When humans became bipedal, shoulders began to suffer from various conditions because of their unique structure and function. More recently, lifestyle changes and sports participation have made the situation even more complicated. Both the young and old suffer from more shoulder problems than ever before.
Achievements by pioneers like Codman and his contemporaries in the first half of the twentieth century established shoulder surgery as a respectable subspecialty. Golding, in his 1961 lecture “The shoulder — the forgotten joint,”1 emphasized the importance of radiological examination despite the frequent absence of positive radiological findings in stiff and painful shoulders.
In the middle of the twentieth century, a wave of second-generation specialists was led by Neer and made progress on all fronts, especially in the field of arthroplasty. Giant steps forward took place in the 1980s when:
New imaging modalities and arthroscopy joined our armamentarium for diagnosis and treatment.
Multidisciplinary investigations became more commonplace in the basic scientific studies of “shoulderology.”
National, regional, and international organizations of shoulder surgery were formed, facilitating the exchange of expertise; e.g., The Journal of Shoulder and Elbow Surgery was launched in 1992.
The purpose of this article is to look back at the development of modern shoulder surgery and to look ahead to its future. In this review, we shall mention notable historic events and the auspicious articles of our specialty — milestones, so to speak. We would also like to discuss ways to develop shoulder surgery in the non-English-speaking world.
Codman and his contemporaries
Some 100 years ago, Ernest Amory Codman of Boston (Fig. 1) began his study of stiff and painful shoulders. There had been anatomical observations of the full-thickness tear of the rotator cuff, but he was the first, in 1909, to successfully operate in two cases, and to establish the condition as a definite entity. It is truly remarkable that he made the correct preoperative diagnosis based only on clinical findings.
Fig. 1.
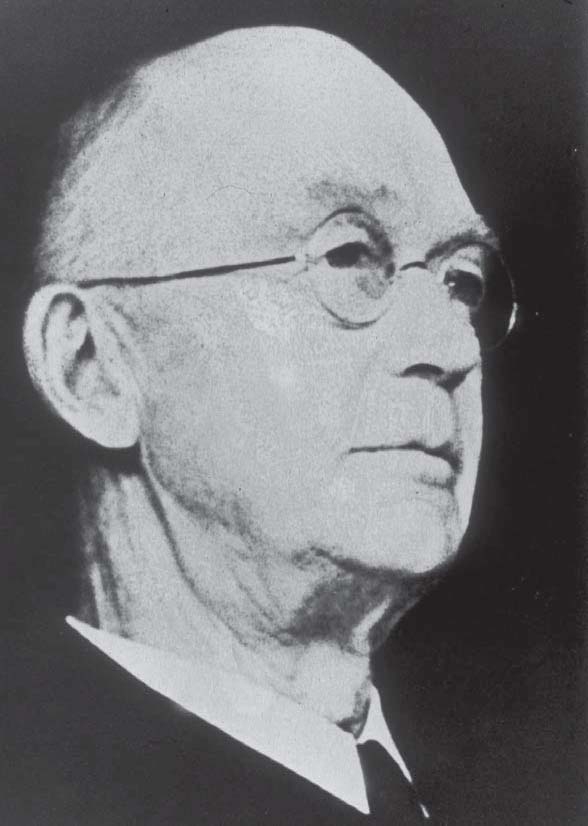
Ernest Amory Codman (1869–1940)
His life’s work is found in the book The Shoulder, published privately in 1934.2 It is the Bible, the Mount Everest, of modern shoulder surgery. In it, he (1) looked at the joint from anatomical, biomechanical, and pathological points of view and (2) analyzed all the categories of disorders, placing a special emphasis on the subacromial bursa and the supraspinatus tendon.
We all agree that this monumental opus has been the keystone from which all other works have evolved. In addition, he instituted the Bone Sarcoma Registry and also developed the end-result idea in clinical medicine (today’s evidence-based medicine), which was not kindly received by his Boston colleagues. His foresight was amazing: both ideas are now well accepted and practiced all over the world!
Codman’s career, philosophy, struggle, accomplishments, dreams, and even hobbies are best described by himself in “an autobiographic preface” and “an epilogue” of his book, encompassing 36 and 29 pages respectively.
Codman’s contemporaries made the following contributions:
Perthes (1906),3 in Germany, was the first to describe reattachment of the anterior labrum both with sutures and with staples in recurrent instability of the glenohumeral joint.
Bankart (1923),4 in the United Kingdom, popularized labral reattachment in the English-speaking world.
Lindblom (1939),5 in Sweden, introduced arthrography to the glenohumeral joint, which enabled us to diagnose evidentially the full-thickness tear of the rotator cuff. He stated that the idea of injecting contrast medium into the shoulder joint was suggested by Codman.
Bosworth (1940)6 and McLaughlin (1944),7 both in the United States, reported their surgical results on the rotator cuff tear. The latter described in detail reattachment of the retracted stump of the supraspinatus tendon more proximally, when necessary, than its anatomical facet on the greater tuberosity, which is now known as the McLaughlin advancement technique.
Neer and his contemporaries
In 1953 Charles S. Neer II (Fig. 2) published his first article8 on the humeral prosthesis for comminuted proximal humeral fractures, thus opening the door for the subsequent development of hemi- and total shoulder arthroplasty. In 1970 he advocated the “four-part” classification for proximal humeral fractures,9,10 which has direct implication in treatment because of the viability of the head fragment. The anterior acromioplasty for subacromial impingement syndrome (1972) was devised with the idea of decompressing the site responsible for impingement of the acromion and providing exposure for surgery, while minimizing morbidity of the deltoid function.11 The inferior capsular shift procedure was developed for multidirectional instability (1980); this procedure reduces the glenohumeral joint volume from all sides.12 All of this work is in the book Shoulder Reconstruction published in 1990.13
Fig. 2.
