Abstract
Introduction
Malaria is re-emerging in most of the African highlands exposing the non immune population to deadly epidemics. A better understanding of the factors impacting transmission in the highlands is crucial to improve well targeted malaria control strategies.
Methods and Findings
A conceptual model of potential malaria risk factors in the highlands was built based on the available literature. Furthermore, the relative importance of these factors on malaria can be estimated through “classification and regression trees”, an unexploited statistical method in the malaria field. This CART method was used to analyse the malaria risk factors in the Burundi highlands. The results showed that Anopheles density was the best predictor for high malaria prevalence. Then lower rainfall, no vector control, higher minimum temperature and houses near breeding sites were associated by order of importance to higher Anopheles density.
Conclusions
In Burundi highlands monitoring Anopheles densities when rainfall is low may be able to predict epidemics. The conceptual model combined with the CART analysis is a decision support tool that could provide an important contribution toward the prevention and control of malaria by identifying major risk factors.
Introduction
In recent decades, highland malaria has been a re-emerging problem in several African countries (Ethiopia, Uganda, Kenya, Tanzania, Rwanda, Burundi and Madagascar) [1], [2]. The spread of the vectors distribution in time and space exposes the human populations to a longer transmission season, resulting in a higher endemicity in the highlands [2], [3]. Besides, deadly epidemics have been reported with higher frequency and amplitude than before [4]–[8]. Indeed, one fifth of the African population lives in malaria epidemic prone areas (desert fringes and highlands) [9] where all age groups are at risk of clinical malaria due to the limited acquired immunity. The prevention of malaria in these vulnerable populations is one of the priorities for African leaders and international agencies [10]. It is therefore, essential to understand the factors fuelling these changes in transmission so that a national strategy plan for epidemic prevention and control can be developed in highland regions.
Former reviews published in 1998, have already shown the complexity of factors influencing malaria in the highlands [1], [2]. The aim of the present paper is to summarise and update current knowledge on malaria in the African highlands and build a detailed conceptual model for malaria risk factors. Furthermore, the hierarchical importance of these factors in influencing highland malaria is analysed using classification and regression trees [11], [12] (CART). The CART method is useful when dealing with large numbers of explanatory variables and to explore the relationship and the relative importance of these variables as well as all their possible interactions [13]. Therefore, the conceptual model associated with a CART analysis may be used as a decision support tool and different strategies could be implemented according to the risk factors that emerge as the strongest.
The CART method has been applied to the case of Burundi [14], [15] and measures to control and/or prevent malaria epidemics are discussed.
Methods
Conceptual Model of Malaria Risks Based on Literature Review
Based on a literature review, different risk factors for malaria in African highlands were identified and used to build a conceptual model. The main source of information was peer-reviewed scientific papers obtained through PubMed using the keywords “malaria” and “highland”. Both English and French papers, describing malaria potential risk factors, were used. The reported risk factors were classified according to their impact on vectors or on malaria. To determine the hierarchical importance of different risk factors identified in the conceptual model the Classification and Regression Trees (CART) were used on malaria data collected in the Burundi highlands.
The Burundi Database
A four year vector control programme based on one annual round of Indoor Residual Spraying (IRS) was carried out between 2002 and 2005 in the central highland province of Karuzi, and targeted the valleys where malaria transmission was the highest [14]. Long Lasting Insecticidal Nets were also distributed in 2002. Between 2002 to 2007, bi-annual (May and in November) cross sectional surveys (11 surveys in total) were carried out. The sampling process has been described in detail elsewhere [14], [15]. Briefly, during each survey 450 to 800 houses were sampled and in each of them (total houses sampled for the 11 surveys = 8075), Anopheles were collected with the spray catch method and a blood slide of two randomly selected persons (≤9 and >9 years old) were taken (total person included in the 11 surveys = 12745, 36% of the houses have no children ≤9 and in 6% of the houses one of the selected person was not present). Of the 14,932 An.gambiae and An.funestus that were collected, 244 were found positive for the detection by ELISA of the P.falciparum circumsporozoite antigen (Wirtz). The intervention was evaluated on the basis of the reduction of the Anopheles density, infective bites by house by month and the prevalence of malaria infection. Information on location, housing construction (house size, open eaves, type of wall and roof), livestock, separate kitchen, vector control activities (net use and spraying), prior antimalarial treatment, sex and age was also collected. Altitude and distance to the marsh of the houses were registered with a hand held positioning system (GPS 76, Garmin®). Average monthly minimum and maximum temperatures and monthly rainfall, recorded at the Karuzi meteorological station, were obtained from the Institute of Geography of Burundi (IGEBU).
A verbal informed consent was obtained for the blood slides and mosquito collections. For children the consent was obtained from the parents. In case of refusal, other persons or the next household was asked for consent. Present procedure and the full study was approved by the Commission of Medical Ethics of the Prince Leopold Institute of Tropical Medicine Antwerp (Belgium) (ref number 04 26 4 461). At the time of the implementation of the study, the Institutional Ethical Committee was not functional in Burundi. However, the Ministry of Health signed an agreement for the vector control program and the study design and the national malaria control program (LMTC) offered close collaboration.
The Classification and Regression Trees CART
The non-parametric classification and regression tree (CART) models were used to explore the influence of the specified determinants on the level of malaria and on the Anopheles mosquitoes. CART models are useful tools to explore the interactions between a desired outcome and its determinants [13], [16]. They can be used to analyse either categorical (classification) or continuous data (regression). The analysis was performed using a commercial software CART (Salford systems Inc. Version 6, California, USA).
CART expresses its result in the form of a decision tree, a different approach that the better known parametric techniques. Indeed, in classical regressions the linear combinations are the primary method of expressing the relationships between variables while in CART this does not need to be linear or additive and the possible interactions do not need to be pre-specified or of a particular multiplicative form. The decision tree resulting of CART is useful, as well as the resulting flexibility and the non-parametric form (no assumption upon the covariates). The CART has many advantages, but they are known as instable approach. Therefore in the present paper we used a 10-fold cross-validation as estimation method.
The building of a classification tree begins with a root (parent) node, containing the entire set of observations, and then through a process of yes/no questions, generates descendant nodes. Beginning with the first node, CART finds the best possible variable to split the node into two child nodes. In order to identify the best splitting variable (called splitters), the software checks all possible variables, as well as all possible values of the variable to be used to split the node. In choosing the best splitter, the program seeks to maximize the average “purity” of the two child nodes. The splitting is repeated along the child nodes until a terminal node is reached. Each terminal node is characterized by an average and a standard error (computed as the standard deviation divided by the square root of the terminal node size), indicating the purity of the node. The node purity measure provides an indication of the relative homogeneity (the inverse of impurity) of cases in the terminal nodes. If all cases in each terminal node show identical values, then node impurity is minimal, homogeneity is maximal, and prediction is perfect (at least for the cases used in the computations). In this study, the Gini criterium and the interclass variance were used as a measure of “purity”.
The one standard error rule was applied to select the best tree (the smallest tree within 1 standard error of the minimum error tree). A minimum terminal node size of 500 samples was selected to avoid too many splits, with few observations, that are difficult to explain.
CART also provides a ranking based on the overall contribution of each variable in the construction of the tree. This ranking indicates the importance of each independent variable as a predictor. Importance, for a particular variable, is the sum across all nodes in the tree of the improvement scores between this variable and the best splitter at a particular node [17]. It is thus possible that a variable enters the tree as a second most important splitter in many nodes (and will not appear on the tree), but never as the primary splitter. However, such variable will turn out as very important in the overall variable ranking. The advantage of such an approach is that important contributing determinants are not ignored.
