Abstract
Although early natural menopause has been postulated to increase stroke risk, studies have not produced convincing results. We examined the associations between stroke risks and age at natural menopause or time since natural menopause. 5,731 naturally postmenopausal women more than 65 yr of age were followed from 1993 to 1998. Information on age at menopause and risk factors were obtained using mailed questionnaires. 186 cases of stroke occurred over a total 27,936 person years. After adjusting for age, hypertension, and physical activity, age at menopause was not found to be significantly associated with stroke or cerebral infarction. However, adjusted relative risks (aRRs) showed a significant increasing tendency of hemorrhagic stroke versus age at menopause (aRRs, 0.66, 0.48, 1.00 and 2.33 for the following age groups at menopause; 40-44, 45-49, 50-54 [reference group], and ≥55 yr). Time since menopause (11-20, 21-30, and ≥31 yr) was not found to be significantly associated with cerebral infarction, or hemorrhagic stroke. Late menopause (menopause age ≥55 yr) showed a tendency of a lower risk of cerebral infarction (aRR, 0.79) and a higher risk of hemorrhagic stroke (aRR, 2.33). Further study is warranted to determine stroke risk in women during the decade following menopause.
Keywords: Menopause, Stroke, Cerebrovascular Accident, Aged, Women, Cohort Studies
INTRODUCTION
The incidence of stroke is generally higher in men than in women, but this difference decreases above age 65 (1). Premenopausal women seem to be protected against cardiovascular morbidity and mortality as compared with postmenopausal women of a similar age (2, 3). The loss of ovarian function and the subsequent endogenous estrogen deficiency have been suggested to increase the risk of cardiovascular disease and death after menopause (4, 5). Moreover, if endogenous estrogen protects against stroke, an early menopause might incur a higher risk, because of a lower exposure to estrogen. However, evidence supporting this hypothesis is inconclusive (6-10), and most studies have limitations.
An 18-yr study of 35,616 naturally postmenopausal women, age at natural menopause was not found to be significantly associated with ischemic or hemorrhagic stroke (6). Other studies that reported an insignificant association between age at menopause and severe stroke leading to death investigated mortality risk due to stroke, and not the total risk of incidental stroke (7, 8). These studies also investigated the mortality risk of stroke by combining ischemic and hemorrhagic stroke, and did not investigate them separately (7, 8). However, in a 20-yr study of 12,115 women, an early menopause was found to be significantly associated with a higher risk of cardiovascular death (9), but the study was designed to investigate the association between age at menopause and total cardiovascular mortality, which included stroke and coronary heart disease as a single entity. The study found that women with a late menopause had significantly less atherosclerosis of the carotid artery than women with an early menopause, but was limited, because women with a natural menopause and women with an artificial menopause due to surgery were not segregated (10). Moreover, sex hormone concentrations in postmenopausal women seem to decrease with time since menopause (11). However, no study has been conducted on the association between time since menopause and stroke.
Stroke occurs more frequently among Asians and Blacks than among Caucasians (1, 12, 13). However, to the best of our knowledge, the association between age at menopause and stroke has not yet been studied in Asian countries. Thus, the aim of this study was to examine the association between age at menopause or time since menopause and the risk of stroke in Korean elderly women that had experienced a natural menopause.
MATERIALS AND METHODS
Subjects and assessment of risk factors
The Korean Elderly Pharmacoepidemiologic Cohort (KEPEC) was a dynamic cohort that consisted of 46,113 beneficiaries of the Korean Medical Insurance Corporation (KMIC) between 1993 and 1998. The subjects were the parents of school teachers or government employees in Busan, Korea, and were aged 65 yr or more (14). The total number of women registered by the KEPEC was 28,883, and 9,573 of these responded to a baseline survey instigated via a mailed questionnaire, and provided written consent. In addition, 6,468 women reported age at menopause on the questionnaire survey.
