Abstract
Between 50 and 80% of the patients diagnosed with schizophrenia have been shown to be partially or totally lacking insight into the presence of their mental disorder. Although a causal chain connecting poor insight with poor treatment adherence and thus with poorer outcome and functioning is straight forward, numerous studies investigating correlates and long-term impact of insight have provided differing results. In addition, higher levels of insight in schizophrenia have been associated with depression and hopelessness, but the causal direction of the relationship is unclear and the data are inconclusive. The current study provides a critical review of 88 studies on the assessment of insight and its impact on symptoms and functioning. Studies published by June 2006 were selected using a keyword search for English peer-reviewed articles in the databases PsycINFO and MEDLINE. The majority of studies support the assumption that insight is associated with adherence during treatment phase, but the association with long-term adherence remains unclear. Insight correlates with better long-term functioning, but this might be explained by its association with symptoms. There is a positive cross-sectional and longitudinal relationship between insight and depression, but the underlying processes need further clarification. In the concluding discussion, the problems relating to definition and study designs are considered responsible for many of the inconclusive findings. Suggestions for further research are derived.
Keywords: insight, adherence, course of symptoms, functional outcome, depression
Introduction
Psychopharmacological and psychological treatments can significantly reduce symptoms in schizophrenia, but the overall treatment effects are at best moderate compared with the changes achieved in other mental disorders.1,2 The long-term course of schizophrenia is frequently characterized by reduced social and occupational functioning, loss of independent living, impaired quality of life, substance abuse, and increased risk of suicidal and violent behavior.3,4
In spite of unclear evidence, many clinicians believe that poor insight is partially responsible for the negative functional and symptomatic prognosis. Insight has been consensually defined as the awareness of having a mental disorder, of its symptoms and of its implications, and has been shown to be at least partly lacking in approximately 50% of the patients with schizophrenia.5–8 There are persuasive reasons to connect lack of insight with poor outcome. Most importantly, insight may cause noncompliance with treatment because patients are not likely to comply with psychiatric treatment for a problem they do not believe to be either present (“I am not ill”) or mental in cause (“All I need is some rest”). Also, patients with low insight might be more prone to develop a delusional interpretation of hallucinations and act upon it, possibly resulting in impulsive or aggressive behavior.
Although presumably a helpful precondition for adherence, growing awareness into the presence and implications of a major mental disorder can be painful and even traumatizing for patients, particularly, if health care professionals cling to outdated illness concepts such as dementia praecox that overemphasize mental and social decline. Historically, deficits in insight have often been understood as serving the defensive function of warding off feelings of negative selfesteem or hopelessness. Thus, growing insight has been considered responsible for postpsychotic depression.9
There has been considerable growth in the literature on insight in schizophrenia. Today, a researcher who enters the search words “insight” or “awareness” and “schizophrenia” or “psychoses” into the databases PsycINFO and MEDLINE is confronted with approximately 1700 articles, many of which address the impact of insight on adherence, symptoms, and functioning. These studies have arrived at conflicting conclusions, and the lack of systematic reviews makes it difficult to gain an objective picture of the evidence for an association between insight, adherence, and outcome. Introduction sections, in which statements are lightly underlined by a couple of confirming literature references, regardless of the number of contradicting studies, are characteristic for the field of insight research. A systematic and detailed review of the studies on insight and outcome would allow more reliable conclusions concerning the strength of the proposed association.
There have been a few recent reviews and meta-analyses on insight and outcome, but these have covered very specific topics, such as the association between insight and violence,10 or insight and suicide.11 Other reviews either refer to older literature12,13 or are not based on a transparent systematic research.14–17
We attempt to fill the gap of a systematic and extensive review of the literature addressing correlates and long-term consequences of poor insight. Specifically, we are interested in the strength of the association between insight and treatment adherence and the impact of poor insight on the course of psychotic symptoms, functioning, and aggressive behavior. Finally, before possibly proposing that insight must be encouraged, we will review studies that have investigated potentially negative implications of gain in insight, such as depression and suicide.
Methods
Selection of Studies
Articles for consideration were identified through a literature search of abstracts in PsycINFO and MEDLINE in June 2006 without restriction of the time period. In a first step, we used the search terms “schizophrenia” or “psychosis” combined with “insight” or “awareness” to search for English articles published in peer-reviewed journals. From this pool of studies, we selected articles by searching the abstracts for additional keywords: assessment, outcome, compliance, adherence, prognosis, violence, positive symptoms, negative symptoms, depression, and suicide. Because there is large diversity in the terms used for outcome and adherence, all abstracts were screened additionally to select those relevant to these topics. Finally, we included articles that we encountered during the lecture of the literature.
Studies were excluded from the review if no assessment procedure for insight with demonstrated reliability and validity was employed (as described in “Assessment of Insight” section). In the case of studies investigating the impact of insight on depression or on symptoms, measures for depression or symptoms were also required to have demonstrated validity and reliability. Furthermore, studies were excluded if the sample consisted of heterogeneous patient samples (eg, including affective or anxiety disorders), and data for schizophrenia or schizophrenia spectrum disorders was not analyzed separately.
Procedure
The emphasis in the review was placed on studies that were conducted using longitudinal designs which allow for causal inferences. To save space while preventing loss of important information, cross-sectional studies are not presented in the tables but are either summarized in the accompanying text or—in some cases—results from other reviews are cited. An additional table summarizing the numerous cross-sectional studies on adherence and functional outcome is available on request from the authors. The first section provides a description and comparison of measures assessing insight. Because some of the instruments tap different aspects of insight, this section is a precondition for understanding and interpreting the reviewed studies.
Results
Assessment of Insight
The assessment of insight is incorporated in many clinical scales. The Schedule for Affective Disorders and Schizophrenia18, the Hamilton Depression Rating Scale19, the Present State Examination (PSE20), and the Positive and Negative Syndrome Scale (PANSS21) each include one insight item. The Manual for the Documentation of Psychopathology22 includes 3 items assessing lack of feeling of illness, lack of insight, and uncooperativeness.
To date, most researchers agree that insight is best seen as varying along a continuum involving multiple dimensions such as awareness of having a disorder, attribution of one's symptoms to the disorder, and acknowledging the need for treatment.23 During the last 15 years, a row of more detailed and valid measures of insight have been developed that encompass these different dimensions. These are presented in table 1.
Table 1.
Scales That Assess Insight in Schizophrenia, Sorted by Date of Publication
| Scale | Dimensions | Psychometric properties |
| Attitude Questionnaire24 | Eleven aspects of attitude: illness positive or negative, integrate or isolate illness, blame self, blame family, blame events, insight positive or negative, future positive or negative | Reliability and validity: only scale intercorrelations are described. Positive and negative attitudes toward illness correlate significantly (r = −.62) and positive attitudes correlate significantly with integrate scores, a positive attitude toward the future and a high value for insight in solving present problems. |
| Insight Instrument25 | Beliefs about symptoms, awareness of illness and causes of hospitalization, feeling of vulnerability to recurrences, and beliefs about treatment benefit | Reliability: Cronbach alpha = .91 |
| ITAQ26 | Questions address the recognition of mental illness, the need for hospital care, and the need to take medication | Validity: significant correlation (r = .85) of ITAQ scores with open interview to assess insight. ITAQ is highly correlated with the SAI (r = .82) and the PANSS insight item (r = .90)27; factor analysis: PCA extracted one factor. |
| SAI23,28 | Assesses 3 components of insight: awareness of illness, the capacity to relabel psychotic experiences as abnormal, and treatment compliance | Validity: total insight is highly correlated with insight in the PSE (r = .72) and moderately with the total PSE Score (r = −.31). All components correlate with each other and with insight in the PSE (r = .58–.60). Correlations with PANSS insight (r = .88) and ITAQ (r = .82) are high27; factor structure: a PCA did not support the postulated 3 dimensions but provided a single-factor solution accounting for 60.2% of the variance. |
| Marková and Berrios Insight Scale29 | Questions address hospitalization, mental illness, perception of being ill, changes in self, control over situation, perception of environment, wish to understand situation. In the revised scale, items on hospitalization and medication were deleted and more emphasis laid on awareness of changes and relationship to the environment. | Validity: Sanz et al27 found associations with other insight scales (SAI, PANSS, ITAQ) to be low to moderate, ranging from r = .34–.55. Factor analysis revealed 5 interpretable factors for the items in group A and 3 factors for group B items; reliability: Cronbach alpha for group A = .71, for group B = .55. |
| Marková and Berrios Insight Scale—revised (self-report)30 | For the revised form Cronbach alpha is .88, and retest reliability (assessed by 10 patients repeating the assessment 1 d later) is r = .65. | |
| SUMD31 | Separate assessment of present and past insight into mental disorder (item 1), social consequences (item 2), need for treatment (item 3), and perception of each present symptom and attribution of symptom to disorder (items 4–20). Total: 74 items | Validity: items 1 and 2 for present illness are highly correlated with the insight rating on a mental status examination (r = .88; r = .60); insight in the HDRS (r = .89; r = .80). The correlations for item 3 were moderate (r = .43; r = .62), whereas past awareness revealed lower or insignificant correlations. Present insight is highly correlated with PANSS insight (r = .7332) intra class correlations (ICCs) and ITAQ scores (r = .46 to r = .74)33; reliability: intra class correlations for subscale scores range from 0.52 (past attribution) to 0.90 (current awareness). |
| IS (self-report)34 | Designed to be sensitive to changes in levels of insight and capture the following dimensions of insight: need for treatment, awareness of illness, and relabeling of symptoms as pathological | Validity: high correlations (r = .74–.85) between subscales and total scores of IS and SUMD in a group that completed the IS before being observer rated. In the observer rated, first group associations were low. Insight was rated as lower in the IS as compared with the SUMD35; reliability: Cronbach alpha for total scale = .75, test-retest reliability (1 wk) = .90; factor structure: PCA extracted one factor that accounted for 60% of the variance. |
| AII36 | Assessment of recognition of mental illness (3 questions) and perceived need for psychiatric treatment (4 questions) | Reliability: Cronbach alpha for total scale = .84 (for subscale 1 = .86, for subscale 2 = .75); ICCs for total scale = .79 (for subscale 1 = .81, for subscale 2 = .75). Factor structure: factor analysis revealed 2 factors accounting for 69% of the variance. Factor loadings and intercorrelations only partially support the assumption of the postulated dimensions. |
| SALI37 | Four subscales: treatment acceptance, treatment efficacy awareness, awareness of possibility of recurrence of illness, and own explanation of cause of illness | Validity: the first 3 scales significantly correlated with PANSS insight item (.64–.74) and items assessing insight into positive symptoms (.41–.69). Scales assessing treatment efficacy awareness and possibility of recurrence were significantly correlated with insight into negative symptoms (.55–.58); reliability: Cronbach alpha for complete scale = .85. “Own explanation for illness” revealed negative correlations with the other subscales and was omitted. |
| BABS38 | Assesses delusionality of beliefs (conviction, perception of others views of belief, explanation of differing views, fixity of ideas, attempts to disprove beliefs, insight, delusions of reference) in various disorders | For schizophrenia,39 validity: medium correlation with SUMD in sample of patients with schizophrenia or schizoaffective disorder (.55). No significant correlation with clinicians global insight rating and with scales assessing positive and negative symptoms (BPRS, SANS, SAPS). Reliability: Cronbach alpha for complete scale = .89. |
| SAIQ (self-report)40 | Assesses acknowledgment of illness, acknowledgment of need for psychiatric treatment, and extent of worry about illness and illness-related issues | Factor analysis found 3 factors accounting for 53% of the variance: (1) need for treatment, (2) worry, and (3) presence/outcome of illness. |
| Validity: factor 1 revealed significant associations with the PANSS insight item (r = .58) and the SUMD total (r = .63). Associations were lower but also significant for factor 2 (r = .47; r = .43). Factor 3 was not significantly related to SUMD or PANSS insight; reliability: Cronbach alpha for complete score = .83 and ranged from .72–.86 for the 3 subscales. | ||
| BCIS (self-report)41 | Two components of cognitive insight are assessed: self-reflectiveness (expression of introspection and willingness to acknowledge fallibility) and self-certainty (certainty about beliefs or judgments). | Validity: The Composite Index was correlated (r = −.62) with the SUMD mental disorder item; self-reflectiveness was associated with SUMD delusions (r = −.67). Correlations of self-reflectiveness with IS total score were low (r = .26) and moderate with the IS subscore for awareness of symptoms (r = .36)42; reliability: Cronbach alpha for self-reflectiveness and self-certainty were .67 and .61 for patients with schizophrenia; factor structure: factor analysis supported the 2-factor structure.42 |
Note: ITAQ, Insight and Treatment Attitudes Questionnaire; PSE, Present State Examination; PCA, principal components analysis; SAI, Schedule for Assessing the 3 Components of Insight; PANSS, Positive and Negative Syndrome Scale; SUMD, Scale to Assess Unawareness of Mental Disorder; HDRS, Hamilton Depression Rating Scale; IS, Insight Scale; AII, Awareness of Illness Interview; SALI, Scale to Assess Lack of Insight; BABS, Brown Assessment of Insight Scale; BPRS, Brief Psychiatric Rating Scale; SANS, Scale for the Assessment of Negative Symptoms; SAPS, Scale for the Assessment of Positive Symptoms; SAIQ, Self-Appraisal of Illness Questionnaire; BCIS, Beck Cognitive Insight Scale.
