Abstract
Objectives
To examine the relationship between pharmacy college/school affiliation and community pharmacies' involvement in immunization and emergency preparedness activities.
Methods
Telephone interviews were completed with 1,704 community pharmacies randomly sampled from 17 states to determine the pharmacies' involvement in immunization promotion, vaccine distribution, in-house immunization delivery, and health emergency preparedness and response, affiliation with college/school of pharmacy, and selected pharmacy and public health-related characteristics.
Results
Pharmacy college/school-affiliated community pharmacies were more likely than non-affiliated pharmacies to participate in immunization and emergency preparedness when controlling for pharmacy characteristics. College/school affiliation generally became nonsignificant, however, when public health-related characteristics were included in the analysis.
Conclusions
Affiliation with a college/school of pharmacy was related to community pharmacies' involvement in immunization and emergency preparedness.
Keywords: experiential learning, public health, school of pharmacy, college of pharmacy, community pharmacy, immunization
INTRODUCTION
Pharmacists have a responsibility to engage in disease prevention and health promotion activities such as smoking cessation, immunization delivery, and prevention of heart disease, stroke, and diabetes.1,2 The 2004 educational outcomes released by the Center for the Advancement of Pharmaceutical Education (CAPE) include public health as a major competency in pharmaceutical education.3 The Accreditation Council for Pharmacy Education (ACPE) also incorporated these outcomes into Standards 2007.4 Hence, colleges and schools of pharmacy must prepare future pharmacists for expanding public health roles by incorporating public health content in their curricula.
While teaching public health can be accomplished through didactic coursework,5 colleges and schools of pharmacy should go beyond this to integrate public health into experiential education.6-8 Experiential education has long been recognized as an effective way to facilitate student learning.9 During experiential education, students should have opportunities to actively participate in pharmacy-based public health activities, acquire in-depth experiences, and master public health skills.
The need for exceptional experiential education sites to guide the development of pharmacy students is great.10 Sending students to experiential education sites that do not provide public health services may cause student frustration due to the perceived dissonance between what they are being taught as the ideal practice and what they see in actual practice.11 Students assigned to sites who do not engage in public health activities may not gain sufficient experiences to master the skills necessary to provide public health activities and achieve the outcomes specified by CAPE.
Community pharmacies' participation as experiential education sites is an essential mechanism for pharmacies to be affiliated with colleges/schools of pharmacy. In addition, community pharmacies' affiliations with colleges and schools of pharmacy may be based on the pharmacy's participation in practice-based research networks, residency programs, and/or classroom teaching or research activities. Little information is available regarding the extent to which pharmacies affiliated with colleges and schools of pharmacy offer public health services and how these pharmacies compare to non-affiliated pharmacies in terms of involvement in public health activities.
The goal of this study was to better understand the relationship between a pharmacy's affiliation with a pharmacy college/school and its involvement in public health activities. In this study, public health activities were conceptualized as innovations to be studied. Social network theory was used to provide an explanation for why college/school-affiliated pharmacies were more involved in public health activities than their non-affiliated counterparts. According to this theory, knowledge transfer and resource sharing occur among organizations that are connected to one another in the same social context.12,13 Information and resource exchange enhance organizations' capabilities to discover new opportunities, obtain new knowledge, and explore new innovations.14-16 In the case of community pharmacies, through affiliation with colleges and schools of pharmacy, community pharmacies learn new knowledge, are exposed to new opportunities, and gain critical competencies that contribute to advancement in their practices. We then posited that community pharmacies affiliated with a pharmacy college/school were more likely to be involved in public health activities than community pharmacies not affiliated with a pharmacy college/school. We explored 4 selected public health activities: immunization promotion, vaccine distribution, in-house immunization delivery, and emergency preparedness and response. Our objectives were to: (1) compare community pharmacies with and without pharmacy college/school affiliation in terms of general pharmacy characteristics and public health-related characteristics, (2) compare community pharmacies with and without pharmacy college/school affiliation in terms of extent and type of public health involvement, and (3) examine the relationship between pharmacy college/school affiliation and pharmacy involvement in public health activities when controlling for general pharmacy characteristics and public health-related characteristics.
