Abstract
Background
Contemporary understanding of the biomechanics, natural history, and methods of treating thoracolumbar spine injuries continues to evolve. Current classification schemes of these injuries, however, can be either too simplified or overly complex for clinical use.
Methods
The Spine Trauma Group was given a survey to identify similarities in treatment algorithms for common thoracolumbar injuries, as well as to identify characteristics of injury that played a key role in the decision-making process.
Results
Based on the survey, the Spine Trauma Group has developed a classification system and an injury severity score (thoracolumbar injury classification and severity score, or TLICS), which may facilitate communication between physicians and serve as a guideline for treating these injuries. The classification system is based on the morphology of the injury, integrity of the posterior ligamentous complex, and neurological status of the patient. Points are assigned for each category, and the final total points suggest a possible treatment option.
Conclusions
The usefulness of this new system will have to be proven in future studies investigating inter- and intraobserver reliability, as well as long-term outcome studies for operative and nonoperative treatment methods.
Introduction
Classification systems for thoracolumbar trauma continue to evolve.1 A comprehensive classification system, however, has been difficult to create, partly due to the complexity of spinal anatomy and mechanisms of injury, as well as widely differing philosophies in treatment. Over the last several decades, incremental improvements in understanding the natural history of thoracolumbar spine fractures has spawned classification systems that have incorporated these new data.
History of thoracolumbar classification systems
Böhler2 initially attempted to classify thoracolumbar spine fractures using five injury types. He combined both anatomic appearance and mechanisms of injury to include compression fractures, flexion-distraction injuries, extension fractures, shear fractures, and rotational injuries in his classification scheme. Böhler, however, did not attempt to define instability patterns based on the anatomical appearance of the injury.
Watson-Jones3 recognized that the concept of “instability” would be crucial in any effective treatment algorithm on thoracolumbar injuries. He identified ligamentous integrity as one of the key determinants of stability in various injury subtypes. Nicoll,4 in a study of spine injuries in 152 miners, identified four anatomical structures (vertebral bodies, facet joints, posterior ligaments, discs) involved in any injury pattern. He, like Watson-Jones, emphasized the danger of progressive neurological injury and deformity if an instability pattern is overlooked.
Holdsworth,5 in his now classic scheme of injury patterns, introduced the columnar concept of stability. He visualized the spine as two columns: the anterior column consisting of the vertebral body and intervertebral disk, and the posterior column consisting of facet joints and the posterior ligamentous complex. He insisted that the integrity of the posterior column is necessary for stability of the thoracolumbar spine. His classification scheme, which includes anterior compression fractures, fracture-dislocation, rotation fracture-dislocation, extension injuries, burst fractures, and shear injuries, remains the most influential to modern classifications schemes. The most important criticism of this classification system was that it oversimplified the biomechanics of injury in thoracolumbar fractures. For example, unstable burst fractures based on their natural history were falsely categorized as “stable” when, in fact, many of these fractures progressed to kyphosis and increased neurological deficits.6,7
The era of computed tomography (CT) provided a new opportunity to improve on the existing thoracolumbar classification schemes. CT imaging allowed visualization of finer details of spinal injuries, including osseous anatomy surrounding the spinal canal. Using this technology, Denis introduced a classification scheme based on the three-column concept. Differing from Holdsworth’s system, Denis defined the anterior column as the anterior longitudinal ligament to the anterior two-thirds of the vertebral body, the middle column as the posterior one-third of the vertebral body including the anulus fibrosus and posterior longitudinal ligament, and the posterior column, which includes all structures posterior to the posterior longitudinal ligament. Denis defined four distinct fractures types: compression fractures, burst fractures, fracture-dislocations, and seatbelt injuries. Denis also recognized that mechanical instability and progressive neurologic deterioration could occur separately or together. Mechanical instability may lead to progressive kyphosis without neurologic instability, and neurologic deterioration may occur without radiographic signs of instability, as in the case of burst fractures. More unstable fractures, such as fractures associated with dislocations of the facets or disc interspace were usually associated with neurologic deterioration. Denis called isolated mechanical instability “first degree” injuries, neurologic deterioration as “second degree” injuries, and combined mechanical and neurologic deterioration as “third degree” injuries. This classification scheme remains the most popular to date, mostly because of its simplicity. Denis’ anatomic divisions of columns are easily visualized on CT images, and his original concept of instability has been oversimplified to state that instability exists if two of three columns are disrupted. This oversimplification, however, has led to the loss of Denis’ original emphasis on the distinction of mechanical and neurologic instability.