Multivariate Analysis
The risk of a positive slide was analyzed using the survey logistic regression in Stata 9.2 (Stata Corporation, College station, Texas, USA), taking into account the study design. Negative binomial regressions were used for the analysis of Anopheles density.
Results
Conceptual Model for Malaria Risk in the Highlands
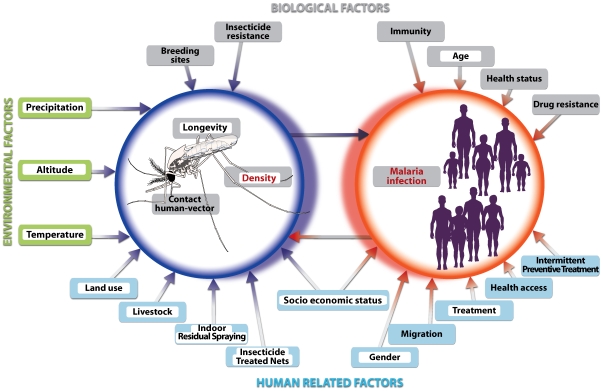
Due to the instability of transmission in the highlands small variations in environmental or human related factors can have dramatic consequences for malaria transmission due to the low immune status of the human population [2], [18]. Different factors can drive these changes by influencing the vector's transmission capacity and the malaria prevalence. These factors can be grouped into three classes: (1) environmental factors such as altitude and climate (2) biological factors related to the Anopheles vector, the parasite and the human host and (3) human related factors such as socio-economic status, health access, migration, gender, control activities (IRS, Insecticide Treated Net, and Intermittent Preventive Treatment) and land use (irrigation, deforestation, swamp drainage and living near breeding sites). The conceptual model of potential factors influencing either Anopheles (density, longevity or/and contact with human) or the outcome of transmission (i.e. malaria infection) in the highland based on this review is presented in Figure 1.
Figure 1. Conceptual model of important risk factors affecting malaria prevalence in the African Highlands.
Factors are regrouped in 3 main classes (environmental factors: green label, biological factors: grey label and human related factors: blue label). Dependant variables included in the CART analysis are displayed in red and predictor variables are highlighted in white.
Factors Influencing Malaria
The ability to suppress malaria infection depends on immunity. It has been suggested by Bodker et al [18] that acquired immunity is both exposure and age-dependent. At a moderate level of transmission (0.1 to 2 infective bites per year), immunity will develop with increasing transmission but after a certain age (2–3 years) the immunity will increase independently of transmission intensity. In low transmission areas, however, prevalence of infection and clinical malaria is similar in all age group.
The health status of the population can have an important impact on malaria infection. Malnutrition can weaken children's immunity and can increase the level of malaria morbidity and mortality [19], [20]. HIV has been associated with an increased level of malaria transmission in South Africa [21] and might enhance malaria parasite biomass [22]. It has also been observed that in all endemic areas the frequency of malaria infection is greater in pregnant women than in non pregnant women. However in low or unstable transmission areas, as in the African highlands, the effect of parity is less pronounced or even absent as compared to high transmission areas [23], [24]. Conversely, the implementation of intermittent preventive treatment is able to reduce morbidity in pregnant women [25] and in infants [26].
In several countries, the resurgence of malaria has been largely attributed to the emergence and spread of drug-resistant parasites [27]–[31]. The progressive build-up of the gametocyte pool in the human reservoir, contributing to the speed-up of transmission, could be enhanced by treatment failure of sulphadoxine-pyrimethamine [32] and chloroquine [33]. In contrast, implementation of effective treatment, such as artemisin-based combination therapy, has improved cure rates, decreased the gametocyte carriage and, therefore, resulted in a reduced transmission in low endemic areas [34], [35].
Finally, other human related factors, such as population migrations [36], reduced health systems access and quality [2], and socio-economic pressure as population growth [37], [38] have also created favourable conditions for malaria outbreaks.
Factors Influencing the Vector
Mosquitos' longevity, man-vector contact and mosquito density determine the transmission capacity of a vector population. First, a reduction in the lifespan of the mosquitoes will reduce the sporozoite rate and hence the proportion of infective bites. Secondly, a reduction in the human/vector contact will decrease the proportion of blood meals taken on human hosts. Finally, a reduction of vector density by decreasing the number of adult or larvae will also reduce transmission intensity. Therefore, any factors that could have an impact on any of these components will influence malaria transmission. According to the MacDonald model [39], factors influencing longevity will have more impact on transmission than factors affecting human-vector contact or density.
An altitude around 1800–2000 meters is usually considered the upper limit at which malaria transmission occurs [2], though epidemics have been recorded higher [19], [40]. The protective effect of altitude is linked to the decreasing temperature (0.5°C to 0.7°C every 100 meters) [41], [42] that increase the length of the extrinsic incubation period and hence decrease the likelihood of a mosquito of becoming infectious. Optimum conditions for the extrinsic development of the parasite are between 25°C and 30°C [41]. Below 16–19°C, few vectors survive before the completion of the sporogonic cycle and this temperature range is often considered as the threshold for stable malaria transmission. Temperature will also influence the longevity and feeding frequency of a mosquito [41]. The aquatic stage of anopheline is also temperature-dependant. In the laboratory, it was observed that larval mortality increased considerably when water temperature fell below 18°C [43]. In the Kenyan highlands only a small larval survival rate was observed at low temperatures [44], while the adult mosquitoes could survive inside houses with temperatures 2 to 3 degrees higher [40], [45]. Therefore, a small temperature rise either through seasonal variability [46], local microclimatic changes due to modification in vegetation cover [47]–[49] or to global warming [50]–[52] can increase malaria transmission and distribution.
Rainfalls play a crucial role in malaria epidemiology by providing breeding sites for the aquatic stages of the mosquito's life cycle. In addition, rainfalls may increase the relative humidity; above 60%, adult mosquitoes longevity, and consequently the vectorial capacity, increases [41]. By contrast, heavy rain showers can flush away and kill larvae [53]. In Ethiopia [19] and Uganda [5], [54], for example, extreme rainfalls were associated with malaria epidemics, whereas in Tanzania malaria decreased after intense rains [55].
In highland settings, malaria transmission is negatively correlated with the increasing breeding sites-house distance [14], [56], [57]. The topography of highland areas affects the spatial distribution of breeding sites [58] and land use changes such as irrigation [59]–[61] and swamp drainage for cultivation [49], [62], [63], or for other economic activities [64] can create new habitats for malaria vectors such as Anopheles gambiae and Anopheles funestus. Environmental management, on the other hand, can reduce the availability of the breeding sites and therefore decrease the vectors density population [65]–[67]. Vector control measure such as Indoor Residual Spraying (IRS) and Insecticide Treated Net (ITN) have a high impact on transmission by reducing both Anopheles survival and density, if the coverage is high [14], [68]. ITN can also decrease the man-vector contact and reduced the human blood feeding success [69], [70]. However, the emergence of insecticide resistance may decrease the effectiveness of these methods [71], [72].
Household and socio-economic factors have also an impact on malaria transmission by influencing the human-vector contact. For example, more mosquitoes were found in poorly constructed houses as compared to good ones [73], [74]. Other factors such as keeping livestock inside the house, type of roof, open eaves, no separate kitchen were also associated with increase malaria risk [74], [75].
