FEMALE ATHLETES demonstrate a 4 to 6 times higher incidence of non-contact anterior cruciate ligament (ACL) injury than male athletes participating in the same landing and pivoting sports.1-3 This greater risk of ACL injury, coupled with a dramatic increase in participation (doubling each decade), has led to a significant rise in the number of ACL injuries in female athletes. This gender disparity in non-contact ACL injury risk, combined with evidence that the primary cause may be neuromuscular in nature, have lead to the development of neuromuscular interventions designed to prevent injury.4-9 Initial interventions aimed at reducing the incidence of ACL injuries in female athletes were developed based on empirical evidence from coaching and training female athletes and from performance enhancement research.4,10 More current techniques, developed from identified injury mechanism (dynamic knee valgus11) and objective analysis of training methods,12-19 may further reduce traumatic ACL injuries in female athletes.5-7 The programs that have demonstrated ACL injury reduction are comprehensive, and include multiple training components that may induce the neuromuscular changes. The purpose of this report is to discuss the current evidence related to modifiable ACL injury mechanisms during landing and to present a novel “clinician-friendly” assessment and training technique that can be used to identify these mechanisms in high-risk female athletes.
Key Points
Use of the tuck jump assessment to identify neuromuscular imbalances may provide direction for targeted treatment for those at high risk for ACL injury.
Improvement in neuromuscular techniques may be assessed and continually monitored with repeated measurement using the tuck jump assessment.
Multiple factors may underlie the differences in ACL injury risk in male and females, neuromuscular control may be the most important and modifiable factor that can be addressed with plyometric training.
Identification of Modifiable ACL Injury Mechanisms Associated With Landing Techniques
Hewett et al.10 tested the hypothesis that insufficient neuromuscular control of lower limb biomechanics, particularly the knee joint, lead to high risk patterns in female athletes during execution of common (albeit potentially hazardous) movements. The results of this study demonstrated that peak landing forces were significantly predicted by valgus torque at the knee in females, females developed decreased relative knee flexor torque during landing compared to males, and females had greater side to side differences in normalized hamstrings peak torque. Ford et al.20 demonstrated similar gender differences during the performance of a drop vertical jump from a drop height of 31 cm. This study determined that female athletes landed with a greater maximum valgus knee angle and greater total valgus knee motion than male athletes. Female athletes also had significant differences between dominant and non-dominant side in maximum valgus knee angle. These differences in valgus measures and limb-to-limb asymmetries reflect neuromuscular deficits that may be indicative of decreased dynamic knee joint control in female athletes.20 Kernozek and colleagues also reported similar coronal plane gender differences in their investigation of drop landing from a greater height (60 cm).21
Subsequent studies evaluated more proximal neuromuscular control at the hip and trunk to help determine a potential contributing mechanism to high risk knee mechanics during landing.22,23 When performing single-leg landing tasks, female athletes demonstrated increased trunk flexion and lateral tilt. This decreased proximal control was hypothesized to be a potential contributor to high-risk mechanics at the knee.24 Further evidence from multiple, potentially high-risk landing movements indicated that variables at the hip contributed to dynamic valgus while electromyographic (EMG) data demonstrated female to male differences in firing patterns of the hip musculature.22 The purpose of these studies was to identify gender differences in hip motion, kinetics, and muscle firing patterns during single-leg agility and landing maneuvers. The hypothesis was that female athletes would display increased hip adduction angles and external adduction moments during this multicomponent dynamic maneuver that may contribute to lower extremity valgus. The results demonstrated that female athletes had greater hip adduction angles and torques than males during multidirectional single-leg landing. These differences were limited to the frontal plane and were not observed in the sagittal plane. EMG patterns showed increased quadriceps firing and decreased gluteal firing in females.22 Another study examined gender differences during single-leg landings from either a medial or lateral direction.25 In addition to greater knee abduction angles (valgus displacement), female athletes had increased hip coronal plane excursion compared to males during both types of landings.25 The increased hip adduction (hip varus) motion seen in the coronal plane during athletic activities likely contributes to the dynamic valgus knee position that may place the athlete at increased risk for ACL injury.23,25
