ABSTRACT
Fecal incontinence may be due to postpartum anal sphincter injuries or neurological damage even in the absence of obvious perineal trauma. Anal physiologic testing with transrectal ultrasound, manometry, and pudendal nerve terminal latency studies help to identify those patients with anal sphincter injuries who might benefit from anal sphincter repair. In this article, the authors discuss the specific tests that are available and how to interpret them.
Keywords: Anal sphincter injuries, fecal incontinence, anal physiology testing
Fecal incontinence (FI) is a devastating condition and the humiliation and suffering to the individual is only known to them.1 In otherwise healthy younger women, direct sphincter trauma or neuropathic injuries from vaginal deliveries are the principal causative factors in the development of FI.2 A delayed presentation of FI can also occur as the effects of menopause summate with those of pelvic muscular and neurologic injuries to produce overt symptoms of urinary incontinence, pelvic organ prolapse, and FI.3,4 Prospective studies using anal physiologic studies have shown that anal sphincter injuries can occur after vaginal deliveries without any visible signs of perineal trauma in 11.5 to 35% of patients.2,5,6,7,8,9 In general, anal manometric pressures are reduced after vaginal delivery, but resting and squeeze pressures are significantly lower if an anal sphincter defect is present.2,3,4,5,6,7 Pudendal nerve terminal latencies are prolonged initially, but in most cases return to normal 6 months postpartum.2,10 Snooks et al showed that women who had forceps delivery have increased pudendal nerve terminal latencies and are at increased risk for FI on 5-year follow-up.11
Transrectal ultrasound (TRUS), anal manometry, and pudendal nerve terminal latencies (PNTML) are the diagnostic studies that we use to evaluate individuals with fecal incontinence.12 These tests provide us with objective evaluation of anal neuromuscular function that would not be otherwise detected on clinical examination.
TRANSRECTAL ULTRASOUND
Transrectal ultrasound (TRUS) is a validated technique that is highly accurate for the detection of abnormalities in anal sphincter morphology.13 TRUS findings of anal sphincter tears are correlated with electromyography and manometric findings and are both sensitive and specific for anal sphincter tears at subsequent surgery.14
Transrectal ultrasound is also referred to as endorectal ultrasound or endoanal ultrasound. Transvaginal and transperineal ultrasonography have also been reported for anal muscular evaluation, but are limited because they cannot provide a circumferential view of the circular anal musculature.15,16 For rectal imaging, a balloon surrounding a transducer is filled with water so that it comes into direct contact with the rectal wall. For anal imaging a rigid cap filled with degassed water is utilized. A 360-degree rotating transducer allows for visualization of the anal musculature. Scanning can be performed with a 7 or 10 megahertz frequency crystal. Lower frequencies have better penetration, but cannot separate small reflectors; higher frequencies are used for superficial structures with low penetration. In the United States, standard orientation is such that anterior structures are at the top of the display, posterior structures at the bottom, left-sided structures at the right of the display and right-sided structures at the left of the display.
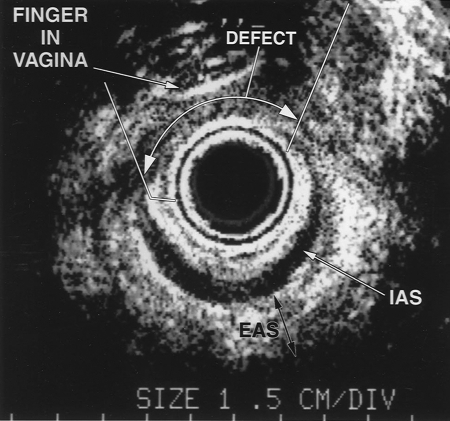
The patient is examined in the left lateral position. The probe is moved in or out of the anal canal and images are taken at the upper, middle, and distal anal canal. At the upper anal canal, the puborectalis is visualized as a hyperechoic U-shaped structure. At the middle anal canal, the external and internal sphincter muscles form a complete ring and outer hyperechoic and inner hypoechoic circles are visualized. At the lower anal canal, only the subcutaneous EAS is visualized as a hyperechoic ring. As one pulls the probe further externally the external sphincter becomes clearer, especially in the anterior location. In the setting of a possible obstetric injury, it is helpful to insert a finger in the vagina and apply pressure posteriorly. This helps to visualize discontinuity of the external sphincter and distinguish striated muscle from surrounding scar tissue. Anal sphincter injuries are detected by a break in the muscular ring. Defects may be reported as external anal sphincter (EAS), internal anal sphincter (IAS), or combined injuries. To confirm a true defect, it must be viewed in two out of three locations. The degree of separation of the muscular margins is not correlated with function (Figs. 1–6).17
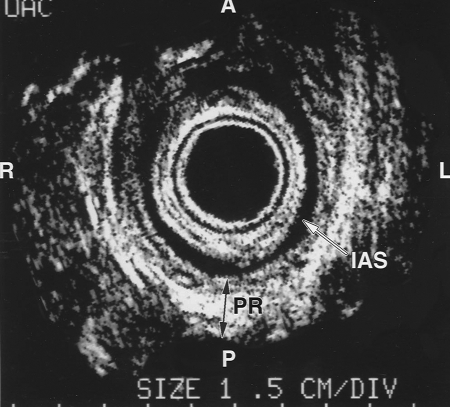
Figure 1.
