ABSTRACT
Acute colonic pseudo-obstruction (ACPO), also known as Ogilvie's syndrome, is a condition characterized by massive colonic distension in the absence of mechanical obstruction. Patients presenting with Ogilvie's syndrome have underlying medical and surgical conditions predisposing them to the syndrome. Ogilvie's syndrome can often be managed by conservative therapy. However, unrecognized and untreated, the continued distension associated with Ogilvie's syndrome can lead to perforation that is associated with a high mortality rate. In this article, the pathophysiology, epidemiology, and treatment options are reviewed.
Keywords: Acute intestinal pseudo-obstruction, Ogilvie's syndrome
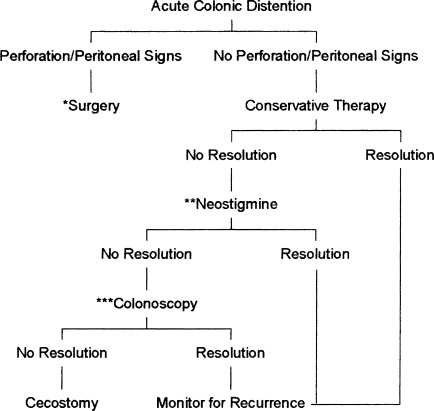
Acute colonic pseudo-obstruction (ACPO), also known as Ogilvie's syndrome, is a condition characterized by massive colonic distension in the absence of mechanical obstruction. Patients presenting with Ogilvie's syndrome have underlying medical and surgical conditions predisposing them to the syndrome. Ogilvie's syndrome can often be managed by conservative therapy (Fig. 1). However, unrecognized and untreated, the continued distension associated with Ogilvie's syndrome can lead to perforation that is associated with a high mortality rate. In this article, the pathophysiology, epidemiology, and treatment options are reviewed.
Figure 1.
Algorithm for acute colonic pseudo-obstruction. *If evidence of ischemia or perforation develop at any time, laparotomy is indicated. **Neostigmine may be repeated as necessary. ***Colonoscopy may be repeated once if initial colonoscopy shows no resolution.
PATHOPHYSIOLOGY
In 1948, Sir W.H. Ogilvie first described ACPO in two cases of patients with retroperitoneal malignancy who had an acute onset of nonobstructive colon dilatation.1 In both patients, the tumor had invaded the celiac plexus, causing Ogilvie to suggest sympathetic deprivation as the etiology of the massive distension.2 Advances in gastrointestinal physiology have further delineated the functions of the autonomic nervous system of the colon. Colonic motor and secretory functions are mediated by the autonomic nervous system. The sympathetic nervous system arises from the spinal cord at the level of the thoracic and lumbar spinal cord. Parasympathetic supply to the colon is delivered from two nerve trunks. The ascending colon to the level of the sigmoid receives parasympathetic innervation from the medulla oblongata via the vagus nerve. Distal to the splenic flexure, lumbar nerves from spinal segments S2 to S4 supply parasympathetic innervation.3
In general, the parasympathetic nervous system increases gut motility and the sympathetic system decreases motility.4 Abnormalities of the autonomic nervous system, characterized by sympathetic dysfunction, parasympathetic dysfunction, or a combination of both, have been used to explain the etiology of ACPO. In contrast to Ogilvie's initial theory of sympathetic deprivation, the success of neostigmine suggests that parasympathetic dysfunction is the likely etiology for Ogilvie's syndrome.5
EPIDEMIOLOGY
In 1986, Vanek published a survey of the scientific literature and reviewed 400 cases of Ogilvie's syndrome. In this series, males presented more frequently than females, with males presenting at an average age of 59.9 compared with 56.5 for the female patients. Female patients present at a somewhat younger age because of an association with cesarean section.6,7 Of the patients, 94.5% had an associated medical or surgical condition.6 Nonoperative trauma was the most commonly associated condition, although other large studies have seen an association with orthopedic surgery, infection, cardiac disease, recent postoperative status, and renal failure.5,6,8 Other factors contributing to the development of Ogilvie's syndrome include electrolyte disturbances and narcotic use.
