Abstract
Antibodies against prothrombin are detected by enzyme immunoassays (EIA) in sera of patients with antiphospholipid syndrome (APS). However, there are two methods for antiprothrombin EIA; one that uses high binding plates (aPT-A), and another that utilizes phosphatidylserine bound plates (aPS/PT). We aimed to evaluate and compare aPT-A and aPS/PT in a clinical setting. We performed EIA for anti-PT, anti-PS/PT, IgG, and IgM anticardiolipin antibodies (aCL), and IgG β2-glycoprotein I-dependent aCL (aβ2GPI/CL) with serum samples from 139 systemic lupus erythematosus (SLE) patients (16 with history of at least one thrombotic episode) and 148 controls. We observed that: (1) although titers of anti-PT and anti-PS/PT were significantly related with each other (P < 0.0001, ρ = 0.548), titer of anti-PT and anti-PS/PT differed greatly in some samples; (2) odds ratio and 95% confidence interval for each assay was 3.556 (1.221–10.355) for aPT-A, 4.591 (1.555–15.560) for aPS/PT, 4.204 (1.250–14.148) for IgG aCL, 1.809 (0.354–9.232) for IgM aCL, and 7.246 (2.391–21.966) for aβ2GPI/CL. We conclude that, while all EIA performed in this study except IgM aCL are of potential value in assessing the risk of thrombosis, aPS/PT and aβ2GPI/CL seemed to be highly valuable in clinical practice, and that autoantibodies detected by anti-PT and anti-PS/PT are not completely identical.
Key words: Antiphospholipid syndrome, Antiprothrombin antibody, Enzyme immunoassay, Systemic lupus erythematosus (SLE)
Introduction
Antiphospholipid antibodies (aPL) are a group of heterogeneous autoantibodies against a variety of phospholipid binding proteins. Detection of aPL by radioimmunoassay was first reported by Harris et al.,1 and detection of anticardiolipin antibody (aCL) by enzyme immunoassay (EIA) was reported by Koike et al. in 1984.2 The development of these relatively simple methods enabled researchers to perform a number of clinical studies, and the clinical entity antiphospholipid syndrome (APS), proposed by Hughes et al., was established during the 1980s. This syndrome is characterized by the presence of aPL and occurrence of thrombotic episodes and/or intrauterine fetal deaths.
Methods currently used for detecting aPL can be divided to two categories: lupus anticoagulant (LAC) tests and EIA. Enzyme immunoassays are frequently used for detection of aPL, due to their relative simplicity and reliability. A standardized aCL EIA, described by Harris et al.,3 is widely used for detection of aPL and the diagnosis of APS. However, during the last decade it has become evident that anticardiolipin antibodies are in fact autoantibodies against phospholipid binding proteins. The first such protein described is β2-glycoprotein I (β2GPI). It is suggested that β2GPI undergo a conformational change upon binding to negatively charged phospholipids, which in turn causes exposure of neoepitopes that are detected by aCL. Alternatively, the density of β2GPI may be important for recognition by aCL, and appropriate β2GPI density is achieved by binding to negatively charged phospholipids. Enzyme immunoassay for detection of β2GPI dependent aCL is reported to be of value in clinical practice4–6 and is included in the proposed Sapporo criteria for classification of APS.7 Enzyme immunoassays using β2GPI directly coated on oxidized plates (high binding plates) are also reported to be useful.8–12
Prothrombin is another important autoantigen recognized by aPL. Shortly after the description of β2GPI as the aCL “cofactor,”13–15 Bevers et al.16 reported that the IgG with LAC activity recognizes a complex of phospholipids and prothrombin. Thereafter, a number of studies with regard to the relationship between thrombotic events and presence of antiprothrombin antibodies as measured by EIA have been reported, with conflicting conclusions.17 Interestingly, two methods for antiprothrombin antibody detection have been suggested, similar to the case for anti-β2GPI detection. One is an assay that utilizes prothrombin coated directly onto high binding plates (in this paper referred to as aPT-A), and the other is an assay that detects antibodies bound to prothrombin on phosphatidylserinecoated plates (in this paper referred to as aPS/PT). The large differences in the results among the reports that studied the relevance of antiprothrombin EIA may partly be due to the methods of the EIA employed in individual studies. However, very few studies have directly compared the aPT-A and the aPS/PT assays.18,19
In this study, we aimed to compare these two antiprothrombin EIA, along with other aPL EIA (IgG and IgM aCL, IgG aβ2GPI/CL) and LAC, for their values in assessing the risk of thrombosis in patients with systemic lupus erythematosus (SLE). In particular, for all EIA, we measured the values of each antibody in our own healthy controls and have set the cutoff points anew to enable comparison of these assays from a same viewpoint.
