Abstract
Background
The Carpal Tunnel Syndrome Instrument (CTSI) is a disease-specific, self-administered questionnaire that consists of a symptom severity scale (SS) and a functional status scale (FS). The CTSI was cross-culturally adapted and developed by the Impairment Evaluation Committee, Japanese Society for Surgery of the Hand (JSSH). The purpose of this study was to test the reliability, validity, and responsiveness of the Japanese version of the CTSI (CTSI-JSSH).
Methods
A consecutive series of 87 patients with carpal tunnel syndrome completed the CTSI-JSSH, the JSSH version of the Disability of the Arm, Shoulder, and Hand questionnaire (DASH-JSSH), and the 36-Item Short-Form Health Survey (SF-36). Seventy-two of the patients were reassessed for test–retest reliability 1 or 2 weeks later. Reliability was investigated by the reproducibility and the internal consistency. To analyze the validity, a factor analysis (principal axis factoring) of the CTSI-JSSH and the correlation coefficients between the CTSI-JSSH and DASH-JSSH were obtained. The responsiveness was examined by calculating the standardized response mean (SRM; mean change/SD) and effect size (mean change/SD of baseline value) after carpal tunnel release in 42 patients.
Results
Cronbach’s alpha coefficients for the CTSI-JSSH-SS and the CTSI-JSSH-FS were 0.84 and 0.90, respectively, and the intraclass correlation coefficients were 0.82 and 0.83, respectively. The unidimensionality of the CTSI-JSSH-SS was barely confirmed; the unidimensionality of the CTSI-JSSH-FS was confirmed. The correlation coefficients between the CTSI-JSSH-FS and the CTSI-JSSH-SS or DASH-JSSH were 0.58 and 0.80, respectively. The correlation coefficient between the CTSI-JSSH-SS and DASH-JSSH was 0.54. The correlation coefficients between the subscales of SF-36 and the CTSI-JSSH-SS or the CTSI-JSSH-FS ranged from −0.23 to −0.66 and from −0.19 to −0.63, respectively. The SRMs/effect sizes of the CTSI-JSSH-SS and the CTSI-JSSH-FS were −0.85/−0.99 and −0.70/−0.61, which indicated that they were more than moderately sensitive.
Conclusions
The CTSI-JSSH has sufficient reliability, validity, and responsiveness to assess the health status in carpal tunnel syndrome.
Introduction
Health measurement scales are important patient outcome tools to measure health status and to evaluate medical intervention.1 Recently, several measures for the evaluation of upper extremity function have been developed.2–5 Some of them are joint-specific measures2,3 or region-specific measures.4,5 Others are intended to evaluate the symptoms and function of the upper extremity using disease-specific measures.6 Among the region-specific measures, the Disability of the Arm, Shoulder and Hand (DASH) questionnaire5 and its short version (QuickDASH)7 are the most recently devised scales and now are widely used in several countries, including Japan, Sweden, France, Germany, Spain, the Netherlands, Italy, and China.8–16 As one of the disease-specific measures, a self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome was originally devised by Levine et al.6 This instrument has been called by several names, e.g., the Carpal Tunnel Syndrome Instrument (CTSI),17 Brigham and Women’s Carpal Tunnel Questionnaire,18 and the Boston Carpal Tunnel Syndrome Questionnaire.19 We adopted the CTSI for the current study. The CTSI is now available in a few languages and has been used in several countries (e.g., Sweden,17 Spain,13 Italy,20 and the Netherlands21). The only studies of reliability and validity of the CTSI that have been published are for the original CTSI6 and for the Swedish version.17
We, the Impairment Evaluation Committee of the Japanese Society for Surgery of the Hand (JSSH), have completed cross-cultural adaptation and have developed the JSSH version of the CTSI (CTSI-JSSH).22 The purpose of this study was to test the reliability, validity, and responsiveness of the CTSI-JSSH and to make the CTSI-JSSH available for use in Japan.
Materials and methods
In accordance with published guidelines,23 we set up the CTSI-JSSH committee and recruited translators, researchers, a methodologist, and a Japanese language expert, and culturally adapted the CTSI into Japanese, as had been done for DASH-JSSH.8
The adaptation process
The English version of the CTSI6 was translated into Japanese by two translators whose first language was Japanese. One of them had no medical background and the other did have a medical background. Their two “forward” translations were synthesized into one version after being reviewed and discussed by the committee. This Japanese version (the prefinal version) was translated back into English by two other translators whose first language was English. One of them was blinded to the concepts being investigated and had no medical background; the other had a medical background. After we compared these two back-translations with the original CTSI, we developed the CTSI-JSSH (prefinal version 2). Then we commenced the pilot test. After analyzing the pilot test data, we modified prefinal version 2 of the CTSI-JSSH into a final version. The final CTSI-JSSH version22 was then evaluated with regard to reliability, validity, and responsiveness.
