Abstract
Behçet's disease (BD) is a multisystemic chronic inflammatory disease. It is characterized by recurrent oral and genital ulcers, uveitis, skin lesions and other manifestations, including neurologic, vascular, joint, and gastrointestinal ulcers of variable severity. Recurrent aphthous ulcer (RAU) represents a very common, but poorly understood, mucosal disorder. If a patient of RAU without any other typical symptoms of BD has gastrointestinal symptoms, it is difficult to distinguish this RAU from true BD with gastrointestinal involvement. Because pathognomonic clinical features and tools are absent, the differential diagnosis of these two diseases relies on the characteristic clinical features and the judgement of an experienced physician. Sixty-five out of a total 960 RAU patients and forty-four of 556 BD patients with gastrointestinal symptoms between January 1996 and December 2003 participated in this study. All were evaluated with esophagogastroduodenoscopy and colonoscopy. Clinical, endoscopic and histopathologic findings were analyzed and ELISA tests were conducted to detect serum levels of ASCA and pANCA. No significant difference was found between the two groups. Differential diagnosis between RAU with gastrointestinal symptoms and BD with gastrointestinal involvement requires further prospective, large-scale study.
Keywords: Behçet's Syndrome; Stomatitis, Aphthous; Saccharomyces cerevisiae; Antibodies, Antineutrophil Cytoplasmic; Gastrointestinal Tract
INTRODUCTION
Behçet's disease (BD) is a multisystemic, chronic, relapsing vasculitis that affects nearly all organs and systems. The gastrointestinal (GI) tract is not infrequently involved in patients with BD. The frequency of GI involvement varies in different countries: there are several studies, mostly from Japan, reporting a high frequency (50-60%) of GI involvement in BD (1), while a significant lower rate, less than 5%, is seen in Turkish patients (2). GI involvement has been reported in 8% of patients in the United States (3). Any portion of the GI tract may be involved. The upper GI tract is less frequently affected, but ulcerations in the esophagus and stomach have been reported. These patients commonly present with symptoms of hematemesis, melena, and epigastric pain. The terminal ileum, cecum, and ascending colon are the sites most frequently affected, resulting in abdominal pain, diarrhea, and hematemesis.
Recurrent aphthous ulcer (RAU) represent a very common but poorly understood mucosal disorder. They occur in men and women of all ages, races and geographic regions. It is estimated that at least 1 in 5 individuals has at least once been afflicted with aphthous ulcers (4). The condition is classified as minor, major, and herpetiform on the basis of ulcer size and number. Attacks may be precipitated by local trauma, stress, food intake, drugs, hormonal changes and vitamin and trace element deficiencies (4). Local and systemic conditions, and genetic, immunological and microbial factors all may play a role in the pathogenesis of recurrent aphthous ulceration. However, to date, no principal cause has been discovered. Since the etiology is unknown, diagnosis is entirely based on history and clinical criteria and no laboratory procedures exist to confirmthe diagnosis. Although RAU may be a marker of an underlying systemic illness such as celiac disease, or may present as one of the features of BD, in most cases no additional body systems are affected, and patients otherwise remain fit and well.
We often see patients of RAU with GI symptoms without any other symptoms of BD on out-patient clinic. In many cases it is difficult to distinguish intestinal BD from RAU with gastrointestinal symptom. Because the pathognomonic clinical features and tools are absent, the diagnosis of these two diseases relies on the characteristic clinical features and the judgement of the experienced physician.
The aim of this study is to help the differential diagnosis of intestinal BD and RAU with gastrointestinal symptoms through the comparison of clinical, endoscopic, histopathologic, and serologic findings.
MATERIALS AND METHODS
Patients
Sixty five of total 960 RAU patients and 44 of total 556 BD patients who visited the Depatment of Dermatology of Ajou University School of Medicine, Suwon, Korea, between January 1996 and December 2003 were invited to participate in this study and all of the patients had GI symptoms and were evaluated with esophagoduodenoscopy and colonoscopy. Sera were obtained from 12 patients with RAU, 16 patients with BD, and 4 healthy volunteers.