CLINICAL PRESENTATION
Clinically, Ogilvie's syndrome arises in patients as massive colonic dilatation without mechanical obstruction. The exclusion of mechanical large bowel obstruction early in the evaluation is important as the two entities arise similarly but mechanical obstruction is likely to require urgent surgical intervention. The distinction between Ogilvie's syndrome and obstruction may be difficult to make. Both groups of patients present with obstructive symptoms, including nausea, vomiting, and abdominal pain. In contrast, patients with Ogilvie's syndrome report continuing to pass flatus in 40% to 50% of cases.6,7
Interestingly, it is also difficult to distinguish between patients with perforation or ischemia and those with uncomplicated distension. With the exception of peritoneal signs and fever, there is a similar cohort of symptoms among patients who have perforated or ischemic bowel and those with Ogilvie's syndrome.6 Therefore, a high index of suspicion and use of diagnostic studies are important early in the evaluation of massive colonic distension.
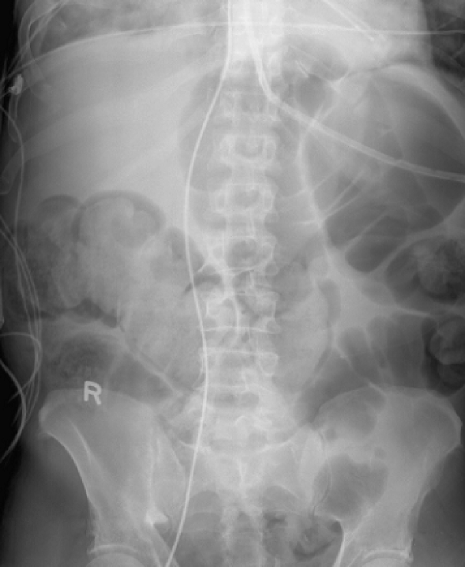
Radiographic studies are essential in differentiating Ogilvie's syndrome from other causes of large bowel distension. Flat and upright radiography reveals massively dilated colon (Fig. 2), often limited to the cecum and right colon.6,7,9 Preferably, a water-soluble contrast enema should be performed to rule out mechanical obstruction. In addition to being diagnostic, the water-soluble contrast enema may be successful in decompressing ACPO.10
Figure 2.
Abdominal radiograph showing dilated colon consistent with Ogilvie's syndrome in a patient with septic shock and complete heart block.
COMPLICATIONS
The most feared complication of Ogilvie's syndrome is cecal perforation. Fortunately, perforation is rare, occurring in only 1% to 3% of patients.4,6 Perforation is associated with a mortality rate of 50% to 71%, compared with 8% in the nonperforated group.4,6 Historically, cecal distension was thought to pose a threat of perforation when radiographically measured to be greater than 9 cm. However, several studies indicate that perforation is rare with cecal diameter less than 12 cm; when cecal diameter is greater than 14 cm, perforation occurs more commonly, in up to 23%.6,11 Thus, timely recognition is of utmost importance in the initial assessment of patients with ACPO.
INTERVENTIONS
Conservative Management
Patients presenting with ACPO with cecal distension less than 12 cm, provided they are not exhibiting evidence of ischemic or perforated bowel, should undergo a trial of conservative management of the disease. Conservative management involves a trial of bowel rest, nasogastric tube decompression, and rectal tube placement. In addition, the patients should undergo correction of electrolyte imbalances, discontinuation of narcotics, and treatment of underlying infection. Successful resolution is achieved in 83% to 96% of patients within 2 to 6 days of initiating therapy.9 Conservative therapy is not appropriate for patients exhibiting peritoneal signs or with radiographic evidence of perforation. Conservative management requires close surveillance of patients with serial examinations, plain film x-rays, and laboratory studies. In general, conservative therapy should be employed for 48 to 72 hours unless the patient demonstrates clinical deterioration or increasing cecal distension beyond 12 cm.
