Abstract
We developed and tested the validity of a brief scale to assess everyday functioning in persons with serious mental illness. A sample of 434 adults with schizophrenia or schizoaffective disorder were administered the University of California, San Diego, Performance-Based Skills Assessment (UPSA), which assesses functional skills in 5 areas of life functioning (eg, finances and planning). Through use of factor analysis, we developed the UPSA-Brief, which consists of 2 subscales (communication and financial) from the original UPSA. UPSA-Brief scores were correlated with cognitive functioning, symptoms of psychosis, age, and education. We further tested the sensitivity and specificity of the UPSA-Brief for predicting residential independence using receiver-operating characteristic (ROC) curves. Finally, sensitivity to change was assessed through comparison of 2 interventions for improving UPSA-Brief scores. UPSA-Brief scores were highly correlated with scores on the full version of the UPSA (r = .91), with overall cognitive functioning (r = .57), and with negative symptoms (r = −.32). The discriminant validity of the UPSA-Brief was adequate (ROC area under the curve [AUC] = 0.73; 95% confidence interval [CI]: 0.67–0.78), with greatest dichotomization for the UPSA-Brief at a cutoff score of 60. The UPSA-Brief was significantly better than the Dementia Rating Scale, Positive and Negative Syndromes Scale positive, and Positive and Negative Syndromes Scale negative at predicting residential independence (all P values < .05). Participants receiving a behavioral intervention also improved significantly compared with a support condition (P = .023). The UPSA-Brief has adequate psychometric properties, predicts residential independence, is sensitive to change, and requires only 10–15 minutes to administer. Therefore, the UPSA-Brief may be a useful performance-based functional outcome scale.
Keywords: functional capacity, schizophrenia, independence, psychotherapy
Introduction
Persons with schizophrenia are noted to have significant deficits in numerous areas of life functioning including independent living, employment, and interpersonal skills.1–4 Investigators comparing various approaches to measuring functioning in patients with schizophrenia have concluded that performance-based measures are generally superior to self-report and reports of other informants.5–8 Until recently, a single performance-based measure capable of measuring overall functioning in these multiple domains has been lacking. The University of California, San Diego (UCSD), Performance-Based Skills Assessment (UPSA) was developed in 2001 to address the need for an instrument that assesses the capacity of persons with schizophrenia to adequately perform skills necessary for daily functioning.9 Specifically, the UPSA consists of 5 subscales which assess a person's ability to comprehend and plan for the future (eg, planning an outing to the beach), manage finances (eg, count correct change, write a check to pay a bill), communicate with others (eg, dial an emergency telephone number, reschedule a medical appointment), utilize transportation (ie, read a bus schedule, use public transportation), and shop (eg, create or follow a shopping list). Since its development, the UPSA has been translated into over 20 languages and is utilized in over 22 countries worldwide. Further, the UPSA has demonstrated high correlations with measures of neurocognitive functioning, personal care skills, interpersonal skills, and community activities.1,10 Similarly, other studies have shown UPSA performance to be correlated with level of independence in living.10,11 Specifically, Mausbach et al11 found scores of 75 or above on the UPSA to be predictive of one's ability to live independently in the community.
While the full version of the UPSA takes approximately 30 minutes to administer, development of a brief version could allow for a more expedient assessment of patient functioning which could then be used to assess improvement related to treatment interventions as well as facilitate discharge planning (eg, discharge to independent or supervised care setting). The purpose of the present study is to present initial validation of a brief version of the UPSA (ie, UPSA-Brief). To achieve this aim, we present results from 2 studies. The first study consisted of 434 community-residing patients diagnosed with either schizophrenia or schizoaffective disorder. The purpose of this study was to identify subscales for the UPSA-Brief and establish its initial concurrent validity by demonstrating its relationship with other measures of functioning in patients diagnosed with schizophrenia (eg, neurocognitive functioning, symptoms of psychosis, residential independence). We further sought to establish the sensitivity of the UPSA-Brief to change via interventions. To establish this, we utilized a subset (n = 240) of our overall 434 patients who participated in a randomized clinical trial examining the efficacy of a psychosocial intervention designed to improve everyday living skills of middle-aged and older outpatients with chronic psychotic disorders.
Methods
Participants
Participants for this study consisted of 434 individuals diagnosed with either schizophrenia or schizoaffective disorder. All subjects were ongoing research participants at the UCSD Advanced Center for Interventions and Services Research, which examines, among other aspects, functional abilities of these patients. Diagnosis of schizophrenia-related disorders was established by Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV)–based chart diagnosis using the patients’ research charts. All participants volunteered and provided written, informed consent to participate in research studies.