METHODS
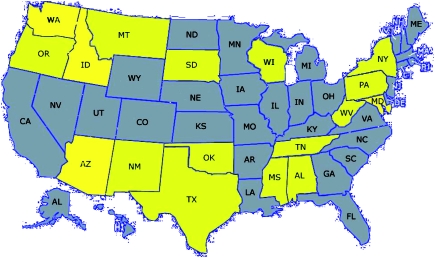
This study was part of a larger national study (17 states) describing community pharmacies' participation in immunization and emergency preparedness and response activities. Seventeen states were purposely selected to maximize variability along 3 dimensions: the flexibility of state immunization-related laws, the overall level of pharmacist/pharmacy participation in public health activities at the state-level, and geographical location (Figure 1).17 This study received exempt status by the University of Wisconsin-Madison's Institutional Review Board.
Figure 1.
States with a lighter shade were included in this study.
A systematic random sample of 150 community pharmacies (158 in one state due to error) was selected from each state. Prenotification letters and study descriptions were sent to 2,558 pharmacies prior to contacting them by telephone. A computer-assisted telephone interview was then conducted with key informants (pharmacy managers or on-duty pharmacists) at each of the pharmacies between July 2005 and February 2006. When making telephone contact, the interviewer requested to speak with the pharmacy manager or a pharmacist on duty. If an appropriate individual was not available, the interviewer attempted to call back; calling was limited to 35 attempts per sampled pharmacy. Details of interview procedures appear in a previously published study.18
Variables
We determined each pharmacy's affiliation status by asking key informants whether their practice site was affiliated with a college or school of pharmacy (response recorded as yes or no). To measure pharmacy involvement in public health activities, the key informants were asked to identify whether their pharmacy was involved in immunization promotion, vaccine distribution, in-house immunization delivery, or emergency preparedness and response. For example, for immunization promotion, key informants were asked whether their practice site participated in any campaign to promote the importance of immunizations. Similarly, 3 additional questions were asked about their involvement in vaccine distribution, immunization delivery, and emergency preparedness and response. These 4 questions yielded 4 dichotomous variables (yes/no). A fifth dichotomous dependent variable was created based on key informants' responses related to the 4 public health activities; if the key informant responded yes to at least 1 of the targeted public health activities, the pharmacy was coded 1; pharmacies offering none of these services were coded 0.
Control variables were categorized into 2 groups: general pharmacy characteristics and characteristics related to public health. General pharmacy characteristics included type of pharmacy (independent/chain/mass merchant/supermarket), pharmacy location (rural/suburban/urban), number of full-time equivalent pharmacists (count), and pharmacist workload (prescriptions filled per full-time pharmacist per week). For the public health-related characteristics, key informants were asked to report whether their practice site had at least 1 pharmacist trained in in-house immunization delivery (yes/no) and in emergency preparedness and response (yes/no). They also were asked the extent of perceived support from various groups for in-house immunization delivery and for emergency preparedness and response. These groups were: pharmacy profession (state board, state/local pharmacy associations, and national pharmacy associations), public health (health department and physicians/clinics), and pharmacy practice (employing organization, supervisor, and other pharmacists). To measure perceived support variables, key informants were asked to rate how strongly each group opposed or supported pharmacist participation in these activities on a scale ranging from -5 (strongly oppose) to 5 (strongly support). A zero was assigned when the key informants saw a particular group as neither supportive nor opposed or had no opinions.
Data Analysis
Data were analyzed using SPSS, version 16.0 (SPSS, Chicago). To assess the potential for nonresponse bias, characteristics of hard-to-contact pharmacies (those requiring more than 9 calls) and easy-to-contact pharmacies (those requiring less than 2 calls) were compared.18
Descriptive statistics, including general pharmacy characteristics and characteristics related to public health, were used to describe participating pharmacies. Bivariate analyses were conducted to assess relationships between pharmacy college/school affiliation and (1) pharmacy characteristics, (2) public health-related characteristics (characteristics specific to immunization delivery and emergency preparedness and response), and (3) pharmacy involvement in public health activities. A series of logistic regression analyses were conducted to assess the relationship between pharmacy college/school affiliation and public health involvement when controlling for pharmacy characteristics and characteristics specific to immunization delivery and emergency preparedness and response.