Normal anal ultrasound of the upper anal canal. The internal anal sphincter (IAS) is a darker band (white arrow) and the puborectalis (PR) is visualized as a white U-shaped structure (dark arrow) surrounding the IAS. The top of the figure is anterior. Reproduced with permission from the Cleveland Clinic Foundation, Cleveland, Ohio.
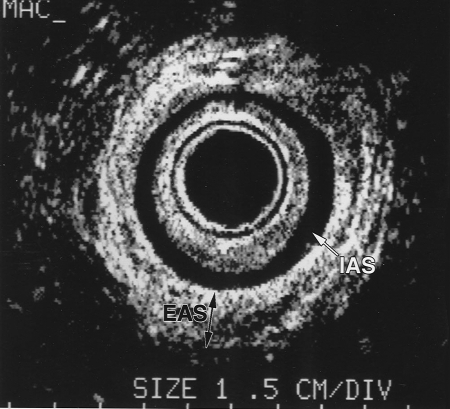
Figure 2.
Normal anal ultrasound of the middle anal canal. The darker homogenous ring is the internal anal sphincter (IAS; white arrow). The white heterogeneous ring is the external anal sphincter (EAS; dark arrow). The external sphincter is forming a 360-degree intact circle. Reproduced with permission from the Cleveland Clinic Foundation, Cleveland, Ohio.
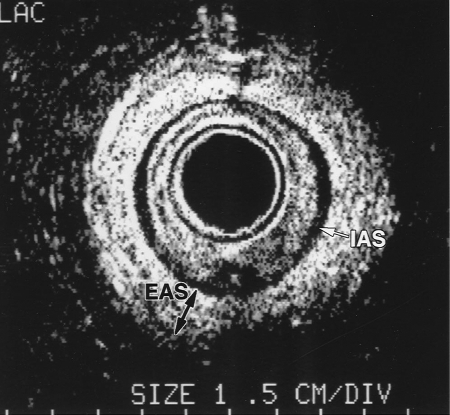
Figure 3.
Normal anal ultrasound of the lower anal canal. The white heterogeneous ring represents the external anal sphincter (EAS), which is most prominent (dark arrow) at the lower anal canal. There is a thin darker rim of internal anal sphincter muscle (IAS; white arrow). Reproduced with permission from the Cleveland Clinic Foundation, Cleveland, Ohio.
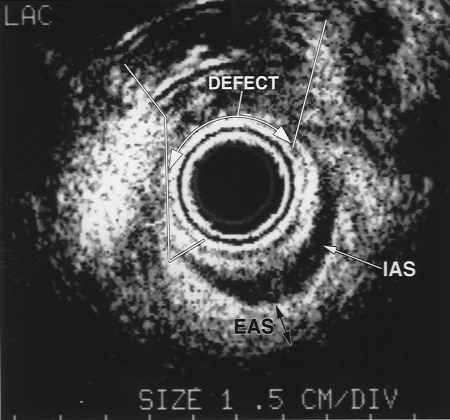
Figure 4.
Transanal ultrasound image with a finger placed into the vagina and gentle application of pressure posteriorly. Discontinuity of the external anal sphincter and internal anal sphincter muscle is visualized (defect; white arrow). The darker inner ring is the internal anal sphincter (IAS; white arrow) and the darker outer ring is the external anal sphincter (EAS; dark arrow). Reproduced with permission from the Cleveland Clinic Foundation, Cleveland, Ohio.