The baseline survey self-administered questionnaire had been previously evaluated and found to have good validity medical history, smoking (never, ex-smoker, current-smoker), alcohol consumption (never, ex-drinker, current-drinker), weight, height, salt diet (low, medium, high), physical activity (frequency of climbing stairs above ten; rare, sometimes, often), parity, age at first birth, age at last birth, breast feeding, history of hysterectomy or ovariectomy, and use of postmenopausal hormones. In a validation study using a subsample of the KEPEC, the reliability coefficients of age at menopause were 0.99 for self-self response and 0.60-0.80 for self-proxy response (15).
Data on 93 women with stroke at baseline, on 24 women not regarded as reliable with respect to reported age at menopause, and on 95 women who used postmenopausal hormones were excluded (no case of stroke occurred in this latter group during the follow-up period). Finally, the data of 525 women who had undergone hysterectomy or ovariectomy were also excluded, because we could not confirm whether these were the causes of menopause. The remaining 5,731 naturally postmenopausal women of more than 65 yr of age were composed our study subjects. All of the study subjects had experience of breast-feeding. We should add that the proportion of women with a biological age of ≥80 was larger in the 23,152 women not included in the present analysis than in the 5,731 women included (10.9% vs. 6.6%).
Ascertainment of stroke
Potential incident cases of stroke that occurred between 1 January 1993 and 31 December 1998 were identified from; claim data at medical care institutions in Busan, mortality data from the Korean National Statistical Office (KNSO), and from women who reported having experienced a stroke during this follow-up period on the questionnaire.
Subjects admitted at hospitals with a diagnosis of International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) 430-434, 436-438 between 1993 and the first half of 1995, or ICD-10/I60-I69 between the latter half of 1995 and 1998, were screened from the claims data. Trained medical students visited the hospitals at which potential cases were admitted to review and abstract medical records using a standard abstracting form. Two neurologists reviewed the abstract forms blindly. Ninety-two cases were designated as confirmed cases based on their fulfilling at least one of the symptoms detailed by the World Health Organization (WHO), i.e., as rapidly developing signs of focal (or global) disturbance of cerebral function (lasting longer than 24 hr or leading to death) without apparent cause other than a vascular origin (16), ICD-9-CM 430-434, 436-438 or ICD-10/I60-I69 on discharge summary, or a brain CT or MRI finding of acute stroke. We included spontaneous subarachnoid hemorrhage, but excluded subdural and extradural hematomas and transient ischemic attacks.
During the period 1993 to 1998, six deaths due to a diagnosis of ICD-9-CM 430-434, 436-438 or ICD-10/I60-I69 were found among mortality data from KNSO. Seventy-three women reported having experienced a stroke during the follow-up period on the questionnaire. In addition to these, 15 cases, for which no medical records were available, but who were admitted with a diagnosis of stroke on claims data, were designated as probable cases.
All cases confirmed by reviewing medical records and probable cases were included in the data analysis, because when we excluded probable cases we obtained near identical results (data not shown). All cases were classified as cerebral infarction, hemorrhagic stroke, or stroke of an unclassified type according to neuroimaging findings, ICD-9-CM or ICD-10.
Statistical analysis
Age at menopause was categorized into 5 groups (i.e., <40, 40-44, 45-49, 50-54 [reference group], ≥55 yr) (6, 7), and time since menopause was categorized into 3 groups (i.e., 11-20 [reference group], 21-30, ≥31 yr). Ninety-three women with a time since menopause of ≤10 yr were excluded from the analysis. The risk of stroke for those ≤10 yr since menopause could not be assessed, because women who experienced natural menopause at an average age and stroke before age 65 were excluded from the present study. The starting point of the follow-up period was the latest date among the date on which any subject reached 65 yr old, the date of becoming a beneficiary of the KMIC in Busan, or 1 January 1993. The end point was the earliest date among the onset date of stroke, the date of death, or 31 December 1998.
