Before rubella vaccine was introduced for schoolgirls and susceptible women in 1970, 200-300 babies were born annually in England and Wales with congenital defects associated with maternal rubella. In 1988 the combined measles, mumps, and rubella vaccine was introduced for all 1 year olds; in 1994, to help avert a predicted measles epidemic, all 5-16 year olds were offered combined measles and rubella vaccine. The schoolgirl immunisation programme has now ceased, but antenatal screening continues, with postpartum vaccination for susceptible women. We report the findings from the national congenital rubella surveillance programme from 1971 to 1996.
Methods and results
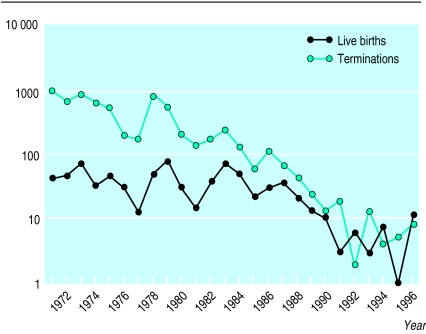
Births of babies with congenital rubella have been monitored through the national programme since 1971, with active surveillance through the British Paediatric Surveillance Unit since 1990.1 The Office for National Statistics records terminations associated with rubella. Reports of such births and terminations have fallen from an average 48 births and 742 terminations annually in 1971-5 to four and nine respectively in 1991-5 (figure). In 1996, however, after a resurgence of rubella infection in the community, 12 births and nine terminations were reported.
In 1991-5 only 4 of 19 mothers of children with reported congenital rubella had been born in Britain; none of these reported vaccination, though three should have been offered it previously. Five women had acquired infection abroad (Bangladesh, India, Pakistan, Thailand, Republic of Ireland) before entering Britain in late pregnancy, and a sixth on holiday in Poland. Another five women had been in Britain less than two years at delivery.
In contrast, in 1996 only 2 of 12 mothers acquired infection abroad, one in Bangladesh and the other (born in Britain) on holiday in Spain. Three of the 10 women who acquired infection in Britain were born abroad but were not recent arrivals. All eight women born in Britain were primigravidas and had been eligible for schoolgirl vaccination. Three women reported previous vaccination—in one, rubella reinfection was confirmed.2
At least 20/31 mothers registered with the programme in 1991-6 had symptomatic rubella infection in pregnancy; eight of these were diagnosed and opted to continue to term. Four women reported symptoms antenatally, but infection was not diagnosed; four reported symptoms retrospectively, and in four it was unclear when symptoms were reported or what action was taken.
Before 1991 about 40% of babies with congenital rubella had typical heart or eye defects, compared with over 80% since then. Rubella IgG antibodies in young children with otherwise unexplained sensorineural hearing loss used to suggest congenital rubella, but as most now have vaccine induced antibodies, hearing loss without other defects due to congenital rubella may be underdiagnosed.
Comment
The decline in reports of congenital rubella has resulted in a higher proportion of cases associated with infection acquired abroad or occurring in women with previous vaccination or infection (neither of which confers absolute protection). Immigrant women are more susceptible than the indigenous population; targeting them for immunisation may be appropriate.
The increased incidence of rubella in spring 1996—concentrated in young men who had never been offered vaccination—was followed by an increase in congenital rubella, with all but one baby (whose mother acquired infection abroad) born between the end of July and mid-October. Uptake of the measles, mumps, and rubella vaccine has declined since 1995 (with the largest decrease in 1997-83) because of public anxiety about vaccine safety.4 If high uptake is not maintained, rubella could once again circulate among young children. Women and health professionals must be aware of the potentially devastating effects of rubella infection. An “immune” result after routine antenatal testing does not preclude recent or current infection, and all pregnant women with suspected symptoms or exposure in the first four months of pregnancy should be offered diagnostic investigation.5
Figure.
Births of babies with congenital rubella (England, Scotland, and Wales) and terminations associated with rubella disease or contact (England and Wales only), 1971-96
Acknowledgments
We thank colleagues at the Public Health Laboratory Service who support and advise the national congenital rubella surveillance programme, particularly those who are responsible for rubella serosurveillance and for the COVER/Körner programmes; paediatricians who have notified cases; the British Paediatric Surveillance Unit; general practitioners; Sense—the National Deafblind and Rubella Association; colleagues at the Institute of Child Health, Scottish Centre for Infection and Environmental Health, and the Office for National Statistics; and everyone else who has contributed to the surveillance programme over many years.
Footnotes
Funding: The national congenital rubella surveillance programme was originally funded by the Medical Research Council and is currently funded by the Public Health Laboratory Service. The British Paediatric Surveillance Unit of the Royal College of Paediatrics and Child Health was supported by the Medical Research Fund of Children Nationwide at the time of the study.
Competing interests: None declared.
References
- 1.Hall SM, Nicoll A. The British Paediatric Surveillance Unit—a pioneering method for investigating the less common disorders of childhood. Child Care Health Dev. 1998;24:129–143. doi: 10.1046/j.1365-2214.1998.00052.x. . (Report of a seminar held in June 1995.) [DOI] [PubMed] [Google Scholar]
- 2.Thomas HIJ. Specific antibody avidity studies in clinical microbiology: past, present and future. PHLS Microbiology Digest. 1995;12(2):97–102. [Google Scholar]
- 3.Sentinel surveillance shows small decline in MMR coverage. Commun Dis Rep CDR Wkly. 1998;8(36):317. , 320. [PubMed] [Google Scholar]
- 4.Begg N, Ramsay M, White J, Bozoky Z. Media dents confidence in MMR vaccine. BMJ. 1998;316:56. [Google Scholar]
- 5.Department of Health; Welsh Office; Scottish Office Department of Health; DHSS (Northern Ireland) Immunisation against infectious disease. London: HMSO; 1996. [Google Scholar]