Abstract
Background
The outcome after displaced intra-articular calcaneal fractures is influenced by the condition of the surrounding soft tissues. To avoid secondary soft tissue complications after surgical treatment, several less-invasive procedures for reduction and fixation have been introduced. The percutaneous technique according to Forgon and Zadravecz is suitable for all types of displaced intra-articular calcaneal fractures and was therefore introduced in our clinic. The aim of this study was to evaluate the long-term outcome of percutaneous treatment according to Forgon and Zadravecz in patients with displaced intra-articular calcaneal fractures.
Methods
A cohort of patients with displaced intra-articular calcaneal fractures treated with percutaneous surgery was retrospectively defined. Clinical outcome was evaluated by standardized physical examination, radiographs, three published outcome scores, and a visual analogue scale of patient satisfaction.
Results
Fifty patients with 61 calcaneal fractures were included. After a mean follow-up period of 35 months, the mean values of the Maryland foot score, the Creighton-Nebraska score, and the American Orthopaedic Foot and Ankle Society score were 79, 76, and 83 points out of 100, respectively. The average visual analogue scale was 7.2 points out of 10. The average range of motion of the ankle joint was 90% of normal and subtalar joint movements were almost 70% compared with the healthy side or normal values. Superficial wound complications occurred in seven cases (11%) and deep infections in two (3%). A secondary arthrodesis of the subtalar joint was performed in five patients and was scheduled in four patients (15%).
Conclusions
Compared with the outcome of historic controls from randomized trials and meta-analyses, this study indicates favorable results for the percutaneous technique compared with the open technique. Despite similar rates of postoperative infection and secondary arthrodesis, the total outcome scores and preserved subtalar motion are overall good to excellent.
Introduction
Owing to their complexity and the diverse treatment options, displaced intra-articular calcaneal fractures remain a therapeutic challenge. The clinical evidence supporting operative treatment for selected patient groups is limited, whereas long-term complications and adverse outcomes are frequently documented.1–3 One of the adverse effects of operative treatment is secondary damage to soft tissues after extensive surgical procedures. To avoid soft tissue complications, several less-invasive procedures have been introduced. The most frequently used minimally invasive technique for the tonguetype fracture was proposed by Westhues in 1935, modified by Gissane, and propagated by Essex-Lopresti.4 In 1983 Forgon and Zadravecz introduced a new minimally invasive technique using an external distractor applied percutaneously, followed by percutaneous fixation.5,6 This technique applies the principle of distraction-reduction (ligamentotaxis) of the fracture fragments and is suitable for all types of intra-articular fractures.7
The aim of this study was to evaluate the long-term outcome of percutaneous treatment according to Forgon and Zadravecz in patients with displaced intraarticular calcaneal fractures.
Patients and methods
Patient selection
A study cohort was retrospectively defined to include all patients with displaced intra-articular calcaneal fractures treated according to Forgon and Zadravecz5,6 over a 5-year period at our institution. Approval for the study was obtained from the Institutional Reviewing Board (IRB). Patients who died (n = 2), had a spinal cord lesion (n = 1), moved to a foreign country (n = 4), or whose addresses were unknown (n = 5) were excluded. After a follow-up period of at least 12 months (mean 35 months, range 13–75 months), patients were interviewed after informed consent was given and were evaluated for their functional outcome. Patients who had undergone secondary subtalar arthrodesis in the follow-up period were considered to have had a poor outcome for the primary surgery.