Clinical and endoscopic findings
The clinical records of these patients were reviewed. BD was diagnosed according to the Japanese diagnostic criteria for BD revised in 1987. Our study was based on BD patients with gastrointestinal symptoms and recurrent oral ulceration. We found out that RAU patients had no other symptom of BD. Contents reviewed were age, sex, age of onset, first manifestation, gastrointesinal symptoms, other symptoms of BD.
We investigated the endoscopic findings with respect to location, distribution, and morphology of the ulceration.
Histopathologic findings
A part of each specimen was fixed in 10% buffered neutral formalin and was embedded in paraffin. Sections were deparaffinized and rehydrated by sequential immersion in xylene, graded concentration of ethanol, and distilled water. Hematoxylin-eosin stain was done to observe the general histological changes.
We investigated all specimens with respect to presence of vasculitis and granuloma, infiltration type, dominant cell type and crypt architecture.
Serologic findings (ASCA and pANCA)
Serum was obtained from 12 patients with RAU, 12 patients with BD, and 4 healthy volunteers. Each serum was collected in a sterile tube with EDTA coating. The test tubes were centrifuged at 4℃, 3,000 rpm for 5 min. The serum was kept at -20℃ until the assay.
ASCA immunoglobin G (IgG) was evaluated by a commercially available enzyme-linked immunosorbent assay (ELISA) kit (Inova Diagnostics, San Diego, CA, U.S.A.). ASCA ELISA was performed according to the manufacturer's manuals. The antigen consisted of phosphopeptidomannan extracted from Saccharomyces cerevisiae. All sera were tested in duplicate. Results were expressed as arbitrary units with a cut-off for positivity of 25 U/mL.
The ANCA indirect immunofluorescence assay was performed according to the following method. In short, human peripheral blood neutrophils were smeared on 12-well Nutacon slides (Nutacon BV, Leimuiden, the Netherlands) and fixed in 96% ethanol (10 min at -20℃). Slides were incubated with 1:20 diluted patient's serum (in phosphate buffered saline) and stained with rabbit anti-human IgG-fluorescein isothiocyanate (FITC) conjugate (Dako A/S, Glostrup, Denmark). The slides were evaluated by fluorescence microscopy. All sera were tested in duplicate and scored by two well-trained observers who were unaware of the patients' diagnoses. Depending on the brightness of the immunofluorescence staining pattern, the reactions were graded either negative (-) or positive (+).
Statistics
Statistical analysis was done by Wilcoxon rank sum test and logistic regression. A p value of less than 0.05 was considered as statistically significant.
RESULTS
Clinical and endoscopic findings
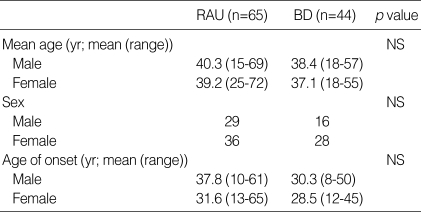
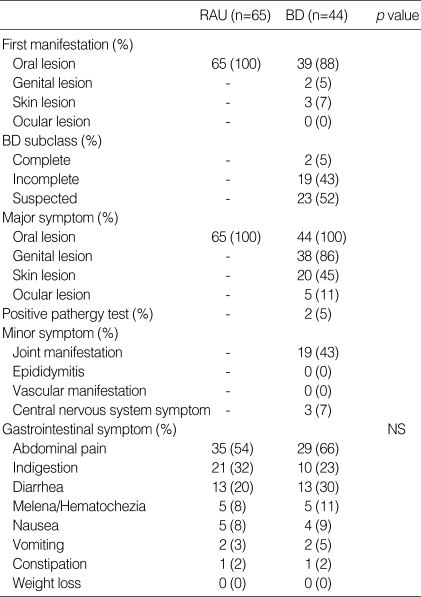
There were no significant differences in clinical findings between patients with RAU and BD by statistical analysis. Oral lesion was the most common first manifestation of BD patients. Abdominal pain was the most common gastrointestinal symptom of both groups (Table 1, 2).
Table 1.