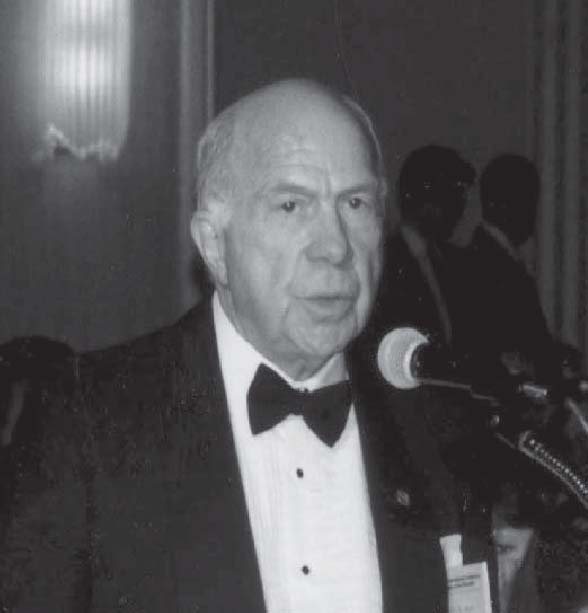
Charles S Neer II (1917–). Photograph was taken at the 4th ICSS in New York City in 1989
In addition, Neer devoted himself to propagating shoulder surgery as the Chair of the International Board of Shoulder Surgery (IBSS) from 1992 to 2001 and promoted publication of The Journal of Shoulder and Elbow Surgery as the first chair of its board of trustees from 1991 to 1994. He is truly the father of modern shoulder surgery.
Several of Neer’s contemporaries also wrote textbooks:
Moseley, Recurrent Dislocation of the Shoulder (1961)14 and Shoulder Lesions (3rd ed, 1969);15
Bateman, The Shoulder and Neck (2nd ed, 1978);16
DePalma, Surgery of the Shoulder (3rd ed, 1983);17
Rowe, The Shoulder (1988);18 and
Rockwood et al., The Shoulder (3rd ed, 2004).19
Rowe, in particular, studied instability of the shoulder from the 1950s to the 1980s; his publications cover areas ranging from the prognosis of the traumatic dislocation (1956),20 voluntary dislocation (1973),21 and the Bankart procedure (1978)22 to recurrent transient subluxation (1981).23
Saha (1961), in India, published the book The theory of shoulder mechanism: descriptive and applied24 in which he emphasized the importance of recognizing and applying the zero-position (vide infra) when treating unimpacted fractures of the neck of the humerus, separation of the proximal epiphysis of the humerus, and fractures of the upper third of the humeral shaft. The zero-position of the glenohumeral joint is defined as an abduction of 155° and a horizontal flexion of 45°, where there is minimum rotation, minimum active gliding of the joint surfaces, and circumduction. In this position, the humerus is neither internally nor externally rotated and its mechanical axis is in alignment with the scapular spine.
Uhthoff (1975) clarified calcifying tendonitis as an active, cell-mediated process, rather than a degenerative condition,25 as formerly believed. He organized the international course for rotator cuff disorders in Ottawa in 1988 and 1993, promoting relevant basic science.
New organizations and movements
The first international shoulder seminar was organized in 1963 by Moseley in Montreal; its papers were published in toto with a group photograph of the faculty (Fig. 3).26 Dr. Neer was the youngest.
Fig. 3.
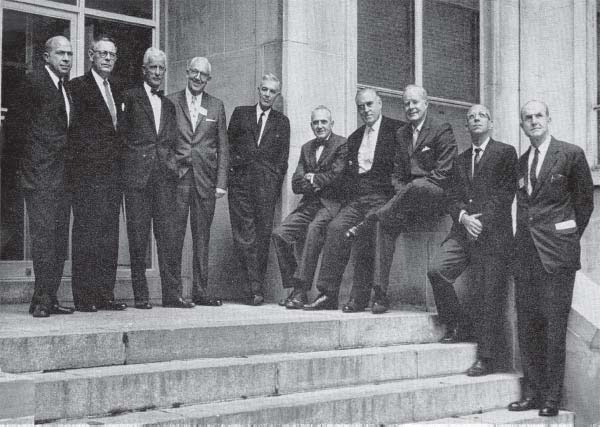
The faculty of the Symposium on Surgery of the Shoulder Region held in Montreal in 1963. Left to right: Charles S. Neer, II, M.D.; Thomas B. Quigley, M.D.; Professor R. Merle d’Aubigne; Julius S. Neviaser, M.D.; Harrison L. McLaughlin, M.D.; Alexander P. Aitken, M.D.; H. Fred Moseley, D.M.; James E. Bateman, M.D.; Anthony F. DePalma, M.D.; and Carter R. Rowe, M.D. Absent: Ernest Gardner, M.D. and John V. Basmajian, M.D. (Reproduced by permission from Surg Clin N Am 1963;43:1462. WB Saunders Company/Elsevier)
The Japan Shoulder Society (JSS) was established in 1974 as the first national body and now has 1253 enrollees, including 1199 regular, 33 executive, 19 honorary, and 2 supporting members (June 2006). The JSS started to publish its own journal in Japanese three times a year in 1977; English abstracts were added in 1983.
The first International Conference on Surgery of the Shoulder (ICSS) was organized by Kessel in London in 1980, which has subsequently been held every third year: Toronto (1983), Fukuoka (1986), New York (1989), Paris (1992), Helsinki/Stockholm (1995), Sydney (1998), Cape Town (2001) and Washington, DC, (2004). Incorporating elbow surgery, the ICSS became the International Conference on Surgery of the Shoulder and Elbow (ICSSE) in 2004. The future venues of ICSSE will be San Salvador in 2007 and Edinburgh in 2010.
The American Shoulder and Elbow Surgeons (ASES) was founded in 1982 and now has 279 members, including 116 active, 56 associate, 77 corresponding, 18 senior, 11 affiliate members, and 1 honorary member from 21 countries (March 2006).
The European Society for Surgery of Shoulder and Elbow (ESSSE) was formed in 1987, and currently has 342 members, with 177 regular, 155 associate, and 10 emeritus members from 22 countries (August 2006). The South African Shoulder and Elbow Surgeons (SASES) was established in 1990 and currently has 38 members (September 2006). The Shoulder and Elbow Society of Australia (SESA) was initiated in 1990.
The International Board of Shoulder Surgery (IBSS) was organized in 1992 to preside over international relations, especially in matters of the ICSS. The Chairs of the IBSS was Neer (1992–2001), followed by Cofield (2001–2004) and Copeland (2004–).
The concept of The Journal of Shoulder and Elbow Surgery (JSES) was formulated in 1990 by the ASES executive committee, and the publication was finally realized as the January/February 1992 issue with Cofield as its first Editor. It is peer-reviewed and is now the official journal of the ten national, regional, and international organizations, and has an extensive editorial network covering five continents.