The CTSI questionnaire
The CTSI questionnaire developed by Levine et al.6 contains two subscales: a symptom severity scale (CTSISS) (Table 1) and a functional status scale (CTSI-FS) (Table 2).
Table 1.
Symptom severity scale of the Carpal Tunnel Syndrome Instrument
| Item code | Scale item |
|---|---|
| SS-1 | Severity of nocturnal pain |
| SS-2 | Frequency of nocturnal awakening due to pain |
| SS-3 | Severity of daytime pain |
| SS-4 | Frequency of daytime pain |
| SS-5 | Duration of daytime pain |
| SS-6 | Severity of numbness |
| SS-7 | Severity of weakness |
| SS-8 | Severity of tingling |
| SS-9 | Severity of nocturnal numbness or tingling |
| SS-10 | Frequency of nocturnal awakening due to numbness or tingling |
| SS-11 | Difficulty with grasping and use of small objects |
Table 2.
Functional status scale of the Carpal Tunnel Syndrome Instrument
| Item code | Scale item |
|---|---|
| FS-1 | Writing |
| FS-2 | Buttoning clothes |
| FS-3 | Holding a book while reading |
| FS-4 | Gripping the telephone receiver |
| FS-5 | Opening jars |
| FS-6 | Performing household chores |
| FS-7 | Carrying of grocery bags |
| FS-8 | Bathing and dressing |
The CTSI-SS consists of eleven items which were derived from six clinical domains for carpal tunnel syndrome: pain (three items, numbers 3–5), paresthesia (one item, number 8), numbness (one item, number 6), weakness (one item, number 7), nocturnal symptoms (four items, numbers 1,2,9,10), and overall functional status (one item, number 11). The eleven questions have multiple-choice responses, scored from 1 point (no symptom) to 5 points (most severe symptom). The overall symptom severity score is calculated as the mean of the scores for the eleven individual items.
The CTSI-FS consists of eight functional activities commonly affected by carpal tunnel syndrome. The answers are rated from 1 point (no difficulty with the activity) to 5 points (cannot perform the activity at all). The overall score for functional status is calculated as the mean of all eight items.
Patients and setting
The study was conducted on a consecutive series of 87 patients (15 men, 66 women) with a clinical diagnosis of carpal tunnel syndrome seen on an outpatient or inpatient basis in five orthopedic surgery departments in Japan. The mean age was 58.3 years (SD 13.8 years, range 21–86 years). After informed consent was obtained from the patients to participate in this study, they answered the CTSI-JSSH questionnaire,22 the JSSH version of the DASH (DASH-JSSH) questionnaire,8 the official Japanese version of the 36-Item Short-Form Health Survey (SF-36, version 1.2),24 and the Visual Analog Scale (VAS) (0–10 scale) for pain. The data collected from the 87 patients were used as a baseline value. Among the 87 patients, the 72 who had received no treatment such as medication or rehabilitation during the consecutive visits were readministered the CTSI-JSSH questionnaire 1 or 2 weeks later. The 45 patients who underwent carpal tunnel release answered the CTSI-JSSH and the DASH-JSSH questionnaires twice, once preoperatively and once postoperatively, 3 months after surgery. The protocol of this study was reviewed and approved by the institutional review boards prior to implementation.
Assessment of reliability, validity, and responsiveness
Reliability was investigated by looking at the reproducibility and internal consistency based on the test-retest method. The following analyses were conducted to examine the validity. A factor analysis (principal axis factoring) was conducted to examine the construct validity and the unidimensionality of the CTSI-JSSH-SS and CTSI-JSSH-FS. The completeness of item responses for the CTSI-JSSH was examined.
Correlation coefficients between the CTSI-JSSH (SS and FS) and DASH-JSSH were obtained, and the following hypotheses were examined to investigate concurrent validity: (1) the CTSI-JSSH-SS would exhibit a moderate association with DASH-JSSH; (2) the CTSI-JSSH-FS would exhibit the strongest association with DASH-JSSH.
Correlation coefficients between the CTSI and SF-36 were also obtained, and the following hypotheses were examined to investigate concurrent validity: (1) the CTSI-JSSH-SS would exhibit the strongest association with “bodily pain” (SF-36-BP) among the SF-36 subscales; (2) the CTSI-JSSH-FS would exhibit the strongest association with “physical functioning” (SF-36-PF) or “role-physical” (SF-36-RP). These three subscales of SF-36 were chosen because the correlation between DASH-JSSH and the three subscales of SF-36 was more than moderate.8
The responsiveness of both the CTSI-JSSH and DASH-JSSH were examined by calculating the standardized response mean (SRM; mean change/SD)25 and the effect size (mean change/SD of baseline value)26 after carpal tunnel release.