Denis’ classification does not clearly provide a useful algorithm for treating unstable injuries. With the oversimplification of his scheme, it has been widely accepted that when two of three columns are injured operative stabilization may be necessary for a satisfactory outcome. Several studies, however, have shown that nonoperative treatment of two-column injuries may achieve a satisfactory outcome.8–10 Also, Denis’ classification is unclear on how ligamentous injuries (which may lead to occult, progressive instability) can be identified. Therefore, the subset of patients who require surgical intervention to prevent painful deformity or progressive neurologic deficit may be missed. With the advent of modern magnetic imaging (MRI) studies, occult ligamentous injuries may be easier to define. Yet, there is no classification to date that incorporates this new technology in its scheme.
A modern classification system, then, should incorporate the current understanding of the biomechanics of thoracolumbar injuries and the availability of modern imaging modalities including MRI; it should also acknowledge the advancements in anesthesia and internal fixation that may allow early mobilization and rehabilitation of the injured patient. The classification system should be relatively simple to achieve high inter- and intraobserver reliability. In addition, it should give general guidelines of treatment based on the current understanding of the natural history of thoracolumbar spine injuries.
Thoracolumbar injury classification and severity score: a classification system and treatment algorithm
The thoracolumbar injury classification and severity score (TLICS) was conceptualized based on a survey given to the Spine Trauma Study Group, which consists of worldwide experts in the field of spinal trauma. The goal of the survey was to identify similarities in treatment algorithms for common thoracolumbar injuries as well as to identify characteristics of injury that played a key role in the decision-making process. Using these data, a new classification system and algorithm of treatment was developed.11
The classification system is based on three major categories: the morphology of the injury; the integrity of the posterior ligamentous complex; and the neurologic status of the patient.11 To classify an injury, the treating physician first describes the morphology of injury followed by the status of the integrity of the posterior ligamentous complex and finally the patient’s neurologic examination. For example, a patient has a T7 flexion compression burst fracture with disruption of the posterior ligamentous complex and a complete cord injury on neurologic examination. The morphology of injury and the integrity of the posterior ligamentous complex are both defined by the appearance of the injury on imaging studies. Based on the severity of these categories, specific points are allocated, and the sum of the points defines the possible treatment alternatives (Table 1). Higher total points indicate a more severe injury, and those injuries are more likely to benefit from surgical intervention based on the opinions of the Spine Trauma Study Group.
Table 1.
TLICS scoring
| Parameter | Points |
|---|---|
| Morphology | |
| Compression fracture | 1 |
| Burst fracture | 2 |
| Translational/rotational | 3 |
| Distraction | 4 |
| Neurologic involvement | |
| Intact | 0 |
| Nerve root | 2 |
| Cord, conus medullaris | |
| Incomplete | 3 |
| Complete | 2 |
| Cauda equina | 3 |
| Posterior ligamentous complex | |
| Intact | 0 |
| Injury suspected/indeterminate | 2 |
| Injured | 3 |
Morphology of injury
The initial step is to scrutinize available imaging studies to identify the injury morphology. The three major morphologic subcategories are: (1) compression injuries, (2) translational/rotational injuries, and (3) distraction injuries (Fig. 1). Anywhere from one to four points are assigned to these morphologies, with more severe bony and ligamentous injuries receiving more points. If there are injuries at multiple levels, only the more severe morphology is counted. If multiple primary morphologies are involved at a single level, only the most severe is counted. For example, a patient with both a compression and a distraction injury at the same level would only receive a score for distraction. Similarly, a patient with a compression and a distraction injury at separate levels would only be scored at the level with the higher total point value.
Fig. 1.