Material and methods
Subjects and samples
Serum and plasma samples were taken from 139 SLE patients followed at University of Tsukuba Hospital, Tsukuba, Ibaraki, Japan. All SLE patients fulfilled the 1987 ACR criteria20,21 for the classification of SLE. Among these patients, 16 had one or more documented episodes of thrombosis (11 with arterial thromboses, 8 with venous thromboses, 3 with both arterial and venous thromboses). Mean follow-up period at the time of blood sampling was 9.95 ± 8.23 (mean ± SD) years; 9.00 ± 9.49 years for patients with history of thromboses, and 10.07 ± 8.09 years for patients without history of thromboses. Warfarin was started in 11 patients after diagnosis of thrombosis, and in a mean follow-up of 2.64 ± 2.87 years, no additional thrombotic episodes were noticed. Samples from 148 healthy volunteers, with no apparent history of thrombosis or autoimmune diseases, served as controls. Written informed consent was obtained from all subjects of this study, and the study was approved by the ethics committee of the University of Tsukuba.
Antiphospholipid antibody assays
Antiprothrombin antibodies measurement using high binding plates
Nunc Maxisorp plates (Nalge Nunc, Rochester, NY) were used. One hundred microliters per well (μl/well) of human prothrombin (Haematologica Technologies, Essex Junction, VT, USA) in carbonate buffer, pH 9.6, at a concentration of 10 μg/ml was coated onto wells at room temperature overnight. After blocking by 1% bovine serum albumin (BSA) in Tris-buffered saline including 5mM calcium (TBS), 100μl/well of sample sera diluted 1 : 200 in TBS with 1% BSA and 0.5% Tween-20 (TBS/Tw) were added to the wells, and the plates were incubated for 2h at room temperature. After washing with TBS/Tw, alkaline phosphatase labeled goat antihuman IgG antibody (American Qualex, SanClemente, CA, USA) diluted 1:2500 in TBS/Tw were added to the wells, and the plates were incubated for 1h at room temperature. After further washing, substrate was added and the optical density was measured at 405nM by an autoreader. A standard curve was always generated using a standard serum, the antibody concentration in which designated as 100 units/ml.
Anti-phosphatidylserine/prothrombin antibodies
For the measurement of aPS/PT, a commercially available EIA kit (Medical and Biological Laboratories, Nagoya, Japan)22 was used. The kit detects aPS/PT in the presence of calcium and follows, in principle, the method described by Atsumi et al.18 The wells of the plates are coated with phosphatidylserine/human prothrombin by the supplier. Sample sera were diluted at 1 : 100 with the supplied dilution buffer, and 100 μl of each sample were added to the wells. The plates were incubated for 1h at room temperature, and bound antibodies were detected by a peroxidase labeled goat anti-human IgG antibody.
Anticardiolipin antibodies
Anticardiolipin antibodies were measured according to the methods described by Harris et al.,3 using a Mesacup cardiolipin kit (Medical and Biological Laboratories) and a Mesacup cardiolipin IgM kit (Medical and Biological Laboratories).
Anticardiolipin/β2-glycoprotein I antibodies
Serum aβ2GPI/CL were measured using anticardiolipin/β2-glycoprotein I antibody enzyme-linked immunosorbent assay (ELISA) kit (Yamasa Shoyu, Chosi, Japan). The kit is supplied with plates coated with cardiolipin. The wells were first incubated with sample dilution buffer with or without β2GPI. Sample sera were diluted at 1 : 101 with the supplied dilution buffer, and 50μl /well of each sample was added to both the aβ2GPI added and non-added wells. Plates were incubated for 30 min at room temperature. Bound antibodies were detected by a peroxidase labeled anti-human IgG antibody. Samples were considered positive for aβ2GPI/CL when the values obtained from the β2GPI added wells exceeded the cutoff point, and were above the values obtained from β2GPI non-added wells.
Determination of cutoff levels for enzyme immunoassays
Although the cutoff levels for commercially available EIA tests are determined by the suppliers, the definition of a cutoff level differs among assays, and different control populations are used for the determination of each cutoff level in an assay. Therefore, to compare various assays from a same viewpoint, the cutoff levels for all EIA were determined anew. For all assays, the cutoff levels were set at mean + 2SD of our control samples.
Lupus anticoagulant assay
Lupus anticoagulant assay was performed using an LA test kit (Gradipore, North Ryde, Australia), which is based on a simplified dilute Russel viper venom time described by Exner et al.23 Ratios equal to or larger than 1.3 were considered positive for LA.