Identifying and Ranking Malaria Risk Factors in Burundi Highlands
Based on the conceptual model (Figure 1), variables among the three classes (environmental, biological and human related) were chosen from the Burundi database and used in the CART analysis to determine their impact either on the malaria infection or on Anopheles prevalence. Predictive factors for malaria infection included in the CART analysis were Anopheles density, density of infected Anopheles, individual human characteristics (age and sex), housing condition, past treatment, and “survey” (Table 1). The variable “survey” was included in the prevalence model and represents the possible time-related variables not covered by the parameters included in the vector density and prevalence analyses. To study the impact on Anopheles, two regression trees were developed, one with as a dependant variable the Anopheles density and the other with as a dependant variable the density Anopheles infected with Plasmodium falciparum. The factors included were monthly rainfall and average monthly minimum and maximum temperatures (during the month of the survey and 1–2 months before the survey), housing conditions, vector control activities, and environmental parameters. Detailed information of the houses was available on the Burundi database. The characteristics of these houses were scored by size and type of construction: house size (floor area size score 1 = <25 m2, score 2 = 25–50 m2, score 3 = >50 m2), type of wall (1 = thatch, 2 = mud, and 3 = bricks), type of roof (1 = thatch, 2 = iron sheet, and 3 = tiles) and separate kitchen (1 = no, 2 = yes). The score of the houses' characteristics were combined and divided into four categories (score 4–5 = 1: poorest housing condition, score 6–7 = 2, score 8–9 = 3, score 10–11 = 4: best housing condition). Other factors presented in the conceptual model were not collected in our study and could not be included in the analysis.
Table 1. Dependant and predictor variables introduced in the CART analysis.
| Dependant Variable | Variables classes | Predictor Variables |
| Anopheles density | Environmental | |
| ○ Precipitation | Current monthly rainfall (mm) | |
| Lagged monthly rainfall: one month (mm) | ||
| Lagged monthly rainfall: two months (mm) | ||
| ○ Temperature | Lagged average monthly minimum T°: one month (°C) | |
| Lagged average monthly minimum T°: two months (°C) | ||
| Lagged average monthly maximum T°: one month (°C) | ||
| Lagged average monthly maximum T°: two months (°C) | ||
| ○ Altitude | Altitude houses (m) | |
| • ≤1450 | ||
| • 1451–1500 | ||
| • 1501–1550 | ||
| • 1551–1600 | ||
| • 1601–1650 | ||
| • >1650 | ||
| Human | ||
| ○ Land use | Distance to marsh (m) | |
| • ≤300 | ||
| • 301–500 | ||
| • 501–700 | ||
| • 701–900 | ||
| • 901–1100 | ||
| • >1100 | ||
| Type of crop in the marsh | ||
| • Two crops/year: rice and vegetable | ||
| • Rice field | ||
| • Vegetable | ||
| • Few crop | ||
| ○ Housing | Houses: Poor constructions to better (4 categories) | |
| ○ Livestock | Keep livestock in the houses (yes/no) | |
| ○ IRS | Houses in sprayed areas (yes/no) | |
| ○ ITN | Use of insecticide treated nets (yes/no) | |
| Positive slide | Biological | |
| Age (year) | ||
| Sex | ||
| Anopheles density (number/houses) | ||
| Density of infected Anopheles (number/houses) | ||
| Human | ||
| Past treatment during the 3 previous months (yes/no) | ||
| Keep livestock in the houses (yes/no) | ||
| Sleep under a net (yes/no) | ||
| Houses: Poor constructions to better (4 categories) | ||
| Other | ||
| Survey |
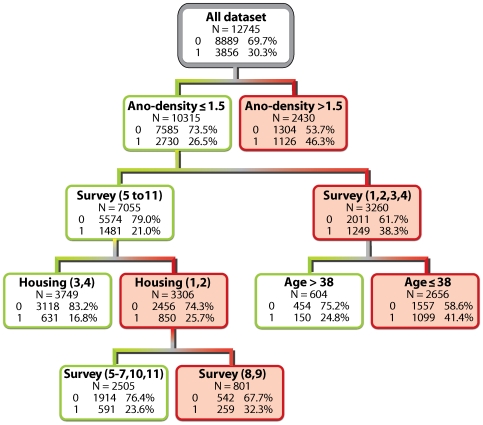
The overall ranking of predictor variables for malaria infection is presented in Table 2. Surveys and Anopheles density were the two most important factors. Housing conditions that influence the human-vector contact and infective mosquitoes were ranked third and sixth. In the corresponding classification tree, Anopheles density was the first splitter (Figure 2) with a higher prevalence (46.3%) in houses with more than 1.5 Anopheles compared to houses with fewer Anopheles (prevalence: 26.5%). Then, in this last group, malaria prevalence was lower in surveys 5 to 11 (year 2004 to 2007) compared to surveys 1 to 4 (year 2002 to 2003). For surveys 1 to 4, age was the best discriminator with a threshold at 38 years; for survey 5 to 11, malaria prevalence among people living in the poorest houses was higher (25.7%) than for people living in the better-constructed ones (16.8%). Each terminal node is categorised as 1 (positive) or 0 (negative) depending on whether the proportion of 1's exceeds the proportion of 1's in the population (30.3%). From all negative individuals, 62% (5486/8889) were properly classified as negative (0) and from all positive individuals, 64% (2484/3856) were properly classified as positive.
Table 2. Ranking of predictor variables for malaria prevalence by their overall power as discriminant.
| Variables | Power |
| Survey | 100 |
| Anopheles density | 91.0 |
| Housing | 23.4 |
| Age | 22.8 |
| Past malaria treatment | 5.8 |
| Density of infected Anopheles | 1.0 |
| Livestock in houses | 0.9 |
| Sleep under a net | 0.0 |
| Sex | 0.0 |
Figure 2. Classification trees representing the important risk factors for malaria prevalence.
The high risk groups are displayed in red. In each node 0 stands for negative slide and 1 for positive slide. The following variables were selected by the tree as important risk factors: Anopheles density (Ano-density) with a cut off of 1.5 Anopheles per house; Survey number 1 to 11; Housing (1,2 = poorest housing condition and 3,4 highest housing condition); Age with a cut off of 38 years old.