Statistical analysis
The distributions of the CTSI-JSSH, DASH-JSSH, SF-36, VAS for pain, the ages of the subjects, and the time required to fill out the CTSI-JSSH questionnaire were assessed. The interval measurements (CTSI-JSSH-SS, CTSI-JSSH-FS, DASH-JSSH, SF-36-BP, age) were normally distributed and the other interval measurements (SF-36-PF, SF-36-RP, VAS for pain, and time required to fill out the questionnaire of the CTSI-JSSH) were not normally distributed. Then Cronbach’s alpha was used to assess internal consistency of the CTSI-JSSH (SS and FS). The instrument test-retest reliability of CTSI-JSSH (SS and FS) was assessed with the intraclass correlation coefficient (ICC). All correlation coeffi cients among the CTSI-JSSH, DASH-JSSH, and SF-36 results were calculated with use of Spearman’s rank correlation coefficient. The changes in measurements after carpal tunnel release were assessed with a parametric test (paired t test). All statistical analyses were conducted using the Statistical Package for Social Science (SPSS) version 14.0J software (SPSS Japan, Tokyo). The critical values for significance were set at P < 0.05.
Results
Completeness of item responses
No patients had difficulty completing the CTSI-JSSH questionnaire. It took them 5 min 40 s, on average, to finish the questionnaire (median: 5 min, range: 2–30 min). Most of the patients considered all the items of the CTSI to be clear. Nine of the 72 patients (nonrespondent group) did not answer one or more items of the CTSI. Two of these patients failed to answer more than two items, with each leaving four items unanswered. Items 5, 7, and 8 of the CTSI-JSSH-SS were left unanswered by one patient each. Three patients did not answer items 1 and 3 of the CTSI-JSSH-FS. Two patients did not respond to item 7 of the CTSI-JSSH-FS. Items 2, 4, 6, and 8 of CTSI-JSSH-FS were each unanswered by one patient. The mean age [70 ± 12 (SD) years] of the nonrespondent group (n = 9) was significantly larger than the mean age (57 ± 13 years) of the respondent group (n = 78) who completed all the items (P = 0.008).
The mean, median, SD, and range of the CTSI-JSSH, DASH-JSSH, SF-36, and VAS for pain scores are shown in Table 3. The number of ceiling scores in the CTSI-JSSH were identified. One and five patients had the minimum disability score of zero (ceiling) on the CTSI-JSSH-SS and the CTSI-JSSH-FS, respectively. No patient had a maximum disability score of 5 (floor) either on the CTSI-JSSH-SS or on the CTSI-JSSH-FS.
Table 3.
Mean scores and range of scores for CTSI, DASH, SF-36, and VAS
| Instrument scale (n) | Mean | SD | Median | Minimum | Maximum |
|---|---|---|---|---|---|
| CTSI-JSSH-SS (87) | 2.53 | 0.72 | 2.54 | 1.00a | 4.27 |
| CTSI-JSSH-FS (87) | 2.20 | 0.80 | 2.00 | 1.00a | 4.00 |
| DASH-JSSH (79) | 31.2 | 18.3 | 27.5 | 0a | 74.1 |
| SF-36-PF (77) | 65.2 | 29.2 | 75.0 | 0b | 100a |
| SF-36-RP (66) | 56.6 | 40.2 | 75.0 | 0b | 100a |
| SF-36-BP (77) | 44.9 | 19.9 | 41.0 | 0b | 100a |
| VAS (77) | 3.4 | 3.0 | 3.0 | 0a | 10b |
CTSI-JSSH-SS, the symptom severity scale of the Japanese Society for Surgery of the Hand versión of the Carpal Tunnel Syndrome Instrument (CTSI-JSSH); CTSI-JSSH-FS, the functional status scale of the CTSI-JSSH; DASH-JSSH, the disability/symptom scale of the Japanese versión of the Disability of the Arm, Shoulder, and Hand questionnaire; SF-36-PF, physical functioning subscale of the 36-Item Short-Form Health Survey (SF-36); SF-36-RP, role-physical subscale of SF-36; SF-36-BP, bodily pain subscale of SF-36; VAS, Visual Analog Scale for pain (0–10 scale)
a Maximum health status scores (ceiling)
b Minimum health status scores (floor)
Reliability
Internal consistency was assessed by use of Cronbach’s alpha coefficient. The alpha coefficient for the 11 items in the CTSI-JSSH-SS was 0.839 (n = 84). When the al pha coefficient was calculated for each of the 11 items by eliminating each item, one by one, the range was 0.814–0.838; no item was found to change the internal consistency substantially. The alpha coefficient for the 8 items of the CTSI-JSSH-FS was 0.900 (n = 82). When the alpha coefficient was calculated for each of the 8 items by eliminating each item, one by one, the range was 0.879–0.900; no item was found to change the internal consistency substantially.