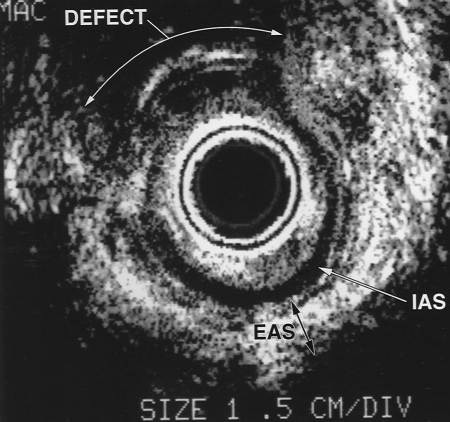
Figure 5.
Transanal ultrasound of traumatic anal sphincter injury. The large arrows represent the retracted muscle ends. Anteriorly there is disorganization and mixed echogenicity of the anterior defect. IAS, internal anal sphincter; EAS, external anal sphincter. Reproduced with permission from the Cleveland Clinic Foundation, Cleveland, Ohio.
Figure 6.
Transanal ultrasound of traumatic anal sphincter injury. The large arrows represent the retracted muscle ends. Anteriorly there is disorganization and mixed echogenicity of the anterior defect. IAS, internal anal sphincter; EAS, external anal sphincter. Reproduced with permission from the Cleveland Clinic Foundation, Cleveland, Ohio.
It has been reported that endoanal ultrasound is most reliable for identification of internal anal sphincter defects.18 Assessment of the EAS is more subjective, operator dependant, and confounded by normal anatomic variations including an external sphincter “gap” in many normal patients. Anomalous insertions of the external sphincter are reported in 14%.19 Ultrasound evaluation of the perineal body increases the sensitivity of detecting anal sphincter injuries,20 and measurements less than 10 mm are suspicious for sphincter injuries.21
Three-dimensional (3D) anorectal endosonography is the latest TRUS advancement. This technique takes the data from a series of closely spaced two-dimensional (2D) images and combines them to form a 3D image. The probe is inserted into the distal rectum and is stabilized. Once the probe is positioned, data acquisition is automatic, averaging 30 seconds to get a full set of 3D images. The scans are reviewed in the coronal plane to examine the anterior part of the external anal sphincter looking for a complete ring of muscle. The ability to image the sphincter in the coronal plane is a useful adjunct for confirming sphincter trauma, but does not show any trauma not already diagnosed using conventional axial images.22 Coronal views can be misleading unless axial views are correctly oriented. The advantages of the 3D ultrasound over the conventional 2D axial images is the study can be reviewed in detail using the 3D volume as a cine loop to repeatedly investigate suspicious areas. It is also possible to distinguish external sphincter tears from other closely related structures (Figs. 7–9).23
Figure 7.
B-K Medical (Herlev, Denmark) three-dimensional (3D) anorectal ultrasound equipment. The data from a series of closely spaced two dimensional images is combined to create a 3D image that can be freely rotated and sliced. The data stored in a file originating from one acquisition can be reviewed many times. Reproduced with permission from the Cleveland Clinic Foundation, Cleveland, Ohio.
Figure 8.
B-K Medical (Herlev, Denmark) ultrasound three-dimensional (3D) probe type 2050. There is a built in high resolution 3D acquisition system that can be operated at different levels of definition. Reproduced with permission from the Cleveland Clinic Foundation, Cleveland, Ohio.
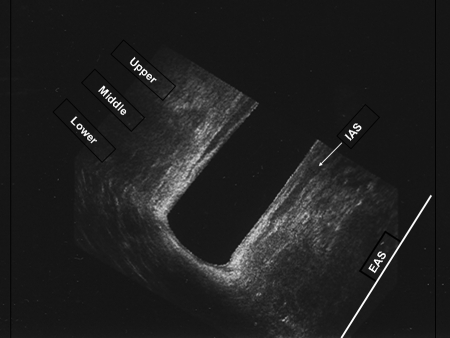
Figure 9.
Transanal ultrasound three-dimensional (3D) coronal view of normal anal canal. The upper, middle, and lower anal canals are depicted. The darker interior is the internal sphincter muscle (IAS; white arrow) and the whiter tissue is the external sphincter muscle. Reproduced with permission from the Cleveland Clinic Foundation, Cleveland, Ohio.
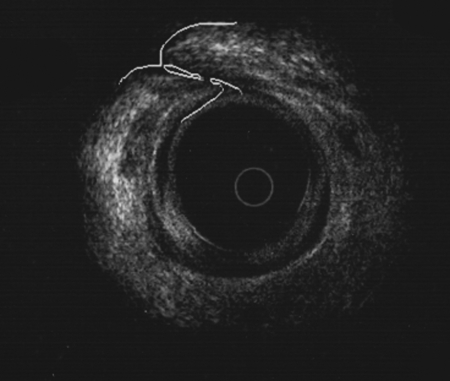
Ultrasound can also be used to study the patient who has persistent symptoms following sphincteroplasty. The repaired muscle has the sonographic appearance of the number “6” (Fig. 10).