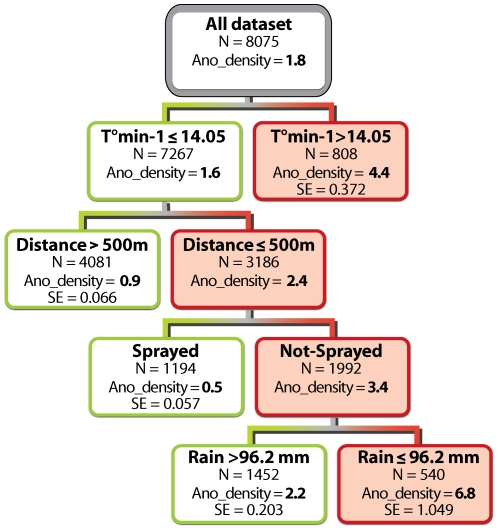
As the Anopheles density was more important than density of infected Anopheles for the malaria prevalence (Table 3), only the regression trees with the dependent variable Anopheles density is presented. According to their overall discriminatory power, monthly rainfalls in the current month and with one month time lag, emerged as the two strongest predictors for Anopheles density, followed in decreasing order of importance by spraying, net-use, monthly minimum temperature with one and two months time lag, distance to the marsh, altitude of houses, and two months lagged rainfall (Table 3). The resulting regression tree is presented in Figure 3. Every important predictor divides a node into two sub-nodes, either with a higher or a lower Anopheles density. A one month lag minimum temperature was the main splitter, with temperature below 14.05°C being associated with the lowest Anopheles density (mean: 1.6/house). This sub-node was further split by the variable “distance to the marshes”. The highest Anopheles density (2.4/house) was found in houses located within 500 metres from the marsh. Spraying was then the best discriminative variable for this node, Anopheles density being the highest (3.4/house) when houses were not in treated areas. In this group, current rainfall had an influence over the average Anopheles density. Monthly rainfalls higher than 96.2 mm were associated with lower Anopheles density (2.2/house). Monthly rainfalls in the preceding month (power: 99.9), net use (power: 83.1) and a lag minimum temperature of two months (power: 73.0) did not appeared as main splitters in the final tree whereas they were identified as important risk factors for Anopheles density as shown by the ranking of their discriminatory power (Table 3). This happens because at many stages in the tree building they are important but never as important as the main splitter.
Table 3. Ranking of predictor variables for Anopheles density by their overall power as discriminant.
| Variables | Power |
| Rain | 100 |
| Rain - 1 month | 99.9 |
| Spraying | 96.7 |
| ITN use | 83.1 |
| T°min - 1 month | 75.7 |
| T°min - 2 months | 73.0 |
| Distance from the marsh | 42.3 |
| Altitude of the houses | 31.9 |
| Rain - 2 months | 22.4 |
| Type of crop | 9.3 |
| T°max - 1 month | 5.7 |
| T°max - 2 months | 5.1 |
| Housing | 0.0 |
| Livestock in houses | 0.0 |
Figure 3. Regression trees representing the important risk factors for the Anopheles density per/house (Ano_density).
The selected splitting variables (Minimum temperature the previous month = T°min-1; Distance of the houses to the marsh with a cut off of 500 metres; Area sprayed or not; Monthly rainfall in the current month with a cut off of 96.2 mm) are shown in the nodes.
The logistic regression, showed the surveys, density of Anopheles, type of house, age and density of infected Anopheles to be significant (results not shown). In the negative binomial regression the following variables were retained in the model: rain with one and two months time lag, spraying, net used, minimum temperature the previous month, distance to the marsh, altitude and presence of animals in the house.
Discussion
The conceptual model used in this study provides insight into a complex disease, malaria, by listing all the potential risk factors influencing the transmission capacity of the vectors and the malaria prevalence in the human population. Such complexity requires tools that enable to explore the hierarchical importance of these risk factors. CART is such a tool and has proven its adequacy and usefulness in other contexts, for example for bovine spongiform encephalopathy [76]. In the Malaria field, CART methods (or similar approaches) were used for spatial analysis of malaria risk [77] and has been also used recently to report the accurate and dynamic picture of the main risk factors for malaria infection in Vietnam [12].CART has also the advantage to be user and reader friendly, generating results comprehensible for a wider audience. Therefore, the conceptual model-CART approach will lead to a better understanding of the local malaria epidemiology and a better targeting of control efforts.
Variables of high importance in both CART and parametric analysis are almost the same, except for rain which is non significant in the logistic regression. This can probably be explained by high colinearity with other rain variables (with time lag of one and two months). A CART Analysis works with (non-predefined) interactions. This means that the only similarity between a parametric model and a CART model will be the first split. The variable “animals” was ranked last in CART, probably because it is important only at the first step in the CART tree (in analogy with a parametric model) but will only contribute a small part to the final importance which is obtained by adding contributions at different splits in the tree.
In the Burundi highlands, Anopheles density, hence vector density because 95% of the collected Anopheles mosquitoes in the study area were malaria vectors [14], was the second best predictor for malaria infection in the human population. The infective mosquitoes were only the sixth most important predictor variable in the overall ranking. Likewise, Bodker et al [78] found that a decline in malaria transmission due to altitude is primarily due to a diminution of vector abundance and, to a lesser extent, by a reduction in the proportion of infective mosquitoes. In other studies, such as in Kenya and Madagascar, the importance of vector density in unstable highland malaria has been highlighted [60]. Indeed, in these countries the introduction of irrigated rice fields increased the number of breeding sites available and exposed the non-immune population to higher transmission. Nevertheless, in endemic areas this is not always the case, as sometimes very high vector densities may result in a low vectorial capacity [79].
In the current study, important variations in prevalence between surveys were observed and cannot be explained by any of the factors included in this analysis. Some variables such as health access, health status, and migration were not collected during the surveys. Differences between the first four surveys (year 2002 and 2003) and the later ones could be attributed to the normal decline of malaria prevalence after the malaria epidemic of 2001 [80], or/and to the introduction of the artemisin-based combination therapy and Rapid diagnostic tests in December 2003. Mosquitoes and blood samples were collected at the same time. However, when considering the time needed for the parasite to develop in the vector and the human host, postponing the parasitological surveys by about one month could have improved the predicting power of Anopheles density on malaria prevalence. It is surprising that ITN-use was not associated with lower malaria prevalence while it affects the Anopheles density, a good predictor of malaria infection. This finding can be explained by the absence of any additional impact of ITNs on transmission once an almost full coverage of IRS has been achieved [14].
In the highlands of Burundi, the CART analysis shows that factors responsible for high Anopheles density are in agreement with other studies, i.e. lower rainfall [55]–[57], no vector control implementation in houses [75], higher minimum temperatures [46], [81], and breeding sites proximity [56], [57]. In Karuzi, high rainfalls, current or during the previous month, have a negative effect on vector densities. Minimum temperatures with 1 or 2 months time-lag are good predictors of vector density, while housing conditions and livestock in houses have no predictive value. This is most likely due to the predominance of the very anthropophilic vector An. gambiae s.s. (Form S) [82] in the study area (98.2% of the complex) [14]. In the presence of An. arabiensis, however, it has been observed that keeping cattle in houses was a risk factor for malaria [74], [83]. It is also obvious that vector control (ITN or IRS) using pyrethroids insecticides reduces vector density in treated houses due to either the excito-repellent effect of this class of insecticides or by their mass killing effect. Monthly cumulated temperature and rainfall data have been used in this work to assess the importance of environmental factors. However to improve the predictive value, weekly data in different locations would me more appropriate especially in the highland where environmental factors can vary greatly between valleys and where precipitations are non homogenous through the month.
Climate (temperature and rainfall) is an important determinant of malaria vectors in the highlands. An increase in temperature and a modification in the frequency or amount of rainfall would affect future transmission of malaria. Different biological and statistical models have assessed the potential geographical expansion of malaria ranging from small change in the next decades [84], [85] to substantial extension by the end of the century [86], [87]. However, the models mostly focused on the effect of temperature on parasites development and vectors' longevity and should now evaluate the impact of climate warming on Anopheles density. The attribution of malaria resurgence observed in recent decades in African highlands to climate change is, however, controversial. Whereas some studies have associated warming trends to the increase in malaria transmission [50], [52], [88], other studies show no association [8], [89]–[91]. In Burundi, Bonora et al [92] attribute the upsurge of malaria infection in the highlands, leading to the 2000 epidemic, to climate warming. However, in Karuzi, temperatures were recorded since 1988 and no warming trend in monthly mean, maximum and minimum temperature was observed until the 2000 epidemic [93]. An unusually high precipitation occurred at the time of the malaria peak (November) and could not be responsible for triggering the epidemic, but was probably responsible for stopping or decreasing malaria transmission [53]. For instance, it is commonly known that high rainfalls trigger malaria epidemic whereas in our analysis lower precipitations were associated with high Anopheles density, a powerful predictor of malaria infection. The long dry season preceding the epidemic of 2000 [80] may thus partially explain the outbreak.