Statistical analyses
Relationships between the levels of EIA were compared by Spearman’s rank correlation test. Differences in titer of any aPL measured by EIA between SLE patients with history of thromboses and patients without such history were compared by the Mann-Whitney U-test. Positivity for any aPL assay and having histories of thromboses were compared by Fisher’s exact test. P values equal to or less than 0.05 were considered as statistically significant.
Results
Cutoff levels of enzyme immunoassays
The cutoff levels of all five EIA performed in this study were determined anew from the same 148 sample sera. The cutoff levels for aPT-A, aPS/PT, aβ2GPI/CL, IgG aCL, and IgM aCL assays were 17.95, 17.83, 0.57, 15.43, and 5.69, respectively. Values above these cutoff levels were considered positive for a given assay.
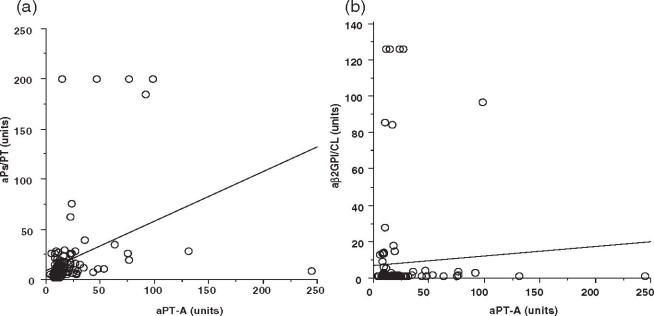
Titer of various antiphospholipid antibodies in SLE patients with or without history of thrombotic episodes
The levels of each EIA were compared between patients with history of thrombosis and those without thrombosis. In all assays, patients with history of thrombosis had signifi- cantly higher values compared to those without such history (Fig. 1). The differences observed between patients with or without thrombotic episodes seemed especially large in aPS/PT, although it is difficult to compare the assays in this way since the “unit” in each assay was defined independently among each other.
Fig. 1.
Values of antiphospholipid antibodies as measured by enzyme immunoassays in patients with systemic lupus erythematosus. One hundred and thirty-nine patients with systemic lupus erythematosus were divided into two groups (patients with or without history of thrombosis) and were applied to various antiphospholipid antibody enzyme immunoassays. Values are in arbitrary units determined independently for each enzyme immunoassay. Numbers above indicate P values calculated by Mann-Whitney U-test aPT-A, antiprothrombin antibody measured using high binding plates; aPS/PT, antiphosphatidylserine/prothrombin antibody; aCL, anticardiolipin antibody; aβ2GPI/CL, β2 glycoprotein I-dependent anticardiolipin antibody
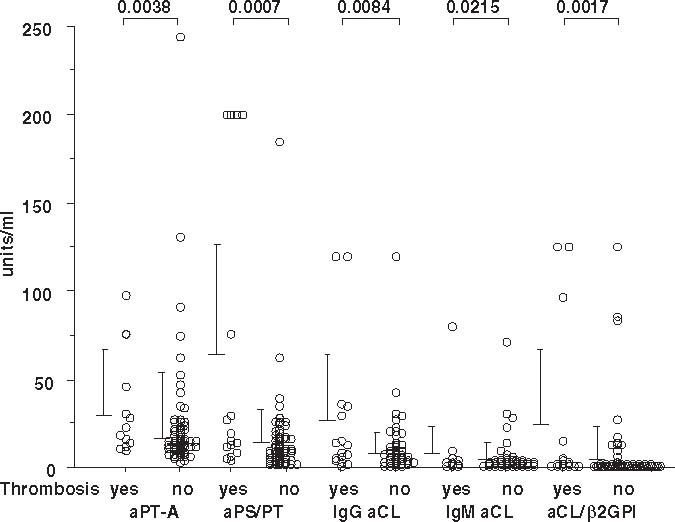
Results of antiprothrombin antibodies detected using high binding plates and those of antiphosphatidylserine/prothromnbin antibodies are significantly correlated with each other
It has been suggested that the values obtained by aPT-A and aPS/PT assays do not necessarily correlate with each other.18 We compared the values of aPT-A and aPS/PT among sera from SLE patients. These values were significantly correlated with each other (ρ = 0.514, P < 0.0001 by Spearman’s rank correlation), compared to relationships among other aPL such as between aPT-A and aβ2GPI/CL (Fig. 2 and results not shown). However, some sera had high value for only one or the other of those assays.
Fig. 2a,b.
