Abstract
Background
There is a growing movement, globally and in the Africa region, to reduce financial barriers to health care generally, but with particular emphasis on high priority services and vulnerable groups.
Objective
This article reports on the experience of implementing a national policy to exempt women from paying for delivery care in public, mission and private health facilities in Ghana.
Design
Using data from a complex evaluation which was carried out in 2005–2006, lessons are drawn which can inform other countries starting or planning to implement similar service-based exemption policies.
Results
On the positive side, the experience of Ghana suggests that delivery exemptions can be effective and cost-effective, and that despite being universal in application, they can benefit the poor. However, certain ‘negative’ lessons are also drawn from the Ghana case study, particularly on the need for adequate funding, and for strong institutional ownership. It is also important to monitor the financial transfers which reach households, to ensure that providers are passing on benefits in full, while being adequately reimbursed themselves for their loss of revenue. Careful consideration should also be given to staff motivation and the role of different providers, as well as quality of care constraints, when designing the exemptions policy. All of this should be supported by a proactive approach to monitoring and evaluation.
Conclusion
The recent movement towards making delivery care free to all women is a bold and timely action which is supported by evidence from within and beyond Ghana. However, the potential for this to translate into reduced mortality for mothers and babies fundamentally depends on the effectiveness of its implementation.
Keywords: maternal health, exemptions, Ghana, health financing, equity, evaluation
There is a growing movement, globally and particularly in the Africa region, to reduce financial barriers to health care generally, but with special emphasis on high priority services and vulnerable groups. In Burundi, for example, free services for pregnant women and the under-fives were introduced in 2006, and utilisation appears to have increased as a result, though no formal evaluation has been undertaken (1). In Zambia, fees were suspended for rural districts in 2006. In Burkina Faso, an 80% subsidy policy for deliveries was launched in 2006 (2). Other countries have followed suit, though with varying target groups, and all still at the stage of being elaborated. In Kenya, for example, various changes have been made to the user fee regime – most recently, in 2007, deliveries were announced to be free, though there is no evidence yet of implementation or impact. Liberia suspended fees for primary care in 2007. Niger announced free care for children late in 2007. Sudan announced free care for caesarean sections and children in January 2008. It is, however, too early yet to assess how these policies have been implemented and the size and nature of their effects.
In Ghana, an exemptions policy for delivery fees was introduced in 2004 (3). It was intended to cover all facility costs for intrapartum care in both public and private facilities. Initially payment was effected through the local government administration but later through the health system. Funding was provided from a debt relief fund, under the Highly Indebted Poor Countries (HIPC) initiative. This was gradually phased out and was replaced by health insurance in 2008.
Between October 2005 and November 2006, an evaluation of the policy in six districts each in the Central and Volta regions was conducted by an international research initiative – the Initiative for Maternal Mortality Programme Assessment (IMMPACT) (4). The evaluation used eight main tools, including key informant interviews; financial flows tracking; a health worker incentives survey; a household cost survey; a utilisation survey; community and provider interviews; confidential enquiry in hospitals; and clinical case note extraction in health centres. The findings provide useful lessons for countries that are planning or starting to operate maternal or other service-based exemption policies.
Background
Reducing maternal mortality and reaching the Millennium Development Goal (MDG) 5 target by 2015 is proving a serious challenge for many countries, including Ghana. The estimate of the maternal mortality ratio (MMR) in Ghana in 2005 was 560 per 100,000 live births (range: 200–1,300) (5), putting it clearly in the category of countries with a high burden of maternal mortality. In this year's Aide Memoire, the Honourable Minister of Health declared the high maternal mortality in the country as a national emergency and highlighted the need to accord greater priority to reproductive health services (6).
Demographic and Health Survey figures for the 10-year period from 1993 to 2003 show a steady improvement in the proportion of deliveries with skilled attendants – one of the two proxy indicators for tracking MDG5 (7). Recent figures however indicate that this trend has been reversed. According to the independent review of 2007, the proportion of deliveries attended by skilled health personnel declined from 54% to 35% between 2005 and 2007 (8). This decline in skilled attendants at delivery may be linked to the under-funding and then abolition of the exemptions policy for delivery fees, which was introduced in 2004, as well as the health worker strike of 2007. In parallel, institutional mortality rates and the proportion of births attended by traditional birth attendants are reported to be increasing. The recent Countdown to 2015 report indicates that Ghana has only half of the recommended minimum national provision of Emergency Obstetric Care services (9).