RESULTS
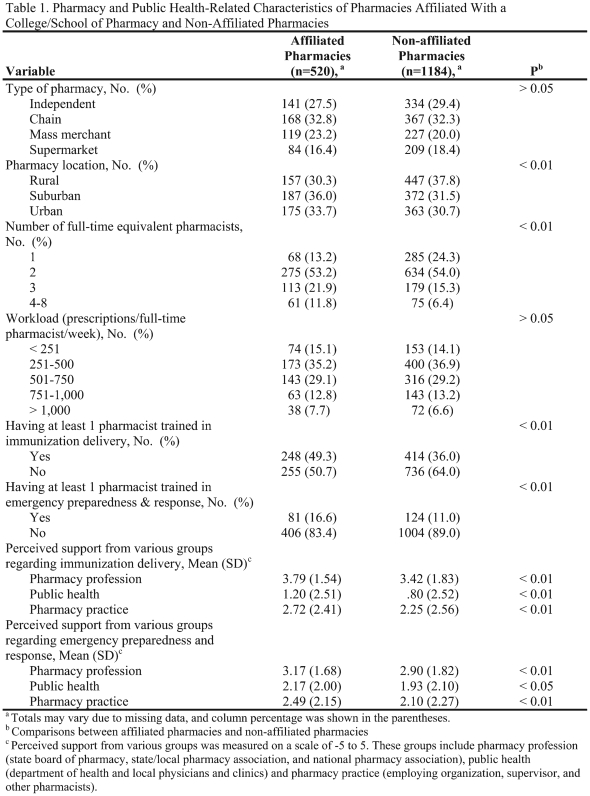
Of the 2,558 randomly selected community pharmacies, 92 were excluded because they did not provide direct pharmacy services to the public, were nonpharmacy telephone numbers, or were non-working telephone numbers. Results showed no significant differences between easy- and hard-to-contact pharmacies with respect to general pharmacy characteristics and involvement in emergency preparedness and response. However, easy-to-contact cases differed from hard-to-contact cases in that those who provided immunization services were more prompt in responding to the telephone survey request. Of the 1,704 (69% response rate) participating pharmacies, 520 were affiliated with a college or school of pharmacy and 1,184 were not (Table 1). Pharmacies affiliated with pharmacy college or school differed from non-affiliated pharmacies in terms of their location (χ2 = 9.1; p < 0.01) and number of full-time equivalent pharmacists (χ2 = 43.4; p < 0.01). Pharmacies affiliated with a college/school were more likely to be located in suburban and urban locations and to employ a greater number of full-time equivalent pharmacists compared to non-affiliated pharmacies. As for the public health-related characteristics, pharmacies affiliated with a college/school were more likely to have at least 1 pharmacist trained in immunization delivery (χ2 = 25.8; p < 0.01) and in emergency preparedness and response (χ2 = 9.8; p < 0.01). Further, pharmacies affiliated with a college/school perceived a greater level of support from the pharmacy profession, public health, and pharmacy practice groups compared to pharmacies that were not affiliated with a college or school of pharmacy.
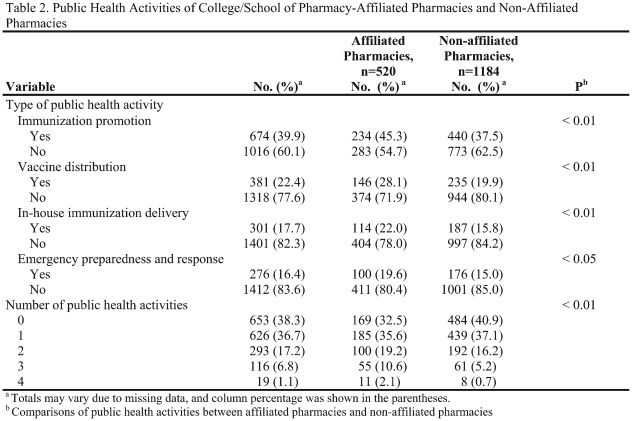
Compared to non-affiliated pharmacies, pharmacies affiliated with a college/school were more likely to be involved in each of the 4 targeted public health activities (Table 2). For example, 28.1% of pharmacies affiliated with a college/school were involved in vaccine distribution, compared to 19.9% of non-affiliated pharmacies (χ2 = 13.8; p < 0.01). Pharmacies affiliated with a college/school of pharmacy were involved in a greater number of public health activities than non-affiliated pharmacies (χ2 = 31.1; p < 0.01; Table 2). An independent t test was also employed to examine the difference in the total number of public health activities in which affiliated and non-affiliated pharmacies were involved. On average, pharmacies affiliated with a college/school engaged in 1.14 activities, which was significantly higher than the average of 0.88 activities engaged in by non-affiliated pharmacies (t = 4.99; p < 0.01; data not shown in Table 2).