Differences in the proportions of potential confounders by age at menopause were assessed using the chi-square test. Crude relative risk (cRR) of all strokes was computed as the rate in a specific category divided by that in the reference category of each potential confounder. Confounders that were differently distributed at p<0.1 and had a significantly high cRR of stroke at p<0.05, were included in the multivariate analysis using Cox's proportional hazard model to examine the association between age at menopause or time since menopause and stroke. We also considered age at menopause as a continuous variable and estimated the adjusted RRs (aRRs) of stroke for each 1-yr increase.
Differences in times between menopause and the onset of any stroke or cerebral infarction for the age at menopause groups were assessed by ANOVA. Difference in times between menopause and the onset of hemorrhagic stroke among these same groups was assessed using the Kruskal-Wallis test.
RESULTS
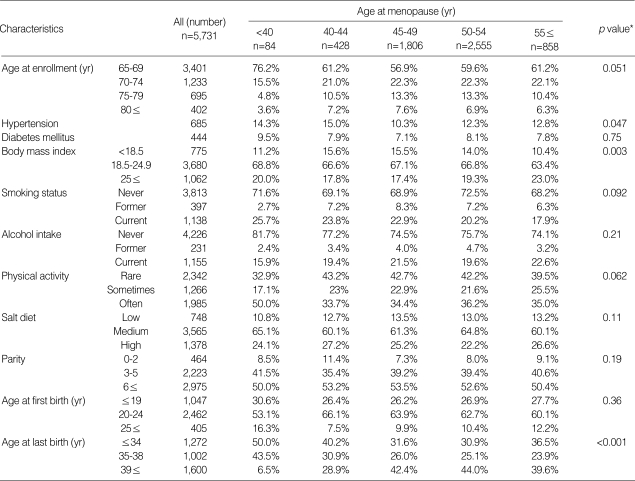
The mean age of the 5,731 study subject at the time of enrollment was 69.8±5.5 yr, and their mean age at natural menopause was 49.6±4.6 yr. History of diabetes mellitus (DM), alcohol intake, salt in diet, parity, and age at first birth were not significantly related to age at menopause. An earlier menopause was associated with a history of hypertension, a lower body mass index (BMI), a younger age at enrollment and at last birth, current smoking, and more frequent exercise (p<0.1) (Table 1).
Table 1.
Subject sociodemographic characteristics and their distributions by age at natural menopause
*p-value by χ2-tests.
During 27,936 person-yr of follow-up, 186 incident cases of stroke (93 of cerebral infarction, 20 of hemorrhagic stroke, and 73 of an unclassified type) occurred. The incidence densities of all strokes, cerebral infarction, and hemorrhagic stroke were 666 (95% confidence interval [CI], 570-762), 333 (95% CI, 265-401) and 72 (95% CI, 40-103) per 100,000 person-years, respectively.
Women with histories of hypertension or DM were found to have an increased risk of stroke, with cRRs of 2.13 (95% CI, 1.49-3.04) and 1.61 (95% CI, 1.01-2.56), respectively. Women who climbed more than ten stairs sometimes or often were at lower risk of stroke (cRR=0.52 and 95% CI, 0.35-0.78, in the "sometimes" group; cRR=0.43 and 95% CI, 0.30-0.62, in the "often" group). No significant changes in the cRRs of stroke were found for; age at enrollment, BMI, smoking status, alcohol intake, salt diet, parity, age at first birth, or age at last birth.
