Abstract
INTRODUCTION
Pemphigoid gestationis, also known as herpes gestationis, is a rare autoimmune blistering disease associated with pregnancy. It usually occurs during the second or third trimester, but it may be present at any stage of pregnancy or the puerperium. The clinical, histologic, and immunopathological features of pemphigoid gestationis are similar to those of the pemphigoid group of disorders.
METHODS
We hereby report seven patients who were diagnosed with pemphigoid gestationis and followed at the Autoimmune Blistering Disease Clinic in the Department of Dermatology of the University of Sao Paulo Medical School between 1996 and 2008.
DISCUSSION
Demographic and clinical findings, such as median age, sites of involvement, and gestational age of onset or C3 of our patients, coincide with those described in previous reports. The majority of patients (85%) exhibited complement C3 and immunoglobulin G (IgG) deposition along the basement membrane zone (BMZ) on immunofluorescence. Herpes gestationis factor (HG) factor was postitive in four out of six patients (67%), and three out of five patients recognized the bullous pemphigoid recombinant antigen (BP180) by ELISA.
CONCLUSION
This study revealed a good outcome of the newborns from pemphigoid gestationis affected mothers, based on the absence of pemphigoid gestationis cutaneous lesions, mean birth weight, and normal Apgar scores and gestational age at birth.
Keywords: Autoimmunity, Dermatoses of pregnancy, Herpes gestationis, Blistering disease, BP180
INTRODUCTION
Pemphigoid gestationis (PG), also known as herpes gestationis, is a rare autoimmune blistering disease associated with pregnancy. It usually occurs during the second or third trimester of pregnancy, but it may be present at any stage of pregnancy or during the puerperium. It has an estimated incidence of 1 in 50,000 (general population) worldwide. Its clinical, histopathologic, and immunopathological features are similar to those of the pemphigoid group of blistering disorders. PG and bullous pemphigoid (BP) auto-antibodies bind to a common antigenic site within the non-collagenous domain (NC16A) of the transmembrane 180 kDa BP2 antigen.1–3
Classically, PG presents as erythematous urticarial plaques that can subsequently develop into tense blisters. The periumbilical area is usually the first site involved. Pruritus is an important symptom associated with the onset of disease.1
We report on seven patients who were diagnosed with pemphigoid gestationis and followed at the Autoimmune Blistering Disease Clinic in the Department of Dermatology of the University of Sao Paulo Medical School between 1996 and 2008, focusing on their clinical, histological, and immunopathological features.
METHODS
We reviewed the records of PG patients who were diagnosed with pemphigoid gestationis and followed at the Autoimmune Blistering Disease Clinic, Department of Dermatology, University of São Paulo Medical School between 1996 and 2008. Demographic data (age), clinical features including timing of disease onset, site of lesions, and symptoms (pruritus) were analyzed, and laboratory evaluation, included histological examination, direct and indirect immunofluorescence techniques (DIF and IIF), with the complement fixation test (herpes gestationis factor), and enzyme-linked immunosorbent assay (ELISA) for the detection of anti BP-180 antibodies).
RESULTS
Demographic Data and Clinical Presentations
Seven cases of PG were diagnosed in our department between 1996 and 2008, and the patient age ranged from 19 to 39 years (mean, 30.3 years). Disease onset was reported in the second trimester of pregnancy in four patients and in the third trimester of pregnancy in three patients. One patient had a flare up of symptoms during the puerperium. Main sites of involvement were lower limbs (mainly thighs), forearms, trunk, and abdomen (Figure 1). One patient had initial lesions that resembled erythema multiforme on her palms and soles. None of the patients had facial or mucosal lesions. Pruritus was the main complaint in all patients. No history of associated autoimmune disorders (such as Grave’s disease) or malignancies was present in any patient. Five patients developed the disease after previous normal pregnancies and two had PG during their first pregnancy. One of the latter had three subsequent pregnancies also affected by the disease. There was no mention in her chart of a worsening of her clinical features or an earlier onset of her symptoms in each subsequent pregnancy as described in the literature.
Figure 1.
Pemphigoid Gestationis: Pruritic urticarial lesions and tense blisters on the trunk
Demographic, clinical, and treatment data are compiled in Table 1.
Table 1.