Clinical data of patients with RAU and BD
RAU, recurrent aphthous ulcer; BD, Behçet's disease; NS, not significant.
Table 2.
Clinical characteristic of patients with RAU and BD
RAU, recurrent aphthous ulcer; BD, Behçet's disease; NS, not significant.
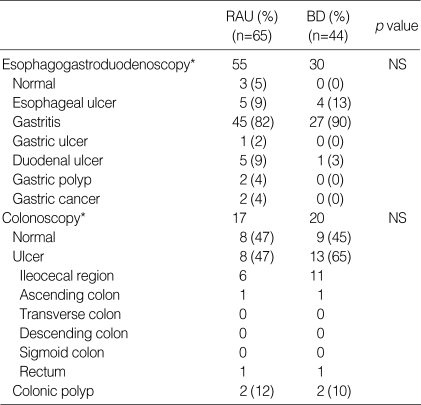
There were no significant differences in endoscopic characteristics between patients with RAU and BD (Table 3). On esophagoduodenoscopy, ulcerations were observed in 20% of RAU and 16% of BD. On colonoscopy, ulceration were observed in 47% of RAU and 65% of BD. Ileocecal region was most common ulceration site of both two groups.
Table 3.
Endoscopic characteristic of patients with RAU and BD
RAU, recurrent aphthous ulcer; BD, Behçet's disease; NS, not significant.
*A patient may have multiple esophagogastroduodenoscopy or colonoscopy findings.
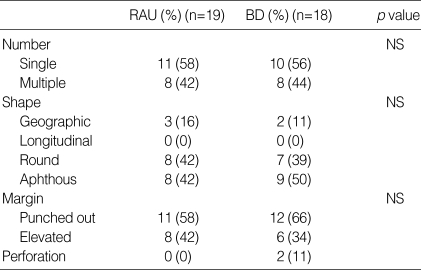
There were no statistical differences in ulcer characteristic between patients with RAU and BD (Table 4). But two cases of BD had ulcer perforation.
Table 4.
Ulcer characteristic of patients with RAU and BD
RAU, recurrent aphthous ulcer; BD, Behçet's disease; NS, not significant.
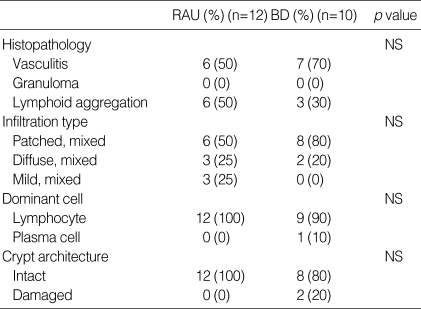
Histopathologic findings
Most common histopathologic findings of RAU and BD were vasculitis, patch mixed lymphocyte dominant infiltration (Table 5). There were no statistical differences between patients with RAU and BD.
Table 5.
Histopathologic characteristic of patients with RAU and BD
RAU, recurrent aphthous ulcer; BD, Behçet's disease; NS, not significant.
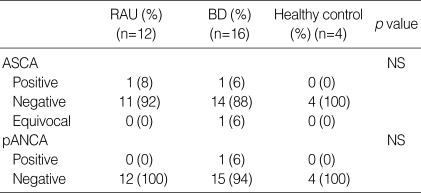
Serologic findings
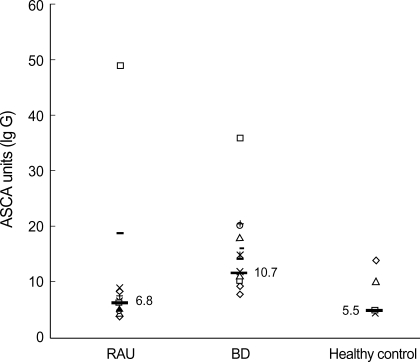
Only one patient (6%) with intestinal BD and one patient (8%) with RAU were IgG ASCA positive. Median level of ASCA was highest in serum of patient with BD (Fig 1). And one patient with intestinal BD was pANCA positive. However, there were no statistical differences between patients with intestinal BD, RAU and healthy volunteers (Table 6).
Fig. 1.
