Abstract
Purpose
Assessment of current practice with a valid set of indicators is the key to successfully improving the quality of patient-centred care. For improvement purposes, we developed indicators of patient-centred cancer care and tested them on a population of patients with non-small cell lung cancer (NSCLC).
Methods
Recommendations for patient-centred care were extracted from clinical guidelines, and patients were interviewed to develop indicators for assessing the patient-centredness of cancer care. These indicators were tested with regard to psychometric characteristics (room for improvement, applicability, discriminating capacity and reliability) on 132 patients with NSCLC treated in six hospitals in the east Netherlands. Data were collected from patients by means of questionnaires.
Results
Eight domains of patient-centred cancer care were extracted from 61 oncology guidelines and 37 patient interviews and were translated into 56 indicators. The practice test amongst patients with NSCLC showed the most room for improvement within the domains ‘emotional and psychosocial support’, ‘physical support’ and ‘information supply’. Overall, 26 of the 56 indicators had good psychometric characteristics.
Conclusions
Developing a valid set of patient-centred indicators is a first step towards improving the patient centredness of cancer care. Indicators can be based on recommendations from guidelines, but adding patient opinions leads to a more complete picture of patient centredness. The practice test on patients with NSCLC showed that the patient centredness of cancer care can be improved. Our set of indicators may also be useful for future quality assessments for other patients with cancers or chronic diseases.
Keywords: Cancer, Oncology, Quality indicators, Health care, Patient-centred care, Quality of health care
Introduction
As a cause of death in the USA and Europe, cancer is exceeded only by cardiovascular disease [2]. Earlier diagnosis, improved treatment modalities and enhanced supportive care result in cancer taking on the characteristics of a chronic disease more and more [32]. The management of care for cancer patients is complex. First, cancer has a very significant impact on the patient’s physical, emotional and social well-being. Second, various professionals are involved in prevention, diagnosis, treatment and follow-up. This complexity can lead to suboptimal care and result in discontinuity and fragmentation of care [1, 20, 24]. Therefore, there is a need to organise health care delivery in a way that is more patient centred and not disease or provider centred. Patient centredness means that care is organised around the physical, social and emotional needs and preferences of patients and that patients are actively involved in their own care [25, 36].
Literature shows that the patient centredness of cancer care can be improved in several ways, such as more supportive care, better communication, better information supply and better cooperation amongst physicians [23, 30, 35]. To improve the quality of the patient centredness of care for patients with cancer, current practice needs to be reliably assessed [15]. However, this assessment is not straightforward, and selecting appropriate indicators to assess care is difficult. Evidence-based clinical guidelines for the management of patients with cancer can provide recommendations for patient-centred care. The available recommendations from these guidelines should be combined with opinions of the patients themselves so that we can assess additional aspects for which evidence alone is insufficient or absent [18]. To measure the quality of patient centredness, ‘patient-centred’ recommendations in these guidelines need to be translated into so-called quality indicators. Quality indicators are ‘measurable elements of practice performance for which there is evidence or consensus that they can be used to assess the quality of care’ [8]. There are some well-known instruments for measuring patient satisfaction [3, 4] and patients’ experiences [21, 22]. These instruments are based on existing patient-satisfaction questionnaires, interviews and focus groups. However, quality indicators for measuring patient centredness of cancer care based on evidence-based guidelines and opinions of patients do not exist.
This study reports the first step in improving patient-centred cancer care in which we have systematically developed a set of indicators to measure the patient centredness of cancer care. We used a practice test to assess both the feasibility of this set of indicators with regard to psychometric characteristics and the quality of patient-centred cancer care for patients with non-small cell lung cancer (NSCLC) in the Dutch eastern comprehensive cancer region.
Materials and methods
Development of indicators
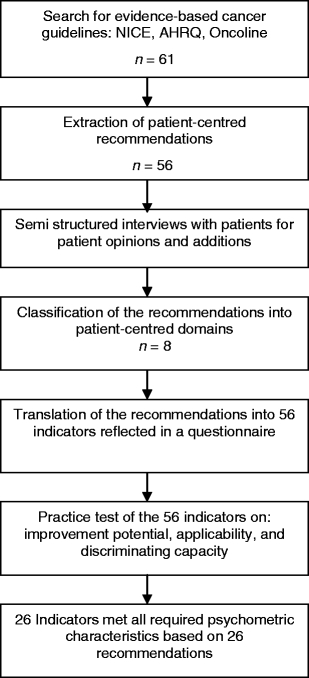
The development of indicators started with a search for evidence-based guidelines regarding the management of patients with all types of cancer. We searched the two largest English-language national databases for evidence-based guidelines (UK: National Institute for Health and Clinical Excellence; USA: Agency for Healthcare Research and Quality) and the Dutch oncology database Oncoline (www.oncoline.nl; www.guideline.gov; www.nice.org.uk). All guidelines for the general management of patients with all types of cancer were included. Guidelines for specific aspects of care management for patients with cancer were excluded (e.g. pain management). One researcher extracted all the recommendations from the guidelines that had to do with organising care around the physical, social and emotional needs and the preferences of patients. We used a semi-structured method to interview 30 patients with head and neck cancer, as well as all seven patient representatives from the Dutch national association of patients with lung cancer. The interviewer read the recommendations aloud, and the patients and their representatives were asked to rate the recommendations on a nine-point Likert scale to determine their degree of importance for the patient centredness of care (a score of 1 meant ‘not important at all’ and 9 meant ‘very important’). They were also given a chance to add new items. All recommendations with a mean score of 8 points or more were included in the final set. Domains were extracted from the guidelines and two researchers classified all the recommendations into the domains of patient centredness. Two researchers translated the recommendations into indicators, a process of defining numerators and denominators. A panel of four researchers judged the translation process from recommendation to indicator (Fig. 1).