Monitoring the most important malaria risk factors will help to more adequately prevent and control increases in malaria. The forecasting or early detection of meteorological variability could give time for the implementation of control measures. For example, in the Burundi, a more careful monitoring of the impact of rainfall and temperature variability on Anopheles density should be further evaluated and a threshold risk set up in different areas. If such rainfall variability could be assessed a few weeks in advance, the follow up of the residual Anopheles densities when rainfall is low could help in predicting or early detecting epidemics [94]. However, the practical use of these data for early warning and especially the initiation of expansive control interventions based on it, need to be assessed especially in the highlands [95].
It is commonly known that decrease in mosquito longevity will be more effective to limit transmission than reducing mosquito density [39]. Therefore, environmental management aiming at larval source reduction will contribute little to the overall decrease of malaria burden [96]. However, this activity may be re-considered when Anopheles density is the most important factor determining malaria infections; any means aiming at reducing the Anopheles population will have an impact on malaria. In the past, successful malaria prevention programmes targeting larval habitats were implemented [97], [98] even in Africa [66]. During the last few years renewed consideration has been given to environmental management [99] with a recent successful implementation reported in the highlands of Ethiopia [67]. To be fully effective, such a method necessitates substantial information on vector ecology, distribution of breeding sites and local environmental conditions and should be combined with insecticidal adult vector control [100]. Indeed, in our model, IRS and ITN are strongly related to Anopheles density.
In conclusion, the conceptual model of highland risk factors in combination with a CART analysis can be considered as a simple decision support tool to better understand malaria epidemiology in various high altitude settings. The ranking of risk factors will help to prioritize monitoring, prevention and control efforts to the most important identified factors.
Acknowledgments
The authors thank the Burundian Health authorities for their support and particularly the staff of the malaria national control program. We would like also to thank the provincial administration of Karuzi for their strong collaboration.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This work was funded by MSF-Belgium and the Belgian co-operation. MSF Belgium has a role in the study design, data collection and analysis, decision to publish and preparation of the manuscript. The Belgian cooperation has no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Mouchet J, Manguin S, Sircoulon J, Laventure S, Faye O, et al. Evolution of malaria in Africa for the past 40 years: impact of climatic and human factors. J Am Mosq Control Assoc. 1998;14:121–130. [PubMed] [Google Scholar]
- 2.Lindsay SW, Martens WJ. Malaria in the African highlands: past, present and future. Bull World Health Organ. 1998;76:33–45. [PMC free article] [PubMed] [Google Scholar]
- 3.Hay SI, Noor AM, Simba M, Busolo M, Guyatt HL, et al. Clinical epidemiology of malaria in the highlands of western Kenya. Emerg Infect Dis. 2002;8:543–548. doi: 10.3201/eid0806.010309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Malakooti MA, Biomndo K, Shanks GD. Reemergence of epidemic malaria in the highlands of western Kenya. Emerg Infect Dis. 1998;4:671–676. doi: 10.3201/eid0404.980422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lindblade KA, Walker ED, Onapa AW, Katungu J, Wilson ML. Highland malaria in Uganda: prospective analysis of an epidemic associated with El Nino. Trans R Soc Trop Med Hyg. 1999;93:480–487. doi: 10.1016/s0035-9203(99)90344-9. [DOI] [PubMed] [Google Scholar]
- 6.Mouchet J, Laventure S, Blanchy S, Fioramonti R, Rakotonjanabelo A, et al. La reconquête des hautes terres de Madagascar par le paludisme. Bull Soc Pathol Exot. 1997;90:162–168. [PubMed] [Google Scholar]
- 7.Negash K, Kebede A, Medhin A, Argaw D, Babaniyi O, et al. Malaria epidemics in the highlands of Ethiopia. East Afr Med J. 2005;82:186–192. doi: 10.4314/eamj.v82i4.9279. [DOI] [PubMed] [Google Scholar]
- 8.Zhou G, Minakawa N, Githeko AK, Yan G. Association between climate variability and malaria epidemics in the East African highlands. Proc Natl Acad Sci U S A. 2004;101:2375–2380. doi: 10.1073/pnas.0308714100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO. The Africa malaria report 2006. 2006.
- 10.WHO. The African summit on Roll Back Malaria. 2000. WHO/CDS/RBM/2000.17:
- 11.Held TK, Weinke T, Mansmann U, Trautmann M, Pohle HD. Malaria prophylaxis: identifying risk groups for non-compliance. Q J Med. 1994;87:17–22. [PubMed] [Google Scholar]
- 12.Thang ND, Erhart A, Speybroeck N, Hung lX, Thuan lK, et al. Malaria in central Vietnam: analysis of risk factors by multivariate analysis and classification tree models. Malar J. 2008;7:28. doi: 10.1186/1475-2875-7-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Speybroeck N, Berkvens D, Mfoukou-Ntsakala A, Aerts M, Hens N, et al. Classification trees versus multinomial models in the analysis of urban farming systems in Central Africa. Agric Syst. 2004;80:133–149. [Google Scholar]
- 14.Protopopoff N, Van Bortel W, Marcotty T, Van Herp M, Maes P, et al. Spatial targeted vector control in the highlands of Burundi and its impact on malaria transmission. Malar J. 2007;6:158. doi: 10.1186/1475-2875-6-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Protopopoff N, Van Bortel W, Marcotty T, Van Herp M, Maes P, et al. Spatial targeted vector control is able to reduce malaria prevalence in the highlands of Burundi. Am J Trop Med Hyg. 2008;79:12–18. [PubMed] [Google Scholar]
- 16.Breiman L, Friedman JH, Stone CJ, Olshen RA. New York: Chapman and Hall; 1993. Classification and regression trees. [Google Scholar]
- 17.McCarthy FD, Wolf H, Wu Y. The growth costs of Malaria. National Bureau of Economic Research, inc NBER working papers. 2000;7541 [Google Scholar]
- 18.Bodker R, Msangeni HA, Kisinza W, Lindsay SW. Relationship between the intensity of exposure to malaria parasites and infection in the Usambara Mountains, Tanzania. Am J Trop Med Hyg. 2006;74:716–723. [PubMed] [Google Scholar]