Pemphigoid gestationis: demographic, clinical and treatment data
| Patient | Age (years) | Obstetric history | Previous affected pregnancies | Onset of symptoms | Sites of involvement | Treatment | Remission of lesions |
|---|---|---|---|---|---|---|---|
| 1 | 33 | IVG IIP IIA | − | 2nd trimester | Trunk, abdomen, upper arms and legs | Prednisone | Two months after delivery |
| 2 | 19 | IIG IIP 0A | − | 2nd trimester | Trunk, abdomen, upper arms and legs | Prednisone | 15 days after delivery. Pre menstrual exacerbations for 6 months. |
| 3 | 23 | IG IP 0A | − | 3rd trimester | Abdomen, thighs, trunk, upper arms, legs, palms and soles | Prednisone | 45 days after delivery (Flare up after birth) |
| 4 | 32 | IIG IIP 0A | − | 3rd trimester | Upper arms, trunk, abdomen and thighs | Prednisone and azathioprine | One year after delivery |
| 5 | 35 | VG VP 0A | − | 3rd trimester | Trunk, abdomen, and legs | Prednisone | After birth, follow up not available |
| 6 | 31 | IIIG IIIP 0A | − | 2nd trimester | Abdomen, upper arms and legs | Prednisone | One month after delivery |
| 7 | 39 | VIIG VP IIA | + All previous pregnancies, except for the two first trimester abortions | 2nd trimester | Trunk, abdomen, upper arms and legs | Only topical corticosteroids and antihistaminic agents | After birth, follow up not available |
Histopathological and Immunofluorescence Findings
The histopathologic (HE) and immunofluorescence (IF) findings are presented in Table 2.
Table 2.
Pemphigoid gestationis: histopathology, direct immunofluorescence, indirect complement-added imunofluorescence (HG factor) and BP180 ELISA results (cutoff index ELISA: ≥ 9)
| Patient | Histopathology | DIF | HG factor | Elisa BP180 |
|---|---|---|---|---|
| 1 | Subepidermal bulla with eosinophilia | C3 | + | Not performed |
| 2 | Eosinophilic inflammatory infiltrate at the dermis | C3 and IgG | + | + (70) |
| 3 | Subepidermal bulla with eosinophilia | C3 and IgG | + | −(out of activity) |
| 4 | Not available | C3 | − | + (184) |
| 5 | Subepidermal bulla with eosinophilia | C3 | Not performed | Not performed |
| 6 | Eosinophilic inflammatory infiltrate at the dermis | C3 | − | − |
| 7 | Eosinophilic inflammatory infiltrate at the dermis. | IgM | + | + (130) |
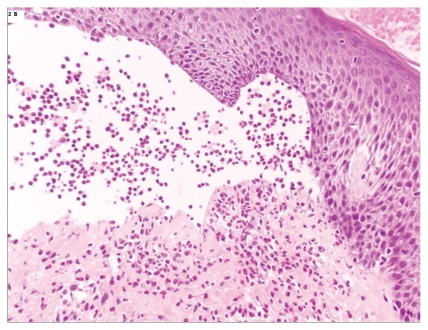
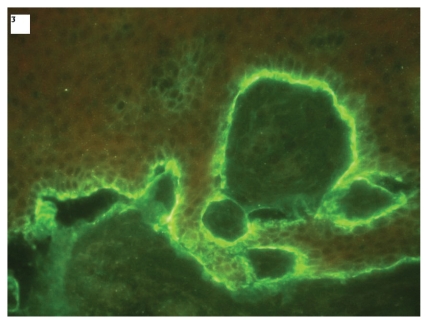
Subepidermal bullae with eosinophilic infiltrates (Figure 2) were found in three out of the six patients who underwent histopathological evaluation, and inflammatory eosinophilic infiltrates were found at the dermis in the other three patients. DIF staining revealed linear C3 deposition along the BMZ in four out of seven patients (Figure 3). Two patients exhibited linear C3 and IgG deposits along the BMZ and one patient exhibited linear IgM deposits along the BMZ.
Figure 2.
Pemphigoid Gestationis: Histopathology (HE): subepidermal bulla with eosinophils (X40)
Figure 3.
Pemphigoid Gestationis: Direct immunofluorescence of peri-lesional skin, showing linear deposition of complement (C3) along the BMZ (X40)
The HG factor (indirect complement-added IF) was positive in four out of six patients. Two umbilical cord blood samples were collected at the time of delivery for each subject, and circulating IgG anti-BP180 antibodies were found in one sample. Five patients underwent ELISA testing for the presence of anti-BP180, and three out of five patients tested positive for anti-BP180 and had high titers. The assayed sample from one of the patients that was negative for the presence of anti-BP180 by ELISA had been collected five years after delivery, whereas the other samples were collected while the patients had active disease.
Evaluation of the Newborns
The Apgar scores and weights of the newborns were available in six out of seven PG patients’ charts. None of them had low Apgar scores (defined as below a minimum score of eight at the first minute of life and below a minimum score of nine at the tenth minute of life). Only one newborn had low birth weight, but the mother had other clinical disorders (gestational diabetes and essential hypertension) that might have affected the birth weight. One newborn was premature (35 weeks of pregnancy) due to chorioamnionitis secondary to early amniorrhexis. None of the newborns had PG lesions.