Relationship between values of antiprothrombin antibody and antiphosphatidylserine/prothrombin antibody in sera of patients with systemic lupus erythematosus. The values of antiprothrombin antibody and antiphosphatidylserine/prothrombin antibody in patients with systemic lupus erythematosus were compared. For comparison, the values of antiprothrombin antibody and β2-glycoprotein I-dependent anticardiolipin antibody were also compared. a Antiprothrombin antibody and antiphosphatidylserine/prothrombin antibody. ρ = 0.514, P < 0.0001 by Spearman’s rank correlation. b Antiprothrombin antibody and β2 glycoprotein I-dependent anticardiolipin antibody. ρ = 0.086, P = 0.3103 by Spearman’s rank correlation. aPT-A, antiprothrombin antibody measured using high binding plates; aPS/PT, antiphosphatidylserine/prothrombin antibody; aβ2GPI/CL, β2 glycoprotein I-dependent anticardiolipin antibody
Positivity of antiphosphatidylserine/prothrombin antibody and/or antiprothrombin antibody is correlated with having histories of thrombotic episodes
Positivity for aPS/PT was significantly related with having history of thrombosis (Tables 1 and 2). aPT-A positivity was also significantly related with history of thrombosis.
Table1.
Relationshipbetweenpositivityofantiphospholipidassaysandhistoryofthrombosis
| Thrombosis | Total | Oddsratio | 95%CI | Pvalue | |||
|---|---|---|---|---|---|---|---|
| Yes | No | ||||||
| aPT-A | Positive | 8 | 27 | 35 | 3.556 | 1.221–10.355 | 0.0278 |
| Negative | 8 | 96 | 104 | ||||
| aPS/PT | Positive | 8 | 22 | 30 | 4.591 | 1.555–15.560 | 0.0072 |
| Negative | 8 | 101 | 109 | ||||
| aβ2GPI/CL | Positive | 10 | 23 | 33 | 7.246 | 2.39–21.966 | 0.0005 |
| Negative | 6 | 100 | 106 | ||||
| IgGaCL | Positive | 5 | 12 | 17 | 4.204 | 1.250–14.148 | 0.0282 |
| Negative | 11 | 111 | 122 | ||||
| IgMaCL | Positive | 2 | 9 | 11 | 1.809 | 0.354–9.232 | 0.6158 |
| Negative | 14 | 114 | 128 | ||||
| LAC | Positive | 7 | 9 | 16 | 9.852 | 2.972–32.657 | 0.0004 |
| Negative | 9 | 114 | 123 | ||||
aPT-A, antiprothrombin antibody measured using high binding plates; aPS/PT, antiphosphatidylserine/prothrombin antibody; aβ2GPI/CL, β2-glycoprotein I dependent anticardiolipin antibody; aCL, anticardiolipin antibody; LAC, lupus anticoagulant
Table 2.
Sensitivity, specificity, and positive predictive values of antiphospholipid assays for history of thromboses in patients with systemic lupus erythematosus
| Sensitivity | Specificity | Positive predictive value | |
|---|---|---|---|
| aPT-A | 0.500 | 0.775 | 0.229 |
| aPS/PT | 0.500 | 0.821 | 0.267 |
| aβ2GPI/CL | 0.625 | 0.813 | 0.303 |
| IgG aCL | 0.313 | 0.902 | 0.294 |
| IgM aCL | 0.125 | 0.927 | 0.182 |
| LAC | 0.438 | 0.927 | 0.438 |
aPT-A, antiprothrombin antibody measured using high binding plates; aPS/PT, antiphosphatidylserine/prothrombin antibody; aβ2GPI/CL, β2-glycoprotein I dependent anticardiolipin antibody; aCL, anticardiolipin antibody; LAC, lupus anticoagulant
Positivity of β2GPI-dependent aCL and/or lupus anticoagulant is significantly correlated with having histories of thrombotic events
When the cutoff level of aβ2GPI/CL was set at 3.5 units as recommended by the supplier, 17 were positive, among whom 5 had history of thrombotic episodes (P = 0.0282 by Fisher’s exact test). When the cutoff level was adjusted using data from our own healthy controls, a more significant relationship was observed (Tables 1 and 2). The OD values equivalent to 0.6 units were around 0.060–0.070 in the presence of β2GPI, and around 0.015–0.040 in the absence of β2GPI (not shown). Being positive for LAC was also significantly associated with history of thrombosis.
Relationships between conventional aCL assays, lupus anticoagulant assay, and history of thrombosis
The relationship between positivity of IgG aCL and history of thrombosis was statistically significant when the cutoff value was set at mean + 2SD of our control samples (Table 1). When the cutoff level was set at 10 units, originally set by the manufacturer, among the 31 patients positive for IgG aCL, 8 had history of one or more thrombosis episodes, yielding a P value of 0.0091 as calculated by Fisher’s exact test. No association between IgM aCL positivity and history of thrombosis was seen, regardless of whether the cutoff point was set at the values set by the manufacturer (1 of 7 positive patients with history of thrombosis, P = 0.5837 by Fisher’s exact test), or that set by ourselves (Table 1).