Medical Therapies
Most pharmacologic therapy has been directed at counteracting the sympathetic-parasympathetic imbalance associated with Ogilvie's. The best evidence for medical treatment is available for neostigmine. Neostigmine is an anticholinesterase that inhibits acetylcholinesterase to allow increased synaptic levels of acetylcholine. Clinical trials of neostigmine were initially performed in conjunction with guanethidine. Patients in this study were tried on conservative therapy for 48 hours. At the end of the conservative trial, patients were treated with an initial dose of guanethidine (an adrenergic blocker) followed by neostigmine (a parasympathomimetic). Eight of 11 patients had clinical improvement, and there were no recurrences among these patients.12 The researchers noted that improvement came after treatment with neostigmine administration, further supporting the theory that pseudo-obstruction is caused by parasympathetic suppression as opposed to sympathetic overactivity.12 Subsequent prospective studies supported the efficacy of neostigmine in treating ACPO.13,14,15,16,17 Patients had improvement in symptoms with only occasional mild side effects such as sweating and transient bradycardia. Recurrences were rare, ranging from 0% to 33%.4,14,15
Based on the success of these prospective trials, Ponec et al performed a prospective, randomized, double-blinded, placebo-controlled trial of neostigmine as a treatment for acute colonic pseudo-obstruction. Inclusion criteria were patients with cecal diameter of 10 cm in whom 24 hours of conservative treatment failed. Twenty patients were enrolled and randomly assigned to 2 mg neostigmine IV over a 3- to 5-minute period or normal saline placebo. All patients were monitored for the administration, and atropine was available at the bedside for symptomatic bradycardia. Ultimately, of the 18 patients receiving neostigmine therapy, 17 had an immediate response, and only 2 had recurrent colonic distension.4
Neostigmine is not without side effects. Patients in all trials were excluded because of a low baseline heart rate (< 60), low systolic blood pressure, or signs of perforation including peritoneal signs or free air on radiography. Patients should be monitored with cardiac monitors while receiving the medication, and atropine should be available at the bedside to counter neostigmine-induced bradycardia.4,14,16,17 Overall, however, neostigmine proved an effective and appropriate intervention in patients in whom conservative treatment failed.
Neostigmine may be repeated for patients with an incomplete response, patients without a response, or those with a recurrence. Whereas Ponec et al used 2 mg of neostigmine, most series have reported using 2.5 mg per dose.9,14,16,17 If the second dose of neostigmine fails to resolve the cecal dilatation, the patient should proceed to more aggressive measures of decompression. Contraindications to neostigmine include known hypersensitivity and mechanical urinary or intestinal obstruction. Relative contraindications include recent myocardial infarction, acidosis, asthma, bradycardia, peptic ulcer disease, and β-blocker therapy.18
Additional trials of prokinetics have not been as successful in treating ACPO. Only anecdotal cases utilizing erythromycin, metoclopramide, and cisapride have been reported.9,19 In addition, the use of epidural anesthesia as a block of excess sympathetic tone demonstrated only moderate success.20
One small study of 18 patients assessed the efficacy of a diatrizoate meglumine (Cystografin™) enema in relieving colonic distension. With this method, 78% of the patients were successfully decompressed.10 The mechanism is thought to be due to the hyperosmolality of the enema increasing intracolonic fluid. In patients with contraindications to neostigmine, Cystografin enema may offer a noninvasive alternative for decompression.
Medical therapy is reserved for patients in whom conservative measures fail. In the absence of contraindications, 2.5 mg of neostigmine should be administered to appropriately monitored patients without evidence of perforation or ischemia who have not responded to conservative measures or to patients with cecal diameter greater then 12 cm at presentation.
Endoscopic Decompression
Colonoscopic decompression of ACPO was first described in 1977. Five of six patients were successfully treated with colonoscopic decompression without any recurrences noted. Additional benefits of decompression included definitive assessment of the colon to exclude mechanical obstruction.21 Prior to the introduction of neostigmine, colonoscopy was the second-line treatment in patients not responding to conservative measures and is still an important aspect of the treatment armamentarium for Ogilvie's syndrome.
Colonoscopic decompression of the colon is effective, causing decreased cecal diameter in 73% to 100% of cases.22 However, recurrence rates of 10% to 65% have been noted after initial success as documented by increased cecal diameter on radiography.22,23,24 In the patients with a recurrence, repeated colonoscopic decompression was achieved in 56% to 87% but with higher rates of subsequent cecal distension.6,22 One technique that may decrease recurrence is placement of a decompression tube at the time of endoscopy. These tubes may be placed over a guide wire advanced through a colonoscope, held by forceps within the colonoscope as the colonoscope is advanced, or tied onto the colonoscope during the initial evaluation and released by shears.24,25,26 Use of tube decompression improves the overall success of decompression if placed in an area affected by Ogilvie's syndrome.11,27,28
In the largest series, involving 50 patients with Ogilvie's syndrome who underwent endoscopic decompression with attempted decompression tube placement, 88% of patients were successfully decompressed by endoscopy. Of patients receiving tube decompression, 80% were successfully treated compared with a 25% success rate when a tube was not used.11 There is some controversy over where the tube needs to be placed for effective decompression. Cannulation of the right colon results in the greatest reduction in cecal distension; however, provided the tube cannulates a portion of the colon affected by Ogilvie's, some degree of decompression is achieved.11,26,27,28 Postendoscopy management of the decompression tubes is also challenging as the tubes are susceptible to clogging.11,24,27,28 Overall, use of decompression tubes is an important adjunct to colonoscopic manipulation in Ogilvie's syndrome.