A subset of these 434 participants also enrolled in a randomized trial examining the efficacy of a psychosocial intervention for improving scores on the full UPSA.12 Specifically, of the 434 participants, 240 were part of this intervention trial. To be eligible for this intervention trial, participants were required to be 40 years of age or older and have a DSM-IV–based chart diagnosis of schizophrenia or schizoaffective disorder. Participants were excluded if they had a DSM-IV diagnosis of dementia, represented a serious suicide risk, could not complete the assessment battery, or were participating in any other psychosocial intervention or drug research at the time of intake. More details on the sample and recruitment can be found in Patterson et al.12
Measures
The criterion measures used to assess the construct validity of the UPSA-Brief included the full UCSD UPSA,9 the Mattis Dementia Rating Scale (DRS),13 and the Positive and Negative Syndromes Scale (PANSS).14 As discussed above, the UPSA consists of 5 subscales assessing a variety of everyday functional skills including planning recreational activities, household chores, communication, transportation, and finance. Previous reports indicate that the interrater reliability of the UPSA is excellent.9 The DRS is used to assess overall cognitive functioning; there are 5 subscales in the DRS: (1) attention, (2) initiation, (3) memory, (4) conceptualization, and (5) construction. The PANSS assesses severity of psychotic symptoms and has subscales for both positive and negative symptoms.
Consistent with our prior article,11 residential independence was defined as living alone in an apartment, house, or single-resident occupancy (eg, hotel room). Participants who resided in a care facility (eg, Board and Care home, Skilled Nursing Facility) were classified as nonindependent. Participants who resided with a roommate (eg, spouse, family member) were not included in this study because we were not able to assess the level of assistance these roommates offered to the patient.
Statistical Analysis
All data analyses were conducted using available data from previous or ongoing research studies at UCSD. We have previously published data for these participants for full UPSA scores11 and intervention outcomes,12 but not for the UPSA-Brief. A receiver-operating characteristic (ROC) curve was plotted to determine whether the UPSA-Brief adequately predicted residential independence (ie, patients who were living alone in an apartment or house or in an assisted living environment such as a Board and Care). To compare the AUCs for the UPSA-Brief and the full version of the UPSA, we used the methods described by Hanley and McNeil.15,16
Repeated measures analysis of covariance was used to determine if participation in the Functional Adaptations and Skills Training (FAST) intervention was more effective than the support condition for improving UPSA-Brief scores. All the participants were tested at baseline and immediately following completion of the 6-month intervention. Our group variable had 2 levels (ie, FAST vs Support). Six-month scores on the UPSA-Brief served as our dependent variable, and in order to control for participant skill level at study entry, we covaried for baseline UPSA-Brief performance. Further, because age and education are associated with functional outcome measures, these variables were entered as covariates in our model. Alpha was set at .05.
Results
Sample Characteristics
Characteristics of the sample can be found in table 1. The average age for participants was 50 years (range = 26–77), and most participants were Caucasian (66%) and had at least a high school education (74%).
Table 1.
Characteristics of the sample by independence status
| Characteristic | Independent (n = 99) | Nonindependent (n = 335) | df | t, χ2 | P Value |
| Age (y), mean (SD) | 50.6 (9.4) | 50.2 (7.5) | 432 | 0.47 | .658 |
| Gender (male), n (%) | 69 (70) | 220 (66) | 1 | 0.56 | .456 |
| Race/ethnicity, n (%) | |||||
| Caucasian | 54 (55) | 234 (70) | 4 | 10.07 | .039 |
| African American | 21 (21) | 41 (12) | |||
| Hispanic | 14 (14) | 31 (9) | |||
| Asian | 6 (6) | 12 (4) | |||
| Other | 4 (4) | 17 (5) | |||
| Education level, n (%) | |||||
| Less than high school graduate | 16 (16) | 98 (29) | 2 | 9.50 | .007 |
| High School | 34 (34) | 121 (36) | |||
| Some college and above | 49 (50) | 116 (35) | |||
| UPSA-Full, mean (SD) | 78.4 (15.3) | 63.0 (20.3) | 430 | 7.00 | <.001 |
| UPSA-Brief, mean (SD) | 72.5 (18.8) | 54.5 (22.9) | 432 | 7.12 | <.001 |
| DRS total, mean (SD) | 132.0 (10.0) | 126.0 (15.3) | 356 | 3.17 | .002 |
| DRS attention, mean (SD) | 35.3 (1.6) | 34.2 (3.2) | 356 | 2.81 | .005 |
| DRS memory, mean (SD) | 22.4 (3.1) | 20.7 (3.5) | 356 | 3.88 | <.001 |
| DRS initiation, mean (SD) | 33.4 (4.4) | 31.6 (6.1) | 356 | 2.36 | .019 |
| DRS conceptualization, mean (SD) | 35.5 (3.7) | 34.1 (4.9) | 356 | 2.29 | .023 |
| DRS construction, mean (SD) | 5.4 (1.2) | 5.4 (3.6) | 356 | −0.02 | .980 |
| PANSS positive, mean (SD) | 15.6 (6.2) | 14.4 (5.8) | 426 | 1.70 | .089 |
| PANSS Negative, mean (SD) | 13.8 (4.2) | 14.9 (5.4) | 424 | −1.80 | .073 |
Note: UPSA, University of California, San Diego, Performance-Based Skills Assessment; DRS, Dementia Rating Scale; PANSS, Positive and Negative Syndromes Scale.