Fig. 1.
Study design
Questionnaire
The indicators were reflected in a questionnaire for cancer patients. The questionnaire asked patients for their actual experiences with care and not for their satisfaction. We asked patients with NSCLC to rate their experiences regarding 56 aspects of patient-centred care on a four-point Likert scale (1 = not done; 2 = done, but inadequately; 3 = done adequately; 4 = done excellently) or on a YES or NO scale. The indicators evaluated on a Likert scale were coded as dichotomous scores: adherence to the indicator ‘yes’ (score 1 or 2) or ‘no’ (score 3 or 4). These 56 aspects of care are part of one of the eight domains of patient-centred care, namely, access (e.g. ‘Did you start therapy within 35 days of your first visit to the specialist’), follow-up (‘Did you know which medicine to take at home?’), communication and respect (‘Do you trust your specialist?’), involvement (‘Were family and friends involved during care and follow-up?’), information (‘Did you receive written information about treatment?’), coordination (‘Did you know how to reach specialists?’), physical support (‘Did you get support to control your pain?’) and emotional and psychosocial support (‘Did the specialist ask about fear and your mental state?’).
Practice test
The questionnaire was tested in a group of 132 patients with NSCLC. This practice test took place in six hospitals in the Dutch eastern comprehensive cancer region (Table 1). The period patients were asked to evaluate was from the first visit until the beginning of treatment. After the ethics committee of the Radboud University Medical Centre in Nijmegen, The Netherlands approved the study, we included all consecutive patients newly diagnosed with NSCLC in the 6 months from September 2004 to February 2005 inclusive. The staff members of the Eastern Comprehensive Cancer Centre retrospectively included the patients by pathology diagnosis. Each hospital’s pulmonologist checked the patient records to ensure that all questionnaire recipients were still alive. The researchers sent the questionnaires to the patients’ homes, in a way that ensured patient anonymity, after the inclusion period had ended. The questionnaires were accompanied by a letter from each patient’s own pulmonologist. A reminder was sent to each patient who had not replied after 2 weeks.
Table 1.
Descriptive characteristics of the six hospitals
| Number | Percentage (range) | |
|---|---|---|
| Teaching hospital | 4 | 67 |
| Hospital beds, mean (range) | 630 | (200–960) |
| Lung cancer patients (NSCLC) seen per year, mean (range) | 100 | (30–160) |
| Availability of a multidisciplinary team for lung cancer | 2 | 33 |
| Specialised nurse with coordination tasks | 1 | 17 |
To test the feasibility of our set of indicators, we assessed the following psychometric characteristics: room for quality improvement, applicability, and discriminating capacity and reliability. Indicators must be capable of detecting improvements in the quality of care. If, for example, indicator performance is invariably high, there is little room for improvement. We considered that room for improvement was limited when the score for an indicator was 90% or more [31]. Applicability was measured as the proportion of patients to whom the indicator was applicable. Applicability was considered poor if this proportion was less than 75% [31, 34]. When the range between the lowest and highest hospital scores is broad (we assumed 20% or more), an indicator has discriminating potential and is sensitive in detecting differences.
Ultimately, we tested all the indicators that fulfilled the psychometric criteria for reliability regarding the eight domains of patient centredness by calculating Cronbach’s alpha coefficients for the domains. A Cronbach’s alpha score of 0.7 or more implies that the measures within one domain are reliably related to other measures included within the same domain [12].
Results
Development of indicators
We found 61 evidence-based oncology guidelines in the three databases, from which we extracted 56 recommendations. Patients or their representatives who were interviewed (n = 37) found all the recommendations important (mean score of 8 or more), so we included all of them [10]. Adding patient opinions had added value concerning criteria for waiting times and information supply. The guidelines often recommended speeding up the diagnosis and starting treatment as soon as possible. However, they provided hardly any concrete information about acceptable waiting times. The criteria for waiting and throughput times in our study came from the patient interviews as answers to the question of acceptable waiting times. Furthermore, the patients added three specific information items, namely, ‘information about the possible course of the disease’, ‘the possibility of a second opinion’ and ‘information about the treatment option of “no active therapy”’. The eight domains of patient centredness are access, follow-up, communication and respect, patient and family involvement, information, coordination, physical support and emotional and psychosocial support. The domains most often mentioned in the guidelines were ‘follow-up’ (38%), ‘emotional and psychosocial support’ (34%) and ‘multidisciplinary patient care team’ (30%). The least mentioned domain was ‘paramedical support, e.g. dietician’ (10%; Table 3). All the recommendations were translated into a set of 56 indicators (Fig. 1).