ASCA levels in patients with recurrent aphthous ulcer (RAU), Behçet's disease (BD), and healthy controls. Levels equal to or greater than 25 units are considered positive. Horizontal bar is the median value.
Table 6.
ASCA and pANCA test results of patients with RAU, BD and healthy control
RAU, recurrent aphthous ulcer; BD, Behçet's disease; ASCA, Anti-Saccharomyces cerevisiae mannan antibody; pANCA, perinuclear antineutrophil cytoplasmic autoantibody; NS, not significant.
DISCUSSION
The clinical diagnosis of BD may pose considerable difficulties. Since the disease is multi-systemic and does not have any pathognomonic symptom or laboratory findings, the diagnosis is based on a cluster of clinical manifestations. Thus, the presence of a relatively specific laboratory marker can substantially facilitate the diagnosis of BD, and possibly support a diagnosis before all disease manifestations have occurred.
RAU is seen in most patients with BD; it commonly precedes other systemic features. However, it is difficult to predict with certainty those patients initially presenting with RAU who will subsequently proceed to develop multisystem involvement as part of BD. A clinical comparison between 38 patients with BD and RAU-only controls showed an increased number of concurrent ulcers and involvement of the soft palate and oropharynx in those diagnosed with BD (5). No differences were detected with respect to duration, frequency, age of onset or family history. The aphthae in BD often occur in the soft palate and oropharynx and have been observed on the hard palate, which is an unusual site for RAU in patients without BD (5). Bang et al. examined the prognosis of the clinical relevance of recurrent oral ulceration in BD, and the investigators found that approximately half the patients who were initially diagnosed as RAU-only, developed other manifestations of BD in an average of 7.7 yr after onset (6). They reported that highly recurrent RAU had appeared to be a warning signal for BD.
Many authors consider the onset to be the age at which the patient fulfilled the diagnostic criteria. The third decade is the most commonly reported age of onset for BD, and the fourth decade for intestinal BD (7). In our study, intestinal BD occurred at a mean age of 29.0 yr and RAU occurred at a mean age of 34.7 yr. Although the mean age of RAU was higher than BD, no difference was found between the two groups in statistical analysis.
The male to female ratio in BD also differs geographically (1); however, the gender ratio in terms of intestinal BD has not been well characterized in Mediterranean and Western countries, probably because of its relative rarity. The male to female ratio of BD in this study (0.57:1) was incompatible with the reported ratio in Korea (0.7-1.3:1) (8) and Japan (1.7: 1) (7). But there were no significant differences with BD and RAU (0.8:1).
It has been well known for many years that BD is often accompanied by such gastrointestinal symptoms as nausea, vomiting, and abdominal pain (9). About 22 percent of patients with intestinal BD developed appendicitis-like symptoms during the clinical course (10). Our study showed that the most common presenting symptom in intestinal BD and RAU with GI symptoms is abdominal pain (66% and 54%). Diarrhea and indigestion were the next common presenting symptoms in these two groups.
The pathologic hallmark of intestinal BD is known to be the presence of a few punched-out ulcers of variable size and appearance (11). The smaller ulcers ("aphthoid ulcers") have been considered histologically to be similar to the oral aphthous ulcers of BD (12). Larger ulcers usually have an oval or irregular configuration. The depth of penetration of the ulcers varies. Superficial ulcers occasionally have been shown to resolve (13), but deeper ulcers, often with a narrow fissuring appearance, can extend through the bowel wall. Intestinal perforation is, therefore, a common complication (14). Prognosis of intestinal BD is worse than other inflammatory bowel disease, which is due to high perforation rate in intestinal BD (15). Although intestinal BD is diagnosed radiologically or endoscopically in many cases, relatively few descriptions about the endoscopic characteristics of intestinal BD exist in literature. Morphological characteristics of intestinal BD have been reported to be discrete ulcerations that have a confluent and discrete border, appearing most commonly in the ileocecal region (9, 14).