Potential to Modify Landing Techniques and Reduce ACI Injury Risk
There is strong evidence that neuromuscular training decreases ACL injury incidence,4-9,19 and that it alters a biomechanical risk factor (knee abduction) for ACL injury13,16,17 and improves the performance capabilities of female athletes.10,13,15 Effective neuromuscular training programs utilize plyometric power training, biomechanical technique training, strength training, balance training, and core stability training to induce neuromuscular changes.5,7,10,13,15-17,26,27 A systematic review18 of the published literature yielded six interventions that targeted ACL injury prevention in female athletes.4,7-9,26,28 Out of these six studies, four significantly reduced knee injury incidence in both genders and three significantly reduced ACL injury incidence in females. A meta-analysis19 of these six studies demonstrated a significant effect of neuromuscular training programs on ACL injury incidence in female athletes (Z = 4.31, P <.001). Examination of the similarities and differences between the training regimens may provide insight into the development of more effective and efficient interventions.18
Exercise Modes and Techniques Used to Reduce ACL Injury Risk
When comparing the data extracted from the intervention studies, one might generate a few potentially valuable generalizations. Plyometric training combined with biomechanical analysis and technique training were the two common components of all 4 studies that effectively reduced ACL injury incidence.4-7 In addition, balance training alone is probably not as effective for injury prevention as when it is combined with other types of training.18 One needs to consider whether the teams’ or athletes’ primary goal is injury prevention, performance enhancement or both. In-season training alone is probably the most cost-effective and efficient method for achieving beneficial injury prevention effects,5,19 though the absence of high-intensity overload in these programs may preclude measurable performance enhancement effects. High-intensity pre-season neuromuscular training programs are effective to increase performance and reduce injury risk.10,13,17,27 Probably the most important finding, however, is that all four studies4-7 that incorporated high-intensity plyometrics reduced incidence of ACL injuries, while the studies that did not incorporate high-intensity plyometrics8,9 had no reduction in incidence of ACL injuries.19
The plyometric component of these interventions, which trains the muscles, connective tissue, and nervous system to effectively carry out the stretch-shortening cycle29 and that focuses on proper technique and body mechanics, appears to reduce ACL injuries.4-7 Injury prevention programs that combine techniques demonstrated to enhance performance capabilities have positive preventive and biomechanical effects;13,18 however, training programs that utilized more single-faceted training approaches that did not incorporate plyometric training have demonstrated limited success in reducing knee injury incidence or risk factors in female athletes.9,30-32
“Clinician-Friendly” Plyometric Assessment and Technique Training
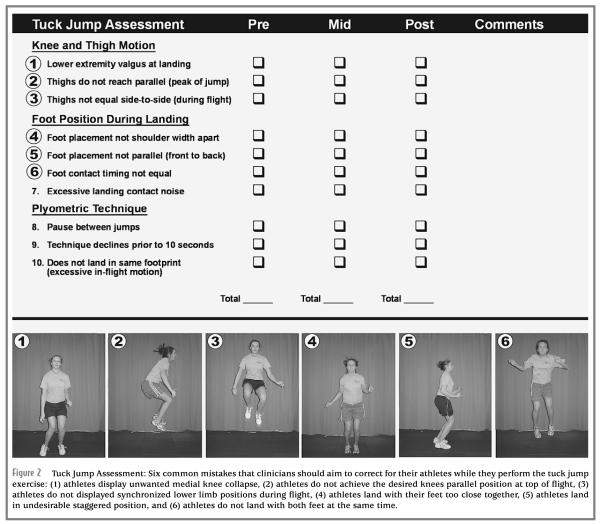
The tuck jump exercise (Figure 1) may be useful to the clinician for the identification of lower extremity landing technique flaws during a plyometric activity.12 The tuck jump requires a high-level effort from the athlete. Initially, the athlete may place most of his or her cognitive efforts solely on the performance of this difficult jump. The clinician may readily identify potential performance deficiencies (Figure 2), especially during the first few repetitions.12 In addition, the tuck jump exercise may be used to assess improvement in lower extremity biomechanics as the athletes progress through their training.12
Figure 1.