Positivity of antiphospholipid antibodies among SLE patients with history of thrombosis
The 16 SLE patients with history of thrombosis were assessed for their aPL positivity (Table 3). Thirteen patients were positive for at least one of the antiphospholipid antibody assays performed. While a combination of IgG aCL and LAC enabled us to judge 8 patients as positive for aPL, a combination of aPS/PT and aβ2GPI/CL indicated 10 as positive for aPL.
Table 3.
Positivity of antiphospholipid assays in patients with history of thrombosis
| Patient | Thrombosis | aPT-A | aPS/PT | aβ2GPI/CL | IgG aCL | IgM aCL | LAC |
|---|---|---|---|---|---|---|---|
| 1 | A | − | − | − | − | − | − |
| 2 | A | − | − | − | − | − | − |
| 3 | A | + | + | + | − | − | − |
| 4 | V | + | − | + | − | − | + |
| 5 | V | − | − | − | − | − | + |
| 6 | A,V | + | + | + | − | − | + |
| 7 | A | + | − | − | + | − | − |
| 8 | A | + | + | + | + | − | + |
| 9 | A | + | + | + | + | − | + |
| 10 | A | − | − | − | − | − | − |
| 11 | V | + | − | − | − | − | − |
| 12 | V | − | + | + | + | + | + |
| 13 | A,V | − | + | + | − | + | − |
| 14 | A | − | − | + | − | − | − |
| 15 | V | − | + | + | − | − | − |
| 16 | A,V | + | + | + | + | − | + |
A, with history of arterial thromboses; V, with history of venous thromboses; aPT-A, antiprothrombin antibody measured using high binding plates; aPS/PT, antiphosphatidylserine/prothrombin antibody; aβ2GPI/CL, β2-glycoprotein I-dependent anticardiolipin antibody; aCL, anticardiolipin antibody; LAC, lupus anticoagulant
Summary of thrombotic history: 1. Cerebral infarction (CI), occurring before diagnosis of systemic lupus erythematosus (SLE). No additional events with low-dose aspirin. 2. Left atrial thrombosis, found at the time of diagnosis of SLE. No recurrence with warfarin plus low-dose aspirin. 3. CI, occurring 21 years after diagnosis of SLE, while on low-dose aspirin. No further events after addition of warfarin. 4. Deep vein thrombosis (DVT) and pulmonary embolism (PE), occurring 3 years after diagnosis of SLE, while on low-dose aspirin. No further events after addition of warfarin. 5. PE found 2 years after diagnosis of SLE, while without any anticoagulation. Dipyridamole was added. Warfarin added 10 years after diagnosis of SLE to delay the progression of pulmonary hypertension. 6. Old lung infarction noticed 22 years after diagnosis of SLE, while under low-dose aspirin. No further episodes. 7. CI occurred 15 years before occurrence of SLE. 8. DVT occurred in the first year after diagnosis of SLE while under low-dose aspirin. Warfarin was added and no further episodes noticed. 9. PE, found 17 years after diagnosis of SLE while drug free. No episodes after addition of warfarin. 10. CI, occurring before diagnosis of SLE. 11. DVT, occurring 4 years after diagnosis of SLE. No recurrence after addition of warfarin. 12. DVT, found at the time of diagnosis of SLE. No recurrence after addition of warfarin and low-dose aspirin. 13. DVT, PE, both found at the time of diagnosis of SLE. No recurrence after addition of warfarin and low-dose aspirin. 14. Myocardial infarction occurring 24 years after diagnosis of SLE. CI found by further examination. No recurrence after low-dose aspirin and ticlopidine hydrochloride. 15. DVT, occurring 5 years after diagnosis of SLE while under no anticoagulation. No recurrence after addition of warfarin and low-dose aspirin. 16. CI, PE, both found at the time of diagnosis of SLE. No recurrence after addition of warfarin
Positivity of antiphospholipid antibodies among SLE patients with history of pregnancy
Among 69 SLE patients who had history of at least one pregnancy, only 3 had a history of recurrent fetal losses. Among patients with history of at least one pregnancy, the number of patients positive for a given antibody and with history of fetal loss, the number of patients of patients positive for the antibody, P values calculated by Fisher’s exact test were 2/16, 0.1321 for aPT-A, 1/17, >0.9999 for aPS/PT, 0/5, >0.9999 for IgG aCL, 0/4, >0.9999 for IgM aCL, 2/13, 0.0888 for aβ2GPI/CL, and 1/6, 0.2421 for LAC, respectively. For aβ2GPI/CL, when the cutoff value was set at 3.5 units, as determined by the supplier, the numbers became 2/8 and 0.0337. Other assays did not yield significant P values. However, the number of patients with history of recurrent fetal losses was too small to allow us to draw a reliable conclusion.
