ABSTRACT
Because the incidence of colonic diverticulosis is high in the general population, incidental asymptomatic diverticulosis is commonly seen on radiology imaging studies. However, diagnostic imaging performed specifically for diverticular disease is essentially limited to imaging of suspected acute colonic diverticulitis (ACD) and its complications. The clinical diagnosis of ACD can be challenging, and imaging has become an essential tool to aid in diagnosis, assess severity of disease, and aid in treatment planning. Computed tomography (CT) has replaced contrast enema as the imaging procedure of choice for diverticulitis. Ultrasound has also been successfully used for diagnosis, and magnetic resonance imaging (MRI) has significant potential as a radiation-free imaging test for acute colonic diverticulitis.
Keywords: Acute colonic diverticulitis, diagnostic imaging, contrast enema, computed tomography, magnetic resonance imaging, ultrasound
PLAIN FILM RADIOGRAPHY
Plain film radiography is usually of little value in the assessment of suspected diverticulitis unless there is free intraperitoneal air from perforation, portal venous gas, or signs of bowel ileus or obstruction. However, these findings are nonspecific. Plain film radiography may fail to demonstrate the small contained perforations commonly encountered on computed tomography (CT) scans of patients with acute colonic diverticulitis, and is not sensitive for other complications such as abscess and fistula.
CONTRAST ENEMA
Until the 1980s when it was replaced by CT, contrast enema was the primary imaging modality for colonic diverticulitis. Today, barium enema is not performed in the acute setting due to the risk of perforation and peritonitis, even though several studies have shown it is safe if there are no clinical signs of perforation. Barium also causes artifacts that may preclude diagnosis if a CT scan is necessary. Water-soluble contrast enema (CE) can be safely performed with low morbidity and low cost, is widely available, and easy to perform, but is not as sensitive as CT (80 to 92% for CE vs up to 99% for CT).1,2 In the appropriate clinical setting, CE findings of fold thickening, segmental spasm, sinus tract, fistula, mass effect from abscess and extraluminal free or contained contrast may be demonstrated and can be diagnostic of acute diverticulitis. Contrast enemas are most useful in the setting of chronic diverticulitis,3 for follow-up in problem cases when diverticulitis is suspected but not seen on CT, or for assisting to differentiate diverticulitis from colon carcinoma. Delayed follow-up after acute symptoms have subsided should show preservation of the colonic mucosa to confirm diverticulitis. Involvement of longer segments of colon is also more typical of diverticulitis than malignancy.4 CE is a more time-consuming and involved exam for the patient when compared with other imaging modalities like CT, and generally it is not a good test to identify alternative diagnoses.
COMPUTED TOMOGRAPHY
The advent of CT has revolutionized the diagnosis and management of patients with diverticulitis. Multidetector CT is now considered the gold standard for assessing this disease. The preferred examination for evaluation of acute left lower quadrant pain and suspected diverticulitis is CT of the abdomen and pelvis with oral, rectal, and intravenous (IV) contrast. Acquisition of thin (1 mm or less) axial source images allows generation of high-quality reconstructed 3 mm axial and coronal images. Oral contrast is generally used, but often does not reach the sigmoid colon by the time imaging is performed. Rectal contrast may not be necessary for the evaluation of diverticulitis, but can improve colonic distention, opacify fistula tracts and increase the accuracy of the examination.5 Unless there are contraindications, intravenous (IV) contrast is routinely administered to assist with identification of abscesses and to demonstrate enhancement of the colonic wall. IV contrast is also useful in the diagnosis of alternative disease entities that mimic diverticulitis.6
Sigmoid diverticulitis is the most common cause of left lower quadrant pain in adults, and when imaging is required, CT is the most appropriate diagnostic imaging tool to confirm suspected left colonic diverticulitis. The American College of Radiology rates CT of the abdomen and pelvis with oral and/or colonic contrast as the preferred procedure in the setting of left lower quadrant pain with or without fever, except in women of childbearing age when ultrasound (US) is the initial preferred modality for unexplained left lower quadrant pain.7 When a patient has known diverticulosis and signs of uncomplicated diverticulitis, some physicians elect to treat the patient without imaging confirmation.