In addition to concerns about the direction of change in the summary indicators, there are continuing and increasing inequalities in access to skilled attendants at delivery. In Ghana, the absolute differences between the bottom and top quintiles in terms of delivery by a health professional, as evidenced by DHS data, increased from 60% in 1993 to 68% in 1998 and nearly 70% in 2003. This compares with an average poor–rich gap of 42% for a selection of sub-Saharan African countries (10).
Funding is increasingly available to support initiatives to reduce financial barriers as part of the international effort to improve progress towards the MDG goals. A recent example was the bilateral UK grant of £42.5m to Ghana. Part of this grant is being used to support the policy of free medical care for pregnant women announced by the President in May 2008, to be implemented through the National Health Insurance Scheme (NHIS). As this new initiative is rolled out, it is important that it builds on lessons (both positive and negative) from the evaluation of the previous exemption policy.
Lessons from an evaluation of the delivery exemption policy
1. The exemption policy can be cost-effective
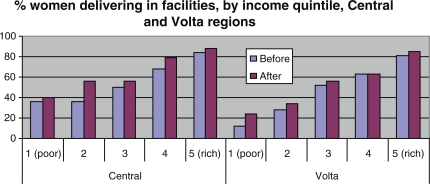
The evaluation by IMMPACT found that the exemptions were effective in raising utilisation significantly, with some modest equity gains (11) (Fig. 1). Overall public expenditure on the policy was $22 per delivery (of all types), or $62 per additional delivery. (This indicates the marginal benefits of the policy by dividing the total cost of the policy by the increase in delivery numbers over the period, making the assumption that these are attributable to the policy.) (12). However, future costs will be higher if a more integrated package (including other pregnancy-related and non-pregnancy related care) is offered through the NHIS.
Fig. 1. .
Proportion of women delivering in health facilities before & after fee exemption, by income, Central and Volta regions. Source: based on data from Penfold et al. (2007).
2. Equity issues can be effectively addressed
The results from the evaluation suggest that inequalities can decrease in response to a universal exemption (Fig. 1). In the 18 months after fee exemption was introduced, the largest increase in facility utilisation in Volta Region was amongst the poorest (first quintile), while in Central Region it was amongst the poor (second quintile). In terms of household payments, the incidence of catastrophic out-of-pocket (OOP) payment was found to fall (13). For the poorest quintile, the proportion paying more than 2.5% of their income dropped from 55% before the policy to 46% after. Using the poverty head count, the proportion of households falling into extreme poverty as a result of their delivery payments reduced from 2.5% before the policy to 1.3% after.
However, the proportionate decrease in OOP payments was greater for the richest households (22%), compared to the poorest (13%). Moreover, to reach the poorest and the poor in some areas, additional demand-side cost issues such as transportation costs, might need to be addressed.
3. Ensuring adequate funding flows is critical
The previous exemption scheme in Ghana was under-funded, causing debts at facility level and intermittent implementation of the scheme (14). This was exacerbated by the rapid scaling up of the exemptions policy, which was extended from four poorer regions in 2004 to the whole country in 2005, before an evaluation of early results could be conducted. The inadequate funding flows created friction between communities and health staff and between facility managers and higher levels of the health system. There is a risk of this scenario being repeated under the new insurance-based approach. To ensure adequate funds requires not only realistic planning and budgeting, but also a reliable and long-term source of funding. This will require stronger inter-ministerial negotiations with the Ministry of Finance and also the ability to deliver and document policy success.
4. Building institutional ownership early on is important
Establishing clear lines of responsibility early on in the implementation process is crucial, with a unit or even individuals within the Ministry having a specific responsibility to develop, fine-tune, manage and monitor the policy. The delivery exemption policy in Ghana suffered from a lack of such ownership (14).
5. The exemptions should effectively address the main household cost barriers
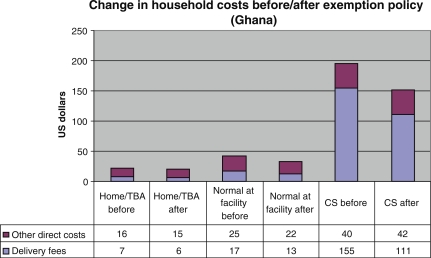
Exemptions do not address non-facility costs. This is reasonable in areas which have easy access to services, but will be inadequate in areas with substantial distance barriers. The IMMPACT evaluation found that facility costs formed the largest proportion of overall household costs for deliveries in Ghana, particularly for more expensive procedures (40% of costs for normal deliveries but 80% for caesarean sections prior to the exemptions policy) (13). These emergency procedures are both life-saving and potentially catastrophic for households, and should therefore receive priority in exemptions policies.