The Asian Shoulder Association (ASA) was officially organized in 1993 and its first Congress was held in Taipei in 1994. The ASA is now represented by 74 members from 11 countries (August 2006). The Korean Shoulder and Elbow Society was established in 1993 and has 150 members (August 2006).
The South American Shoulder and Elbow Society (SASES) was inaugurated in 1994 at the initiative of the Brazilian Shoulder and Elbow Society, which was organized in 1988, as the first body of its kind in Latin America. SASES was renamed the Latin American Shoulder and Elbow Society in 2005, and now has approximately 1200 members from 13 countries (September 2006).
Accomplishments by category
Basic science
What is the role of basic science for practicing surgeons? It is to substantiate clinical impressions or hypotheses, and to bring the results of investigation from the lab bench to the bedside. Multidisciplinary methodologies have been applied to the basic science of “shoulderology,” including anatomy, histology, immunohistochemistry, imaging techniques, biomechanics, and computer science.
Outcome assessment is important in clinical care to compare the effectiveness of treatments. Codman introduced this concept in the early 1900s and the evaluation of shoulder and elbow surgery has been extensive over the past two decades.
The Constant Score is a joint-specific instrument for the shoulder, consisting of a 100-point scoring system in which 35 points are allocated for the patient’s reported pain and function and the remaining 65 points for the range of motion and strength. Age- and sex-matched normative data are available for the Score. Despite some drawbacks, such as having only one pain scale and nonstandardized strength testing, the Constant Score has been widely used since it was first reported in 1987.27 Further refinement is needed for the measurement properties of a number of outcome instruments in specific patient populations.
Inman et al.28 (1944) observed the function of the shoulder joint in the living body for the first time, inserting metallic markers into bones for measurements. They reported that once 30° of abduction, or 60° of flexion has been reached, the relationship of scapular to humeral motion remains remarkably constant at a ratio of 1 : 2. The recognition of the force-couple principle in the joint motion was also emphasized. Their study was a breakthrough in shoulder biomechanics. Meticulous microanatomical work on the rotator cuff by Clark and Harryman29 in 1992, and on the capsule of the glenohumeral joint by Gohlke et al.30 in 1994 are considered fundamental works and are often cited.
Instability
Endo et al.31 reported in 1971 on multidirectional instability (MDI) as “loose shoulder” in which the patients, often with multiple joint laxity, complained of recurrent motion pain and dullness in the shoulder girdle without apparent cause. The instability is characterized by the inferior subluxation of the shoulder joint when the upper extremity is allowed to droop or downward traction is applied to the forearm. The subluxation is readily reduced if the shoulder girdle muscles are strained. Considering the pathogenesis of the loose shoulder to be deficient strength in abduction and external rotation of the scapula, they performed transfer of a portion of the pectoralis major to the inferior angle of the scapula to add strength. Neer et al. recommended the inferior capsular shift procedure for involuntary inferior and MDI of the shoulder in 1980.12 They tried to reduce the capsular volume from all sides, considering this condition more three-dimensionally than Endo et al. did. The problem of MDI, however, has not been fully solved as yet.
In 1973, Rowe et al. published their comprehensive description of voluntary instability.21 In this classic study, patients with underlying psychiatric dysfunction did poorly with all types of treatment. For most patients, a rehabilitation program for muscle strength and coordination was recommended. In 1985, Kumar and Balasubramaniam, in Singapore, described the role of atmospheric pressure in stabilizing the shoulder in a cadaveric experiment.32
Regarding traumatic primary anterior dislocation of the shoulder, Rowe documented that the recurrence rates were dependent on the age of the patient at the time of the initial episode. In patients younger than 20 years of age, a 94% recurrence rate was observed; the figure becomes 79% in patients 21–30 years of age, 50% in patients 31–40 years of age, and 14% in patients over the age of 40.20 Hovelius et al.33 did a 10-year follow-up study on 257 patients younger than 40 years. At the 10-year follow-up, 48% of these patients had experienced recurrent dislocation and 23% required operative reconstruction. Their conclusions were that: (1) the recurrence rate was inversely correlated with the age at primary dislocation, (2) the rate of dislocation arthropathy was 20%, which was unrelated to the surgical treatment or number of recurrences, and (3) the effectiveness of the initial treatment had no effect on the recurrence rate.
Internal rotation with the arm at the side has been the position of immobilization after reduction of primary anterior dislocation. However, Itoi et al.34 have recently recommended the position of external rotation after reduction, which prevents the dislocation from recurring because of spontaneous healing of the injury. Their magnetic resonance imaging study revealed that, in external rotation, the avulsed anterior stabilizing mechanism (the anterior band of the inferior gleno humeral ligament and axillary pouch) was anatomically reduced by the tension of the subscapularis muscle, while the mechanism remained displaced in internal rotation. Their prospective, randomized, multicenter clinical trials indeed showed a decrease of the recurrence rate, and a long-term follow-up study is awaited.
Rotator cuff disease
In 1972 Neer,11 using cadaveric material, demonstrated variations in the shape and slope of acromions, and the presence of osteophyte formation in the acromial attachment of the coracoacromial ligament and on the undersurface of the anterior one-third of the acromion. He hypothesized that these anatomic variations and degenerative changes were important factors of repeated microtraumata to the critical portion of the supraspinatus tendon and the subjacent biceps tendon. Based on this impingement concept, anterior acromioplasty was introduced, and the results confirmed the importance of this subacromial impingement in the genesis and perpetuation of lesions of the rotator cuff and biceps tendon. If impingement continues, the pathologic process progresses from inflammation to fibrosis and eventually to tearing of the rotator cuff. During the last three decades, there were extensive studies35 on the diagnosis and pathogenesis of partial-thickness rotator cuff tears. Clarifying pathogenesis of the rotator cuff tear is much easier in partial-thickness than in full-thickness tears, just as the investigation of a fire is easier when a house is half burned than when it is totally destroyed.
Evidence has been accumulating that the pathogenesis of the rotator cuff tear is multifactorial and there is an interplay of age-related tissue degeneration, re peated microtraumata, blunt injuries, hypovascularity, the inherent property of the supraspinatus tendon, enthesopathy, and subacromial impingement.