Discussion
Previous studies suggested that aPT-A and aPS/PT assays detect significantly different populations of autoantibodies and the results of the two assays may not correlate with each other. We applied the two assays to the same samples consisting of SLE patients and healthy individuals to assess the differences between the two assays. Results show that both assays, aPS/PT in particular, are of potential value in assessing the risk of thrombosis in SLE patients.
Very recently, Bertolaccini et al.19 also compared the results of aPT-A and aPS/PT in their cohort of 212 SLE patients. In their study they also found a significant relationship between the results of aPT-A and aPT/PS. Similar to our study, they also noted the presence of a number of patients with discrepant results. Thus, along with the results of our study, it is conceivable that aPT-A and aPT/PS recognize an overlapping, but not identical, population of autoantibodies. In their study, Bertolaccini et al. found a slightly stronger relationship between positivity of IgG aPS/PS and a history of thromboses than IgG aPT-A positivity and a history of thromboses. However, they have not documented how the aPS/PT-positive and aPT-A-positive patients overlap, when the presence of thrombotic history of thrombosis was put into consideration. In our study, between 8 aPT-Apositive SLE patients with a history of thrombosis and 8 aPS/PT-positive patients with a history of thrombosis, only 5 overlapped. These results could imply that performing both aPT-A and aPS/PT assays, if possible, or developing a new method that would enable detection of both populations of autoantibodies would be desirable for more sensitive detection of clinically relevant antiprothrombin antibodies. The reason why aPT-A and aPS/PT assays recognize overlapping, but not identical, populations of autoantibodies is not clear, but a most reasonable explanation would be that the nature of conformational changes introduced to prothrombin is different between when prothrombin is bound to high binding plates and when it is bound to phosphatidylserine bound plates. It is possible that the conformational changes introduced when bound to phosphatidylserine-coated plates is more similar to the changes introduced in vivo, and this may account for the higher clinical relevance of aPS/PT assay than that of aPTA assay observed in our study.
Assay for aβ2GPI/CL has become increasingly popular in the clinical management of SLE in Japan. The assay has been approved by the Ministry of Science Health and Welfare of Japan as a tool for diagnosis of APS. As seen in Table 1, positivity for this antibody was strongly correlated with histories of thrombosis, suggesting its value in a clinical setting. However, the cutoff value of aβ2GPI/CL in this study was set at 0.57 units, different from 3.5 units recommended by the manufacturer of the assay kit. In addition, the OD values at 0.6 units were around 0.060 in the assay we used. Thus, while setting the cutoff value at this level does give us a better P value, implying the validity of the assay, refinement of the assay would be necessary to more accurately measure low-titer aβ2GPI/CL. By standardizing the methodology and appropriately setting the cutoff levels, aβ2GPI/CL could become a more widely used measure for the diagnosis of APS. Efforts to standardize this assay are necessary. Previously, we have suggested24 that aβ2GPI/CL assays may be suitable to be included in the 1987 ACR criteria,20,21 which currently includes only LAC and conventional aCL assays as means of aPL detection. Results presented in this study imply that aβ2GPI/CL EIA has similar or superior value for the detection of aPL as IgG aCL. We believe that inclusion of aβ2GPI/CL in the ACR criteria for SLE may be beneficial.
Currently, the Sapporo criteria, proposed in 1999, are widely used for the diagnosis of APS.7 In the Sapporo criteria, for the detection of aPL, aCL, aβ2GPI/aCL, and LAC assays are recommended. However, studies reported thereafter have suggested the values of antiprothrombin assays in the diagnosis of APS. We wished to determine the values of aPT-A and aPS/PT in a clinical setting and in particular, wanted to determine whether routine measurement of these antibodies would aid in the diagnosis of APS. For this purpose, we decided to set the cutoff level of each EIA anew, to evaluate each assay from the same viewpoint. Among our 16 SLE patients with history of thrombosis, 8 were judged positive for aPL by the combination of IgG aCL and LAC. Addition of aβ2GPI/aCL raised the number of patients positive for aPL to 12, while addition of either aPT-A or aPS/PT raised the number to 11. A combination of aβ2GPI/aCL and aPS/PT judged 10 patients as positive for aPL, and a combination of aPT-A, aPS/PT, and aβ2GPI/aCL judged 12 as aPL-positive (Table 3). In our SLE patients, among the patients with history of thrombosis, all but one of those positive for LAC were positive for at least either aPS/PT or aβ2GPI/aCL. These results are quite reasonable since a large part, if not the majority, of LAC activity is β2GPI or prothrombin dependent. Refinement of these assays may show that these assays should have a position in the diagnostic criteria of APS, and that they have the potential to substitute LAC assays in the future. Although the clinical significance of LAC assays is well established, carefully collected and preserved plasma needs to be used, the methods are tedious and are still not completely standardized.