With some exceptions, the scales reveal medium to high intercorrelations (compare table 1). In particular, there are high correlations between the Insight and Treatment Attitudes Questionnaire (ITAQ26), the PANSS insight item,21 the Schedule for Assessing the Three Components of Insight (SAI23,28), the items in the Scale to Assess Unawareness of Mental Disorder (SUMD31) that assess present insight into disorder and social consequences, the insight item of the PSE,20 the Insight Scale (IS34), and the Scale to Assess Lack of Insight,37 which suggests that these measures target a common factor. Correlations with general insight are lower for scales or subscales that address additional aspects of insight, such as insight into past disorder, or are based on a different concept of insight, such as cognitive insight.
The Attitude Questionnaire by Soskis and Bowers24 is not—strictly speaking—an insight scale. Although 2 subscales include the word “insight” the scale assesses attitudes toward illness rather than insight and seems to be more suitable for individuals who already have insight into the presence of disorder. Patients who do not consider themselves as ill might feel resentful toward questions that refer to an illness (eg, “My illness was a big setback in my life”). The Cognitive Insight Scale by Beck and colleagues41 is also based on a different construct, cognitive flexibility, which is claimed to be a necessary precondition for insight.
Self-report scales do not generally differ in terms of internal consistency or reliability, but their association with observer-rated assessments is merely modest. In one study, it was demonstrated that correlations between self- and observer-rated insight are higher if the self-reports are conducted before the observer-rated insight.35 While it seems likely that trained observers might provide a more valid assessment of the construct, their ratings can also be biased by the observation of psychotic symptoms, which is why Amador and Kronengold43 point out the necessity for symptom and insight ratings to be blinded to one another when investigating their relationship.
Many researchers have emphasized the need to use detailed, multidimensional scales. The high correlations between the one-item measures with the total scores of more detailed scales suggest that they seem to be assessing the same construct and that one-item measures might suffice for a screening of overall insight. However, it must be noted that measures that are comprised of multiple items are inherently more stable and reliable than single-item measures and thus generally preferable. In order to draw conclusions about specific aspects of insight, researchers are advised to employ a measure with factor-analytically confirmed dimensions. For example, in studying the relationship between insight and adherence, it might be informative to assess insight into the need for treatment, whereas in the relationship between insight and depression, the awareness of the disorder and its consequences could be more relevant.
Insight and Adherence to Medication
As mentioned above, the link between insight and adherence to treatment seems obvious. Fifteen cross-sectional studies fulfilled our selection criteria. Nine of them found an association between insight and adherence,36,44–51 5 found trends or mixed results,52–56 and 157 found no relationship. Thus, the majority of these studies speak for a clear association of insight and treatment adherence. But does this suffice to predict good long-term adherence for a patient with high insight at discharge? While it seems plausible that poor insight leads to poor adherence, it is also possible that poor adherence results in poor insight either directly (eg, symptoms are denied or mitigated for fear of treatment or future consequences) or mediated by symptom severity. These questions can be clarified using longitudinal designs. We found 9 longitudinal studies on this issue, which are presented in table 2.
Table 2.
Longitudinal Studies Investigating the Impact of Insight on Adherence
| Study | Design | Participants | Measures | Results |
| McEvoy et al58 | Acute episode at baseline, follow-up after 30 d and between 2.5 and 3.5 y | 52 patients with schizophrenia (DSM-III criteria) | Insight: ITAQ | There was a trend for patients with more insight to be more compliant 30 d after discharge. |
| Outcome: phone calls to aftercare clinicians about the patient's outpatient care compliance (appointments and medication) | ||||
| Buchanan59 | Assessment at discharge, follow-up at 1 and 2 y | 61 patients with schizophrenia (Research Diagnostic Criteria) | Insight: Attitude Questionnaire | A “future-positive” view was associated with outpatient attendance and drug treatment compliance at 1 y but not at 2-y follow-up |
| Outcome: records of out-patient compliance (attended appointments) and medication compliance (urinary drug testing) | ||||
| Cuffel et al36 | Assessment at discharge, 6-mo follow-up | 89 patients with schizophrenia (Structured Clinical Interview for DSM, SCID) | Insight: AII | No significant association between baseline awareness and service use/medication adherence during the follow-up period |
| Outcome: compliance self-reports and interviews with collaterals | ||||
| Coldham et al46 | Outpatient at baseline, 1-y follow-up | 143 outpatients with schizophrenia or schizophreniform disorder (SCID) | Insight: PANSS | The nonadherent group had significant poorer insight at both assessments. In a logistic regression analyses, controlling for age, family involvement, premorbid functioning, and cannabis use, insight was not significant. |
| Outcome: scale to rate adherence | ||||
| Novak-Grubik and Tavcar60 | Assessment during inpatient treatment and at 1-y follow-up | 56 patients with schizophrenia, schizophreniform, or schizoaffective disorder (ICD-10) | Insight: PANSS | In a multivariate Cox regression analyses, poor insight at discharge predicted noncompliance with outpatient treatment (OR = 2.00, R2 = .26, ß = 0.69). |
| Outcome: attendance of appointments and medication compliance assessed as self-report and/or reports from key-relatives | ||||
| Tait et al61 | Acute psychosis at baseline, 3- and 6-mo follow-up | 42 patients (at third follow-up) with schizophrenia | Insight: IS | No significant correlation between insight at 3-mo follow-up and service engagement at 6-mo follow-up. |
| Outcome: Service Engagement Scale | ||||
| Byerly et al62 | Outpatient at baseline, trial of compliance therapy, follow-up assessment at 5 mo | 30 patients with schizophrenia or schizoaffective disorder (DSM-IV) | Insight: SAI | In the hierarchical linear model, insight was the only baseline characteristic associated with greater adherence during the follow-up period. |
| Outcome: Medication Event Monitoring, clinical ratings, Medication Adherence Rating Scale | ||||
| Yen et al48 | In remission at baseline, 1-y follow-up | 74 patients with schizophrenia (DSM-IV) | Insight: SAI, SAI-E | Insight correlated positively (r = .24) with medication adherence at index interview but not at 1-y follow-up. |
| Outcome: Medication Adherence Behavior Scale | ||||
| Kamali et al63 | Inpatient at baseline, 6-mo follow-up | N = 60 | Insight: PANSS | Reduced insight is a strong predictor of nonadherence in patients who do not abuse alcohol or other drugs and a weaker but significant predictor in the sample as a whole. |
| First-episode schizophrenia or schizophreniform disorder (SCID) | Outcome: Compliance Interview |
Note: Abbreviations are explained in footnote to table 1. DSM-III, Diagnostic and Statistical Manual for Mental Disorders, Third Edition; ICD-10, International Classification of Diseases, 10th Revision; DSM-IV, Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition, SAI-E Schedule for Assessing the 3 components of insight-Expanded Version.
Among these, 2 studies60,62 investigating comparatively small samples found a relationship between insight and adherence. The first study included only first-episode patients60 and found a clear association between insight and adherence even after controlling for confounding factors such as symptom severity or attitudes toward hospitalization. The second study62 was designed as a treatment study testing for the effect of compliance therapy on adherence. While compliance therapy did not improve adherence, insight was the only characteristic that was associated with greater compliance during the follow-up period. Four studies46,58,59,63 found at least partial associations or trends, and 3 studies36,48,61 did not find a prospective association.