Figure 10.
Transanal ultrasound of overlapping sphincter repair. The white outer circle represents the external anal sphincter complex, which is overlapped after sphincter repair. Reproduced with permission from the Cleveland Clinic Foundation, Cleveland, Ohio.
ANAL MANOMETRY
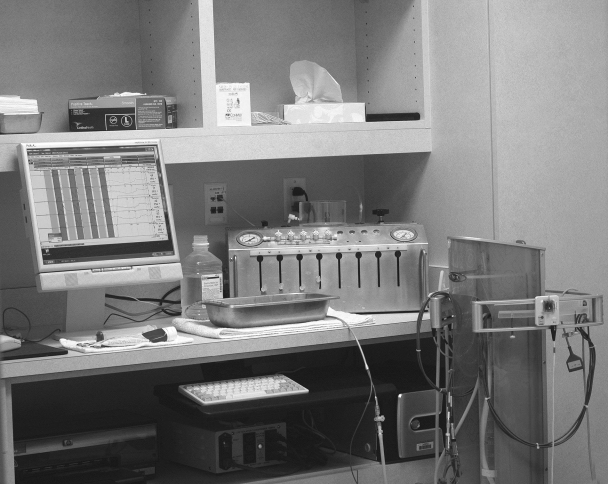
Methods to assess the anorectal sphincter have been in existence for more than 120 years. There are many excellent reviews on this topic.24,25 The basic concept for this technique is that an intraanal or intrarectal pressure-sensing device is linked to a recording apparatus, which is displayed on a computer monitor. The evaluation is performed by placing a specially designed catheter or balloon into the lower rectum and anal canal. The goal is to record reproducible measurements for quantitative assessment of the anal sphincter. The procedure is painless and simple; it can be performed in both adults and children in an ambulatory setting. The parameters evaluated during anal manometry include internal and external anal sphincter pressures; anal and rectal pressure response during straining; anal sphincter length; rectal sensation, capacity, and compliance; and anal sphincter muscle reflexes (Figs. 11–14).
Figure 11.
Anal manometry apparatus. The electronic catheter (Triton; Laborie Corp., Toronto, Canada) is linked to the polygraph and computer monitor. Reproduced with permission from the Cleveland Clinic Foundation, Cleveland, Ohio.
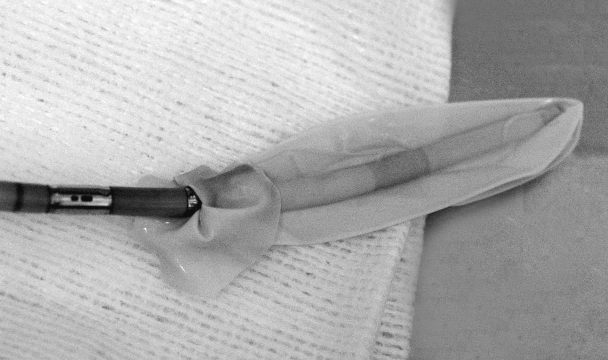
Figure 12.
Manometry catheter with balloon. This is an electronic manometry catheter (Unisensor USA, New York, NY) with four sensors. A balloon is tied to the end of the catheter for evaluation of rectal sensation. Reproduced with permission from the Cleveland Clinic Foundation, Cleveland, Ohio.
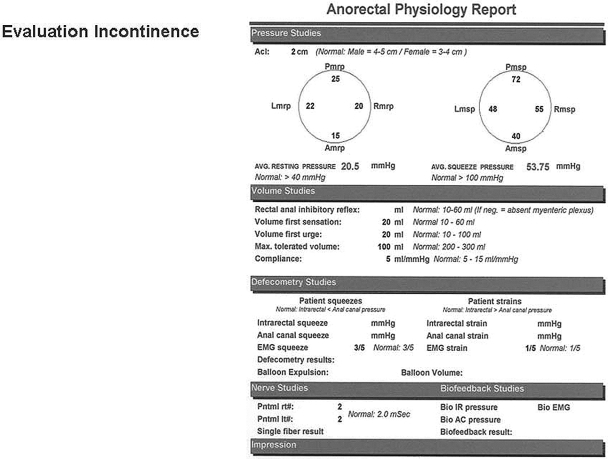
Figure 13.