Tuck jumps are an example of an exercise used to train athletes to increase lower body power. The tuck jump can also be used as an assessment to grade improvement in technique. to perform the tuck jump, athletes start in the athletic position with feet shoulder-width apart. They initiate the jump with a slight crouch downward while extending their arms behind them. They then swing their arms forward as they simultaneously jump straight up and pull their knees up as high as possible. At the highest point of the jump, the athletes are in the air with thighs parallel to the ground. When landing, the athletes should immediately begin the next tuck jump. Encourage the athletes to land softly, using a toe to mid-foot rocker landing. The athletes should not continue this jump if they cannot control the high landing force or if they demonstrate a knock-kneed landing.
Figure 2.
Tuck Jump Assessment: Six common mistakes that clinicians should aim to correct for their athletes while they perform the tuck jump exercise: (1) athletes display unwanted medial knee collapse, (2) athletes do not achieve the desired knees parallel position at top of flight, (3) athletes do not displayed synchronized lower limb positions during flight, (4) athletes land with their feet too close together, (5) athletes land in undesirable staggered position, and (6) athletes do not land with both feet at the same time.
Figure 2 provides the “clinician friendly” landing technique assessment clinicians may use to monitor an athlete’s performance of the tuck jump before, during, and after training. Specifically, the athletes perform repeated tuck jumps for 10 seconds, which allows the clinician to visually grade the outlined criteria. To further improve accuracy of the assessment, standard 2D camera photos acquired in the frontal and sagittal planes may be utilized to assist the clinician. The athletes’ techniques (Figure 2) are subjectively rated as either having an apparent deficit (checked) or not. The deficits are then tallied for the final assessment score. Indicators of flawed techniques should be noted for each athlete and should be the focus of feedback during subsequent training sessions. The athletes’ baseline performances can be compared to repeated assessments performed at the mid-point and conclusion of a training program, to objectively track improvement with jumping and landing technique (Figure 2). Empirical evidence from our laboratory suggests that athletes who do not improve their scores, or who demonstrate 6 or more flawed techniques, should be targeted for further technique training. Pilot work in our laboratory has indicated that the intrarater reliability is high; R = 0.84 (range 0.72-0.97). These data indicate that the tuck jump assessment may be adequate for a single clinician to reassess athletes to determine changes in technical performance of the tuck jump exercise.33 Additional investigation between clinicians is currently being performed.
One specific area that the clinician should focus on when training to reduce incidence of ACL injury is the correction of lower extremity valgus at landing and equalization of side-to-side differences in lower extremity movements, which are both emphasized in the tuck jump assessment (Figure 2). The link between valgus knee loading and resultant increases in ACL strain has been demonstrated through cadaver, in vivo, and computer modeling experiments.34-37 Valgus torque on the knee can significantly increase tibial subluxation and load on the ACL.36 A prospective combined biomechanical-epidemiologic study showed that knee abduction moments (valgus torque) and angles measured during a plyometric activity were significant predictors of future ACL injury.11 The tuck jump assessment can be utilized to improve these high-risk deficiencies during an exercise that requires a high-level effort from the athlete. Athletes may place most of their cognitive efforts on the performance of this difficult jump and demonstrate many technical flaws that are indicative of increased risk for injury; however, if they can improve neuromuscular control during this difficult jump and landing sequence, they may gain skill that can be transferred to competitive play.
Conclusion
The authors acknowledge that more research is needed to determine the validity and between-rater reliability of the proposed assessment method. However, the use of the tuck jump assessment may provide a clinician-friendly means to identify high-risk landing mechanics and may provide direction for a targeted intervention to reduce risk of ACL injury.17 In addition, improvement in neuromuscular control may be assessed and continually monitored with repeated testing of the athlete. Although multiple factors may underlie the differences in ACL injury risk between males and females, neuromuscular control may be the most important and modifiable factor.