When imaging is necessary, CT is the test of choice because of its high sensitivity and specificity, reproducibility, availability, and it is less invasive when compared with CE. It can be performed in acutely ill patients. CT serves the following functions in the setting of left lower quadrant pain: (1) confirms the diagnosis of diverticulitis, (2) evaluates the severity and extent of disease, (3) allows for treatment planning of complications such as abscess, and (4) demonstrates other causes of abdominal pain that may mimic diverticulitis.
The reported sensitivity for diverticulitis on CT is 79 to 99%.8,9,10 In the literature, higher sensitivity and specificity has been reported more recently, commensurate with the advancement of CT technology, with most institutions now using multidetector CT scanning with better resolution and the ability to generate high-quality sagittal and coronal images.11 The two most common CT findings in uncomplicated diverticulitis are colonic wall thickening (wall thickness is greater than 3 mm on the short axis of the lumen) and pericolic fat stranding (Fig. 1).12,13 Often, these signs are associated with an identifiable inflamed diverticulum. Wall thickening associated with muscular hypertrophy from diverticulosis may be difficult to distinguish from that associated with diverticulitis when pericolonic inflammatory changes are absent (Fig. 2).2 The degree of fat stranding may vary from minimal “dirty fat” (Fig. 3) to severe inflammation and phlegmonous change. CT may fail to demonstrate early, mild cases of diverticulitis. Coronal reformatted images may be helpful to show mild pericolonic fat stranding associated with horizontally oriented segments of colon (Fig. 3B). The CT findings in complicated diverticulitis may include the presence of an abscess (defined as a fluid-containing mass with or without air and an enhancing wall), and contained or free extraluminal air bubbles or pockets (Fig. 4). Other complications such as bowel obstruction, hepatic abscess (Fig. 5), fistula and inferior mesenteric vein thrombosis can often be demonstrated with CT. Fistulas frequently communicate with an abscess or other hollow viscus, and colovesicular fistulas are the most common (Fig. 6). Fistula tracts can often be directly visualized if rectal contrast is administered.
Figure 1.
Diverticulitis. Axial computed tomography (CT) image of a 27-year-old man showing sigmoid wall thickening (arrow) and adjacent fat stranding (arrowhead).
Figure 2.

Diverticulosis. Axial computed tomography (CT) image in a 49-year-old man with diverticulosis. Rectally administered contrast helps define thickened sigmoid wall, staggered haustra, and diverticular outpouchings. Note absence of adjacent fat stranding.
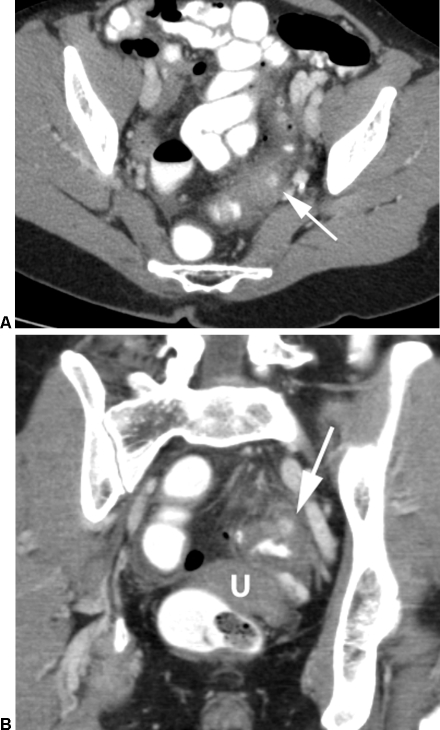
Figure 3.
Mild diverticulitis. Computed tomography (CT) images from a 54-year-old woman with fever, vomiting, and left lower quadrant pain. (A) Mild sigmoid wall thickening and fat stranding around an indistinct diverticulum (arrow). (B) Image in coronal plane shows the inflamed diverticulum (arrow) at the superior aspect of mid sigmoid (U denotes uterine fundus).