Identification of Candidate Subscales
A factor analysis of the full UPSA was conducted to identify candidate subscales for the UPSA-Brief. Results of this factor analysis indicated all 5 subscales loaded on a single factor, accounting for 60% of the variance in the observed data. Following methods similar to those of previous reports17,18, we created the UPSA-Brief from the 2 subscales that loaded most heavily on this factor, namely the finance (factor loading = .85) and communication (factor loading = .80) subscales. All items on the finance and communication subscales were retained for the UPSA-Brief. To be consistent with the scoring method used on the full UPSA, we readjusted the finance and communication subscale scores for the UPSA-Brief by converting each to reflect a range of 0–50. This was done by multiplying the percentage of items correct on each of these 2 subscales by a value of 50. Adding these 2 subscale scores therefore yielded a total UPSA-Brief score also between 0 and 100.
Construct Validity of the UPSA-Brief
Of the 434 participants who completed the UPSA, DRS data were available for 359, PANSS positive for 427 participants, and PANSS positive data were available for 429 individuals. Intercorrelations between measures are described in table 2. As can be seen, the UPSA-Brief was significantly correlated with the full 5-scale UPSA (r = .91). Because the UPSA-Brief consists of 2 subscales found on the full UPSA, we also conducted correlations between the remaining 3 UPSA subscales and the UPSA-Brief. Results indicated that the UPSA-Brief was correlated at .74 with the 3 remaining subscales (ie, planning recreational activities, transportation, and household chores).
Table 2.
Intercorrelations Among Study Measures
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
| 1. UPSA-Full | ||||||||||||
| 2. UPSA-3 | .95** (n = 434) | |||||||||||
| 3. UPSA-Brief | .91** (n = 434) | .74** (n = 434) | ||||||||||
| 4. DRS total | .63** (n = 356) | .59** (n = 357) | .57** (n = 358) | |||||||||
| 5. DRS attention | .45** (n = 356) | .41** (n = 357) | .42** (n = 358) | .70** (n = 359) | ||||||||
| 6. DRS memory | .62** (n = 356) | .58** (n = 357) | .57** (n = 358) | .77** (n = 359) | .50** (n = 359) | |||||||
| 7. DRS initiation | .50** (n = 356) | .48** (n = 357) | .44** (n = 358) | .81** (n = 359) | .44** (n = 359) | .51** (n = 359) | ||||||
| 8. DRS conceptualization | .50** (n = 356) | .47** (n = 357) | .46** (n = 358) | .81** (n = 359) | .54** (n = 359) | .59** (n = 359) | .51** (n = 359) | |||||
| 9. DRS construction | .14* (n = 356) | .13* (n = 357) | .12* (n = 358) | .40** (n = 359) | .10* (n = 359) | .17** (n = 359) | .16** (n = 359) | .17** (n = 359) | ||||
| 10. PANSS positive | −.09 (n = 427) | −.08 (n = 428) | −.09 (n = 429) | −.10 (n = 358) | −.05 (n = 358) | −.11* (n = 358) | −.12* (n = 358) | −.04 (n = 358) | −.01 (n = 358) | |||
| 11. PANSS negative | −.32** (n = 425) | −.28** (n = 426) | −.32** (n = 427) | −.31** (n = 358) | −.18** (n = 358) | −.21** (n = 358) | −.35** (n = 358) | −.19** (n = 358) | −.09 (n = 358) | .25** (n = 431) | ||
| 12. Age | −.18** (n = 433) | −.20** (n = 434) | −.12* (n = 435) | −.16** (n = 359) | −.05 (n = 359) | −.13* (n = 359) | −.19** (n = 359) | −.10 (n = 359) | −.07 (n = 359) | −.07 (n = 432) | .08 (n = 430) | |
| 13. Education | .26** (n = 434) | .24** (n = 435) | .24** (n = 436) | .22** (n = 359) | .07 (n = 359) | .13* (n = 359) | .18** (n = 359) | .18** (n = 359) | .20** (n = 359) | −.06 (n = 433) | −.01 (n = 439) | −.01 (n = 439) |
Note: UPSA-Full, full version of the UPSA; UPSA-3, transportation, planning recreational activities, and household chores subscales; DRS, Dementia Rating Scale; PANSS, Positive and Negative Syndromes Scale.
*p < .05
**p < .01
Correlations between the UPSA-Brief and each of the 5 subscales of the DRS were all significant (range = .12 for construction to .57 for memory), as was the correlation between the UPSA-Brief and overall cognitive functioning (r = .57). Whereas negative symptoms were significantly correlated with the UPSA-Brief (r = −.32), positive symptoms were not (P > .05). As expected, younger participants and those with more education performed better on the UPSA-Brief. Correlations between these constructs and UPSA-Brief scores were highly similar to those of the full UPSA.