By directly comparing aPS/PT and aPT-A assays along with other aPL assays, using the same samples and the same criteria to set cutoff levels, our current study indicated that aPS/PT and aβ2GPI/aCL assays have more clinical relevance than the aPT-A assay. However, aPT-A assay seemed to be detecting a spectrum of autoantibodies not detected by aPS/PT, and we believe that it is premature to dismiss the assay as clinically meaningless.
In conclusion, we have shown the heterogeneity of autoantibodies detected by aPT-A or aPS/PT assays, but have also shown that these EIAs may be valuable in the diagnosis of APS. Although interlaboratory studies and standardization of the assays are necessary, we believe that these assays may have the potential to be included in the future diagnostic criteria for APS and SLE.
References
- 1.Harris EN, Gharavi AE, Boey ML, Patel BM, Mackworth-Young CG, Loizou S, et al. Anticardiolipin antibodies: detection by radioimmunoassay and association with thrombosis in systemic lupus erythematosus. Lancet. 1983;2:1211–4. doi: 10.1016/S0140-6736(83)91267-9. [DOI] [PubMed] [Google Scholar]
- 2.Koike T, Sueishi M, Funaki H, Tomioka H, Yoshida S. Anti-phospholipid antibodies and biological false positive serological test for syphilis in patients with systemic lupus erythematosus. Clin Exp Immunol. 1984;56:193–9. [PMC free article] [PubMed] [Google Scholar]
- 3.Harris EN, Gharavi AE, Patel SP, Hughes GR. Evaluation of the anti-cardiolipin antibody test: report of an international workshop held 4 April 1986. Clin Exp Immunol. 1987;68:215–22. [PMC free article] [PubMed] [Google Scholar]
- 4.Kaburaki J, Kuwana M, Yamamoto M, Kawai S, Matsuura E, Ikeda Y. Clinical significance of phospholipid-dependent anti-β2-glycoprotein I (β2-GPI) antibodies in systemic lupus erythematosus. Lupus. 1995;4:472–6. doi: 10.1177/096120339500400609. [DOI] [PubMed] [Google Scholar]
- 5.Kaburaki J, Kuwana M, Yamamoto M, Kawai S, Matsuura E, Ikeda Y. Phospholipid-dependent anti-β2-glycoprotein I (β2-GPI) antibodies and antiphospholipid syndrome. Intern Med. 1996;35:105–10. doi: 10.2169/internalmedicine.35.105. [DOI] [PubMed] [Google Scholar]
- 6.Aoki K, Dudkiewicz AB, Matsuura E, Novotny M, Kaberlein G, Gleicher N. Clinical significance of β2-glycoprotein I-dependent anticardiolipin antibodies in the reproductive autoimmune failure syndrome: correlation with conventional antiphospholipid antibody detection systems. Am J Obstet Gynecol. 1995;172:926–31. doi: 10.1016/0002-9378(95)90023-3. [DOI] [PubMed] [Google Scholar]
- 7.Wilson WA, Gharavi AE, Koike T, Lockshin MD, Branch DW, Piette JC, et al. International consensus statement on preliminary classification criteria for definite antiphospholipid syndrome: report of an international workshop. Arthritis Rheum. 1999;42:1309–11. doi: 10.1002/1529-0131(199907)42:7<1309::AID-ANR1>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 8.Martinuzzo ME, Forastiero RR, Carreras LO. Anti β2-glycoprotein I antibodies: detection and association with thrombosis. Br J Haematol. 1995;89:397–402. doi: 10.1111/j.1365-2141.1995.tb03317.x. [DOI] [PubMed] [Google Scholar]
- 9.Pengo V, Biasiolo A, Fior MG. Autoimmune antiphospholipid antibodies are directed against a cryptic epitope expressed when β2-glycoprotein I is bound to a suitable surface. Thromb Haemost. 1995;73:29–34. [PubMed] [Google Scholar]
- 10.Tsutsumi A, Matsuura E, Ichikawa K, Fujisaku A, Mukai M, Kobayashi S, et al. Antibodies to β2-glycoprotein I and clinical manifestations in patients with systemic lupus erythematosus. Arthritis Rheum. 1996;39:1466–74. doi: 10.1002/art.1780390905. [DOI] [PubMed] [Google Scholar]