Acknowledgment
The authors would like to acknowledge funding support from National Institutes of Health, Grant R01-AR 049735.
Biography
Gregory D. Myer is the sports biomechanist at the Cincinnati Children’s Hospital Sports Medicine Biodynamics Center. His work in the Human Performance Laboratory allows him to incorporate the most advanced research findings into athletic development and injury prevention training protocols.
Kevin R. Ford is a research biomechanist at the Cincinnati Children’s Hospital Sports Medicine Biodynamics Center. His area of research is focused on applied full body biomechanics in injury prevention.
Timothy E. Hewett is the Director of the Sports Medicine Biodynamics Center at Cincinnati Children’s Hospital Medical Center and Associate Professor of Pediatrics, Orthopaedic Surgery, Biomedical Engineering and Rehabilitation Sciences at the University of Cincinnati. Dr. Hewett’s work focuses on the mechanisms and prevention of ACL injury.
References
- 1.Myklebust G, Maehlum S, Holm I, Bahr R. A prospective cohort study of anterior cruciate ligament injuries in elite Norwegian team handball. Scand J Med Sci Sports. 1998;8(3):149–153. doi: 10.1111/j.1600-0838.1998.tb00185.x. [DOI] [PubMed] [Google Scholar]
- 2.Malone TR, Hardaker WT, Garrett WE, Feagin JA, Bassett FH. Relationship of gender to anterior cruciate ligament injuries in intercollegiate basketball players. J South Orthop Assoc. 1993;2(1):36–39. [Google Scholar]
- 3.Arendt E, Dick R. Knee injury patterns among men and women in collegiate basketball and soccer. NCAA data and review of literature. Am J Sports Med. 1995;23(6):694–701. doi: 10.1177/036354659502300611. [DOI] [PubMed] [Google Scholar]
- 4.Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. The effect of neuromuscular training on the incidence of knee injury in female athletes. a prospective study. Am J Sports Med. 1999 Nov-Dec;27(6):699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 5.Mandelbaum BR, Silvers HJ, Watanabe D, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing the incidence of ACL injuries in female athletes: two-year follow up. Am J Sport Med. 2005;33(6):1003–1010. doi: 10.1177/0363546504272261. [DOI] [PubMed] [Google Scholar]
- 6.Petersen W, Braun C, Bock W, et al. A controlled prospective case control study of a prevention training program in female team handball players: the German experience. Arch Orthop Trauma Surg. 2006;125(9):614–621. doi: 10.1007/s00402-005-0793-7. [DOI] [PubMed] [Google Scholar]
- 7.Myklebust G, Engebretsen L, Braekken IH, Skjolberg A, Olsen OE, Bahr R. Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sport Med. Mar. 2003;13(2):71–78. doi: 10.1097/00042752-200303000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Heidt RS, Jr., Sweeterman LM, Carlonas RL, Traub JA, Tekulve FX. Avoidance of soccer injuries with preseason conditioning. Am J Sports Med. 2000 Sep-Oct;28(5):659–662. doi: 10.1177/03635465000280050601. [DOI] [PubMed] [Google Scholar]
- 9.Soderman K, Werner S, Pietila T, Engstrom B, Alfredson H. Balance board training: prevention of traumatic injuries of the lower extremities in female soccer players? A prospective randomized intervention study. Knee Surg Sports Traumatol Arthrosc. 2000;8(6):356–363. doi: 10.1007/s001670000147. [DOI] [PubMed] [Google Scholar]
- 10.Hewett TE, Stroupe AL, Nance TA, Noyes FR. Plyometric training in female athletes. Decreased impact forces and increased hamstring torques. Am J Sports Med. 1996;24(6):765–773. doi: 10.1177/036354659602400611. [DOI] [PubMed] [Google Scholar]