Some thought needs to be given to the differing results on the relationship between insight on future adherence. Possibly, the association between insight and adherence fades over time. Yen et al48 for example found a correlation between insight and adherence at index interview but not at 1-year follow-up. McEvoy et al58 found a trend toward more adherence with outpatient treatment among patients who had insight at discharge for the 30-day follow-up but not for the 2-year follow-up. Insight could be a necessary but not a sufficient precondition for adherence in many patients. Other factors might gain more influence on the patients' adherence over time: eg, the benefit/cost analyses might change and the efforts connected with continuous adherence become more prominent. In particular, medication side effects, such as weight gain, extrapyramidal side effects, or virility problems, might be causing nonadherence in spite of full insight. In addition, attitude toward the disorder or the use of alternative dysfunctional coping strategies could be having a strong impact on adherence. The latter is supported by the fact that some studies found an association between insight and adherence only among patients without drug abuse54,58,63 and the only longitudinal study that found a clear association60 excluded patients with drug abuse. Finally, the weakened relationship between insight and adherence over time may parsimoniously be the result of successful clinical intervention. Patients with poor insight and adherence to medication are more likely to be targeted for interventions such as long-acting injectable antipsychotic medication, participation in motivation-enhancing therapy, or assertive community treatment. That this kind of clinical interventions can be effective in improving compliance is clearly demonstrated in the literature.64–67 Thus, the correlation between insight and adherence might disappear because of the effective intervention. Most of the studies reviewed did not report on interventions that the patients received. Some did report that a large part of patients were receiving medication48,59,60,62 or therapy,62 but it is unclear whether patients with low insight were treated differently.
In addition, there could be a methodological reason for the weakening of association over time. During hospital stay, where most of the index interviews were conducted, there might be more variance in the insight scores, in particular one could expect more patients to have very low insight. For the majority of patients, insight improves with or following treatment.32,68–70 The lower variance in insight scores at follow-up assessments complicates the detection of associations. Finally, symptoms of schizophrenia wax and wane and syndromatic patterns often change over time (eg, a patient may display full-blown psychotic symptoms at first but reveal only negative symptoms at discharge) so that insight and adherence may relate to different phenomena in the course of treatment. For example, a patient may have insight for his/her depression and appreciate antidepressant treatment but might have refused tranquilizers in a state of agitation at admission for fear of their addictive potential.
In sum, the assumption that lack of insight leads to poorer adherence—despite being seemingly obvious—is not clearly supported. The conflicting study results and methodological considerations point to the necessity to investigate shorter periods of time and to control for relevant factors that might have an impact on adherence, such as attitude toward the disorder, use of alternative dysfunctional coping strategies, or treatment factors.
Insight and Course of Symptoms
In their meta-analysis, Mintz et al71 found small but significant mean effect sizes in cross-sectional designs, indicating that higher insight is associated with less global psychopathology as well as with less positive and negative symptoms. The longitudinal studies on insight and pathology can be divided into 4 categories of interest (compare table 3).
Table 3.
Longitudinal Studies Investigating the Relationship Between Insight and Symptoms and Insight and Readmissions
| Study | Design | Participants | Measures | Results |
| Soskis and Bowers24 | Assessment at discharge, follow-up range 3–7 y | 32 patients with schizophrenia | Insight: Attitude Questionnaire | No significant correlation between number of rehospitalizations and attitude variables. |
| Outcome: number of rehospitalizations | ||||
| McEvoy et al26,58 | Assessment approximately 5 d after admission, after 2 wk and at discharge | 52 patients with DSM-III schizophrenia | Insight: ITAQ | No significant correlation between insight and psychopathology at time 1. At time 2 global severity (r = −.41) and BPRS (r = −.35) and at discharge global severity (r = −.30) correlated significantly with insight. Change in insight showed no significant association to change in psychopathology. Significantly less readmissions among patients with insight. |
| Psychopathology: BPRS and CGI Global Severity Item, records about readmissions and time in hospital | ||||
| McEvoy72 | Assessment in outpatient settings, follow-up at 1 y | 25 patients with DSM-III schizophrenia and schizoaffective disorder | Insight: ITAQ | Insight was not related to exacerbation of symptoms. The 3 patients who were rehospitalized had lower insight scores at baseline (15.3 vs 19.2). |
| Outcome: BPRS, CGI, and hospitalizations | ||||
| Michalakes et al70 | Assessment at admission, after 15 and 30 d, and at discharge | 42 patients with schizophrenia | Insight: ITAQ | Insight improved significantly and was significantly related to BPRS scores only at discharge (r = −.40) |
| Psychopathology: BPRS | ||||
| Kemp and Lambert32 | Assessment at admission and at discharge (3–6 wk after admission) | 29 patients admitted to acute ward and met DSM-III-R criteria for schizophrenia | Insight: modified version of SUMD | Symptoms were significantly correlated with insight subscales at admission and discharge. Improvement in present insight was not associated with change in symptoms. Improved insight into past symptoms was associated with improvement in negative (r = .53) and positive symptoms (r = .41) and general psychopathology (r = .53). |
| Psychopathology: PANSS | ||||
| Jørgensen et al68 | Assessment in first week of admission, reassessment every 2 wk. Total of 5 assessments. | 50 patients with DSM-IV and ICD-10 schizophrenia (and at least one previous admission) | Insight: IS | Patients were divided into 3 categories: total remission of delusional beliefs, partial remission, and no remission. Insight increased in all groups. For the majority of patients (68%), insight was not influenced by the recovery from delusional beliefs. However, of the minority of patients who remained low on insight (22%), all recovered only partially from symptoms. |
| Psychopathology: PANSS | ||||
| Smith et al73 | Assessment at discharge and after a mean of 20.4 (inpatients) and 86.7 d (outpatients) | 33 patients with schizophrenia and schizoaffective disorders (Structural Clinical Interview for DSM-IV) | Insight: SUMD | No significant correlation between insight and positive, negative, and disorganized symptoms at discharge. At follow-up, disorganized symptoms were correlated with current awareness and misattribution. Changes in past awareness were associated with changes in disorganized symptoms but not with changes in positive or negative symptoms. |
| Psychopathology: SANS, SAPS | ||||
| Chen74 | Assessment at admission and at discharge | 59 inpatients with schizophrenia or schizoaffective disorder | Insight: SUMD | Insight was not related to symptoms at time 1. Upon discharge, emotional withdrawal, disorganization, hostility, suspiciousness, unusual thought content, and uncooperativeness were related to poor insight. Reductions in uncooperativeness and emotional withdrawal were correlated with improved insight. |
| Psychopathology: BPRS | ||||
| Caroll et al75 | Assessment before discharge, assignment to intervention or control group, and reassessment after 12 wk | 100 patients with DSM-III-R schizophrenia (with at least one previous psychotic episode) | Insight: ITAQ | At baseline, insight correlated negatively with positive (r = −.41) and negative symptoms (r = −.20). In the stepwise regression final equation, only positive symptoms (ß = .43) and depression scores (ß = .26) made significant contributions to predicting insight. |
| Symptoms: PANSS | Change in positive and negative symptoms did not correlate significantly with change in insight. | |||
| Weiler et al69 | Assessment at admission and discharge from psychiatric hospital | 81 patients (DSM-III-R schizophrenia) | Insight: ITAQ | Change in insight and change in BPRS total correlated significantly (r = .52) as well as insight change and change in positive symptoms (r = .40). Associations were strongest for the disorganized subtype and lowest for the paranoid subtype. |
| Psychopathology: BPRS | ||||
| Yen et al76 | Baseline assessment of outpatients, 1-y follow-up | 74 patients with schizophrenia (DSM-IV) | Insight: SAI, SAI-E | Rehospitalized patients had significant lower scores for insight into treatment at index assessment but not for insight into mental health status, psychotic experiences, or total SAI-E scores. |
| Outcome: frequency of hospitalization | ||||
| Mintz et al77 | Assessment at admission to early psychosis program, after 3, 6, and 12 mo. | 180 patients with first-episode psychosisa | Insight: PANSS insight item (G12) | Participants with low insight had more positive and negative symptoms at all assessments. |
| Psychopathology: PANSS | Stable insight was associated with improved symptoms compared with stable lack of insight or detoriation in insight. Improved insight by 1 y was associated with improved symptoms. | |||
| Gharabawi et al8 | First assessment at enrollment in a risperidone treatment trial, followed by assessments at weeks 12, 24, 48, and 50. | 614 patients with schizophrenia or schizoaffective disorder | Insight: PANSS insight item (G12). | Patients improved significantly on PANSS total from baseline to end point, regardless of baseline insight. Patients with severe lack of insight at baseline had the highest overall level of symptoms at baseline and follow-up. Changes in insight scores corresponded with changes in symptom domains. Correlations were highest for changes in disorganized thought, followed by negative symptoms and anxiety/depressive symptoms. |
| Symptoms: PANSS total and 3 factors: negative symptoms, anxiety/depressive symptoms, and disorganized thought |
Note: Abbreviations are explained in footnote to table 1. DSM-IV, schizophrenia, schizophreniform disorder, delusional disorder, brief psychotic disorder, psychotic disorder not otherwise specified, or drug induced psychosis; CGI, Clinical Global Impressions; DSM-III, Diagnostic and Statistical Manual for Mental Disorders, Third Edition; DSM-III-R, Diagnostic and Statistical Manual for Mental Disorders, Revised Third Edition; DSM-IV, Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition; ICD-10, International Classification of Diseases, 10th Revision; SAI-E, Schedule for Assessing the 3 components of Insight Expanded Version.
Seven studies investigated cross-sectional associations at 2 or more time points. These studies are not longitudinal in the strict sense of investigating the impact of insight at time one on symptoms at a later time. However, the repetition of assessments contributes to our knowledge of the long-term stability of the association between insight and symptoms. The results of these studies do not support the idea of a stable association of symptom severity and insight. While 2 studies found insight and symptoms to be significantly correlated at both assessments,32,77 the majority found the association only for the second assessment.26,70,73,74 In the meta-analysis by Mintz et al,71 acute patient status was found to be a moderator for the relationship between symptoms and insight. However, their results suggest that the relationship is stronger for acute patients.
Eight studies investigated whether changes in insight are associated with changes in symptoms. Of these, 3 studies found change in present insight to be unrelated to change in symptoms,26,32,75 2 found mixed results,68,73 and 4 found significant associations.8,69,74,77 If significant associations are detected, they seem to be stronger for past insight32,73 and for symptoms of disorganization.8,69,73,74 It must also be pointed out that the study by Smith et al,73 finding an association between change in past insight and change in symptoms of disorganization, was the only study to report the use of different raters for symptoms and insight as advised by Amador and Kronengold.43
No study investigated whether insight at first assessment predicts symptoms at the second time point, although Mintz et al77 found stable insight to be associated with lower symptom levels at follow-up assessments. Gharabawi et al8 found all patients to improve, but those with high baseline insight to have less symptoms at baseline and end point compared with those with moderate or low baseline insight.