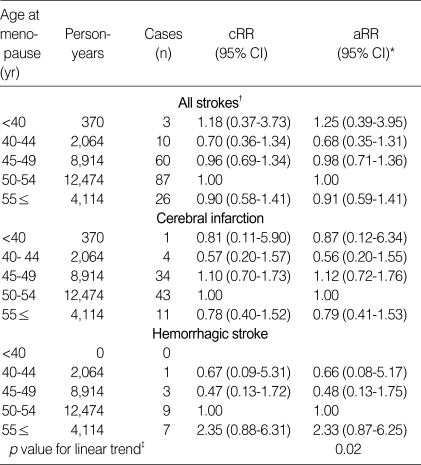
After adjusting for age at enrollment, physical activity, and history of hypertension the aRRs for all strokes were 1.25 (95% CI, 0.39-3.95), 0.68 (95% CI, 0.35-1.31), 0.98 (95% CI, 0.71-1.36), and 0.91 (95% CI, 0.59-1.41) for natural menopause at age <40, 40-44, 45-49, and ≥55 yr, respectively. Further adjustment by age at last birth, BMI, smoking status, and history of DM did not substantially change these estimates (data not shown). The aRR of all strokes was 1.00 (95% CI, 0.97-1.03) for single-year increase interval of age at menopause. For classifiable cerebral infarction and hemorrhagic stroke, no significant changes in aRR were observed in the different age at menopause categories. However, aRRs showed a significant increasing tendency on increasing age at menopause with respect to hemorrhagic stroke (Table 2).
Table 2.
Crude and adjusted relative risks and their 95% confidence intervals (CI) for stroke by age at natural menopause among 5,731 postmenopausal women
*, Adjusted relative risk by Cox's proportional hazard model analysis for age at enrollment, physical activity, and a history of hypertension. †, Strokes of an unclassified type were included in all strokes but were not analyzed separately. ‡, p value determined using likelihood ratio test for the linear trend.
After adjusting for age, a history of hypertension, and physical activity, the aRRs of all strokes among those with a time since menopause of 21-30 or >31 yr were 1.08 (95% CI, 0.69-1.71) and 1.09 (95% CI, 0.53-2.24), respectively. Also, no significant changes were observed in aRRs of cerebral infarction or hemorrhagic stroke among the higher categories of time since menopause.
For the five age at menopause groups (<40, 40-44, 45-49, 50-54 and ≥55 yr), the time intervals between age at menopause and strokes were 29.7±0.4, 32.2±6.4, 27.6±6.0, 22.9±5.7 and 14.8±4.8 yr, and for cerebral infarction were 30.2, 31.5±4.4, 26.9±4.7, 23.8±5.8 and 14.8±4.8 yr. Differences between these times were significant for all strokes (F [4, 181]=29.7, p<0.001) and for cerebral infarction (F [4, 88]=12.9, p<0.001). The mean times between menopause and the onset of hemorrhagic stroke were 27.3, 30.7±8.5, 21.0±4.3 and 13.6±7.2 yr, for four age at menopause groups (40-44, 45-49, 50-54 and ±55 yr), respectively, and these time intervals for the four groups were significantly different (p<0.05).
DISCUSSION
In this prospective cohort study, we found no significant association between a younger age at menopause and a higher risk of stroke or of cerebral infarction among women ≥65 yr old who experienced a natural menopause and had never used postmenopausal hormone.
Women who had experienced younger age at menopause and a stroke before reaching 65 yr old were excluded from this elderly cohort. This might have resulted in no significant association between a younger age at menopause and a higher risk of stroke. However in a 20-yr study of 35,616 women aged 30 to 50 yr, age at natural menopause was not found to be significantly associated with stroke (6).
Because the proportion of women with a younger age at menopause was smaller in our study than in previously reported studies (1.5% vs. 2.4-4.5% and 7.5% vs. 10-11%, for age at menopause of <40 yr and 40-45 yr, respectively) (7-9), the association between a younger age at menopause and a higher risk of stroke might not have been significant. However, in studies with a higher proportion of women with a younger age at menopause, age at natural menopause was found not to be significantly associated with cardiovascular mortality (7, 8).
The risk of cardiovascular mortality due to early menopause has been reported to decrease with increasing biological age (7, 9). However, as the mean age of subjects in the present study was older than those of previous studies (7, 8), this association between an early menopause and stroke risk might not have been significant.
The statistical power of the present study was high, 97.7% (Zβ, -1.99). In a previous autopsy-based study, degree of atherosclerosis was found to rise steadily with increasing biological age (18), however, no association was found between atherosclerosis severity and age at menopause.