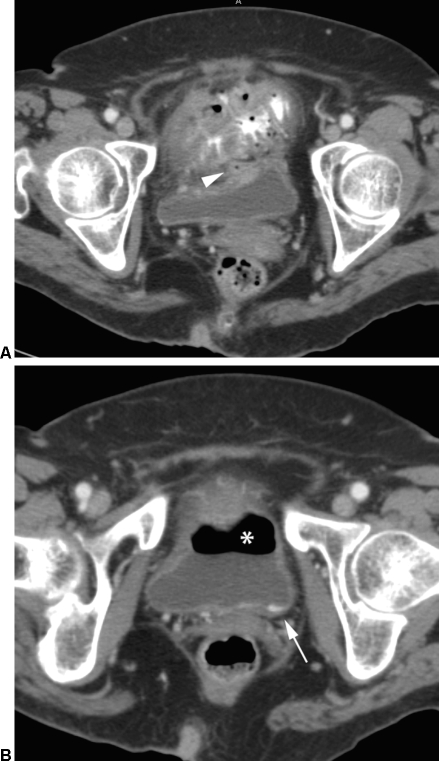
Figure 4.

Severe diverticulitis with perforation. Computed tomography (CT) image of a 44-year-old man presenting with abdominal pain, fever, and rebound tenderness. Axial image shows sigmoid wall thickening (asterisk) and extensive fat stranding as well as small amounts of free fluid, extraluminal air (arrowhead), and trace extravasated luminal contrast (arrow).
Figure 5.
Hepatic abscess. Axial computed tomography (CT) of 56-year-old man with sigmoid diverticulitis with multiloculated fluid collection (asterisk) in left lobe of liver, subsequently drained under CT guidance.
Figure 6.
Colovesicular fistula secondary to diverticulitis. Axial computed tomography (CT) images of an 82-year-old woman with fever and chills despite antibiotics for urinary tract infection. (A) Inflamed sigmoid with trace of air in fistula tract (arrowhead) extending to urinary bladder. (B) Ventral air (asterisk) and dependent traces of rectally administered contrast (arrow) within the urinary bladder.
CT findings may be used to direct clinical management. Some authors have associated CT findings with the Hinchey classification and modified Hinchey classification (adapted from Wasvary et al), showing how CT can effectively guide medical or surgical treatment.1,14,15,16,17,18
When abscesses are identified, CT-guided percutaneous drainage can preclude the need for surgery (Fig. 7) and can limit the need for multistage surgical procedures (Fig. 8).14,19,20 The size of diverticular abscesses is important in directing treatment based on expected outcomes.21,22 Patients with abscesses <3 cm can be treated with conservative management alone, and those with abscesses >3 cm benefit from percutaneous drainage with referral for surgical follow-up. Prior to catheter removal, a tube injection with iodinated contrast performed under fluoroscopy is recommended to exclude communication with the colon. Even in cases where communication to the colon is documented, continued percutaneous drainage can result in resolution of the fistula without surgical intervention (Fig. 7D). Abscess should be distinguished from cavities with broad communication to the colon (auto draining) and giant colonic diverticulum.
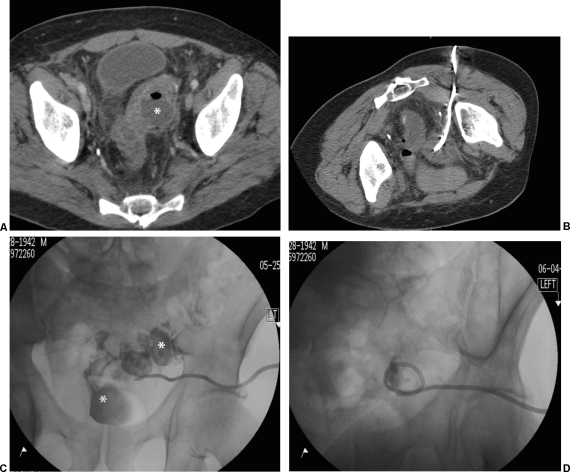
Figure 7.
Transgluteal percutaneous drainage of diverticular abscess. (A) Axial computed tomography (CT) image of 64-year-old man with fever and 3.5 cm rim enhancing fluid collection (asterisk) containing foci of air adjacent to sigmoid. (B) Image taken at conclusion of CT-guided percutaneous drain placement via transgluteal approach. (C) Fluoroscopic image from abscessogram at 1 week shows decompression of abscess cavity, but fistulous communication to rectosigmoid, outlined by contrast injected through a tube (asterisks). (D) Repeat tube injection shows decompressed abscess and lack of filling of rectosigmoid indicating resolution.
Figure 8.