Four studies investigated the impact of insight on rehospitalizations. Three of these58,72,76 found that greater insight was connected to fewer rehospitalizations. Only one study failed to find an association,24 but this study employed an attitude questionnaire, whereas the others used insight scales, such as the ITAQ26 and the SAI.23,28
So far, the results speak for a complex association of insight and symptoms over time, although it must be pointed out that no study has directly investigated the predictive value of insight in a suitable design, by analyzing the relationship between insight at baseline (eg, discharge) and symptom severity at time 2 while controlling for insight at time 2. Also, studies on course of symptoms have largely failed to control for patient status (acute, in remission, remitted) as well as time of investigation (admission, discharge, follow-up), but this would be helpful as status and time of assessment seem to have an impact on the strength of the relationship.
Insight and Functional Outcome
Studies exploring the impact of insight on functioning have focused on different components. While some investigated functional outcome in the classical sense (general level of functioning), others concentrated on more specific aspects, such as work behavior or social functioning.
Among the 13 cross-sectional studies, 86,45,78–83 found significant or at least partially significant results, and 5 did not find insight to be associated with functioning.84–88 All 5 longitudinal studies, that are presented in table 47,24,76,79,89 found at least partially significant results.
Table 4.
Longitudinal Studies Investigating the Impact of Insight on Social Adjustment and Functional Outcome
| Study | Design | Participants | Measures | Results |
| Soskis and Bowers24 | Baseline at discharge, follow-up range 3–7 y | 32 patients with schizophrenia | Insight: Attitude questionnaire | Social adjustment—a positive, integrating attitude was correlated with higher levels of performance of socially expected activities and lower levels of symptom discomfort |
| Outcome: Brief Follow-up Rating, Katz Adjustment Scale | ||||
| Lysaker89 | At baseline enrolled in rehabilitation, 5-wk follow-up | 42 patients with schizophrenia and schizoaffective disorder (DSM-III-R) | Insight: PANSS | Work performance and participation—insight was significantly related to fewer weeks of participation (r = −.37), poorer social skills (r = −.37), and personal presentation on the job (r = −.33). In a stepwise regression analyses controlling for symptoms, insight was not significant. |
| Outcome: Work Personality Profile, Work participation | ||||
| Schwartz et al79 | Inpatient at baseline, 1-y follow-up | 23 patients with chronic schizophrenia (DSM-IV) | Insight: SUMD | Functional level—significant relationship between total insight and Functional Skill Rating Form baseline (r = .53) and follow-up scores (r = .70) and Global Assessment of Functioning follow-up scores (r = .65). Insight into illness accounted for 28% of the variance in functional skill level at baseline and approximately half of the variance in functional skill and global functioning after treatment. Insight did not predict functional skills and global functioning at initial assessment but improvement by follow-up. |
| Outcome: Global Assessment of Functioning, Functional Skill Rating Form | ||||
| Lysaker et al7 | Outpatient at baseline, 3-, 5-, and 7-wk follow-up | 85 patients with schizophrenia and schizoaffective disorder (SCID) | Insight: SUMD | Work performance—after controlling for neurocognitive deficits, the impaired insight group showed significantly poorer performance in cooperativeness and personal presentation, trends in poorer work habits and quality, and no differences for social skills. |
| Outcome: Work Behavior Inventory | ||||
| Yen et al 76 | Outpatient at baseline, 1-y follow-up | 74 patients with schizophrenia (DSM-IV) | Insight: SAI, SAI-E | Social functioning-patients with good social adjustment had higher index scores for insight into treatment than patients with poor social adjustment. There were no differences for the other SAI and SAI-E scores |
| Outcome: Community Life Scale |
Note: Abbreviations are explained in footnote to table 1. DSM-III-R, Diagnostic and Statistical Manual for Mental Disorders, Revised Third Edition; DSM-IV, Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition.
Thus, it seems that insight is not related to present functioning but has an impact on improvements in functioning. This assumption is supported by the study from Schwartz et al.79 They found a general level of functioning to be only partly related to insight at baseline. After baseline assessment, each patient received cognitive behavioral counseling. At follow-up, baseline insight was found to predict the improvement on the 2 investigated functional level scales.
The long-term relationship between insight and functional outcome is likely to be mediated by symptom severity. As was shown in the “Insight and Course of Symptoms” section, higher baseline insight is associated with less symptoms and fewer rehospitalizations at follow-up and this might explain better functioning. Most studies did not control for symptom severity and in the only study that did89 the association was no longer significant in the multivariate analysis.
Insight and Aggressive Behavior
In his recent review, Bjørkly10 reports a total of 9 studies on insight and violence in mentally ill patients. Our literature search added one additional study.90 Five of these studies found a positive relationship between lack of insight and violence91–95 and 5 did not.76,90,96–98 However, the exclusion of studies investigating diagnostically heterogeneous patient samples93,94 leads to a somewhat different picture. In the study by Foley et al,95 patients were analyzed separately by diagnosis, and the significant relationship between insight and violence that was found for the whole group was not found for the subsample of schizophrenia patients. Taken together, only 2 studies remain that found a significant relationship between insight and violence in patients with schizophrenia.91,92 One of these employed a prospective, longitudinal design.91 In contrast, 6 studies investigating patients with schizophrenia did not find an association between insight and violence,76,90,95–98 of these, 2 studies76,90 applied prospective longitudinal designs. Thus, in spite of an intuitive link between insight and violence, the present state of research does not provide clear support for a causal relationship. In order to gain a more definite answer, further studies are needed that apply prospective study designs. In addition, the lack of significant findings might be due to the failure to take into account relevant moderator variables such as adherence and substance abuse, which in turn lead to an exacerbation of symptoms, resulting in more violence.
Insight and Depression and Suicide
Fifteen studies that investigated the association between insight and depression in cross-sectional designs were analyzed in the meta-analysis by Mintz et al.71 They found a low positive association of r = .18 (confidence interval = −0.14–0.49) between insight and depression, interpreted as “as depressive symptoms increased, insight increased.” This association has been replicated in more recent studies.98,99 Moreover, all the reviewed cross-sectional studies found insight to be related with increased suicidal ideation or actions.100–105 Again, the problem with cross-sectional designs is the interpretation of causal direction. Increase in insight could be causing increase in symptoms of depression, as postulated by defense theorists (eg, if growing insight into the presence of a mental disorder and its long-term consequences results in feelings of worthlessness and hopelessness). On the other hand, more cognitively oriented research emphasizes the role of attribution in understanding insight because there is some evidence that persons with a higher level of depression are more accurate in their self-evaluations (compare Amador and Kronengold for a description of these studies43). Thus, depressed mood could be causing change in attribution processes resulting in a more accurate view of the self and thus a higher level of insight. Longitudinal studies in support of the defense theory should find growing insight to precede depression, whereas attribution theories would be supported if depression precedes insight.
Longitudinal Studies that Measure Insight and Depressive Symptoms over time are presented in table 5.
Table 5.
Longitudinal Studies Investigating the Relationship Between Insight and Depression
| Study | Design | Participants | Measures | Results |
| Smith et al73 | Assessment at discharge and after an average of 20.4 d for inpatients and 86.7 d for outpatients | 33 patients with schizophrenia and schizoaffective disorders (Structured Clinical Interview for DSM-IV) | Insight: SUMD | Unawareness of current and past symptoms and misattribution of current symptoms were correlated with depression at time one (r = −.46–.58). After entering depression, disorganized symptoms, positive symptoms, and treatment unit in linear regression analyses, depression was the only significant predictor for unawareness and misattribution of current symptoms (R2 = 28–31%). Increase in depression by 2. Assessment was associated with more awareness |
| Depression: BPRS | ||||
| Symptoms: SANS, SAPS | ||||
| Crumlish et al106 | Assessment at presentation to clinic, at 6 mo and 4 y | 101 patients with first episode of schizophrenia or schizoaffective disorder | Insight: PANSS insight, IS. | The PANSS lack of insight items at presentation and at 6 mo did not predict depression at 4 y or suicide in the follow-up period. Using the Birchwood Scale, greater insight at 6 mo predicted higher depression at 4 y and suicide in the follow-up period. |
| Depression: PANSS anxiety, depression, somatic concern, and guilt items | ||||
| Drake et al107 | Assessment within 14 d after admission, reassessments after 6 and 12 wk and 18 mo | 257 patients with schizophrenia, schizoaffective, schizophreniform, delusional disorder, or psychosis not otherwise specified (DSM-IV) | Insight: IS, PANSS insight | The association between depression and insight at baseline was r = .43, and for insight and self-esteem r = .37. Cross-lagged associations were generally weak. The pattern of associations was similar at each stage: Better insight predicted more depression and was associated with lower self-esteem. Greater paranoia predicted greater depression. The link between insight and depression was not just mediated by low self-esteem or paranoia. |
| Depression: PANSS anxiety, depression, avolition, and guilt | ||||
| Self-esteem: Rosenberg Self-Esteem Scale | ||||
| Smith et al108 | Assessment at discharge and follow-up at 6 mo) | 50 patients with schizophrenia or schizoaffective disorder (SCID for DSM-IV) | Insight: SUMD | Depression at discharge was not associated with current awareness of positive or negative symptoms, but patients with depression showed more improvement of insight into past symptoms (ß = −.36 in regression model) |
| Depression: BPRS | ||||
| Symptoms: BPRS | ||||
| Iqbal et al109 | Assessment during acute stage, upon recovery and 12 mo after recovery | 105 patients with ICD-10 schizophrenia (of which 78% completed all assessments) | Insight: IS | Prior to postpsychotic, patients reported more negative appraisals of the disorder and lower self-esteem in comparison to those without postpsychotic depression but did not differ in insight. During depression, patients reported higher insight into disorder, increase in negative appraisals, and decrease in self-esteem. |
| Attitudes: PBIQ | ||||
| Depression: BDI, CDSS, DEQ | ||||
| Self-esteem: Self-Esteem Scale | ||||
| Caroll et al75 | Assessment before discharge, random assignment to intervention or control group and reassessment after 12 wk | 100 patients with DSM-III-R schizophrenia (with at least one previous psychotic episode in the past) | Insight: ITAQ | At baseline, insight correlated positively with depression (r = .23). 22% of the variance of baseline insight could be explained by gender, depression, positive and negative symptoms, age, and illness duration. In the final equation, only positive symptoms (ß = .43) and MADRS scores (ß = .26) made significant contributions to predicting insight. |
| Symptoms: PANSS | In the regression analysis to predict change in insight by change in positive and negative symptoms and depression, only MADRS change contributed significantly (ß = .24) | |||
| Depression: MADRS | ||||
| Yen et al76 | Assessment in out and inpatient settings, follow-up at 1 y. | 74 patients with DSM-IV schizophrenia in remission | Insight: SAI | One patient had committed suicide by follow-up and 7 had planned suicide attempts. Insight was not significantly correlated with suicidal tendency during the 1-y follow-up. |
| Symptoms: PANSS | ||||
| Suicide: VASA | ||||
| Bourgeois et al110 | Weekly assessment of suicide events in months 1–6, biweekly in months 6–24. Assessment of depression and awareness at weeks 24, 52, and 104. | 980 patients with schizophrenia or schizoaffective disorder and high risk for suicide | Insight: Item 12 from Scale of Functioning | Results of Cox proportional hazards analysis for main effects of baseline variables demonstrated that greater awareness significantly predicted suicide events (hazards ratio = 1.17). However, the inclusion of depression at in the model baseline rendered awareness nonsignificant. |
| Depression: CDSS | ||||
| Suicide: blinded judgments of suicide events (suicide attempt or hospitalization to prevent suicide) | Although baseline awareness was a risk factor, increases in awareness as a function of treatment were associated with a decreased risk of suicide events (hazards ratio = 0.75). |
Note: DSM-IV, Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition; ICD-10, International Classification of Diseases, 10th Revision; PBIQ, Personal Beliefs About Illness Questionnaire; BDI, Beck Depression Inventory; CDSS, Calgary Depression Scale for Schizophrenia; DEQ, Depressive Experiences Questionnaire; DSM-III-R, Diagnostic and Statistical Manual for Mental Disorders, Revised Third Edition; MADRS, Montgomery and Asberg Depression Rating; VASA, Violence and Suicide Assessment Scale.