In our series, most of the ulcers in intestinal BD and RAU on colonoscopy were found in the ileocecal areas, but they may be present at any site throughout the digestive system. Many of the patients had single or relatively few ulcers with localized distribution. The colonoscopic characteristics of intestinal BD could be summarized as large sized, round/oval or geographically shaped, deep and discrete ulcer with elevated margins. Because we only have examined the endoscopy photographs, it was difficult to find the differences in ulcer shape, location and distribution pattern between intestinal BD and RAU.
Lee et al. classified BD patients into typical (complete and incomplete) and atypical (suspected and possible) group. And after comparing the clinical and colonoscopic characteristics of the two groups, concluded that there was no significant difference between the two groups and that a "suspected or possible" type could be included in the BD category if an intestinal involvement was identified (16). Since over half of the patients in our study were diagnosed as BD suspected type, there may not have been a significant difference with the RAU group.
The ulcers from the intestinal BD tend to be deep and penetrating and, thus, frequently require surgical interventions (17, 18). Complications of GI ulceration in BD may include perforation and enterocutaneous fistula. Surgical treatment is often necessary, but postoperative recurrence is as high as 68% (8). In the current study, we found that two cases of intestinal BD recurred after operation. Therefore, more attention should be paid in patients with perforating type of intestinal BD.
The intestinal ulcer of BD is characterized not only by absence of the granulomatous formation of Crohn's disease, but also by deeper penetration of ulcer to regions nearer the serous membrane than the ulcers of ulcerative colitis. But these characteristics are not helpful in the diagnosis of BD. Histologically, Behçet's ulcers contain nonspecific chronic inflammation. A nonnecrotizing lymphocytic vasculitis affects small veins and venules without thrombosis (19). But still it is necessary to carefully examine the clinical symptoms and signs and the histopathological appearance, since in many cases the differential diagnosis is very difficult.
In our study, most common histopathologic findings of intestinal ulcers in BD were vasculitis, patched mixed lymphocyte dominant infiltration. There were no significant differences between patients with intestinal BD and RAU.
Since 1990, perinuclear anti-neutrophil cytoplasmatic antibodies (pANCAs), which show a specific staining on indirect immunofluorescence, have been consistently found in 40-80% of patients suffering from ulcerative colitis (20, 21). They are spontaneously produced by lamina propria and mesenteric node lymphocytes (21). In ulcerative colitis, the antigen recognized by pANCAs is located in the inner side of the nuclear periphery and is DNase sensitive, but the exact epitope remains yet unknown. It is hypothesized that the pANCAs are due to cross-reactivity with bacterial antigens (22, 23)
Antibodies to baker's yeast and brewer's yeast (ASCA) have been described in up to 65% of patients with Crohn's disease (24, 25). It has been demonstrated that the specific antigen is a mannan localized in the yeast cell wall (25). The significance of ASCAs in Crohn's disease is completely unknown, but one hypothesis links them to increased intestinal permeability (26). Due to this presumed break in the epithelial barrier, increased exposure of the epithelium to common food antigens such as yeasts may result in an exaggerated antibody response.
Kim et al. have reported that ASCA may be associated with Crohn's disease and BD and pANCA with ulcerative colitis. A result that is ASCA positive and pANCA negative was associated with Crohn's disease and BD, whereas a positive pANCA in combination with a negative ASCA result was strongly correlated with ulcerative colitis. A combination of both tests may aid the differential diagnosis of inflammatory bowel disease (27). Recently, Krause et al. have reported significantly higher ASCA values in BD patients compared with patients with RAU, SLE or healthy volunteers. This implies that ASCA, taken in appropriate clinical context, could become a useful diagnostic tool for BD (28). Also, they have reported ASCA titers were significantly higher in BD patients companied to their healthy family members. ASCA seem to be strongly related to BD expression and are not associated with environmental or genetic factors.
Unlike previous reports in our study, ASCA and pANCA levels were not different between the two groups. The median value of ASCA level was higher in BD but this finding was not statistically significant. There were neither clinical, endoscopical, histopathological nor serological differences between patients with intestinal BD, RAU and healthy volunteers in ASCA and pANCA. Further prospective studies with a larger number of patients are needed to make a diagnosis tool of intestinal BD and RAU.