The advantage of endoscopic decompression is that mortality rates for colonoscopic decompression were 1% to 5% compared with 12% to 20% for tube cecostomy.23 Colonoscopy may be repeated to decompress the colon effectively, but again this is associated with a higher recurrence rate in patients who do not respond to the initial decompression. In all cases, colonoscopy is contraindicated with evidence of ischemia or perforation as these patients should proceed to surgical intervention.21 In summary, colonoscopy is a useful tool for assessment and treatment of patients with Ogilvie's syndrome. Colonoscopy should be employed in patients in whom conservative measures have failed, in those with a contraindication to neostigmine, or when neostigmine is not effective at decompressing the colon.
Role of Surgery: Cecostomy
Ogilvie's syndrome is one of the few indications for cecostomy. Surgical cecostomy is the definitive intervention for patients with ACPO unresponsive to other therapies and without evidence of ischemia or perforation. Traditionally, cecostomy is performed by limited laparotomy through a small incision overlying the cecum. Such an incision provides limited exposure of the colon and thus may result in misdiagnosis of ischemia or infarction. However, cecostomy provides decompression of the massively dilated cecum when performed in the appropriate patient.29
Other techniques for cecal tube decompression have been reported: as an adjunct to endoscopic decompression, using a percutaneous approach with computed tomography guidance, or by a laparoscopic approach.30,31,32 Colonoscopically guided cecostomy has been described as a minimally invasive method to treat massive colonic distension.32 In a review of 67 patients, 26 (39%) had cecostomy performed for pseudo-obstruction. Among these patients, there were five mortalities, none attributable specifically to the cecostomy. One patient went on to require colon resection, but all other patients were successfully decompressed. Complications occurred in 13 patients (50%) and included pericatheter leak, superficial wound infection, colocutaneous fistula, and premature catheter disruption.32 Advantages of the approach include the relative simplicity of the procedure and the prompt decompression.
Case reports describe additional approaches to cecostomy that may be less morbid than laparotomy. Techniques similar to gastrostomy tube placement using T-fasteners by a laparoscopic or an endoscopic approach may prove an effective and safer means to decompress the colon.30,33 The additional benefit of laparoscopy may be better visualization of the colon to diagnose unsuspected ischemia or infarction.
These novel techniques emphasize less invasive but definitive treatments for refractory Ogilvie's syndrome. This illustrates the challenge of managing this condition in a group of patients with significant underlying diseases and recent acute illnesses, trauma, or surgery that predisposed them to ACPO.
Regardless of technique, cecostomy is associated with postoperative management challenges including tube appliance management issues, the corrosive nature of the effluent, and catheter displacement.26 Such morbidity, however, is acceptable for a procedure that represents the final option for prevention of infarction and perforation.
Formal laparotomy is reserved for treatment of patients displaying peritoneal signs or perforation. In previous reviews, the actual surgical procedure performed was based on the status of the bowel at the time of operation. Procedures ranged from surgical cecostomy to right hemicolectomy to total abdominal colectomy.5,6,18 Mortality rates ranged from 35% to 60% with operative intervention.5,6,18 The high mortality was attributed to the comorbidities and the underlying acute conditions in this group of patients. Nevertheless, the high mortality of patients who undergo laparotomy illustrates the gravity of ischemia and perforation and underscores the need for prompt diagnosis, institution of management, and early surgical consultation. Again, serial assessment of a patient with Ogilvie's is critical for timely intervention. In the presence of ischemia or perforation, bowel resection with fecal diversion and mucous fistula is indicated.
SUMMARY
Ogilvie's syndrome or acute colonic pseudo-obstruction is a clinical syndrome arising with marked abdominal distension without evidence of mechanical obstruction. Diagnosis is confirmed by abdominal radiology. Prompt treatment is important to avoid the complication of perforated cecum. Treatment should include an initial trial of conservative measures with nasogastric decompression, bowel rest, and correction of electrolytes. Cessation of medications with the potential to exacerbate the condition, such as opioids, is also important. After a 24- to 48-hour period, if there is no improvement, the patient should have a trial of neostigmine provided there are no contraindications. Use of colonoscopy, decompression tube placement in the ascending colon, and cecostomy should be reserved for patients who do not respond to neostigmine administration. In the presence of peritoneal signs or perforation, surgery is the appropriate first intervention.