Instrument test-retest reliability was assessed with the intraclass correlation coefficient (ICC). There were 72 patients involved in the assessment of test-retest reliability, and the period between the first and second tests was on average 10.7 days (SD 6.0 days). The ICCs for the CTSI-JSSH-SS and the CTSI-JSSH-FS were 0.82 (95%CI: 0.79–0.89) and 0.83 (95%CI: 0.74–0.89), respectively. Both ICCs for the CTSI-JSSH subscales indicate sufficient reproducibility.
Validity
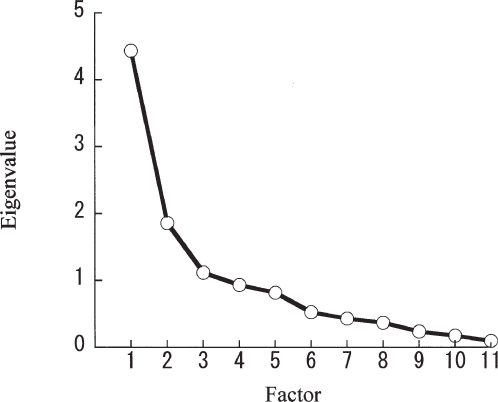
A factor analysis (principal axis factoring) was conducted to confirm the unidimensionality of the CTSI-JSSH-SS and the CTSI-JSSH-FS. The first factor of the CTSI-JSSH-SS had an eigenvalue (amount of variation in the total sample accounted for by that factor)14 of 4.44, which explained 40% of the total variance of the CTSI-JSSH-SS scores of the patients (Fig. 1). The second factor of the CTSI-JSSH-SS had an eigenvalue of 1.86, which explained 17% of the total variance of the CTSI-JSSH-SS scores of the patients, these two factors thus explain 57% of the cumulative variance of the CTSI-JSSH-SS scores of the patients (Fig. 1). Factor analysis indicated the presence of at least two factors in the CTSI-JSSH-SS, which means bidimensionality. Next, further factor analysis (principal axis factoring set for two factors, rotation: promax) was conducted. When looking at the first factor loading for each item, some items (items 1, 2, 6, 9, 10, and 11) had a loading (the correlation with the total score) of 0.4 or higher (Table 4). When looking at the second factor loading for each item, some items (items 3, 4, and 5) had a loading of 0.4 or higher (Table 4). When we adopted one factor to conduct factor analysis (principal axis factoring) of the CTSI-JSSH-SS, the loading of all factors was more than 0.4, except for item 11.
Fig. 1.
Scree plot of the factors in the symptom severity scale of the Japanese Society for Surgery of the Hand version of the Carpal Tunnel Syndrome Instrument (CTSI-JSSH)
Table 4.
Pattern matrix (rotated, promax) of factor analysis for CTSI-SS
| Component | ||
|---|---|---|
| Item | 1 | 2 |
| CTSI-SS-2 | 0.827 | |
| CTSI-SS-9 | 0.805 | |
| CTSI-SS-10 | 0.795 | |
| CTSI-SS-6 | 0.607 | |
| CTSI-SS-1 | 0.542 | 0.324 |
| CTSI-SS-11 | 0.415 | |
| CTSI-SS-7 | 0.319 | 0.204 |
| CTSI-SS-8 | 0.271 | 0.222 |
| CTSI-SS-4 | 1.042 | |
| CTSI-SS-5 | 0.771 | |
| CTSI-SS-3 | 0.746 | |
Loadings of more trian 0.2 are shown in this table
Bold figures indícate values greater than 0.4
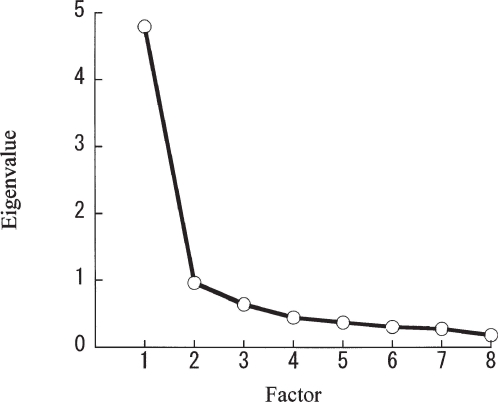
The first factor of the CTSI-JSSH-FS had an eigenvalue of 4.79, which explained 60% of the total variance of the CTSI-JSSH-FS scores of the patients (Fig. 2). The unidimensionality of the CTSI-JSSH-FS was found to be strong as a result of the low eigenvalue of the second factor (0.96, Fig. 2). When looking at the first factor loading for each item, all items had a loading of 0.4 or higher.