References
- 1.Shimizu T, Ehrlich GE, Inaba G, Hayashi K. Behçet disease (Behçet syndrome) Semin Arthritis Rheum. 1979;8:223–260. doi: 10.1016/0049-0172(79)90004-0. [DOI] [PubMed] [Google Scholar]
- 2.Yurdakul S, Tuzuner N, Yurdakul Z, Hamuryudan V, Yazici H. Gastrointestinal involvement in Behçet's syndrome: a controlled study. Ann Rheum Dis. 1996;55:208–221. doi: 10.1136/ard.55.3.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Balabanova M, Calamia KT, Perniciaro C, O'Duffy JD. A study of the cutaneous manifestations of Behçet's disease in patients from the United States. J Am Acad Dermatol. 1999;41:540–545. [PubMed] [Google Scholar]
- 4.Natah SS, Konttinen YT, Enattah NS, Ashammakhi N, Sharkey KA, Hayrinen-Immonen R. Recurrent aphthous ulcers today: a review of the growing knowledge. Int J Oral Maxillofac Surg. 2004;33:221–234. doi: 10.1006/ijom.2002.0446. [DOI] [PubMed] [Google Scholar]
- 5.Main DM, Chamberlain MA. Clinical differentiation of oral ulceration in Behçet's disease. Br J Rheumatol. 1992;31:767–770. doi: 10.1093/rheumatology/31.11.767. [DOI] [PubMed] [Google Scholar]
- 6.Bang D, Yoon KH, Chung HG, Choi EH, Lee ES, Lee S. Epidemiological and clinical features of Behçet's disease in Korea. Yonsei Med J. 1997;38:428–436. doi: 10.3349/ymj.1997.38.6.428. [DOI] [PubMed] [Google Scholar]
- 7.Kasahara Y, Tanaka S, Nishino M, Umemura H, Shiraha S, Kuyama T. Intestinal involvement in Behçet's disease: review of 136 surgical cases in Japanese literature. Dis Colon Rectum. 1981;24:103–106. doi: 10.1007/BF02604297. [DOI] [PubMed] [Google Scholar]
- 8.Choi IJ, Kim JS, Cha SD, Jung HC, Park JG, Song IS, Kim CY. Long-term clinical course and prognostic factors in intestinal Behçet's disease. Dis Colon Rectum. 2000;43:692–700. doi: 10.1007/BF02235590. [DOI] [PubMed] [Google Scholar]
- 9.Bayraktar Y, Özaslan E, Van Thiel DH. Gastrointestinal manifestations of Behçet's disease. J Clin Gastroenterol. 2000;30:144–154. doi: 10.1097/00004836-200003000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Kodama H. Intestinal Behçet's. Surg Ther. 1977;37:51–58. [Google Scholar]
- 11.Lee RG. The colitis of Behçet's syndrome. Am J Surg Pathol. 1986;10:888–893. doi: 10.1097/00000478-198612000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Thach BT, Cummings NA. Behçet syndrome with "aphthous colitis". Arch Intern Med. 1976;136:705–709. [PubMed] [Google Scholar]
- 13.Lebwohl O, Forde KA, Berdon WE, Morrison S, Challop R. Ulcerative esophagitis and colitis in a pediatric patient with Behçet's syndrome. Response to steroid therapy. Am J Gastroenterol. 1977;68:550–555. [PubMed] [Google Scholar]
- 14.Lee KS, Kim SJ, Lee BC, Yoon DS, Lee WJ, Chi HS. Surgical treatment of intestinal Behçet's disease. Yonsei Med J. 1997;38:455–460. doi: 10.3349/ymj.1997.38.6.455. [DOI] [PubMed] [Google Scholar]
- 15.Choi IJ, Kim JS, Park MJ, Kim YS, Lee JH, Lee DH, Jung HC, Song IS, Kim CY. Evaluation of prognosis and cumulative operation rate of intestinal Behçet's disease in comparison with Crohn's disease. Korean J Gastroenterol. 2000;36:504–514. [Google Scholar]
- 16.Lee CR, Kim WH, Cho YS, Kim MH, Kim JH, Park IS, Bang DS. Colonoscopic findings in intestinal Behçet's disease. Inflamm Bowel Dis. 2001;7:243–249. doi: 10.1097/00054725-200108000-00010. [DOI] [PubMed] [Google Scholar]