- 19.Fontaine RE, Najjar AE, Prince JS. The 1958 malaria epidemic in Ethiopia. Am J Trop Med Hyg. 1961;10:795–803. doi: 10.4269/ajtmh.1961.10.795. [DOI] [PubMed] [Google Scholar]
- 20.Shankar AH. Nutritional modulation of malaria morbidity and mortality. J Infect Dis. 2000;182(Suppl 1):S37–S53. doi: 10.1086/315906. [DOI] [PubMed] [Google Scholar]
- 21.Craig MH, Kleinschmidt I, Le Sueur D, Sharp BL. Exploring 30 years of malaria case data in KwaZulu-Natal, South Africa: part II. The impact of non-climatic factors. Trop Med Int Health. 2004;9:1258–1266. doi: 10.1111/j.1365-3156.2004.01341.x. [DOI] [PubMed] [Google Scholar]
- 22.Van Geertruyden JP, Menten J, Colebunders R, Korenromp E, D'Alessandro U. The impact of HIV-1 on the malaria parasite biomass in adults in sub-Saharan Africa contributes to the emergence of antimalarial drug resistance. Malar J. 2008;7:134. doi: 10.1186/1475-2875-7-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Elghazali G, Adam I, Hamad A, El Bashir MI. Plasmodium falciparum infection during pregnancy in an unstable transmission area in eastern Sudan. East Mediterr Health J. 2003;9:570–580. [PubMed] [Google Scholar]
- 24.Menendez C. Malaria during pregnancy: a priority area of malaria research and control. Parasitol Today. 1995;11:178–183. doi: 10.1016/0169-4758(95)80151-0. [DOI] [PubMed] [Google Scholar]
- 25.Van Eijk AM, Ayisi JG, Ter Kuile FO, Otieno JA, Misore AO, et al. Effectiveness of intermittent preventive treatment with sulphadoxine-pyrimethamine for control of malaria in pregnancy in western Kenya: a hospital-based study. Trop Med Int Health. 2004;9:351–360. doi: 10.1111/j.1365-3156.2004.01196.x. [DOI] [PubMed] [Google Scholar]
- 26.Massaga JJ, Kitua AY, Lemnge MM, Akida JA, Malle LN, et al. Effect of intermittent treatment with amodiaquine on anaemia and malarial fevers in infants in Tanzania: a randomised placebo-controlled trial. Lancet. 2003;361:1853–1860. doi: 10.1016/s0140-6736(03)13504-0. [DOI] [PubMed] [Google Scholar]
- 27.Bodker R, Kisinza W, Malima R, Msangeni H, Lindsay S. Resurgence of malaria in the Usambara mountains, Tanzania, an epidemic of drug-resistant parasites. Glob Change Hum Health. 2000;1:134–153. [Google Scholar]
- 28.Shanks GD, Biomndo K, Hay SI, Snow RW. Changing patterns of clinical malaria since 1965 among a tea estate population located in the Kenyan highlands. Trans R Soc Trop Med Hyg. 2000;94:253–255. doi: 10.1016/s0035-9203(00)90310-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hay SI, Rogers DJ, Randolph SE, Stern DI, Cox J, et al. Hot topic or hot air? Climate change and malaria resurgence in East African highlands. Trends Parasitol. 2002;18:530–534. doi: 10.1016/s1471-4922(02)02374-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bjorkman A, Bhattarai A. Public health impact of drug resistant Plasmodium falciparum malaria. Acta Trop. 2005;94:163–169. doi: 10.1016/j.actatropica.2005.04.015. [DOI] [PubMed] [Google Scholar]
- 31.Trape JF. The public health impact of chloroquine resistance in Africa. Am J Trop Med Hyg. 2001;64:12–17. doi: 10.4269/ajtmh.2001.64.12. [DOI] [PubMed] [Google Scholar]
- 32.Bousema JT, Gouagna LC, Meutstege AM, Okech BE, Akim NI, et al. Treatment failure of pyrimethamine-sulphadoxine and induction of Plasmodium falciparum gametocytaemia in children in western Kenya. Trop Med Int Health. 2003;8:427–430. doi: 10.1046/j.1365-3156.2003.01047.x. [DOI] [PubMed] [Google Scholar]
- 33.Sowunmi A, Fateye BA. Plasmodium falciparum gametocytaemia in Nigerian children: before, during and after treatment with antimalarial drugs. Trop Med Int Health. 2003;8:783–792. doi: 10.1046/j.1365-3156.2003.01093.x. [DOI] [PubMed] [Google Scholar]
- 34.Nosten F, Van Vugt M, Price R, Luxemburger C, Thway KL, et al. Effects of artesunate-mefloquine combination on incidence of Plasmodium falciparum malaria and mefloquine resistance in western Thailand: a prospective study. Lancet. 2000;356:297–302. doi: 10.1016/s0140-6736(00)02505-8. [DOI] [PubMed] [Google Scholar]
- 35.Barnes KI, Durrheim DN, Little F, Jackson A, Mehta U, et al. Effect of artemether-lumefantrine policy and improved vector control on malaria burden in KwaZulu-Natal, South Africa. PLoS Med. 2005;2:e330. doi: 10.1371/journal.pmed.0020330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Martens P, Hall L. Malaria on the move: human population movement and malaria transmission. Emerg Infect Dis. 2000;6:103–109. doi: 10.3201/eid0602.000202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hay SI, Guerra CA, Tatem AJ, Noor AM, Snow RW. The global distribution and population at risk of malaria: past, present, and future. Lancet Infect Dis. 2004;4:327–336. doi: 10.1016/S1473-3099(04)01043-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moffett A, Shackelford N, Sarkar S. Malaria in Africa: vector species' niche models and relative risk maps. PLoS ONE. 2007;2:e824. doi: 10.1371/journal.pone.0000824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.MacDonald G. London: Oxford University Press; 1957. The epidemiology and control of malaria. [Google Scholar]
- 40.Garnham PCC. Malaria epidemics at exceptionally high altitudes in Kenya. Br Med J. 1945;2:45–47. doi: 10.1136/bmj.2.4410.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Warrell DA, Gilles HM. Essential Malariology. Arnold 2002 [Google Scholar]
- 42.Balls MJ, Bodker R, Thomas CJ, Kisinza W, Msangeni HA, et al. Effect of topography on the risk of malaria infection in the Usambara Mountains, Tanzania. Trans R Soc Trop Med Hyg. 2004;98:400–408. doi: 10.1016/j.trstmh.2003.11.005. [DOI] [PubMed] [Google Scholar]
- 43.Bayoh MN, Lindsay SW. Temperature-related duration of aquatic stages of the Afrotropical malaria vector mosquito Anopheles gambiae in the laboratory. Med Vet Entomol. 2004;18:174–179. doi: 10.1111/j.0269-283X.2004.00495.x. [DOI] [PubMed] [Google Scholar]
- 44.Koenraadt CJ, Paaijmans KP, Schneider P, Githeko AK, Takken W. Low larval vector survival explains unstable malaria in the western Kenya highlands. Trop Med Int Health. 2006;11:1195–1205. doi: 10.1111/j.1365-3156.2006.01675.x. [DOI] [PubMed] [Google Scholar]
- 45.Vincke IH, Jadin JB. Contribution à l'étude de l'anophélisme en pays d'altitude. Ann Soc Belg Med Trop. 1946;26:483–500. [Google Scholar]
- 46.Abeku TA, Van Oormarssen GJ, Borsboom G, de Vlas SJ, Habbema JD. Spatial and temporal variations of malaria epidemic risk in Ethiopia: factors involved and implications. Acta Trop. 2003;87:331–340. doi: 10.1016/s0001-706x(03)00123-2. [DOI] [PubMed] [Google Scholar]
