge University Press; New York, NY: 1998. [Google Scholar]
- 82.Carver CS, Scheier MF, Boekaerts M, Pintrich PR, Zeidner M. On the Structure of Behavioral Self-regulation. Handbook of Self-regulation. Academic Press/Harcourt; San Diego, CA: 2002. p. 41. [Google Scholar]
- 83.Creer TL, Holroyd KA. Self-management. In: Baum A, Newman S, Weinman J, West R, McManus C, editors. Cambridge Handbook of Psychology, Health and Medicine. Cambridge University Press; Cambridge, England: 1997. pp. 255–258. [Google Scholar]
- 84.Holroyd KA, Creer TL. Self-management of Chronic Disease: Handbook of Clinical Interventions and Research. Academic Press Inc; Orlando, FL: 1986. [Google Scholar]
- 85.Karoly P. Mechanisms of self-regulation: a systems view. Annu Rev Psychol. 1993;44:23–52. [Google Scholar]
- 86.Jenerette CM, Phillips RCS. An examination of differences in intra-personal resources, self-care management, and health outcomes in older and younger adults with sickle cell disease. South Online J Nurs Res. 2006;7:1–24. [Google Scholar]
- 87.Mancini JA, Bowen GL, Martin JA. Community social organization: a conceptual linchpin in examining families in the context of community. Fam Relations. 2005;54(5):570–582. [Google Scholar]
- 88.Shoor S, Lorig KR. Self-care and the doctor-patient relationship. Med Care. 2002;40(4 suppl):II–40–II–44. doi: 10.1097/00005650-200204001-00007. [DOI] [PubMed] [Google Scholar]
- 89.Bodenheimer T, Lorig KR, Holman HR, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002;288(19):2469–2475. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 90.Burckhardt CS. Educating patients: self-management approaches. Disabil Rehabil. 2005;27(12):703–709. doi: 10.1080/09638280400009097. [DOI] [PubMed] [Google Scholar]
- 91.Cincinnati Children's Hospital Chronic Care: Self-Management Guideline Team [February 2008];Chronic care: self-management. www.cincinnatichildrens.org/syc/alpha/h/health-policy/ev-based/chronic-care.htm.
- 92.Coates VE, Boore JR. Self-management of chronic illness: implications for nursing. Int J Nurs Stud. 1995;32(6):628–640. doi: 10.1016/0020-7489(95)00043-5. [DOI] [PubMed] [Google Scholar]
- 93.Lorig K, Holman H. Living a Healthy Life With Chronic Conditions. Self-management of Heart Disease, Arthritis, Diabetes, Asthma, Bronchitis, Emphysema and Others. Bull; Palo Alto, CA: 2000. [Google Scholar]
- 94.Lorig K, Ritter P, Stewart AL, et al. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Med Care. 2001;39(11):1217–1223. doi: 10.1097/00005650-200111000-00008. [DOI] [PubMed] [Google Scholar]
- 95.Newman S, Steed L, Mulligan K. Self-management interventions for chronic illness. Lancet. 2004;364:1523–37. doi: 10.1016/S0140-6736(04)17277-2. [DOI] [PubMed] [Google Scholar]
- 96.Wagner EH. [July 20, 2007];Chronic care model. http://www.ihi.org/IHI/Topics/ChronicConditions/AllConditions/Changes.
- 97.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic disease. Milbank Q. 1996;74(4):511–544. [PubMed] [Google Scholar]
- 98.Warsi A, Wang PS, LaValley M, Avorn J, Solomon DH. Self-management education programs in chronic disease: a systematic review and methodological critique of the literature. Arch Intern Med. 2004;164(15):1641–1649. doi: 10.1001/archinte.164.15.1641. [DOI] [PubMed] [Google Scholar]
- 99.Brown S. Patient-Centered Communication. Annu Rev Nurs Res. 1999;17:85–104. [PubMed] [Google Scholar]
- 100.Lauver DR, Ward SE, Heidrich SM, et al. Patient-centered interventions. Res Nurs Health. 2002;25:246. doi: 10.1002/nur.10044. [DOI] [PubMed] [Google Scholar]
- 101.McCormack B, McCance TV. Development of a framework for person-centered nursing. J Adv Nurs. 2006;56(5):472–479. doi: 10.1111/j.1365-2648.2006.04042.x. [DOI] [PubMed] [Google Scholar]
- 102.Gage H, Hampson S, Skinner TC, et al. Educational and psychosocial programs for adolescents with diabetes: approaches, outcomes and cost-effectiveness. Patient Educ Couns. 2004;53(3):333–346. doi: 10.1016/j.pec.2003.06.003. [DOI] [PubMed] [Google Scholar]
- 103.Sobel DS. The Cost-effectiveness of Mind-Body Medicine Interventions. JAMA. 2000;284:1705. [PubMed] [Google Scholar]
- 104.Ryan P, Pumilia NJ, Henak B, Chang T. Evaluating performance usability of a tailored intervention. Comput Inform Nurs. doi: 10.1097/NCN.0b013e3181b21779. In press. [DOI] [PubMed] [Google Scholar]
- 105.Blanz K, Lewis FM, Rimer BK, editors. Health Behavior and Education: Theory, Research and Practice. 2nd ed. Jossey-Bass; San Francisco, CA: 1985. [Google Scholar]
- 106.Institute of Medicine: Committee on Communication for Behavior Change in the 21st Century . Speaking of Health: Assessing Health Communication Strategies for Diverse Populations. The National Academies Press; Washington, DC: 2002. [PubMed] [Google Scholar]
- 107.Lorig KR. Self-management education: more than a nice extra. Med Care. 2003;41(6):699–701. doi: 10.1097/01.MLR.0000072811.54551.38. [DOI] [PubMed] [Google Scholar]
- 108.Lorig KR. Taking patient ed to the next level. RN. 2003;66(12):35–38. [PubMed] [Google Scholar]
- 109.Lorig KR, Mazonson PH, Holman HR. Evidence suggesting that health education for self-management in patients with chronic arthritis has sustained health benefits while reducing health costs. Arthritis Rheum. 1992;36(4):439–446. doi: 10.1002/art.1780360403. [DOI] [PubMed] [Google Scholar]
- 110.Paasche-Orlow MK, Wolf M. The causal pathways linking health literacy to health outcomes. Am J Health Behav. 2007;31(S1):S19–S26. doi: 10.5555/ajhb.2007.31.supp.S19. [DOI] [PubMed] [Google Scholar]
- 111.Parcel GS, Bartlett EE, Bruhn JG. The role of health education in self-management. In: Holroyd KA, Creer TL, editors. Self-management of Chronic Disease: Handbook of Clinical Interventions and Research. Academic Press; Orlando, FL: 1986. pp. 3–27. [Google Scholar]
- 112.The Centers for the Advancement of Health [March 2008];Essential elements of self-management interventions. http://www.cfah.org/.