Table 3.
Patient-centred domains in 61 general oncology guidelines
| Oncoline (n = 14) | AHRQ (n = 36) | NICE (n = 11) | Total (n = 61) | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| 1. Access to care | 1 | 7 | 2 | 6 | 5 | 45 | 8 | 13 |
| 2. Follow-up | 12 | 86 | 13 | 36 | 6 | 55 | 23 | 38 |
| 3. Communication and respect | 2 | 14 | 6 | 17 | 2 | 18 | 10 | 16 |
| 4. Patient and family involvement | 2 | 14 | 4 | 11 | 2 | 18 | 8 | 13 |
| 5. Information | 4 | 29 | 5 | 14 | 6 | 55 | 15 | 25 |
| 6. Coordination | ||||||||
| Specialists/multidisciplinary patient care team | 4 | 29 | 5 | 14 | 9 | 82 | 18 | 30 |
| Oncology nurse with case management tasks | 2 | 14 | 5 | 14 | 6 | 55 | 13 | 21 |
| Paramedical support | 3 | 21 | 3 | 27 | 6 | 10 | ||
| 7. Physical support (pain, nausea, etc.) | 3 | 21 | 4 | 11 | 5 | 50 | 12 | 20 |
| 8. Emotional and psychosocial support | 9 | 64 | 6 | 17 | 6 | 55 | 21 | 34 |
The table shows the number of times a patient-centred domain was mentioned in the guideline, e.g. recommendations on follow-up were mentioned in 38% of all guidelines (23 of 38)
AHRQ Agency for Healthcare Research and Quality, NICE National Institute for Health and Clinical Excellence
Practice test
Study population
During the study period of 6 months, a population of 276 patients with NSCLC were included. However, because many patients with NSCLC die within months after diagnosis, we were only able to send 132 of the 276 patients a questionnaire.
All patients received the questionnaire 2 to 6 months after their first visit to the pulmonologist. Seventy-six percent of the patients returned the questionnaire. The responders (n = 100) and non-responders (n = 32) did not significantly differ in sex, age and disease stage (Table 2).
Table 2.
Descriptive characteristics of the 132 patients
| Response (n = 100) [n (%)] | Non-response (n = 32) [n (%)] | |
|---|---|---|
| Mean age in years | 66 | 68 |
| Men | 65 (66) | 19 (60) |
| Disease stage IV | 23 (24) | 9 (32) |
| Other cancer 5 years or longer ago | 9 (9) | 6 (18) |
Psychometric characteristics: room for improvement
The least room for improvement was found within the domains ‘communication and respect’ (mean score of 95% and all indicators in this domain scored 89% or more), followed by the domain ‘patient and family involvement’ (mean score of 84% and individual scores of 71% or more; Table 4) Most room for improvement was found within the domains ‘physical support’, ‘emotional and psychosocial support’ and ‘information’. Patients did get physical support during the hospital stay (80%), but hardly any at home (36%), and only 58% of the patients felt that they had received enough support to control their physical complaints of pain, suffocation, nausea, weight loss, insomnia, tingling and blood coughs (Table 4). About one third of the patients stated that they were asked if they had psychological complaints or had problems with living conditions, but only 39% of the patients who needed support from caregivers who specialise in mental health actually got this care (Table 4). Regarding information, only 19% of the patients stated that they received enough information about all ten information items (Table 4). The information items mentioned most often were ‘aim and follow-up of diagnostic procedures’ and ‘treatment options and pros and cons’. The items mentioned least were ‘availability of emotional support’, ‘opportunity of contacting a companion in distress’ and ‘the possibility of a second opinion’. Overall, 44 of the 56 indicators (79%) had an improvement potential of 10% or more (Fig. 2).
Table 4.