- 47.Lindblade KA, Walker ED, Onapa AW, Katungu J, Wilson ML. Land use change alters malaria transmission parameters by modifying temperature in a highland area of Uganda. Trop Med Int Health. 2000;5:263–274. doi: 10.1046/j.1365-3156.2000.00551.x. [DOI] [PubMed] [Google Scholar]
- 48.Afrane YA, Lawson BW, Githeko AK, Yan G. Effects of microclimatic changes caused by land use and land cover on duration of gonotrophic cycles of Anopheles gambiae (Diptera: Culicidae) in western Kenya highlands. J Med Entomol. 2005;42:974–980. doi: 10.1093/jmedent/42.6.974. [DOI] [PubMed] [Google Scholar]
- 49.Munga S, Minakawa N, Zhou G, Mushinzimana E, Barrack OO, et al. Association between land cover and habitat productivity of malaria vectors in western Kenyan highlands. Am J Trop Med Hyg. 2006;74:69–75. [PubMed] [Google Scholar]
- 50.Loevinsohn ME. Climatic warming and increased malaria incidence in Rwanda. Lancet. 1994;343:714–718. doi: 10.1016/s0140-6736(94)91586-5. [DOI] [PubMed] [Google Scholar]
- 51.Minakawa N, Sonye G, Mogi M, Githeko A, Yan G. The effects of climatic factors on the distribution and abundance of malaria vectors in Kenya. J Med Entomol. 2002;39:833–841. doi: 10.1603/0022-2585-39.6.833. [DOI] [PubMed] [Google Scholar]
- 52.Pascual M, Ahumada JA, Chaves LF, Rodo X, Bouma M. Malaria resurgence in the East African highlands: temperature trends revisited. Proc Natl Acad Sci U S A. 2006;103:5829–5834. doi: 10.1073/pnas.0508929103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Paaijmans KP, Wandago MO, Githeko AK, Takken W. Unexpected high losses of Anopheles gambiae larvae due to rainfall. PLoS ONE. 2007;2:e1146. doi: 10.1371/journal.pone.0001146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kilian AH, Langi P, Talisuna A, Kabagambe G. Rainfall pattern, El Nino and malaria in Uganda. Trans R Soc Trop Med Hyg. 1999;93:22–23. doi: 10.1016/s0035-9203(99)90165-7. [DOI] [PubMed] [Google Scholar]
- 55.Lindsay SW, Bodker R, Malima R, Msangeni HA, Kisinza W. Effect of 1997-98 El Nino on highland malaria in Tanzania. Lancet. 2000;355:989–990. doi: 10.1016/s0140-6736(00)90022-9. [DOI] [PubMed] [Google Scholar]
- 56.Minakawa N, Sonye G, Mogi M, Yan G. Habitat characteristics of Anopheles gambiae s.s. larvae in a Kenyan highland. Med Vet Entomol. 2004;18:301–305. doi: 10.1111/j.0269-283X.2004.00503.x. [DOI] [PubMed] [Google Scholar]
- 57.Zhou G, Minakawa N, Githeko A, Yan G. Spatial distribution patterns of malaria vectors and sample size determination in spatially heterogeneous environments: a case study in the west Kenyan highland. J Med Entomol. 2004;41:1001–1009. doi: 10.1603/0022-2585-41.6.1001. [DOI] [PubMed] [Google Scholar]
- 58.Minakawa N, Munga S, Atieli F, Mushinzimana E, Zhou G, et al. Spatial distribution of anopheline larval habitats in Western Kenyan highlands: effects of land cover types and topography. Am J Trop Med Hyg. 2005;73:157–165. [PubMed] [Google Scholar]
- 59.Khaemba BM, Mutani A, Bett MK. Studies of anopheline mosquitoes transmitting malaria in a newly developed highland urban area: a case study of Moi University and its environs. East Afr Med J. 1994;71:159–164. [PubMed] [Google Scholar]
- 60.Ijumba JN, Lindsay SW. Impact of irrigation on malaria in Africa: paddies paradox. Med Vet Entomol. 2001;15:1–11. doi: 10.1046/j.1365-2915.2001.00279.x. [DOI] [PubMed] [Google Scholar]
- 61.Sissoko MS, Dicko A, Briet OJ, Sissoko M, Sagara I, et al. Malaria incidence in relation to rice cultivation in the irrigated Sahel of Mali. Acta Trop. 2004;89:161–170. doi: 10.1016/j.actatropica.2003.10.015. [DOI] [PubMed] [Google Scholar]
- 62.Garnham PCC, Wilson DB, Wilson ME. Malaria in Kigezi, Uganda. Trop Med Hyg. 1948;51:156–159. [PubMed] [Google Scholar]
- 63.Schwetz J. Paludisme endémique et paludisme epidémique dans des régions de haute altitude de l'Afrique centrale. Acta Trop. 1948;5:78–81. [PubMed] [Google Scholar]
- 64.Carlson JC, Byrd BD, Omlin FX. Field assessments in western Kenya link malaria vectors to environmentally disturbed habitats during the dry season. BMC Public Health. 2004;4:33. doi: 10.1186/1471-2458-4-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Stevens PA. Environmental management activities in malaria control in Africa. Bull World Health Organ. 1984;62(Suppl):77–80. [PMC free article] [PubMed] [Google Scholar]
- 66.Utzinger J, Tozan Y, Singer BH. Efficacy and cost-effectiveness of environmental management for malaria control. Trop Med Int Health. 2001;6:677–687. doi: 10.1046/j.1365-3156.2001.00769.x. [DOI] [PubMed] [Google Scholar]
- 67.Yohannes M, Haile M, Ghebreyesus TA, Witten KH, Getachew A, et al. Can source reduction of mosquito larval habitat reduce malaria transmission in Tigray, Ethiopia? Trop Med Int Health. 2005;10:1274–1285. doi: 10.1111/j.1365-3156.2005.01512.x. [DOI] [PubMed] [Google Scholar]
- 68.Curtis CF, Jana-Kara B, Maxwell CA. Insecticide treated nets: impact on vector populations and relevance of initial intensity of transmission and pyrethroid resistance. J Vector Borne Dis. 2003;40:1–8. [PubMed] [Google Scholar]
- 69.Mathenge EM, Gimnig JE, Kolczak M, Ombok M, Irungu LW, et al. Effect of permethrin-impregnated nets on exiting behavior, blood feeding success, and time of feeding of malaria mosquitoes (Diptera: Culicidae) in western Kenya. J Med Entomol. 2001;38:531–536. doi: 10.1603/0022-2585-38.4.531. [DOI] [PubMed] [Google Scholar]
- 70.Lindsay SW, Adiamah JH, Miller JE, Armstrong JR. Pyrethroid-treated bednet effects on mosquitoes of the Anopheles gambiae complex in The Gambia. Med Vet Entomol. 1991;5:477–483. doi: 10.1111/j.1365-2915.1991.tb00576.x. [DOI] [PubMed] [Google Scholar]
- 71.Hargreaves K, Koekemoer LL, Brooke BD, Hunt RH, Mthembu J, et al. Anopheles funestus resistant to pyrethroid insecticides in South Africa. Med Vet Entomol. 2000;14:181–189. doi: 10.1046/j.1365-2915.2000.00234.x. [DOI] [PubMed] [Google Scholar]
- 72.Sharp BL, Ridl FC, Govender D, Kuklinski J, Kleinschmidt I. Malaria vector control by indoor residual insecticide spraying on the tropical island of Bioko, Equatorial Guinea. Malar J. 2007;6:52. doi: 10.1186/1475-2875-6-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gamage-Mendis AC, Carter R, Mendis C, De Zoysa AP, Herath PR, et al. Clustering of malaria infections within an endemic population: risk of malaria associated with the type of housing construction. Am J Trop Med Hyg. 1991;45:77–85. doi: 10.4269/ajtmh.1991.45.77. [DOI] [PubMed] [Google Scholar]