Surgical procedure
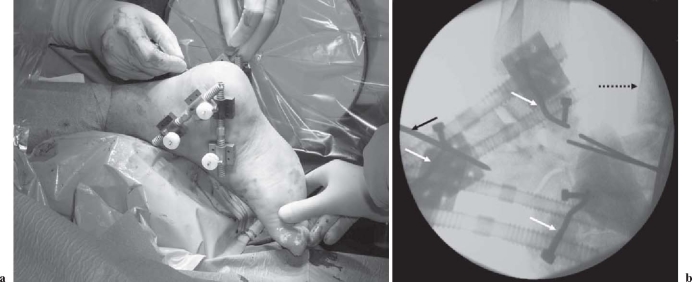
Surgical treatment according to the technique described by Forgon and Zadravecz5,6 with three minor modifications was carried out by three staff trauma surgeons. The patient was placed in the prone position and received spinal analgesia and antibiotic prophylaxis prior to the operation. Two fluoroscopes were installed to provide imaging in two orthogonal planes. Three 3-mm Kirschner wires were inserted from the lateral side through the calcaneal tuberosity, the cuboid, and the talar neck. The first modification concerned the placement of the distractors. These were positioned on both sides of the foot between the tuberosity of the calcaneus and talus and between the tuberosity and cuboid. Zadravecz et al. placed the latter between the cuboid and talus (Fig. 1). Through the distracting force generated between the three pins, the tuber angle of Böhler can be restored. The second modification concerned the insertion of a blunt drifter introduced from the plantar side to unlock and push up any remaining depressed parts of the subtalar joint surface of the calcaneus; Forgon and colleagues used pin leveraging from the lateral side to manipulate these fragments. The third modification was the discarding of the Böhler bone press to reduce the width of the fractured calcaneus. When an acceptable reduction was achieved, two Kirschner wires or two cancellous screws were inserted from the posterior aspect of the tuberosity. If necessary, a third screw was inserted from the lateral side of the calcaneus toward the sustentaculum tali to reduce bulging of the lateral wall. Postoperatively, patients remained non-weight-bearing for 3 months.
Fig. 1.
a Medial and lateral distractor in place during percutaneous surgery. b Fluoroscopic image showing the distractor and the osseous structures of the foot. The white arrows show the three Kirschner wires for distraction in the calcaneal tuberositas, the talus, and the cuboid. The black solid arrow shows a Kirschner wire inserted posteriorly for fixation. The black dotted arrow shows the contralateral foot in which the calcaneal fracture has already been distracted and fixated with two Kirschner wires
Functional outcome
Patients completed three questionnaires: the Maryland foot score (MFS), the Creighton-Nebraska (CN) score, and the American Orthopaedic Foot and Ankle Society (AOFAS) hindfoot score.8–10 A modified visual analogue scale (VAS) was used to measure patient satisfaction on a scale of 1–10. Patients with a bilateral fracture completed the questionnaire for the foot with the most complaints and functional disability.6 For the purposes of comparison, the AOFAS scores were divided into the same groups used for the MFS: a score of 90–100 was graded as an excellent result; 75–89 as good; 50–74 as fair, and less than 49 points was graded as a failure.11,12 This differed slightly from the CN score, in which an excellent score is 90–100; good is 80–89; fair is 65–79, and poor is a score of less than 64 points.8
Physical examination
Physical assessments (walking ability on heels and toes, heel width, calf circumference, stability and alignment of the heel) were performed in the outpatient clinic by the investigator (TS). The ranges of motion of the ankle and the subtalar joint were measured according to the Association for Osteosynthesis (AO) neutral zero method. The subtalar range of motion was measured with patients sitting on their knees to measure only the subtalar joint motion.13 In patients with unilateral fractures, these measurements were compared with the values of the uninjured foot and ankle. In patients with bilateral fractures, standard normal values according to McMaster were used (inversion of 25° and 5° of eversion).14 The mean normal sagittal (flexion and extension) range of motion of the ankle joint was set at 60°.13
Radiographic data
The preoperative radiographs and computed tomography (CT) scans were classified according to the classifications of Essex-Lopresti and Sanders, respectively, the latter without the use of subclasses.10,15 Immediately after the operation, radiographs in the lateral and axial plane were obtained to show the status of fracture reduction. At the time of inclusion in this study additional weight-bearing lateral, axial, and 45° inverted foot (Anthonson) views of the calcaneocuboid joint were obtained for both feet. The angles of Böhler and Gissane on preoperative and immediate postoperative radiographs were compared with the follow-up values and with normal values in patients with a unilateral fracture.15,16 The length, height, and width of the calcaneus were measured on the radiographs. The Zwipp score was used, in which the osteoarthrosis of the ankle joint, subtalar joint, and the calcaneocuboid joint, together with the difference in the Böhler’s angle were scored.17,18 A radiographic score of less than 6 points was considered a poor result, 7–8 points fair, 9–10 a good result, and 11–12 points an excellent result.18 All radiographs were evaluated together with a radiologist.