Menopause and early menopause were found to be associated with the presence of carotid atherosclerosis in two case-control studies (10, 19). However, in several large-scale prospective studies with a long-term follow-up, age at natural menopause was not found to be associated with the risk of stroke (6-8, 20). Recently, the Heart and Estrogen/Progestin Replacement Study (HERS) found no overall reduction in the risk of stroke among those administered estrogen plus progestin in a randomized, blind, placebo-controlled trial among postmenopausal women with coronary heart disease (21, 22). Hormone replacement therapy was found to be associated with an elevated risk of ischemic stroke (23). It was also reported that long-term hormone therapy increases platelet activation significantly and that this may contribute to thromboembolism development (24).
We observed that the aRRs of hemorrhagic stroke showed a significant increasing tendency as age at menopause increased. A case-control study showed a significant association between a younger age at menarche and higher risk of intracerebral hemorrhage or subarachnoid hemorrhage (25). And, the case-controlled study found that the risks of intracerebral hemorrhage or subarachnoid hemorrhage are significantly higher in women with an age at menopause of 47-49 yr than in women with an age at menopause of ≤46 yr. Moreover, a longer exposure to estrogen may be associated with a high risk of hemorrhagic stroke. However, 73 cases of stroke were unclassified in the present study. Thus the rate of cerebral infarction or hemorrhagic stroke determined by the present study might have been lower than the true rate, and the reliability of our results on the associations between cerebral infarction or hemorrhagic stroke and age at menopause or time since menopause might be limited.
In the present study, increased time since natural menopause was not found to be associated with a higher risk of stroke. Moreover, natural menopause causes a gradual, rather than an abrupt, decline in estrogen production (6). And, the risks of cardiovascular mortality or total mortality, including stroke, due to early menopause have been reported to show a decreasing trend vs. biological age (7, 9). Thus an increase in time since menopause may not be associated with a risk of stroke. However, in the present study, we were unable to assess the risk of stroke in those with a time since menopause of ≤10 yr. Further study is warranted to determine stroke risk in women during the decade following menopause.
The times between menopause and stroke onset seemed to increase with decreasing age at menopause. The sums of mean ages at menopause and the mean times between menopause and stroke onset fell in the range 70 to 74 yr for all five age at menopause groups (<40, 40-44, 45-49, 50-54, ≥55 yr). This result indicates that age at menopause is not associated with the risk of stroke.
The proportion of women with a biological age of ≥80 yr was larger among non-participants in the present analysis, probably because women of this age were unable to respond to the questionnaire due to illiteracy, disease, or indifference. Moreover, elderly women above 80 yr that had experienced a stroke might have been unable to complete the questionnaire. Thus the incidence densities of stroke in this study may have be underestimated.
The accuracy of the present study in terms of assessing risk factors may be limited by the use of a questionnaire approach as compared with direct blood testing or physical examinations. Some women at risk of stroke did not realize that they had risk factors. The presence of hypercholesterolemia was not investigated in this study.
In the present study, we reviewed the medical records of only those stroke cases treated at conventional hospitals in Busan, and thus we cannot comment on those treated at hospitals in areas other than Busan or on those that received traditional (oriental) medical care. Thus, we might have included false positive cases among stroke events. However, after excluding probable cases our results were virtually the same as those obtained when probable cases were included. Our study also has the limitation that it did not examine the association between stroke risk and age at natural menopause in women younger than 65 yr.
In summary, we found no significant association between the risk of stroke for any cause or the risk of cerebral infarction and a younger age at menopause or time since menopause, among women over 65 yr of age who had experienced a natural menopause and had never used hormone therapy. For hemorrhagic stroke, we observed a significant tendency for aRRs to increase as age at menopause increased. Further study of the possible associations between the risk of stroke and a younger age at menopause, or time since menopause among women younger than 65 yr, is warranted.
ACKNOWLEDGMENTS
We appreciate the help of the staff at the National Health Insurance Corporation and of medical students at Seoul National University College of Medicine who participated in the hospital survey.