Although glenohumeral arthritis in a rotator cuff-deficient shoulder had been variously reported, the term cuff-tear arthropathy was first used by Neer et al. in 198336 to describe glenohumeral arthritis in the setting of a massive rotator cuff tear with characteristic collapse and superior migration of the humeral head. This condition still poses a therapeutic challenge to the shoulder specialist.
Massive rotator cuff tears are associated with profound changes of the respective muscles. On computed tomography scans, Goutallier et al.37 (1994) observed fatty degeneration of the rotator cuff musculature and classified it into five stages. The degree of such degeneration has a direct impact on the functional outcome after the treatment.
The intrinsic healing capacity of torn supraspinatus tendons was confirmed in an in-situ hybridization study by Hamada et al.38 (1997), which has implications for the natural history and conservative treatment of rotator cuff tears. The repair of chronic, massive rotator cuff tears is associated with a high rate of failure. In order to improve the outcomes, Gerber et al.39 found that the mechanical properties of several current techniques of tendon-to-bone suture employed in rotator cuff repair are poor. This shortcoming can be greatly improved by (1) using good material, e.g., number-3 braided polyester suture, (2) using an improved tendon-grasping suture, i.e., a new modification of the Mason-Allen suture, and (3) performing augmentation at the bone attachment. In a separate experiment using the rotator cuff of sheep, Gerber et al.40 reconfirmed the aforementioned findings and emphasized the need for postoperative protection of the repair site from tension overload during the healing period.
Proximal humeral fracture
The vascular anatomy of the proximal humerus is relevant to the occurrence of osteonecrosis of the articular segment in proximal humeral fractures. Laing’s41 and Gerber’s42 studies show that the anterolateral branch of the anterior humeral circumflex artery is the primary blood supply to the proximal humerus. Gerber also found that the posteromedial branch of the posterior humeral circumflex artery supplies the posterior portion of the greater tuberosity and a small posteroinferior part of the head. Thus, injury of the arterial supply to the articular segment, especially the ascending branch of the anterior humeral circumflex artery, can result in osteonecrosis.
Many cases of proximal humeral fractures are minimally displaced and can be treated successfully without surgery. Less commonly, surgical treatment is indicated for displaced fractures. The Neer classification system of proximal humeral fractures has been the gold standard in the orthopedic literature since its publication in 1970.9,10 The system is based on the accurate identification of the four segments of the proximal humerus on plain radiographs and their relation to each other. Emphasis is placed on determining the vascular viability of the humeral head, because osteonecrosis is a complication in which the incidence increases in proportion to fracture comminution and soft-tissue displacement. Neer’s classification represents a monumental advancement in the understanding and treatment of this problem.
Recently, the Arbeitsgemeinshaft für Osteosynthesefragen (AO) classification of proximal humeral fractures43 was proposed in which, in contrast to the Neer system, the valgus-impacted anatomical neck fracture is clearly identified as distinct from other fourpart fractures. Valgus-impacted fractures, unlike true four-part fractures, can have partial preservation of the vascularity to the articular segment through the intact medial capsule. The AO system has been referenced less often in the orthopedic literature than the Neer system, due mainly to its complexity. Admittedly, both systems have limited interobserver reliability, since any displacement of the fracture segment is in a continuum of the spectrum; still, they are clinically useful to help triage various injuries to be treated appropriately.
Arthroplasty
The most dramatic advance in shoulder surgery in the past 50 years is the introduction of replacement arthroplasty. It is of historic interest that the first shoulder arthroplasty was reported in 1893 by the French surgeon Jules-Emile Péan for a case of draining tuberculous infection of the upper humerus.44 The design of the modern prosthesis was developed by Neer in the early 1950s.8 The original prosthesis was a monoblock type, made of vitallium to replace the articular surface of the humeral head for comminuted fractures as hemiarthroplasty (the first-generation prosthesis). In 1973, Neer redesigned the humeral component to mate with the polyethylene glenoid component, and a completely nonconstrained but fully conforming total shoulder system became available for general use. Neer’s principle for shoulder arthroplasty was to retain as much of the normal anatomy as possible. Since then, unconstrained prosthetic arthroplasty with various models has been widely used to treat glenohumeral osteoarthritis, rheumatoid arthritis, and osteonecrosis, with good and reproducible results.45 However, the outcome for old trauma and cuff-tear arthropathy has been less predictable. Because of the limited variety of sizes of the original Neer prosthesis, new modular, or second-generation, prostheses were developed in the early 1990s, in an attempt to better conform to the variable dimensions of the head and medullary canal of the humerus (Biomet, Cofield, Global). Unfortunately, the second-generation prostheses were not very successful in replicating the normal anatomy, in that the prosthetic head was often oversized and malpositioned, creating new biomechanical problems. In the 1990s, Boileau and Walch46 and others47 showed that the shape of the proximal humerus is more complex than previously had been described. The articular surface of the head was found to be offset both posteriorly and medially in relation to the proximal medullary axis, and variably oriented in the vertical and horizontal planes, namely in inclination and retroversion. These findings led to modifications in the design of the prosthesis and in the surgical technique. Thus, the Aequalis prosthesis (Tornier, Ismier, France) was designed providing both modularity and adaptability of the implant to the complex three-dimensional geometry of the proximal humerus. It is the first third-generation unconstrained shoulder prosthesis, which has come close to Neer’s original principle of recreating the normal anatomy. The early clinical results with this implant are promising.48
In 1987, the Delta reverse prosthesis (DePuy-International, UK) became available. It was designed by Grammont et al.49 for cuff-deficient shoulders, in which it is often considered difficult to reestablish function with other types of prostheses. This new model is semiconstrained with a humeral cup articulating on a spherical glenoid component, and moves the center of rotation medially, theoretically decreasing the shear stress on the glenoid component. Thus, the reverse prosthesis relies essentially on the deltoid function alone in a new biomechanical environment. Practical strength in rotation cannot be expected postoperatively. The experience with this implant in Europe for cuff-tear arthropathies, revisions, and tumors is promising in terms of pain relief and acceptable function for the activities of daily living.50
Arthroscopy
Arthroscopy was introduced to shoulder surgery in the 1980s, first for diagnostic purposes, then for ablative procedures, and finally for reconstructive procedures. Now it is an essential tool for the treatment of instability, rotator cuff disease, shoulder contracture, sports-related disorders, and others. In instability, arthroscopic treatment has evolved from staple fixation,51 then to transglenoid suture repair,52,53 and finally to repair with suture anchor54 of the avulsed anterior stabilizing mechanism. The procedure can manage deformed glenoid rim morphology,55 concomitant superior labrum tear, or redundant rotator interval. The outcome after arthroscopic repair for instability is comparable with that of open procedures.