Scores and psychometric characteristics of the patient-centred cancer care indicators
| Domains of patient-centred cancer care (total n = 100) | Score (%) | Room for improvement (%) | Applicability (%) | Range (%) |
|---|---|---|---|---|
| 1. Access (mean score, 68%) | ||||
| Waiting time first visit lung specialist <5 days | 49 | 51 | 100 | 42–56 |
| Waiting time start first treatment from first visit specialist <35 daysa | 62 | 38 | 100 | 40–80 |
| Waiting time diagnostic procedures from first visit specialist <21 daysa | 71 | 29 | 100 | 50–89 |
| Waiting time general practitioner <2 days | 90 | 10 | 100 | 82–100 |
| 2. Follow-up (mean score, 81%) | ||||
| Home care knows about the patient’s situation | 46 | 54 | 64 | 14–80 |
| Patient knows which activities are allowed at homea | 70 | 30 | 91 | 57–86 |
| Patient knows which side effects to be aware ofa | 73 | 27 | 86 | 55–100 |
| Patient knows when to contact the primary care doctor or specialista | 77 | 23 | 98 | 57–100 |
| Patient knows at discharge which medication to take and why | 89 | 11 | 94 | 83–100 |
| The primary care doctor knows about the patient’s situation | 92 | 8 | 93 | 83–100 |
| Patient follow-up takes place on an agreed schedule | 95 | 5 | 98 | 87–100 |
| Specialist has enough time during consultations | 95 | 5 | 100 | 93–100 |
| Patient can reach the specialist between consultations | 94 | 6 | 83 | 89–100 |
| 3. Communication and respect (mean score, 95%) | ||||
| Specialist showed interest in you as a persona | 89 | 11 | 99 | 67–100 |
| Specialists talked to others as if you were not there | 95 | 5 | 95 | 91–100 |
| Nurses talked as if you were not there | 96 | 4 | 93 | 91–100 |
| Nurses showed interest in you as a person | 96 | 4 | 97 | 86–100 |
| Patient trusts in the specialists | 97 | 3 | 98 | 91–100 |
| Patient trusts the nurses | 97 | 3 | 96 | 86–100 |
| Patient feels respected during treatment | 98 | 2 | 99 | 91–100 |
| 4. Patient and family involvement (mean score, 84%) | ||||
| Nurses involved family and friends during care and follow-upa | 71 | 29 | 98 | 61–100 |
| Specialists involved family and friends during treatment and follow-upa | 82 | 18 | 97 | 73–100 |
| Specialists shared the decision making with the patienta | 82 | 18 | 97 | 67–100 |
| Family and friends had opportunities to ask the specialists questionsa | 83 | 17 | 94 | 60–100 |
| Family and friends had opportunities to ask the nurses questionsa | 86 | 14 | 89 | 76–100 |
| Patient had the knowledge and support to make decisions | 88 | 12 | 97 | 82–100 |
| Patient had opportunities to ask questionsa | 89 | 11 | 98 | 76–100 |
| Specialists discussed aim and follow-up of the treatment with the patient | 92 | 8 | 99 | 87–100 |
| 5. Information (mean score, 68%) | ||||
| Patient received information on all ten information itemsa (see note under Table 5) | 19 | 81 | 95 | 17–57 |
| Patient received written informationa | 75 | 25 | 99 | 64–86 |
| Patient received clear answers from the nurses | 77 | 13 | 97 | 83–100 |
| Patient received contradictory information | 79 | 11 | 94 | 85–100 |
| Patient received clear answers from the specialistsa | 90 | 10 | 100 | 77–100 |
| 6. Coordination (mean score, 71%) | ||||
| Coordination: specialists (mean score, 87%) | ||||
| Specialists involved knew patient’s history | 83 | 17 | 94 | 75–94 |
| Patient knew how to reach specialistsa | 84 | 16 | 100 | 65–100 |
| Patient knew about being discussed in a multidisciplinary team of specialistsa | 85 | 15 | 100 | 67–100 |
| Specialists involved took care of the coordinationa | 87 | 13 | 75 | 73–100 |
| Patient knew which specialist is his main contact person | 95 | 5 | 100 | 87–100 |
| Coordination: specialised nurse(s) (mean score, 55%) | ||||
| Oncology nurse was present during bad news consultationa | 36 | 64 | 100 | 21–63 |
| Existence of an oncology nurse was known by patienta | 53 | 47 | 93 | 33–86 |
| Patient knew how to reach oncology nursea | 53 | 47 | 100 | 46–86 |
| Oncology nurse knew patient’s history | 61 | 39 | 29 | 38–100 |
| Oncology nurses took care of the coordination | 71 | 29 | 50 | 50–100 |
| Coordination: Paramedics (mean score, 70%) | ||||
| Patient knew how to reach paramedic professionals | 55 | 45 | 61 | 36–100 |
| Paramedic professionals involved knew patient’s history | 76 | 24 | 62 | 53–100 |
| Paramedic professionals involved took care of the coordination | 80 | 20 | 43 | 50–100 |
| 7. Physical support (mean score, 58%) | ||||
| Patient got support for daily activities at home | 36 | 74 | 72 | 10–40 |
| Patient got support to control physical complaintsa | 58 | 42 | 89 | 25–78 |
| Patient got support for daily activities in the hospital | 80 | 20 | 88 | 73–92 |
| 8. Emotional and psychosocial support (mean score, 46%) | ||||
| Patient was offered contact with companion in distressa | 13 | 87 | 100 | 0–43 |
| Patient was asked whether he had psychological complaintsa | 34 | 66 | 83 | 18–60 |
| Patient was asked whether he had problems with living conditionsa | 36 | 64 | 85 | 23–60 |
| Patient received support from specialised caregivers in mental health if needed | 39 | 61 | 28 | 0–100 |
| Specialist asked patient about fear and mental statea | 52 | 48 | 88 | 32–100 |
| Patient received emotional support from nurses if needed | 74 | 26 | 65 | 63–100 |
| Patient received emotional support from specialists if needed | 74 | 26 | 60 | 46–100 |
aIndicator that met all psychometric characteristics
Fig. 2.