These studies all report significant relationships between insight and depression, but the interpretation of the results is complicated by the fact that they investigated different directions of causal relationships and have used different methods. Some studies investigated whether an increase in depression is associated with more awareness73 or whether depression predicted improvement in insight,75,108 while others investigated whether insight predicted later depression.106,107,109 Thus, so far, the results of these studies could be interpreted as evidence for both “defense theories” and “attribution theories,” and authors have drawn different conclusions from the results. Unfortunately, most studies have applied designs that do not allow to infer which of the postulated mechanisms is more appropriate because the strength of associations have not been compared and attributions have not been assessed. An exception to this is the study by Iqbal et al.109 In this study, patients who developed postpsychotic depression reported more negative attitudes toward their disorder, such as greater loss, humiliation, and entrapment by the disorder and were more likely to see themselves in a lower social status in future than patients who did not develop postpsychotic depression. However, while the differences in appraisal between depressed and not depressed participants could be found prior to postpsychotic depression, the differences in insight were only found during the postpsychotic depression. Following from the results of this study, it seems that the appraisal of the disorder and its implications are relevant mechanisms for the development of postpsychotic depression and not the amount of prior insight. These results do not support a defense theory of insight because insight does not increase before depression. However, they also do not provide clear support for attribution theories because the negative evaluations precede postpsychotic depression rather that resulting from depression. Some data in support of an attribution explanation is provided by Moore et al111 who found that scores for self-deception correlated significantly with current awareness of disorder and insight into the social consequences. In addition, the studies that investigated the impact of insight on long-term suicide76,110 both report negative findings, which also seems to contradict a defense theory of insight. Additional support for attribution theories could be derived from the consistent finding that insight is higher in persons diagnosed with major depression as compared with persons with schizophrenia.81,112 However, it must be noted that both Pini et al112 and Amador et al,81 who report on these findings do not state that depression increases insight but rather that the higher level of insight in depressive patients might be due to differences in cognitive impairment. Taken together, the processes connecting insight to depression need further clarification before conclusions can be drawn. It seems likely that insight and symptoms of depression are in a constant day-to-day interaction process that is difficult to assess by studies applying broad time frames and assessments. In order to estimate the risk associated with growing insight, it could be informative to distinguish between depression in the sense of an affective mental disorder and depression in the sense of a normal psychological reaction to a negative life event.
Discussion and Implications for Future Research
The current review aimed at gaining a clearer picture of the impact of insight on adherence, course of symptoms, and functioning in persons with schizophrenia. Overall, the reviewed studies did not provide definite clarity in many of the target domains. Nevertheless, some preliminary conclusions can be drawn and more importantly some recommendations for future research to which we will turn later: insight is associated with adherence during treatment phase, but the relationship between insight and long-term adherence needs further clarification because nonsignificant findings might be explained by confounding factors. Insight is also associated with higher symptom levels during treatment and, for the majority of patients, insight increases while symptoms, particularly disorganization, decrease. Insight seems to have predictive value for functioning, although this finding might be accounted for by the association between symptoms and insight. Finally, in spite of clear evidence for cross-sectional and longitudinal relationships between insight and depression, the causal direction of the relationship remains unclear.
A general problem that we encountered in this review is the apparent divergence of findings. We think that some of the main reasons for this can be found in the imprecise definitions of insight and differences in study designs.
Problems With the Definition and Assessment of Insight
A precise definition and assessment of insight and insight dimensions is a necessary precondition for conclusive insight research. With the exception of the self-report, Self-Appraisal of Illness Questionnaire (SAIQ40) measures of insight have largely failed to support the postulated separate dimensions. Specifically, factor analyses of the items in the ITAQ,26 the IS,34 the SAI,23 and the Awareness of Illness Interview36 all failed to produce separate factors for awareness of disorder and need for treatment. Interpretation of the factor analyses is complicated by the fact that many of the measures do not directly assess the insight into symptoms, which is likely to be a necessary precondition to any other dimension of insight. A patient who is not aware of the presence of symptoms will have problems answering questions about the attribution of symptoms to an illness or the need for treatment and might provide inconsistent answers to questions addressing these aspects. Thus, we suggest to separate the concept of awareness of symptoms from the attribution of symptoms as mental as in the approach taken by Amador et al in the SUMD.31 Second, we think that awareness of need for treatment, awareness of social consequences of the disorder or worry (as assessed in the SAIQ40) are more appropriately defined as “attitudes concerning illness” and are possibly influenced by different factors than insight, such as prior experiences with the mental health system or cultural beliefs. Again, it may be that insight into disorder is a necessary precondition for consistent answers to questions concerning attitudes.
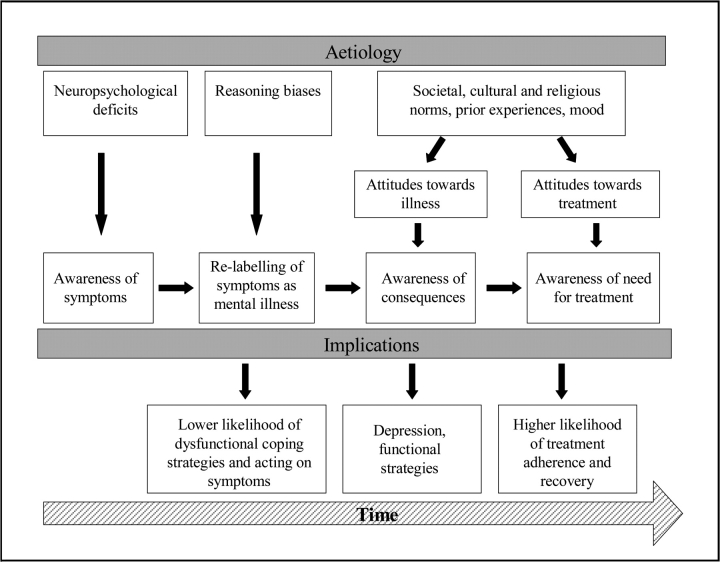
With regard to research on the impact of insight on adherence and outcome, we suggest analyzing the interaction of insight dimensions in an hierarchical order and hypothesize that several steps of insight have to be traversed before insight can be expected to predict treatment adherence. An investigation of this process should take into account that the different components of insight might also differ in their etiology. For example, unawareness of symptoms might be more directly associated with neuropsychological deficits and the labeling of symptoms as mental illness might be associated with reasoning biases (eg, external attribution, jumping to conclusions), whereas not accepting the diagnosis of mental disorder or its implications might be closely linked to attitudes toward treatment. In figure 1 we present a graphical depiction of a possible hierarchical course of insight components over time and the way in which they are likely to differ in origin and implications.
Fig. 1.
Model of the Etiology and Implications of Insight Components over Time.
To complicate the matter of assessment further, it cannot necessarily be assumed that patients are being open about their level of insight. Clinical observations show that some patients tend to verbally express insight in order to be left alone by doctors or therapists. In these cases, we can hardly expect insight to produce the same changes in behavior as in a person with “real” insight.
Problems in Study Designs
In summarizing the studies, we have gained the impression that only very few studies were originally designed to investigate the role of insight. For one, studies have not been sufficiently precise in the aspect of insight that is to be investigated. As pointed out above, different dimensions of insight are probably related to different aspects of outcome, and this needs to be reflected in the study-planning phase. In addition, researchers have not always chosen the most rigorous methodological designs. This accounts specifically for studies that have investigated long periods of time, mostly involving discharge from hospital and reintegration, without assessing and controlling the relevant moderating variables for the relationship of interest. Specifically, we suggest to control for treatment effects, attitudes to treatment, and dysfunctional coping behavior in the relationship between insight and adherence, for symptom severity in the relationship of insight and functioning, for symptoms, adherence, and substance abuse in the relationship between insight and violence, for attributions in the relationship between insight and depression, and for patient status in the relationship between insight and symptoms.
In conclusion, while more and better research on the phenomenology, etiology, and impact of insight is needed in order to estimate the strength of the associations, the current review seems to underline that insight plays an important role in the recovery process of schizophrenia. The association between growing insight, negative attributions, and depression on the one hand and better functioning and reduction of symptoms on the other fits in well with the consumer-oriented approach to recovery, which emphasizes the nonlinear process of recovery in which the consumer gradually adapts to and moves beyond the illness on a journey “that bumps along the way.”113 From the clinical perspective, the key to minimizing the risk of depression and suicide while promoting functional coping behaviors following increase in insight could be to increase “usable insight” that separates the symptoms of the disorder from reality and separates the disorder from identity while preserving hope.14 This approach is in line with some of the recent recommendations for effective recovery-oriented services113 but is empirically supported by a study from Lysaker et al,114 who found that insight in connection with hope predicts better functional coping. Normalizing approaches to explaining the development and maintenance of symptoms, as have been put forward in cognitive behavior therapy approaches to delusions and hallucinations, (eg,115) can be helpful in promoting usable insight. By emphasizing the similarities to normal experiences rather than the differences, health professionals can support patients in developing a nonthreatening explanation of symptoms that is more likely to lead to functional coping behavior rather than to depression or hopelessness.