Usefulness of the UPSA-Brief for Predicting Residential Independence
An ROC curve was plotted for the UPSA-Brief. The ROC curve shows the sensitivity vs 1 minus the specificity for every possible cutoff point; optimal cutoff points are determined by visually assessing which score combines maximum sensitivity and specificity. The AUC with 95% CIs was used as an indicator of the ability of the UPSA-Brief to differentiate patients who were living independently in the community (eg, living alone in an apartment) or not living independently (eg, living in a Board and Care facility). In addition, we used the methods described by Hanley and McNeil15,16 to compare the AUCs for the full UPSA and the UPSA-Brief for predicting residential independence.
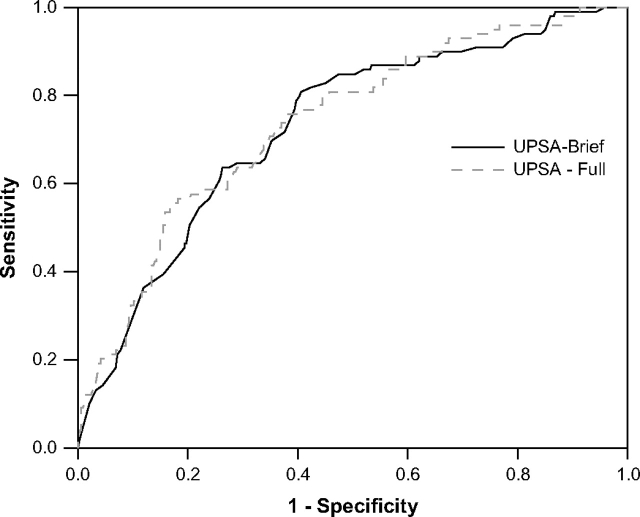
Ninety-nine of the 434 participants (23%) were residentially independent at the time of testing. Table 3 indicates the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and percent correctly identified as residentially independent for different cutoff scores on the UPSA. As discussed in our previous article, sensitivity and specificity refer to how well the UPSA-Brief correctly identified people who were residing independently and nonindependently, respectively.11 PPV refers to the percentage of patients with positive test results who are correctly classified as independent, whereas NPV refers to the percentage of patients with negative test results who are correctly classified as dependent.19 The ROC curves for the UPSA and UPSA-Brief are shown in figure 1. The estimated AUC for the UPSA was 0.74 (95% CI: 0.68–0.79), whereas the estimated AUC for the UPSA-Brief was 0.73 (95% CI: 0.67–0.78). Both scales were significantly greater (P < .001) than the area of no information (an area of 0.50), and they were not significantly different from each other (z = 0.66, P = .255).
Table 3.
Sensitivity, Specificity, Positive Predictive Value (PPV), Negative Predictive Value (NPV), and Percent Subjects Correctly Identified as Residentially Independent With UPSA-Brief Cutoffs
| Cutoff | 40 | 50 | 60* | 70 | 80 |
| Sensitivity | 0.91 | 0.87 | 0.82 | 0.65 | 0.37 |
| Specificity | 0.27 | 0.44 | 0.58 | 0.71 | 0.87 |
| PPV | 0.27 | 0.32 | 0.36 | 0.40 | 0.46 |
| NPV | 0.91 | 0.92 | 0.91 | 0.87 | 0.82 |
| % Correctly Identified | 59 | 66 | 70 | 68 | 62 |
Note: *Maximum Sensitivity and Specificity
Fig. 1.
Receiver-operating characteristic analysis of comparison: prediction of residential independence. The UPSA-Brief and UPSA area under the curve estimates were 0.73 (95% confidence interval [CI]: 0.67–0.78) and 0.74 (95% CI: 0.68–0.79), respectively. UPSA = University of California, San Diego, Performance-Based Skills Assessment.
We also compared the UPSA-Brief area under the curve for predicting residential independence with that of the DRS total score and both positive and negative symptoms of the PANSS. The estimated AUC for DRS total scores was 0.65 (95% CI: 0.58–0.73). Using the estimate of average correlation provided by Hanley and McNeil,16 we compared the AUCs for the UPSA-Brief and DRS for the 358 participants who had data available on both tests. The UPSA-Brief AUC estimate of 0.73 (95% CI: 0.67–0.80) was significantly greater than that of the DRS described above (z = 2.39, P = .017). Comparison of the UPSA-Brief to PANSS negative (z = 3.88, P < .001) and PANSS positive scores (z = 5.48, P < .001) were also significant in favor of the UPSA-Brief.
As seen in table 3, the best UPSA-Brief cutoff score was 60. At this cutoff, the UPSA-Brief correctly identified 70% of the residentially independent sample. The sensitivity of 0.82 was greater than the specificity of 0.58.