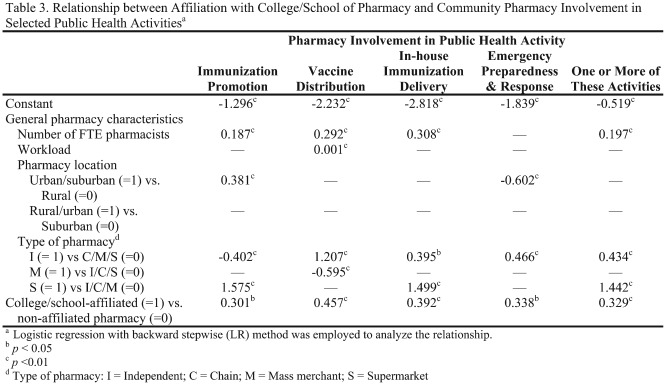
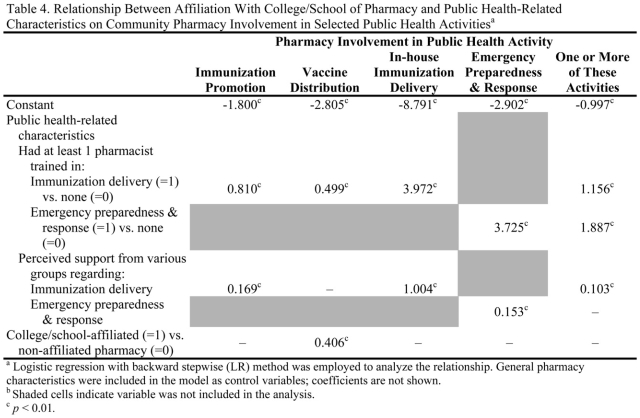
Even when controlling for the effect of general pharmacy characteristics, pharmacy college/school affiliation remained a significant predictor (Table 3). We next included public health-related characteristics in logistic regression analyses (Table 4). Characteristics related to immunization delivery (whether pharmacy had at least 1 pharmacist trained in immunization delivery and perceived support regarding immunization delivery) were included in the analyses of pharmacy involvement in immunization promotion, vaccine distribution, and in-house immunization delivery. Similarly, characteristics related to emergency preparedness and response (whether pharmacy had at least 1 pharmacist trained in emergency preparedness and response and perceived support regarding emergency preparedness and response) were included when the analysis of pharmacy involvement in emergency preparedness and response. All characteristics related to in-house immunization delivery and emergency preparedness and response were included in the analysis of pharmacy involvement in at least 1 public health activity. General pharmacy characteristics also were included in these analyses. Because all coefficients of general pharmacy characteristics were consistent with those shown in Table 3, results were omitted from Table 4 to simplify presentation.
The relationship between pharmacy college/school affiliation and pharmacy involvement in vaccine distribution remained significant when other public health-related variables were added to the analysis. Specifically, for pharmacy involvement in vaccine distribution, coefficients for affiliation (B = 0.4; p < 0.01) and having at least 1 pharmacist trained in immunization delivery (B = 0.5, p < 0.01) were significant. College/school of pharmacy affiliation was no longer a significant predictor of involvement in other immunization or emergency preparedness and response activities when other public health-related variables were included in the analysis, however. Immunization promotion activity and in-house immunization delivery were predicted by having at least 1 pharmacist trained in immunization delivery and by perceived greater support from various immunization-related groups (Table 4). Similarly, pharmacy involvement in emergency preparedness and response was predicted by having at least 1 pharmacist trained in this area (B = 3.7; p < 0.01) and by perceived greater support from various groups involved in emergency preparedness and response (B = 0.2; p < 0.01).