Results
A total of 59 patients with 71 fractures were considered for analysis. Nine patients refused to participate (Fig. 2). The remaining 50 patients, with a total of 61 fractures, showed a mean time from trauma to operation of 5 days (range 0–17 days) and a mean hospital stay of 8 days (range 1–77 days). The trauma mechanism was a traffic accident in 8 patients and a fall from height in 42 patients. In the latter group, 16 patients fell from stairs or a ladder and 5 had attempted suicide. A total of 60 additional injuries were found in 46% of the patients, of which ten patients had vertebral fractures. The patient demographics and fracture characteristics are shown in Table 1. Forty-two patients were seen at the outpatient clinic; eight did not attend but completed the questionnaire at home.
Fig. 2.
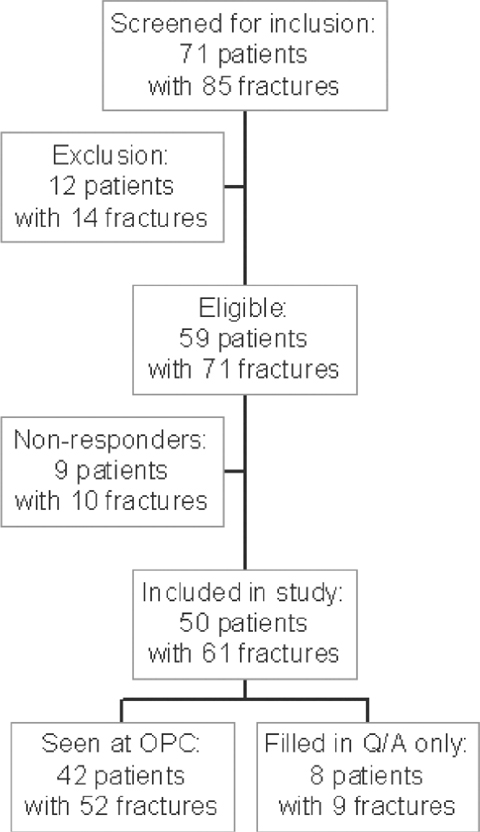
Flowchart showing the process of inclusion of patients in the study. OPC, outpatient clinic; Q/A, questionnaires
Table 1.
Patient demographics and fracture characteristics of 50 patients with 61 fractures
| Sex | |
| Male | 36 (72%) |
| Female | 14 (28%) |
| Age (years) | 46 (range 16–65) |
| Fracture side | |
| Right | 21 (42%) |
| Left | 18 (36%) |
| Bilateral | 11 (22%) |
| Soft tissue | |
| Closed | 57 (93%) |
| Open | 4 (7%) |
| Essex-Lopresti classification | |
| Joint depression | 23 (38%) |
| Tongue type | 9 (15%) |
| Comminuted | 27 (44%) |
| Unknown | 2 (3%) |
| Sanders classification | |
| Type II | 23 (38%) |
| Type III | 17 (28%) |
| Type IV | 17 (28%) |
| Unknown | 4 (6%) |
| Calcaneocuboid joint involvement | |
| Yes | 27 (44%) |
| No | 29 (48%) |
| Unknown | 5 (8%) |
For fractures where radiographs or computed tomography scans could not be traced, the fracture classification is documented as unknown
Infectious complications
The complications related to the fractured calcaneus or the operation were collected from medical records and the visits to the outpatient clinic. Infectious complications occurred in 9 of 61 (15%) feet that had undergone an operation. Seven patients had a superficial wound infection that was treated conservatively with antibiotics or operatively by removal of hardware. Two patients developed a deep infection: one osteomyelitis and one pin tract infection. One patient had an impingement of the peroneal tendon.
Outcome
A total of five calcaneal fractures in five patients had been treated with a secondary (triple) arthrodesis and four patients had the procedure planned (total 9/61 feet; 15%) because of disabling residual pain. The five patients who had already undergone arthrodesis did not complete the questionnaire and were considered to have had a poor result from the primary treatment. The functional outcomes are presented in Table 2. A good to excellent result was found in 42% to 72% of patients, depending on the outcome score used. Patient satisfaction, as represented by the VAS, was on average 7.2 (range 0–10). Five patients (two who had already retired) did not reach the level of activity they enjoyed prior to the accident and were not working at the time of the follow-up. The other patients (90%) were able to work. Eighty-two percent of patients were able to wear normal shoes.