Anal physiology report. Normal values identified for this laboratory are reported after each of the measurements. Reproduced with permission from the Cleveland Clinic Foundation, Cleveland, Ohio.
Figure 14.
Pudendal nerve stimulating electrode (Dantec, Skovlunde, Denmark) mounted on the examiners gloved finger. Reproduced with permission from the Cleveland Clinic Foundation, Cleveland, Ohio.
There are several different techniques for measuring anorectal pressures. They include fluid-filled and air-filled balloon systems, microballoons, and microtransducers. There are water-perfused catheters and solid-state catheters. Every technique is associated with inherent advantages and disadvantages. The procedures as well as the equipment used during anal manometry are not yet standardized and comparing results among centers is difficult.
One of the most common methods for measuring anorectal pressure utilizes a closed balloon system. The pressure result obtained with balloon recording is an average of all pressures acting on the balloon. Larger balloons are not physiologic because they may cause reflex contractions, but the results obtained are more representative of a greater area of the sphincter. The air-filled balloon technique reported by Schuster involves a larger balloon with more artifacts and this technique is better for measuring pressure changes than actual pressures.26 A small balloon tube technique is advantageous because the device itself only causes mild irritation of the sphincter.
The microtips are small electronic devices that are mounted on a solid-state catheter. The recordings are more physiologic due to diminished stretch artifacts of the sphincter complex compared with balloons or larger catheters. These devices are easy to handle, stable against temperature changes, sensitive to pressure changes and well tolerated by the patient. The disadvantages are that the recording area are very small, pressures are only measured in one direction and not circumferential, and that these catheters are more expensive.
The most widely used anal manometry system is water perfused. Pressures recorded are resistance pressures to a flow of water out of the catheter. The advantages include its wide availability, the specific measurements, the longitudinal or radial positioning, and low cost. Flexible catheters are more comfortable for the patient, but can twist in the anal canal. The outside diameter should not exceed 8 mm to diminish artifacts. There are open-ended and side-open catheters with 2 to 8 lumens. Up to eight channels are used to give precise pressure measurements, but four channels are adequate. The catheters are marked at 1-cm intervals.
Solid-state catheters have microtip catheters for pressure measurement. They require no water perfusion setup and are therefore easy to use and give reliable, accurate results. These catheters are available in a variety of configurations and come with attached probe adapters, which can be used in the ambulatory setting.
There are several manometric techniques. The catheter can be left in one position (stationary technique) or manually or automatically withdrawn (pull-through technique).
Stationary technique: the catheter is left in one position during recording
Stationary pull-through technique: the catheter is placed within the anal canal, and measurements are taken at 1-cm set intervals
Continuous pull-through technique: the catheter is moved through the lower rectum and the anal canal with a specially designed puller at a constant speed (1 cm/second) and the pressures are simultaneously recorded
Prior to undergoing anal manometry the patient should be reassured and put at ease because patient participation and relaxation is crucial. Enema clean out is preferred especially for constipated patients where fecal material can impair positioning of the catheter. The examination is performed with the patient in the left lateral position. The equipment is calibrated and the lubricated catheter is inserted to the 6-cm mark. The equipment is equilibrated and using the stationary manual pull-through technique resting, squeeze, and push pressures are recorded for 30 seconds. With the stationary pull-through technique, the following parameters are evaluated:
Mean resting pressure: the mean of all resting pressures calculated in the high-pressure zone
Maximal resting pressure: the highest resting pressure in the resting status in the high-pressure zone
Mean squeeze pressure: the mean of all squeeze pressures calculated in the high- pressure zone
Maximal squeeze pressure: the highest pressure achieved during squeezing in the high-pressure zone
High-pressure zone: an increase of 50% in the pressures while retracting the catheter
If a mechanical puller is used for the continuous pull through technique, then a 3D sphincter model can be calculated by computer imaging, volume vectography. Pressures are recorded and there should be a graduated increase in pressure proceeding distally. The highest resting pressures are generally recorded from 1 to 2 cm from the anal verge, but this varies. Women have lower pressures than men and pressures decrease with advancing age.27 Low anal pressures are seen in patients with incontinence from anal sphincter defects, neurogenic incontinence, rectal prolapse, and perineal descent. During normal squeeze effort, intraanal pressures double or triple their baseline resting pressures. Normal pressures vary from laboratory to laboratory.