Fig. 2.
Scree plot of the factors in the functional status scale of CTSI-JSSH
The correlation coefficients between the CTSI-JSSH-SS and the CTSI-JSSH-FS or the DASH-JSSH were 0.58 and 0.54, respectively (Table 5, P < 0.01). These results indicate a moderate correlation between the CTSI-JSSH-SS and the CTSI-JSSH-FS, and between the CTSI-JSSH-SS and DASH-JSSH. The correlation coefficient between the CTSI-JSSH-FS and DASHJSSH was 0.80 (Table 5, P < 0.01), which indicates a strong correlation between them. These results support the hypotheses set down in advance.
Table 5.
CTSI, DASH, SF-36, VAS and their correlation
| Correlationa with | |||
|---|---|---|---|
| Instrument scale (n) | CTSI-JSSH-SS (87) | CTSI-JSSH-FS | DASH-JSSH |
| CTSI-JSSH-FS (87) | 0.58** | — | — |
| DASH-JSSH (79) | 0.54** | 0.80** | — |
| SF-36-PF (77) | −0.23 | −0.19 | −0.34** |
| SF-36-RP (66) | −0.29* | −0.50** | −0.71** |
| SF-36-BP (77) | −0.66** | −0.63** | −0.68** |
| VAS (77) | 0.40** | 0.23* | 0.32** |
*P<0.05
**P<0.01
a Spearman’s rank correlation
The correlations between the CTSI-JSSH-SS score and the subscales of the SF-36 scale ranged from −0.23 to −0.66 (Table 5). The strongest correlation was observed for “bodily pain.” The correlation between the CTSI-JSSH-SS and “role-physical” or “physical functioning” were somewhat weak. These results support the hypotheses set down in advance.
The correlations between the CTSI-JSSH-FS score and the subscales of the SF-36 scale ranged from −0.19 to −0.63 (Table 5). The strongest correlation was observed for “bodily pain” followed by “role-physical.” The correlation between the CTSI-JSSH-FS and “physical functioning” was somewhat weak. These results contradicted the hypotheses set down in advance, except for “role-physical.”
No statistical difference (P = 0.904) in age was found between men [mean (SD): 60 (12) years] and women [mean (SD): 59 (13) years]. The CTSI-JSSH-SS scores for men [mean (SD): 2.68 (0.80)] and women [mean (SD): 2.49 (0.68)] were compared by Student’s t test. There was no statistical difference between them (P = 0.29). The CTSI-JSSH-FS scores for men [mean (SD): 2.40 (0.80)] and women [mean (SD): 2.21 (0.74)] were similarly compared and there was no statistical difference between them (P = 0.37). These results support our hypothesis. The correlation between age and the CTSI-JSSH-SS or the CTSI-JSSH-FS score was weak (r = −0.041, P = 0.704; r = 0.014, P = 0.898, respectively).
The correlation between the CTSI-JSSH-SS score and VAS for pain was moderate but the correlation between the CTSI-JSSH-FS score and VAS for pain was weak (Table 5).
Responsiveness
Forty-two patients of the 45 who underwent carpal tunnel release completed the CTSI-JSSH and the DASH-JSSH questionnaires at 3 months (mean: 96 days, SD: 9 days) after the surgery. The mean subject age was 62 years (SD: 14 years, range: 21–86 years). There were 5 men and 37 women. The calculated standardized response mean (SRM) and effect size for CTSI-JSSH-SS (n = 42), CTSI-JSSH-FS (n = 42), and DASH-JSSH (n = 40) was −0.85/−0.99, −0.70/−0.61, and −0.35/−0.36, respectively. There were statistical differences between the mean value of preoperative and postoperative CTSI-JSSH-SS scores (P < 0.001), CTSI-JSSH-FS scores (P < 0.001), and DASH-JSSH scores (P = 0.034).
Discussion
Adaptation of the CTSI questionnaire for Japanese patients was performed following a systematic standardized approach.23 The purpose of this study was to examine the psychometric qualities of the CTSI by assessing its psychometric standards in the areas of reliability, validity, and responsiveness.
The CTSI consists of an 11-item symptom severity scale and an 8-item functional status scale. It took patients a shorter time to complete the CTSI-JSSH compared with the time to complete the DASH-JSSH.8 This indicated that the questionnaire was easy to understand. Most older patients left no more than two items unanswered and those were thought to be pertaining to specific activities that those individuals did not perform. The lack of floor effects assures the authors of the validity of both subscales of the CTSI-JSSH.
