To the Editor. The shortage of pharmacy faculty members has been described by the American Association of Colleges of Pharmacy (AACP). In 2006, 427 pharmacy faculty positions were vacant, with almost half of the positions open for at least 6 months.1 The majority of these positions were at the Assistant Professor level.1 These data demonstrate that the pharmacy profession must develop avenues to prepare young pharmacists for a transition into faculty roles. Postgraduate training programs, such as residencies and fellowships, provide an opportunity to refine the pharmacist's expertise in clinical practice, research, and education.
As the profession of pharmacy expands to include higher levels of community-based patient care, the recruitment of pharmacy faculty members with expertise in community practice and research becomes essential. According to the American Pharmacists Association, 68 postgraduate year-one (PGY-1) community pharmacy residency programs are currently available for pharmacy graduates who are interested in practicing in the community.2 The experience that the participants gain through these residency positions becomes invaluable to schools of pharmacy that are currently establishing or expanding community-based programs.
Community-based PGY-1 residency programs are designed to meet practice development needs, however, they may not fully prepare residents to engage in scholarly work or to compete for limited research dollars. Ellis et al demonstrated that while pharmacy-practice-residency training improved residents' perception of their ability to conduct research, this was not confirmed by their scores on an objective 18-item test of research-related skills.3 Further, Clark et al found that graduating community pharmacy residents do not feel well-prepared to engage in research.4 A more objective measure of preparation for research activities is the successful publication of resident research findings. In a survey of residency program directors, Murphy et al found that while almost half of resident research projects were believed to have had a positive impact on pharmacy services at their institution, only 13% had been published.5
A recent survey showed that only 8% of the 2005-2006 community pharmacy residents had accepted faculty positions at the conclusion of their residency. Feeling unprepared for a faculty role was a factor influencing residents' decision not to apply for these positions.4
Residents interested in pursuing faculty positions that involve engaging in scholarly efforts may benefit from more formalized research training than what is currently offered in most residency programs. A research fellowship program could serve as a valuable springboard for advancing future faculty preparedness to conduct research. The American College of Clinical Pharmacy (ACCP) defines research fellowships as “directed, highly individualized, postgraduate training programs designed to prepare the participant to function as an independent investigator.”6
In order to address the needs of both academia and community practice, the University of Pittsburgh School of Pharmacy has created a Community Practice Research Fellowship modeled after program criteria set forth by ACCP.6 The community practice research fellowship program was established within the Department of Pharmacy and Therapeutics at the University of Pittsburgh in 2007, through the financial support of an anonymous alumnus of the school. The development of this program is in line with the school's mission to improve the standard of care for community-based patients. Previous school initiatives in the community setting include the establishment of a PGY-1 community pharmacy residency program in 2006 and the development of a nationally-recognized model for pharmacist-provided Medication Therapy Management (MTM) services.7
The goal of this fellowship program is to provide graduates with a solid foundation in scholarship pertaining to community pharmacy practice, and emphasis is placed on developing future faculty members. The intent is that pharmacists will complete the fellowship after a PGY-1 community practice residency. To our knowledge, this program is the first 24-month postdoctoral fellowship to focus on research pertaining to community pharmacy practice.
Key Features
General Structure.
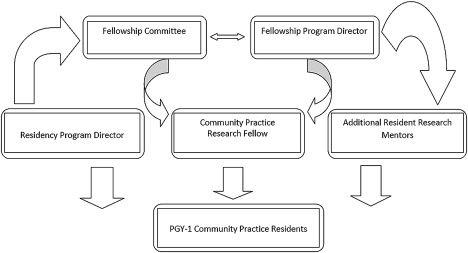
The fellowship program was designed to build upon the school's other community-based initiatives while assisting in setting a research agenda for community-based scholarship. The close relationship between the fellowship and the PGY-1 community practice residency program is depicted in Figure 1. This collaboration is enhanced through regular meetings and shared office space between the residents and the fellow.
Figure 1.
Program.
Fellowship Learning Experiences.