Table 2.
Outcome according to four scoring systems after percutaneous treatment of intra-articular calcaneal fractures
| Score | Average ± SD (n = 45) | Excellent (%, n = 50) | Excellent Good (%, n = 50) | Fair (%, n = 50) | Poor/failure (%, n = 50) |
|---|---|---|---|---|---|
| AOFAS | 83 ± 15 | 36 | 36 | 16 | 12 |
| MFS | 79 ± 16 | 28 | 32 | 24 | 16 |
| CN | 76 ± 17 | 18 | 24 | 28 | 30 |
| VAS | 7.2 ± 2 | — | — | — | — |
Average scores measured using different scoring systems for 45 patients not undergoing arthrodesis. The grouped outcomes include the five patients who underwent arthrodesis; these five patients were considered as having had a poor result for primary treatment
AOFAS, American Orthopaedic Foot and Ankle Society score; CN, Creighton-Nebraska score; MFS, Maryland foot score; VAS, visual analogue scale
Physical examination
The average sagittal range of motion of the ankle joint (plantar plus dorsiflexion) was 53° (range 25°–75°, n = 37), which represents 88% of the normal range of motion. The average range of motion of the subtalar joint was 20° (range 5°–40°), 67% of the normal value. There was an increase in heel width of almost 6% and a decrease in calf circumference of 5%. All feet showed a normal level of stability, and of the 61 fractured feet, 3 had a slight malalignment.
Radiographic evaluation
The results of the radiographic examination of the investigated feet at three different points in time are presented in Table 3. The Zwipp score for osteoarthritis was 8 points on average. A total of four patients scored 6 points or less, meaning a poor radiologic outcome.
Table 3.
Radiographic data at follow-up
| Parameters | Trauma (n = 61) | Postoperatively (n = 61) | Follow-up (n = 37) | Healthy side (n = 32) |
|---|---|---|---|---|
| Böler angle in degrees (SD) | −2 (16) | 19 (10) | 14 (12) | 31 (5) |
| Gissane angle in degrees (SD) | 116 (18) | 114 (12) | 113 (15) | 109 (9) |
| Height in mm (SD) | — | — | 47 (5) | 50 (3) |
| Length in mm (SD) | — | — | 82 (5) | 83 (5) |
| Width in mm (SD) | — | — | 46 (5) | 40 (3) |
Radiological follow-up data at the time of trauma, immediate postoperatively, and after a mean follow-up of 35 months. All measurements were compared in patients with unilateral fractures without arthrodesis
Discussion
Various percutaneous and minimally invasive techniques have been introduced because of the skin and wound complications associated with open surgical techniques for the treatment of intra-articular calcaneal fractures. Forgon and Zadravecz combined several lessinvasive techniques for percutaneous reduction and fixation through the use of an external distractor.4–6,19 In this study, the outcome of the percutaneous treatment according to Forgon and Zadravecz of patients with a displaced intra-articular calcaneal fracture was evaluated over the long term.
Patients in this study achieved a good to excellent result in 42% to 72% of cases, according to the use of three different outcome scores. The range of motion of the ankle joint was nearly normal, and the range of motion of the subtalar joint was approximately 70% compared with the uninjured side.
A limitation of this study is the absence of a control group treated with a different method. In the level-1 setting where the study was conducted, no other technique was implemented, thus removing the possibility of a concurrent control group. Migrants, the homeless, and patients receiving psychiatric treatment were mostly lost to follow-up; however, their fracture characteristics and patient characteristics were not significantly different from the patients analyzed. Murhagnan showed an equivalent level of patients lost to follow-up, however they found that the attenders and nonattenders in a calcaneal fracture trial constituted two significantly different groups. It is therefore not prudent to extrapolate the results of this study to all patients who were treated in the study period; this constitutes a second limitation.20 The largest published series of patients treated with the percutaneous distractor method comprised 265 cases and presented good to excellent results in approximately 85% of patients.21 Differences in study parameters and outcome scores make it difficult to compare the results as presented by Forgon and Zadravecz and those of this study.