As for internal consistency, the Cronbach’s alpha coefficients for CTSI-JSSH-SS (0.83) and CTSI-JSSH-FS (0.90) were equivalent to those of the original version of the CTSI (SS: 0.89, FS: 0.91)6 and those of the Swedish version of the CTSI (SS: 0.80, FS: 0.87).17 As for reproducibility, the ICC of the CTSI-JSSH-SS (0.82) and the CTSI-JSSH-FS (0.83) were not equivalent to the Pearson correlation coefficients of the original version of the CTSI (SS: 0.91, FS: 0.93)6 but were equivalent to the Pearson correlation coefficients of the Swedish version of the CTSI (SS: 0.80, FS: 0.87).17 Therefore the results for the internal consistency and reproducibility of the CTSI-JSSH indicate sufficient reliability.
As for measurement precision, recommended reliability standards for individual-level applications range from a low of 0.90 to a high of 0.95, which is the desired standard.27 Most general health status measures [e.g., SF-36, the Nottingham Health Profile (NHP), and the Functional Status Questionnaire (FSQ)],27 as well as lesion- or joint-specific questionnaires [e.g., the Roland-Morris Disability Questionnaire28 and the Western Ontario and McMaster Universities osteoarthritis index (WOMAC)] cannot meet this standard, whether they are designed for individual patient applications or group-level applications. Most translated DASH versions8,10,12–15 as well as the original DASH29 have internal consistency values higher than 0.95 and meet this standard. But the symptom severity scale and functional status scale of the CTSI-JSSH had internal consistency values of 0.84 and 0.90. We would thus prefer that the CTSI-JSSH be used for groups of patients or workers.
There are many types of validation processes of quality of life (QOL) questionnaires. The present study adopted correlation between CTSI-JSSH and other QOL questionnaires such as SF-36 and DASH. Although Levine et al.6 and Atroshi et al.17 did not demonstrate those correlations, Gay et al.30 studied the correlation between the original DASH and the original CTSI 6 weeks after carpal tunnel release. The correlation coefficients between the CTSI-SS and the CTSI-FS or DASH were 0.74 and 0.88 respectively.30 The validation process of the CTSI-JSSH questionnaire has shown that it has lower validity than the original CTSI.30 The strong correlations between the CTSI-JSSH and DASH-JSSH support the validity of CTSI-JSSH (Table 5). The moderate correlations between the CTSI-JSSH and SF-36 subscales (physical functioning and bodily pain) also support this validity. These results demonstrate that the CTSI-JSSH measures the important elements that make up health-related QOL.
Another validation method is factor analysis, which was not adopted in other validation studies of the CTSI.6,17 The symptom severity scale of the CTSI-JSSH exhibited bidimensionality (Table 4, Fig. 1). The two factors could be identified from this table. The second factor is “daytime pain” (items 3–5). The first factor is other symptoms such as nocturnal symptoms (items 1, 2, 9, 10), numbness (item 6), weakness (item 7), paresthesia (item 8), and overall functional status (item 11). Atroshi et al.17 divided the symptom severity scale into two components: the pain component (items 1–5) and the sensory component (items 6 and 8–11), and successfully demonstrated that the responsiveness of the sensory component is larger than that of the pain component, although they did not conduct a factor analysis. Theoretically, overall functional status (item 11 of symptom severity) could be included in the functional status scale. These results show that the symptom severity scale of the CTSI-JSSH could be divided into two. If we adopt one factor for the symptom severity scale of the CTSI-JSSH, it barely maintains unidimensionality from the results of factor loading. This means that the symptom severity scale of the CTSI-JSSH has a high quality of validation.
The functional status scale of the CTSI-JSSH exhibited high unidimensionality and there was no low item-scale correlation. The loading of this scale was very high. These results show that the functional status scale of the CTSI-JSSH has a high quality of validation.
Cohen’s rule of thumb for interpreting the “effect size index” (i.e., a value of 0.2 is small, 0.5 is moderate, and 0.8 or greater is large) can be applied to the SRM.25 The responsiveness of the symptom severity scale and functional status scale of the CTSI-JSSH for patients with carpal tunnel syndrome was large and moderate, respectively, 3 months after carpal tunnel release operation, although other studies of the CTSI17,30 showed twice the responsiveness levels of our results. The responsiveness levels of both subscales of CTSI-JSSH were twice that of DASH-JSSH. Gay et al.30 also described similar findings. Moreover, there were statistical differences between the mean value of preoperative and postoperative subscale scores for the CTSI-JSSH.
We believe that the strengths of this study are that the CTSI-JSSH demonstrated good reproducibility, consistency, and validity. Moreover, it had at least moderate responsiveness. A limitation of the present study is that we could not successfully demonstrate the responsiveness of the CTSI-JSSH because the sample size was relatively small and the patients’ response rate was low. Moreover, the subjects of this study are not representative of the general population.