Footnotes
This study was supported by the Ministry of Health and Welfare (Grant No. 01-PJ1-PG3-21900-0005), Republic of Korea Government.
References
- 1.Dyken ML, Wolf PA, Barnett HJM, Bergan JJ, Hass WK, Kannel WB, Kuller L, Kurtzke JF, Sundt TM. Risk factors in stroke. A statement for physicians by the Subcommittee on risk factors and stroke of the Stroke Council. Stroke. 1984;15:1105–1111. [Google Scholar]
- 2.Kannel WB, Hjortland MC, McNamara PM, Gordon T. Menopause and risk of cardiovascular disease. The Framingham study. Ann Intern Med. 1976;85:447–452. doi: 10.7326/0003-4819-85-4-447. [DOI] [PubMed] [Google Scholar]
- 3.Gordon T, Kannel WB, Hjortland MC, McNamara PM. Menopause and coronary heart disease. The Framingham Study. Ann Intern Med. 1978;89:157–161. doi: 10.7326/0003-4819-89-2-157. [DOI] [PubMed] [Google Scholar]
- 4.Parrish HM, Carr CA, Hall DG, King TM. Time interval from castration in premenopausal women to development of excessive coronary atherosclerosis. Am J Obstet Gynecol. 1967;99:155–162. doi: 10.1016/0002-9378(67)90314-6. [DOI] [PubMed] [Google Scholar]
- 5.Robinson RW, Higano N, Cohen WD. Increased incidence of coronary heart disease in women castrated prior to the menopause. Arch Int Med. 1959;104:908–913. doi: 10.1001/archinte.1959.00270120064010. [DOI] [PubMed] [Google Scholar]
- 6.Hu FB, Grodstein F, Hennekens CH, Colditz GA, Johnson M, Manson JE, Rosner B, Stampfer MJ. Age at natural menopause and risk of cardiovascular disease. Arch Intern Med. 1999;159:1061–1066. doi: 10.1001/archinte.159.10.1061. [DOI] [PubMed] [Google Scholar]
- 7.Snowdon DA, Kane RL, Beeson WL, Burke GL, Sprafka JM, Potter J, Iso H, Jacobs DR, Jr, Phillips RL. Is early natural menopause a biologic marker of health and aging? Am J Public Health. 1989;79:709–714. doi: 10.2105/ajph.79.6.709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cooper GS, Sandler DP. Age at natural menopause and mortality. Ann Epidemiol. 1988;8:229–235. doi: 10.1016/s1047-2797(97)00207-x. [DOI] [PubMed] [Google Scholar]
- 9.van der Schouw YT, van der Graaf Y, Steyerberg EW, Eijkemans MJC, Banga JD. Age at menopause as a risk factor for cardiovascular mortality. Lancet. 1996;347:714–718. doi: 10.1016/s0140-6736(96)90075-6. [DOI] [PubMed] [Google Scholar]
- 10.Joakimsen O, Bønaa KH, Stensland-Bugge E, Jacobsen BK. Population-based study of age at menopause and ultrasound assessed carotid atherosclerosis. The Tromsø study. J Clin Epidemiol. 2000;53:525–530. doi: 10.1016/s0895-4356(99)00197-3. [DOI] [PubMed] [Google Scholar]
- 11.Vermeulen A, Verdonck L. Sex hormone concentrations in post-menopausal women. Relation to obesity, fat mass, age and years post-menopause. Clin Endocrinol. 1978;9:59–66. doi: 10.1111/j.1365-2265.1978.tb03572.x. [DOI] [PubMed] [Google Scholar]
- 12.Kagan A, Popper JS, Rhoads GG. Factors related to stroke incidence in Hawaii Japanese men. The Honolulu Heart Study. Stroke. 1980;11:14–21. doi: 10.1161/01.str.11.1.14. [DOI] [PubMed] [Google Scholar]