In Ghana, however, the evaluation found that even facility costs were not reduced to zero by the exemption policy – the reduction was of a magnitude of 28% for caesarean sections and 26% for normal deliveries (Fig. 2).
Fig. 2. .
Delivery costs before and after exemption, Ghana. Source: based on data from Asante et al. (2007).
This points to the need to assess real impact on households to ensure that subsidies are adequate and that they are being passed on in reality to users. Analysis of funding flows to the delivery exemption policy found an average public expenditure on the scheme of $22 per delivery compared with an average ‘benefit’ to clients of around $10 per delivery (12). This difference in value may reflect regional differences (the cost data came from Central Region while the benefits data came from Volta) or it may reflect facilities not passing on the full cost reduction to users. Minimising any such loss of benefits within the system is crucial. Maintaining community confidence in a clearly defined and predictable benefits package is essential, and this has been problematic in the past.
6. Facilities must be adequately (but not over-generously) reimbursed for their costs
In Ghana, as in many countries, user fees fund much of the recurrent non-salary costs of care. If this revenue stream is not adequately replaced, it is not realistic to expect providers to implement an exemptions policy effectively. Analysis of funding flows found that while funding was available from the national level, facilities benefited from the exemption scheme, gaining a more reliable stream of funding (15). However, a more rigorous system of monitoring and auditing was not in place and would be needed in the longer term for cost control.
7. Staff must be motivated to provide appropriate care to all
The costing of the policy has to assess whether salary costs are likely to be affected and whether existing staff can cope with the projected increase in workload. In Ghana, staff reported working long hours (79 hours per week for public midwives, 109 for doctors, and 129 for medical assistants, who are in sole charge of health centres around the clock). However, the increase in workload over the period of policy introduction (which was largest for public midwives – an increase of 27% in terms of working hours) was indirectly compensated by a rising general health worker pay level (16). In future, if the insurance-based approach is successful, increased numbers of core health staff and increased pay levels may be required and these costs will have to be taken into account in planning national budgets.
8. Attention should be paid to improving quality of care
The evaluation included a number of components investigating quality of maternity care, all of which concluded that the exemption policy had not led to a deterioration, but that quality of care – before and after – was an area of concern (17). A look at scores obtained for five care components of labour and delivery care at health centre level revealed that when compared with their respective maximum expected scores, the lowest scores were obtained for management of the first stage of labour, use of the partograph and for immediate post partum monitoring of mother and baby (18). Confidential enquiry techniques also found that women received poor quality care in hospitals, resulting in many potentially avoidable deaths (19). However, health systems factors, such as availability of consumables and basic equipment for providing comprehensive emergency obstetric care, were generally found to be adequate. Qualitative investigations found very variable relationships between health workers and clients, ranging from positive to antagonistic. If fee exemptions are to be effective in improving health, these quality issues have to be addressed.
9. The whole range of providers should be included
The Ghana policy provided for deliveries conducted by public, mission and private providers, with differential tariffs to reflect the varying public subsidies which these players receive. Informal providers were not included in the policy. However, the community investigations for the evaluation of the delivery exemption policy found widespread trust in traditional birth attendants (TBAs) (20). Some districts did in practice provide for trained TBAs to refer and accompany pregnant women, thus ensuring continuity of care. This is particularly important in more remote areas, where access to facilities is problematic.
10. A strong monitoring and evaluation component should be built in
Underpinning all of these lessons is the need for a strong monitoring and evaluation component to address problems early and market successes. This should be established from the beginning, involving Ministries of Health in partnership with independent evaluation institutions.
Conclusion
The recent movement towards making delivery care free to all women is a bold and timely action which is supported by evidence from within and beyond the Africa region. The potential for this to translate into reduced mortality for mothers and babies fundamentally depends on the effectiveness of its implementation and the actions taken to assure quality of services. There are clear lessons from the evaluation of the fee exemption scheme in Ghana which can help strengthen the provision of free services to pregnant women globally.
Acknowledgements
This work was undertaken as part of an international research programme – IMMPACT (Initiative for Maternal Mortality Programme Assessment), funded by the Bill & Melinda Gates Foundation, the Department for International Development, the European Commission and USAID. The funders have no responsibility for the information provided or views expressed in this paper. The views expressed herein are solely those of the authors.