Conclusions
We can conclude that the Japanese Society for Surgery of the Hand version of the Carpal Tunnel Syndrome Instrument (CTSI-JSSH) has sufficient reliability, validity, and responsiveness to assess the severity of symptoms and the functional status in carpal tunnel syndrome. Above all, the CTSI-JSSH can be used for groups of patients.
References
- 1.Dawson J, Carr A. Outcomes evaluation in orthopaedics. J Bone Joint Surg Br. 2001;83:313–5. doi: 10.1302/0301-620X.83B3.12148. [DOI] [PubMed] [Google Scholar]
- 2.Constant CR, Murley AHG. A clinical method of functional assessment of the shoulder. Clin Orthop. 1987;214:160–4. [PubMed] [Google Scholar]
- 3.Research Committee, American Shoulder and Elbow Surgeons. Richards R, An KN, Bigliani LU, Friedman RJ, Gartsman GM, Gristina AG, et al. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3:347–52. doi: 10.1016/S1058-2746(09)80019-0. [DOI] [PubMed] [Google Scholar]
- 4.Martin DP, Engelberg R, Agel J, Swiontrowski MF. Comparison of the Musculoskeletal Function Assessment questionnaire with the Short Form-36, the Western Ontario and McMaster Universities Osteoarthritis Index, and the Sickness Impact Profile health status measures. J Bone Joint Surg Am. 1997;79:1323–35. doi: 10.2106/00004623-199709000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Hudak PL, Amadio PC, Bombardier C, Upper the. Extremity Collaborative Group (UECG). Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected] Am J Ind Med. 1996;29:602–8. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 6.Levine DW, Simmons BP, Koris MJ, Daltroy LH, Hohl GG, Fossel AH, et al. A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. J Bone Joint Surg Am. 1993;75:1585–92. doi: 10.2106/00004623-199311000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Beaton DE, Wright JG, Katz JN, Upper Extremity Collaborative Group . Development of the QuickDASH: comparison of the three item-reduction approaches. J Bone Joint Surg Am. 2005;87:1038–46. doi: 10.2106/JBJS.D.02060. [DOI] [PubMed] [Google Scholar]
- 8.Imaeda T, Toh S, Nakao Y, Nishida J, Hirata H, Ijichi M, for the Impairment Evaluation Committee, Japanese Society for Surgery of the Hand et al. Validation of the Japanese Society for Surgery of the Hand version of the Disability of the Arm, Shoulder, and Hand questionnaire. J Orthop Sci. 2005;10:353–9. doi: 10.1007/s00776-005-0917-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Imaeda T, Toh S, Wada T, Uchiyama S, Okinaga S, Kusunose K, et al. for the Impairment Evaluation Committee, Japanese Society for Surgery of the Hand. Validation of the Japanese Society for Surgery of the Hand Version of the Quick Disability of the Arm, Shoulder, and Hand (QuickDASH-JSSH) questionnaire. J Orthop Sci. 2006;11:248–53. doi: 10.1007/s00776-006-1013-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Atroshi I, Gummesson C, Andersson B, Dahlgren E, Johansson A. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: reliability and validity of the Swedish version evaluated in 176 patients. Acta Orthop Scand. 2000;71:613–8. doi: 10.1080/000164700317362262. [DOI] [PubMed] [Google Scholar]
- 11.Dubert T, Voche P, Dumontier C, Dinh A. Le questionnaire DASH. Adaptation française d’un outil d’évaluation international. Chir Main. 2001;20:294–302. doi: 10.1016/S1297-3203(01)00049-X. [DOI] [PubMed] [Google Scholar]
- 12.Offenbaecher M, Ewert T, Sangha O, Stucki G. Validation of a German version of the Disabilities of Arm, Shoulder, and Hand questionnaire (DASH-G) J Rheumatol. 2002;29:401–2. [PubMed] [Google Scholar]
- 13.Rosales RS, Delgado EB, De la Lastra-Bosch ID. Evaluation of the Spanish version of the DASH and carpal tunnel syndrome health-related quality-of-life instruments: cross-cultural adaptation process and reliability. J Hand Surg [Am] 2002;27:334–43. doi: 10.1053/jhsu.2002.30059. [DOI] [PubMed] [Google Scholar]
- 14.Veehof MM, Sleegers EJA, van Veldhoven NHMJ, Schuurman AH, van Meeteren NLU. Psychometric qualities of the Dutch language version of the Disabilities of the Arm, Shoulder, and Hand questionnaire (DASH-DLV) J Hand Ther. 2002;15:347–54. doi: 10.1016/s0894-1130(02)80006-0. [DOI] [PubMed] [Google Scholar]