In the treatment of rotator cuff tears, Ellman devised arthroscopic subacromial decompression (ASD) in 1985,56 and this became the first established procedure of arthroscopic surgery. Then the “mini-open” procedure was developed, which is tenorrhaphy under direct vision through a small incision after ASD. Ultimately, a purely intra-articular tendon repair is now performed under arthroscopic control. In this operation, the stump of the torn rotator cuff can be securely reattached to the greater tuberosity by suture anchors without resulting in serious morbidity to the deltoid. Recently, the double- row procedure was developed to reconstruct the footprint of the greater tuberosity anatomically, through which the postoperative cuff integrity was much improved.57 The idea is to anchor the cuff stump onto the bone, not onto a point or line, but onto an area. The early outcome of arthroscopic repair of the rotator cuff is promising.
Thanks to arthroscopy, two new pathological entities have been uncovered: one is tears in the superior labrum at the origin of the biceps tendon and the other is internal glenoid impingement. Although tendinitis of the long head of the biceps has long been recognized as a cause of shoulder pain, a symptomatic tear of the superior labrum at the origin of the biceps tendon has only recently been recognized as an entity. Andrews et al. first described this lesion in athletes in 1985,58 and Snyder et al. further characterized and classified the pathology in 1990,59 attaching the acronym SLAP (superior labrum anterior and posterior lesions). Although SLAP lesions cause significant dysfunction in the overhead athlete, these can also occur in nonathletes as a result of traumata.
Walch. et al.60 in 1992 and Jobe61 in 1993 observed arthroscopically that the rotator cuff could be pinched against the posterosuperior glenoid rim with the shoulder abducted to 90° and maximally externally rotated, resulting in articular surface partial cuff tears. The cause of this injury is postulated to be due to abnormal anterior translation of the humeral head on the glenoid before the internal impingement occurs. The surgeon must always consider both SLAP and internal impingement lesions in the differential diagnosis when evaluating a painful shoulder.
There are, however, limitations in arthroscopy: (1) inability to perform layer-by-layer dissection, thereby increasing the possibility of injuring important but uninvolved structures, such as vessels and nerves and (2) visual inaccessibility to intramural lesions, such as an interstitial tear of the rotator cuff or intraosseous pathology. Beyond these limitations, the most important issue in arthroscopic surgery today is how to acquire and update the skills required. Since the arthroscope is an instrument, and the skills of individual surgeons continue to develop, the surgeon must be mindful to operate within his or her current level of skill. This is especially true when contemplating arthroscopic procedures for which there is an open procedure with a higher success rate. In such a situation, we have to be skilled equally in both open and arthroscopic techniques and use our well balanced judgment.
Japanese contribution to “shoulderology”
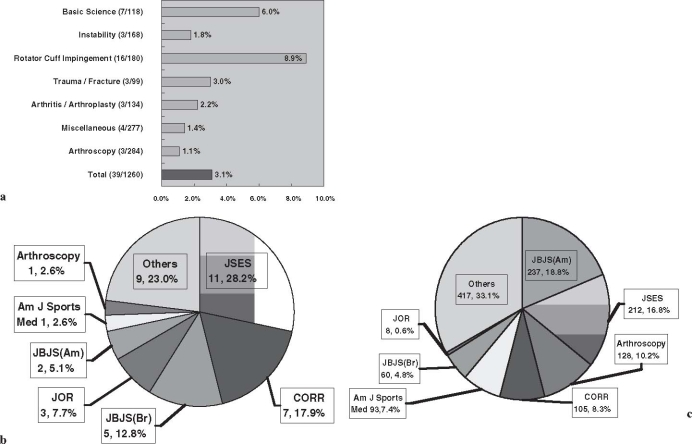
The Japan Shoulder Society was founded in 1974 as the first national body of this subspecialty in the world. It is now 32 years since its inauguration, so how much has it accomplished? As a method of assessment, the citation of the published articles by Japanese researchers in Orthopaedic Knowledge Update: Shoulder and Elbow 2 (AAOS 2002)62 was evaluated. Excluding the elbow chapter, the total number of citations was 1260, of which those with the Japanese as senior authors were 39 (3.1%). When the same paper was cited elsewhere in a different chapter, it was counted anew.
When analyzing according to category, the citation rate was the highest in rotator cuff impingement, 8.9% (16/180), and the second highest was for basic science, 5.9% (7/118) and so forth (Fig. 4a). The order of peer-reviewed journals publishing these 39 articles was: (1) The Journal of Shoulder and Elbow Surgery (JSES), 11 articles (28.2%); (2) Clinical Orthopaedics and Related Research (CORR), 7 (20.5%); (3) The Journal of Bone and Joint Surgery, British Volume (JBJS Br), 5 (12.8%); (4) The Journal of Orthopaedic Research (JOR), 3 (7.7%), (5) The Journal of Bone and Joint Surgery, American Volume (JBJS Am), 2 (5.1%); and others, 11 (28.2%) (Fig. 4b).
Fig. 4.
a Citation rate of Japanese articles by category in Orthopaedic Knowledge Update: Shoulder and Elbow 2. American Academy of Orthopaedic Surgeons, 2002. b Journals publishing Japanese articles cited in Orthopaedic Knowledge Update: Shoulder and Elbow 2. c Journals publishing all cited articles in Orthopaedic Knowledge Update: Shoulder and Elbow 2
When compared with journals publishing all the cited articles in Orthopaedic Knowledge Update: Shoulder and Elbow 2, the order was: (1) JBJS Am, 237 articles (18.8%); (2) JSES, 212 (16.8%); (3) The Arthroscopy, 128 (10.2%); (4) CORR, 105 (8.3%); (5) The American Journal of Sports Medicine, 93 (7.4%); (6) JBJS Br, 60 (4.8%), and others, 425 (33.7%) (Fig. 4c).