The functional results presented in this study appear to be slightly less favorable than those reported for open reduction and internal fixation (ORIF) groups in the literature, but appear to be better than those for conservatively treated patients.10,19,22,23 The infection and wound complication rates in this study appear similar to those of ORIF and the infections that occurred at the insertion site of the traction pins were not severe. Historically complication rates as high as 30%–40% have been reported for ORIF. Reports from the last 5 to 10 years show a superficial skin infection or wound dehiscence rate of about 10%. Deep infections such as osteomyelitis occur at a lower rate.24,25 The largest prospective, randomized multicenter study of Buckley et al. in 2002 showed a superficial infection and wound complication rate of 17% and a deep infection rate of 5% for ORIF.2
With a 15% arthrodesis rate, our study results appear more favorable than those for conservatively treated patients, but less favorable than for open reduced and fixated fractures.2 Buckley et al. showed that the need for arthrodesis was 4% in the ORIF group versus 20% in the conservatively treated group.2
Many studies point out restrictions at the subtalar joint for both surgically and conservatively treated fractures. The average range of motion is approximately halved compared with the uninjured foot.26 The more favorable results presented in this study are supported by the findings of other authors.27 The percutaneous approach minimizes secondary trauma to the soft tissues, which may lead to less scar tissue formation around the ankle and subtalar joint and may thus lead to less stiffness of the joint.19
In conclusion, this study confirms that the function of the calcaneus and subtalar joint can be restored by percutaneous reduction and fixation in patients with a displaced intra-articular calcaneal fracture. Despite similar infectious complication rates and higher secondary arthrodesis rates compared with open procedures, the good outcome scores and the preservation of the subtalar range of motion at 3-year follow-up indicate little benefit of open procedures, as reported in the literature, over percutaneous reduction and fixation.
References
- 1.Randle JA, Kreder HJ, Stephen D, Williams J, Jaglal S, Hu R. Should calcaneal fractures be treated surgically? A metaanalysis. Clin Orthop. 2000;377:217–27. doi: 10.1097/00003086-200008000-00029. [DOI] [PubMed] [Google Scholar]
- 2.Buckley R, Tough S, McCormack R, Pate G, Leighton R, Petrie D, et al. Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures: a prospective, randomized, controlled multicenter trial. J Bone Joint Surg Am. 2002;84:1733–44. doi: 10.2106/00004623-200210000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Bridgman SA, Dunn KM, McBride DJ, Richards PJ. Interventions for treating calcaneal fractures. Cochrane Database Syst Rev. 2000;2:CD001161. doi: 10.1002/14651858.CD001161. [DOI] [PubMed] [Google Scholar]
- 4.Tornetta P., III Percutaneous treatment of calcaneal fractures. Clin Orthop. 2000;375:91–6. doi: 10.1097/00003086-200006000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Forgon M, Zadravecz G. Die Kalkaneusfraktur. Berlin: Springer-Verlag; 1990. pp. 1–104. [Google Scholar]
- 6.Zadravecz G, Szekeres P. Late results of our treatment method in calcaneus fractures. Aktuelle Traumatol. 1984;14:218–26. [PubMed] [Google Scholar]
- 7.Gill GG. A three-pin method for treatment of severely comminuted fractures of os calcis. Surg Gynecol Obstet. 1944;78:653–6. [Google Scholar]
- 8.Crosby LA, Fitzgibbons T. Computerized tomography scanning of acute intra-articular fractures of the calcaneus. A new classification system. J Bone Joint Surg Am. 1990;72-6:852–9. [PubMed] [Google Scholar]