Balloon distention is used to detect the first rectal sensory threshold, the urgency to defecate, and the sensation of pain otherwise known as the maximum tolerable volume. Rectal compliance is the capacity of the rectum to accommodate different volumes without altering rectal pressures. The first rectal sensation is usually between 10 to 20 mL of air. As more air is introduced, the rectum distends and the patient reports the urge to move their bowels. Viscous and elastic properties intrinsic to the rectum allow it to maintain a low intraluminal pressure despite a large volume.28 Through this mechanism of rectal compliance, stool contents can be accommodated so that defecation can be delayed. Low rectal compliance is identified in patients with inflammation to the rectum such as proctitis and inflammatory bowel disease and in patients with anal sphincter injuries. Some believe that the development and maintenance of a compliant rectum is related to a competent sphincter.29 It is unclear if poor rectal compliance is a cause or a consequence of fecal incontinence. High sensory thresholds have been associated with diabetes, peripheral neuropathy, perineal descent syndrome, fecal impaction, encopresis, spina bifida, and meningocele and may be related to overflow fecal incontinence or difficult evacuation.30
The rectal anal inhibitory reflex (RAIR) and rectal sensation are measured by insufflating 10 to 30 cc of air into an intrarectal balloon at the end of the catheter. Rectal distention causes reflex transient IAS relaxation and EAS contraction thus permitting rectal sampling of fecal contents. Patients with Hirschsprung and Chagas disease have an absent RAIR.
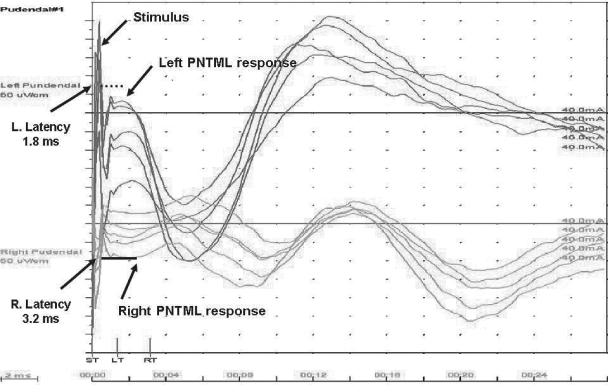
Pudendal Nerve Latency
Pudendal nerve terminal latency is a measurement of time from stimulation of the pudendal nerve to muscular contraction of the external anal sphincter. A disposable electrode on a St. Mark's catheter is placed on the examiner's gloved index finger and inserted into the anal canal. The ischial spine is palpated on the left and the pudendal nerve is stimulated transrectally. The response is detected when there is a contraction of the striated external anal sphincter muscle. This is repeated on the right side. Recordings are made from both sides of the pelvis because pudendal nerve damage may be asymmetric. The latency of normal pudendal nerve is 2.1 milliseconds ± 0.2 milliseconds (Figs. 14 and 15).
Figure 15.
Pudendal nerve terminal latency tracing. The left and right tracings are superimposed on one another. The stimulus is the large spike and muscular response is visualized at the take off of the curve (arrows). The latency measurement is the difference of the stimulus to the muscular contraction (arrows). On the left, the measurement is normal at 1.8 milliseconds. On the right, it is delayed at 3.2 milliseconds. Normal values are 2.0 ± 2 milliseconds.
Prolongation of the PNTML indicates damage to the pudendal nerve; however, the nature and the site of the lesion remain uncertain.31 Latency increases with age and is dependant on the size and degree of myelination of the nerve fibers. Neuropathies affecting myelin are seen in diabetes and affect speed of conduction. Moreover, the conduction velocity of a nerve may have little bearing on its functional integrity. The prevalence of prolonged PNTML in patients presenting for anorectal physiology studies is reported at 20 to 28% with unilateral neuropathy and 11 to 12% with bilateral neuropathy.31,32 Bilateral, not unilateral pudendal neuropathy is associated with diminished sphincter function and higher incontinence scores. The significance of pudendal nerve terminal latencies has been debated, however, there are few methods available to assess pelvic floor neurologic function. Furthermore, in some studies prolonged pudendal nerve latencies have been shown to be an important prognostic factor in patients undergoing anal sphincter repair.33
CONCLUSION
TRUS, manometry, and pudendal nerve latencies are important diagnostic studies in the evaluation of patients with fecal incontinence. These tests help to identify patients with anal sphincter injuries from other etiologies of fecal incontinence. Furthermore, it helps us to identify patients who might benefit from anal sphincter repair.