- 11.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005 Feb 8;33(4):492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 12.Myer GD, Ford KR, Hewett TE. Rationale and clinical techniques for anterior cruciate ligament injury prevention among female athletes. J Athl Train. 2004 Dec;39(4):352–364. [PMC free article] [PubMed] [Google Scholar]
- 13.Myer GD, Ford KR, Palumbo JP, Hewett TE. Neuromuscular training improves performance and lower-extremity biomechanics in female athletes. J Strength Cond Res. 2005 Feb;19(1):51–60. doi: 10.1519/13643.1. [DOI] [PubMed] [Google Scholar]
- 14.Myer GD, Ford KR, Brent JL, Hewett TE. The effects of plyometric versus dynamic balance training on landing force and center of pressure stabilization in female athletes. Br J Sports Med. 2005;39(6):397. [Google Scholar]
- 15.Myer GD, Ford KR, Brent JL, Hewett TE. The effects of plyometric versus dynamic balance training on power, balance and landing force in female athletes. J Strength Cond Res. 2006;20(2):345–353. doi: 10.1519/R-17955.1. [DOI] [PubMed] [Google Scholar]
- 16.Myer GD, Ford KR, McLean SG, Hewett TE. The effects of plyometric versus dynamic stabilization and balance training on lower extremity biomechanics. Am J Sports Med. 2006;34(3):490–498. doi: 10.1177/0363546505281241. [DOI] [PubMed] [Google Scholar]
- 17.Myer GD, Ford KR, Brent JL, Hewett TE. Differential neuromuscular training effects on ACL injury risk factors in “high-risk” versus “low-risk” athletes. BMC Musculoskelet Disord. 2007;8(39):1–7. doi: 10.1186/1471-2474-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hewett TE, Myer GD, Ford KR. Reducing knee and anterior cruciate ligament injuries among female athletes: a systematic review of neuromuscular training interventions. J Knee Surg. 2005 Jan;18(1):82–88. doi: 10.1055/s-0030-1248163. [DOI] [PubMed] [Google Scholar]
- 19.Hewett TE, Ford KR, Myer GD. Anterior cruciate ligament injuries in female athletes: part 2, a meta-analysis of neuromuscular interventions aimed at injury prevention. Am J Sports Med. 2006 Dec 28;34(3):490–498. doi: 10.1177/0363546505282619. [DOI] [PubMed] [Google Scholar]
- 20.Ford KR, Myer GD, Hewett TE. Valgus knee motion during landing in high school female and male basketball players. Med Sci Sports Exerc. 2003 Oct;35(10):1745–1750. doi: 10.1249/01.MSS.0000089346.85744.D9. [DOI] [PubMed] [Google Scholar]
- 21.Kernozek TW, Torry MR, H. VH, Cowley H, Tanner S. Gender differences in frontal and sagittal plane biomechanics during drop landings. Med Sci Sports Exerc. 2005 Jun;37(6):1003–1012. discussion 1013. [PubMed] [Google Scholar]
- 22.Zazulak BT, Ponce PL, Straub SJ, Medvecky MJ, Avedisian L, Hewett TE. Gender comparison of hip muscle activity during single-leg landing. J Orthop Sports Phys Ther. 2005 May;35(5):292–299. doi: 10.2519/jospt.2005.35.5.292. [DOI] [PubMed] [Google Scholar]
- 23.Hewett TE, Ford KR, Myer GD, Wanstrath K, Scheper M. Gender differences in hip adduction motion and torque during a single leg agility maneuver. J Orthop Res. 2006;24(3):416–421. doi: 10.1002/jor.20056. [DOI] [PubMed] [Google Scholar]
- 24.Ford KR, Myer GD, Hewett TE. Increased trunk motion in female athletes compared to males during single leg landing. Med Sci Sports Exerc. 2007;39(5):S70. [Google Scholar]