REFERENCES
- 1.Ogilvie W H. Large intestine colic due to sympathetic deprivation: a new clinical syndrome. Br Med J. 1948;2:671–673. doi: 10.1136/bmj.2.4579.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saunders M D, Kimmey M B. Colonic pseudo-obstruction: the dilated colon in the ICU. Semin Gastrointest Dis. 2003;14:20–27. [PubMed] [Google Scholar]
- 3.Law N M, Bharucha A E, Undale A S, Zinmeister A R. Cholinergic stimulation enhances colonic motor activity, transit, sensation in humans. Am J Physiol Gastrointest Liver Physiol. 2001;281:G1228–G1237. doi: 10.1152/ajpgi.2001.281.5.G1228. [DOI] [PubMed] [Google Scholar]
- 4.Ponec R J, Saunders M D, Kimmey M B. Neostigmine for the treatment of acute colonic pseudo-obstruction. N Engl J Med. 1999;341:137–141. doi: 10.1056/NEJM199907153410301. [DOI] [PubMed] [Google Scholar]
- 5.Tenofsky P L, Beamer R L, Smith R S. Ogilvie syndrome as a postoperative complication. Arch Surg. 2000;135:682–687. doi: 10.1001/archsurg.135.6.682. [DOI] [PubMed] [Google Scholar]
- 6.Vanek V W, Al-Salti M. Acute pseudo-obstruction of the colon (Ogilvie's syndrome): an analysis of 400 cases. Dis Colon Rectum. 1986;29:203–210. doi: 10.1007/BF02555027. [DOI] [PubMed] [Google Scholar]
- 7.Moons V, Coremans G, Tack J. An update on acute colonic pseudo-obstruction (Ogilvie's syndrome) Acta Gastroenterol Belg. 2003;66:150–153. [PubMed] [Google Scholar]
- 8.Anuras S, Shirazi S S. Colonic pseudo-obstruction. Am J Gastroenterol. 1984;79:525–531. [PubMed] [Google Scholar]
- 9.Delgado-Aros S, Camilleri M. Pseudo-obstruction in the critically ill. Best Pract Res Clin Gastroenterol. 2003;17:427–444. doi: 10.1016/s1521-6918(03)00023-4. [DOI] [PubMed] [Google Scholar]
- 10.Schermer C R, Hanosh J J, Davis M, Pitcher D E. Ogilvie's syndrome in the surgical patient: a new therapeutic modality. J Gastrointest Surg. 1999;3:173–177. doi: 10.1016/s1091-255x(99)80029-8. [DOI] [PubMed] [Google Scholar]
- 11.Geller A, Petersen B T, Gostout C J. Endoscopic decompression for acute colonic pseudo-obstruction. Gastrointest Endosc. 1996;44:144–150. doi: 10.1016/s0016-5107(96)70131-1. [DOI] [PubMed] [Google Scholar]
- 12.Hutchinson R, Griffiths C. Acute colonic pseudo-obstruction: a pharmacologic approach. Ann R Coll Surg Engl. 1992;74:364–367. [PMC free article] [PubMed] [Google Scholar]
- 13.Amaro R, Rogers A I. Neostigmine infusion: new standard of care for acute colonic pseudo-obstruction? Am J Gastroenterol. 2000;95:304–305. doi: 10.1111/j.1572-0241.2000.01737.x. [DOI] [PubMed] [Google Scholar]
- 14.Trevisani G T, Hyman N H, Church J M. Neostigmine: safe and effective treatment for acute colonic pseudo-obstruction. Dis Colon Rectum. 2000;43:599–603. doi: 10.1007/BF02235569. [DOI] [PubMed] [Google Scholar]
- 15.Loftus C G, Harewood G C, Baron T H. Assessment of predictors of response to neostigmine for acute colonic pseudo-obstruction. Am J Gastroenterol. 2002;97:3118–3122. doi: 10.1111/j.1572-0241.2002.07108.x. [DOI] [PubMed] [Google Scholar]
- 16.Stephenson B M, Morgan A R, Salaman J R, Wheeler M H. Ogilvie's syndrome: a new approach to an old problem. Dis Colon Rectum. 1995;38:424–427. doi: 10.1007/BF02054234. [DOI] [PubMed] [Google Scholar]