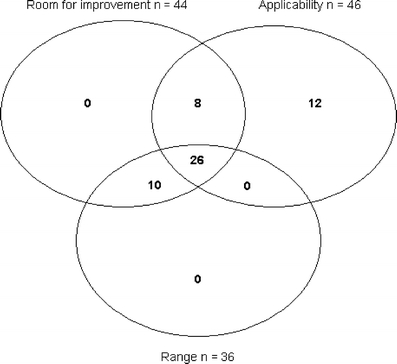
The 56 indicators and their psychometric characteristics
Psychometric characteristics: applicability
We found that ten of the 56 indicators were applicable to less than 75% of the population (Table 4). Low applicability scores were found for some indicators regarding oncology nurses, patients in need of specialised mental care who actually received this support, involvement of paramedical professionals and involvement of home care. Overall, 46 indicators had good applicability (Fig. 2).
Psychometric characteristics: discriminating capacity
Our study showed that 36 indicators had scores with a range of 20% or more between the highest and lowest scoring hospitals (Table 4). The largest ranges between the six hospitals were for the indicators ‘patients receive support from caregivers who specialise in mental health if needed’ (the lowest hospital score was 0% and the highest was 100%) and ‘specialist asked patient about fear and mental state’ (the lowest hospital score was 32% and the highest was 100%).
Psychometric characteristics: reliability
The best indicators for quality improvement are those that have more that 10% room for improvement, good applicability (75% or more) and good discriminating capacities (at least 20% difference between lowest and highest scoring hospitals). In our study, 26 of the 56 indicators had good scores on all three psychometric characteristics (Fig. 2). They cover eight domains of patient centredness as shown in grey in Table 3. The recommendations on which these indicators are based are shown in Table 4. Seven of these eight domains had a Cronbach’s alpha of 0.67 or more, and the reliability was acceptable. The domain ‘coordination of specialists’ had an alpha of 0.22 (Table 5).
Table 5.
Recommendations for patient-centred cancer care tested on patient with non-small cell lung cancer
| Alpha coefficient | |
|---|---|
| Access | |
| Patient receives all necessary diagnostic procedures within 21 days after his first visit to the specialist | 0.87 |
| Patient starts his treatment within 35 days after his first visit to the specialist | |
| Follow-up | |
| Patient knows which side effects to be aware of at home | 0.78 |
| Patient knows which activities are allowed at home | |
| Patient knows when to contact the primary care doctor or specialist | |
| Communication and respect | |
| Specialist shows interest in the patient as a person | |
| Patient and family involvement | |
| Nurses involve family and friends during care and follow-up | 0.85 |
| Specialists involve family and friends during treatment and follow-up | |
| Specialists share the decision making with the patient | |
| Family and friends have opportunities to ask the specialists questions | |
| Family and friends have opportunities to ask the nurses questions | |
| Patient has opportunities to ask questions | |
| Information | |
| Patient receives information on all ten items if applicablea | 0.78 |
| Patient receives written information on all applicable itemsa | |
| Patient receives clear answers from the specialists | |
| Coordination: specialists | |
| Patient knows how to reach the specialists | 0.22 |
| Patient knows being discussed in a multidisciplinary team of specialists | |
| The specialists involved take care of the coordination | |
| Coordination: oncology nurse(s) | |
| An oncology nurse was present during the bad news consultation | 0.68 |
| Patient knows that nurses specialising in oncology exist | |
| Patient knows how to reach the oncology nurse | |
| Physical support | |
| Patient gets support to control physical complaints such as pain, suffocation, nausea, blood coughs, tingling, weight loss and insomnia | |
| Emotional support | |
| Patient is offered contact with a companion in distress | 0.67 |
| Patient is asked about psychological complaints | |
| Patient is asked whether has problems with living conditions | |
| Specialist asks the patient about possible fear and mental state | |
aAim and follow-up of diagnostic procedures, treatment options and pros and cons, treatment option ‘no active therapy’, estimation of possible course of illness, possible loss of weight during treatment and the importance of eating well, options for pain medication, options for anaesthesia in case of operation, opportunities for emotional support, companion in distress, possibility of a second opinion
Discussion
Patient centredness is an important principle for delivering high-quality integrated care. Before patient centredness can be improved, it must be assessed with a valid set of indicators. The development of a valid set of indicators for patient centredness that is applicable to all patients with cancer is an initial step towards improving the care. In our study, we developed 56 indicators for patient centredness covering eight domains of cancer care. There was considerable variation in the domains discussed in the guidelines. The indicators were evaluated in a practice test of the following psychometric characteristics: room for improvement, applicability and discriminating capacity and reliability. Twenty-six of the 56 indicators for patient-centred cancer care had good psychometric characteristics and were tested for reliability.