Anterior percutaneous drainage of diverticular abscess. (A) Axial computed tomography (CT) of 55-year-old woman with large diverticular abscess in cul de sac (asterisk). Note foci of air within endometrial cavity (arrowhead). (B) Computed tomography (CT) image obtained at conclusion of percutaneous drainage procedure showing pigtail catheter in abscess cavity. (C) Oblique radiograph from abscessogram 10 days after procedure shows contrast injected through drain filling the residual abscess cavity (asterisk) with fistulous communication to right fallopian tube (arrow), endometrial cavity (arrowhead) and vagina (v). (D) Eventual follow-up CT after drain removal shows normal uterus (U) and resolved abscess.
Although seen more often in the younger age group, right colonic diverticulitis is uncommon, with the cecum involved in only 5% of patients. The preoperative diagnosis is challenging because there are no clinical signs and symptoms that are truly specific. The clinical presentation can mimic cholecystitis or appendicitis. CT findings in right colonic diverticulitis are similar to other areas of the colon (Fig. 9), with colon wall thickening and pericolonic fat stranding seen in all patients on one prospective study.23 Other individual findings included submucosal thickening in 60%, diverticula in 60%, an inflamed diverticulum in 30%, pericolonic phlegmon in 40%, ileocolic lymphadenopathy in 90%, and visualization of a normal appendix in 60%. Right colonic diverticulitis can be difficult to distinguish from colon carcinoma, especially if the inflamed diverticulum is not well visualized on CT. After supportive management, colonoscopy or contrast enema is recommended to confirm the diagnosis.
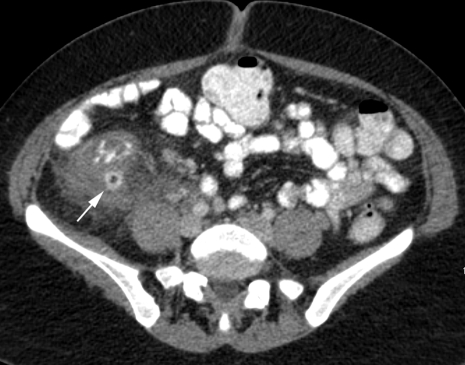
Figure 9.
Right-sided diverticulitis. Computed tomography (CT) image of a 30-year-old woman with right abdominal pain obtained after ultrasound showed a normal gallbladder. CT shows ascending colonic wall thickening with fat stranding around inflamed diverticulum (arrow).
CT is helpful in identifying and/or excluding other causes of abdominal pain when diverticulitis is not the etiology. Differential diagnosis includes neoplasm, appendicitis, epiploic appendagitis, ischemic colitis, and inflammatory bowel disease. Primary colon carcinoma is the main consideration in the differential for findings of diverticulitis on CT (Fig. 10) because it may present with eccentric or circumferential wall thickening, varying degrees of inflammation, and signs of obstruction.4,24,25,26 Perforated colon carcinoma may mimic diverticulitis. In general, fluid at the root of the mesentery and engorgement of regional vasculature suggests an inflammatory process, and pericolonic fat stranding is more typical of diverticulitis or other inflammation than of colon carcinoma. Colonic wall thickening is usually greater (measuring >2 cm) with neoplasm and is more often eccentric. Diverticulitis and neoplasm may both involve short segments of bowel; however, when a segment of >10 cm is involved, this is considered specific for diverticulitis. Left-sided pericolonic lymphadenopathy (lymph nodes measuring 1 cm or more in the short axis) are usually more specific for colon carcinoma, but are not uncommon with right colonic diverticulitis. The presence of diverticula in an involved segment suggests diverticulitis, but the high prevalence of diverticulosis in the general population dictates that the presence of diverticula cannot be used as a mitigating factor to exclude neoplasm. When the findings are equivocal for diverticulitis versus colon carcinoma, follow-up colonoscopy or imaging is suggested.