- 17.Turego-Fuentes F, Munoz-Jiminez F, Del Valle-Hernandez E, et al. Early resolution of Ogilvie's syndrome with intravenous neostigmine. Dis Colon Rectum. 1997;40:1353–1357. doi: 10.1007/BF02050822. [DOI] [PubMed] [Google Scholar]
- 18.Eisen G M, Baron T H, Dominitz J A, et al. Acute colonic pseudo-obstruction. Gastrointest Endosc. 2002;56:789–792. doi: 10.1016/s0016-5107(02)70348-9. [DOI] [PubMed] [Google Scholar]
- 19.MacColl C, MacCannell K L, Baylis B, Lee S S. Treatment of acute colonic pseudoobstruction with cisapride. Gastroenterology. 1990;98:773–776. doi: 10.1016/0016-5085(90)90301-g. [DOI] [PubMed] [Google Scholar]
- 20.Lee J T, Taylor B M, Singleton B C. Epidural anesthesia for acute pseudo-obstruction of the colon (Ogilvie's syndrome) Dis Colon Rectum. 1988;31:686–691. doi: 10.1007/BF02552584. [DOI] [PubMed] [Google Scholar]
- 21.Kukora J S, Dent T L. Colonic decompression of massive nonobstructive cecal dilation. Arch Surg. 1977;112:512–517. doi: 10.1001/archsurg.1977.01370040164025. [DOI] [PubMed] [Google Scholar]
- 22.Gosche J R, Sharpe J N, Larson G M. Colonoscopic decompression for pseudo-obstruction of the colon. Am Surg. 1989;55:111–115. [PubMed] [Google Scholar]
- 23.Bode W E, Beart R W, Spencer R J, Culp C E, Wolff B G, Taylor B M. Colonoscopic decompression for acute pseudo-obstruction of the colon (Ogilvie's syndrome) Am J Surg. 1984;147:243–245. doi: 10.1016/0002-9610(84)90098-9. [DOI] [PubMed] [Google Scholar]
- 24.Nano D, Prindiville T, Pauly M, Chow H, Ross K, Trudeau W. Colonoscopic therapy of acute pseudoobstruction of the colon. Am J Gastroenterol. 1987;82:145–148. [PubMed] [Google Scholar]
- 25.Groff W. Colonoscopic decompression and intubation of the cecum for Ogilvie's syndrome. Dis Colon Rectum. 1985;26:503–506. doi: 10.1007/BF02563739. [DOI] [PubMed] [Google Scholar]
- 26.Rex D K. Acute colonic pseudo-obstruction (Ogilvie's syndrome) Gastroenterologist. 1994;2:233–238. [PubMed] [Google Scholar]
- 27.Sariego J, Matsumoto T, Kerstein M D. Colonoscopically guided tube decompression in Ogilvie's syndrome. Dis Colon Rectum. 1991;34:720–722. doi: 10.1007/BF02050359. [DOI] [PubMed] [Google Scholar]
- 28.Fausel C S, Goff J S. Nonoperative management of acute idiopathic colonic pseudo-obstruction (Ogilvie's syndrome) West J Med. 1985;143:50–54. [PMC free article] [PubMed] [Google Scholar]
- 29.Corman M L. Colon and Rectal Surgery. 4th ed. Philadelphia: Lippincott-Williams and Wilkins; 1998.
- 30.Duh Q Y, Way L W. Diagnostic laparoscopy and laparoscopic cecostomy for colonic pseudo-obstruction. Dis Colon Rectum. 1993;36:65–70. doi: 10.1007/BF02050304. [DOI] [PubMed] [Google Scholar]
- 31.Casola G, Withers C, vanSonnenberg E, Herba M J, Saba R M, Brown R A. Percutaneous cecostomy for decompression of the massively distended cecum. Radiology. 1986;158:793–794. doi: 10.1148/radiology.158.3.3945754. [DOI] [PubMed] [Google Scholar]
- 32.Benacci J C, Wolff B G. Cecostomy: therapeutic indications and results. Dis Colon Rectum. 1995;38:530–534. doi: 10.1007/BF02148855. [DOI] [PubMed] [Google Scholar]
- 33.Ramage J I, Baron T H. Percutaneous endoscopic cecostomy: a case series. Gastrointest Endosc. 2003;57:752–755. doi: 10.1067/mge.2003.197. [DOI] [PubMed] [Google Scholar]