The core learning experiences of the fellowship program consist of mentored research and graduate coursework (approximately 80%-90% of the fellow's effort), with the remaining time devoted to teaching and/or community-based direct patient care. Specific activities are individualized to meet the fellow's interests and career goals. The fellow is advised by the program director and a committee consisting of faculty members with expertise in community pharmacy practice and health services/health outcomes research. The fellow meets weekly with the program director and every 6 months with the full committee.
-
Mentored research activities. The ACCP Guidelines for Clinical Research Fellowship Training Programs list several skills that are essential to achieving competency in clinical research.6 In the community practice research fellowship, the majority of these skills are developed through the completion of research activities under the guidance of the fellowship director and other researcher preceptors. As part of these research efforts, the fellow is required to gain experience in grantsmanship through authoring and submitting at least 1 grant application for funding consideration.
Due to the emphasis on training future faculty members, the fellow is also required to gain experience in the scholarship of teaching, providing the opportunity for course material design, and formal evaluation.
Graduate coursework. Specific coursework is dependent on the needs and interests of the fellow, however, the fellow is encouraged to enroll in 1 of several degree programs at the University of Pittsburgh, leading to a certificate in clinical research, a master of science, or master of public health degree.
Experience with the Program.
While the program has graduated only 1 fellow to date (in July 2009) and limited outcomes “data” are available, we believe others may benefit from considering this educational model at their own institutions. The collaboration structure highlighted in Figure 1 generated 7 successful foundation grant applications (fellow as principal investigator on 3) and 2 publications that are in press. Several additional papers are in the preparation and submission/review stages. All of the research efforts relate to the common goal of improving the delivery of community-based pharmacist care and emphasize understanding the social, administrative, and behavioral aspects of these services. At the University of Pittsburgh, the fellowship served as a natural next step for the school's first PGY-1 community practice resident who was interested in academia.
Faculty members from 2 other colleges of pharmacy have approached the authors to express interest in establishing similar programs at their institutions. Others interested in discussing further our experiences with the fellowship are invited to contact us for more information.
Margie E. Snyder, PharmD, MPHa,b
Melissa Somma McGivney, PharmDb
Randall B. Smith, PhDb
a Purdue University School of Pharmacy and Pharmaceutical Sciences
b University of Pittsburgh School of Pharmacy, Pittsburgh, PA
REFERENCES
- 1.Beardsley R, Matzke G, Rospond R, et al. Factors influencing the pharmacy faculty workforce. Am J Pharm Educ. 2008;72 doi: 10.5688/aj720234. Article 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. American Pharmacists Association. 2008-2009 Community Pharmacy Residency Program Directory. http://www.pharmacist.com/AM/Template.cfm?Section=Residencies_Advanced_Training&CONTENTID=18238&TEMPLATE=/CM/ContentDisplay.cfm Accessed October 26, 2009.
- 3.Ellis JJ, McCreadie SR, McGregory M, Streetman DS. Effect of pharmacy practice residency training on residents' knowledge of and interest in clinical research. Am J Health-Syst Pharm. 2007;64:2055–2063. doi: 10.2146/ajhp070063. [DOI] [PubMed] [Google Scholar]
- 4.Clark CA, Mehta BH, Rodis JL, Pruchnicki MC, Pedersen CA. Assessment of factors influencing community pharmacy residents' pursuit of academic positions. Am J Pharm Educ. 2008;72 doi: 10.5688/aj720103. Article 03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murphy JE, Downhour N. Perceived value and outcomes of residency projects. Am J Health-Syst Pharm. 2001;58:889–895. doi: 10.1093/ajhp/58.10.889. [DOI] [PubMed] [Google Scholar]
- 6. American College of Clinical Pharmacy. Guidelines for Clinical Research Fellowship Training Programs. Available at: http://www.accp.com/resandfel/guidelines.aspx. Accessed September 15, 2009.
- 7.Somma MA, Szymczak MA, Berringer RA, Schwartz H, Drew G, Smith RB, Kroboth PD, Schwinghammer TL. A standardized medication therapy management service (MTMS) in a community pharmacy chain. APhA Annual Meeting; April, 2005; Orlando, FL. [Google Scholar]