- 17.Sayek I, Aran O, Uzunalimoglu B, Hersek E. Intestinal Behçet's disease; surgical experience in seven cases. Hepatogastroenterology. 1991;38:81–83. [PubMed] [Google Scholar]
- 18.Kim JS, Lim SH, Choi IJ, Moon H, Jung HC, Song IS, Kim CY. Prediction of clinical course according to the macroscopic type by colonoscopy in Behçet's colitis. Endoscopsy. 2000;32:635–640. doi: 10.1055/s-2000-9012. [DOI] [PubMed] [Google Scholar]
- 19.Yoo TW. Morphological differences between Crohn's disease and intestinal Behçet's disease involving colon. Seoul: Yonsei Univ.; 1993. [dissertation] [Google Scholar]
- 20.Rump JA, Schölmerich J, Gross V. A new type of perinuclear anti-neutrophil cytoplasmic antibody in active ulcerative colitis but not in Crohn's disease. Immunobiology. 1990;181:406–413. doi: 10.1016/S0171-2985(11)80509-7. [DOI] [PubMed] [Google Scholar]
- 21.Peeters M, Joossens S, Vermeire S, Vlietinck R, Bossuyt X, Rutgeerts P. Diagnostic value of anti-Saccharomyces cerevisiae and anti-neutrophil cytoplasmic autoantibodies in inflammatory bowel disease. Am J Gastroenterol. 2001;96:730–734. doi: 10.1111/j.1572-0241.2001.03613.x. [DOI] [PubMed] [Google Scholar]
- 22.Targan SR, Landers CJ, Cobb L, MacDermott RP, Vidrich A. Perinuclear anti-neutrophil cytoplasmic antibodies are spontaneously produced by mucosal B cells of ulcerative colitis patients. J Immunol. 1995;155:3262–3267. [PubMed] [Google Scholar]
- 23.Cohavy O, Bruckner D, Gordon LK, Misra R, Wei B, Eggena ME, Targan SR, Braun J. Colonic bacteria express an ulcerative colitis pANCA-related protein epitope. Infect Immun. 2000;68:1542–1548. doi: 10.1128/iai.68.3.1542-1548.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Main J, McKenzie H, Yeaman GR, Kerr MA, Robson D, Pennington CR, Parratt D. Antibody to Saccharomyces cerevisiae (baker's yeast) in Crohn's disease. BMJ. 1988;297:1105–1106. doi: 10.1136/bmj.297.6656.1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sendid B, Colombel JF, Jacquinot PM, Faille C, Fruit J, Cortot A, Lucidarme D, Camus D, Poulain D. Specific antibody response to oligomannoside epitopes in Crohn's disease. Clin Diagn Lab Immunol. 1996;3:219–226. doi: 10.1128/cdli.3.2.219-226.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vermeire S, Peeters M, Vlietinck R, Joossens S, Den Hond E, Bulteel V, Bossuyt X, Geypens B, Rutgeerts P. Anti-Saccharomyces cerevisiae antibodies (ASCA), phenotypes of IBD, and intestinal permeability: a study in IBD families. Inflamm Bowel Dis. 2001;7:8–15. doi: 10.1097/00054725-200102000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Kim BG, Kim YS, Kim JS, Jung HC, Song IS. Diagnostic role of anti-Saccharomyces cerevisiae mannan antibodies combined with antineutrophil cytoplasmic antibodies in patients with inflammatory bowel disease. Dis Colon Rectum. 2002;45:1062–1069. doi: 10.1007/s10350-004-6361-3. [DOI] [PubMed] [Google Scholar]
- 28.Krause I, Monselise Y, Milo G, Weinberger A. Anti-saccharomyces cerevisiae antibodies: A novel serologic marker for Behçets disease. Clin Exp Rheumatol. 2002;20(4) Suppl 26:S21–S24. [PubMed] [Google Scholar]