Sensitivity of the UPSA-Brief to Change
All participants completed a baseline UPSA-Brief assessment and were randomly assigned to 1 of 2 manualized group-based interventions. The first, called FAST (n = 124), was a behavioral intervention based on social cognitive theory.20 This intervention consisted of 24 weekly sessions (120 minutes each) and taught participants a variety of everyday functional skills. The second intervention was a time-equivalent support condition (Support; n = 116) whereby patients were offered opportunity to address personal issues and receive support and advice from other group participants. More details on these interventions can be found elsewhere.12,21
Linear Change on the UPSA-Brief
Mean baseline scores ± standard error for the FAST and Support conditions were 51.4 ± 2.1 and 56.6 ± 2.1, respectively (t = 1.71, df = 238, P = .088). A total of 194 participants (101 FAST and 93 Support) completed both a baseline and follow-up UPSA-Brief. After controlling for baseline UPSA scores, age, and education, patients in the FAST group had significantly higher postintervention (6-month) UPSA-Brief scores than Support participants (F = 5.24, df = 1, 189, P = .023; Cohen's d = 0.33). Estimated mean follow-up scores for the FAST participants were 61.5 ± 1.5 compared with 56.5 ± 1.6 for Support participants.
“Prognostic” Categorization Change—Likelihood of Residential Independence
In addition to linear change on the UPSA-Brief, we determined whether participation in the FAST psychosocial intervention was superior to a control condition for moving participants above our cutoff score of 60 on the UPSA-Brief, thereby indicating greater likelihood of living independently. We assigned participants to a “residential prognosis” category (ie, “low” vs “high”) for both baseline and 6-month follow-up assessments. Then, we classified participants as having either a “successful” or “unsuccessful” treatment response based on the following definitions: (1) unsuccessful = patient stayed <60 from baseline to follow-up or moved from ≥60 on the UPSA-Brief to <60 at follow-up or (2) successful = patient moved from <60 on the UPSA-Brief to ≥60 at follow-up. These criteria resulted in a subgroup of 128 participants, with the remaining participants scoring ≥60 at both baseline and 6-month follow-up. A chi-square analysis was used to compare intervention differences in these categorizations. Results of this analysis indicated a significant difference between FAST and Support interventions (χ2 = 4.62, df = 1, P = .032), with those in the FAST intervention significantly more likely to be classified as a “success”. The percentage of participants in these categories is presented in table 4.
Table 4.
Summary of Pearson Chi-Square Test for Success of Treatment Groups for Moving Patients Toward Likelihood of Residential Independence
| Group | Unsuccessful | Successful | Odds of Treatment Failure |
| FAST, n (%) | 44 (65) | 24 (35) | 1.86 |
| Support, n (%) | 49 (82) | 11 (18) | 4.56 |
Note: Unsuccessful = patient stayed <60 on UPSA-Brief from baseline to 6-month follow-up or moved from ≥60 to <60; successful = patient moved from < 60 to ≥ 60; χ2 = 4.62, df = 1, P = .032; odds ratio = 2.45; number needed to treat = 5.88; FAST = Functional Adaptations and Skills Training.
Calculation of Treatment Effect Size Estimates
In order to provide investigators with information on the magnitude of the intervention effect (ie, the FAST treatment vs the Support condition) on UPSA-Brief scores, we utilized the data from table 4 to compute effect size estimates. These estimates included Cohen's d,22 the odds ratio (OR), and number needed to treat (NNT). These latter 2 effect size estimates are recommended by Kraemer et al.23 Cohen's d reflects mean differences between treatment groups in standard deviation units, with estimates of 0.2, 0.5, and 0.8 indicating small, medium, and large effects, respectively.22 However, it should be noted that interpretation of Cohen's d effect sizes should be made within the context of the construct being measured, whereby in some contexts effect sizes less than 0.8 might be considered large.23 OR refers to the odds of a successful response in the FAST condition compared with the Support condition. NNT is the number of patients who must be treated in order to generate one more success than would have been expected had all persons been given the Support condition. In the present study, Cohen's d was estimated as approximately 0.30. The OR was 2.45, indicating that FAST participants were over twice as likely to have a successful treatment response than Support participants. NNT was 5.88, indicating that 1 patient out of 6 would reach a threshold of 60 on the UPSA-Brief as a function of being in the FAST intervention.
Discussion
Persons with schizophrenia are noted to have significant deficits in numerous areas of life functioning which may inhibit their ability to adapt to the demands of society. These deficits thereby necessitate the development of treatments that improve functioning along with coinciding measures that adequately gauge one's ability to function in his/her environment. Ideally, these measures should be brief, reliable, and demonstrate both internal and external validity. This study provides initial validation of the UPSA-Brief, a measure designed to provide fast assessment of overall functioning in patients with schizophrenia and other chronic psychoses. Our major findings are (1) the UPSA-Brief is highly correlated with other major areas of functioning including cognitive functioning and negative symptoms of psychosis and, as expected, is sensitive to age and education levels of those being assessed, (2) the UPSA-Brief can accurately predict patient ability to live independently, even when compared with the full version of the UPSA, the DRS, and the PANSS, and (3) scores on the UPSA-Brief are sensitive to change via psychosocial interventions.
There are several advantages for developing a brief version of the UPSA. First, whereas the full version of the UPSA can be administered in approximately 30 minutes, the UPSA-Brief can be administered in approximately 10–15 minutes. This is advantageous from both a patient and administrator perspective. For example, some patients with schizophrenia may not be capable of completing the full UPSA in conjunction with other psychosocial and medical assessments due to attentional difficulties, and utilization of the UPSA-Brief would minimize this limitation. An additional feature of the UPSA-Brief is that subscales from the full UPSA that require a maximum number of props (such as a pantry and maps) are not included on the UPSA Brief, making its portability across cites even greater than that for the full UPSA.