DISCUSSION
Our literature review found few empirical studies that directly investigated the relationship between college/school of pharmacy affiliation and pharmacy innovations and practice change. For example, in an exploratory study of 6 independent community pharmacies, regular interaction with practice change advocates such as colleges/schools of pharmacy was a key factor to support practice change.19 While this study was useful in identifying key facilitators to practice change, their findings had limited generalizability as the data were collected from 6 selected independent community pharmacies.19 The second study examined factors associated with the provision of pharmaceutical care services by surveying 2,048 pharmacies.20 Pharmaceutical care services were more frequently offered by university-affiliated pharmacies than non-affiliated pharmacies.20 Since both studies were exploratory in nature, they provided limited explanations as to why and how school affiliation was associated with practice innovations.
Building on these studies, we used Social Network Theory to provide a possible explanation for why, when controlling for general pharmacy characteristics, pharmacies affiliated with college/schools of pharmacy were more involved in public health activities than their non-affiliated counterparts. This theory suggests that social connections with pharmacy colleges/schools allow affiliated community pharmacies to gain new knowledge and exposure to new opportunities. Learning about new opportunities may prompt these pharmacies to obtain competencies that contribute to their practice advancement in the area of public health activities. This, in turn, leads us to argue that pharmacy colleges/schools should serve as change agents by facilitating the diffusion of public health activities among community pharmacies.21 To accomplish this, colleges and schools should introduce innovative ideas in community pharmacies, assist practitioners in developing a need for change, help practitioners translate intent to change into action, and stabilize the adoption of new practices.21 Relationships developed through network connections between community pharmacies and pharmacy colleges/schools are mutually beneficial. For example, community pharmacies that serve as experiential education sites may learn new ideas from preceptor training programs offered by colleges/schools and subsequently develop their competencies to build competitive advantage. Benefits for the college/school of pharmacy result when students gain experiences during their experiential education and ultimately are able to achieve the outcomes at the level specified by CAPE.3
Public health-related variables were added to the model; The effects of college/school affiliation diminished. This was true for all selected public health activities except vaccine distribution. These findings do not contradict our previous explanations of the relationship between college/school and pharmacy involvement in public health activities; instead, they provide additional insights into the importance of social networks. First, the findings emphasized the importance of having at least 1 staff pharmacist who was trained in immunization delivery or emergency preparedness and response. Through connections with a college/school of pharmacy, staff pharmacists may have been exposed to new opportunities and thus sought formal training to advance their practice sites. We recommend that to facilitate pharmacy involvement in public health activities colleges/school of pharmacy offer training programs in immunization delivery and emergency preparedness and response for community pharmacies on a regular basis. Second, another significant factor included in the analysis was the degree of perceived support for public health activities; community pharmacies were more likely to participate in public health activities if they perceived a greater degree of support from various groups, including physicians and clinics, health departments, employing organizations, and the state board of pharmacy. Similar to the explanation given above for affiliation with a college/school of pharmacy, network connections between community pharmacies and these groups may help facilitate the implementation of public health activities. For example, for pharmacies to provide in-house immunization services, state boards of pharmacy need to grant or recognize authority for pharmacists in their states to administer vaccines, employing organizations and supervisors need to provide support for immunization activities, and physicians need to provide support by referring patients to and/or entering into collaborative practice agreements with community pharmacies. Without such supports, community pharmacies cannot engage in successful public health activities. For this reason, we also recommend that colleges/schools of pharmacy communicate with these groups regarding how pharmacists and pharmacies can help to promote public health.