The eight domains of patient-centred cancer care correspond to patient-centred care dimensions that others mention (www.pickerinstitute.com) [28]. We recommend that specific domains for patient centredness always be addressed in clinical guidelines for the management of patients with cancer, such as, for example, the domains mentioned in this study. Although the literature shows that oncology guidelines have significantly higher scores for the consideration of patients’ views than guidelines for other patient groups [6], we found a large variation within oncology literature covering patient-centred issues. The relatively few patient-centred recommendations in some guidelines may be due to the fact that patients are often not involved in guideline development. However, this is one of the key criteria for good clinical guidelines as proposed by the Appraisal of Guidelines Research and Evaluation collaboration [14]. We believe that involving patients in both guideline development and indicator development may improve patient centredness. In our study, involving patients in indicator development resulted in some additional points that would not otherwise have been noticed as information items and criteria for waiting and throughput times.
The literature provides only a few studies about indicator development [26, 27], and our study is the first to develop and test a general set of indicators for patient-centred cancer care. Our method of combining recommendations from guidelines with patients’ opinions led to a large set of indicators. The usefulness of a quality indicator depends on various psychometric characteristics, and we decided to test our set of indicators on some psychometric characteristics to come up with a core set. There are not many studies on psychometric characteristics of indicators or norms for ’good characteristics’. Our choice of psychometric criteria and norms was based on the literature and our experiences in other studies and was therefore disputable. We chose ‘room for improvement’ because indicators that invariably have high scores provide little room for improvement and are therefore less suited for quality improvement. Other criteria for good indicators are ‘applicable to a large part of the population’ and ‘high variation between hospitals’. We did not test the indicator set for criterion validity because a golden standard for patient centredness is lacking.
Further research should test the original set of 56 indicators on other populations of cancer patients to provide additional evidence for the applicability of these indicators.
The scores for the criterion ‘room for improvement’ shows many improvement opportunities for patients with NSCLC. In line with other studies, our practice test regarding patients with NSCLC showed that patients reported poor management and evaluation of their physical symptoms and psychosocial problems, and they were not fully informed [23, 30, 35]. Cancer is a serious and life-threatening illness, especially for patients with NSCLC, because the disease is most often incurable [19]. The impact of lung cancer and its symptoms on the patient’s psychological, social and physical state should be identified early, and patients should be referred to the appropriate specialist for further assessment, if needed. The literature shows that screening lists for quality-of-life issues could be helpful [11] and that structured follow-up by nurses can improve psychosocial functioning [29]. Failure to provide sufficient information about disease-related issues is the most frequent source of patient dissatisfaction [13]. A good supply of information has positive effects on patient satisfaction and quality of life [16]. Suggested interventions in the literature to make sure that patients are informed properly include printed material [9], consultation preparation packages [7] and audiocassettes of consultations[5].
There are some good examples of instruments that measure patient satisfaction and patient experiences [3, 4, 21, 22], but they are not based on clinical guidelines. Our focus on the evaluation of clinical guidelines can be seen as a complement to other measures to obtain patients’ assessments of the quality of health care. Our evaluation shows an original and innovative approach to the practice test and development of indicators for patient centredness in cancer care. Our set of indicators can be useful to anyone interested in measuring the degree of patient centredness of cancer care. The recommendations on which the indicators are based are not part of all general oncology guidelines. The recommendations for patient centredness on which the indicators are based could be considered for incorporation into general oncology guidelines.
The indicators of patient centredness were measured by means of patient questionnaires. Obviously, the subjective opinion of patients may have biased the outcome to some degree. The outcome of treatment and the stage of the disease may have had a negative impact on the recall of initial conversations with the doctor. To deal with this, we asked patients for their actual experiences of clinical care, as suggested in the literature, and not for their satisfaction with care provided [10]. It should be noted that the literature is contradictory about the influence of patient characteristics on their assessments of care [17, 33].
Conclusion
In conclusion, the development of a valid set of indicators for the patient centredness of cancer care is an initial step towards improvement. Indicators can be based on recommendations from guidelines, but adding patients’ opinions leads to a more complete picture of patient centredness. In this study, we have developed and tested a general set of indicators for patient centredness. Our practice test showed that many of them appeared to be useful for patients with NSCLC and that there are many improvement opportunities. Our set of indicators may also be useful for future quality assessments for other patients with cancers or chronic diseases. Therefore, the indicators developed in this study should be verified in a practice test in other patient groups to see which indicators also apply to them.
Acknowledgements
We thank our contacts at the six participating hospitals for their cooperation: M. van der Drift, Radboud University Hospital, Nijmegen; H. Smit, Rijnstate Hospital, Arnhem; R. Termeer, Canisius Wilhelmina Hospital, Nijmegen; R. Bunnik, Pantein Hospital, Boxmeer; M. Oudijk, Gelders Valley Hospital, Ede and G. Bosman, Slingeland Hospital, Doetinchem.
Conflict of interest
No conflicts of interest
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Footnotes
Radboud University Nijmegen Medical Centre, The Netherlands.