- 13.Worth RM, Kato H, Rhoads GG, Kagan A, Syme SL. Epidemiologic studies of coronary heart disease and stroke in Japanese men living in Japan, Hawaii and California: mortality. Am J Epidemiol. 1975;102:481–490. doi: 10.1093/oxfordjournals.aje.a112186. [DOI] [PubMed] [Google Scholar]
- 14.Park BJ, Cho YK, Kim SA. Construction of the Korea Elderly Pharmacoepidemiologic Cohort: drug utilization review of cephalosporins in geriatric inpatients. Pharmacoepidemiol Drug Saf. 2001;10:487–492. doi: 10.1002/pds.665. [DOI] [PubMed] [Google Scholar]
- 15.Park BJ, Kim DS, Koo HW, Bae JM. Reliability and validity study of a life style questionnaire for elderly people. Korean J Prev Med. 1998;31:49–58. [Google Scholar]
- 16.The World Health Organization. MONICA Project (monitoring of trends and determinants in cardiovascular disease): a major international collaboration. WHO Monica Project principal investigators. J Clin Epidemiol. 1988;41:105–114. doi: 10.1016/0895-4356(88)90084-4. [DOI] [PubMed] [Google Scholar]
- 17.Jacobsen BK, Heuch I, Kvåle G. Age at natural menopause and all-cause mortality: a 37-year follow-up of 19,731 Norwegian women. Am J Epidemiol. 2003;157:923–929. doi: 10.1093/aje/kwg066. [DOI] [PubMed] [Google Scholar]
- 18.Ackerman RF, Dry TJ, Edwards JE. Relationship of various factors to the degree of coronary atherosclerosis in women. Circulation. 1950;1:1345–1354. doi: 10.1161/01.cir.1.6.1345. [DOI] [PubMed] [Google Scholar]
- 19.Dobs AS, Nieto FJ, Szklo M, Barnes R, Sharrett AR, Ko WJ. Risk factors for popliteal and carotid wall thicknesses in the atherosclerosis risk in communities (ARIC) study. Am J Epidemiol. 1999;150:1055–1067. doi: 10.1093/oxfordjournals.aje.a009929. [DOI] [PubMed] [Google Scholar]
- 20.Jacobsen BK, Heuch I, Kvale G. Age at natural menopause and stroke mortality: cohort study with 3561 stroke deaths during 37-year follow-up. Stroke. 2004;35:1548–1551. doi: 10.1161/01.STR.0000131746.49082.5c. [DOI] [PubMed] [Google Scholar]
- 21.Hulley S, Grady D, Bush T, Furberg C, Herrington D, Riggs B, Vittinghoff E. Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in postmenopausal women. JAMA. 1998;280:605–613. doi: 10.1001/jama.280.7.605. [DOI] [PubMed] [Google Scholar]
- 22.Grady D, Herrington D, Bittner V, Blumenthal R, Davidson M, Hlatky M, Hsia J, Hulley S, Herd A, Khan S, Newby LK, Waters D, Vittinghoff E, Wenger N. Cardiovascular disease outcomes during 6.8 years of hormone therapy. Heart and Estrogen/Progestin Replacement Study follow-up (HERS II) JAMA. 2002;288:49–57. doi: 10.1001/jama.288.1.49. [DOI] [PubMed] [Google Scholar]
- 23.Bath PM, Gray LJ. Association between hormone replacement therapy and subsequent stroke: a meta-analysis. BMJ. 2005;330:342. doi: 10.1136/bmj.38331.655347.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Im JA, Kim SH, Lee DC. Effects of Long term hormone therapy on platelet activation in postmenopausal women. J Korean Acad Fam Med. 2004;25:754–759. [Google Scholar]
- 25.Park JK, Kim HJ, Chang SJ, Koh SB, Koh SY. Risk factors for hemorrhagic stroke in Wonju, Korea. Yonsei Med J. 1998;39:229–235. doi: 10.3349/ymj.1998.39.3.229. [DOI] [PubMed] [Google Scholar]