- 113.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288(14):1775–1779. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- 114.Lorig K, Ritter P, Gonzalez VM. Hispanic chronic disease self-management: a randomized community-based outcome trial. Nurs Res. 2003;52(6):361–369. doi: 10.1097/00006199-200311000-00003. [DOI] [PubMed] [Google Scholar]
- 115.Lorig KR, Sobel DS, Stewart AL, et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Med Care. 1999;37(1):5–14. doi: 10.1097/00005650-199901000-00003. [DOI] [PubMed] [Google Scholar]
- 116.Lorig KR, Ritter PL, Laurent DD, Fries JF. Long-term randomized controlled trials of tailored-print and small-group arthritis self-management interventions. Med Care. 2004;42(4):346–354. doi: 10.1097/01.mlr.0000118709.74348.65. [DOI] [PubMed] [Google Scholar]
- 117.US Department of Health and Human Services Centers for Medicare and Medicaid Services [July 2007];Evidence report and evidence based recommendations: chronic disease self management for diabetes, osteoarthritis, post-myocardial infarction care, and hypertension. http://www.cms.hhs.gov/PrevntionGenInfo/Downloads/CDSM%20Report.pdf.
- 118.Weiss M. Weight management in post-partum women: Reigner Award. Marquette University College of Nursing; Milwaukee, WI: 2005. [Google Scholar]
- 119.Cummings S, Cosman F, Jamal SA, Charney P. Osteoporosis: An Evidence-Based Guide to Prevention and Management. American College of Physicians; Philadelphia, PA: 2002. [Google Scholar]
- 120.Field-Munves E, Gueldner SH, Burke MS, Smiciklas-Wright H. Osteoporosis: Patient Identification and Evaluation. Preventing and Managing Osteoporosis. Springer; New York, NY: 2000. p. 63. [Google Scholar]
- 121.Anonymous Osteoporosis: review of the evidence for prevention, diagnosis and treatment and cost-effectiveness analysis. Osteoporos Int. 1998;8(suppl 4):S7–S80. [PubMed] [Google Scholar]
- 122.National Institutes of Health . NIH Consensus Statement: Osteoporosis Prevention, Diagnosis, and Therapy. NIH; Kensington, MD: 2000. [PubMed] [Google Scholar]
- 123.National Osteoporosis Foundation . Physician's Guide to Prevention and Treatment of Osteoporosis. National Osteoporosis Foundation; Washington, DC: 1998. [Google Scholar]
- 124.Ryan P, Lauver DR. The efficacy of tailored interventions. J Nurs Scholarsh. 2002;34(4):331–337. doi: 10.1111/j.1547-5069.2002.00331.x. [DOI] [PubMed] [Google Scholar]
- 125.Lutz KF, Dupree JK, Kendall J. Expanding the praxis debate: contribution to clinical inquiry. Adv Nurs Sci. 1997;20(2):21–31. doi: 10.1097/00012272-199712000-00004. [DOI] [PubMed] [Google Scholar]
- 126.Morse JM. Toward a praxis theory of suffering. Adv Nurs Sci. 2001;24(1):47–59. doi: 10.1097/00012272-200109000-00007. [DOI] [PubMed] [Google Scholar]
- 127.Seng JS. Praxis as a conceptual framework for participatory research in nursing. Adv Nurs Sci. 1998;20(4):37–48. doi: 10.1097/00012272-199806000-00005. [DOI] [PubMed] [Google Scholar]
- 128.Schwartz-Barcott D, Patterson BJ, Lusardi P, Farmer BC. From practice to theory: tightening the link via three fieldwork strategies. J Adv Nurs. 2002;39(3):281–289. doi: 10.1046/j.1365-2648.2000.02275.x. [DOI] [PubMed] [Google Scholar]
- 129.Im EO, Meleis AI. Situation-specific theories: philosophical roots, properties, and approach. Adv Nurs Sci. 1999;22(2):11–24. doi: 10.1097/00012272-199912000-00003. [DOI] [PubMed] [Google Scholar]
- 130.Ryan P, Sawin KJ. The individual and family self-management theory: background and perspectives on context, process and outcomes. Nurs Outlook. doi: 10.1016/j.outlook.2008.10.004. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]