East Comprehensive Cancer Centre, Nijmegen, The Netherlands.
References
- 1.Allgar VL, Neal RD. Delays in the diagnosis of six cancers: analysis of data from the National Survey of NHS Patients: cancer. Br J Cancer. 2005;92:1959–1970. doi: 10.1038/sj.bjc.6602587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boyle P, Ferlay J. Cancer incidence and mortality in Europe. Ann Oncol. 2004;16:481–488. doi: 10.1093/annonc/mdi098. [DOI] [PubMed] [Google Scholar]
- 3.Bredart A, Mignot V, Rousseau A, Dolbeault S, Beauloye N, Adam V. Validation of the EORTC QLQ-SAT32 cancer inpatient satisfaction questionnaire by self- versus interview-assessment comparison. Patient Educ Couns. 2004;54:207–2012. doi: 10.1016/S0738-3991(03)00210-6. [DOI] [PubMed] [Google Scholar]
- 4.Bredart A, Bottomley A, Blazeby JM, Conroy T, Coens C, D’Haese S. An international prospective study of the EORTC cancer in-patient satisfaction with care measure (EORTC IN-PATSAT32) Eur J Cancer. 2005;41:2120–2131. doi: 10.1016/j.ejca.2005.04.041. [DOI] [PubMed] [Google Scholar]
- 5.Bruera E, Pituskin E, Calder K, Neumann CM, Hanson J. The addition of an audiocassette recording of a consultation to written recommendations for patients with advanced cancer: a randomized, controlled trial. Cancer. 1999;86:2420–2425. doi: 10.1002/(SICI)1097-0142(19991201)86:11<2420::AID-CNCR33>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 6.Burgers JS, Fervers B, Haugh M, Brouwers M, Browman G, Philip T. International assessment of the quality of clinical practice guidelines in oncology using the appraisal of guidelines and research and evaluation instrument. J Clin Oncol. 2004;22:2000–2007. doi: 10.1200/JCO.2004.06.157. [DOI] [PubMed] [Google Scholar]
- 7.Butow P, Devine R, Boyer M, Pendlebury S, Jackson M, Tattersall MH. Cancer consultation preparation package: changing patients but not physicians is not enough. J Clin Oncol. 2004;22:4401–4409. doi: 10.1200/JCO.2004.66.155. [DOI] [PubMed] [Google Scholar]
- 8.Campbell SM, Braspenning J, Hutchinson A, Marshall MN. Research methods used in developing and applying quality indicators in primary care. BMJ. 2003;326:816–819. doi: 10.1136/bmj.326.7393.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chan Y, Irish JC, Wood SJ, Rotstein LE, Brown DH, Gullane PJ. Patient education and informed consent in head and neck surgery. Arch Otolaryngol Head Neck Surg. 2002;128:1269–1274. doi: 10.1001/archotol.128.11.1269. [DOI] [PubMed] [Google Scholar]
- 10.Coulter A. Can patients assess the quality of health care? BMJ. 2006;333:1–2. doi: 10.1136/bmj.333.7557.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Detmar SB, Muller MJ, Schornagel JH, Wever LD, Aaronson NK. Health-related quality-of-life assessments and patient–physician communication: a randomized controlled trial. JAMA. 2002;288:3027–3034. doi: 10.1001/jama.288.23.3027. [DOI] [PubMed] [Google Scholar]
- 12.DeVillis R. Scale development. Applications and theory. Newbury Park, CA: Sage; 1991. [Google Scholar]
- 13.Grol R, Wensing M, Mainz J, Jung HP, Ferreira P, Hearnshaw H. Patients in Europe evaluate general practice care: an international comparison. Br J Gen Pract. 2000;50:882–887. [PMC free article] [PubMed] [Google Scholar]
- 14.Grol R, Cluzeau FA, Burgers JS. Clinical practice guidelines: towards better quality guidelines and increased international collaboration. Br J Cancer. 2003;89(Suppl):S4–S8. doi: 10.1038/sj.bjc.6601077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grol R, Wensing M, Eccles M. Improving patient care; the implementation of change in clinical practice. London: Elsevier; 2005. [Google Scholar]
- 16.Haggmark C, Bohman L, Ilmoni-Brandt K, Naslund I, Sjoden PO, Nilsson B. Effects of information supply on satisfaction with information and quality of life in cancer patients receiving curative radiation therapy. Patient Educ Couns. 2001;45:173–179. doi: 10.1016/S0738-3991(01)00116-1. [DOI] [PubMed] [Google Scholar]
- 17.Hargraves JL, Wilson IB, Zaslavsky A, James C, Walker JD, Rogers G. Adjusting for patient characteristics when analyzing reports from patients about hospital care. Med Care. 2001;39:635–641. doi: 10.1097/00005650-200106000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Hermens RP, Ouwens MM, Vonk-Okhuijsen SY, van der Wel Y, Tjan-Heijnen VC, van den Broek LD. Development of quality indicators for diagnosis and treatment of patients with non-small cell lung cancer: a first step toward implementing a multidisciplinary, evidence-based guideline. Lung Cancer. 2006;54:117–124. doi: 10.1016/j.lungcan.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 19.Janssen-Heijnen ML, Coebergh JW. The changing epidemiology of lung cancer in Europe. Lung Cancer. 2003;41:245–258. doi: 10.1016/S0169-5002(03)00230-7. [DOI] [PubMed] [Google Scholar]