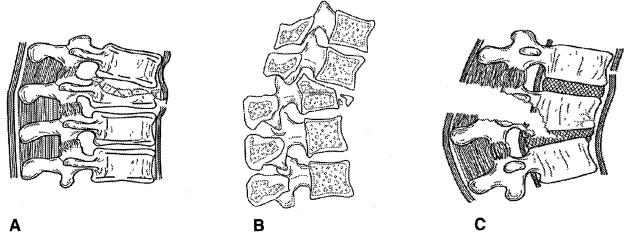
Morphology. A Compression (compression fracture or burst). B Rotation/translation. C Distraction
Compression injuries are the most common form of thoracolumbar fractures (Fig. 1). This type of injury results from an axial load to the spine. One form of this injury is the compression fracture, where an axial load is transferred to the anterior vertebral body. The anterior vertebral body deforms into a wedge, causing varying degrees of kyphosis. The posterior vertebral body remains intact. Another form of this injury pattern is the burst fracture, where an axial load is transferred to both the anterior and posterior vertebral walls. In this case, both the anterior and posterior cortex of the vertebral body is disrupted in varying degrees, with retropulsion of the bone into the spinal canal. The thoracolumbar injury severity score assigns one point to compression fractures and an additional point if a burst fracture is present.
Translational/rotational injuries are significant injuries that result from violent torsional, shear forces, or both (Fig. 1). These injuries usually cause significant ligamentous or osseous damage that result in an unstable spine. Because of the severity, the thoracolumbar injury severity score assigns three points to this mechanism.
Distraction injuries describe a tensile disruption of the spinal column. The distraction can cause osseous, ligamentous, or combined injuries of the spine and usually results in a circumferential instability. This injury is assigned four points in the thoracolumbar injury severity scoring paradigm. One caveat to scoring distraction morphologies is that it must be a definitive diagnosis. For instance, a distraction morphology cannot be selected in a flexion compression injury if injury to the PLC is indeterminent.
Neurologic injury
There are five categories of neurologic injury: (1) intact; (2) nerve root injury; (3) complete spinal cord injury; (4) incomplete spinal cord injury; (5) cauda equina syndrome. Patients with an intact neurologic status are assigned zero points, and those with either nerve root injury or complete spinal cord injury are assigned two points. Patients with an incomplete spinal cord injury or cauda equina syndrome are assigned three points owing to the relative value of surgical decompression in these neurologic subgroups.
Posterior ligamentous complex
There are three descriptive categories when evaluating the integrity of the posterior ligamentous complex. An intact posterior ligamentous complex is determined by the absence of a palpable gap between spinous processes, interspinous widening on plain films or CT images, or absence of posterior ligamentous hyperintensity on fat-suppressed T2-weighted MRI images. An intact posterior ligamentous complex is assigned zero points. Indeterminate disruption of the posterior ligamentous complex is given two points, and a definite disruption is given three points.
Total points
The total score is determined by adding the assigned points in all the major categories. Determination of the total points is designed to help surgeons and nonsurgeons assess the severity of the injury and to guide the decision-between operative and nonoperative management. Patients with ≤3 total points are considered nonoperative candidates, whereas patients with ≥5 points are operative candidates (Table 2). Patients with a total score of 4 fall into an indistinct category, where either nonoperative or operative treatment may be considered.
Table 2.
Management as per TLICS score
| Management | Points |
|---|---|
| Nonoperative | 0–3 |
| Nonoperative or operative | 4 |
| Operative | ≥5 |
Caveats
The above algorithm represents an objective way to determine treatment for patients with thoracolumbar injuries. Although it is a systematic approach to determine injury severity, the TLICS score does not provide subjective criteria that may also be crucial in the decision-making process. These factors include medical co-morbidities, traumatic injuries other than those involving the spine (e.g., multiple limb fractures, closed head injury, internal organ injuries), abrasions over potential operative sites, or excessive kyphosis.11,12 Other preexisting osseous disorders, such as ankylosing spondylitis, diffuse idiopathic skeletal hyperostosis, or osteoporosis, may also affect treatment decisions. These factors have not been incorporated in the TLICS score to keep the algorithm purely objective and as simple as possible. The TLICS score is designed only as a guideline for surgeons and nonsurgeons to help determine possible treatment options; it is not meant to be an absolute end-all in decision-making. Therefore, incorporation of these subjective factors is critical when ultimately choosing nonoperative or operative treatment.