Our study uses Social Network Theory to offer one explanation for the relationships between affiliation with a college/school of pharmacy and pharmacies involvement in public health activities. Since a key limitation of this study is its use of cross-sectional data, causal effects cannot be established and at least 2 alternative explanations for these findings should be noted. First, pharmacy involvement in public health could facilitate affiliation with a college/school of pharmacy. That is, pharmacies that are involved in public health may be attractive to colleges/schools of pharmacy, prompting the colleges/schools to seek out these pharmacies and ask to collaborate with them, for example, by serving as experiential education sites or participating in a practice-based research network. A second alternative explanation for our results is that the significant relationship between affiliation with a pharmacy college/school and pharmacy involvement in public health activities was a result of a spurious effect. That is, affiliation may have had no causal connection with public health involvement; instead both variables could have been caused by a third factor, such as being an innovative practitioner. For example, an innovative practitioner might both affiliate with a pharmacy college/school and provide public health-related services. Since our study could not establish causal effect, future research should examine processes that could further explain the relationship between college/school of pharmacy affiliation and pharmacy involvement in public health or other innovations. A study of the processes in which pharmacy schools attract and collaborate with experiential education sites could provide important insights into research questions such as: How did connection between the pharmacy and the college/school originate? What characteristics attracted the college/school to the pharmacy and/or the pharmacy to the college/school? What types of assistance do experiential education sites receive from colleges/schools of pharmacy and what effects do these have? And what are mechanisms used by the college/school of pharmacy to advance experiential education sites?
Our study shows that affiliation with colleges/schools was positively associated with community pharmacies' involvement in public health activities. We recognize that the nature of college/school affiliation may differ across participating pharmacies; for example, some affiliated pharmacies serve as experiential education sites while others serve as practice-based research sites. Therefore, future research should address the following questions: What is the nature and strength of college/school affiliation(s) in relation to pharmacy involvement in public health activities or other innovative practices? How do different types of college/school affiliation influence pharmacy involvement in public health activities or innovative practices? How might the influence of affiliation be enhanced?
Experiential education sites that engage in public health activities are needed to provide adequate opportunities for students to actively participate in pharmacy-based public health activities and acquire in-depth experiences in public health activities. College/school of pharmacy goals are to ensure that student learning achieves the CAPE outcomes and prepare them for expanded public health roles. Because little is known about how best to improve student learning outcomes related to public health, colleges and schools of pharmacy should reexamine their curricula to ensure that competencies in public health are adequately achieved to prepare future pharmacists.22 Future research should explore the following possible research questions: To what extent do students engage in public health activities during pharmacy practice experiences? What mechanisms used in experiential education sites improve student learning outcomes? And what methods can best prepare students to carry out key public health activities?
Limitations
Beyond reliance on cross-sectional data, certain limitations need to be considered when interpreting and generalizing the results presented here. First, key informants may have been subject to recall errors. We did not believe this was a problem, as key informants were able to access pharmacy records while being interviewed. Second, this study investigated the effects of only particular factors; it did not evaluate all factors that may be associated with pharmacy involvement in public health activities. Lastly, the study may have limited generalizability to nonrespondents, other states beyond the 17 study states, other public health activities, and pharmacy practice innovations.
CONCLUSION
Pharmacy college/school-affiliated community pharmacies were more likely than non-affiliated pharmacies to participate in public health activities. However, affiliation generally became nonsignificant when other public health-related characteristics were included in the analysis. Research further examining how best to develop experiential education sites and improve student-learning outcomes related to public health activities is needed.
ACKNOWLEDGEMENTS
This research was supported by grant R06-CCR 523387 from the Public Health Law Program of the US Centers for Disease Control and Prevention (CDC). The ideas expressed in this manuscript are those of the authors and in no way are intended to represent the position of University of Wisconsin-Madison School of Pharmacy and Harrison School of Pharmacy Auburn University.
REFERENCES
- 1.Babb VJ, Babb J. Pharmacist involvement in healthy people 2010. J Am Pharm Assoc. 2003;43(1):56–60. [PubMed] [Google Scholar]
- 2.Hurd PD, Levin BL, Hanson A. Introduction and overview of pharmacy and public health. In: Levin BL, Hurd PD, Hanson A, editors. Introduction to Public Health in Pharmacy. Sadbury, MA: Jones and Bartlett Publishers; 2007. pp. 1–15. [Google Scholar]
- 3. American Association of Colleges of Pharmacy, Center for the Advancement of Pharmaceutical Education (CAPE). Educational outcomes, revised version 2004. http://www.aacp.org/resources/education/Documents/CAPE2004.pdf Accessed October 20, 2009.