Clinicians and researchers also benefit from the brevity of the UPSA-Brief by allowing them to maximize resources for assessment of other functional areas. For example, the UPSA-Brief allows researchers and clinicians to maximize resources without sacrificing validity and accuracy. Specifically, we find that the UPSA-Brief is highly correlated with global measures of neuropsychological performance as well as specific neuropsychological constructs including memory, attention, initiation, and conceptualization. Further, we demonstrated that the UPSA-Brief is significantly better than a global measure of cognitive functioning (ie, the DRS) and both positive and negative symptoms of psychosis for predicting residential independence, while maintaining a level of accuracy consistent with that of the full UPSA. This allows clinicians to utilize the UPSA-Brief, in conjunction with other measures, as one means of discharge planning from hospital settings.
Another advantage to this study was our demonstration that the UPSA-Brief is sensitive to change via psychosocial interventions. Based on results from our study, clinicians and researchers may utilize either raw UPSA-Brief scores or a cutoff of 60 to establish treatment success. Specifically, treatment personnel (eg, physicians, nurses, etc.) may use raw scores to determine change in functioning over the course of medical treatments or set a score of 60 or above on the UPSA-Brief as a treatment goal for discharge planning. Indeed, other indicators of treatment success, such as assignment of Global Assessment of Functioning scores,24 appear notably weak at predicting outcomes in patients with chronic psychosis.25,26 Therefore, use of a new outcome appears warranted.
Similarly, the sensitivity of the UPSA-Brief to change via psychosocial interventions is important as it demonstrates that these interventions may move individuals closer to establishing independence in the community. Specifically, we indicated that FAST participants were over twice as likely to have a successful treatment response than Support participants. We believe this is because our psychosocial intervention focused on developing functional skills in patients with schizophrenia. The NNT for this intervention is quite small and comparable to that of many widely accepted medical and psychiatric interventions (eg, obtaining remission in depression with serotonin specific reuptake inhibitor treatment). We acknowledge that medication interventions require less effort to administer than a full psychosocial intervention. However, we also note that medications likely cannot produce the outcomes targeted by our intervention (ie, functional skills), and clinicians need to consider for themselves whether they feel the effort expended in this intervention is worth the outcomes gained (eg, potential residential independence, improved medication management). NNT is a good effect size because individual clinicians can weigh the amount of effort it would take to achieve a cutoff score of 60 on the UPSA-Brief. In this case, every sixth participant would achieve this cutoff as a function of participating in the FAST intervention vs the control condition.
Because this is the first instance in which these effect sizes are reported for the UPSA-Brief, they lay the groundwork by which other treatments may be measured in terms of treatment success. Nonetheless, future studies should examine the efficacy of other interventions, particularly those that emphasize targets other than functional skills (eg, assertive community treatment [ACT], medication to improve cognition), and report comparable effect sizes for promoting change in the UPSA-Brief. These future studies will not only help further establish the UPSA-Brief as a valid outcome measure but will also help pinpoint treatment targets which do or do not impact functional capacity and likelihood of patients being able to reside independently.
Our factor analysis indicated that the 5 subscales of the full UPSA were highly correlated, as demonstrated by all 5 scales loading on 1 factor. In developing the UPSA, we desired to assess basic skills necessary for life functioning. Basic life skills are often learned in consort with one another during formative stages of one's development.27 Thus, successful acquisition of one skill would likely be associated with development of the other skills assessed by the UPSA. It is for this reason we feel the UPSA-Brief is an excellent brief measure of functional capacity.
Our study has several limitations. For example, we examined the ability of the UPSA-Brief for predicting current residential independence, and future studies will need to establish the ability of this measure for predicting long-term independence. Further, we were not able to examine other outcomes relevant to real-world functioning, such as employment and/or work ability. A third limitation is that our population was administered the UPSA-Brief in English. We are aware that the UPSA has been translated into other languages and is currently being used in research in Mexico and Sweden. How well our results would generalize to these and other populations is not established. Therefore, validation of the UPSA-Brief for different languages and cultural/ethnic groups should be examined. Further, the sample studied was approximately 10 years older than the average age for clinical trials in schizophrenia, and there appear to be a number of clinical issues relevant to late-life schizophrenia. These include, but are not limited to, neuropsychological changes over time, remission, medical comorbidities, and antipsychotic side effects.28 How these factors impact residential independence and response to psychosocial treatments is unknown, and how our results generalize to younger samples is yet unclear. More research is recommended to evaluate the impact of age on these outcomes and to determine whether results from our study generalize to younger samples.