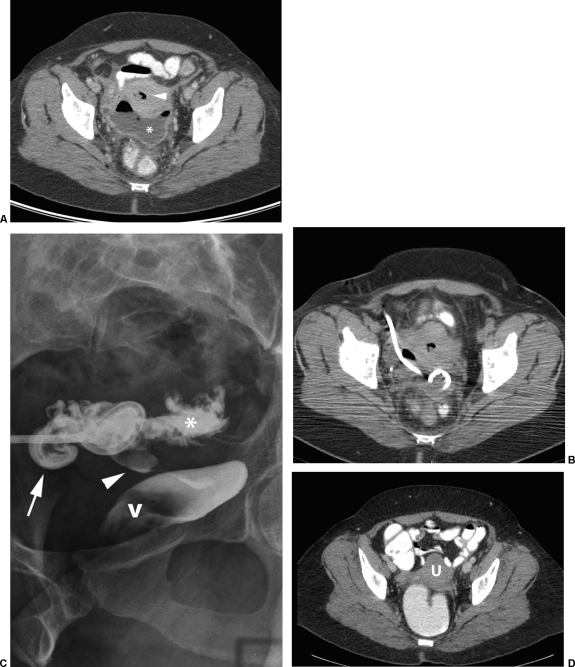
Figure 10.
Adenocarcinoma. Axial computed tomography (CT) image of a 42-year-old woman presenting with weight loss and lower abdominal pain shows marked wall thickening of sigmoid (asterisk) with left pelvic sidewall involvement. Note lack of fat stranding anterior to sigmoid.
Appendicitis is the main differential concern for right-sided diverticulitis, and is the most common cause of nongenitourinary right lower quadrant pain. Small bowel pathology can also mimic diverticulitis, and CT is helpful to distinguish these patients. Epiploic appendagitis is a nonsurgical entity that results from torsion and venous occlusion of an epiploic appendage, and patients present with signs and symptoms that mimic diverticulitis. A CT scan in these patients reveals an ovoid fat attenuation mass with surrounding inflammation on the antimesenteric side, usually in the absence of colonic wall thickening (Fig. 11).
Figure 11.
Epiploic appendagitis. Axial computed tomography (CT) image of a 42-year-old man with acute left lower quadrant pain caused by epiploic appendagitis, with ovoid fat attenuation structure (arrow) with adjacent fat stranding, anterior to the normal proximal sigmoid colon.
ULTRASOUND
Transabdominal sonography is an alternative technique for evaluating patients with suspected diverticulitis, but is not as widely used as a first imaging test in the United States. Those who advocate the use of US stress its lower cost and wider availability over other imaging modalities. It is considered safer for patients because it lacks radiation exposure and there is no need for IV contract administration. However, US is operator dependent, is not as accurate as CT for identifying alternative diagnoses, and is not as useful for surgical planning when intervention is required. In a meta-analysis of the test accuracy of ultrasound, Laméris et al found that there were no significant differences in the diagnostic accuracy of US versus CT in diagnosing acute colonic diverticulitis.27 Graded compression US is used to reduce inconclusive findings from overlying bowel loops, and has been shown to have a sensitivity of 77 to 98% and a specificity of 80 to 99%.28,29 US can accurately measure bowel wall thickness, demonstrate pericolonic fat inflammation, and identify abscess.30,31 Although US can detect some complications of diverticulitis and occasionally demonstrate alternative diagnoses, it is not as sensitive as CT for these indications.
MAGNETIC RESONANCE IMAGING
Magnetic resonance imaging (MRI) can effectively diagnose acute diverticulitis, with reported sensitivity of 86 to 94% and specificity of 88 to 92%.32,33 It is likely that continually improving MRI techniques may result in higher sensitivity and specificity in the future. Buckley et al described MRI findings in patients with acute colonic diverticulitis, identifying findings similar to CT: bowel wall thickening, pericolic stranding, presence of diverticula, and complications (Fig. 12).34 MRI is also comparable with CT in its ability to identify alternative diagnoses. Similar to ultrasound, MRI has the benefit of no radiation exposure, but because it is operator independent, it may be more applicable as the test of choice as the medical community becomes more aware of the risks of radiation exposure and seeks alternative imaging modalities to CT. The inability to percutaneously drain abscesses using MRI has been described as a limitation of this modality. Certainly, MRI-guided procedures have become the mainstay for other organ systems (breast, brain) and should be easily extrapolated to the abdomen in the near future.
Figure 12.
Magnetic resonance image (MRI) of right-sided diverticulitis. Axial MRI of a 30-year-old woman with right abdominal pain obtained after ultrasound showed a normal gallbladder (same patient as Fig. 9). T2-weighted MRI at same level as CT shows ascending colonic wall thickening with fat stranding around inflamed diverticulum (arrow).