- 4. Accreditation Council for Pharmacy Education. Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree (ACPE Standards 2007). http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf Accessed October 20, 2009.
- 5.Crawford SY. Pharmacists' roles in health promotion and disease prevention. Am J Pharm Educ. 2005;69(4):534–540. [Google Scholar]
- 6.Globe DR, Johnson K, Conant L, Frausto S. Implementing a community-based health promotion program into the pharmacy curriculum: the USC FUENTE initiative. Am J Pharm Educ. 2004;68(2) Article 32. [Google Scholar]
- 7.Doty RE, Latham KM, Stewart RB. Public health screenings as a component of introductory practice experiences. Am J Pharm Educ. 2000;64(4):425–430. [Google Scholar]
- 8.Anderson AS, Goode J-VR. Engaging students in wellness and disease prevention services. Am J Pharm Educ. 2006;70(2) doi: 10.5688/aj700240. Article 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beck DE, Thomas SG, Janer AL. Introductory practice experiences: a conceptual framework. Am J Pharm Educ. 1996;60(2):122–131. [Google Scholar]
- 10.Cerulli J. Experiential education in community pharmacy. Am J Pharm Educ. 2006;70(1) doi: 10.5688/aj700119. Article 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Speedie M. Introductory experiential education: a means for introducing concepts of healthcare improvement. Am J Pharm Educ. 2006;70(6) Article 145. [Google Scholar]
- 12.Blau PM, Scott WR. Formal Organizations: A Comparative Approach. Stanford: CA: Stanford University Press; 2003. [Google Scholar]
- 13.Gresov C, Stephens C. The context of interunit influence attempts. Adm Sci Q. 1993;38(2):252–276. [Google Scholar]
- 14.The distinctive domain of entrepreneurship research. In: Venkataraman S, editor; Katz JA, editor. Advances in Entrepreneurship, Firm Emergence and Growth; No. 3. Greenwich, CT: JAI Press; 1997. [Google Scholar]
- 15.Tsai W. Knowledge transfer in intraorganizational networks: effects of network position and absorptive capacity on business unit innovation and performance. Acad Manage J. 2001;44(5):996–1004. [Google Scholar]
- 16.Ahuja G. Collaboration networks, structural holes, and innovation: a longitudinal study. Adm Sci Q. 2000;45(3):425–455. [Google Scholar]
- 17.Westrick SC, Mount JK, Watcharadamrongkun S, Breland ML. Pharmacy stages of involvement in pharmacy-based immunization services: results from a 17-state survey. J Am Pharm Assoc. 2008;48(6):764–773. doi: 10.1331/JAPhA.2008.07118. [DOI] [PubMed] [Google Scholar]
- 18.Westrick SC, Mount JK. Effects of repeated callbacks on response rate and nonresponse bias: results from a 17-state pharmacy survey. Res Social Adm Pharm. 2008;4(1):46–58. doi: 10.1016/j.sapharm.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 19.Doucette WR, Koch YD. An exploratory study of community pharmacy practice change. J Am Pharm Assoc. 2000;40(3):384–391. doi: 10.1016/s1086-5802(16)31087-7. [DOI] [PubMed] [Google Scholar]
- 20.McDermott JH, Christensen DB. Provision of pharmaceutical care services in North Carolina: a 1999 survey. J Am Pharm Assoc. 2002;42(1):26–35. doi: 10.1331/108658002763538044. [DOI] [PubMed] [Google Scholar]
- 21.Rogers EM. Diffusion of Innovations. 5th ed. New York: Free Press; 2003. [Google Scholar]
- 22.O'Neil CK, Levin BL, Hanson A. Education and training. In: Levin BL, Hurd PD, Hanson A, editors. Introduction to public health in pharmacy. Sudbury, MA: Jones and Bartlett Publishers; 2008. pp. 337–350. [Google Scholar]