Residential independence represents a complex outcome criterion because for some individuals living situation may be determined more by the economic or social support resources available to the patient and less by their cognitive functioning or functional capacity. These and other factors might limit the ability of the UPSA-Brief (or other measures) to distinguish among groups. Because of this complexity, it is strongly recommended that future research control for these factors in predicting residential independence or determine for whom and under what circumstances the UPSA-Brief predicts residential independence. Finally, we did not use residential independence as an outcome for our intervention trial. Rather, we assessed patient capacity to reside independently by examining the ability of our FAST intervention to move patients over our established UPSA-Brief cutoff of 60. We therefore recommend that future trials examine the ability of interventions for successfully achieving short- and long-term residential independence.
In sum, the UPSA-Brief provides a time-efficient measure of functional capacity that is sensitive to neurocognitive performance, negative symptoms, living situation, and change via a psychosocial intervention. We believe the UPSA-Brief can be used in both research and community settings as a fast, objective assessment of overall functioning in patients with schizophrenia and other chronic psychoses. Specifically, those working in these settings may use the UPSA-Brief to assess magnitude of improvement via treatment and as a prognostic indicator of an individual's ability to reside independently in the community (eg, discharge planning). Future research should examine the efficacy of other interventions (eg, ACT, cognition-enhancing medications) for improving UPSA-Brief scores and explore the relationship between the UPSA-Brief and other outcome measures.
Acknowledgments
This research was supported, in part, by MH 62554 by the National Institute of Mental Health to Dr Patterson, MH 66248 by the National Institute of Mental Health to Dr Jeste, and award MH 63116 by the National Institute of Mental Health to Dr Harvey, as well as the VA VISN-22 and VA VISN-3 MIRECC.
Appendix
UPSA-Brief
The UPSA-Brief is a measure of functional capacity in which patients are asked to role-play tasks in 2 areas of functioning: (1) communication and (2) finances. The UPSA-Brief requires approximately 10–15 minutes to complete and may be administered by a suitably trained lay professional.
Communication. The communication subtest revolves around several role-play exercises using an unplugged telephone. For the first exercise, patients are asked to show the tester what number they would dial if they had an emergency. A second exercise requires the patient to call information to get a specific telephone number, after which they are asked to dial the number from memory. Next, patients are given a medical appointment confirmation letter that details how the patient is to prepare for the medical appointment (eg, fast for a blood draw) and what 2 items they need to bring with them to the doctor (eg, insurance card and list of medications). After reading the letter, the patient is asked to describe how the letter requested them to prepare for the appointment. In addition, the patient is asked to call to the hospital to reschedule the doctor's appointment. There are a total of 9 communication subtasks that require about 5 minutes to complete.
Finance. This subtest tests the patient's ability to count change, read a utility bill, and write checks. Patients are first provided with real currency (coins and bills) and asked to count out given amounts (eg, $12.17, $6.73, $1.02) and make change from 10 dollars. Next, patients are shown a real bill from a utility company (eg, San Diego Gas and Electric) and given a blank check. Using this check, patients are asked to make out a check to the utility company for the amount owed. Points are given for each correct element of this process (the check is made out to San Diego Gas and Electric, the written amount corresponds to the bill, the check is signed, etc.). This subtest takes approximately 8 minutes to complete.
Test Information
Any individual interested in obtaining a copy of the UPSA-Brief and scoring sheets may contact the corresponding author.
References
- 1.Bowie CR, Reichenberg A, Patterson TL, Heaton RK, Harvey PD. Determinants of real-world functioning performance in schizophrenia: correlations with cognition, functional capacity, and symptoms. Am J Psychiatry. 2006;163:418–425. doi: 10.1176/appi.ajp.163.3.418. [DOI] [PubMed] [Google Scholar]
- 2.Liberman RP. Assessment of social skills. Schizophr Bull. 1982;8:62–83. doi: 10.1093/schbul/8.1.62. [DOI] [PubMed] [Google Scholar]
- 3.Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry. 1996;153:321–330. doi: 10.1176/ajp.153.3.321. [DOI] [PubMed] [Google Scholar]
- 4.Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr Bull. 2000;26:119–136. doi: 10.1093/oxfordjournals.schbul.a033430. [DOI] [PubMed] [Google Scholar]