Acknowledgments
We would like to thank Privat Dozeut Dr Steffen Moritz and Prof Reinhard Maß for their helpful comments on earlier versions of the manuscript.
References
- 1.Jones C, Cormac I, Silveira da Mota Neto JI, Campbell C. Cognitive therapy for schizophrenia. Cochrane Database Syst Rev. 2004;4:1–57. doi: 10.1002/14651858.CD000524.pub2. [DOI] [PubMed] [Google Scholar]
- 2.Leucht S, Pitschel-Walz G, Abraham D, Kissling W. Efficacy and extrapyramidal side-effects of the new antipsychotics olanzapine, quetiapine, risperidone, and sertindole compared to conventional antipsychotics and placebo. A meta-analysis of randomized controlled trials. Schizophr Res. 1999;35:51–68. doi: 10.1016/s0920-9964(98)00105-4. [DOI] [PubMed] [Google Scholar]
- 3.Wallace C, Mullen P, Burgess P. Criminal offending in schizophrenia over a 25-year period marked by deinstitutionalization and increasing prevalence of comorbid substance use disorders. Am J Psychiatry. 2004;161:716–727. doi: 10.1176/appi.ajp.161.4.716. [DOI] [PubMed] [Google Scholar]
- 4.Wiersma D, Wanderling J, Dragomirecka E, et al. Social disability in schizophrenia: its development and prediction over 15 years in incidence cohorts in six European countries. Psychol Med. 2000;30:1155–1167. doi: 10.1017/s0033291799002627. [DOI] [PubMed] [Google Scholar]
- 5.Sevy S, Nathanson K, Visweswaraiah H, Amador X. The relationship between insight and symptoms in schizophrenia. Compr Psychiatry. 2004;45:16–19. doi: 10.1016/j.comppsych.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 6.Dickerson FB, Boronow JJ, Ringel N, Parente F. Lack of insight among outpatients with schizophrenia. Psychiatr Serv. 1997;48:195–199. doi: 10.1176/ps.48.2.195. [DOI] [PubMed] [Google Scholar]
- 7.Lysaker P, Bryson GJ, Bell M. Insight and work performance in schizophrenia. J Nerv Ment Dis. 2002;190:142–146. doi: 10.1097/00005053-200203000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Gharabawi GM, Lasser RA, Bossie CA, Zhu Y, Amador X. Insight and its relationship to clinical outcomes in patients with schizophrenia or schizoaffective disorder receiving long-acting risperidone. Int Clin Psychopharmacol. 2006;21:233–240. doi: 10.1097/00004850-200607000-00006. [DOI] [PubMed] [Google Scholar]
- 9.McGlashan TH, Carpenter WTJ. Postpsychotic depression in schizophrenia. Arch Gen Psychiatry. 1976;33:231–239. doi: 10.1001/archpsyc.1976.01770020065011. [DOI] [PubMed] [Google Scholar]
- 10.Bjørkly S. Empirical evidence of a relationship between insight and risk of violence in the mentally ill—a review of the literature. Aggress Violent Behav. 2006;11:414–423. [Google Scholar]
- 11.Pompili M, Ruberto A, Kotzalidis G, Girardi P, Tatarelli R. Suicide and awareness of illness in schizophrenia: an overview. Bull Menninger Clin. 2004;68:297–318. doi: 10.1521/bumc.68.4.297.56643. [DOI] [PubMed] [Google Scholar]
- 12.Amador XF, Strauss DH, Yale SA, Gorman JM. Awareness of illness in schizophrenia. Schizophr Bull. 1991;17:113–132. doi: 10.1093/schbul/17.1.113. [DOI] [PubMed] [Google Scholar]
- 13.Schwartz RC. The relationship between insight, illness and treatment outcome in schizophrenia. Psychiatr Q. 1998;69:1–22. doi: 10.1023/a:1022141322657. [DOI] [PubMed] [Google Scholar]
- 14.Lewis L. Mourning, insight reduction of suicide risk in schizophrenia. Bull Menninger Clin. 2004;68:231–244. doi: 10.1521/bumc.68.3.231.40405. [DOI] [PubMed] [Google Scholar]
- 15.Dam J. Insight in schizophrenia: a review. Nordic J Psychiatry. 2006;60:114–120. doi: 10.1080/08039480600600185. [DOI] [PubMed] [Google Scholar]
- 16.McEvoy JP. The relationship between insight into psychosis and compliance with medications. In: Amador X, David A, editors. Insight and Psychosis. Awareness of Illness in Schizophrenia and Related Disorders. Oxford: University Press; 2004. pp. 311–333. [Google Scholar]
- 17.Torrey EF. The relationship of insight to violent behaviour and stigma. In: Amador X, David A, editors. Insight and Psychosis. Awareness of Illness in Schizophrenia and Related Disorders. Oxford, England: University Press; 2004. pp. 243–256. [Google Scholar]
- 18.Endicott J, Spitzer RL. A diagnostic interview: the schedule for affective disorders and schizophrenia. Arch Gen Psychiatry. 1978;35:837–844. doi: 10.1001/archpsyc.1978.01770310043002. [DOI] [PubMed] [Google Scholar]
- 19.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wing JK, Cooper JE, Sartorius N. Measurement and classification of psychiatric symptoms: an instruction manual for the PSE and catego programme. Cambridge, England: Cambridge University Press; 1974. [Google Scholar]
- 21.Kay SR, Fiszbein A, Opler LA. The Positive and Negative Syndrome Scale (PANSS) for Schizophrenia. Schizophr Bull. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 22.AMDP . Manual zur Dokumentation Psychiatrischer Befunde. Goettingen, Germany: Hogrefe; 2000. Das AMDP-System. [Google Scholar]
- 23.David AS. Insight and psychosis. Br J Psychiatry. 1990;156:798–808. doi: 10.1192/bjp.156.6.798. [DOI] [PubMed] [Google Scholar]
- 24.Soskis DA, Bowers MB. The schizophrenic experience. A follow-up study of attitude and post hospital adjustment. J Nerv Ment Dis. 1969;149:443–449. [PubMed] [Google Scholar]
- 25.Davidhizar RE. Beliefs, feelings and insight of patients with schiozophrenia about taking medication. J Adv Nurs. 1987;12:177–182. doi: 10.1111/j.1365-2648.1987.tb01318.x. [DOI] [PubMed] [Google Scholar]
- 26.McEvoy JP, Apperson LJ, Applebaum PS, et al. Insight in schizophrenia. Its relationship to acute psychopathology. J Nerv Ment Dis. 1989;177:43–47. doi: 10.1097/00005053-198901000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Sanz M, Constable G, Lopez-Ibor I, Kemp R, David AS. A comparative study of insight scales and their relationship to psychopathological and clinical variables. Psychol Med. 1998;28:437–446. doi: 10.1017/s0033291797006296. [DOI] [PubMed] [Google Scholar]
- 28.David A, Buchanan A, Reed A, Almeida O. The assessment of insight in psychosis. Br J Psychiatry. 1992;161:599–602. doi: 10.1192/bjp.161.5.599. [DOI] [PubMed] [Google Scholar]
- 29.Marková I, Berrios GE. The assessment of insight in clinical psychiatry: a new scale. Acta Psychiatr Scand. 1992;86:159–164. doi: 10.1111/j.1600-0447.1992.tb03245.x. [DOI] [PubMed] [Google Scholar]
- 30.Marková I, Berrios GE. Insight in clinical psychiatry. J Nerv Ment Dis. 1995;183:743–751. doi: 10.1097/00005053-199512000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Amador XF, Strauss DH, Yale SA, Flaum MM, Endicott J, Gorman JM. The assessment of insight in psychosis. Am J Psychiatry. 1993;150:873–879. doi: 10.1176/ajp.150.6.873. [DOI] [PubMed] [Google Scholar]
- 32.Kemp RA, Lambert TJ. Insight in schizophrenia and its relationship to psychopathology. Schizophr Res. 1995;18:21–28. doi: 10.1016/0920-9964(95)00018-6. [DOI] [PubMed] [Google Scholar]
- 33.Cuesta MJ, Peralta V, Zarzuela A. Reappraising insight in psychosis: multi-scale longitudinal study. Br J Psychiatry. 2000;177:233–240. doi: 10.1192/bjp.177.3.233. [DOI] [PubMed] [Google Scholar]
- 34.Birchwood M, Smith J, Drury V, Healy J, MacMillian F, Slade MA. A self-report insight scale for psychosis: reliability, validity, and sensitivity to change. Acta Psychiatr Scand. 1994;89:62–67. doi: 10.1111/j.1600-0447.1994.tb01487.x. [DOI] [PubMed] [Google Scholar]
- 35.Young DA, Campbell Z, Zakzanis KK, Weinstein E. A comparison between an interview and a self-report method of insight assessment in chronic schizophrenia. Schizophr Res. 2003;63:103–109. doi: 10.1016/s0920-9964(02)00378-x. [DOI] [PubMed] [Google Scholar]
- 36.Cuffel BJ, Alford J, Fischer EP, Owen RR. Awareness of illness in schizophrenia and outpatient treatment adherence. J Nerv Ment Dis. 1996;184:653–659. doi: 10.1097/00005053-199611000-00001. [DOI] [PubMed] [Google Scholar]
- 37.Dębowska G, Grzywa A, Kucharska-Pietura K. Insight in paranoid schizophrenia—its relationship to psychopathology and premorbid adjustment. Compr Psychiatry. 1998;39:255–260. doi: 10.1016/s0010-440x(98)90032-3. [DOI] [PubMed] [Google Scholar]
- 38.Eisen JL, Philipps KA, Baer L, Beer DA, Atala KD, Rasmussen SA. The Brown Assessment of Beliefs Scale: reliability and validity. Am J Psychiatry. 1998;155:102–108. doi: 10.1176/ajp.155.1.102. [DOI] [PubMed] [Google Scholar]
- 39.Kaplan GB, Phillips KA, Vaccaro A, Eisen JE. Assessment of insight into delusional beliefs in schizophrenia using the Brown Assessment of Beliefs Scale. Schizophr Res. 2006;82:279–281. doi: 10.1016/j.schres.2005.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Marks KA, Fastenau PS, Lysaker PH, Bond GR. Self-Appraisal of Illness Questionnaire (SAIQ): relationship to researcher-rated insight and neuropsychological function in schizophrenia. Schizophr Res. 2000;45:203–211. doi: 10.1016/s0920-9964(99)00208-x. [DOI] [PubMed] [Google Scholar]