- 25.Ford KR, Myer GD, Smith RL, Vianello RM, Seiwert SL, Hewett TE. A comparison of dynamic coronal plane excursion between matched male and female athletes when performing single leg landings. Clin Biomech. 2006;21(1):33–40. doi: 10.1016/j.clinbiomech.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 26.Petersen W, Braun C, Bock W, et al. A controlled prospective case control study of a prevention training program in female team hand-ball players: the German experience. Arch Orthop Trauma Surg. 2005 Feb 10; doi: 10.1007/s00402-005-0793-7. [DOI] [PubMed] [Google Scholar]
- 27.Hewett TE, Paterno MV, Noyes FR. Differences in single leg Balance on an unstable platform between female and male normal, ACL-deficient and ACL-reconstructed knees. In: Lephardt S, Fu FH, editors. Proprioception and Neuromuscular Control in Joint Stability. Human Kinetics; Champaign, IL: 1999. pp. 77–88. [Google Scholar]
- 28.Mandelbaum BR, Silvers HJ, Watanabe D, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing the incidence of ACL injuries in female athletes: two-year follow up. Am J Sports Med. 2004 doi: 10.1177/0363546504272261. In Press. [DOI] [PubMed] [Google Scholar]
- 29.Chmielewski TL, Myer GD, Kauffman D, Tillman S. Plyometric Exercise in the rehabilitation of athletes: physiological responses and clinical application. J Orthop Sports Phys Ther. 2006;36(5):308–319. doi: 10.2519/jospt.2006.2013. [DOI] [PubMed] [Google Scholar]
- 30.Pfeiffer RP, Shea KG, Roberts D, Grandstrand S, Bond L. Lack of effect of a knee ligament injury prevention program on the incidence of noncontact anterior cruciate ligament injury. J Bone Joint Surg Am. 2006 Aug;88(8):1769–1774. doi: 10.2106/JBJS.E.00616. [DOI] [PubMed] [Google Scholar]
- 31.Mcginn PA, Mattacola CG, Malone TR, Johnson DL, Shapiro R. Strength training for 6 weeks does not significanlty alter landing mechanics of female collegiate basketball athletes. J Orthopaed Sports Physic Ther. 2007;37(2):A24. [Google Scholar]
- 32.Herman DC, Weinhold PS, Guskiewicz KM, Garrett WE, Yu B, Padua DA. The effects of strength training on the lower extremity biomechanics of female recreational athletes during a stop-jump task. Am J Sports Med. 2008 Jan 22; doi: 10.1177/0363546507311602. [DOI] [PubMed] [Google Scholar]
- 33.Myer GD, Paterno MV, Ford KR, Quatman CE, Hewett TE. Rehabilitation after anterior cruciate ligament reconstruction: criteria based progression through the return to sport phase. J Orthop Sports Phys Ther. 2006;36(6):385–402. doi: 10.2519/jospt.2006.2222. [DOI] [PubMed] [Google Scholar]
- 34.Markolf KL, Burchfield DM, Shapiro MM, Shepard MF, Finerman GA, Slauterbeck JL. Combined knee loading states that generate high anterior cruciate ligament forces. J Orthop Res. 1995 Nov;13(6):930–935. doi: 10.1002/jor.1100130618. [DOI] [PubMed] [Google Scholar]
- 35.Kanamori A, Woo SL, Ma CB, et al. The forces in the anterior cruciate ligament and knee kinematics during a simulated pivot shift test: a human cadaveric study using robotic technology. Arthroscopy. 2000 Sep;16(6):633–639. doi: 10.1053/jars.2000.7682. [DOI] [PubMed] [Google Scholar]
- 36.Fukuda Y, Woo SL, Loh JC, et al. A quantitative analysis of valgus torque on the ACL: a human cadaveric study. J Orthop Res. 2003 Nov;21(6):1107–1112. doi: 10.1016/S0736-0266(03)00084-6. [DOI] [PubMed] [Google Scholar]
- 37.Lloyd DG, Buchanan TS. Strategies of muscular support of varus and valgus isometric loads at the human knee. J Biomech. 2001;34(10):1257–1267. doi: 10.1016/s0021-9290(01)00095-1. [DOI] [PubMed] [Google Scholar]