Recently, Bosker et al.63 reported the international rank order of the number of publications in 15 major clinical orthopedic journals from 2000 to 2004. Japan was the second, following the United States, in the top ten countries ranked according to the number of publications; 1070 of the total publication of 13 311 articles (8.0%). When corrected for the size of the population, smaller European countries outrank the others, with Sweden being first, Switzerland second, Finland third, the United States sixth, and Japan sixteenth. In JSES, Japan was second, behind the United States, with 43 of 435 articles (9.9%) (Table 1). Bosker et al. consider that the number of citations in top journals might be a more sensitive marker of scientific influence than the impact factor and the number of publications, but this is difficult to assess. Despite some potential selection bias, Japanese contributions to “shoulderology” are emerging and are being recognized.
Table 1.
Top ten countries ranked according to the number of publications in The Journal of Shoulder and Elbow Surgery (2000–2004)
| United States | 206 | 47.4% |
| Japan | 43 | 9.9% |
| United Kingdom | 29 | 6.7% |
| Germany | 25 | 5.7% |
| Australia | 21 | 4.8% |
| Switzerland | 18 | 4.1% |
| France | 17 | 3.9% |
| Canada | 14 | 3.2% |
| Sweden | 7 | 1.6% |
| Netherlands | 6 | 1.4% |
| Finland | 6 | 1.4% |
| Others | 43 | 9.9% |
| Total | 435 | 100% |
Modified from Bosker BH, Verheyen CCPM. J Bone Joint Surg Br 2006;88:156–8
To develop shoulder surgery in the non-English-speaking world
There is no question that English is the tool of international communication. Samuel Johnson once said “A man may write at any time, if he will set himself doggedly to it.” This is true, but it requires a lot of time and energy to do so in English for those whose mother tongue is not English. To develop shoulder surgery in the non-English-speaking world, we suggest the following efforts from our experience.
I. For individuals: (1) read, read, and read both classic and current literature of both orthopedic and general medicine, (2) seek mentor(s), (3) think originally, i.e., “outside the box,” (4) present papers overseas, (5) submit articles to peer-reviewed journals in English, and (6) cultivate an international awareness.
A new ring retractor was developed64 to help expose the glenoid surface, as required in a Bankart repair of the labrum or in the insertion of the glenoid implant in a total shoulder arthroplasty (Fig. 5). The retractor was invented by the current authors, and may be considered an example of thinking “outside the box.” Serendipity strikes when a relevant issue is seriously thought out. It is essential that continuing commitment, particularly to the JSES, be maintained and every effort made to encourage non-English-speaking colleagues not only to subscribe to this prestigious journal, but also to submit worthy articles for publication.
Fig. 5.
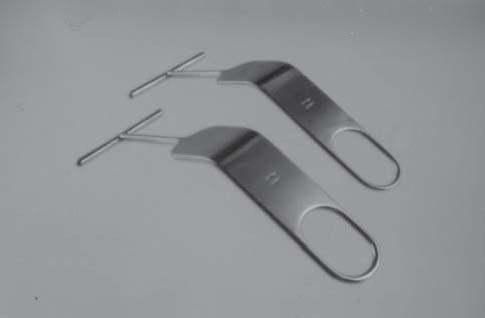
The ring retractor. When in use, the tip of the ring is placed posteriorly to the glenoid rim while the humeral head acts as a fulcrum. Thus, the glenoid surface is well and stably exposed. The middle portion of the handle is bent and flattened and is used to retract the deltoid laterally
II. For each shoulder team: (1) consider forging a closer relationship between basic research and clinical medicine — “bring the lab to the bedside.” Since its inception in 1974, our Society (JSS) has endeavored to promote the effective integration of basic scientific research and its clinical application. We believe this approach will help to decipher many vexing problems facing us and our patients; and (2) organize multicenter, multidisciplinary, cohort, prospective, randomized, and long-term projects as much as possible.
III. For regional and national shoulder societies: (1) participate actively worldwide and maintain contact with shoulder authorities and centers of excellence overseas, and (2) standardize the knowledge-base and operative techniques through regular instructional courses, hands-on sessions, and arthroscopic training centers, for example. Even when these criteria are met, we must move forward, ever advancing our knowledge, keeping up with our skills, and learning from each other so that we become one world of healers against our common adversity — shoulder pain and disability.
Summary
A historical review is presented on trends in modern shoulder surgery.
The pioneering and central roles of Codman and Neer are discussed.
New developments are covered, especially since the 1980s with the introduction of new imaging modalities and arthroscopy.
Japanese contributions are emerging and are being recognized.
Suggestions are made to develop this subspecialty in the non-English-speaking world “shoulder to shoulder” with overseas colleagues.
Acknowledgment
The authors are grateful to Yasuo Ishida, M.D., of St Louis, MO, USA, for his help in preparing this manuscript.
Footnotes
An erratum to this article is available at http://dx.doi.org/10.1007/s00776-006-1130-x.