- 74.Ghebreyesus TA, Haile M, Witten KH, Getachew A, Yohannes M, et al. Household risk factors for malaria among children in the Ethiopian highlands. Trans R Soc Trop Med Hyg. 2000;94:17–21. doi: 10.1016/s0035-9203(00)90424-3. [DOI] [PubMed] [Google Scholar]
- 75.Deressa W, Ali A, Berhane Y. Household and socioeconomic factors associated with childhood febrile illnesses and treatment seeking behaviour in an area of epidemic malaria in rural Ethiopia. Trans R Soc Trop Med Hyg. 2007;101:939–947. doi: 10.1016/j.trstmh.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 76.Saegerman C, Speybroeck N, Roels S, Vanopdenbosch E, Thiry E, et al. Decision support tools for clinical diagnosis of disease in cows with suspected bovine spongiform encephalopathy. J Clin Microbiol. 2004;42:172–178. doi: 10.1128/JCM.42.1.172-178.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gaudart J, Poudiougou B, Ranque S, Doumbo O. Oblique decision trees for spatial pattern detection: optimal algorithm and application to malaria risk. BMC Med Res Methodol. 2005;5:22. doi: 10.1186/1471-2288-5-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bodker R, Akida J, Shayo D, Kisinza W, Msangeni HA, et al. Relationship between altitude and intensity of malaria transmission in the Usambara Mountains, Tanzania. J Med Entomol. 2003;40:706–717. doi: 10.1603/0022-2585-40.5.706. [DOI] [PubMed] [Google Scholar]
- 79.Coosemans MH. Comparaison de l'endémie malarienne dans une zone de riziculture et dans une zone de culture de coton dans la plaine de la Rusizi, Burundi. Ann Soc Belg Med Trop. 1985;65(Suppl 2):187–200. [PubMed] [Google Scholar]
- 80.Protopopoff N, Van Herp M, Maes P, Reid T, Baza D, et al. Vector control in a malaria epidemic occurring within a complex emergency situation in Burundi: A case study. Malar J. 2007;6:93. doi: 10.1186/1475-2875-6-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Teklehaimanot HD, Lipsitch M, Teklehaimanot A, Schwartz J. Weather-based prediction of Plasmodium falciparum malaria in epidemic-prone regions of Ethiopia I. Patterns of lagged weather effects reflect biological mechanisms. Malar J. 2004;3:41. doi: 10.1186/1475-2875-3-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Protopopoff N, Verhaeghen K, Van Bortel W, Roelants P, Marcotty T, et al. A significant increase in kdr in Anopheles gambiae is associated with an intensive vector control intervention in Burundi highlands. Trop Med Int Health. 2008;13:1479–1487. doi: 10.1111/j.1365-3156.2008.02164.x. [DOI] [PubMed] [Google Scholar]
- 83.Seyoum A, Balcha F, Balkew M, Ali A, Gebre-Michael T. Impact of cattle keeping on human biting rate of anopheline mosquitoes and malaria transmission around Ziway, Ethiopia. East Afr Med J. 2002;79:485–490. doi: 10.4314/eamj.v79i9.9121. [DOI] [PubMed] [Google Scholar]
- 84.Rogers DJ, Randolph SE. The global spread of malaria in a future, warmer world. Science. 2000;289:1763–1766. doi: 10.1126/science.289.5485.1763. [DOI] [PubMed] [Google Scholar]
- 85.Thomas CJ, Davies G, Dunn CE. Mixed picture for changes in stable malaria distribution with future climate in Africa. Trends Parasitol. 2004;20:216–220. doi: 10.1016/j.pt.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 86.Tanser FC, Sharp B, Le Sueur D. Potential effect of climate change on malaria transmission in Africa. Lancet. 2003;362:1792–1798. doi: 10.1016/S0140-6736(03)14898-2. [DOI] [PubMed] [Google Scholar]
- 87.Martens WJ, Niessen LW, Rotmans J, Jetten TH, McMichael AJ. Potential impact of global climate change on malaria risk. Environ Health Perspect. 1995;103:458–464. doi: 10.1289/ehp.95103458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Patz JA, Hulme M, Rosenzweig C, Mitchell TD, Goldberg RA, et al. Climate change: Regional warming and malaria resurgence. Nature. 2002;420:627–628. doi: 10.1038/420627a. [DOI] [PubMed] [Google Scholar]
- 89.Hay SI, Cox J, Rogers DJ, Randolph SE, Stern DI, et al. Climate change and the resurgence of malaria in the East African highlands. Nature. 2002;415:905–909. doi: 10.1038/415905a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Shanks GD, Hay SI, Stern DI, Biomndo K, Snow RW. Meteorologic influences on Plasmodium falciparum malaria in the Highland Tea Estates of Kericho, Western Kenya. Emerg Infect Dis. 2002;8:1404–1408. doi: 10.3201/eid0812.020077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Small J, Goetz SJ, Hay SI. Climatic suitability for malaria transmission in Africa, 1911-1995. Proc Natl Acad Sci U S A. 2003;100:15341–15345. doi: 10.1073/pnas.2236969100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bonora S, De Rosa FG, Boffito M, Di Perri G, Rossati A. Rising temperature and the malaria epidemic in Burundi. Trends Parasitol. 2001;17:572–573. doi: 10.1016/s1471-4922(01)02095-5. [DOI] [PubMed] [Google Scholar]
- 93.Gomez-Elipe A, Otero A, Van Herp M, Aguirre-Jaime A. Forecasting malaria incidence based on monthly case reports and environmental factors in Karuzi, Burundi, 1997-2003. Malar J. 2007;6:129. doi: 10.1186/1475-2875-6-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Lindblade KA, Walker ED, Wilson ML. Early warning of malaria epidemics in African highlands using Anopheles (Diptera: Culicidae) indoor resting density. J Med Entomol. 2000;37:664–674. doi: 10.1603/0022-2585-37.5.664. [DOI] [PubMed] [Google Scholar]
- 95.Abeku TA. Response to malaria epidemics in Africa. Emerg Infect Dis. 2007;13:681–686. doi: 10.3201/eid1305.061333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Shiff C. Integrated approach to malaria control. Clin Microbiol Rev. 2002;15:278–293. doi: 10.1128/CMR.15.2.278-293.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Walker K, Lynch M. Contributions of Anopheles larval control to malaria suppression in tropical Africa: review of achievements and potential. Med Vet Entomol. 2007;21:2–21. doi: 10.1111/j.1365-2915.2007.00674.x. [DOI] [PubMed] [Google Scholar]
- 98.Ault SK. Environmental management: a re-emerging vector control strategy. Am J Trop Med Hyg. 1994;50:35–49. doi: 10.4269/ajtmh.1994.50.35. [DOI] [PubMed] [Google Scholar]
- 99.Killeen GF, Seyoum A, Knols BG. Rationalizing historical successes of malaria control in Africa in terms of mosquito resource availability management. Am J Trop Med Hyg. 2004;71:87–93. [PubMed] [Google Scholar]
- 100.Zhou G, Munga S, Minakawa N, Githeko AK, Yan G. Spatial relationship between adult malaria vector abundance and environmental factors in Western Kenya highlands. Am J Trop Med Hyg. 2007;77:29–35. [PubMed] [Google Scholar]