- 11.Amengual O, Atsumi T, Khamashta MA, Koike T, Hughes GR. Specificity of ELISA for antibody to β2-glycoprotein I in patients with antiphospholipid syndrome. Br J Rheumatol. 1996;35:1239–43. doi: 10.1093/rheumatology/35.12.1239. [DOI] [PubMed] [Google Scholar]
- 12.Sanfilippo SS, Khamashta MA, Atsumi T, Amengual O, Bertolaccini ML, D’Cruz D, et al. Antibodies to β2-glycoprotein I: a potential marker for clinical features of antiphospholipid antibody syndrome in patients with systemic lupus erythematosus. J Rheumatol. 1998;25:2131–4. [PubMed] [Google Scholar]
- 13.Matsuura E, Igarashi Y, Fujimoto M, Ichikawa K, Koike T. Anticardiolipin cofactor(s) and differential diagnosis of autoimmune disease. Lancet. 1990;336:177–8. doi: 10.1016/0140-6736(90)91697-9. [DOI] [PubMed] [Google Scholar]
- 14.McNeil HP, Simpson RJ, Chesterman CN, Krilis SA. Anti-phospholipid antibodies are directed against a complex antigen that includes a lipid-binding inhibitor of coagulation: β2-glycoprotein I (apolipoprotein H) Proc Natl Acad Sci USA. 1990;87:4120–4. doi: 10.1073/pnas.87.11.4120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Galli M, Comfurius P, Maassen C, Hemker HC, de Baets MH, van Breda-Vriesman PJ, et al. Anticardiolipin antibodies (ACA) directed not to cardiolipin but to a plasma protein cofactor. Lancet. 1990;335:1544–7. doi: 10.1016/0140-6736(90)91374-J. [DOI] [PubMed] [Google Scholar]
- 16.Bevers EM, Galli M, Barbui T, Comfurius P, Zwaal RF. Lupus anticoagulant IgGs (LA) are not directed to phospholipids only, but to a complex of lipid-bound human prothrombin. Thromb Haemost. 1991;66:629–32. [PubMed] [Google Scholar]
- 17.Galli M, Luciani D, Bertolini G, Barbui T. Anti-β2-glycoprotein I, antiprothrombin antibodies, and the risk of thrombosis in the antiphospholipid syndrome. Blood. 2003;102:2717–23. doi: 10.1182/blood-2002-11-3334. [DOI] [PubMed] [Google Scholar]
- 18.Atsumi T, Ieko M, Bertolaccini ML, Ichikawa K, Tsutsumi A, Matsuura E, et al. Association of autoantibodies against the phosphatidylserine-prothrombin complex with manifestations of the antiphospholipid syndrome and with the presence of lupus anticoagulant. Arthritis Rheum. 2000;43:1982–93. doi: 10.1002/1529-0131(200009)43:9<1982::AID-ANR9>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 19.Bertolaccini ML, Atsumi T, Koike T, Hughes GR, Khamashta MA. Antiprothrombin antibodies detected in two different assay systems. Prevalence and clinical significance in systemic lupus erythematosus. Thromb Haemost. 2005;93:289–97. doi: 10.1160/TH04-06-0382. [DOI] [PubMed] [Google Scholar]
- 20.Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfield NF, et al. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1982;25:1271–7. doi: 10.1002/art.1780251101. [DOI] [PubMed] [Google Scholar]
- 21.Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1997;40:1725. doi: 10.1002/art.1780400928. [DOI] [PubMed] [Google Scholar]
- 22.Kaburaki J, Kuwana M, Uehara R, Ohya K. Development of ELISA kit to examine anti-phosphatidylserine/prothrombin complex antibodies (antiprothrombin antibodies) (in Japanese) Jpn J Med Pharm Sci. 2002;47:813–9. [Google Scholar]
- 23.Exner T, Papadopoulos G, Koutts J. Use of a simplified dilute Russell’s viper venom time (DRVVT) confirms heterogeneity among “lupus anticoagulants. Blood Coagul Fibrinolysis. 1990;1:259–66. doi: 10.1097/00001721-199008000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Tsutsumi A, Ichikawa K, Atsumi T, Matsuura E, Koike T, Krilis SA. Use of various methods for anticardiolipin detection in the updated American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus: comment on the letter by Hochberg. Arthritis Rheum. 1998;41:1326–7. doi: 10.1002/1529-0131(199807)41:7<1326::AID-ART29>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]