- 20.Jenkins V, Fallowfield L, Saul J. Information needs of patients with cancer: results from a large study in UK cancer centres. Br J Cancer. 2001;5(84):48–51. doi: 10.1054/bjoc.2000.1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jenkinson C, Coulter A, Bruster S. The Picker Patient Experience Questionnaire: development and validation using data from in-patient surveys in five countries. Int J Qual Health Care. 2002;14:353–358. doi: 10.1093/intqhc/14.5.353. [DOI] [PubMed] [Google Scholar]
- 22.Jenkinson C, Coulter A, Bruster S, Richards N, Chandola T. Patients’ experiences and satisfaction with health care: results of a questionnaire study of specific aspects of care. Qual Saf Health Care. 2002;11:335–339. doi: 10.1136/qhc.11.4.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kash KM, Mago R, Kunkel EJ. Psychosocial oncology: supportive care for the cancer patient. Semin Oncol. 2005;32:211–218. doi: 10.1053/j.seminoncol.2004.11.011. [DOI] [PubMed] [Google Scholar]
- 24.Kerr D, Bevan H, Gowland B, Penny J, Berwick D. Redesigning cancer care. BMJ. 2002;324:164–166. doi: 10.1136/bmj.324.7330.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lewin SA, Zwarenstein M. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev. 2001;4:CD003267. doi: 10.1002/14651858.CD003267. [DOI] [PubMed] [Google Scholar]
- 26.Malin JL, Asch SM, Kerr EA, McGlynn EA. Evaluating the quality of cancer care: development of cancer quality indicators for a global quality assessment tool. Cancer. 2000;88:701–707. doi: 10.1002/(SICI)1097-0142(20000201)88:3<701::AID-CNCR29>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 27.Malin JL, Schneider EC, Epstein AM, Adams J, Emanuel EJ, Kahn KL. Results of the National Initiative for Cancer Care Quality: how can we improve the quality of cancer care in the United States? J Clin Oncol. 2006;24:626–634. doi: 10.1200/JCO.2005.03.3365. [DOI] [PubMed] [Google Scholar]
- 28.Mead N, Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Soc Sci Med. 2000;51:1087–1110. doi: 10.1016/S0277-9536(00)00098-8. [DOI] [PubMed] [Google Scholar]
- 29.Moore S, Corner J, Haviland J, Wells M, Salmon E, Normand C. Nurse led follow up and conventional medical follow up in management of patients with lung cancer: randomised trial. BMJ. 2002;325:1145. doi: 10.1136/bmj.325.7373.1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Oskay-Ozcelik G, Lehmacher W, Konsgen D, Christ H, Kaufmann M, Lichtenegger W. Breast cancer patients’ expectations in respect of the physician-patient relationship and treatment management results of a survey of 617 patients. Ann Oncol. 2007;18:479–484. doi: 10.1093/annonc/mdl456. [DOI] [PubMed] [Google Scholar]
- 31.Ouwens MM, Marres HA, Hermens RR, Hulscher MM, van den Hoogen FJ, Grol RP. Quality of integrated care for patients with head and neck cancer: development and measurement of clinical indicators. Head Neck. 2007;29:378–386. doi: 10.1002/hed.20532. [DOI] [PubMed] [Google Scholar]
- 32.Piro L, Doctor J. Managed oncology care: the disease management model. Cancer. 1998;82(10 Suppl):2068–2075. doi: 10.1002/(SICI)1097-0142(19980515)82:10+<2068::AID-CNCR16>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 33.Sandoval GA, Brown AD, Sullivan T, Green E. Factors that influence cancer patients’ overall perceptions of the quality of care. Int J Qual Health Care. 2006;18:266–274. doi: 10.1093/intqhc/mzl014. [DOI] [PubMed] [Google Scholar]
- 34.Schouten JA, Hulscher ME, Wollersheim H, Braspennning J, Kullberg BJ, van der Meer JW. Quality of antibiotic use for lower respiratory tract infections at hospitals: (how) can we measure it? Clin Infect Dis. 2005;41:450–460. doi: 10.1086/431983. [DOI] [PubMed] [Google Scholar]
- 35.Shilling V, Jenkins V, Fallowfield L. Factors affecting patient and clinician satisfaction with the clinical consultation: can communication skills training for clinicians improve satisfaction? Psychooncology. 2003;12:599–611. doi: 10.1002/pon.731. [DOI] [PubMed] [Google Scholar]
- 36.Wagner EH. Care for chronic diseases. BMJ. 2002;325:913–914. doi: 10.1136/bmj.325.7370.913. [DOI] [PMC free article] [PubMed] [Google Scholar]