- 9.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349–53. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 10.Sanders R, Fortin P, DiPasquale T, Walling A. Operative treatment in 120 displaced intraarticular calcaneal fractures. Results using a prognostic computed tomography scan classification. Clin Orthop. 1993;290:87–95. [PubMed] [Google Scholar]
- 11.Follak N, Merk H. The benefit of gait analysis in functional diagnostics in the rehabilitation in patients after operative treatment of calcaneal fractures. Foot Ankle Surg. 2003;9:209–14. doi: 10.1016/S1268-7731(03)00092-4. [DOI] [Google Scholar]
- 12.Ebraheim NA, Elgafy H, Sabry FF, Freih M, Abou-Chakra IS. Sinus tarsi approach with trans-articular fixation for displaced intra-articular fractures of the calcaneus. Foot Ankle Int. 2000;21:105–13. doi: 10.1177/107110070002100203. [DOI] [PubMed] [Google Scholar]
- 13.Ryf C, Weymann A. The neutral zero method. A principle of measuring joint function. Injury. 1995;26(Suppl 1):1–11. doi: 10.1016/0020-1383(95)90116-7. [DOI] [Google Scholar]
- 14.Sarrafian SK. Biomechanics of the subtalar joint complex. Clin Orthop. 1993;290:17–26. [PubMed] [Google Scholar]
- 15.Essex-Lopresti P. The mechanism, reduction technique and results in fractures of the os calcis. Br J Surg. 1952;39:395–419. doi: 10.1002/bjs.18003915704. [DOI] [PubMed] [Google Scholar]
- 16.Böhler L. Diagnosis, pathology and treatment of fractures of the os calcis. J Bone Joint Surg. 1931;13:75–89. [Google Scholar]
- 17.Kennedy JG, Jan WM, McGuinness AJ, Barry K, Curtin J, Cashman WF, et al. An outcomes assessment of intra-articular calcaneal fractures using patient and physician’s assessment profiles. Injury. 2003;34:932–6. doi: 10.1016/S0020-1383(03)00025-1. [DOI] [PubMed] [Google Scholar]
- 18.Siebert CH, Hansen M, Wolter D. Follow-up evaluation of open intra-articular fractures of the calcaneus. Arch Orthop Trauma Surg. 1998;117:442–7. doi: 10.1007/s004020050289. [DOI] [PubMed] [Google Scholar]
- 19.Gavlik JM, Rammelt S, Zwipp H. Percutaneous, arthroscopically-assisted osteosynthesis of calcaneus fractures. Arch Orthop Trauma Surg. 2002;122:424–8. doi: 10.1007/s00402-002-0397-4. [DOI] [PubMed] [Google Scholar]
- 20.Murnaghan ML, Buckley RE. Lost but not forgotten: patients lost to follow-up in a trauma database. Can J Surg. 2002;45:191–5. [PMC free article] [PubMed] [Google Scholar]
- 21.Forgon M. Closed reduction and percutaneous osteosynthesis: technique and results in 265 calcaneal fractures. In: Tscherne H, Schatzker J, editors. Major fractures of the pilon, the talus, and the calcaneus. New York: Springer-Verlag; 1993. pp. 207–13. [Google Scholar]
- 22.Heier KA, Infante AF, Walling AK, Sanders RW. Open fractures of the calcaneus: soft-tissue injury determines outcome. J Bone Joint Surg Am. 2003;85:2276–82. [PubMed] [Google Scholar]
- 23.Leung KS, Yuen KM, Chan WS. Operative treatment of displaced intra-articular fractures of the calcaneum. Medium-term results. J Bone Joint Surg Br. 1993;75:196–201. doi: 10.1302/0301-620X.75B2.8444936. [DOI] [PubMed] [Google Scholar]
- 24.Lim EVA, Leung JPE. Complications of intraarticular calcaneal fractures. Clin Orthop. 2001;391:7–16. doi: 10.1097/00003086-200110000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Abidi NA, Dhawan S, Gruen GS, Vogt MT, Conti SF. Wound-healing risk factors after open reduction and internal fixation of calcaneal fractures. Foot Ankle Int. 1998;19:856–61. doi: 10.1177/107110079801901211. [DOI] [PubMed] [Google Scholar]
- 26.Barei DP, Bellabarba C, Sangeorzan BJ, Benirschke SK. Fractures of the calcaneus. Orthop Clin North Am. 2002;33:263–85. doi: 10.1016/S0030-5898(03)00084-1. [DOI] [PubMed] [Google Scholar]
- 27.Kingwell S, Buckley R, Willis N. The association between subtalar joint motion and outcome satisfaction in patients with displaced intraarticular calcaneal fractures. Foot Ankle Int. 2004;25:666–73. doi: 10.1177/107110070402500912. [DOI] [PubMed] [Google Scholar]