- 15.Padua R, Padua L, Ceccarelli E, Romanini E, Zanoli G, Amadio PC, et al. Italian version of the Disability of the Arm, Shoulder and Hand (DASH) questionnaire. Cross-cultural adaptation and validation. J Hand Surg [Br] 2003;28:179–86. doi: 10.1016/s0266-7681(02)00303-0. [DOI] [PubMed] [Google Scholar]
- 16.Lee EWC, Lau JSY, Chung MMH, Li APS, Lo SK. Evaluation of the Chinese version of the Disability of the Arm, Shoulder and Hand (DASH-HKPWH): cross-cultural adaptation process, internal consistency and reliability study. J Hand Ther. 2004;17:417–23. [PubMed] [Google Scholar]
- 17.Atroshi I, Johnsson R, Sprinchorn A. Self-administered outcome instrument in carpal tunnel syndrome: reliability, validity and responsiveness evaluated in 102 patients. Acta Orthop Scand. 1998;69:82–8. doi: 10.3109/17453679809002363. [DOI] [PubMed] [Google Scholar]
- 18.Amadio PC, Silverstein MD, Ilstrup DM, Schleck CD, Jensen LM. Outcome assessment for carpal tunnel surgery: the relative responsiveness of generic, arthritis-specific, disease-specific, and physical examination measures. J Hand Surg [Am] 1996;21:338–46. doi: 10.1016/S0363-5023(96)80340-6. [DOI] [PubMed] [Google Scholar]
- 19.Hobby JL, Venkatesh R, Motkur P. The effect of age and gender upon symptoms and surgical outcomes in carpal tunnel syndrome. J Hand Surg [Br] 2005;30:599–604. doi: 10.1016/j.jhsb.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 20.Padua L, Padua R, Aprile I, Caliandro P, Tonali P. Boston Carpal Tunnel Questionnaire: the influence of diagnosis on patient-oriented results. Neurol Res. 2005;27:522–4. doi: 10.1179/016164105X17260. [DOI] [PubMed] [Google Scholar]
- 21.Hagebeuk EEO, de Weerd AW. Clinical and electrophysiological follow-up after local steroid injection in the carpal tunnel syndrome. Clin Neurophysiol. 2004;115:1464–8. doi: 10.1016/j.clinph.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 22.Charts for functional evaluation of the hand. 4th ed. Nagoya: Japanese Society for Surgery of the Hand; 2006. pp. 14–5. [Google Scholar]
- 23.Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000;25:3186–91. doi: 10.1097/00007632-200012150-00014. [DOI] [PubMed] [Google Scholar]
- 24.Fukuhara S, Bito S, Green J, Hsiao A, Kurokawa K. Translation, adaptation, and validation of the SF-36 health survey for use in Japan. J Clin Epidemiol. 1998;51:1037–44. doi: 10.1016/S0895-4356(98)00095-X. [DOI] [PubMed] [Google Scholar]
- 25.Liang MH, Fossel AH, Larson MG. Comparisons of five health status instruments for orthopedic evaluation. Med Care. 1990;28:632–42. doi: 10.1097/00005650-199007000-00008. [DOI] [PubMed] [Google Scholar]
- 26.Kazis LE, Anderson JJ, Meenan RF. Effect sizes for interpreting changes in health status. Med Care. 1989;27(suppl):S178–89. doi: 10.1097/00005650-198903001-00015. [DOI] [PubMed] [Google Scholar]
- 27.McHorney CA, Tarlov AR. Individual-patient monitoring in clinical practice: are available health status surveys adequate? Qual Life Res. 1995;4:293–307. doi: 10.1007/BF01593882. [DOI] [PubMed] [Google Scholar]
- 28.Suzukamo Y, Fukuhara S, Kikuchi S, Konno S, Roland M, Iwamoto Y, et al. Committee on Science Project, Japanese Orthopaedic Association. Validation of the Japanese version of the Roland-Morris Disability Questionnaire. J Orthop Sci. 2003;8:543–8. doi: 10.1007/s00776-003-0679-x. [DOI] [PubMed] [Google Scholar]
- 29.Beaton DE, Katz JN, Fossel AH, Wright JG, Tarasuk V. Measuring the whole or the parts? Validity, reliability, and responsiveness of the Disabilities of the Arm, Shoulder and Hand outcome measure in different regions of the upper extremity. J Hand Ther. 2001;14:128–46. [PubMed] [Google Scholar]
- 30.Gay RE, Amadio PC, Johnson JC. Comparative responsiveness of the Disabilities of the Arm, Shoulder, and Hand, the carpal tunnel questionnaire, and the SF-36 to clinical change after carpal tunnel release. J Hand Surg [Am] 2003;28:250–4. doi: 10.1053/jhsu.2003.50043. [DOI] [PubMed] [Google Scholar]