- 41.Beck A-T, Baruch E, Balter JM, Steer RA, Warman DM. A new instrument for measuring insight: the Beck Cognitive Insight Scale. Schizophr Res. 2003;68:319–329. doi: 10.1016/S0920-9964(03)00189-0. [DOI] [PubMed] [Google Scholar]
- 42.Pedrelli P, McQuaid JR, Granholm E, et al. Measuring cognitive insight in middle-aged and older patients with psychotic disorders. Schizophr Res. 2004;71:297–305. doi: 10.1016/j.schres.2004.02.019. [DOI] [PubMed] [Google Scholar]
- 43.Amador X, Kronengold H. Understanding and assessing insight. In: Amador X, David A, editors. Insight and Psychosis. Awareness of Illness in Schizophrenia and Related Disorders. Oxford, England: University Press; 2004. [Google Scholar]
- 44.Macpherson R, Jerrom B, Hughes A. Drug refusal among schizophrenic patients treated in the community. J Ment Health. 1997;6:141–147. [Google Scholar]
- 45.Smith TE, Hull JW, Goodman M, et al. The relative influences of symptoms, insight, and neurocognition on social adjustment in schizophrenia and schizoaffective disorder. J Nerv Ment Dis. 1999;187:102–108. doi: 10.1097/00005053-199902000-00006. [DOI] [PubMed] [Google Scholar]
- 46.Coldham EL, Addington J, Addington D. Medication adherence of individuals with a first episode of psychosis. Acta Psychiatr Scand. 2002;106:286–290. doi: 10.1034/j.1600-0447.2002.02437.x. [DOI] [PubMed] [Google Scholar]
- 47.Kozuki Y, Froelicher ES. Lack of awareness and nonadherence in schizophrenia. West J Nurs Res. 2003;25:57–74. doi: 10.1177/0193945902238836. [DOI] [PubMed] [Google Scholar]
- 48.Yen C-F, Chen C-S, Ko C-H, et al. Relationships between insight and medication adherence in outpatients with schizophrenia an bipolar disorder: a prospective study. Psychiatry Clin Neurosci. 2005;59:403–409. doi: 10.1111/j.1440-1819.2005.01392.x. [DOI] [PubMed] [Google Scholar]
- 49.Watson PWP, Garety PA, Weinman J, et al. Emotional dysfunction in schizophrenia spectrum psychosis: the role of illness perceptions. Psychol Med. 2006;36:761–770. doi: 10.1017/S0033291706007458. [DOI] [PubMed] [Google Scholar]
- 50.Mutsata SH, Joyce EM, Hutton SB, et al. Clinical correlates of early medication adherence: West London first episode schizophrenia study. Acta Psychiatr Scand. 2003;108:439–446. doi: 10.1046/j.0001-690x.2003.00193.x. [DOI] [PubMed] [Google Scholar]
- 51.Donohoe G, Owens N, O'Donnell C, et al. Predictors of compliance with neuroleptic medication among inpatients with schizophrenia: a discriminant function analyses. Eur Psychiatry. 2001;16:293–298. doi: 10.1016/s0924-9338(01)00581-8. [DOI] [PubMed] [Google Scholar]
- 52.Smith CM, Barzman D, Pristach CA. Effect of patient and family insight on compliance of schizophrenic patients. J Clin Pharmacol. 1997;37:147–154. doi: 10.1002/j.1552-4604.1997.tb04773.x. [DOI] [PubMed] [Google Scholar]
- 53.Moore A, Sellwood W, Stirling J. Compliance and psychological reactance in schizophrenia. Br J Clin Psychol. 2000;39:287–295. doi: 10.1348/014466500163293. [DOI] [PubMed] [Google Scholar]
- 54.Kamali M, Kelly L, Gervin M, Browne S, Larkin C, O'Callaghan E. Insight and comorbid substance misuse and medication compliance among patients with schizophrenia. Psychiatr Serv. 2001;52:161–166. doi: 10.1176/appi.ps.52.2.161. [DOI] [PubMed] [Google Scholar]
- 55.Agarwal MR, Sharma VK, Kumar K, Lowe D. Non-compliance with treatment in patients suffering from schizophrenia: a study to evaluate possible contributing factors. Int J Soc Psychiatry. 1998;44:92–106. doi: 10.1177/002076409804400202. [DOI] [PubMed] [Google Scholar]
- 56.Garavan J, Browne S, Gervin M, Lane A, Larkin C, O'Callaghan E. Compliance with neuroleptic medication in outpatients with schizoprenia; relationship to subjective response to neuroleptics; attitudes to medication and insight. Compr Psychiatry. 1998;39:215–219. doi: 10.1016/s0010-440x(98)90063-3. [DOI] [PubMed] [Google Scholar]
- 57.Day JC, Bentall R, Roberts C, et al. Attitudes toward antipsychotic medication—the impact of clinical variables and relationships with health professionals. Arch Gen Psychiatry. 2005;62:717–724. doi: 10.1001/archpsyc.62.7.717. [DOI] [PubMed] [Google Scholar]
- 58.McEvoy JP, Freter S, Everett G, et al. Insight and the clinical outcome of schizophrenic patients. J Nerv Ment Dis. 1989;177:48–51. doi: 10.1097/00005053-198901000-00008. [DOI] [PubMed] [Google Scholar]
- 59.Buchanan A. A two-year prospective study of treatment compliance in patients with schizophrenia. Psychol Med. 1992;22:789–797. doi: 10.1017/s0033291700038228. [DOI] [PubMed] [Google Scholar]
- 60.Novak-Grubic V, Tavcar R. Predictors of noncompliance in males with first-episode schizophrenia, schizophreniform and schizoaffective disorder. Eur Psychiatry. 2002;17:148–154. doi: 10.1016/s0924-9338(02)00645-4. [DOI] [PubMed] [Google Scholar]
- 61.Tait L, Birchwood M, Trower P. Predicting engagement with services for psychosis: insight, symptoms and recovery style. Br J Psychiatry. 2003;182:123–128. doi: 10.1192/bjp.182.2.123. [DOI] [PubMed] [Google Scholar]
- 62.Byerly MJ, Fischer R, Carmody T, Rush AJ. A trial of compliance therapy in outpatients with schizophrenia or schizoaffective disorder. J Clin Psychiatry. 2005;66:997–1001. doi: 10.4088/jcp.v66n0806. [DOI] [PubMed] [Google Scholar]
- 63.Kamali M, Kelly BD, Clarke M, et al. A prospective evaluation of adherence to medication in first episode schizophrenia. Eur Psychiatry. 2006;21:29–33. doi: 10.1016/j.eurpsy.2005.05.015. [DOI] [PubMed] [Google Scholar]
- 64.Bhanji NH, Chouinard G, Margolese HC. A review of compliance, depot intramuscular antipsychotics and the new long-acting injectable atypical antipsychotic risperidone in schizophrenia. Eur Neuropsychopharmacol. 2004;14:87–92. doi: 10.1016/S0924-977X(03)00109-3. [DOI] [PubMed] [Google Scholar]
- 65.Pitschel-Walz G, Bäuml J, Bender W, Engel RR, Wagner M, Kissling W. Psychoeducation and compliance in the treatment of schizophrenia: results of the Munich Psychosis Information Project Study. J Clin Psychiatry. 2006;67:443–452. doi: 10.4088/jcp.v67n0316. [DOI] [PubMed] [Google Scholar]
- 66.Zygmund A, Olfson M, Boyer CA, Mechanic D. Interventions to improve medication adherence in schizophrenia. Am J Psychiatry. 2002;159:1653–1664. doi: 10.1176/appi.ajp.159.10.1653. [DOI] [PubMed] [Google Scholar]
- 67.Ziguras SJ, Stuart GW. A meta-analysis of the effectiveness of mental health case management over 20 years. Psychiatr Serv. 2000;51:1410–1421. doi: 10.1176/appi.ps.51.11.1410. [DOI] [PubMed] [Google Scholar]
- 68.Jørgensen P. Recovery and insight in schizophrenia. Acta Psychiatr Scand. 1995;92:436–440. doi: 10.1111/j.1600-0447.1995.tb09609.x. [DOI] [PubMed] [Google Scholar]
- 69.Weiler MA, Fleisher MH, McArthur-Campbell D. Insight and symptom change in schizophrenia and other disorders. Schizophr Res. 2000;45:29–36. doi: 10.1016/s0920-9964(99)00215-7. [DOI] [PubMed] [Google Scholar]
- 70.Michalakes A, Skoutas C, Charalambous A, et al. Insight in schizophrenia and mood disorders and its relation to psychopathology. Acta Psychiatr Scand. 1994;90:46–49. doi: 10.1111/j.1600-0447.1994.tb01554.x. [DOI] [PubMed] [Google Scholar]
- 71.Mintz AR, Dobson KS, Romney DM. Insight in schizophrenia: a meta-analysis. Schizophr Res. 2003;61:75–88. doi: 10.1016/s0920-9964(02)00316-x. [DOI] [PubMed] [Google Scholar]
- 72.McEvoy JP, Freter S, Merritt M, Apperson LJ. Insight about psychosis among outpatients with schizophrenia. Hosp Community Psychiatry. 1993;44:883–884. doi: 10.1176/ps.44.9.883. [DOI] [PubMed] [Google Scholar]
- 73.Smith TE, Hull JW, Santos L. The relationship between symptoms and insight in schizophrenia: a longitudinal perspective. Schizophr Res. 1998;33:63–67. doi: 10.1016/s0920-9964(98)00063-2. [DOI] [PubMed] [Google Scholar]
- 74.Chen EY-H. Insight and symptoms of psychosis: a prospective inpatient study. Schizophr Res. 1998;29:34. [Google Scholar]
- 75.Carroll A, Fattah S, Clyde Z, Coffey I, Owens DGC, Johnstone EC. Correlates of insight and insight change in schizophrenia. Schizophr Res. 1999;35:247–253. doi: 10.1016/s0920-9964(98)00142-x. [DOI] [PubMed] [Google Scholar]
- 76.Yen C-F, Yeh M-L, Chen C-S, Chung H-H. Predictive value of insight for suicide, violence, hospitalization, and social adjustment for outpatients with schizophrenia: a prospective study. Compr Psychiatry. 2002;43:443–447. doi: 10.1053/comp.2002.35901. [DOI] [PubMed] [Google Scholar]
- 77.Mintz AR, Addington J, Addington D. Insight in early psychosis: a 1-year follow-up. Schizophr Res. 2004;67:213–217. doi: 10.1016/S0920-9964(03)00047-1. [DOI] [PubMed] [Google Scholar]
- 78.Simon AE, Berger GE, Giacomini V, Ferrero F, Mohr S. Insight in relation to psychosocial adjustment in schizophrenia. J Nerv Ment Dis. 2004;192:442–445. doi: 10.1097/01.nmd.0000130137.85640.70. [DOI] [PubMed] [Google Scholar]