REFERENCES
- 1.Johanson J F, Lafferty J. Epidemiology of fecal incontinence: the silent affliction. Am J Gastroenterol. 1996;91:33–36. [PubMed] [Google Scholar]
- 2.Sultan A H, Kamm M A, Hudson C N, et al. Anal sphincter disruption during vaginal delivery. N Engl J Med. 1993;329:1956–1957. doi: 10.1056/NEJM199312233292601. [DOI] [PubMed] [Google Scholar]
- 3.Donnelly V, O'Connell P R, O'Herlihy C. The influence of oestrogen replacement on faecal incontinence in post menopausal women. Br J Obstet Gynaecol. 1997;104:311–315. doi: 10.1111/j.1471-0528.1997.tb11459.x. [DOI] [PubMed] [Google Scholar]
- 4.Nichols C M, Ramakrishnan V, Gill E J, Hurt W G. Anal incontinence in women with and those without pelvic floor disorders. Obstet Gynecol. 2005;106(6):1266–1271. doi: 10.1097/01.AOG.0000187303.43011.12. [DOI] [PubMed] [Google Scholar]
- 5.Willis S, Faridi A, Schelzig S, et al. Childbirth and incontinence: a prospective study on anal sphincter morphology and function before and early after vaginal delivery. Arch Surg. 2002;387:101–107. doi: 10.1007/s00423-002-0296-8. [DOI] [PubMed] [Google Scholar]
- 6.Zetterstrom J, Mellgren A, Jensen L L, et al. Effects of delivery on anal sphincter morphology and function. Dis Colon Rectum. 1999;42:1253–1260. doi: 10.1007/BF02234209. [DOI] [PubMed] [Google Scholar]
- 7.Varma A, Gunn J, Gardiner A, Lindow S W, Duthie G S. Obstetric anal sphincter injury: prospective evaluation of incidence 1999. Dis Colon Rectum. 1999;42:1537–1543. doi: 10.1007/BF02236202. [DOI] [PubMed] [Google Scholar]
- 8.Abramowitz L, Sobhani I, Ganansia R, et al. Are sphincter defects the cause of anal incontinence after vaginal delivery? Results of a prospective study. Dis Colon Rectum. 2000;43:590–598. doi: 10.1007/BF02235567. [DOI] [PubMed] [Google Scholar]
- 9.Chaliha C, Kalia V, Sultan A H, Monga A K, Stanton S L. Anal function: effect of pregnancy and delivery. Am J Obstet Gynecol. 2001;185:427–432. doi: 10.1067/mob.2001.115997. [DOI] [PubMed] [Google Scholar]
- 10.Snooks S J, Swash M, Setchell M, Henry M M. Injury to the innervation of the pelvic floor sphincter musculature in childbirth. Lancet. 1984;2:546–550. doi: 10.1016/s0140-6736(84)90766-9. [DOI] [PubMed] [Google Scholar]
- 11.Snooks S J, Swash M, Mathers S E, Henry M M. Effect of vaginal delivery on the pelvic floor—a five year follow up. Br J Surg. 1990;77:1358–1360. doi: 10.1002/bjs.1800771213. [DOI] [PubMed] [Google Scholar]
- 12.Rao S S, Patel R S. How useful are manometric tests of anorectal functions in the management of defecation disorders? Am J Gastroenterol. 1997;92:469–475. [PubMed] [Google Scholar]
- 13.Deen K I, Kumar D, Williams J G, Oliff J, Keighley M R. Anal sphincter defects: correlation between endoanal ultrasound and surgery. Ann Surg. 1993;218:201–205. doi: 10.1097/00000658-199308000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tjandra J J, Milsom J W, Schroeder T, Fazio V W. Endoluminal ultrasound is preferable to electromyography in mapping anal sphincter defects. Dis Colon Rectum. 1993;36:689–692. doi: 10.1007/BF02238597. [DOI] [PubMed] [Google Scholar]
- 15.Sultan A H, Loder P B, Bartram C I, Kamm M A, Hudson C N. Vaginal endosonography: new approach to image the undisturbed anal sphincter. Dis Colon Rectum. 1994;37:1296–1299. doi: 10.1007/BF02257800. [DOI] [PubMed] [Google Scholar]
- 16.Lee J H, Pretorius D H, Weinstein M, Guaderrama N M, Nager C W, Mittal R K. Transperineal three-dimensional ultrasound in evaluating anal sphincter muscles. Ultrasound Obstet Gynecol. 2007;30(2):201–209. doi: 10.1002/uog.4057. [DOI] [PubMed] [Google Scholar]