Conclusions
Ultimately, any classification system or treatment algorithm needs to undergo rigorous validation studies to ensure high inter- and intraobserver reliability. Denis’s classification system, which represents the most popular in use currently, has good inter- and intraobserver reliability, with a kappa coefficient of 0.6.13 Oversimplification of the injury mechanism of the Denis’ system, however, may lead to incorrectly treating potentially unstable injuries nonoperatively or stable fractures with unnecessary surgery. As a system becomes more comprehensive, the inter- and intraobserver reliability becomes poor. For example, the AO classification of thoracolumbar fractures, which is a comprehensive categorization of more than 50 types of fracture, has poor inter- and intraobserver reliability. Blauth et al. distributed 14 plain films of thoracolumbar injuries to 22 institutions in an attempt to quantify the interobserver reliability of the AO classification. They concluded that the kappa value for interobserver reliability for the AO classification was only 0.33.14
When designing the TLICS score, an attempt was made to emphasize only a few critical factors useful for guiding treatment options. In doing so, key morphologies and radiographic/neurologic findings were isolated and included in the algorithm. The goal was to keep the system simple and straightforward for both surgeons and nonsurgeons alike. This system still requires rigorous validity and reliability testing to determine its usefulness, and it will undoubtedly be further modified as our understanding of this complex injury improves.
Acknowledgment
This work was supported by members of the Spine Trauma Study Group and funded by an educational grant from Medtronic Sofamor Danek.
Footnotes
Presented at the 78th Annual Meeting of the Japanese Orthopaedic Association, Yokohama, Japan, May 14, 2005
References
- 1.Öner FC. Thoracolumbar spine fractures: diagnostic and prognostic parameters. Thesis. Universiteit Utrecht 1999.
- 2.Bohler L. Die techniek de knochenbruchbehandlung imgrieden und im kriege. Verlag von Wilhelm Maudrich 1930 (in German)
- 3.Watson-Jones R. Fractures and joint injuries. 3rd edn. Edinburgh: E&S Livingstone; 1943. [Google Scholar]
- 4.Nicholl EA. Fractures of the dorsolumbar spine. J Bone Joint Surg Br. 1949;31:376–94. [PubMed] [Google Scholar]
- 5.Holdsworth F. Fractures, dislocations, and fracture-dislocations of the spine. J Bone Joint Surg Am. 1970;52:1534–51. [PubMed] [Google Scholar]
- 6.Roberts JB, Curtiss PH., Jr Stability of the thoracic and lumbar spine in traumatic paraplegia following fracture or fracture-dislocation. J Bone Joint Surg Am. 1970;52:1115–30. [PubMed] [Google Scholar]
- 7.Whitesides TE., Jr Traumatic kyphosis of the thoracolumbar spine. Clin Orthop. 1977;128:78–92. [PubMed] [Google Scholar]
- 8.Agus H, Kayali C, Arslantas M. Nonoperative treatment of burst-type thoracolumbar vertebra fractures: clinical and radiological results of 29 patients. Eur Spine J. 2004;14:536–40. doi: 10.1007/s00586-004-0740-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wood K, Buttermann G, Mehbod A, Garvey T, Jhanjee R, Sechriest V, et al. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit: a prospective, randomized study. J Bone Joint Surg Am. 2003;85:773–81. doi: 10.1302/0301-620X.85B3.13849. [DOI] [PubMed] [Google Scholar]
- 10.Kelly RP, Whitesides TE., Jr Treatment of lumbodorsal fracture-dislocations. Ann Surg. 1968;167:705–17. doi: 10.1097/00000658-196805000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vaccaro AR, Zeiller SC, Hulbert RJ, Anderson PA, Harris M, Hedlund R, et al. The thoracolumbar injury severity score: a proposed treatment algorithm. J Spinal Disord Tech. 2005;18:209–15. [PubMed] [Google Scholar]
- 12.Vaccaro AR, Kim DH, Brodke DS, Harris M, Chapman JR, Schildhauer T, et al. Diagnosis and management of thoracolumbar spine fractures. Instr Course Lect. 2004;53:359–73. [PubMed] [Google Scholar]
- 13.Öner FC, Ramos LM, Simmermacher RK, Kingma PT, Diekerhof CH, Dhert WJ, et al. Classification of thoracic and lumbar spine fractures: problems of reproducibility: a study of 53 patients using CT and MRI. Eur Spine J. 2002;11:235–45. doi: 10.1007/s00586-001-0364-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blauth M, Bastian L, Knop C, Lange U, Tusch G. Inter-observer reliability in the classification of thoraco-lumbar spinal injuries. Orthopade. 1999;28:662–81. doi: 10.1007/s001320050397. [DOI] [PubMed] [Google Scholar]