References
- 1.Golding FC. The shoulder — the forgotten joint. Brit J Radiol. 1962;35:149–58. doi: 10.1259/0007-1285-35-411-149. [DOI] [PubMed] [Google Scholar]
- 2.Codman EA. The shoulder — rupture of the supraspinatus tendon and other lesions in or about the subacromial bursa. Boston: Thomas Todd; 1934. [Google Scholar]
- 3.Perthes G. Ueber Operationen bei habitueller Schulterluxation. Dtsch Z Chir. 1906;85:199–227. [Google Scholar]
- 4.Bankart ASB. Recurrent or habitual dislocation of the shoulder joint. BMJ. 1923;2:1132–3. doi: 10.1136/bmj.2.3285.1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lindblom K. Arthrography and roentgenography in ruptures of the tendon of the shoulder joint. Acta Radiol. 1939;20:548–62. doi: 10.3109/00016923909174876. [DOI] [Google Scholar]
- 6.Bosworth DM. An analysis of 28 consecutive cases of incapacitating shoulder lesions, radically explored and repaired. J Bone Joint Surg. 1940;22:369–92. [Google Scholar]
- 7.McLaughlin HL. Lesions of the musculotendinous cuff of the shoulder, I. The exposure and treatment of tears with retraction. J Bone Joint Surg. 1944;26:31–51. [Google Scholar]
- 8.Neer CS, II, Brown TH, McLaughlin HL. Fracture of the neck of the humerus with dislocation of the head fragment. Am J Surg. 1953;85:252–8. doi: 10.1016/0002-9610(53)90606-0. [DOI] [PubMed] [Google Scholar]
- 9.Neer CS., II Displaced proximal humeral fractures: I. Classification and evaluation. J Bone Joint Surg Am. 1970;52:1077–89. [PubMed] [Google Scholar]
- 10.Neer CS., II Displaced proximal humeral fractures: II. Treatment of three-part and four-part displacement. J Bone Joint Surg Am. 1970;52:1090–103. [PubMed] [Google Scholar]
- 11.Neer CS., II Anterior acromioplasty for the chronic impingement syndrome in the shoulder. A preliminary report. J Bone Joint Surg Am. 1972;54:41–50. [PubMed] [Google Scholar]
- 12.Neer CS, II, Foster CR. Inferior capsular shift for involuntary inferior and multidirectional instability of the shoulder: a preliminary report. J Bone Joint Surg Am. 1980;62:897–908. [PubMed] [Google Scholar]
- 13.Neer CS., II . Shoulder reconstruction. 1st ed. Philadelphia: WB Saunders; 1990. [Google Scholar]
- 14.Moseley HF. Recurrent dislocation of the shoulder. Montreal: McGill Univ Press; 1961. [Google Scholar]
- 15.Moseley HF. Shoulder lesions. 2nd ed. Edinburgh: E & S Livingstone; 1969. [Google Scholar]
- 16.Bateman JE. The shoulder and neck. 2nd ed. Philadelphia: WB Saunders; 1978. [Google Scholar]
- 17.DePalma AF. Surgery of the shoulder. 3rd ed. Philadelphia: JB Lippincott; 1983. [Google Scholar]
- 18.Rowe CR. The shoulder. 1st ed. New York: Churchill Livingstone; 1988. [Google Scholar]
- 19.Rockwood CA, Jr, Matsen FA, III, Wirth MA, Lippitt SB. The shoulder. 3rd ed. Philadelphia: WB Saunders; 2004. [Google Scholar]
- 20.Rowe CR. Prognosis in dislocations of the shoulder. J Bone Joint Surg Am. 1956;38:957–77. [PubMed] [Google Scholar]
- 21.Rowe CR, Pierce DS, Clark JG. Voluntary dislocation of the shoulder: a preliminary report on a clinical, electromyographic, and psychiatric study of 26 patients. J Bone Joint Surg Am. 1973;55:445–60. [PubMed] [Google Scholar]
- 22.Rowe CR, Patel D, Southmoyd WW. The Bankart procedure. A long-term end-result study. J Bone Joint Surg Am. 1978;60:1–16. [PubMed] [Google Scholar]
- 23.Rowe CR, Zarins B. Recurrent transient subluxation of the glenohumeral joint. J Bone Joint Surg Am. 1981;63:863–72. [PubMed] [Google Scholar]
- 24.Saha AK. Theory of shoulder mechanism: descriptive and applied. Springfield, IL, USA: Charles C Thomas; 1961. [Google Scholar]
- 25.Uhthoff HK. Calcifying tendonitis, an active, cell-mediated calcification. Virchows Arch Anat. 1975;366:51–8. doi: 10.1007/BF00438677. [DOI] [PubMed] [Google Scholar]
- 26.Moseley HF ed. Symposium on surgery of the shoulder region. Surg Clin N Am 1963;43:1463–1726
- 27.Constant CR, Murley AHG. A clinical method of functional assessment of the shoulder. Clin Orthop Rel Res. 1987;214:160–4. [PubMed] [Google Scholar]
- 28.Inman VT, Saunders JB, Abbott LC. Observations on the function of the shoulder joint. J Bone Joint Surg Am. 1944;26:1–30. [Google Scholar]
- 29.Clark JM, Harryman DT., II Tendons, ligaments, and capsule of the rotator cuff: gross and microscopic anatomy. J Bone Joint Surg Am. 1992;74:713–25. [PubMed] [Google Scholar]
- 30.Gohlke F, Essigkrug B, Schmitz F. The pattern of the collagen fiber bundles of the capsule of the glenohumeral joint. J Shoulder Elbow Surg. 1994;3:111–28. doi: 10.1016/S1058-2746(09)80090-6. [DOI] [PubMed] [Google Scholar]
- 31.Endo H, Takigawa H, Takata K, et al. A method of diagnosis and treatment for loose shoulder. Central Jpn J Orthop Surg Traumatol. 1971;14:630–32. doi: 10.1016/j.jse.2012.03.018. [DOI] [PubMed] [Google Scholar]
- 32.Kumar VP, Balasubramaniam P. The role of atmospheric pressure in stabilizing the shoulder: an experimental study. J Bone Joint Surg Br. 1985;67:719–21. doi: 10.1302/0301-620X.67B5.4055867. [DOI] [PubMed] [Google Scholar]
- 33.Hovelius L, Augustini BG, Fredin H, et al. Primary anterior dislocation of the shoulder in young patients: a ten-year prospective study. J Bone Joint Surg Am. 1996;78:1677–84. doi: 10.2106/00004623-199611000-00006. [DOI] [PubMed] [Google Scholar]
- 34.Itoi E, Sashi R, Minagawa H, et al. Position of immobilization after dislocation of the glenohumeral joint: a study with use of magnetic resonance imaging. J Bone Joint Surg Am. 2001;83:661–7. doi: 10.2106/00004623-200105000-00003. [DOI] [PubMed] [Google Scholar]