Treatment
Systemic corticosteroids (prednisone, initial dose: 0.5–1.0 mg/kg/day) were administered to six out of the seven patients. Each patient was treated for as long as active lesions were observed. Corticosteroids were gradually withdrawn after the lesions had cleared. One patient reported premenstrual exacerbations while withdrawing from corticosteroids. Mild topical corticosteroids and antihistaminic agents were necessary to control symptoms in only one patient. Six out of seven patients had complete remission by two months after delivery. Only one patient had a prolonged course of the disease: she achieved complete remission one year after delivery. Of note, she was the only patient that received adjuvant immunosuppressant therapy (azathioprine 2 mg/kg/day), which was initiated after she had finished breast feeding.
DISCUSSION
PG is a rare autoimmune pregnancy-associated blistering disease. Pathogenesis of PG involves the production of auto-antibodies, mainly of the IgG1 subclass, that bind to the extracellular NC16A domain of the carboxyl terminus of the 180 kDa bullous pemphigoid antigen (BPAg2). Once bound, the antigen-antibody complex fixes complement via the classical complement pathway. Complement activation leads to chemotaxis of eosinophils to the site of the antigen-antibody complex on the BMZ. Once there, the eosinophils degranulate, and are thought to damage the dermal-epidermal junction, leading to blister formation. The initiating immunological event that stimulates this immune response remains unknown.5
The clinical presentation and course of PG is variable. Most cases remit in the first several weeks after delivery. Exacerbations have been documented during subsequent pregnancies, during menstruation, and with oral contraceptive use.1,5,6
Our demographic and clinical results (e.g., median age, sites of involvement, and gestational age at onset) are similar to those described by other authors.1–6 It is important to highlight that, in our study no infants were affected by PG lesions. The newborns born to PG-affected mothers had good outcomes in this study; the mean birth weights, Apgar scores, and gestational age at birth of these infants were all normal. A review of the recent literature revealed findings similar to those of our study: there is not an increase in maternal or fetal morbidity in mothers with PG.1–5
One of the most important conditions from which PG must be differentiated is polymorphic urticarial papules and plaques of pregnancy (PUPPP).2,7 PUPPP is a pruritic eruption of unknown etiology and resembles non-bullous PG. Differentiation between PG and PUPPP depends on demonstration of the presence of anti-BMZ auto-antibodies by immunofluorescence, immunoblotting, or ELISA in patients with PG. The precise diagnosis of these two conditions is relevant, once PUPPP is usually treated with topical emollients and corticosteroids, poses no risk to the newborn, and rarely recurs during future pregnancies,6,7 whereas PG often requires systemic treatment, may affect the newborn, and often recurs (as high as 92% of the time) during subsequent pregnancies,1 with possible earlier onset of the disease and worsening of the clinical symptoms.1 In light of this, correct diagnosis is important to allow for early control of the disease and appropriate counseling of the mother regarding her course of treatment and risk of developing PG during future pregnancies.
DIF staining is the preferred method for routine diagnosis of PG.2 Serological analysis, including testing for the presence of HG factor and BP180 ELISA, played a key role in the diagnosis of one patient in our evaluation. Previous studies have similarly described the clinical utility of serological analysis. Recent findings have demonstrated the high sensitivity and specificity of BP180 ELISA tests for diagnosing PG.7–9 Aoyama et al.10 described an association between BP180 ELISA titers and disease severity as well as the important role that anti-BP180 titers may play in therapeutic planning.
Regarding treatment, the majority of our patients were controlled with high doses of systemic corticosteroids. One patient received azathioprine due to the chronic course of her disease, and the lesions lasted for over one year. Prolonged courses of PG,11–14 as well as transformation of the disease into BP 15 have been described. Many attempts to differentiate chronic PG from BP have been made: PG is associated with HLA DR3 and DR4, while BP is associated with HLA-DQ3.2,16,17 In addition, a higher prevalence of C3 over IgG deposition along the BMZ indicates the presence of PG.16 However, the differential diagnosis between the two conditions is often difficult.
Brazil is a country known as endemic for pemphigus foliaceus, which suggests an environmental role in the pathogenesis of this cutaneous blistering autoimmune disease. Therefore, the behavior of other autoimmune blistering diseases, such as PG in this country is relevant. Our study revealed that demographic data, clinical presentation, laboratory findings, and treatment of our PG patients shared many similarities with many other studies performed worldwide, indicating that environmental triggers are seldom related to the pathogenesis of PG.