References
- 1.Batungwanayo C, Reyntjens L. L'impact du decret presidentiel pour la gratuite des soins sur la qualite des services de soin de sante au Burundi. Bujumbura: Ministere de la Sante Publique, OMS; 2006. [Google Scholar]
- 2.Ministere de la Sante. Ougadougou: Direction de la Sante de la Famille; 2006. Strategie nationale de subvention des accouchements et des soins obstetricaux et neonatals d'urgence au Burkina Faso. [Google Scholar]
- 3.Ministry of Health. Accra: Ministry of Health; 2004. Guidelines for implementing the exemption policy on maternal deliveries. Report No.: MoH/Policy, Planning, Monitoring and Evaluation-59. [Google Scholar]
- 4.Armar-Klemesu M, Graham W, Arhinful D, Hussein J, Asante F, Witter S, et al. Aberdeen and Accra: IMMPACT; 2006. An evaluation of Ghana's policy of universal fee exemption for delivery care. [Google Scholar]
- 5.WHO; UNICEF; UNFPA. Geneva: WHO; 2007. World Bank. Maternal mortality in 2005. [Google Scholar]
- 6.MoH/Health Partners. Accra: MoH; 2008. Joint Ministry of Health/Partners business meeting: Aide Memoire. [Google Scholar]
- 7.Ghana Statistical Service. Accra: GSS, NMIR, ORC Macro; 2004. Ghana demographic and health service survey 2003. [Google Scholar]
- 8.Ministry of Health. Accra: MoH; 2008. Independent review: health sector programme of work 2007. [Google Scholar]
- 9.UNICEF. Countdown to 2015: tracking progress in maternal, newborn and child survival: 2008 report; New York: UNICEF; 2008. [Google Scholar]
- 10.Gwatkin D, Rutstein S, Johnson K, Suliman E, Wagstaff A, Amouzou A. Socioeconomic differences in health, nutrition and population in developing countries: an overview. Washington, DC: World Bank; 2007. [PubMed] [Google Scholar]
- 11.Penfold S, Harrison E, Bell J, Fitzmaurice A. Evaluation of the delivery-fee-exemption policy in Ghana: population estimates of changes in delivery service utilisation in two regions. Ghana Med J. 2007;41:100–9. [PMC free article] [PubMed] [Google Scholar]
- 12.Witter S, Armar-Klemesu M, Dieng T. National fee exemption schemes for deliveries: comparing the recent experiences of Ghana and Senegal. In: Richard F, Witter S, De Brouwere V, editors. Financing obstetric care. Antwerp: ITM; 2008. [Google Scholar]
- 13.Asante F, Chikwama C, Daniels A, Armar-Klemesu M. Evaluating the economic outcomes of the policy of fee exemption for maternal delivery care in Ghana. Ghana Med J. 2007;41:110–7. doi: 10.4314/gmj.v41i3.55277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Witter S, Adjei S. Start-stop funding, its causes and consequences: a case study of the delivery exemptions policy in Ghana. Int J Health Plann Manage. 2007;22:133–43. doi: 10.1002/hpm.867. [DOI] [PubMed] [Google Scholar]
- 15.Witter S, Aikins M, Kusi T. University of Aberdeen: IMMPACT; 2006. Funding and sustainability of the delivery exemptions scheme in Ghana. [Google Scholar]
- 16.Witter S, Kusi A, Aikins M. Working practices and incomes of health workers: evidence from an evaluation of a delivery fee exemption scheme in Ghana. Hum Resources Health. 2007;5:2. doi: 10.1186/1478-4491-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bosu W, Bell J, Armar-Klemesu M, Tornui J. Effect of delivery care user fee exemption policy on institutional maternal deaths in the Central and Volta Regions of Ghana. Ghana Med J. 2007;41:118–24. doi: 10.4314/gmj.v41i3.55278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deganus S, Tornui J. Aberdeen and Accra: IMMPACT; 2006. Impact of free delivery policy on utilization and quality of care at level B (basic obstetric care) facilities in Ghana. [Google Scholar]
- 19.Tornui J, Armar-Klemesu M, Arhinful D, Penfold S, Hussein J. Hospital based maternity care in Ghana: findings of a confidential enquiry into maternal deaths. Ghana Med J. 2007;41:125–32. doi: 10.4314/gmj.v41i3.55280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arhinful D, Zakariah-Akoto S, Madi B, Mallet-Ashietey B, Armar-Klemesu M. Aberdeen and Accra: IMMPACT; 2006. Effects of free delivery policy on provision and utilisation of skilled care at delivery: views from providers and communities in Central and Volta regions of Ghana. [Google Scholar]