- 35.Fukuda H. The management of partial-thickness tears of the rotator cuff. J Bone joint Surg Br. 2003;85:3–11. doi: 10.1302/0301-620X.85B1.13846. [DOI] [PubMed] [Google Scholar]
- 36.Neer CS, II, Craig EV, Fukuda H. Cuff-tear arthropathy. J Bone Joint Surg Am. 1983;65:1232–44. [PubMed] [Google Scholar]
- 37.Goutallier D, Postel JM, Bernageau J, et al. Fatty muscle degeneration in cuff ruptures: Pre- and postoperative evaluation by CT scan. Clin Orthop. 1994;304:78–83. [PubMed] [Google Scholar]
- 38.Hamada K, Tomonaga A, Gotoh M, et al. Intrinsic healing capacity and tearing process of torn supraspinatus tendons: in situ hybridization study of α (I) procollagen mRNA. J Orthop Res. 1997;15:24–32. doi: 10.1002/jor.1100150105. [DOI] [PubMed] [Google Scholar]
- 39.Gerber C, Schneeberger AG, Beck M, et al. Mechanical strength of repairs of the rotator cuff. J Bone Joint Surg Br. 1994;76:371–80. [PubMed] [Google Scholar]
- 40.Gerber C, Schneeberger AG, Perren SM, et al. Experimental rotator cuff repair: a preliminary study. J Bone Joint Surg Am. 1999;81:1281–90. doi: 10.2106/00004623-199909000-00009. [DOI] [PubMed] [Google Scholar]
- 41.Laing PG. The arterial supply of the adult humerus. J Bone Joint Surg Am. 1956;38:1105–16. [PubMed] [Google Scholar]
- 42.Gerber C, Schneeberger AG, Vinh TS. The arterial vascularization of the humeral head: an anatomical study. J Bone Joint Surg Am. 1990;72:1486–94. [PubMed] [Google Scholar]
- 43.Orthopaedic Trauma Association Committee for Coding and Classification Fracture and dislocation compendium. J Orthop Trauma. 1996;10(suppl 1):1–155. [PubMed] [Google Scholar]
- 44.Lugli T. Artificial shoulder joint by Péan (1893): the facts of an exceptional intervention and the prosthetic method. Clin Orthop Rel Res. 1978;133:215–8. [PubMed] [Google Scholar]
- 45.Neer CS, II, Watson KC, Stanton FJ. Recent experience in total shoulder replacement. J Bone Joint Surg Am. 1982;64:319–37. [PubMed] [Google Scholar]
- 46.Boileau P, Walch G. The three-dimensional geometry of the proximal humerus: implications for surgical technique and prosthetic design. J Bone Joint Surg Br. 1997;79:857–65. doi: 10.1302/0301-620X.79B5.7579. [DOI] [PubMed] [Google Scholar]
- 47.Roberts SN, Foley AP, Swallow HM, et al. The geometry of the humeral head and the design of prostheses. J Bone Joint Surg Br. 1992;73:647–50. doi: 10.1302/0301-620X.73B4.2071652. [DOI] [PubMed] [Google Scholar]
- 48.Godeneche A, Boileau P, Favard L, et al. Prosthetic replacement in the treatment of osteoarthritis of the shoulder: early results of 268 cases. J Shoulder Elbow Surg. 2002;11:11–8. doi: 10.1067/mse.2002.120140. [DOI] [PubMed] [Google Scholar]
- 49.Grammont P, Trouilloud P, Laffay JP, et al. Etude et réalisation d’une nouvelle prothèse d’épaule. Rheumatologie. 1987;39:27–38. [Google Scholar]
- 50.Boileau P, Sinnerton RJ, Chuinard C, et al. Arthroplasty of the shoulder. J Bone Joint Surg Br. 2006;88:562–75. doi: 10.2106/JBJS.E.00817. [DOI] [PubMed] [Google Scholar]
- 51.Johnson LL. Instructional video: arthroscopic staple capsulorrhaphy. East Lancing, MI, USA: Instrument Maker; 1983. [Google Scholar]
- 52.Morgan CD, Bordenstad AB. Arthroscopic Bankart suture repair: technique and early results. Arthroscopy. 1987;3:111–22. doi: 10.1016/s0749-8063(87)80027-0. [DOI] [PubMed] [Google Scholar]
- 53.Caspari RB. Arthroscopic reconstruction for anterior shoulder instability. Oper Tech Orthop. 1988;3:59–66. [Google Scholar]
- 54.Wolf EM. Arthroscopic anterior shoulder capsulorrhaphy. Oper Tech Orthop. 1988;3:67–74. [Google Scholar]
- 55.Sugaya H, Moriishi J, Kanisawa I, et al. Arthroscopic osseous Bankart repair for chronic recurrent traumatic anterior glenohumeral instability. J Bone Joint Surg Am. 2005;87:1752–60. doi: 10.2106/JBJS.D.02204. [DOI] [PubMed] [Google Scholar]
- 56.Ellman H. Arthroscopic subacromial decompression. A preliminary report. Orthop Trans. 1985;9:49. [Google Scholar]
- 57.Lo IK, Burkhart SS. Double-row arthroscopic rotator cuff repair: re-establishing the footprint of the rotator cuff. Arthroscopy. 2003;19:1035–42. doi: 10.1016/j.arthro.2003.09.036. [DOI] [PubMed] [Google Scholar]
- 58.Andrews JR, Carson WG, McLeod WD. Glenoid labrum tears related to the long head of the biceps. Am J Sports Med. 1985;13:337–41. doi: 10.1177/036354658501300508. [DOI] [PubMed] [Google Scholar]
- 59.Snyder SJ, Karzel RP, Dl Pizzo W, et al. SLAP lesions of the shoulder. Arthroscopy. 1990;6:274–9. doi: 10.1016/0749-8063(90)90056-j. [DOI] [PubMed] [Google Scholar]
- 60.Walch G, Boileau P, Noel E, et al. Impingement of the deep surface of the supraspinatus tendon on the posterosuperior glenoid rim: an arthroscopic study. J Shoulder Elbow Surg. 1992;1:238–45. doi: 10.1016/S1058-2746(09)80065-7. [DOI] [PubMed] [Google Scholar]
- 61.Jobe CM. Evidence for a superior glenoid impingement upon the rotator cuff. J Shoulder Elbow Surg. 1993;2:S19. [Google Scholar]
- 62.Norris TR, editor. Orthopaedic knowledge update: shoulder and elbow 2. 2nd ed. Rosemont, Illinois, USA: American Academy of Orthopaedic Surgeons; 2002. [Google Scholar]
- 63.Bosker BH, Verheyen CCPM. The international rank order of publications in major clinical orthopaedic journals from 2000 to 2004. J Bone Joint Surg Br. 2006;88:156–8. doi: 10.1302/0301-620X.88B2.17018. [DOI] [PubMed] [Google Scholar]
- 64.Fukuda H, Mikasa M, Ogawa K. Ring retractor: a new humeral-head retractor. J Bone Joint Surg Am. 1982;64:289. [PubMed] [Google Scholar]