- 79.Schwartz RC, Cohen BN, Grubaugh A. Does insight affect long-term inpatient treatment outcome in chronic schizophrenia? Compr Psychiatry. 1997;38:283–288. doi: 10.1016/s0010-440x(97)90061-4. [DOI] [PubMed] [Google Scholar]
- 80.McGlashan TH, Carpenter WT. Does attitude toward psychosis relate to outcome? Am J Psychiatry. 1981;150:1649–1653. doi: 10.1176/ajp.138.6.797. [DOI] [PubMed] [Google Scholar]
- 81.Amador XF, Flaum MM, Andreasen NC, et al. Awareness of illness in schizophrenia and schizoaffective and mood disorders. Arch Gen Psychiatry. 1994;51:826–836. doi: 10.1001/archpsyc.1994.03950100074007. [DOI] [PubMed] [Google Scholar]
- 82.Rossi A, Arduini L, Prosperini P, Kalyvoka A, Stratta P, Daneluzzo E. Awareness of illness and outcome in schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2000;250:73–75. doi: 10.1007/s004060070037. [DOI] [PubMed] [Google Scholar]
- 83.Chen KC, Chu CL, Yang YK, et al. The relationship among insight, cognitive function of patients with schizophrenia and their relatives' perception. Psychiatry Clin Neurosci. 2005;59:657–660. doi: 10.1111/j.1440-1819.2005.01433.x. [DOI] [PubMed] [Google Scholar]
- 84.Lysaker P, Bell M. Work rehabilitation and improvements in insight in schizophrenia. J Nerv Ment Dis. 1995;183:103–106. doi: 10.1097/00005053-199502000-00007. [DOI] [PubMed] [Google Scholar]
- 85.Schwartz RC. Self-awareness in schizophrenia: its relationship to depressive symptomatology and broad psychiatric impairments. J Nerv Ment Dis. 2001;189:401–403. doi: 10.1097/00005053-200106000-00010. [DOI] [PubMed] [Google Scholar]
- 86.White R, Bebbington P, Pearson J, Johnson S, Ellis D. The social context of insight in schizophrenia. Soc Psychiatry Psychiatr Epidemiol. 2000;35:500–507. doi: 10.1007/s001270050271. [DOI] [PubMed] [Google Scholar]
- 87.Baier M, DeShay E, Owens K, et al. The relationship between insight and clinical factors for persons with schizophrenia. Arch Psychiatr Nurs. 2000;14:259–265. doi: 10.1053/apnu.2000.19088. [DOI] [PubMed] [Google Scholar]
- 88.Cuesta MJ, Peralta V. Lack of insight in schizophrenia. Schizophr Bull. 1994;20:359–366. doi: 10.1093/schbul/20.2.359. [DOI] [PubMed] [Google Scholar]
- 89.Lysaker P, Bell M, Milstein R, Bryson G, Beam-Goulet J. Insight and psychosocial treatment compliance in schizophrenia. Psychiatry. 1994;57:307–315. doi: 10.1080/00332747.1994.11024695. [DOI] [PubMed] [Google Scholar]
- 90.Arango C, Bombín I, González-Salvador T, García-Cabeza I, Bobes J. Randomised clinical trial comparing oral versus depot formulations of zuclopenthixol in patients with schizophrenia and previous violence. Eur Psychiatry. 2006;21:34–40. doi: 10.1016/j.eurpsy.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 91.Arango C, Barba AC, González-Salvador T, Ordóñez AC. Violence in inpatients with schizophrenia: a prospective study. Schizophr Bull. 1999;25:493–503. doi: 10.1093/oxfordjournals.schbul.a033396. [DOI] [PubMed] [Google Scholar]
- 92.Buckley PF, Hrouda DR, Freeman L, Noffsinger SG, Resnick PJ, Camlin-Shinger MSSA. Insight and its relationship to violent behavior in patients with schizophrenia. Am J Psychiatry. 2004;161:1712–1714. doi: 10.1176/appi.ajp.161.9.1712. [DOI] [PubMed] [Google Scholar]
- 93.Strand S, Belfrage H, Fransson G, Levander S. Clinical and risk management factors in risk prediction of mentally disordered offenders-more important than historical data? Legal Criminol Psychol. 1999;4:67–76. [Google Scholar]
- 94.Grevatt A, Thomas-Peter B, Hughes G. Violence, mental disorder and risk assessment: can structured clinical assessments predict the short-term risk of inpatient violence? J Forensic Psychiatry Psychol. 2004;15:278–292. [Google Scholar]
- 95.Foley S, Kelly BD, Clarke M, et al. Incidence and clinical correlates of aggression and violence at presentation in patients with first episode psychosis. Schizophr Res. 2005;72:161–168. doi: 10.1016/j.schres.2004.03.010. [DOI] [PubMed] [Google Scholar]
- 96.Cheung P, Schweitzer I, Crowley K, Tuckwell V. Violence in schizophrenia: role of hallucinations and delusions. Schizophr Res. 1997;26:181–190. doi: 10.1016/s0920-9964(97)00049-2. [DOI] [PubMed] [Google Scholar]
- 97.Swartz MS, Swanson JW, Hiday VA, Borum R, Wagner R, Burns BJ. Violence and severe mental illness: the effects of substance abuse and nonadherence to medication. Am J Psychiatry. 1998;155:226–231. doi: 10.1176/ajp.155.2.226. [DOI] [PubMed] [Google Scholar]
- 98.Carroll A, Pantelis C, Harvey C. Insight and hopelessness in forensic patients with schizophrenia. Aust N Z J Psychiatry. 2004;38:169–173. doi: 10.1080/j.1440-1614.2004.01315.x. [DOI] [PubMed] [Google Scholar]
- 99.Sim K, Mahendran R, Siris SG, Heckers S, Chong SA. Subjective quality of life in first episode schizophrenia spectrum disorders with comorbid depression. Psychiatry Res. 2004;129:141–147. doi: 10.1016/j.psychres.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 100.Schwartz RC, Smith SD. Suicidality and psychosis: the predictive potential of symptomatology and insight into illness. J Psychiatr Res. 2004;38:185–191. doi: 10.1016/s0022-3956(03)00088-8. [DOI] [PubMed] [Google Scholar]
- 101.Amador XF, Friedman JH, Kasapis C, Yale SA, Flaum M, Gorman JM. Suicidal behaviour in schizophrenia and its relationship to awareness of illness. Am J Psychiatry. 1996;153:1185–1188. doi: 10.1176/ajp.153.9.1185. [DOI] [PubMed] [Google Scholar]
- 102.Schwartz RC, Petersen S. The relationship between insight and suicidality among patients with schizophrenia. J Nerv Ment Dis. 1999;187:376–378. doi: 10.1097/00005053-199906000-00007. [DOI] [PubMed] [Google Scholar]
- 103.Schwartz RC. Insight and suicidality in schizophrenia: a replication study. J Nerv Ment Dis. 2000;188:235–237. doi: 10.1097/00005053-200004000-00007. [DOI] [PubMed] [Google Scholar]
- 104.Evren C, Evren B. Characteristics of schizophrenic patients with a history of suicide attempt. Int J Psychiatry Clin Pract. 2004;8:227–234. doi: 10.1080/13651500410005658-1. [DOI] [PubMed] [Google Scholar]
- 105.Kim C-H, Jayathilake K, Meltzer HY. Hopelessness, neurocognitive function. insight in schizophrenia: relationship to suicidal behavior. Schizophr Res. 2003;60:71–80. doi: 10.1016/s0920-9964(02)00310-9. [DOI] [PubMed] [Google Scholar]
- 106.Crumlish N, Whitty P, Kamali M, et al. Early insight predicts depression and attempted suicide after 4 years in first-episode schizophrenia and schizophreniform disorder. Acta Psychiatr Scand. 2005;112:449–455. doi: 10.1111/j.1600-0447.2005.00620.x. [DOI] [PubMed] [Google Scholar]
- 107.Drake RJ, Pickles A, Bentall RP, et al. The evolution of insight, paranoia and depression during early schizophrenia. Psychol Med. 2004;34:285–292. doi: 10.1017/s0033291703008821. [DOI] [PubMed] [Google Scholar]
- 108.Smith TE, Hull JW, Huppert JD, Silverstein SM, Anthony DT, McClough J. Insight and recovery from psychosis in chronic schizophrenia and schizoaffective disorder patients. J Psychiatr Res. 2004;38:169–176. doi: 10.1016/s0022-3956(03)00091-8. [DOI] [PubMed] [Google Scholar]
- 109.Iqbal Z, Birchwood M, Chadwick P, Trower P. Cognitive approach to depression and suicidal thinking in psychosis—2. Testing the validity of a social ranking model. Br J Psychiatry. 2000;177:522–528. [PubMed] [Google Scholar]
- 110.Bourgeois M, Swendsen J, Young F, et al. Awareness of disorder and suicide risk in the treatment of schizophrenia: results of the international suicide prevention trial. Am J Psychiatry. 2004;161:1494–1496. doi: 10.1176/appi.ajp.161.8.1494. [DOI] [PubMed] [Google Scholar]
- 111.Moore O, Cassidy E, Carr A, Callaghan EO. Unawareness of illness and its relationship with depression and self-deception in schizophrenia. Eur J Psychiatry. 1999;14:264–269. doi: 10.1016/s0924-9338(99)00172-8. [DOI] [PubMed] [Google Scholar]
- 112.Pini S, Cassano GB, Dell'Osso L, Amador X. Insight into illness in schizophrenia, schizoaffective disorder, and mood disorders with psychotic features. Am J Psychiatry. 2001;158:122–125. doi: 10.1176/appi.ajp.158.1.122. [DOI] [PubMed] [Google Scholar]
- 113.Bellack AS. Scientific and consumer models of recovery in schizophrenia: concordance, contrasts, and implications. Schizophr Bull. 2006;32:423–442. doi: 10.1093/schbul/sbj044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Lysaker P, Campbell K, Johannesen JK. Hope, awareness of Illness. coping in schizophrenia spectrum disorders—evidence of an interaction. J Nerv Ment Dis. 2005;193:287–292. doi: 10.1097/01.nmd.0000161689.96931.0f. [DOI] [PubMed] [Google Scholar]
- 115.Fowler D, Garety P, Kuipers E. Cognitive Behaviour Therapy for Psychosis. Theory and Practice. Wiley Series in Clinical Psychology. Chichester, England: Wiley; 1995. [Google Scholar]