- 17.Voyvodic F, Rieger Na, Skinner S, et al. Endosonographic imaging of anal sphincter injuries: does the size of the tear correlate with the degree of dysfunction? Dis Colon Rectum. 2003;46:735–741. doi: 10.1007/s10350-004-6650-x. [DOI] [PubMed] [Google Scholar]
- 18.Sentovich S M, Wong W D, Blatchford G J. Accuracy and reliability of transanal ultrasound for anterior anal sphincter injury. Dis Colon Rectum. 1998;41:1000–1004. doi: 10.1007/BF02237390. [DOI] [PubMed] [Google Scholar]
- 19.Sultan A H, Kamm M A, Hudson C N, Nicholls J R, Bartram C I. Endosonography of the anal sphincters: normal anatomy and comparison with manometry. Clin Radiol. 1994;49:368–374. doi: 10.1016/s0009-9260(05)81819-7. [DOI] [PubMed] [Google Scholar]
- 20.Zetterstrom J P, Mellgren A, Madoff R, Kim D, Wong D. Perineal body measurements improves evaluation of anterior sphincter lesions during endo anal ultrasonography. Dis Colon Rectum. 1998;41:705–713. doi: 10.1007/BF02236256. [DOI] [PubMed] [Google Scholar]
- 21.Oberwalder M, Thaler K, Baig M, Dinnewitzer A, Efron J, Weiss E. Anal ultrasound and endo sonographic measurements of perineal body thickness: a new evaluation for fecal incontinence in females. Surg Endosc. 2004;18:650–654. doi: 10.1007/s00464-003-8138-5. [DOI] [PubMed] [Google Scholar]
- 22.Gold D M, Halligan S, Kmiot W A, Bartram C I. Intraobserver and interobserver agreement in anal endosonography. Br J Surg. 1999;86:371–375. doi: 10.1046/j.1365-2168.1999.01032.x. [DOI] [PubMed] [Google Scholar]
- 23.Williams A B, Bartram C I, Halligan S, Spencer J A, Nicholls R J, Kmiot W A. Anal sphincter damage after vaginal delivery using three dimensional endosonography. Obstet Gynecol. 2001;97:770–775. doi: 10.1016/s0029-7844(01)01318-7. [DOI] [PubMed] [Google Scholar]
- 24.Pfeifer J, Oliveira L. In: Wexner SD, Duthie GS, editor. Constipation, Etiology, Evaluation and Management. New York, NY: Thieme Medical Publishers; 2006. Anorectal manometry and the rectoalanal inhibitory reflex. pp. 71–78.
- 25.Jorge J M, Wexner S D. A practical guide to basic anorectal physiology investigations. Contemp Surg. 1996;43:214–224. [Google Scholar]
- 26.Schuster M M. Biofeedback treatment of gastrointestinal disorders. Med Clin North Am. 1977;61:907–912. doi: 10.1016/s0025-7125(16)31306-2. [DOI] [PubMed] [Google Scholar]
- 27.Pfeifer J, Oliveira L, Park U C, Gonzales A, Nogueras J J, Wexner S D. The relation of normal manometry to age and gender. Tech Coloproctol. 1996;4:10–13. [Google Scholar]
- 28.Ahran P, Faverdin C, Persoz B, et al. Relationship between viscoelastic properties of the rectum and anal pressures in man. J Appl Physiol. 1976;41:677–704. doi: 10.1152/jappl.1976.41.5.677. [DOI] [PubMed] [Google Scholar]
- 29.Hancke E, Schurholz M. Impaired rectal sensation in idiopathic fecal incontinence. Int J Colorectal Dis. 1987;2:146–148. doi: 10.1007/BF01647996. [DOI] [PubMed] [Google Scholar]
- 30.Rasmussen O O. Anorectal function. Dis Colon Rectum. 1994;37:386–403. doi: 10.1007/BF02053604. [DOI] [PubMed] [Google Scholar]
- 31.Hill J, Hosker G, Kiff E. Pudendal nerve terminal motor latency measurements: what they do and do not tell us. Br J Surg. 2002;89:1268–1269. doi: 10.1046/j.1365-2168.2002.02209.x. [DOI] [PubMed] [Google Scholar]
- 32.Ricciardi R, Mellgren A F, Madoff R D, et al. The utility of pudendal nerve terminal latencies in idiopathic incontinence. Dis Colon Rectum. 2006;49:852–857. doi: 10.1007/s10350-006-0529-y. [DOI] [PubMed] [Google Scholar]
- 33.Gilliland R, Altomare D, Moreira H, Oliveira L, Gilliland J, Wexner S. Pudendal neuropathy is predictive of failure following anterior overlapping sphincteroplasty. Dis Colon Rectum. 1998;41:1516–1522. doi: 10.1007/BF02237299. [DOI] [PubMed] [Google Scholar]