CONCLUSION
The role of imaging evaluation in acute colonic diverticulitis is to confirm the diagnosis, evaluate the severity and extent of disease, exclude alternative diagnoses, and allow for treatment planning. CT is currently considered the imaging modality of choice for evaluation of patients with suspected acute diverticulitis. Although CT has high accuracy and sensitivity/specificity, it is scrutinized because of the risk of ionizing radiation to patients.35 Because the recurrence rate of diverticulitis is high, it is not uncommon for patients in U.S. hospitals to undergo many CT scans with lifetime cumulative radiation doses of 100 mSv or higher.36,37 As patient safety concerns related to radiation exposure continue to gain a higher profile, there will likely be a shift to using radiation-free imaging modalities to evaluate acute abdominal pathology, especially in the younger population. US is accurate, inexpensive and widely available, but is operator dependent and unlikely to gain momentum as a frontline imaging modality for colonic diverticulitis in the United States. As techniques improve, MRI may supplant CT as the test of choice for ACD because it is accurate, operator independent, and lacks ionizing radiation. Some authors are already recommending the use of MRI (over CT) in patients younger than 60 years.32 Randomized prospective trials looking at all three modalities (CT, US, MRI) will be helpful to guide the appropriate utilization of imaging for evaluating acute colonic diverticulitis.
REFERENCES
- 1.Baker M E. Imaging and interventional techniques in acute left-sided diverticulitis. J Gastrointest Surg. 2008;12(8):1314–1317. doi: 10.1007/s11605-008-0490-2. [DOI] [PubMed] [Google Scholar]
- 2.Balthazar E J, Megibow A, Schinella R A, Gordon R. Limitations in the CT diagnosis of acute diverticulitis: comparison of CT, contrast enema, and pathologic findings in 16 patients. AJR Am J Roentgenol. 1990;154(2):281–285. doi: 10.2214/ajr.154.2.2105015. [DOI] [PubMed] [Google Scholar]
- 3.Sheiman L, Levine M S, Levin A A, et al. Chronic diverticulitis: clinical, radiographic, and pathologic findings. AJR Am J Roentgenol. 2008;191(2):522–528. doi: 10.2214/AJR.07.3597. [DOI] [PubMed] [Google Scholar]
- 4.Hulnick D H, Megibow A J, Balthazar E J, Gordon R B, Surapenini R, Bosniak M A. Perforated colorectal neoplasms: correlation of clinical, contrast enema, and CT examinations. Radiology. 1987;164(3):611–615. doi: 10.1148/radiology.164.3.3615859. [DOI] [PubMed] [Google Scholar]
- 5.Rao P M, Rhea J T, Novelline R A, et al. Helical CT with only colonic contrast material for diagnosing diverticulitis: prospective evaluation of 150 patients. AJR Am J Roentgenol. 1998;170(6):1445–1449. doi: 10.2214/ajr.170.6.9609151. [DOI] [PubMed] [Google Scholar]
- 6.Jang H J, Lim H K, Lee S J, Lee W J, Kim E Y, Kim S H. Acute diverticulitis of the cecum and ascending colon: the value of thin-section helical CT findings in excluding colonic carcinoma. AJR Am J Roentgenol. 2000;174(5):1397–1402. doi: 10.2214/ajr.174.5.1741397. [DOI] [PubMed] [Google Scholar]
- 7.American College of Radiology ACR Appropriateness Criteria. (2008) Available at: http://www.acr.org/SecondaryMainMenuCategories/qualilty_safety/app_criteria.aspx. Accessed April 16, 2009. Available at: http://www.acr.org/SecondaryMainMenuCategories/qualilty_safety/app_criteria.aspx
- 8.Köhler L, Sauerland S, Neugebauer E, The Scientific Committee of the European Association for Endoscopic Surgery Diagnosis and treatment of diverticular disease: results of a consensus development conference. Surg Endosc. 1999;13(4):430–436. doi: 10.1007/s004649901007. [DOI] [PubMed] [Google Scholar]