- 5.Moore DJ, Palmer BW, Patterson TL, Jeste DV. A review of performance-based measures of everyday functioning. J Psychiatr Res. 2007;41:97–118. doi: 10.1016/j.jpsychires.2005.10.008. [DOI] [PubMed] [Google Scholar]
- 6.Evans JD, Heaton RK, Paulsen JS, Palmer BW, Patterson T, Jeste DV. The relationship of neuropsychological abilities to specific domains of functional capacity in older schizophrenia patients. Biol Psychiatry. 2003;53:422–430. doi: 10.1016/s0006-3223(02)01476-2. [DOI] [PubMed] [Google Scholar]
- 7.Klapow J, Evans J, Patterson T, Heaton R, Koch W, Jeste D. Direct assessment of functional status in older patients with schizophrenia. Am J Psychiatry. 1997;154:1022–1024. doi: 10.1176/ajp.154.7.1022. [DOI] [PubMed] [Google Scholar]
- 8.McKibbin C, Patterson TL, Jeste DV. Assessing disability in older patients with schizophrenia: results from the WHODAS-II. J Nerv Ment Dis. 2004;192:405–413. doi: 10.1097/01.nmd.0000130133.32276.83. [DOI] [PubMed] [Google Scholar]
- 9.Patterson TL, Goldman S, McKibbin CL, Hughs T, Jeste DV. UCSD Performance-based Skills Assessment: development of a new measure of everyday functioning for severely mentally ill adults. Schizophr Bull. 2001;27:235–245. doi: 10.1093/oxfordjournals.schbul.a006870. [DOI] [PubMed] [Google Scholar]
- 10.Twamley EW, Doshi RR, Nayak GV, et al. Generalized cognitive impairments, ability to perform everyday tasks, and level of independence in community living situations of older patients with psychosis. Am J Psychiatry. 2002;159:2013–2020. doi: 10.1176/appi.ajp.159.12.2013. [DOI] [PubMed] [Google Scholar]
- 11.Mausbach BT, Bowie CR, Harvey PD, et al. J Psychiatr Res. Usefulness of the UCSD Performance-based Skills Assessment (UPSA) for predicting residential independence in patients with chronic schizophrenia. February 13, 2007; doi:10.1016/j.jpsychires.2006.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patterson TL, Mausbach BT, McKibbin C, Goldman S, Bucardo J, Jeste DV. Functional Adaptation Skills Training (FAST): a randomized trial of a psychosocial intervention for middle-aged and older patients with chronic psychotic disorders. Schizophr Res. 2006;86:291–299. doi: 10.1016/j.schres.2006.05.017. [DOI] [PubMed] [Google Scholar]
- 13.Mattis S. Odessa, FL: Psychological Assessment Resources; 1973. Dementia Rating Scale. [Google Scholar]
- 14.Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 15.Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143:29–36. doi: 10.1148/radiology.143.1.7063747. [DOI] [PubMed] [Google Scholar]
- 16.Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 1983;148:839–843. doi: 10.1148/radiology.148.3.6878708. [DOI] [PubMed] [Google Scholar]
- 17.Sussner BD, Smelson DA, Rodrigues S, Kline A, Losonczy M, Ziedonis D. The validity and reliability of a brief measure of cocaine craving. Drug Alcohol Depend. 2006;83:233–237. doi: 10.1016/j.drugalcdep.2005.11.022. [DOI] [PubMed] [Google Scholar]
- 18.Koenig HG, Cohen HJ, Blazer DG, Meador KG, Westlund R. A brief depression scale for use in the medically ill. Int J Psychiatry Med. 1992;22:183–195. doi: 10.2190/M1F5-F40P-C4KD-YPA3. [DOI] [PubMed] [Google Scholar]
- 19.Altman DG, Bland JM. Diagnostic tests 2: predictive values. BMJ. 1994;309:102. doi: 10.1136/bmj.309.6947.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bandura A. Englewood Cliffs, NJ: Prentice-Hall; 1986. Social Foundations of Thought and Action: A Social Cognitive Theory. [Google Scholar]
- 21.Patterson TL, McKibbin C, Taylor M, et al. Functional adaptation skills training (FAST): a pilot psychosocial intervention study in middle-aged and older patients with chronic psychotic disorders. Am J Geriatr Psychiatry. 2003;11:17–23. [PubMed] [Google Scholar]
- 22.Cohen J. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- 23.Kraemer HC, Morgan GA, Leech NL, Gliner JA, Vaske JJ, Harmon RJ. Measures of clinical significance. J Am Acad Child Adolesc Psychiatry. 2003;42:1524–1529. doi: 10.1097/00004583-200312000-00022. [DOI] [PubMed] [Google Scholar]
- 24.American Psychiatric Association. Washington, DC: American Psychiatric Association; 2000. Diagnostic and Statistical Manual of Mental Disorders Fourth Edition, Text Revision. [Google Scholar]
- 25.Revheim N, Medalia A. The independent living scales as a measure of functional outcome for schizophrenia. Psychiatr Serv. 2004;55:1052–1054. doi: 10.1176/appi.ps.55.9.1052. [DOI] [PubMed] [Google Scholar]
- 26.Roy-Byrne P, Dagadakis C, Unutzer J, Ries R. Evidence for limited validity of the revised global assessment of functioning scale. Psychiatr Serv. 1996;47:864–866. doi: 10.1176/ps.47.8.864. [DOI] [PubMed] [Google Scholar]
- 27.Masten AS, Coatsworth JD. The development of competence in favorable and unfavorable environments: lessons from research on successful children. Am Psychol. 1998;53:205–220. doi: 10.1037//0003-066x.53.2.205. [DOI] [PubMed] [Google Scholar]
- 28.Folsom DP, Lebowitz BD, Lindamer LA, Palmer BW, Patterson TL, Jeste DV. Schizophrenia in late life: emerging issues. Dialogues Clin Neurosci. 2006;8:45–52. doi: 10.31887/DCNS.2006.8.1/dfolsom. [DOI] [PMC free article] [PubMed] [Google Scholar]