REFERENCES
- 1.Jenkis RE, Hern S, Black MM. Clinical features and management of 87 patients with pemphigoid gestationis. Clin Exp Dermatol. 1999;24:255–9. doi: 10.1046/j.1365-2230.1999.00472.x. [DOI] [PubMed] [Google Scholar]
- 2.Castro LA, Lundell RB, Krause PK, Gibson LE. Clinical experience in pemphigoid gestationis: report of 10 cases. J Am Acad Dermatol. 2006;55:823–8. doi: 10.1016/j.jaad.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 3.Lin MS, Arteaga LA, Diaz LA. Herpes Gestationis. Clin Dermatol. 2001;19:697–702. doi: 10.1016/s0738-081x(00)00195-4. [DOI] [PubMed] [Google Scholar]
- 4.Bedocs PM, Kumar V, Mahon MJ. Pemphigoid gestationis: a rare case and review. Arch Gynecol Obstet. 2009;279:235–8. doi: 10.1007/s00404-008-0687-3. [DOI] [PubMed] [Google Scholar]
- 5.Al-Fouzan AS, Galadari I, Oumeish OY. Herpes Gestationis (Pemphigoid Gestationis) Clin Dermatol. 2006;24:109–12. doi: 10.1016/j.clindermatol.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 6.Engineer L, Bhol K, Ahmed AR. Pemphigoid gestationis: a review. Am J Obstet Gynecol. 2000;183:483–91. doi: 10.1067/mob.2000.105430. [DOI] [PubMed] [Google Scholar]
- 7.Powell AM, Sakuma-Oyama Y, Oyama N, Albert S, Bhogal B, Kancko F, et al. Usefulness of BP180 NC16a enzyme-linked immunosorbent assay in the serodiagnosis of pemphigoid gestationis and in differentiating between pemphigoid gestationis and pruritic urticarial papules and plaques of pregnancy. Arch Dermatol. 2005;141:705–10. doi: 10.1001/archderm.141.6.705. [DOI] [PubMed] [Google Scholar]
- 8.Barnadas MA, Rubiales MV, González MJ, Puig L, García P, Baselga E, et al. Enzyme-linked immunosorbent assay (ELISA) and indirect immunofluorescence testing in a bullous pemphigoid and pemphigoid gestationis. Int J Dermatol. 2008;47:1245–9. doi: 10.1111/j.1365-4632.2008.03824.x. [DOI] [PubMed] [Google Scholar]
- 9.Sitaru C, Powell J, Messer G, Bröcker EB, Wojnarowska F, Zillikens D. Immunoblotting and enzyme-linked immunosorbent assay for the diagnosis of pemphigoid gestationis. Obstet Gynecol. 2004;103:757–63. doi: 10.1097/01.AOG.0000115506.76104.ad. [DOI] [PubMed] [Google Scholar]
- 10.Aoyama Y, Asai K, Hioki K, Funato M, Kondo N, Kitajima Y. Herpes gestationis in a mother and newborn: immunoclinical perspectives based on a weekly follow-up of the enzyme-linked immunosorbent assay index of a bullous pemphigoid antigen noncollagenous domain. Arch Dermatol. 2007;143:1168–72. doi: 10.1001/archderm.143.9.1168. [DOI] [PubMed] [Google Scholar]
- 11.Holmes RC, Black MM, Jureka W. Clues to the aetiology and pathogenesis of herpes gestationis. Br J Dermatol. 1983;109:131–9. doi: 10.1111/j.1365-2133.1983.tb07073.x. [DOI] [PubMed] [Google Scholar]
- 12.Fine J, Omura EF. Herpes gestationis: persistent disease activity 11 years post partum. Arch Dermatol. 1985;121:924–6. doi: 10.1001/archderm.121.7.924. [DOI] [PubMed] [Google Scholar]
- 13.Castle SP, Mather-Mondrey M, Bennion S. Chronic herpes gestationis and antiphospholipid antibody syndrome successfully treated with cyclophosphamide. J Am Acad Dermatol. 1996;34:333–6. doi: 10.1016/s0190-9622(07)80003-x. [DOI] [PubMed] [Google Scholar]
- 14.Holmes RC, Williamson DM, Black MM. Herpes gestationis pesisting for 12 years post partum. Arch Dermatol. 1986;122:375–6. [PubMed] [Google Scholar]
- 15.Jenkins RE, Vaughan Jones SA, Black MM. Conversion of pemphigoid gestationis to bullous pemphigoid-two refractory cases high lighting this association. Br J Dermatol. 1995;135:595–8. [PubMed] [Google Scholar]
- 16.Amato L, Mei S, Gallerani I, Moretti S, Fabbri P. A case of chronic herpes gestationis: persistent disease or conversion to bullous pemphigoid? J Am Acad Dermatol. 2003;49:302–7. doi: 10.1067/s0190-9622(03)00412-2. [DOI] [PubMed] [Google Scholar]
- 17.Yip L, McCluskey J, Sinclair R. Immunological aspects of pregnancy. Clin Dermatol. 2006;24:84–7. doi: 10.1016/j.clindermatol.2005.10.022. [DOI] [PubMed] [Google Scholar]