- 9.Cho K C, Morehouse H T, Alterman D D, Thornhill B A. Sigmoid diverticulitis: diagnostic role of CT—comparison with barium enema studies. Radiology. 1990;176(1):111–115. doi: 10.1148/radiology.176.1.2191360. [DOI] [PubMed] [Google Scholar]
- 10.Rao P M, Rhea J T. Colonic diverticulitis: evaluation of the arrowhead sign and the inflamed diverticulum for CT diagnosis. Radiology. 1998;209(3):775–779. doi: 10.1148/radiology.209.3.9844673. [DOI] [PubMed] [Google Scholar]
- 11.Farag S M, Wustner M, Sturm J, et al. Primary diagnostics of acute diverticulitis of the sigmoid. Ultraschall Med. 2004;25:342–347. doi: 10.1055/s-2004-813381. [DOI] [PubMed] [Google Scholar]
- 12.Kircher M F, Rhea J T, Kihiczak D, Novelline R A. Frequency, sensitivity, and specificity of individual signs of diverticulitis on thin-section helical CT with colonic contrast material: experience with 312 cases. AJR Am J Roentgenol. 2002;178(6):1313–1318. doi: 10.2214/ajr.178.6.1781313. [DOI] [PubMed] [Google Scholar]
- 13.Werner A, Diehl S J, Farag-Soliman M, Düber C. Multi-slice spiral CT in routine diagnosis of suspected acute left-sided colonic diverticulitis: a prospective study of 120 patients. Eur Radiol. 2003;13(12):2596–2603. doi: 10.1007/s00330-003-1887-7. [DOI] [PubMed] [Google Scholar]
- 14.Kaiser A M, Jiang J K, Lake J P, et al. The management of complicated diverticulitis and the role of computed tomography. Am J Gastroenterol. 2005;100(4):910–917. doi: 10.1111/j.1572-0241.2005.41154.x. [DOI] [PubMed] [Google Scholar]
- 15.Hinchey E J, Schaal P G, Richards G K. Treatment of perforated diverticular disease of the colon. Adv Surg. 1978;12:85–109. [PubMed] [Google Scholar]
- 16.Wasvary H, Turfah F, Kadro O, Beauregard W. Same hospitalization resection for acute diverticulitis. Am Surg. 1999;65(7):632–635. discussion 636. [PubMed] [Google Scholar]
- 17.Ambrosetti P, Becker C, Terrier F. Colonic diverticulitis: impact of imaging on surgical management–a prospective study of 542 patients. Eur Radiol. 2002;12(5):1145–1149. doi: 10.1007/s00330-001-1143-y. [DOI] [PubMed] [Google Scholar]
- 18.Ambrosetti P. Acute diverticulitis of the left colon: value of the initial CT and timing of elective colectomy. J Gastrointest Surg. 2008;12(8):1318–1320. doi: 10.1007/s11605-008-0489-8. [DOI] [PubMed] [Google Scholar]
- 19.Lohrmann C, Ghanem N, Pache G, Makowiec F, Kotter E, Langer M. CT in acute perforated sigmoid diverticulitis. Eur J Radiol. 2005;56(1):78–83. doi: 10.1016/j.ejrad.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 20.Mueller P R, Saini S, Wittenburg J, et al. Sigmoid diverticular abscesses: percutaneous drainage as an adjunct to surgical resection in 24 cases. Radiology. 1987;164(2):321–325. doi: 10.1148/radiology.164.2.3602369. [DOI] [PubMed] [Google Scholar]
- 21.Siewert B, Tye G, Kruskal J, et al. Impact of CT-guided drainage in the treatment of diverticular abscesses: size matters. AJR Am J Roentgenol. 2006;186(3):680–686. doi: 10.2214/AJR.04.1708. [DOI] [PubMed] [Google Scholar]
- 22.Sarma D, Longo W E, NDSG Diagnostic imaging for diverticulitis. J Clin Gastroenterol. 2008;42(10):1139–1141. doi: 10.1097/MCG.0b013e3181886ed4. [DOI] [PubMed] [Google Scholar]
- 23.Lee I K, Jung S E, Gorden D L, et al. The diagnostic criteria for right colonic diverticulitis: prospective evaluation of 100 patients. Int J Colorectal Dis. 2008;23(12):1151–1157. doi: 10.1007/s00384-008-0512-2. [DOI] [PubMed] [Google Scholar]
- 24.Padidar A M, Jeffrey R B, Jr, Mindelzun R E, Dolph J F. Differentiating sigmoid diverticulitis from carcinoma on CT scans: mesenteric inflammation suggests diverticulitis. AJR Am J Roentgenol. 1994;163(1):81–83. doi: 10.2214/ajr.163.1.8010253. [DOI] [PubMed] [Google Scholar]
- 25.Chintapalli K N, Chopra S, Ghiatas A A, Esola C C, Fields S F, Dodd G D., III Diverticulitis versus colon cancer: differentiation with helical CT findings. Radiology. 1999;210(2):429–435. doi: 10.1148/radiology.210.2.r99fe48429. [DOI] [PubMed] [Google Scholar]
- 26.Goh V, Halligan S, Taylor S A, Burling D, Bassett P, Bartram C I. Differentiation between diverticulitis and colorectal cancer: quantitative CT perfusion measurements versus morphologic criteria–initial experience. Radiology. 2007;242(2):456–462. doi: 10.1148/radiol.2422051670. [DOI] [PubMed] [Google Scholar]
- 27.Laméris W, Randen A van, Bipat S, Bossuyt P M, Boermeester M A, Stoker J. Graded compression ultrasonography and computed tomography in acute colonic diverticulitis: meta-analysis of test accuracy. Eur Radiol. 2008;18(11):2498–2511. doi: 10.1007/s00330-008-1018-6. [DOI] [PubMed] [Google Scholar]
- 28.Pradel J A, Adell J F, Taourel P, Djafari M, Monnin-Delhom E, Bruel J M. Acute colonic diverticulitis: prospective comparative evaluation with US and CT. Radiology. 1997;205(2):503–512. doi: 10.1148/radiology.205.2.9356636. [DOI] [PubMed] [Google Scholar]
- 29.Schwerk W B, Schwarz S, Rothmund M. Sonography in acute colonic diverticulitis. A prospective study. Dis Colon Rectum. 1992;35(11):1077–1084. doi: 10.1007/BF02252999. [DOI] [PubMed] [Google Scholar]
- 30.Ripollés T, Agramunt M, Martínez M J, Costa S, Gómez-Abril S A, Richart J. The role of ultrasound in the diagnosis, management and evolutive prognosis of acute left-sided colonic diverticulitis: a review of 208 patients. Eur Radiol. 2003;13(12):2587–2595. doi: 10.1007/s00330-003-1861-4. [DOI] [PubMed] [Google Scholar]
- 31.Vijayaraghavan S B. High-resolution sonographic spectrum of diverticulosis, diverticulitis, and their complications. J Ultrasound Med. 2006;25(1):75–85. doi: 10.7863/jum.2006.25.1.75. [DOI] [PubMed] [Google Scholar]
- 32.Heverhagen J T, Sitter H, Zielke A, Klose K J. Prospective evaluation of the value of magnetic resonance imaging in suspected acute sigmoid diverticulitis. Dis Colon Rectum. 2008;51(12):1810–1815. doi: 10.1007/s10350-008-9330-4. [DOI] [PubMed] [Google Scholar]
- 33.Ajaj W, Ruehm S G, Lauenstein T, et al. Dark-lumen magnetic resonance colonography in patients with suspected sigmoid diverticulitis: a feasibility study. Eur Radiol. 2005;15(11):2316–2322. doi: 10.1007/s00330-005-2862-2. [DOI] [PubMed] [Google Scholar]
- 34.Buckley O, Geoghegan T, McAuley G, Persaud T, Khosa F, Torreggiani W C. Pictorial review: magnetic resonance imaging of colonic diverticulitis. Eur Radiol. 2007;17(1):221–227. doi: 10.1007/s00330-006-0236-z. [DOI] [PubMed] [Google Scholar]
- 35.Brenner D J, Hall E J. Computed tomography–an increasing source of radiation exposure. N Engl J Med. 2007;357(22):2277–2284. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 36.Aldrich J E, Chang S D, Bilawich A M, Mayo J R. Radiation dose in abdominal computed tomography: the role of patient size and the selection of tube current. Can Assoc Radiol J. 2006;57(3):152–158. [PubMed] [Google Scholar]
- 37.Aldrich J E, Bilawich A M, Mayo J R. Radiation doses to patients receiving computed tomography examinations in British Columbia. Can Assoc Radiol J. 2006;57(2):79–85. [PubMed] [Google Scholar]